Introduction
End-stage renal disease after heart transplant (HT) is associated with higher mortality and cost of care.1,2 Early and late renal failure after HT are caused by pretransplant comorbid factors (age, chronic kidney disease [CKD], diabetes mellitus, hypertension, and smoking), perioperative recurrent acute kidney injury (AKI), and use of nephrotoxic immunosuppressive agents (calcineurin inhibitors).3,4
The rate of simultaneous heart-kidney transplantation (SHKT) due to comorbid kidney disease has increased in the past decade.5 The Organ Procurement and Transplant Network/the United Network for Organ Sharing, which oversees organ transplantation in the United States, has not set a national policy to guide SHKT. Thus, the decision for SHKT is currently left to individual transplant centers’ discretion. A consensus conference in 2019 on heart-kidney transplantation set the stage for developing guidelines for medical eligibility criteria for SHKT for candidates with established CKD (glomerular filtration rate [GFR] <60 ml/min per 1.73 m2) and persistent AKI.6 Their Heart/Kidney Workgroup advised that, based on 2 independent GFR measurements at least 2 weeks apart, patients with established GFR <30 ml/min per 1.73 m2 and selected candidates with GFR of 30 to 44 ml/min per 1.73 m2 (having strong evidence of CKD including small kidney sizes and proteinuria >0.5 g/d) should be considered for SHKT. Remaining patients with CKD with GFR of 45–59 ml/min per 1.73 m2 may not be suitable for SHKT. Nevertheless, applying these criteria to HT alone recipients between 2000 and 2019, approximately 33% of them with an estimated GFR of 30–59 ml/min per 1.73 m2 pretransplant (Supplementary Table S1), not considered as eligible for SHKT, may still be at risk of developing end-stage renal disease. Therefore, a personalized computer-aided model to predict the possibility of advanced kidney failure in early post-transplant period is needed to identify at-risk candidates.
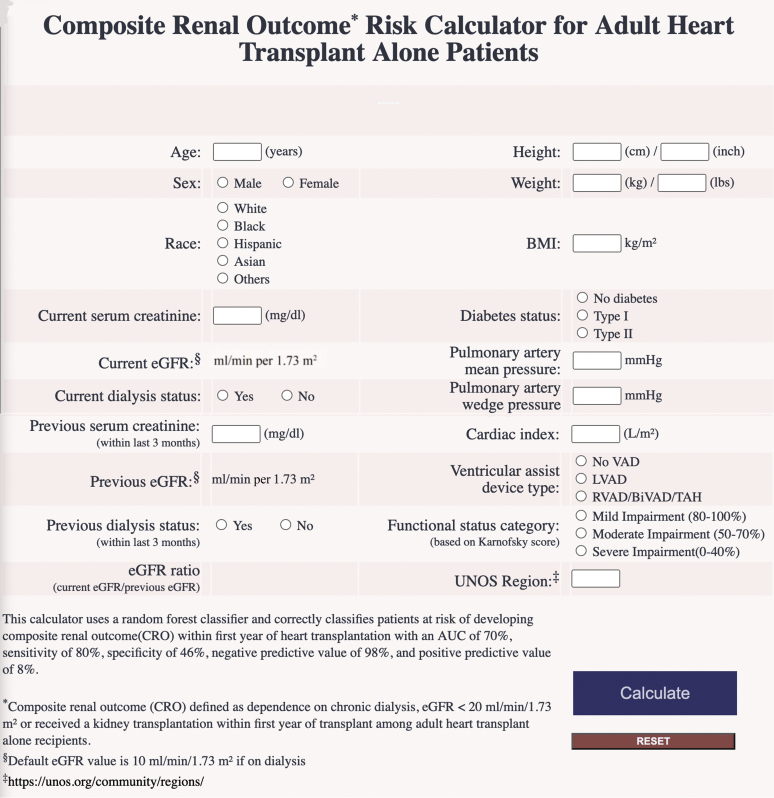
In this study, we developed a machine learning (random forest [RF])–based algorithm to predict composite renal outcomes (CRO defined as dependence on chronic dialysis, GFR <20 ml/min per 1.73 m2, or having received a kidney transplant) among adult HT recipients at risk (GFR <60 ml/min per 1.73 m2) at post-transplant 1 year. We also built a web-based decision tool based on the RF model (Figure 1). The details regarding the study cohort selection (Supplementary Figure S1) and the methods are provided in the Supplementary Materials.
Figure 1.
Web calculator for predicting the composite renal outcome (defined as dependence on chronic dialysis, eGFR <20 ml/min per 1.73 m2, or a received kidney transplantation risk at 1 year) in adult HT alone recipients. AUC, area under the curve; BiVAD, biventricular assist device; BMI, body mass index; CRO, composite renal outcome; eGFR, estimated glomerular filtration rate; HT, heart transplant; LVAD, left ventricular assist device; RVAD, right ventricular assist device; TAH, total artificial heart; UNOS, United Network of Organ Sharing; VAD, ventricular assist device.
Results
Characteristics of the Study Cohort
In this retrospective study, we analyzed a cohort of adult recipients who received HT alone transplants (regardless of listing intention) between January 1, 2000, and September 30, 2019, using the Organ Procurement and Transplant Network national registry, which included 19,861 adult HT recipients with eGFR <60 ml/min per 1.73 m2 at listing and/or pretransplant.
The incidence of the CRO at 1 year between 2000 and 2019 is found in Supplementary Figure S2 (ranging from 2.2% to 6.1%). The characteristics of the study cohort and corresponding deceased donors are found in Table 1 and Supplementary Table S2. The final study cohort included 19,861 patients, of which 783 (3.9%) had incident CRO. The 1-year survival among the patients who developed post-HT CRO (71.0%) was significantly lower compared with the ones who did not (88.3%) (log-rank P < 0.001).
Table 1.
Characteristics and outcomes of the HT alone recipients (eGFR ≤60 ml/min per 1.73 m2 at listing and/or before transplant) between 2000 and 2019 by composite renal outcomes at 1 year in the United States
| Recipient characteristics | Whole cohort | No-CRO | CRO | P valuea |
|---|---|---|---|---|
| n (%) | 19,861 | 19,708 (96.1) | 783 (3.9) | |
| Age, median (IQR) yr | 59 (51–64) | 59 (51–64) | 59 (52–64) | 0.17 |
| Sex (male) | 14,761 (74.3) | 14,195 (74.4) | 566 (72.3) | 0.18 |
| Race | <0.001 | |||
| White | 14,395 (72.5) | 13,883 (72.8) | 512 (65.4) | |
| Black | 3415 (17.2) | 3215 (16.9) | 200 (25.5) | |
| Hispanic | 1302 (6.6) | 1257 (6.6) | 45 (5.8) | |
| Asian | 524 (2.6) | 505 (2.6) | 19 (2.4) | |
| Other | 225 (1.1) | 218 (1.1) | 7 (0.9) | |
| Recipient height (cm) | 173.9 ± 9.8 | 173.9 ± 9.8 | 173.4 ± 10.1 | 0.16 |
| Recipient weight (kg) | 83.4 ± 17.4 | 83.3 ± 17.4 | 85.2 ± 17.8 | 0.003 |
| Body mass index (kg/m2) | 27.5 ± 4.8 | 27.4 ± 4.8 | 28.2 ± 5.0 | <0.001 |
| History of diabetes | <0.001 | |||
| No | 13,932 (70.2) | 13,463 (70.6) | 469 (59.9) | |
| Type I | 382 (1.9) | 362 (1.9) | 20 (2.6) | |
| Type II | 5547 (27.9) | 5253 (27.5) | 294 (37.6) | |
| Etiology of cardiomyopathy | 0.34 | |||
| Ischemic | 7815 (39.4) | 7510 (39.4) | 305 (39.0) | |
| Nonischemic | 7433 (37.4) | 7155 (37.5) | 278 (35.5) | |
| Congenital | 416(2.1) | 401 (2.1) | 15 (1.9) | |
| Otherb | 4197 (21.1) | 4012 (21.0) | 185 (23.6) | |
| Previous HT, n (%) | 695 (3.5) | 663 (3.5) | 32 (4.1) | 0.36 |
| Cardiac output, l/min | 4.54 ± 1.46 | 4.54 ± 1.46 | 4.76 ± 1.53 | <0.001 |
| Cardiac index, l/min per m2 | 2.31 ± 0.70 | 2.30 ± 0.70 | 2.21 ± 0.67 | <0.001 |
| Pulmonary capillary wedge pressure, mm Hg | 18.8 ± 8.6 | 18.8 ± 8.6 | 18.5 ± 8.4 | 0.33 |
| Pulmonary artery mean pressure, mm Hg | 28.3 ± 9.9 | 28.3 ± 9.9 | 28.1 ± 9.3 | 0.58 |
| Mechanical ventilation requirement | 462 (2.3) | 437 (2.3) | 25 (3.2) | 0.10 |
| ECMO | 207 (1.0) | 190 (1.0) | 17 (2.2) | 0.002 |
| IABP | 1536 (7.7) | 1463 (7.7) | 73 (9.3) | 0.09 |
| VAD | <0.001 | |||
| None | 11,698 (58.9) | 11,306 (59.3) | 392 (50.1) | |
| LVAD alone | 6530 (32.9) | 6234 (32.7) | 296 (37.8) | |
| RVAD/BiVAD/TAH | 864 (4.4) | 797 (4.2) | 67 (8.6) | |
| Unknown | 769 (3.9) | 741 (3.9) | 28 (3.6) | |
| eGFR, ml/min per 1.73 m2 at listing (if not on dialysis) | 54.3 ± 17.6 | 54.5 ± 17.5 | 50.9 ± 18.7 | <0.001 |
| eGFR, ml/min per 1.73 m2 before transplant (if not on dialysis) | 53.3 ± 17.6 | 54.5 ± 17.6 | 45.8 ± 17.0 | <0.001 |
| eGFR ratio (before transplant/wait listing) | 1.10 ± 0.90 | 1.10 ± 0.91 | 0.99 ± 0.45 | <0.001 |
| Dialysis at listing, n (%) | 370 (1.9) | 339 (1.8) | 31 (4.0) | <0.001 |
| Dialysis before transplant, n (%) | 1038 (5.2) | 907 (4.8) | 131 (16.7) | <0.001 |
| Functional status by Karnofsky score before transplant, % | <0.001 | |||
| 80–100 | 3309 (16.7) | 3213 (16.8) | 96 (12.3) | |
| 51–79 | 6839 (34.4) | 6603 (34.6) | 316 (40.4) | |
| 0–50 | 8237 (41.5) | 7824 (41.0) | 396 (50.6) | |
| Unknown | 1476 (7.4) | 1438 (7.5) | 38 (4.9) | |
| UNOS region | <0.001 | |||
| 1 | 989 (4.5) | 865 (4.5) | 33 (4.2) | |
| 2 | 2371 (11.9) | 2229 (11.7) | 142 (18.1) | |
| 3 | 2233 (11.4) | 2177 (11.4) | 56 (7.2) | |
| 4 | 2340 (11.8) | 2252 (11.8) | 88 (11.2) | |
| 5 | 3136 (15.8) | 3017 (15.8) | 119 (15.2) | |
| 6 | 656 (3.3) | 640 (3.4) | 16 (2.0) | |
| 7 | 1900 (9.6) | 1831 (9.6) | 69 (8.8) | |
| 8 | 1107 (5.6) | 1067 (5.6) | 40 (5.1) | |
| 9 | 1202 (6.1) | 1127 (5.9) | 75 (9.6) | |
| 10 | 1626 (8.2) | 1583 (8.3) | 43 (5.5) | |
| 11 | 2392 (12.0) | 2290 (12.0) | 102 (13.0) | |
| Waitlisted time (including inactive status), median (IQR), d | 87 (25–251) | 87 (25–250) | 104 (27–285) | |
| Post-transplant patient survival at 1 yr (based on Kaplan Meier estimates), % | 87.3 | 88.3 | 71.0 | <0.001 |
| Composite renal outcome incidence within 1 yr of heart transplantation, mean (the year 2000, the year 2019), % | 3.9 (2.6–6.1) |
Data are presented as n (%), median (IQR) as appropriate.
BiVAD, biventricular assist device; CABG, coronary artery bypass graft; CRO, composite renal outcome; ECMO, extracorporeal membrane oxygenation; eGFR, estimated glomerular filtration rate; HT, heart transplant; IABP, intra-aortic balloon pump; IQR, interquartile range; LV, left ventricular; LVAD, left ventricular assist device; TAH, total artificial heart; UNOS, United Network of Organ Sharing; VAD, ventricular assist device.
P value applies to the comparison of no-CRO and CRO groups.
Other: restrictive cardiomyopathy, congenital, arrhythmia, valvular, and heart transplant-related diagnosis.
Predictors of Post-HT CROs
A total of 15 predictors of post-HT ROC were selected by the RBFOpt library and sorted by RF feature importance score (Supplementary Table S3) among 39 variables in the United Network for Organ Sharing-STAR Dataset (Supplementary Table S4).
Performance of the RF Model
The final RF model performed with a C-statistic of 0.70 (95% CI 0.67–0.74) (Supplementary Figure S3). At the fixed sensitivity of 80.0%, the model resulted in 46.2% specificity, 97.8% negative predictive value, and 8.1% positive predictive value. For the given negative predictive value performance, our RF model mislabeled 2.2% of cases (=100%–97.8%). On the basis of 2019 statistics, the absolute and relative reduction in risk prediction was 3.9% (=6.1%–2.2%) and 64% (=[6.1%–2.2% / 6.1%] × 100), respectively.
Robustness of the Model
To find the robustness of our model, we conducted 2 separate analyses. First, we trained the RF model using a data set that excluded patients who died in the no-CRO group; the model resulted in a C-statistic of 0.71 (95% CI 0.69–0.75). At the fixed sensitivity of 80.0%, the model had 46.3% specificity, 98.1% negative predictive value, and 8.0% positive predictive value. In the second analysis, we developed a RF survival model by treating the death event in the first year as a competing event to CRO occurrence and reported the accuracy of CRO prediction at 1 year. The competing event RF model classified CRO with 70.6% accuracy.
Characteristics of the Patients Who Died
Because post-transplant mortality is relevant to the analysis, we also described comparative characteristics of the patients who died in both groups within 1 year post-transplant (Supplementary Table S5). The post-HT patients with CRO who died were more likely to have diabetes and worse Karnofsky scores and require dialysis pretransplant than the patients in the no-CRO group who died.
Discussion
Our decision tool with a web-based interface is practical as it uses readily existing recipient pretransplant variables and provides a personalized risk of developing CRO within 1 year of HT. The performance RF model did not significantly change with by censoring death in both robustness analyses.
The variables selected in the RF model mostly align with previously described factors, including pretransplant renal function and need for renal replacement treatment, age, sex, race, diabetes mellitus, body mass index, functional status, ventricular assist device requirement, and pretransplant cardiac index.4,7 Deranged cardiac along with heightened risk of individuals with elevated right- and left-sided filling pressures and biventricular dysfunction may predispose these individuals to a greater risk of postoperative AKI.8 If these individuals experience recurrent AKI post-transplantation, these episodes may result in lower GFR at 1 year post-HT and potentially transition into CKD, especially the ones complicated with stage 3 AKI according to the Kidney Disease Improving Global Outcomes guidelines.9
In the setting of pre-HT, a negative prediction by our RF model, which has high negative predictive value, can serve as additional evidence that the patient has a lower risk of CRO post-HT and no need for SHKT. Clinical judgment (thorough physical examination and history taking, medication review, trending renal function on multiple data points, renal imaging, urine analysis, renal biopsy findings if available, etc.) should play a more significant role when the RF model predicts a positive outcome owing to the high false-positive rate and low positive predictive value. This scenario is related to the inability to capture reversibility in certain features (such as postoperative improvement in renal perfusion and renal function), uncertainty around donor quality, and perioperative course.
We also evaluated our RF model with an external cohort (an external validation), 353 patients who underwent SHKT between January 10, 2019, and September 30, 2020. Our predictive model classified 93% of SHKT patient into the positive class and 7% of SHKT patients into the negative class, which suggests that the clinical re-evaluation of 7% of patients for SHKT eligibility is necessary.
Strengths of this study include large sample size and utilization of the RF method with a multidimensional dataset. Nevertheless, the limitations are as follows: (i) potential bias inherent to the observational study design owing to unmeasured patient characteristics; (ii) vulnerability to significant changes in heart donor allocation policies affecting center practice and patient characteristics; and (iii) not capturing uncertainties potentially introducing prolonged AKI resulting from donor characteristics and postoperative complications.
In conclusion, the proposed web-based decision tool powered by an RF-based machine learning method is an objective and cross-validated tool for patient-level identification of CRO risk among at-risk HT candidates.
Disclosure
The author, JLG, served as a consultant in the advisory board of Pfizer, Inc., Alnylam, Eidos Therapeutics, and Sarepta. All the other authors declared no competing interests.
Acknowledgments
This research is partly supported by the University of Texas System Southwestern The George M. O'Brien Kidney Research Core Center NIH P30DK079328 and the Texas Health Resources Scholarship (JLG). This work was supported in part by Health Resources and Services Administration contract 234-2005-37011C. The content is the responsibility of the authors alone. It does not necessarily reflect the Department of Health and Human Services' views or policies, nor does it mention trade names, commercial products, or organizations imply endorsement by the US Government.
Footnotes
Supplementary Methods.
Supplementary References.
Figure S1. Flow chart showing the final study cohort selection (SHKT = simultaneous heart-kidney transplant; eGFR = estimated glomerular filtration rate).
Figure S2. The number of adult heart transplants, the incidence of simultaneous heart kidney transplants, and the composite renal outcome (defined as dependence on chronic dialysis, estimated glomerular filtration rate [eGFR] < 20 ml/min/1.73 m2, or received kidney transplantation) at one-year in the United States between 2000 and 2019.
Figure S3. C-statistic for the ten-fold cross-validation study cohort.
Table S1. Pre-transplant distribution of kidney function and dialysis status of recipients of adult heart transplant alone (excluding all multiorgan transplants, the ones waitlisted for other organs, pediatric group, and missing creatinine values at transplant) between 2000 and 2019 in the U.S.
Table S2. Characteristics of the deceased donors of the study cohort between 2000 and 2019 in the U.S.
Table S3. Variable (feature) ranking in the final random forest prediction model based on the feature importance score (the higher the score, the more important the feature is for accurate prediction).
Table S4. The variables (pre-transplant recipient characteristics, total of 39) selected by the domain experts from the UNOS-STAR Dataset (Thoracic_Data).
Table S5. Characteristics of the adult heart transplant alone patients who died within first year of transplantation in the study cohort (N=2525).
Supplementary Material
Supplementary Methods.
Supplementary References.
Figure S1. Flow chart showing the final study cohort selection (SHKT = simultaneous heart-kidney transplant; eGFR = estimated glomerular filtration rate).
Figure S2. The number of adult heart transplants, the incidence of simultaneous heart kidney transplants, and the composite renal outcome (defined as dependence on chronic dialysis, estimated glomerular filtration rate [eGFR] < 20 ml/min/1.73 m2, or received kidney transplantation) at one-year in the United States between 2000 and 2019.
Figure S3. C-statistic for the ten-fold cross-validation study cohort.
Table S1. Pre-transplant distribution of kidney function and dialysis status of recipients of adult heart transplant alone (excluding all multiorgan transplants, the ones waitlisted for other organs, pediatric group, and missing creatinine values at transplant) between 2000 and 2019 in the U.S.
Table S2. Characteristics of the deceased donors of the study cohort between 2000 and 2019 in the U.S.
Table S3. Variable (feature) ranking in the final random forest prediction model based on the feature importance score (the higher the score, the more important the feature is for accurate prediction).
Table S4. The variables (pre-transplant recipient characteristics, total of 39) selected by the domain experts from the UNOS-STAR Dataset (Thoracic_Data).
Table S5. Characteristics of the adult heart transplant alone patients who died within first year of transplantation in the study cohort (N=2525).
References
- 1.Cantarovich M., Hirsh A., Alam A., et al. The clinical impact of an early decline in kidney function in patients following heart transplantation. Am J Transplant. 2009;9:348–354. doi: 10.1111/j.1600-6143.2008.02490.x. [DOI] [PubMed] [Google Scholar]
- 2.Hornberger J., Best J., Geppert J., McClellan M. Risks and costs of end-stage renal disease after heart transplantation. Transplantation. 1998;66:1763–1770. doi: 10.1097/00007890-199812270-00034. [DOI] [PubMed] [Google Scholar]
- 3.Lachance K., White M., Carrier M., et al. Long-term evolution, secular trends, and risk factors of renal dysfunction following cardiac transplantation. Transpl Int. 2014;27:824–837. doi: 10.1111/tri.12340. [DOI] [PubMed] [Google Scholar]
- 4.Habib P.J., Patel P.C., Hodge D., et al. Pre-orthotopic heart transplant estimated glomerular filtration rate predicts post-transplant mortality and renal outcomes: an analysis of the UNOS database. J Heart Lung Transplant. 2016;35:1471–1479. doi: 10.1016/j.healun.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 5.Ariyamuthu V.K., Amin A.A., Drazner M.H., et al. Induction regimen and survival in simultaneous heart-kidney transplant recipients. J Heart Lung Transplant. 2018;37:587–595. doi: 10.1016/j.healun.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Kobashigawa J., Dadhania D.M., Farr M., et al. Consensus conference on heart-kidney transplantation. Am J Transplant. 2021;21:2459–2467. doi: 10.1111/ajt.16512. [DOI] [PubMed] [Google Scholar]
- 7.Guven G., Brankovic M., Constantinescu A.A., et al. Preoperative right heart hemodynamics predict postoperative acute kidney injury after heart transplantation. Intensive Care Med. 2018;44:588–597. doi: 10.1007/s00134-018-5159-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fortrie G., Manintveld O.C., Caliskan K., Bekkers J.A., Betjes M.G. Acute kidney injury as a complication of cardiac transplantation: incidence, risk factors, and impact on 1-year mortality and renal function. Transplantation. 2016;100:1740–1749. doi: 10.1097/TP.0000000000000956. [DOI] [PubMed] [Google Scholar]
- 9.Chawla L.S., Bellomo R., Bihorac A., et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol. 2017;13:241–257. doi: 10.1038/nrneph.2017.2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.