Abstract
Introduction
The utility of kidney procurement biopsies is controversial. Understanding the current landscape of how clinicians obtain and use biopsies in organ evaluation may help inform consensus-building efforts.
Methods
An electronic survey was distributed to clinicians at US kidney transplant programs (April 22, 2021–June 30, 2021) to evaluate donor biopsy indications, frequency, processing and interpretation, and impact of findings on practices.
Results
Responses from staff involved in organ acceptance (73% surgeons, 20% nephrologists, 6% coordinators) at 95 transplant centers were analyzed, representing 40% of US transplant centers and 50% of recent deceased donor kidney transplant volume. More than a third of centers (35%) reported obtaining procurement biopsies on most-to-all kidneys. Most clinicians decided when to biopsy jointly with the Organ Procurement Organization (OPO) (82%) based on formal criteria for the decision (72%), although 41% reported having requested a biopsy outside of the criteria. Most respondents used a semiquantitative scoring system for interpretation (57%). Many respondents reported rarely or never having access to renal specialty pathologists (37%) or to telepathology (59%). Most respondents reported that a favorable biopsy result would encourage them to accept a "marginal" donor kidney (72%); nearly half (46%) indicated that an unfavorable biopsy result would lead to decline of a standard criteria kidney.
Conclusion
Procurement biopsies are commonly used in organ acceptance decisions despite inconsistent access to experienced renal pathologists and heterogeneous approaches to criteria, scoring, and interpretation. Ongoing study and consensus building are needed to direct procurement biopsy practice toward increasing organ utilization and reducing allocation inefficiency.
Keywords: biopsy, kidney donation, organ procurement, organ quality assessment, practice variation, surveys
Graphical abstract
Kidney procurement biopsies are commonly used as a component of the evaluation of organ quality before acceptance for transplantation. However, the reliability and predictive value of biopsy data are controversial.1 Currently, >50% of deceased donor kidneys recovered for transplant in the United States are biopsied.2 Despite extensive use of procurement biopsies, the value of the information provided is limited by poor intrareader reliability, poor reproducibility, inconsistent association with clinical outcomes, variable acceptance thresholds, and the potential for unnecessary biopsies that increase cold ischemic times and decrease organ acceptance.3, 4, 5, 6, 7, 8
Although the utility of procurement biopsies is increasingly in question, kidneys that undergo procurement biopsies remain 3 times more likely to be discarded.9 Importantly, this association is more pronounced in kidneys with lower kidney donor profile index (KDPI) scores than higher risk organs.2 Recent studies suggest that kidneys which have been biopsied and subsequently discarded may have benefited patients if transplanted in appropriate candidates.10 An evaluation of the outcomes of kidneys transplanted in biopsy-averse European centers with risk-matched discarded kidneys in the United States suggests that long-term survival and significant patient benefit could be achieved with transplantation of these “marginal” donor organs.10 Histologic findings from procurement biopsies have also been found to add little to graft survival prediction compared with clinical characteristics alone.10 Given the profound organ shortage and high waitlist mortality, particularly among older adults, strategies to avoid unnecessary kidney discard while preserving acceptable outcomes are vitally important.11, 12, 13, 14
In the context of the continued high use of procurement biopsies in the setting of known limitations, understanding contemporary attitudes and practices related to the use and interpretation of procurement biopsies at US transplant centers may help inform national discussions. To better understand the landscape of current practices, we designed and conducted an electronic survey of transplant professionals involved in kidney organ acceptance, querying their practices regarding pretransplant biopsy criteria, frequency, and modality, availability of renal specialty pathology services, and interpretation and use in organ acceptance decisions.
Methods
Survey Design
The survey instrument was developed by the study investigators. The final survey instrument comprised 30 questions addressing biopsy frequency, interpretation, and outcomes of interest. The survey also queried information on the respondent's role (nephrologist, transplant surgeon, clinical coordinator, social worker, administrator, or other) at the transplant center and participation in organ acceptance decisions. This study was approved by the Saint Louis University Institutional Review Board (protocol #30342).
Survey Administration and Target Population
The target population was staff at US adult kidney transplant programs, including surgeons, nephrologists, coordinators, and other staff. Potential participants from US kidney transplant programs were derived from the working group’s professional connections and an American Society of Transplant Surgeons e-mail list provided for survey use under a data use agreement. The survey was distributed, and data were collected, through Qualtrics Survey platform (Qualtrics, Provo, UT). Opportunity for self-elected participation through a Qualtrics link was also posted after approval to the American Society of Transplantation Kidney Pancreas Community of Practice listserv. Data are analyzed from distribution between April 22, 2021 to June 30, 2021. The first page of the survey notes that the decision to proceed indicates consent to participate. Up to 2 reminders were provided for nonrespondents.
Statistical Analysis
The primary analysis was limited to responses from clinicians and staff involved in organ offer acceptance. Each program was represented only once in the analysis. For programs with multiple respondents participating in offer evaluation, we selected a single participant to represent the program using a hierarchical algorithm that prioritized responses from surgeons, followed by nephrologists and then other staff, similar to previous methods.15, 16, 17, 18, 19, 20, 21, 22 In the case of multiple responses after that prioritization, we selected the earliest submitted questionnaire. All responses and responses by role were evaluated in secondary analyses. Respondents were allowed to enter free-text responses.
Responses to each survey question were described with percentages and frequencies. To obtain item response proportions, we divided the number of program responses by the total number of programs with responses to the question, such that percentages reflect proportions of programs. For questions where participants were asked to “select all that apply,” the denominator for calculating percentages was the number of programs with respondents to that question, as per previous methods.17,22 When assessing characteristics used to determine whether a biopsy was indicated, a characteristic was categorized as of low, medium, or high importance based on the percentage of respondents who selected this characteristic as a criterion (<25%, 25%–50%, or >50%, respectively). Volume of transplant practice represented by responding programs and volume-level stratifications were computed by center-level linkages to Scientific Registry of Transplant Recipients (SRTR) data. Average annual baseline volume was estimated from SRTR data in a 2-year period before the COVID-19 pandemic (January 1, 2019–January 1, 2021). All analyses were performed using SAS for Windows version 14 (SAS Institute, Inc., Cary, NC).
Results
Sample
A total of 189 survey responses were received. After removing responses from staff who do not participate in offer acceptance (n = 23) and restricting to 1 representative response per center, there were 95 respondents, including 69 transplant surgeons (73%), 19 transplant nephrologists (20%), 6 transplant coordinators (6%), and 1 advanced practice provider (1%). Respondents represented 40% of US transplant centers and 50% of recent deceased donor transplant volume. All United Network for Organ Sharing regions were represented in the analytical sample (Table 1).
Table 1.
Participant role and geographic representation (N = 95)
| Role in transplant program | % (n) |
|---|---|
| Transplant surgeon | 73 (69) |
| Transplant nephrologist | 20 (19) |
| Transplant coordinator | 6 (6) |
| Other | 1 (1) |
| UNOS region | |
|---|---|
| 1 | 5 (5) |
| 2 | 7 (7) |
| 3 | 15 (14) |
| 4 | 22 (21) |
| 5 | 15 (14) |
| 6 | 3 (3) |
| 7 | 4 (4) |
| 8 | 7 (7) |
| 9 | 7 (7) |
| 10 | 6 (6) |
| 11 | 7 (7) |
UNOS, United Network for Organ Sharing.
Biopsy Frequency and Indications
Regarding frequency of biopsy use, 35% of the respondents indicated that biopsies were performed in most of the kidneys evaluated for transplant at their center, whereas 29% indicated that fewer than 25% of donor kidneys were biopsied (Table 2). The decision to perform a procurement biopsy was shared between the OPO and the transplant center in 82% of the centers. When the decision was unilateral, the choice was more commonly driven by the transplant center (13% center only vs. 4% OPO only).
Table 2.
Biopsy frequency, type, and decision to perform
| On what proportion of deceased donor kidneys evaluated for transplant by your center is a procurement biopsy performed? (N = 95) | % (n) |
|---|---|
| <10% | 5 (5) |
| 10 to <25% | 24 (23) |
| 25 to <50% | 35 (33) |
| 50 to <75% | 28 (27) |
| ≥75% | 7 (7) |
| What would you estimate is the relative influence of your transplant center vs. OPO on the decision to biopsy kidney offers evaluated at your center? (N = 94) | % (n) |
|---|---|
| 100% Transplant center | 13 (12) |
| 75% Transplant center/25% OPO | 24 (23) |
| 50% Transplant center/50% OPO | 34 (32) |
| 25% Transplant center/75% OPO | 24 (23) |
| 100% OPO | 4 (4) |
| Which of the following best describes your center’s approach to deciding when to request a kidney procurement biopsy? (N = 95) | % (n) |
|---|---|
| We request a biopsy of most-to-all kidneys considered for transplant | 20 (19) |
| We selectively request biopsy, based on donor characteristics | 71 (67) |
| We rely on the OPO policy/practice to determine the need for a procurement biopsy | 9 (9) |
| We almost never request a procurement biopsy and prefer to rely on clinical characteristics | 0 (0) |
| Does your center have a formal set of criteria for deciding when to perform a kidney procurement biopsy? (N= 94) | % (n) |
|---|---|
| Yes, and only kidneys that meet these criteria are biopsied | 31 (29) |
| Yes, but the clinician reviewing the offer can request a biopsy outside of criteria | 41 (39) |
| No, the decision to biopsy is made without reference to formal criteria | 28 (26) |
| What percentage of procurement biopsies for kidneys evaluated at your center are needle core vs wedge biopsies? (N = 94) | % (n) |
|---|---|
| 100% Needle core | 10 (9) |
| 75% Needle core/25% wedge | 11 (10) |
| 50% Needle core/50% wedge | 23 (22) |
| 25% Needle core/75% wedge | 22 (21) |
| 100% Wedge | 34 (32) |
| What percentage of procurement biopsies for kidneys evaluated at your center are processed as frozen section vs. permanent section? (N = 92) | % (n) |
|---|---|
| 100% Frozen section | 47 (43) |
| 75% Frozen section/25% permanent section | 10 (9) |
| 50% Frozen section/50% permanent section | 13 (12) |
| 25% Frozen section/75% permanent section | 21 (19) |
| 100% Permanent section | 10 (9) |
OPO, Organ Procurement Organization.
N = the item denominator, based on number of respondents.
Formal criteria for determining need for biopsy were used at 72% of responding centers, although only 31% reported biopsy determinations being restricted to these criteria (Table 2). Among the respondents who reported having established center criteria to determine the need for biopsy, only 3 donor characteristics—donor age, donor history of diabetes mellitus, and acute kidney injury (AKI)—were identified by most of the respondents as indications for biopsy (Table 3).
Table 3.
Criteria used to determine whether a kidney is selected to undergo procurement biopsy
| Low importance (<25%) | Medium importance (25%–50%) | High importance (>50%) |
|---|---|---|
| COD: CVA (23%) | Hypertension (48%) | Age (65%) |
| Kidney size discrepancy (23%) | High terminal creatinine (48%) | Acute kidney injury (56%) |
| HCV seropositivity (21%) | High KDPI (47%) | Diabetes (51%) |
| Hematuria (21%) | DIC (43%) | |
| COD: trauma (19%) | DCD status (43%) | |
| eGFR (17%) | High peak creatinine (42%) | |
| Substance use (17%) | ECD classification (41%) | |
| BMI (16%) | Proteinuria (40%) | |
| Sex (14%) | ||
| History of smoking (14%) | ||
| Pulsatile perfusion (13%) | ||
| Import kidney (11%) | ||
| History of malignancy (9%) | ||
| High cold ischemia time (7%) | ||
| Vasopressor use (6%) |
BMI, body mass index; COD, cause of death; CVA, cerebrovascular accident; DCD, donation after cardiac death; DIC, disseminated intravascular coagulation; ECD, expanded criteria donor; eGFR, estimated glomerular filtration rate; HCV, hepatitis C virus; KDPI, Kidney Donor Profile Index.
Importance is assigned by response rate; for example, <25% of respondents selecting a single criterion as an indication for biopsy is categorized as low importance.
Biopsy Type and Interpretation
Most respondents reported obtaining tissue samples via wedge biopsy (56% mostly wedge; 21% mostly core needle), and 44% reported processed samples using both immediate frozen section and delayed permanent section (Table 2). Just more than half of the respondents (57%) preferred to use a scoring system, most commonly the Remuzzi score (21%) and Maryland Aggregate Pathology Index (MAPI) (21%), to interpret the biopsy (Table 4). Of the histologic components examined on the biopsy, the respondents most frequently ranked arteriosclerosis (45%) and glomerulosclerosis (GS) (40%) as highly important, followed by interstitial fibrosis and tubular atrophy (IFTA, 37%) and arterial hyalinosis (25%) (Table 5).
Table 4.
Reported decision-making based on biopsy findings and willingness to accept risk based on histologic pathology
| When examining a procurement biopsy, which of the following scoring systems are used at your center? (N =95) | % (n) |
|---|---|
| Remuzzi score | 21 (20) |
| Donor Chronic Disease Score (DCDS) | 14 (13) |
| Maryland Aggregate Pathology Index (MAPI) | 21 (20) |
| Chronic Allograft Damage Score (CDI) | 7 (7) |
| Other | 3 (3) |
| We do not use any scoring system in evaluating biopsies | 43 (41) |
| In general, how do biopsies typically affect your acceptance decisions for kidneys with marginal clinical characteristics or donor risk factors? (N =95) | % (n) |
|---|---|
| A “good” biopsy will often persuade me to transplant a kidney I would consider marginal based on clinical characteristics alone | 72 (68) |
| A “bad” biopsy will often persuade me to decline a kidney with clinical risk factors (e.g., high KDPI) | 63 (60) |
| I obtain the biopsy for extra information but most commonly rely on clinical characteristics for acceptance decisions | 22 (21) |
| Other | 4 (4) |
| In general, how do biopsies typically affect your acceptance decisions for standard criteria kidneys? (N =95) | % (n) |
|---|---|
| A “good biopsy will often persuade me to transplant a standard criteria kidney | 43 (41) |
| A “bad” biopsy will often persuade me to decline a standard criteria kidney | 46 (44) |
| I obtain the biopsy for extra information but most commonly rely on clinical characteristics for acceptance decisions | 37 (35) |
| Other | 7 (7) |
| How do fibrin thrombi on a biopsy of an otherwise transplantable kidney impact your acceptance decision? (N =95) | % (n) |
|---|---|
| No influence | 19 (18) |
| If diffuse, likely to decline | 63 (60) |
| If limited, likely to decline | 20 (19) |
| If any present, likely to decline | 13 (12) |
KDPI, kidney donor profile index.
N = the item denominator, based on number of respondents. Participants were asked to “select all that apply”; thus, column totals may exceed 100%.
Table 5.
Relative importance of histologic pathology findings and considerations in decision-making
| How do you rate the importance of each of the following biopsy characteristics in considering a kidney for transplant? | % (n) |
|---|---|
| Glomerulosclerosis (N = 89) | |
| Highly important | 40 (36) |
| Important | 56 (50) |
| Not important | 3 (3) |
| Do not know | 0 (0) |
| Arteriosclerosis (N = 95) | |
| Highly important | 45 (43) |
| Important | 49 (47) |
| Not important | 4 (4) |
| Do not know | 1 (1) |
| Arterial hyalinosis (N = 95) | |
| Highly important | 25 (24) |
| Important | 59 (56) |
| Not important | 12 (11) |
| Do not know | 4 (4) |
| Interstitial fibrosis/tubular atrophy (N = 95) | |
| Highly important | 37 (35) |
| Important | 52 (49) |
| Not important | 9 (9) |
| Do not know | 2 (2) |
| When accepting a kidney for your patient, how important are each of the following considerations? | % (n) |
|---|---|
| Reducing waiting time/increasing transplant rate (N = 91) | |
| Very/most important | 65 (59) |
| Somewhat important | 32 (29) |
| Not important | 3 (3) |
| Increasing long-term graft survival (N = 91) | |
| Very/most important | 77 (70) |
| Somewhat important | 22 (20) |
| Not important | 1 (1) |
| Avoiding early transplant complications (e.g., delayed graft function, readmissions; N = 90) | |
| Very/most important | 39 (35) |
| Somewhat important | 53 (48) |
| Not important | 8 (7) |
| Minimizing immunosuppression through better organ matching (N = 90) | |
| Very/most important | 31 (28) |
| Somewhat important | 47 (42) |
| Not important | 22 (20) |
| Other (N = 12) | |
| Very/most important | 58 (7) |
| Somewhat important | 25 (3) |
| Not important | 17 (2) |
N = the item denominator, based on number of respondents.
The severity of senescent lesions that clinicians found acceptable showed trends of variation by the biopsy technique. Clinicians who more commonly used wedge biopsy samples for analysis tended to be more willing to accept high degrees of GS and IFTA but less willing to accept high degrees of arteriosclerosis (Supplementary Table S1). Among respondents who reported that most (≥75%) of their biopsy samples were wedge biopsies, willingness to accept severe GS (>20%) was 23%, compared with 16% among those who reported that most of their biopsies were needle core samples. Furthermore, only 8% of mostly wedge biopsy users were willing to accept severe arteriolosclerosis (vs. 17% of mostly needle core biopsy users), whereas acceptance of severe IFTA was similar between groups (4% of high users of wedge biopsies vs. 6% of high users of needle core biopsies).
Pathology Availability and Ability to Obtain Second Opinions
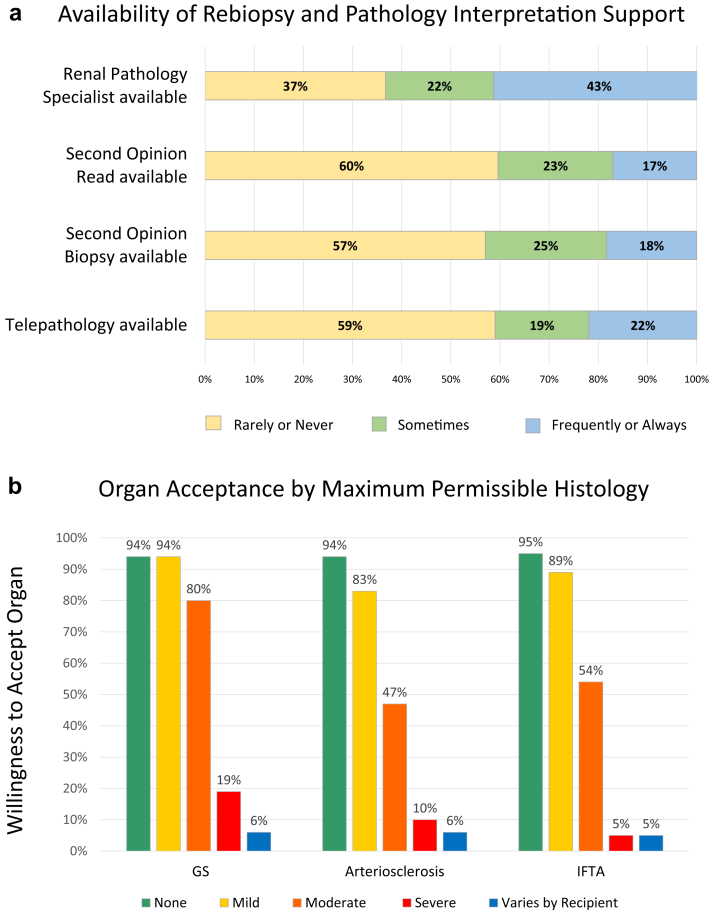
Only 43% of the respondents reported that a renal pathology specialist (RPS) was frequently or always available, whereas 37% reported that such a specialist was rarely or never available (Figure 1a). Imported kidneys were infrequently rebiopsied or reread by pathology for a second opinion, with 57% of the respondents reporting that a repeat biopsy was rarely to never available and 60% reporting that a second opinion pathology read was rarely to never available (Figure 1a). Clinicians reported that telepathology for the purposes of biopsy viewing and reading was seldom available, with most (78%) reporting having access to this service in fewer than half of the cases (Figure 1a).
Figure 1.
Availability of renal pathology specialists, telepathology, and second opinions. (a) Reported willingness to accept organs based on histologic pathology. (b) Levels of disease defined as follows: GS: mild, 0% to 10%; moderate, >10% to 20%; severe, >20%; arterial disease/IFTA: by reading pathologist designation. GS, glomerulosclerosis; IFTA, interstitial fibrosis and tubular atrophy.
Access to an RPS did not significantly change acceptance patterns (Supplementary Table S2). Among respondents who reported they had access to an RPS, most of the time they tended to be slightly less willing to accept severe GS (17% of those with high RPS access vs. 21% with low RPS access willing to accept) but had similar tolerance of severe arteriosclerosis (12% of those with high RPS access vs. 10% with low RPS access) and IFTA (5% of those with high RPS access vs. 7% with low RPS access).
Risk Acceptance
Respondents reported decreasing likelihood of organ acceptance as degree of histologic pathology detected on biopsy rose; the cumulative sum of respondents willing to accept a given grade (mild, moderate, severe) of GS, AS, and IFTA is shown in Figure 1b. Despite finding GS to be highly important, almost a fifth of the respondents (19%) indicated that they would be willing to accept a kidney with >20% GS in some cases. However, few would accept organs in which the biopsy result showed severe arteriosclerosis (10%) or IFTA (5%). Most clinicians (81%) additionally found fibrin thrombi to be an indication to decline (Table 4), although most of these (63%) would only decline for diffuse fibrin thrombi.
When evaluating a “marginal” kidney, more than half of the respondents (63%) felt that a “bad” biopsy would influence them to decline the organ (Table 4). Conversely, most respondents (72%) expressed that a “good” biopsy would persuade them to transplant a kidney with other concerning risk factors. When evaluating a standard criteria kidney, fewer than half felt that a good biopsy would prevent decline (43%) or that a bad biopsy would encourage decline (46%) (Table 4).
Outcomes of Interest in Donor Kidney Evaluation
When considering which outcome measures were most important in evaluating a kidney for transplantation, most respondents considered long-term graft survival (77%) and reducing waiting time (65%) as highly important (Table 5). Fewer than half considered avoidance of early post-transplant complications, such as readmissions or delayed graft function (39%), to be highly important, and fewer still valued better organ matching (31%).
Free-Text Responses
The free-text responses to the survey questions are tabulated in Supplementary Table S3. As noted previously (Table 3), the most common indications for obtaining a procurement biopsy were donor age, diabetes mellitus, and AKI; within these indications, the respondents most commonly endorsed obtaining biopsy at threshold donor ages of 50 or 60 years, with a diabetes duration of at least 5 or 10 years, or with a terminal creatinine of 2.0 mg/dL and above. A KDPI of 85% was the most commonly cited KDPI threshold for biopsy. Among reasons for obtaining a repeat biopsy on an imported kidney, the respondents most commonly were prompted by insufficient biopsy sample and biopsy discordance with clinical history.
Discussion
In a national survey of US kidney transplant centers, we found that deceased donor kidney procurement biopsies are commonly requested and used, with more than a third of programs electing to biopsy most of the kidneys evaluated for implantation despite recent data demonstrating poor correlation between biopsy findings and allograft outcomes. Furthermore, the decision to biopsy is driven jointly by transplant clinicians and OPOs. Most respondents indicate that the biopsy findings influence their clinical decision-making, as nearly half reported that they would decline an organ from an otherwise standard criteria donor for severe pathology on the biopsy.
Although the procurement biopsy is commonly used, data derived from frozen section procurement biopsies appear to be a poor predictor of outcomes.23 Our study identified unwillingness to accept severe GS in more than 80% of the respondents, and even more clinicians indicated that they would decline an organ if a biopsy demonstrated severe arteriosclerosis (90%) or IFTA (95%). However, multiple studies have reported that the information provided by the procurement biopsy is subject both to sampling error3,4 and poor interobserver agreement3,5,6 on the degree of senescent lesions. This variability limits the utility of frozen section biopsy results as an adjunct to clinical characteristics. In addition, differences in biopsy findings may not accurately prognosticate graft outcomes. A systematic review demonstrated that graft failure risk based on the biopsy components varies by study, with no consistent impact noted for any lesion.7 Multivariable analysis designed to isolate the impact of each lesion separately found that these findings lose significance when controlled for clinical variables, such as donor age.24,25 Although it must be acknowledged that the outcome of grafts which are not transplanted as a result of biopsy results (“true positives”) is not known, comparison to outcomes from similar organs transplanted in Europe (where biopsy results are not available before transplant) suggests that many of these organs would provide benefit if transplanted.10
To improve the correlation of biopsy findings with outcomes, multiple semiquantitative scoring systems have been developed, including the Remuzzi score,26 the MAPI,27 and the Donor Chronic Damage Score.28 In our study, we found that just more than half of the respondents reported using a scoring system to evaluate biopsies, most commonly the MAPI and Remuzzi scores. Data on the utility of these systems are slightly more promising than on the utility of biopsy results alone, but results are still mixed. Although a significant association with graft failure has been reported for the Remuzzi29,30 and MAPI31 scores, the c-statistic is low for the more commonly used Remuzzi score (0.59) and only acceptable for the MAPI (0.81).32 In addition, calculation of these scores is logistically challenging: the Remuzzi score heavily weights IFTA, which is difficult to assess on a frozen section procurement biopsy33; and the MAPI comprises multiple variables—including GS, arterial hyalinosis, Banff criteria, cortical scarring, and periglomerular fibrosis—assessment of which may be challenging to an on-call or non-RPS. Therefore, even if a designated scoring system is confirmed to be reliable and reproducible, its broad use to guide organ acceptance in practice will remain challenging.
With or without the use of a scoring system, the use of an on-call pathologist or a non-RPS further decreases the correlation of biopsy findings with outcomes.4,5 Previous studies have shown that reading by an RPS was associated with improved correlation of biopsy scoring and 12-month kidney function.5 We found that almost 60% of the respondents do not have frequent access to this vital expertise, possibly contributing to the poor correlation between biopsy results with subsequent outcomes.23 Similarly, when responding regarding their ability to request that the biopsy be reread for a second opinion—presumably because of a lack of confidence or poor clinical correlation with the original interpretation—60% reported rarely or never having access to a second read. Interestingly, respondents who reported good RPS access were slightly more risk averse when considering kidneys with significant GS. Respondents’ ability to use the biopsy findings in organ acceptance decisions may be compromised by a lack of access to trained RPSs. Telepathology has emerged as a way to provide renal pathology expertise to programs that may not otherwise have access to specialized pathologic readings and has been validated as a reliable tool to transmit images.34 Currently, less than a quarter of respondents reported consistent access to telepathology, indicating this tool may be only partially effective at addressing the need for RPSs for those clinicians who choose to biopsy.
In our analysis, some modest differences in risk acceptance were noted between clinicians who preferentially used wedge biopsies and those who used more needle core biopsies: providers who worked with wedge biopsies tended to be more likely to accept severe GS and less likely to accept severe arteriosclerosis. Differences in behavior may be somewhat attributable to the inherent sampling differences, as subcapsular wedge biopsies tend to more clearly display scarring and GS, and core needle biopsies tend to demonstrate more arterial pathology.35 Clinicians who have seen otherwise “good” kidneys with more of either finding may place a lower relative importance on the component’s impact on graft outcomes. Alternatively, other factors including local practice in areas with aggressive transplant programs may explain this association. As prior reports have demonstrated poor concordance of either type of frozen section procurement biopsy (wedge or needle) with gold-standard postreperfusion biopsies evaluated by trained RPSs after permanent fixation, it is not clear that either method of frozen section biopsy is superior.5
The controversies surrounding the use of procurement biopsies are compounded by the lack of consensus regarding which kidneys should be biopsied. Recent guidance from the Organ Procurement and Transplantation Network (OPTN)/United Network for Organ Sharing suggests that biopsy information should be provided for kidneys from donors with a KDPI > 85% or with a significant history of hypertension, diabetes, or AKI.36 In our survey, approximately half of transplant clinicians reported requesting a biopsy based on any of these indications (47%, 48%, 51%, and 56%, respectively). As recently surveyed by Emmons et al.37 OPOs are somewhat more likely to use these criteria as indications for biopsy (63%, 63%, 60%, and 40%, respectively). As the presence of advanced age, diabetes, and hypertension are highly correlated with senescent lesions on the procurement biopsy,24,25 the heterogeneity in practice may result from beliefs of some clinicians that the histologic findings will not add value to the clinical data.
OPO reluctance to perform biopsies for kidneys outside of recommended guidelines or policies may reflect concerns that the biopsy may lead to inappropriate discard of an otherwise clinically acceptable kidney, whether owing to the histology or the additional cold time necessary to process and read the biopsy. Furthermore, studies of accepted mate kidneys with discordant histology have shown similar graft survival within the kidney pairs despite the histologic differences, suggesting the biopsy results did not impact survival and that discard would have been unnecessary in these cases.38 However, the biopsy was impactful to many of the survey respondents: >60% of respondents reported that they would decline a marginal kidney and 46% that they would decline a standard criteria kidney with “bad” histology. The standard criteria donor responses are consistent with a case-based study39 wherein respondents were provided with a variety of simulated organ offers accompanied by no biopsy, a “poor” biopsy, or a “good” biopsy. The odds of declining an otherwise acceptable kidney from a donor with low serum creatinine but with a “bad” biopsy were 2.5 times that faced by a similar kidney with a “good” biopsy; 31% of the respondents reported that the biopsy prompted them to decline in this situation.39 Similarly, in a national US registry analysis, Lentine et al.2 found that low-KDPI (<20%) donor organs which were biopsied were >6 times (odds ratio, 6.47) as likely to be discarded as kidneys that were not biopsied.2 However, that study suggested that the independent impact of the biopsy on discard rates was not significant in donors with a KDPI >85%,2 contrary to the beliefs of our respondents.2 Reducing the use of biopsies in standard kidneys represents a target for interventions to improve kidney utilization, and further consensus is needed to create consistent biopsy practice and reduce organ discard. Conversely, almost 3 in 4 respondents reported that “good” histology would make them likely to transplant a kidney from a donor with marginal clinical characteristics, suggesting the ability to obtain biopsy results in these scenarios potentially encourages acceptance of organs that might otherwise be discarded. However, additional study is needed to determine whether the inability to assess the histology of kidneys from “marginal” donors would indeed lead to a greater likelihood of discard.
Our study has limitations inherent to the survey study design, such as potential for recall bias. The findings represent practices as they are reported; we cannot verify how accurately the reports represent actual practice at each program. Respondents were identified by online outreach to US transplant professionals, and not all programs are represented. However, the 40% response rate is higher than many contemporary studies of transplant program practices (where response rates in the 30% range are common),20,21,40 likely reflecting the strong community interest in the topic, and the responding centers represent 50% of deceased donor kidney transplant volume. These survey data reflect the opinions and experiences of the respondents at the time of completion, and given the rapidly dynamic nature of transplant practice and evolving discussions of this topic, current responses may not be reflective of future practice. However, these data provide a contemporary assessment of clinician-reported procurement biopsy practice in the United States and offer a benchmark for comparing community opinions as biopsy practice guidelines evolve over time.
In conclusion, clinicians endorse continued, frequent use of the procurement biopsy despite lack consensus on biopsy indications or adherence to formal criteria. Access to both RPSs and telepathology remains limited. Despite the poor reliability of biopsy data, transplant clinicians continue to routinely incorporate the biopsy results into their decision-making. This information is particularly salient as the OPTN seeks to establish minimum donor criteria to require biopsy.41 Ongoing study is needed to better determine the optimal approach to the indications for biopsy, type of biopsy performed, and interpretation of the pathologic findings to productively support organ acceptance decisions that positively improve patient outcomes.
Disclosure
KLL, MAS, and DAA receive consulting fees from CareDx. KLL receives speaker honoraria from Sanofi. All the other authors declared no competing interests.
Acknowledgments
The authors thank survey respondents, including members of the American Society of Transplant Surgeons (ASTS) and the American Society of Transplantation Kidney Pancreas Community of Practice. Survey distribution to the members of the ASTS was conducted with an approved data use agreement. The authors also thank Saint Louis University Biostatisticians Ruixin Li, MS, and Huiling Xiao, MS, for manuscript preparation support. Portions of this work were accepted for presentation at the American Transplant Congress 2022 (Boston, MA).
This work was supported by a grant from the Mid-America Transplant Foundation. KLL is supported by the Mid-America Transplant/Jane A. Beckman Endowed Chair in Transplantation.
Footnotes
Table S1. Thresholds of suboptimal procurement biopsy finding acceptance by biopsy modality.
Table S2. Thresholds of suboptimal procurement biopsy finding acceptance by access to renal pathology specialists.
Table S3. Free-text responses.
Supplementary Material
Table S1. Thresholds of suboptimal procurement biopsy finding acceptance by biopsy modality.
Table S2. Thresholds of suboptimal procurement biopsy finding acceptance by access to renal pathology specialists.
Table S3. Free-text responses.
References
- 1.Lentine K.L., Kasiske B., Axelrod D.A. Procurement biopsies in kidney transplantation: More information may not lead to better decisions. J Am Soc Nephrol. 2021;32:1835–1837. doi: 10.1681/ASN.2021030403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lentine K.L., Naik A.S., Schnitzler M.A., et al. Variation in use of procurement biopsies and its implications for discard of deceased donor kidneys recovered for transplantation. Am J Transplant. 2019;19:2241–2251. doi: 10.1111/ajt.15325. [DOI] [PubMed] [Google Scholar]
- 3.Bröcker V., Schubert V., Scheffner I., et al. Arteriolar lesions in renal transplant biopsies: prevalence, progression, and clinical significance. Am J Pathol. 2012;180:1852–1862. doi: 10.1016/j.ajpath.2012.01.038. [DOI] [PubMed] [Google Scholar]
- 4.Girolami I., Gambaro G., Ghimenton C., et al. Pre-implantation kidney biopsy: value of the expertise in determining histological score and comparison with the whole organ on a series of discarded kidneys. J Nephrol. 2020;33:167–176. doi: 10.1007/s40620-019-00638-7. [DOI] [PubMed] [Google Scholar]
- 5.Azancot M.A., Moreso F., Salcedo M., et al. The reproducibility and predictive value on outcome of renal biopsies from expanded criteria donors. Kidney Int. 2014;85:1161–1168. doi: 10.1038/ki.2013.461. [DOI] [PubMed] [Google Scholar]
- 6.Liapis H., Gaut J.P., Klein C., et al. Banff histopathological consensus criteria for preimplantation kidney biopsies. Am J Transplant. 2017;17:140–150. doi: 10.1111/ajt.13929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C.J., Wetmore J.B., Crary G.S., Kasiske B.L. The donor kidney biopsy and its implications in predicting graft outcomes: a systematic review. Am J Transplant. 2015;15:1903–1914. doi: 10.1111/ajt.13213. [DOI] [PubMed] [Google Scholar]
- 8.Husain S.A., King K.L., Batal I., et al. Reproducibility of deceased donor kidney procurement biopsies. Clin J Am Soc Nephrol. 2020;15:257–264. doi: 10.2215/CJN.09170819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohan S., Chiles M.C., Patzer R.E., et al. Factors leading to the discard of deceased donor kidneys in the United States. Kidney Int. 2018;94:187–198. doi: 10.1016/j.kint.2018.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reese P.P., Aubert O., Naesens M., et al. Assessment of the utility of kidney histology as a basis for discarding organs in the United States: a comparison of international transplant practices and outcomes. J Am Soc Nephrol. 2021;32:397–409. doi: 10.1681/ASN.2020040464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hart A., Lentine K.L., Smith J.M., et al. OPTN/SRTR 2019 annual data report: kidney. Am J Transplant. 2021;21(suppl 2):21–137. doi: 10.1111/ajt.16502. [DOI] [PubMed] [Google Scholar]
- 12.Schold J., Srinivas T.R., Sehgal A.R., Meier-Kriesche H.U. Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin J Am Soc Nephrol. 2009;4:1239–1245. doi: 10.2215/CJN.01280209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stock P.G., Lentine K.L. Maximizing the use of hard to place kidneys: getting the right kidney to the right recipient at the right time. Am J Transplant. 2021;21:3516–3518. doi: 10.1111/ajt.16771. [DOI] [PubMed] [Google Scholar]
- 14.Lentine K.L., Pastan S., Mohan S., et al. A roadmap for innovation to advance transplant access and outcomes: a position statement from the National Kidney Foundation. Am J Kidney Dis. 2021;78:319–332. doi: 10.1053/j.ajkd.2021.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Doshi M.D., Singh N., Hippen B.E., et al. Transplant clinician opinions on use of race in the estimation of glomerular filtration rate. Clin J Am Soc Nephrol. 2021;16:1552–1559. doi: 10.2215/CJN.05490421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lentine K.L., Motter J.D., Henderson M.L., et al. Care of international living kidney donor candidates in the United States: a survey of contemporary experience, practice, and challenges. Clin Transpl. 2020;34 doi: 10.1111/ctr.14064. [DOI] [PubMed] [Google Scholar]
- 17.Lentine K.L., Peipert J.D., Alhamad T., et al. Survey of clinician opinions on kidney transplantation from hepatitis C virus positive donors: identifying and overcoming barriers. Kidney360. 2020;1:1291–1299. doi: 10.34067/KID.0004592020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lentine K.L., Vest L.S., Schnitzler M.A., et al. Survey of US living kidney donation and transplantation practices in the COVID-19 era. Kidney Int Rep. 2020;5:1894–1905. doi: 10.1016/j.ekir.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alhamad T., Lubetzky M., Lentine K.L., et al. Kidney recipients with allograft failure, transition of kidney care (KRAFT): a survey of contemporary practices of transplant providers. Am J Transplant. 2021;21:3034–3042. doi: 10.1111/ajt.16523. [DOI] [PubMed] [Google Scholar]
- 20.Garg N., Lentine K.L., Inker L.A., et al. Metabolic, cardiovascular, and substance use evaluation of living kidney donor candidates: US practices in 2017. Am J Transplant. 2020;20:3390–3400. doi: 10.1111/ajt.15964. [DOI] [PubMed] [Google Scholar]
- 21.Garg N., Lentine K.L., Inker L.A., et al. The kidney evaluation of living kidney donor candidates: US practices in 2017. Am J Transplant. 2020;20:3379–3389. doi: 10.1111/ajt.15951. [DOI] [PubMed] [Google Scholar]
- 22.Axelrod D.A., Ince D., Harhay M.N., et al. Operational challenges in the COVID-19 era: asymptomatic infections and vaccination timing. Clin Transpl. 2021;35 doi: 10.1111/ctr.14437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carpenter D., Husain S.A., Brennan C., et al. Procurement biopsies in the evaluation of deceased donor kidneys. Clin J Am Soc Nephrol. 2018;13:1876–1885. doi: 10.2215/CJN.04150418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Traynor C., Saeed A., O’Ceallaigh E., et al. Pre-transplant histology does not improve prediction of 5-year kidney allograft outcomes above and beyond clinical parameters. Ren Fail. 2017;39:671–677. doi: 10.1080/0886022X.2017.1363778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arias L.F., Blanco J., Sanchez-Fructuoso A., et al. Histologic assessment of donor kidneys and graft outcome: multivariate analyses. Transplant Proc. 2007;39:1368–1370. doi: 10.1016/j.transproceed.2007.01.085. [DOI] [PubMed] [Google Scholar]
- 26.Remuzzi G., Cravedi P., Perna A., et al. Long-term outcome of renal transplantation from older donors. N Engl J Med. 2006;354:343–352. doi: 10.1056/NEJMoa052891. [DOI] [PubMed] [Google Scholar]
- 27.Philosophe B., Malat G.E., Soundararajan S., et al. Validation of the Maryland Aggregate Pathology Index (MAPI), a pre-implantation scoring system that predicts graft outcome. Clin Transplant. 2014;28:897–905. doi: 10.1111/ctr.12400. [DOI] [PubMed] [Google Scholar]
- 28.Lopes J.A., Moreso F., Riera L., et al. Evaluation of pre-implantation kidney biopsies: comparison of Banff criteria to a morphometric approach. Kidney Int. 2005;67:1595–1600. doi: 10.1111/j.1523-1755.2005.00241.x. [DOI] [PubMed] [Google Scholar]
- 29.Losappio V., Stallone G., Infante B., et al. A single-center cohort study to define the role of pretransplant biopsy score in the long-term outcome of kidney transplantation. Transplantation. 2014;97:934–939. doi: 10.1097/01.TP.0000438208.50089.29. [DOI] [PubMed] [Google Scholar]
- 30.De Vusser K., Lerut E., Kuypers D., et al. The predictive value of kidney allograft baseline biopsies for long-term graft survival. J Am Soc Nephrol. 2013;24:1913–1923. doi: 10.1681/ASN.2012111081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Munivenkatappa R.B., Schweitzer E.J., Papadimitriou J.C., et al. The Maryland aggregate pathology index: a deceased donor kidney biopsy scoring system for predicting graft failure. Am J Transplant. 2008;8:2316–2324. doi: 10.1111/j.1600-6143.2008.02370.x. [DOI] [PubMed] [Google Scholar]
- 32.Jackson K.R., Munivenkatappa R.B., Wesson R.N., Garonzik-Wang J., Massie A., Philosophe B. What’s the score? A comparison of deceased donor kidney scoring systems and correlation with graft outcome. Clin Transplant. 2020;34 doi: 10.1111/ctr.13802. [DOI] [PubMed] [Google Scholar]
- 33.Lehtonen S.R., Taskinen E.I., Isoniemi H.M. Histopathological findings in renal allografts at time of transplantation and correlation with onset of graft function. APMIS. 1999;107:945–950. doi: 10.1111/j.1699-0463.1999.tb01495.x. [DOI] [PubMed] [Google Scholar]
- 34.Girolami I., Parwani A., Barresi V., et al. The landscape of digital pathology in transplantation: from the beginning to the virtual E-slide. J Pathol Inform. 2019;10:21. doi: 10.4103/jpi.jpi_27_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Husain S.A., Shah V., Alvarado Verduzco H., et al. Impact of deceased donor kidney procurement biopsy technique on histologic accuracy. Kidney Int Rep. 2020;5:1906–1913. doi: 10.1016/j.ekir.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Organ Procurement and Transplantation Network Guidance on requested deceased donor information. Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/media/2504/opo_guidance_201806.pdf
- 37.Emmons B.R., Husain S.A., King K.L., Adler J.T., Mohan S. Variations in deceased donor kidney procurement biopsy practice patterns: a survey of US organ procurement organizations. Clin Transplant. 2021;35 doi: 10.1111/ctr.14411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Husain S.A., King K.L., Coley S., Natarajan K., Perotte A., Mohan S. Association between procurement biopsy findings and deceased donor kidney outcomes: a paired kidney analysis. Transpl Int. 2021;34:1239–1250. doi: 10.1111/tri.13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stewart D., Shepard B., Rosendale J., et al. Can behavioral research improve transplant decision-making? A mock offer study on the role of kidney procurement biopsies. Kidney360. 2020;1:36. doi: 10.34067/KID.0000212019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mandelbrot D.A., Fleishman A., Rodrigue J.R., et al. Practices in the evaluation of potential kidney transplant recipients who are elderly: A survey of US transplant centers. Clin Transpl. 2017;31 doi: 10.1111/ctr.13088. [DOI] [PubMed] [Google Scholar]
- 41.Organ Procurement and Transplantation Network (OPTN) Establish minimum kidney donor criteria to require biopsy. Organ Procurement and Transplantation Network (OPTN) https://optn.transplant.hrsa.gov/policies-bylaws/public-comment/establish-minimum-kidney-donor-criteria-to-require-biopsy/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.