Abstract
Objective
To assess recent trends in age adjusted mortality rates (AAMRs) in the United States based on county level presidential voting patterns.
Design
Cross sectional study.
Setting
USA, 2001-19.
Participants
99.8% of the US population.
Main outcome measures
AAMR per 100 000 population and average annual percentage change (APC).
Methods
The Centers for Disease Control and Prevention WONDER database was linked to county level data on US presidential elections. County political environment was classified as either Democratic or Republican for the four years that followed a November presidential election. Additional sensitivity analyses analyzed AAMR trends for counties that voted only for one party throughout the study, and county level gubernatorial election results and state level AAMR trends. Joinpoint analysis was used to assess for an inflection point in APC trends.
Results
The study period covered five presidential elections from 2000 to 2019. From 2001 to 2019, the AAMR per 100 000 population decreased by 22% in Democratic counties, from 850.3 to 664.0 (average APC −1.4%, 95% confidence interval −1.5% to −1.2%), but by only 11% in Republican counties, from 867.0 to 771.1 (average APC −0.7%, −0.9% to −0.5%). The gap in AAMR between Democratic and Republican counties therefore widened from 16.7 (95% confidence interval 16.6 to 16.8) to 107.1 (106.5 to 107.7). Statistically significant inflection points in APC occurred for Democratic counties between periods 2001-09 (APC −2.1%, −2.3% to −1.9%) and 2009-19 (APC −0.8%, −1.0% to −0.6%). For Republican counties between 2001 and 2008 the APC was −1.4% (−1.8% to −1.0%), slowing to near zero between 2008 and 2019 (APC −0.2%, −0.4% to 0.0%). Male and female residents of Democratic counties experienced both lower AAMR and twice the relative decrease in AAMR than did those in Republican counties. Black Americans experienced largely similar improvement in AAMR in both Democratic and Republican counties. However, the AAMR gap between white residents in Democratic versus Republican counties increased fourfold, from 24.7 (95% confidence interval 24.6 to 24.8) to 101.3 (101.0 to 101.6). Rural Republican counties experienced the highest AAMR and the least improvement. All trends were similar when comparing counties that did not switch political environment throughout the period and when gubernatorial election results were used. The greatest contributors to the widening AAMR gap between Republican and Democratic counties were heart disease (difference in AAMRs 27.6), cancer (17.3), and chronic lower respiratory tract diseases (8.3), followed by unintentional injuries (3.3) and suicide (3.0).
Conclusion
The mortality gap in Republican voting counties compared with Democratic voting counties has grown over time, especially for white populations, and that gap began to widen after 2008.
Introduction
Health outcomes such as mortality rates vary considerably among different groups and populations in the United States. Inequalities in mortality exist between people of different sexes, races, and ethnicities, and more recent work has highlighted widening gaps between urban and rural areas.1 One less well studied factor is political environment, which is associated with policies, laws, and regulations that influence health, including safety net programmes (eg, Medicaid), tobacco control, gun laws, and environmental protections as well as national and state financial and budgetary decisions, especially for public health related programmes. In addition, political environment is also associated with communicable disease related health behaviors, such as social distancing and vaccine acceptance, as well as traditional health behaviors (healthy diet, exercise).2 3 4
Previous studies have shown that counties that elect Republican candidates tend to experience worse health outcomes, such as fewer gains in life expectancy and increased rates of opioid prescription.5 6 7 8 9 However, it is unknown how these trends have changed since the 2016 presidential election. Furthermore, given that political preference often varies by sex, race, ethnicity, and urban and rural location, it is also not known to what extent county level political environment and mortality rates differ across racial and ethnic groups. For example, although black and Hispanic Americans are more likely to vote for candidates of the Democratic party, it is unclear if black and Hispanic residents of Democratic majority counties have experienced gains or losses in mortality rates compared with those living in Republican majority counties.10 Lastly, although previous analyses have assessed trends in mortality or life expectancy, or both in relation to county political voting status, they have not assessed trends in counties that consistently vote for one party or another or assessed inflection points in mortality trends by political environment.
In this analysis, using national mortality and federal and state election data, we sought to answer three questions. First, how did trends in age adjusted mortality rates (AAMRs) in the US change by residents’ political environment, based on county level presidential election decisions, from 1999 to 2019? Second, did these overall patterns in AAMR differ among key subgroups by sex, race and ethnicity, and urban-rural status? And third, which conditions were responsible for these changes?
Methods
We analyzed adjudicated death certificate data between 2001 and 2019 from the publicly available, deidentified Centers for Disease Control and Prevention Wide-ranging OnLine Data for Epidemiologic Research (CDC WONDER) database.11 We linked these data with US presidential elections data at county level from the MIT (Massachusetts Institute of Technology) Election Data and Science Laboratory from 2000 to 2019.12 Linkage was successful for 3112 of 3143 counties (99.0%) or county equivalents in the US, accounting for 99.8% of the US population. The missing counties or equivalents were based in Alaska, where CDC and election data did not match. Counties were classified as either Democratic voting or Republican voting for the four years that followed a presidential election, based on the results in November of a given election year. For example, AAMRs from 2001 to 2004 were attributed to the November 2000 election result, and so forth. To correctly match counties analyzed in the CDC database and the election result database, we used the Federal Information Processing Standard code, to confirm alignment of counties between the two databases.
AAMRs per 100 000 population were obtained from CDC WONDER. We stratified results by sex (male and female residents), race and ethnicity (non-Hispanic white (white), non-Hispanic black (black), Hispanic). We did not include other racial and ethnic groups, given low counts; especially in smaller counties. For urban-rural designation, we divided the cohort into three county designations as large metropolitan area (≥1 million), medium metropolitan area (50 000-999 999), and rural (<50 000) using the National Center for Health Statistics Urban-Rural Classification Scheme and the 2013 US Census classification.13
Trends in mortality were examined to identify changes in slope using Joinpoint Regression Program version 4.8.0.1, which models consecutive linear segments on a log scale, connected by joinpoints, and can measure when slopes of annual percentage change (APC) undergo a statistically significant change. We estimated the weighted average APC with 95% confidence intervals for the entire study period (2001-19) using Monte Carlo permutation test. Slopes were considered to be increasing or decreasing if the APC slope differed significantly from zero. We considered a two tailed P value of <0.05 as statistically significant.
We performed two additional sensitivity analyses. First, we analyzed and compared overall and subgroup AAMR trends for counties that always voted for Democratic or Republican throughout the five presidential elections, and refer to them as exclusively Democratic or Republican counties. Second, we assessed AAMR trends by county level election results for statewide governor elections. States were divided into five groups based on their election year and term period and election schedule (supplementary table 6).
Patient and public involvement
Although no patients or members of the public were directly involved in this paper, we did speak to patients about the study, and we will widely disseminate the paper to members of the public to read after publication.
Results
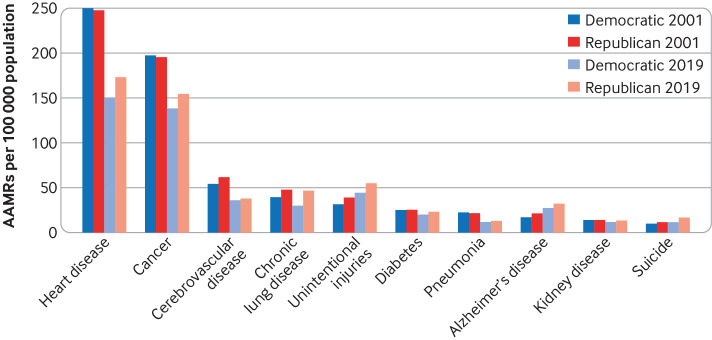
The study period covered five presidential elections from 2000 (673 Democratic counties, 132 833 397 population; 2439 Republican counties, n=147 957 141) to 2019 (490 Democratic counties, n=176 971 611; 2622 Republican counties, n=145 413 920) (supplementary tables 1 and 2). From 2001 to 2019, the AAMR per 100 000 population decreased by 22% in Democratic counties, from 850.3 to 664.0 (average APC −1.4%, 95% confidence interval −1.5% to −1.2%). Over the same time, the AAMR decreased by 11% in Republican counties, from 867.0 to 771.1 (average APC −0.7%, −0.9% to −0.5%) (table 1 and fig 1). Consequently, the gap in AAMR between Democratic and Republican counties widened from 16.7 (95% confidence interval 16.6 to 16.8) in 2001 to 107.1 (106.5 to 107.7) in 2019.
Table 1.
Age adjusted mortality rates (AMMRs) per 100 000 population and average annual percentage change (AAPC) in Democratic and Republican counties overall and by sex, race and ethnicity, and urban-rural status, 2001-19
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | AMMR difference (95% CI) | AAPC (%) (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 858.8 | 855.9 | 843.5 | 813.7 | 815.0 | 791.8 | 775.3 | 774.9 | 749.6 | 747.0 | 741.3 | 732.8 | 731.9 | 724.6 | 733.1 | 728.8 | 731.9 | 723.6 | 715.2 | 143.5 (143.1 to 143.9) | −1.0 (−1.2 to -0.9) |
| Democratic | 850.3 | 843.1 | 828.4 | 800.1 | 789.8 | 768.1 | 750.4 | 746.0 | 721.9 | 716.6 | 711.5 | 701.6 | 697.3 | 688.4 | 696.2 | 692.8 | 680.6 | 672.6 | 664.0 | 186.3 (185.5 to 187.1) | −1.4 (−1.5 to −1.2) |
| Republican | 867.0 | 868.0 | 857.6 | 826.3 | 835.6 | 810.9 | 795.1 | 798.0 | 791.6 | 793.0 | 786.4 | 779.9 | 776.1 | 770.8 | 779.8 | 774.1 | 788.6 | 779.5 | 771.1 | 95.9 (95.5 to 96.3) | −0.7 (−0.9 to −0.5) |
| Democratic | |||||||||||||||||||||
| Male resident | 1028 | 1020 | 998.0 | 963.2 | 947.3 | 922.5 | 900.4 | 891.7 | 862.0 | 854.7 | 845.0 | 834.0 | 828.5 | 818.8 | 826.2 | 826.2 | 810.1 | 802.7 | 793.2 | 234.8 (233.6 to 236) | −1.4 (−1.6 to −1.3) |
| Female resident | 718.1 | 711.3 | 700.3 | 676.8 | 669.6 | 649.6 | 635.0 | 632.8 | 612.6 | 608.5 | 605.6 | 596.0 | 592.2 | 583.5 | 590.5 | 583.7 | 574.0 | 565.2 | 556.5 | 161.6 (160.5 to 162.7) | −1.4 (−1.5 to −1.2) |
| Republican | |||||||||||||||||||||
| Male resident | 1042.6 | 1040.8 | 1021.9 | 982.8 | 991.7 | 960.1 | 940.5 | 939.9 | 934.1 | 935.0 | 920.1 | 911.2 | 907.1 | 900.0 | 908.8 | 903.7 | 923.1 | 912.1 | 903.6 | 139 (138.3 to 139.7) | −0.8 (−1.0 to −0.5) |
| Female resident | 733.0 | 735.4 | 729.3 | 703.4 | 711.2 | 690.8 | 676.9 | 682.0 | 674.3 | 675.8 | 674.0 | 668.9 | 664.3 | 659.9 | 668.0 | 661.3 | 671.3 | 663.1 | 654.3 | 78.7 (78.1 to 79.3) | −0.7 (−0.8 to −0.5) |
| Democratic | |||||||||||||||||||||
| Black | 1116.4 | 1106.9 | 1090.5 | 1054.7 | 1039.9 | 1012.9 | 987.6 | 963.9 | 924.8 | 907.5 | 894.9 | 879.9 | 877.8 | 864.8 | 869.4 | 878.0 | 867.9 | 865.7 | 857.7 | 258.7 (256.7 to 260.7) | −1.5 (−1.6 to −1.3) |
| White | 833.4 | 828.3 | 814.0 | 789.9 | 778.3 | 758.4 | 743.5 | 742.8 | 723.1 | 720.4 | 720.7 | 710.0 | 707.3 | 702.0 | 711.8 | 707.7 | 699.9 | 689.8 | 679.8 | 153.6 (151.9 to 155.3) | −1.1 (−1.2 to −0.9) |
| Hispanic | 651.4 | 638.6 | 638.1 | 605.0 | 618.4 | 598.5 | 578.0 | 576.3 | 560.8 | 558.9 | 542.5 | 541.1 | 539.0 | 525.4 | 527.5 | 530.5 | 523.1 | 522.9 | 523.3 | 128.1 (127.3 to 128.9) | −1.2 (−1.4 to −1.0) |
| Republican | |||||||||||||||||||||
| Black | 1134.9 | 1129.1 | 1116.5 | 1079.1 | 1081.6 | 1031.4 | 1007.5 | 980.1 | 963.3 | 958.9 | 922.4 | 908.9 | 907.3 | 888.9 | 896.1 | 898.0 | 914.2 | 914.2 | 903.3 | 231.6 (221.8 to 241.4) | −1.3 (−1.5 to −1.1) |
| White | 858.1 | 860.7 | 851.3 | 821.3 | 831.8 | 809.6 | 796.1 | 803.3 | 794.6 | 797.5 | 795.4 | 789.3 | 786.2 | 782.6 | 793.2 | 788.5 | 798.6 | 789.4 | 781.1 | 77 (76.7 to 77.3) | −0.5 (−0.7 to −0.4) |
| Hispanic | 682.6 | 675.2 | 656.8 | 636.0 | 640.8 | 611.4 | 598.0 | 584.9 | 555.2 | 557.5 | 532.7 | 530.5 | 521.7 | 514.8 | 516.6 | 509.0 | 527.6 | 525.7 | 523.7 | 158.9 (155.5 to 162.3) | −1.5 (−1.7 to −1.3) |
| Democratic | |||||||||||||||||||||
| Large metropolitan area | 841.2 | 830.3 | 814.4 | 786.7 | 777.8 | 756.5 | 736.5 | 731.0 | 707.0 | 699.9 | 693.0 | 681.6 | 678.2 | 667.5 | 673.8 | 671.6 | 663.9 | 656.5 | 646.7 | 194.5 (193.7 to 195.3) | −1.4 (−1.6 to −1.3) |
| Medium metropolitan area | 845.9 | 845.5 | 834.1 | 804.4 | 798.5 | 776.3 | 761.7 | 759.5 | 740.8 | 738.3 | 736.7 | 730.3 | 728.2 | 723.4 | 734.5 | 729.4 | 720.5 | 711.9 | 706.6 | 139.3 (138.1 to 140.5) | −1.0 (−1.1 to −0.8) |
| Rural | 937.3 | 942.2 | 928.3 | 900.5 | 881.1 | 855.7 | 851.1 | 848.5 | 784.4 | 785.1 | 786.2 | 777.8 | 796.1 | 793.3 | 807.5 | 799.8 | 799.0 | 785.8 | 782.9 | 154.4 (153.1 to 155.7) | −1.0 (−1.3 to −0.8) |
| Republican | |||||||||||||||||||||
| Large metropolitan area | 846.5 | 842.9 | 826.3 | 798.6 | 799.8 | 774.3 | 754.5 | 752.8 | 734.0 | 736.5 | 727.6 | 718.8 | 714.7 | 708.0 | 712.9 | 708.8 | 731.6 | 722.1 | 712.9 | 133.6 (132.2 to 135) | −0.9 (−1.1 to −0.7) |
| Medium metropolitan area | 867.5 | 867.5 | 862.4 | 828.8 | 840.5 | 816.4 | 800.3 | 801.8 | 789.5 | 792.1 | 783.0 | 779.2 | 776.6 | 767.4 | 782.1 | 775.9 | 787.1 | 778.1 | 767.6 | 99.9 (99.4 to 100.4) | −0.7 (−0.8 to −0.5) |
| Rural | 900.5 | 910.2 | 901.5 | 869.3 | 886.8 | 863.3 | 853.3 | 866.0 | 857.9 | 857.8 | 858.3 | 852.2 | 845.5 | 840.3 | 855.9 | 850.4 | 851.9 | 844.3 | 840.7 | 59.8 (59.5 to 60.1) | −0.4 (−0.6 to −0.2) |
Fig 1.
Trends in age adjusted mortality rates (AAMRs) per 100 000 residents of counties voting for Democratic or Republican presidential candidates. Widening gap in AAMR is noted between Democratic and Republican counties. Statistically significant inflection points in annual percentage change (APC) of AAMR occurred for Democratic counties between periods 2001-09 (APC −2.1) and 2009-19 (APC −0.8) and Republican counties between periods 2001-08 (APC −1.4) and 2008-19 (APC −0.2)
Joinpoint analysis shows that statistically significant inflection points in APC of AAMRs per 100 000 population occurred for Democratic counties between periods 2001-09 (APC −2.1%, −2.3% to −1.9%) and 2009-19 (−0.8%, −1.0% to −0.6%). For Republican counties between 2001 and 2008 the APC was −1.4% (−1.8% to −1.0%), slowing to near zero between 2008 and 2019 (−0.2%, −0.4% to 0.0%) (supplementary table 3).
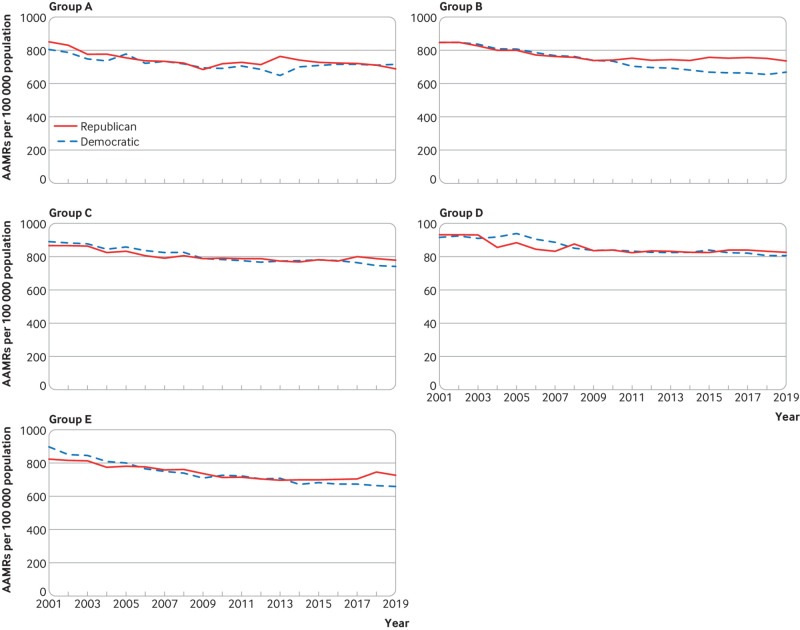
Trends by sex
Over the study period, male and female residents of Democratic counties had lower AAMRs per 100 000 population than their counterparts in Republican counties (table 1 and fig 2). Furthermore, improvements in AAMRs were more pronounced in male residents (average APC −1.4%, −1.6% to −1.3%) and female residents (−1.4%, −1.5% to −1.2%) of Democratic counties than in male residents (−0.8%, −1.0% to −0.5%) and female residents (−0.7%, −0.8% to −0.5%) of Republican counties. Similar trends were noted in counties that voted consistently Democratic or Republican throughout the study period (supplementary table 4 and supplementary figure 2). Statistically significant inflection points in APC of AAMR occurred for male residents of Democratic counties between periods 2001-10 (APC −2.2%, −2.4% to −2.0%) and 2010-19 (−0.7%, −0.9% to −0.5%) and male residents of Republican counties between periods 2001-07 (−1.7%, −2.2% to −1.3%) and 2007-14 (−0.6%, −1.1% to −0.2%), with no significant change noted after additional inflection point between 2014 and 2019 (0.2%, −0.4% to 0.8%). Statistically significant inflection points in APC of AAMR occurred for female residents of Democratic counties between periods 2001-09 (APC −2.0) and 2009-19 (APC −0.9) and for female residents of Republican counties between periods 2001-07 (APC −1.4) and 2007-19 (APC −0.3).
Fig 2.
Trends in age adjusted mortality rates (AAMRs) per 100 000 residents of counties voting for Democratic or Republican presidential candidates by sex. Widening gap in AAMR is noted between male and female residents of Democratic and Republican counties. (Top lines) Statistically significant inflection points in annual percentage change (APC) of AAMR occurred for male residents of Democratic counties between periods 2001-10 (APC −2.2) and 2010-19 (APC −0.7) and male residents of Republican counties between periods 2001-07 (APC −1.7) and 2007-14 (APC −0.6) with no significant change noted after additional inflection point (straight line) between 2014 and 2019. (Bottom lines) Statistically significant inflection points in annual percentage change of AAMR occurred for female residents of Democratic counties between periods 2001-09 (APC −2.0) and 2009-19 (APC −0.9) and female residents of Republican counties between periods 2001-07 (APC −1.4) and 2007-19 (APC −0.3)
Trends by race and ethnicity
Throughout the study period, black Americans had higher AAMRs per 100 000 population than white Americans or Hispanic Americans. However, black Americans experienced a substantial improvement in AAMR in both Democratic (1116.4 to 857.7) and Republican counties (1134.9 to 903.3). Although AAMRs were slightly lower in Democratic counties, black residents of Democratic counties experienced similar improvement (average APC −1.5%, −1.6% to −1.3%) compared with black residents of Republican counties (−1.3%, −1.5% to −1.1%) (table 1 and fig 3). From 2001 to 2019, the AAMR gap between black residents in Democratic versus Republican counties increased from 18.5 (95% confidence interval 18.4 to 18.6) to 45.6 (45.4 to 45.8). However, black residents of Republican counties experienced an improvement in AAMR twice that of all other residents in Republican counties.
Fig 3.
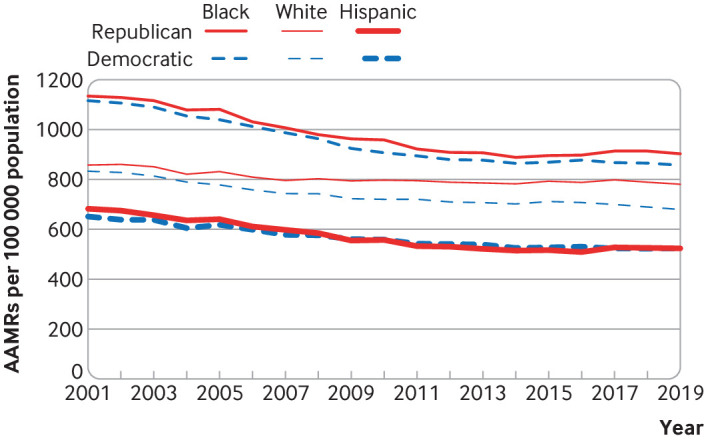
Trends in age adjusted mortality rates (AAMRs) per 100 000 residents of counties voting for Democratic or Republican presidential candidates by race and ethnicity. Widening gap in AAMR is noted most prominently among white residents of Democratic and Republican counties, while the gap appears to narrow for Hispanic residents. AAMR gap for black residents of Democratic and Republican counties oscillates across the study period
Whereas the AAMR per 100 000 population for white residents of Democratic counties decreased from 833.4 to 679.8, with an average APC of −1.1% (95% confidence interval −1.2% to −0.9%), the AAMR for white residents of Republican counties decreased from 858.1 to 781.1 at a much lower average APC of −0.5% (−0.7% to −0.4%), the smallest reduction in average APC of all major racial and ethnic groups in either Democratic or Republican counties (table 1 and fig 3). Over time the widest difference in AAMR by political environment emerged among white Americans. From 2001 to 2019, the AAMR gap between white residents in Democratic versus Republican counties increased fourfold, from 24.7 (95% confidence interval 24.6 to 24.8) to 101.3 (101.0 to 101.6). Therefore, white residents in Democratic counties experienced 15% lower AAMR in 2019 than white residents in Republican counties compared with just 3% in 2001.
Hispanic Americans had lower AAMRs per 100 000 population than either white or black Americans, but there was little gap between those residing in Democratic versus Republican counties (table 1 and fig 3). Trends were similar when exclusively Democratic or Republican counties were analyzed (supplementary table 4 and supplementary figure 3).
Trends by urban-rural status
In 2001, the AAMR per 100 000 population in Democratic counties designated as large metropolitan areas (143 counties, n=91 809 974) was 841.2 and in Republican counties designated as large metropolitan areas (292 counties, n=61 407 202) was 846.5. By 2019, the AAMR in Democratic large metropolitan areas (156 counties, n=133 796 619) decreased to 646.7 (average APC −1.4%, 95% confidence interval −1.6% to −1.3%) and in Republican large metropolitan areas (280 counties, n=46 244 883) decreased to 712.9 (−0.9%, −1.1% to −0.7%) (table 1 and fig 4). Therefore, the gap in AAMR between Democratic and Republican counties designated as large metropolitan areas increased from 5.3 in 2001 to 66.2 in 2019.
Fig 4.
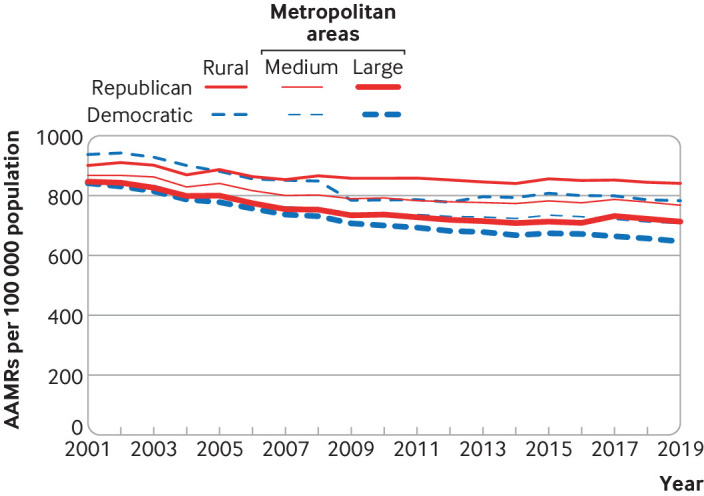
Trends in age adjusted mortality rates (AAMRs) per 100 000 population of residents of counties voting for Democratic or Republican presidential candidates by urban-rural location. Widening gaps in AAMR between Republican and Democratic counties are noted across urban-rural spectrum, from large metropolitan areas, medium metropolitan areas, and rural areas
In 2001, the AAMR per 100 000 population in Democratic counties designated as medium metropolitan areas (176 counties, n=30 901 916) was 845.9 and in Republican counties designated as medium metropolitan areas (551 counties, n=52 116 112) was 867.5. By 2019, the AAMR in Democratic medium metropolitan areas (147 counties, n=37 730 408) decreased to 706.6 (average APC −1.0%, −1.1% to −0.8%) and in Republican medium metropolitan areas (579 counties, n=58 741 769) decreased to 767.6 (−0.7%, −0.8% to −0.5%) (table 1 and fig 4). Therefore, the gap in AAMR between Democratic and Republican counties designated as medium metropolitan areas increased from 21.6 in 2001 to 61.0 in 2019.
In 2001, the AAMR per 100 000 population in Democratic rural areas (354 counties, n=10 121 507) was 937.3 and in Republican rural areas (1596 counties, n=34 433 827) was 900.5. By 2019, the AAMR in Democratic rural areas (187 counties, n=5 444 584) decreased to 782.9 (average APC −1.0%, −1.3% to −0.8%) and in Republican rural areas (1763 counties, n=40 427 268) decreased to 840.7 (−0.4%, −0.6% to −0.2%) (table 1 and fig 4). Therefore, the AAMR in Democratic rural counties was greater by 36.8 in 2001 compared with Republican counties in 2001. In 2019, however, the AAMR was lower by 57.8 in Democratic rural counties versus Republican rural counties. Similar trends in AAMR by urban-rural location were noted for counties that remained exclusively Democratic or Republican (supplementary table 4 and supplementary figure 4).
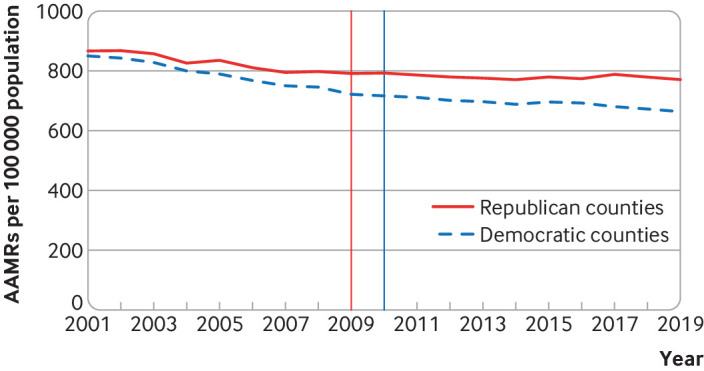
Cause specific analysis
Analysis of the 10 most common causes of death in 2001 revealed that AAMRs per 100 000 population for heart disease, cancer, and influenza and pneumonia were lower in Republican counties than Democratic counties, whereas AAMRs for cerebrovascular disease, unintentional injuries (which include drug overdoses), diabetes mellitus, Alzheimer’s disease, kidney disease, and suicide were all higher in Republican counties (table 2 and fig 5). In 2019, however, AAMRs for all causes of death were higher in Republican counties, and the greatest increases in AAMR gap between Republican and Democratic counties occurred for heart disease (difference in AAMRs 27.6), cancer (17.3), chronic lower respiratory tract diseases (8.3), unintentional injuries (3.3), and suicide (3.0). Compared with Republican counties, Democratic counties experienced greater reductions in AAMR from heart disease, cancer, chronic lower respiratory tract diseases, diabetes, influenza and pneumonia, and kidney disease. Both Democratic and Republican counties experienced a 40% increase in deaths from unintentional injuries; however, Republican counties showed a greater increase in suicide (41.5% v 19.6%) but a lower increase in deaths related to Alzheimer’s disease (49.8% v 61.8%).
Table 2.
Age adjusted mortality rates (AAMRs) per 100 000 population for the 10 most common causes of death in Democratic and Republican counties, 2001-19
| Causes of death | AAMR | AAMR difference | % change, 2001-19 | |||||
|---|---|---|---|---|---|---|---|---|
| 2001 | 2019 | 2001 | 2019 | |||||
| Democratic | Republican | Democratic | Republican | Democratic | Republican | |||
| Heart disease | 251.7 | 247.5 | 150.3 | 173.7 | −4.2 | 23.4 | −40.3 | −29.8 |
| Malignant neoplasms | 197.1 | 195.9 | 138.4 | 154.5 | −1.2 | 16.1 | −29.8 | −21.1 |
| Cerebrovascular diseases | 54.7 | 61.9 | 36.1 | 37.9 | 7.2 | 1.8 | −34.0 | −38.8 |
| Chronic lower respiratory tract diseases | 39.6 | 47.7 | 30.1 | 46.5 | 8.1 | 16.4 | −24.0 | −2.5 |
| Unintentional injuries | 31.7 | 39.2 | 44.4 | 55.2 | 7.5 | 10.8 | 40.1 | 40.8 |
| Diabetes mellitus | 25.1 | 25.7 | 20.4 | 23 | 0.6 | 2.6 | −18.7 | −10.5 |
| Influenza and pneumonia | 22.5 | 21.9 | 11.8 | 12.9 | −0.6 | 1.1 | −47.6 | −41.1 |
| Alzheimer’s disease | 17 | 21.5 | 27.5 | 32.2 | 4.5 | 4.7 | 61.8 | 49.8 |
| Kidney disease | 14.2 | 13.9 | 12.0 | 13.4 | 0.3 | 1.4 | −15.5 | −3.6 |
| Suicide | 9.7 | 11.8 | 11.6 | 16.7 | 2.1 | 5.1 | 19.6 | 41.5 |
Fig 5.
Age adjusted mortality rates (AAMRs) per 100 000 population for the 10 most common causes of death in Democratic and Republican counties in 2001 and 2019. Except for cerebrovascular disease, the gap in AAMR between Republican and Democratic counties increased for every cause of death over the study period driven by heart disease, cancer, chronic lower respiratory tract disease, unintentional injuries (which include drug overdoses), and suicide
AAMR trends in counties that did not switch political environment throughout study period
Throughout the study period there were 356 Democratic counties (number in 2000=111 134 206 (84% of residents in Democratic counties), number in 2016=121 467 959 (67% of residents in Democratic counties)) and 2086 Republican counties (number in 2000=92 944 792 (63% of residents in Republican counties), number in 2016=111 235 319 (76% of residents in Republican counties) that did not change political environment. The AAMR per 100 000 population trends were similar when we compared these exclusively Democratic and Republican counties: AAMR in exclusively Democratic counties decreased by 174.6 (95% confidence interval 173.2 to 176.0), from 838.4 to 663.8 (average APC −1.3%, 95% confidence interval −1.4% to −1.2%), whereas in Republican counties it decreased by 115.2 (114.7, 115.7), from 882.5 to 767.3 (−0.8%, −0.9% to −0.6%) (supplementary table 4 and supplementary figure 1). Therefore, the gap in AAMR between exclusively Democratic counties and exclusively Republican counties increased from 44.1 (95% confidence interval 43.7 to 44.5) to 103.5 (102.9 to 104.1). Joinpoint analysis shows that statistically significant inflection points in APC of AAMR occurred for Democratic counties between periods 2001-10 (APC −2.1, 95% confidence interval −2.2% to −1.9%) and 2010-19 (−0.6%, −0.7% to −0.4%). For Republican counties between 2001 and 2010 the APC was −1.4% (−1.6% to −1.1%), with no significant change between 2010 and 2019 (−0.2%, −0.4% to 0.1%) (supplementary table 5).
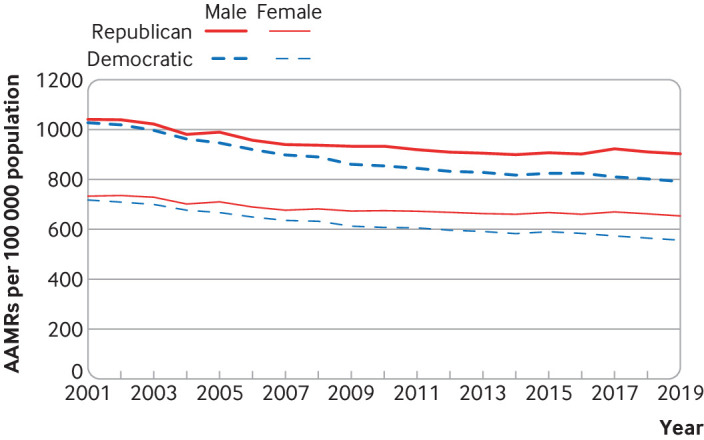
Relationship between county level gubernatorial environment and AAMR
In our second sensitivity analysis, we assessed the relationship between county level gubernatorial political environment and AAMR per 100 000 population. We found, similar to our main analysis, that AAMR improvements in counties with a Democratic gubernatorial environment exceeded those trends noted in Republican environments (fig 6 and supplementary table 6). States were divided into five groups A through E based on their election schedule. In groups B, C, and E, which include 45 states comprising 96% of the 2019 US population (n=316 074 352/330 150 668), Democratic counties had a higher AAMR in 2001 but lower AAMR in 2019.
Fig 6.
Trends in age adjusted mortality rates (AAMRs) per 100 000 population for counties voting for Democratic or Republican governors by state Group from 2001 to 2019. Group A=New Hampshire and Vermont; Group B=Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Florida, Georgia, Hawaii, Idaho, Illinois, Iowa, Kansas, Maine, Maryland, Massachusetts, Michigan, Minnesota, Nebraska, Nevada, New Mexico, New York, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, Wyoming, and Washington DC; Group C=Delaware, Indiana, Missouri, Montana, North Carolina, North Dakota, Utah, Washington, and West Virginia; Group D=Kentucky, Louisiana, and Mississippi; Group E=New Jersey and Virginia
Discussion
To better understand health and healthcare, it is critical to study political environments as a core determinant of health.14 In this national analysis, we found that Americans living in counties that voted Democratic during presidential elections from 2000 to 2016 experienced lower age adjusted mortality rates (AAMRs) than residents of counties that voted for a Republican candidate, and these patterns were consistent across subgroups (sex, race and ethnicity, urban-rural location). The gap in overall AAMR between Democratic and Republican counties increased more than sixfold from 2001 to 2019, driven primarily by changes in deaths due to heart disease, cancer, lower respiratory tract diseases, unintentional injuries, and suicide. These patterns were similar when we assessed mortality rates by state governor election results, with evidence of an increasing gap between Republican and Democratic voting areas over the study period.
Policy implications
The widening gap in death rates between Republican and Democratic voting areas of the US over the past two decades may reflect the influence of political environment on social, economic, and health policies. A previous study showed that more liberal state policies on tobacco control, labor, immigration, civil rights, and environmental protections are all strongly associated with better life expectancy, whereas more conservative state policies—such as restrictions on abortion and reductions in gun control—are associated with lower life expectancy among women.15 In addition, variation in social welfare generosity (eg, unemployment insurance, TANF (Temporary Assistance for Needy Families)), which is often linked to political environment, could potentially be contributing to the diverging trends in mortality that we observed.16 17 More liberal states also tend to enact health policies that serve as a critical safety net for vulnerable populations. For example, Democratic states were more likely than Republican states to adopt Medicaid expansion under the Affordable Care Act, which expanded health insurance coverage to millions of people on a low income.18 A large body of evidence has shown that doing so was associated with important health benefits, including better access to primary and preventive care, improved identification and treatment of chronic conditions, and, perhaps most importantly, reductions in mortality.19 20 21 More broadly, public health spending varies markedly by state, with Republican governors tending to spend significantly less on health than Democratic governors.22 Overall, our finding that Democratic counties have experienced steeper declines in mortality than Republican counties over the past two decades builds upon previous evidence suggesting that more liberal policies, laws, and regulations may be associated with better health outcomes.
We also found that heart disease and cancer remain the leading causes of death in both Democratic and Republican counties. Although heart disease mortality rates were similar between Democratic and Republican counties in 2001, declines were more pronounced in Democratic areas, resulting in a widening gap. Similar patterns were observed for cancer, with higher mortality rates in Republican compared with Democratic areas by the end of our study period. Understanding the factors that are contributing to the growing differences in heart disease and cancer mortality across political environments is critically important. One potential explanation may be related to underlying differences in access to healthcare. Recent evidence suggests that the values and beliefs about whether health insurance coverage should be provided by the federal government vary markedly by political environment, and Republican states tend to have higher uninsurance rates, in part because many elected to not expand Medicaid over the past decade.23 24 Lack of health insurance coverage is associated with lower rates of screening, identification, and treatment of important risk factors (eg, diabetes, hypertension) and chronic conditions (heart disease, cancer). At the same time, health behaviors are associated with political environment, as is trust in the healthcare system, which ultimately could influence health outcomes.25 26 Beyond heart disease and cancer, we found that deaths due to unintentional injuries such as drug overdoses increased over our study period, and they were the third leading causes of death by 2019. In addition, gaps in mortality due to unintentional injuries and suicide increased—albeit modestly—between Republican and Democratic counties, a finding27 that could partially be explained by higher rates of opioid use in Republican counties.7
The analysis shows that health outcomes differed markedly across racial and ethnic groups in Democratic and Republican counties. Whereas black Americans experienced higher AAMRs than all other groups, they also experienced consistent yet similar improvements in AAMRs in both Democratic and Republican counties. It is possible that black Americans have benefitted most from advances in medicine, public health, and healthcare delivery that are independent of county political environment. However, a closer look at AAMR trends shows that although AAMR has been consistently decreasing for black residents in Democratic counties, black residents of Republican counties have experienced increases in AAMR in several years over the study period, including 2004-5, 2009-10, and 2016-17. However, white residents of counties that voted majority for the Republican presidential candidate experienced the smallest reduction in AAMR across all racial and ethnic groups studied. Furthermore, the gap in AAMR between white residents of Republican and Democratic counties grew fourfold over the study period—the greatest increase in gap for any racial-ethnic group. Previous work from our group showed widening gaps in AAMR between large metropolitan areas and rural areas.1 Given that Democratic rural counties fared much better than Republican rural counties, it is likely that political environment has an important role to play in the widening urban-rural mortality gap.
Comparison with other studies
Previous work has evaluated political environment and health outcomes, and our study extends upon these findings in several ways.5 6 7 8 9 First, we performed a longitudinal analysis that evaluated how differences between Republican and Democratic areas changed over time, and we included more contemporary data to 2019. Second, we present a detailed breakdown showing trends by key demographic subgroups, including sex, race and ethnicity, and urban-rural location. These findings have important implications because as the analysis shows, important differences were found, particularly by race and ethnicity and urban-rural location.
Strengths and limitations of this study
Our study has several limitations. We denoted political environment dichotomously based on the party receiving the majority vote. We could not use voting patterns as a continuous variable as joinpoint is unable to analyze continuous data. However, our analysis of counties that always voted for one party across five presidential elections partly selects for counties with greater party vote shares and reached a similar conclusion to our primary analysis. Second, we did not study the effect of flipping political environment to the health status of a county, and this could be studied in future work. However, most residents of Democratic counties (84% in 2000 and 67% in 2016) and residents of Republican counties (63% in 2000 and 76% in 2016) lived in counties that always voted for one party throughout the period. Lastly, we were unable to explore specific factors that might explain the link between political environment and mortality, and the direction of this association, which remain an important area for future research. For example, it is also possible that poor health or social and economic factors that lead to poor health also motivate political preference.5
Conclusions
We found that people living in counties that voted Democratic during presidential elections between 2001 and 2019 experienced lower AAMR than residents of counties that voted for the Republican candidate, a finding that was largely consistent across key subgroups. Declines in mortality over time were more pronounced in Democratic compared with Republican counties, resulting in an increasing gap between these areas, primarily related to changes in heart disease and cancer related deaths. These mortality patterns were similar when assessed by state governor election results. Further research is needed to better elucidate factors driving this widening difference in mortality rates between Republican and Democratic counties, to inform clinical, public health, and policy strategies to improve the health of all Americans.
What is already known on this topic.
Studies have shown that residents of counties with a Republican political environment experience worse health outcomes
Recent trends in mortality differences for residents of Republican and Democratic counties are not known, nor are the conditions that might be driving those changes
What this study adds
Between 2001 and 2019, mortality rates decreased by 22% in Democratic counties but by only 11% in Republican counties
Male and female residents of Democratic counties experienced both lower mortality rates and twice the relative decrease in mortality rates than did those in Republican counties. Black Americans experienced largely similar improvement in age adjusted mortality rates in both Democratic and Republican counties. However, the mortality gap between white residents in Democratic versus Republican counties increased fourfold
Rural Republican counties experienced the highest mortality rates and the least improvement. All trends were similar when comparing counties that did not switch political environment throughout the period, and when governor election results were used
The greatest contributors to the rising mortality gap between Republican and Democratic counties were heart disease, cancer, chronic lower respiratory tract diseases, unintentional injuries, and suicide
Acknowledgments
We acknowledge Charles Stewart, professor of political science and director of the Massachusetts Institute of Technology Election Laboratory for providing critical insights into the manuscript, and Robert M Califf, who contributed to an earlier draft of this paper while he was working for Verily Life Sciences.
Web extra.
Extra material supplied by authors
Supplementary information: Additional tables 1-6 and figures 1-4
Contributors: HJW and PK contributed equally. HJW is the guarantor. All authors contributed to drafting the manuscript and provided critical revisions. PK performed the statistical analysis and all authors contributed to data interpretation. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: None received.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: HW is an advisor for Embrace Prevention Care; RW receives research support from the National Heart, Lung, and Blood Institute (grant K23HL148525-1); KEJM previously did contract work for the US Department of Health and Human Services; no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
The lead author (HJW) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: We plan to share our results on social media platforms and through potential author opinion pieces in mainstream publications that reflect and expand on the findings. We will also share this paper with our media relations team to share with outlets and prepare a press release.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
Not required. Data were publicly available and deidentified and therefore informed consent was not applicable according to HHS regulation 45 CFR 46.101(c).
Data availability statement
This analysis was performed using publicly available databases. Contact the corresponding author (hwarraich@partners.org) for queries about the analysis and statistical code.
References
- 1. Cross SH, Califf RM, Warraich HJ. Rural-Urban Disparity in Mortality in the US From 1999 to 2019. JAMA 2021;325:2312-4. 10.1001/jama.2021.5334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allcott H, Boxell L, Conway J, Gentzkow M, Thaler M, Yang D. Polarization and public health: Partisan differences in social distancing during the coronavirus pandemic. J Public Econ 2020;191:104254. 10.1016/j.jpubeco.2020.104254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kreps S, Prasad S, Brownstein JS, et al. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw Open 2020;3:e2025594. 10.1001/jamanetworkopen.2020.25594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kannan VD, Veazie PJ. Political orientation, political environment, and health behaviors in the United States. Prev Med 2018;114:95-101. 10.1016/j.ypmed.2018.06.011 [DOI] [PubMed] [Google Scholar]
- 5. Goldman L, Lim MP, Chen Q, Jin P, Muennig P, Vagelos A. Independent Relationship of Changes in Death Rates with Changes in US Presidential Voting. J Gen Intern Med 2019;34:363-71. 10.1007/s11606-018-4568-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hamamsy T, Danziger M, Nagler J, Bonneau R. Viewing the US presidential electoral map through the lens of public health. PLoS One 2021;16:e0254001. 10.1371/journal.pone.0254001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goodwin JS, Kuo YF, Brown D, Juurlink D, Raji M. Association of Chronic Opioid Use With Presidential Voting Patterns in US Counties in 2016. JAMA Netw Open 2018;1:e180450. 10.1001/jamanetworkopen.2018.0450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bor J. Diverging Life Expectancies and Voting Patterns in the 2016 US Presidential Election. Am J Public Health 2017;107:1560-2. 10.2105/AJPH.2017.303945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Curtis LH, Hoffman MN, Califf RM, Hammill BG. Life expectancy and voting patterns in the 2020 U.S. presidential election. SSM Popul Health 2021;15:100840. 10.1016/j.ssmph.2021.100840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.What Happened in. 2020. Catalist, 2021. (Accessed Feb 7, 2022, at https://www.dropbox.com/s/ka9n5gzxwotfu1a/wh2020_public_release_crosstabs.xlsx?dl=0.)
- 11.Centers for Disease Control and Prevention. National Center for Health Statistics. Wide-ranging Online Data for Epidemiologic Research. (Accessed August 12, 2021, at https://wonder.cdc.gov.)
- 12.MIT Election Data and Science Lab. County Presidential Election Returns 2000-2020. Harvard Dataverse, V9, UNF:6:qSwUYo7FKxI6vd/3Xev2Ng== [fileUNF]. 2018. (Accessed August 12, 2021) 10.7910/DVN/VOQCHQ. [DOI]
- 13. Ingram DD, Franco SJ. NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat 2 2013;2014:1-73. [PubMed] [Google Scholar]
- 14. Woolf SH. The Growing Influence of State Governments on Population Health in the United States. JAMA 2022;327:1331-2. 10.1001/jama.2022.3785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Montez JK, Beckfield J, Cooney JK, et al. US State Policies, Politics, and Life Expectancy. Milbank Q 2020;98:668-99. 10.1111/1468-0009.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Beckfield J, Bambra C. Shorter lives in stingier states: Social policy shortcomings help explain the US mortality disadvantage. Soc Sci Med 2016;171:30-8. 10.1016/j.socscimed.2016.10.017 [DOI] [PubMed] [Google Scholar]
- 17.Hahn H, Aron, L., Prat, E., Okoli, A. Why Does Cash Welfare Depend on Where You Live? How and Why State TANF Programs Vary. Urban Institute Research Report 2017.
- 18.Status of State Action on the Medicaid Expansion Decision. KFF.org, 2022. (Accessed February 23, 2022, at https://www.kff.org/907f6c5/)
- 19. Wadhera RK, Joynt KE. Insurance and Cardiovascular Health: Time for Evidence to Trump Politics. Circulation 2017;135:1988-90. 10.1161/CIRCULATIONAHA.117.028618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med 2012;367:1025-34. 10.1056/NEJMsa1202099 [DOI] [PubMed] [Google Scholar]
- 21. Sommers BD, Gawande AA, Baicker K. Health Insurance Coverage and Health - What the Recent Evidence Tells Us. N Engl J Med 2017;377:586-93. 10.1056/NEJMsb1706645 [DOI] [PubMed] [Google Scholar]
- 22. Beland L, Oloomim S. Party Affiliation and Public Spending: Evidence from US Governors. Econ Inq 2016;55:982-95 10.1111/ecin.12393. [DOI] [Google Scholar]
- 23. Blendon RJ, Benson JM. Public Opinion about the Future of the Affordable Care Act. N Engl J Med 2017;377:e12. 10.1056/NEJMsr1710032 [DOI] [PubMed] [Google Scholar]
- 24. Blendon RJ, Benson JM, McMurtry CL. Health Care in the 2018 Election. N Engl J Med 2018;379:e32. 10.1056/NEJMsr1813425 [DOI] [PubMed] [Google Scholar]
- 25. Gadarian SK, Goodman SW, Pepinsky TB. Partisanship, health behavior, and policy attitudes in the early stages of the COVID-19 pandemic. PLoS One 2021;16:e0249596. 10.1371/journal.pone.0249596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Funk C, Kennedy B, Johnson C. Trust in Medical Scientists Has Grown in U.S., but Mainly Among Democrats. Pew Research Center, 2020. [Google Scholar]
- 27. Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015;112:15078-83. 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- MIT Election Data and Science Lab. County Presidential Election Returns 2000-2020. Harvard Dataverse, V9, UNF:6:qSwUYo7FKxI6vd/3Xev2Ng== [fileUNF]. 2018. (Accessed August 12, 2021) 10.7910/DVN/VOQCHQ. [DOI]
Supplementary Materials
Supplementary information: Additional tables 1-6 and figures 1-4
Data Availability Statement
This analysis was performed using publicly available databases. Contact the corresponding author (hwarraich@partners.org) for queries about the analysis and statistical code.