Abstract
Loneliness is associated with a myriad of detrimental outcomes in mental and physical health. Previous studies have found that people with schizophrenia report greater loneliness than controls, and that loneliness is related to depressive symptoms. However, research has been limited, particularly regarding contributions of loneliness to social and occupational functioning. Further, few studies have examined associations between loneliness and daily experience in schizophrenia. Thus, we recruited 35 individuals with schizophrenia and 37 controls. All participants completed the UCLA loneliness scale, symptom assessments, and measures of social and occupational functioning. Additionally, participants with schizophrenia completed an ecological momentary assessment (EMA) protocol that indexed daily social and emotional experiences, including loneliness. Similar to previous reports, we found that those with schizophrenia reported greater loneliness than controls. Further, loneliness was positively associated with depressive and negative symptoms, and negatively associated with self-reported social functioning. Interestingly, loneliness remained a significant predictor of functioning even when controlling for other symptoms, suggesting that severity of depressive and negative symptoms cannot fully explain the relationship between loneliness and functioning. In our EMA analyses, loneliness did not significantly differ when individuals were alone versus with others, underscoring the notion that being alone is not the same as feeling lonely. However, self-reported engagement during social interactions was negatively associated with loneliness, at a trend-level, suggesting that quality of social interactions is a potentially important consideration. Taken together, these findings suggest that loneliness is an important treatment target, and provide understanding for how loneliness may manifest in daily life in schizophrenia.
Keywords: schizophrenia, loneliness, social functioning, negative symptoms
General Scientific Summary:
Loneliness is associated with a myriad of detrimental outcomes in mental and physical health. The current study provides support for loneliness as an important treatment target in people with schizophrenia. Further, we provide understanding for how loneliness may manifest in daily life
Introduction
Individual differences in social experience have long been considered core symptoms of schizophrenia (SZ), and are linked to long-term outcome (Childers & Harding, 1990). Historically, phenomenological description of social experience in people with SZ has focused on asociality, defined as reduced frequency of social interaction with the assumption that reduced frequency reflects lack of interest in being around others (Marder & Galderisi, 2017). Modern negative symptom assessment measures (e.g., the Clinical Assessment Interview for Negative Symptoms (CAINS), Brief Negative Symptom Scale (BNSS)) have furthered the conceptualization of asociality by separately assessing both social behavior, as well as interest and motivation for social interaction (Kirkpatrick et al., 2011; Kring et al., 2013a). In contrast, examination of loneliness in people with SZ has received far less attention. This lacuna in the literature is striking given strong evidence for associations between loneliness and many physical and mental health concerns in the general population (Cacioppo, Hawkley, & Berntson, 2003; Cacioppo, Grippo, London, Goossens, & Cacioppo, 2015; Hawkley & Cacioppo, 2010), and high comorbidity between such health concerns and SZ. Thus, examining how loneliness relates to symptoms and social functioning, as well as how loneliness may manifest in daily life remain important avenues for research attempting to understand and intervene on social experience in SZ. In the current manuscript, we aimed to examine loneliness in people with SZ.
Loneliness is defined as “a distressing feeling that accompanies the perception that one’s social needs are not being met by the quantity or especially the quality of one’s social relationships” (Hawkley & Cacioppo, 2010b). Importantly, this definition underscores that being alone is not equivalent to feeling alone. For example, a person may feel lonely in the company of others, or conversely not feel lonely when by oneself. Using this definition, studies have shown that loneliness is an independent risk factor for a multitude of medical and mental health concerns including depression, social anxiety, elevated blood pressure, alcohol use, heightened hypothalamic pituitary adrenocortical axis activity, and diminished immune response in the general population (for review see Cacioppo et al., 2015).
The literature examining loneliness in people with SZ has been limited (for review see (Badcock et al., 2020)). This is in many ways surprising given that prevalent aspects of the disorder such as paranoia, stigma, defeatist performance beliefs, poor occupational functioning, heightened sensory sensitivity, and negative symptoms often lead to an isolating experience for people with SZ (Chrostek et al., 2016; Davidson & Stayner, 1997). Several papers have reported increased loneliness in people with SZ compared to controls (Badcock et al., 2015; Chrostek et al., 2016; Eglit et al., 2018; Lim et al., 2018; Ludwig et al., 2020; Mote et al., 2019; Trémeau et al., 2016). Further, loneliness has been linked to important clinical characteristics in people with SZ (or combined samples of individuals with various psychotic disorders) including diabetes risk, hypertension, substance use, cognitive functioning, and symptom severity (Badcock et al., 2015; Ludwig et al., 2020; Michalska Da Rocha et al., 2018; Trémeau et al., 2016). A preliminary ecological momentary assessment (EMA) study showed that people with SZ report significantly higher ratings of loneliness in daily life, compared to controls (Kimhy et al., 2006a). Further, Fulford and colleagues have shown that loneliness, measured in the lab via self-report, correlates with objective measures of movement (e.g., GPS, actigraphy) collected in daily life in people with SZ and controls (Fulford et al., 2020). Specifically, individuals reporting more loneliness, in the lab, showed decreased movement in daily life (Fulford et al., 2020). Finally, Mote and colleagues recently showed that trait-level loneliness in people with SZ was negatively associated with self-reported happiness and intimacy during social interactions (Mote, Gard, Gonzalez, & Fulford, 2019). However, this study had a limited sample size and state-level loneliness was not probed in the EMA interview. Taken together, previous literature suggests elevated reports of loneliness in those with SZ, as well as associations with important clinical characteristics.
Despite the aforementioned studies, a number of open questions regarding loneliness in people with SZ remain. First, several EMA studies in SZ have measured variables highly associated with loneliness such as including loneliness in composite ratings of negative affect (Myin-Germeys et al., 2001) or assessing dissatisfaction with social circumstance (Edwards et al., 2018; Janssens et al., 2012; M. Schneider et al., 2017). However, only one study, to our knowledge, has explicitly examined momentary experience of loneliness independently in SZ using EMA (Kimhy et al., 2006b), and there may be benefits to probing experience of loneliness specifically in the EMA interview. It is also unclear how measures of trait loneliness (e.g., the UCLA loneliness scale) relate to state measures collected in daily life. Second, it is unknown whether loneliness in people with SZ varies as a function of social context (e.g., Do individuals feel more or less lonely when interacting with other people?). In this vein, Mote and colleagues found that, in people with SZ, quality of social interactions (intimacy experienced) was related to trait-level loneliness but quantity of social interactions was not (Mote et al., 2019). However, experience of loneliness in daily life was not assessed in this study. Thus, associations between momentary experiences of loneliness and state-level variables characterizing social context are not well understood in SZ. Finally, it is not clear how measures of state and trait loneliness correlate with other symptom and functional outcome measures in people with SZ. Particularly, it is unknown whether loneliness predicts measures of functioning independently of other symptoms. Critically, collection of such data is a necessary step in determining the utility of loneliness as an independent treatment target in people with SZ.
In the current study, we aimed to address these gaps in the literature by characterizing social interaction and experience of loneliness in the daily lives of people with SZ. Specifically, we first collected trait measures of loneliness in both people with SZ and controls. Consistent with prior literature, we hypothesized that individuals with SZ would report greater loneliness on this trait-based measure (Badcock et al., 2015; Eglit et al., 2018; Lim et al., 2018; Ludwig et al., 2020; Mote et al., 2019; Trémeau et al., 2016). Next, participants with SZ completed a weeklong EMA protocol during which they were probed about aspects of their social experience (including momentary experiences of loneliness). Here, we aimed to quantify: 1.) the relationship of social context and social engagement to experience of loneliness, 2.) associations between momentary experiences of loneliness and positive and negative affect, given previous reports of strong associations between trait loneliness and negative affect using lab-based measures (Russell et al., 1980a), 3.) associations between state-based loneliness (measured via EMA) and trait-based loneliness (measured via the UCLA Loneliness Scale). Finally, we aimed to examine the relationship between loneliness and social and occupational functioning in SZ. We hypothesized that loneliness would be associated with poorer functioning, as well as greater negative, depressive, and positive symptoms.
Methods
Participants
Study participants included 35 stable outpatients with SZ or schizoaffective disorder as defined by the DSM-IV (American Psychiatric Association, 2000) and 37 controls. Exclusion criteria included: (1) DSM-IV diagnosis of substance abuse or dependence in the past 6 months; (2) IQ less than 70 as measured by the Wechsler Test of Adult Reading (WTAR: Weschler, 2001); and (3) history of severe head trauma and/or loss of consciousness. Participants completed and passed a urine drug screen before each research session. Additional criteria for the patient group included: (1) no medication changes in the two weeks prior to initial study participation or anticipated changes during study completion (2) stable outpatient or partial hospital status. Additional criteria for controls included: (1) no history of SZ, schizoaffective disorder, or bipolar disorder (2) no current major depression (3) no first-degree relative with a history of SZ or schizoaffective disorder (4) no current psychotropic medication. All participants provided written informed consent to the protocol approved by the Washington University Institutional Review Board (IRB protocol number: #20110159, Protocol Title: “Intersection of Cognitive and Negative Symptoms”). Demographics are presented in Table 1. There were no group differences in age, gender, parental education, or ethnicity.
Table 1.
Sample characterization
| HC Group (n= 37) | SZ Group (n = 35) | Test Statistic | p-value | |
|---|---|---|---|---|
|
| ||||
| Demographic and Clinical Characteristics | ||||
|
| ||||
| Age, mean (SD) | 36.2 (11.3) | 37.8 (11.8) | t = −0.6 | 0.57 |
| Education, mean (SD) | ||||
| Participant | 15.4 (2.4) | 12.7 (2.8) | t = 4.4 | < 0.001 |
| Parental | 13.6 (2.2) | 14.4 (3.5) | t = −1.12 | 0.27 |
| Sex, No. | χ2 = 0.45 | 0.5 | ||
| Male | 28 | 24 | ||
| Female | 9 | 11 | ||
| Race/Ethnicity, No. | χ2 = 5.1 | 0.08 | ||
| White | 8 | 16 | ||
| Black | 24 | 17 | ||
| Other | 5 | 2 | ||
| Employment Status | ||||
| Employed | 24 | 4 | ||
| Temporarily/Permanent Disabled | 0 | 22 | ||
| Unemployed | 5 | 6 | ||
| Current Student | 3 | 1 | ||
| Other/Unknown | 5 | 2 | ||
| Marital Status | ||||
| Married | 8 | 9 | ||
| Living with Partner | 2 | 1 | ||
| Divorced/Separated | 2 | 2 | ||
| Never Married | 22 | 23 | ||
| Unknown | 3 | 0 | ||
|
| ||||
| Symptom Assessments | ||||
|
| ||||
| BDI-II, mean (SD) | 3.4 (4.3) | 13.4 (9.2) | t = −5.4 | < 0.001 |
| MAP-SR, mean (Sd) | 42.3 (8.9) | 36.8 (8.9) | t = 2.6 | 0.011 |
| UCLA Loneliness Scale, mean (SD) | 37.6 (8.7) | 44.2 (9.9) | t = −3.0 | 0.004 |
| CAINS, mean (SD) | ||||
| Total Score | 23.3 (7.9) | |||
| MAP Subscale | 17.7 (5.2) | |||
| EXP Subscale | 5.7 (4.0) | |||
| BPRS, mean (SD) | ||||
| Total Score | 38.9 9.4) | |||
| Positive Symptom Subscale | 6.9 (4.3) | |||
Abbreviations: SD = Standard Deviation; BDI-II = Beck Depression Inventory – Second Edition; MAP-SR = Motivation and Pleasure Scale – Self Report; CAINS = Consensus Assessment Interview for Negative Symptoms; BPRS = Brief Psychiatric Rating Scale.
Diagnostic and Clinical Assessment
Diagnostic status was confirmed using the Structured Clinical Interview for DSM-IV-TR conducted by masters or Ph.D. level clinicians (First et al., 2001). All participants were administered the Beck Depression Inventory – Second Edition (BDI-II: (Beck et al., 1996)) to assess depressive symptoms, the Motivation and Pleasure Scale – Self-Report (MAP-SR: (Llerena et al., 2013)) to assess experiential negative symptoms, and the UCLA Loneliness Scale – Revised Edition (Russell et al., 1980b). On the MAP-SR, higher scores indicate greater motivation and pleasure. On all other administered scales, higher scores indicate greater symptoms or impairment.
People with SZ were also assessed for general psychiatric symptoms using the Brief Psychiatric Rating Scale (BPRS; (Overall & Gorham, 1962)), which includes a positive symptom composite score. Negative symptoms were assessed using the Clinical Assessment Interview for Negative Symptoms (CAINS: Kring, Gur, Blanchard, Horan, & Reise, 2013) which includes a Motivation and Pleasure (MAP) and Expression (EXP) subscale, with higher scores indicating greater impairment. Functioning was assessed using the Specific Levels of Functioning (SLOF) scale (L. C. Schneider & Struening, 1983). The SLOF is a self-report measure and thus, may reflect satisfaction/quality of life more so than objective markers of social function (i.e., skills-based or interview rated measure.
Ecological Momentary Assessment (EMA) Protocol and Questionnaire
All SZ participants were provided an Android-enabled smartphone and underwent an EMA protocol. Participants were prompted to complete an EMA questionnaire 4 times per day for 7 days between the hours of 10:00 AM and 7:00 PM. The questionnaires occurred pseudo randomly approximately every 3 hours. Participants were allotted 15 minutes to begin the survey, after which their responses would not be counted. Participants were paid $1.75 for each EMA questionnaire they completed within 15 minutes of the notification.
For the EMA questionnaire, participants were first asked about their emotional experience at the time of the survey on a 5-point Likert scale (1 = not at all to 5 = extremely). Discrete emotions assessed were as follows: happy, calm, sad, and anxious. Ratings for happy and calm were summed at each timepoint to create a positive affect composite score. Ratings for sad and anxious were summed at each timepoint to create a negative affect composite score. Next, participants were asked to select a current social context from a predetermined list (“Who are you with right now? Alone, Spouse/Significant Other, Friend(s), Family Member(s), Stranger(s), Healthcare Workers, Co-workers/Classmates). If participants reported being with others, they were asked about their level of engagement with other people (“How engaged are you with these people?”) on a 5-point Likert Scale (1 = not at all to 5 = extremely). Finally, regardless of social context, participants were asked about current feelings of loneliness (“How lonely do you feel right now?) on a 5-point Likert scale (1 = not at all to 5 = extremely) (EMA Loneliness).
Consistent with previous EMA research, all participants completed at least 33% of surveys and thus were included in the present analyses (Inez Myin-Germeys et al., 2001). Mean response rate was 78% and a total of 773 responses were recorded across all participants.
UCLA Loneliness Scale Analyses
An independent-samples t-test with the total score of the UCLA Loneliness Scale as a dependent variable and an independent variable of diagnostic group was conducted in order to examine diagnostic group differences in loneliness. For both groups, bivariate correlations were conducted between UCLA Loneliness Scale total score and BDI-II total score and MAP-SR total score. In the SZ group, bivariate correlations were conducted between UCLA Loneliness total score and CAINS total score, BPRS Total Score, SLOF total score in order to observe relationships between loneliness and symptom severity, as well as loneliness and level of functioning. Finally, we conducted two multiple regression analyses with SLOF as the dependent variable and UCLA loneliness, BDI-II, and CAINS total as simultaneously-entered predictors, in order to determine whether there was an independent association between loneliness and level of functioning when controlling for other symptoms.
Ecological Momentary Assessment Analyses
We used multilevel modeling (MLM) in R (lme4 package) to investigate relationships between within-subject observations of EMA (Level 1) and between-subject observations including level of functioning (Level 2). MLM is suitable for EMA designs because it accounts for the nested data structure of multiple observations within each subject. Moreover, MLM allows for missing or unbalanced data, which is common in EMA designs where not all participants answer every survey prompt. We conducted several models. In all MLM models momentary reports of loneliness (EMA Loneliness) was the dependent variable. In our first model, we entered social context (dummy coded: 1 = with others, 0 = alone) as a predictor variable, which was allowed to vary randomly across participants. As a follow-up, in a second model, we entered self-reported level of engagement with others as a predictor variable, which was allowed to vary randomly across participants. In a third model, we entered momentary reports of positive and negative affect as predictor variables, which were allowed to vary randomly across participants. In a fourth model, we entered SLOF as a predictor variable, given that the SLOF consists of a single value per participant, this effect was fixed across participants. Finally, in a fifth model, we entered UCLA Loneliness Total Score as a predictor variable, given that the UCLA Total Score consists of a single value per participant, this effect was fixed across participants.
Results
1. UCLA Loneliness Scale (Trait Loneliness)
1.1. Diagnostic Group Differences
Consistent with previous literature, people with SZ reported higher levels of loneliness than healthy controls on the UCLA Loneliness Scale (t(70) = −3.0, p = 0.004, Cohen’s d = −0.7, 95% [−1.2 to −0.23]); Figure 1A). UCLA Loneliness Scale scores were negatively correlated with the MAP-SR (SZ Group: r = −0.34, p = 0.04; HC Group: r = −0.56, p < 0.001; Figure 1B) and positively correlated with self-reported depressive symptoms (BDI-II Total; SZ Group: r = 0.49, p = 0.003; HC Group: r = 0.38, p = 0.04; Figure 1C).
Figure 1. Correlations between loneliness and other symptom domains.

A.) Individuals with schizophrenia report greater loneliness than controls; B.) Loneliness was negatively associated with MAP-SR; C.) Loneliness was positively correlated with depressive symptoms (BDI-II); D.) Loneliness was not associated with interview-based negative symptoms (CAINS Total). Shaded regions indicate 95% confidence intervals and error bars indicate standard error of the mean.
1.2. Associations with Symptoms and Level of Functioning
In the SZ group, the correlation between the UCLA Loneliness Scale and CAINS total score was not significant, (CAINS Total Score: r = 0.07, p = 0.68, CAINS Motivation and Pleasure Subscale: r = 0.07, p = 0.70, CAINS Expressivity Subscale: r = 0.05, p = 0.78). Similarly, UCLA Loneliness was not related to general symptomatology (BPRS Total: r = 0.26, p = 0.13) or severity of positive symptoms (BPRS Positive Symptom Subscale: r = 0.22, p = 0.20).
Regarding levels of social/occupational functioning, loneliness was negatively correlated with participant-rated functioning (SLOF: r = −0.65, p < 0.001). Importantly, the association between loneliness and self-reported level of functioning (SLOF-P) remained significant when covarying severity of depressive and negative symptoms, suggesting severity of depressive and negative symptoms cannot fully explain the relationship between loneliness and functioning (Table 2).
Table 2.
Multiple regression analyses predicting level of social and occupational functioning
| Predicting SLOF Self-Report (N = 35) | ||||
|---|---|---|---|---|
| Standardized Beta | t-value | p-value | 95% CI | |
| CAINS Total | −0.192 | −1.59 | 0.12 | [−0.771, 0.096] |
| BDI-II | −0.486 | −3.50 | 0.001 | [−1.149, −0.303] |
| UCLA Loneliness Scale | −0.398 | −2.94 | 0.006 | [−0.939, −0.170] |
2. Ecological Momentary Assessment Measures of Loneliness (State Loneliness)
2.1. Loneliness and Social Context
Figure 2 illustrates survey responses by social context. Broadly, people with SZ reported being alone on approximately 52% of the survey responses (Top Left). For subject-level mean and ranges of EMA loneliness see Supplemental Materials Figure S1. Self-reported loneliness collected via EMA (EMA Loneliness) did not differ when participants were alone compared to when they were with other people (Figure 2). The qualitative pattern illustrated in Figure 2 was confirmed using a multilevel model. Specifically, we conducted a model predicting momentary experience of loneliness in daily life (EMA Loneliness) by social context. Social context was dummy coded (1 = with others, 0 = alone). In this model, social context failed to significantly predict EMA loneliness (beta = −0.12, SE = 0.11, p = 0.25). Next, we examined whether the quality of the social interaction was associated with feelings of loneliness. For this analysis, we conducted a model predicting EMA Loneliness by self-reported level of engagement in social interactions. In this model, level of engagement was a small, negative predictor of loneliness, but did not reach significance (beta = −0.08, SE = 0.04, p = 0.06). Finally, it may be that particular social relationships have a greater effect on momentary experience of loneliness. To test this hypothesis, we recoded social context (1 = Family/Friend/Spouse, 2 = Alone/Stranger, and removed observations where interactions included co-workers or healthcare workers). In this analysis, social interactions with Family/Friend/Spouse were associated with significantly lower momentary experience of loneliness (beta = −0.34, SE = 0.17, p = 0.04). Taken together, these results suggest that the being alone is not the same as feeling lonely, and that the quality of social interaction, as well as particular social relationships may be meaningful predictors of momentary loneliness in people with SZ.
Figure 2. Daily social interactions and self-reported experience of loneliness.
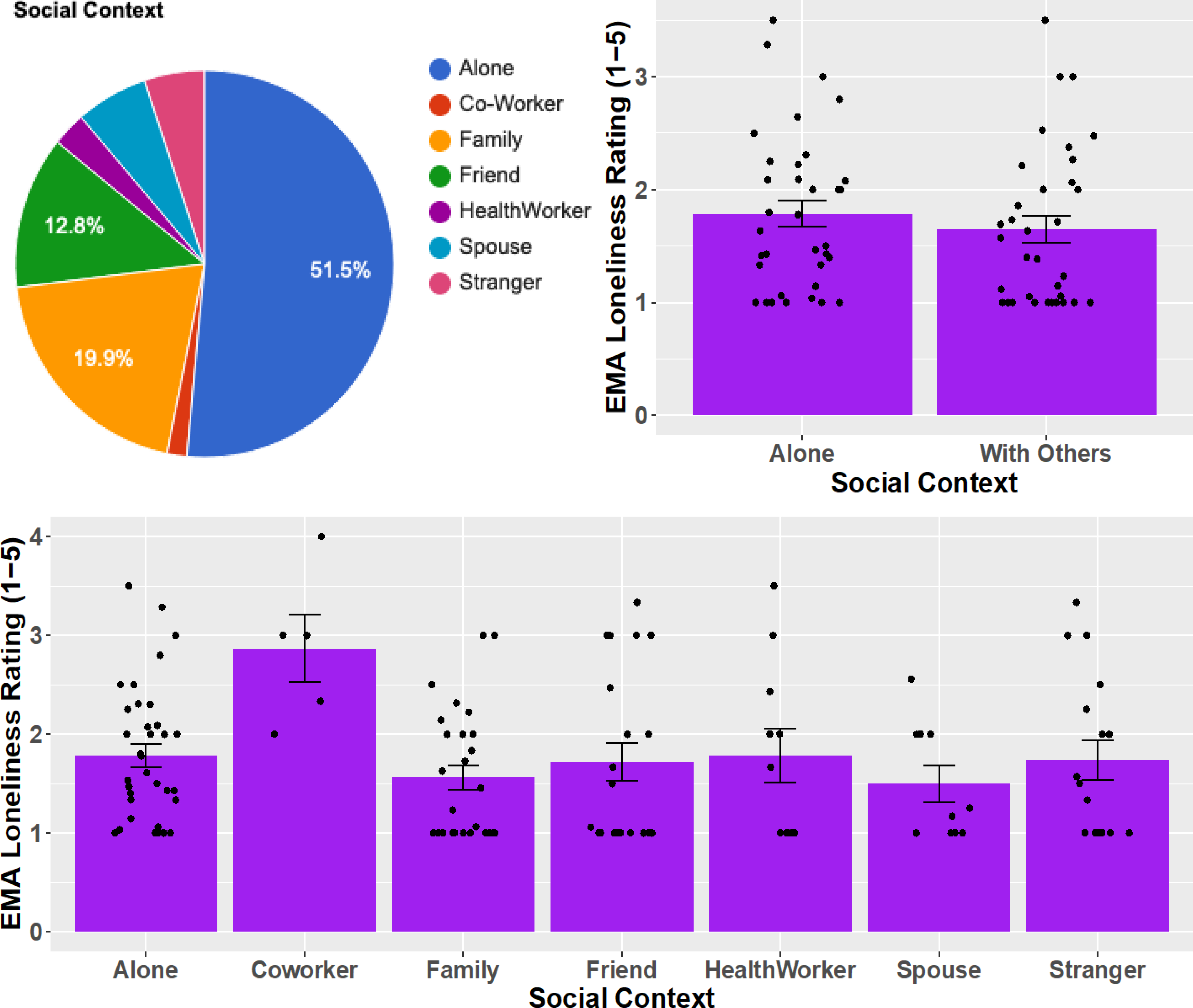
Top Left) Frequency of self-reported social context in people with schizophrenia; Top Right) Loneliness does not vary if alone vs. with others; Bottom) Loneliness for each social context measured. Dots indicate individual participant means. Error bars indicate standard error of the mean at the group level.
2.2. Associations Between EMA Loneliness and Positive/Negative Affect in Daily Life
Next, we examined associations between EMA loneliness and EMA measures of positive and negative affect. As expected, when entered into separate multilevel models, greater self-reported positive affect was associated with lower EMA loneliness (beta = −0.12, SE = 0.04, p = 0.003) and greater negative affect was associated with greater EMA loneliness (beta = 0.25, SE = 0.029, p < 0.001). When positive and negative affect were entered as simultaneous predictors of self-reported loneliness, only negative affect was a significant predictor of EMA loneliness (positive affect: beta = −0.06, SE = 0.035, p = 0.09); negative affect: beta = 0.19, SE = 0.03, p < 0.001), suggesting an independent and potentially more robust relationship between negative affect and self-reported experience of loneliness, compared to positive affect.
2.3. Associations Between EMA Loneliness and Level of Functioning
Given the aforementioned associations between the UCLA Loneliness Scale and social and occupational functioning (SLOF-P), we examined relationships between EMA loneliness and level of functioning. Surprisingly, SLOF-P was not a significant predictor of EMA loneliness (SLOF-P: beta = −0.01, SE = 0.01, p = 0.25).
3. Relationships Between State and Trait Measures of Loneliness
Trait loneliness (measured via the UCLA Loneliness Scale) showed a small, positive but non-significant relationship with state loneliness (measured via EMA) (beta = 0.02, SE = 0.01, p = 0.06).
Discussion
The goal of the current study was to examine potential relationships between loneliness and social and occupational functioning in SZ, as well as characterize experience of loneliness in daily life. Consistent with several previous reports, we found that those with SZ reported greater loneliness than controls on questionnaire-based measures (UCLA Loneliness Scale), and that loneliness was positively correlated with depressive (BDI-II) and negative symptoms (MAP-SR) (Badcock et al., 2015; Chrostek et al., 2016; Eglit et al., 2018; Lim et al., 2018; Ludwig et al., 2020; Mote et al., 2019; Trémeau et al., 2016). We extended these findings by demonstrating significant associations between loneliness and social and occupational functioning in people with SZ. Importantly, loneliness remained a significant predictor of functioning even when controlling for depressive and negative symptoms, suggesting severity of depressive and negative symptoms cannot fully explain the relationship between loneliness and functioning. While preliminary, our data suggest that loneliness may be a promising treatment target worthy of future investigation, when considering factors to improve functioning in SZ. Additionally, our EMA protocol characterized how loneliness may manifest in the daily lives of people with SZ. Specifically, we found that daily experience of loneliness did not significantly vary if someone was alone or with other people, underscoring the notion that being alone is not the same as feeling lonely. However, loneliness did vary when considering particular social relationship (i.e., interactions with Family/Friend/Spouse vs. Stranger/Alone). Further, self-reported level of engagement with others was negatively associated with daily experiences of loneliness, at a trend-level, suggesting that quality vs. quantity of social interaction may be a particularly important contributor to feelings of loneliness. We interpret these findings in the context of the broader literature below.
Historically, phenomenological description of social experience in people with SZ has focused on asociality, defined as reduced frequency of social interaction with the assumption that reduced frequency reflects lack of interest in being around others (Marder & Galderisi, 2017). While modern negative symptom measures (CAINS, BNSS) probe interest for social interaction, as well as social behavior, loneliness still remains an understudied aspect of social experience in SZ. We did not find a significant relationship between loneliness and clinician-rated negative symptoms (CAINS Total); however, we did find a significant relationship between loneliness and experiential negative symptoms measured via self-report (MAP-SR). Further, our data also suggest that loneliness is not wholly accounted for when merely assessing depressive and negative symptoms. In particular, we demonstrate a significant association between loneliness and social/occupational functioning, when covarying depressive and negative symptoms. These data suggest that: 1.) Accounts of social experience in SZ need to be broadened to include loneliness, 2.) Loneliness is not completely captured with measures used for assessing depressive and negative symptoms, and 3.) Given significant associations with functioning after covarying other symptoms, loneliness may be an important factor to consider when developing interventions to improve social and occupational functioning in people with SZ. There is currently no evidence-based intervention that has been firmly established for the treatment of loneliness in SZ (Badcock et al., 2020; Lim et al., 2018; Lim & Gleeson, 2014). However, skills including mindfulness and reappraisal strategies appear to be effective in alleviating loneliness people with other mental health concerns (Badcock et al., 2020). It will be important for future research to begin to test whether such interventions may be effective at alleviating loneliness in SZ, and whether such interventions will have downstream effects on social and occupational functioning.
Consistent with a definition of loneliness as perceived social isolation, we find that feelings of loneliness in people with SZ do not vary when participants are alone versus with others. Importantly, in our design loneliness and social context are reported concurrently via EMA, allowing us to make precise claims regarding the relationships between these variables. This result is similar to earlier work conducted in a large undergraduate sample, which showed that loneliness did not vary with daily activities performed or time spent alone (Hawkley et al., 2003). Our work is also consistent with two recent reports in the SZ literature that used an EMA protocol and showed that the percentage of time people spend with others did not predict trait-level loneliness measured in the lab via self-report (UCLA Loneliness) (Fulford et al., 2020; Mote et al., 2019). One of these reports found that trait-level loneliness did vary with the level of self-reported intimacy experienced in a social interaction, similar to our finding of self-reported loneliness decreasing with social engagement (Mote et al., 2019). These data bring up important considerations with regards to potential treatments for loneliness in people with SZ. Specifically, it does not appear that merely increasing social interactions or even decreasing barriers to social interactions will alleviate experience of loneliness in those with psychosis. Instead, these data point to targeting more active social engagement with meaningful relationships as a means for diminishing loneliness.
As stated in the introduction, loneliness is an independent risk factor for a multitude of physical health concerns including elevated blood pressure, heightened hypothalamic pituitary adrenocortical axis activity, and diminished immune response (Cacioppo et al., 2015). However, the temporal dynamics of these associations in the general population or those with SZ are not well understood. For example, it is not currently known whether cardiovascular function varies on an hour-by-hour or day-by-day basis with reports of loneliness. While one recent paper has included both passive (e.g., actigraphy) and active (e.g., self-report) data streams when examining social function in SZ and found that trait-level loneliness correlated with reduced measures of movement, this approach is underutilized (Fulford et al., 2020). Given the association between loneliness and a myriad of general health problems, passive ambulatory data streams such as measures of cardiovascular function may be particularly relevant to future studies examining the downstream impact of loneliness on daily measures of physical health in people with SZ.
One particularly surprising result of the current manuscript was the low degree of correspondence between measures of state (EMA) and trait (UCLA) loneliness. First, it should be noted that self-reporting loneliness in-the-moment via EMA may be quite different than self-reporting general tendencies towards loneliness on lab-based measures (e.g., the UCLA Loneliness Scale). Importantly, both of these methods of assessment have advantages. In-the-lab measures typically allow for more items and thus more comprehensive assessment of loneliness. EMA measures allow for quantification of contextual factors that may influence loneliness as it happens in daily life. Thus, while these measures may provide different sources of information, each is critical to furthering understanding of loneliness in SZ. Second, we believe that this low degree of correspondence may have resulted from differences in how state and trait loneliness were assessed. Specifically, the UCLA Loneliness Scale does not explicitly ask participant if they are “lonely” but instead assesses loneliness indirectly (e.g., “No one really knows me well”). In contrast, our EMA assessment of loneliness asks participants to identify themselves as lonely (i.e., “How lonely do you feel right now?”). Previous work has shown that participants respond to these questions differently. For example, Borys & Perlman, in a review of the sex differences in loneliness, reported that men typically score higher than women on measures that assess loneliness indirectly (e.g., the UCLA Loneliness Scale), and women typically score higher than men on measures that assess loneliness directly (i.e., self-labeling measures) (Borys & Perlman, 1985). While we were unable to assess such gender differences in the current manuscript due to small sample size, it may be the case that differences in how state and trait loneliness were assessed resulted in a low level of correspondence between these measures. Further, there has been several recent papers in the literature, which have attempted to delineate particular dimensions or types of loneliness (e.g., social vs. emotional loneliness), and it may be important for future work to determine which of these dimensions is most relevant for understanding social experience in people with schizophrenia (Buecker et al., 2020; S. Cacioppo et al., 2015a). Thus, it will be important for future work to consider: 1.) how questions related to loneliness are asked, 2.) which dimensions of loneliness are being assessed, and 3.) how these assessments of loneliness may vary by gender.
While the results of the current report and those of others clearly illustrate the relevance of loneliness to various symptoms and functioning in SZ, conceptual understanding and theories describing the onset and course of loneliness, as well as how loneliness may interact with or result from other symptoms in SZ is ill-defined (Fulford & Mueser, 2020). Future studies examining loneliness in daily life (via EMA), a novel aspect of the current report, will help better understand how loneliness relates to in-the-moment social experiences and symptoms. In regards to negative symptoms, it seems likely that theories detailing the development and maintenance of social defeatist performance beliefs may be particularly relevant, given that such beliefs can lead to isolation in the context of desire for social interaction. Further, although the association between positive symptom severity and loneliness in the current manuscript was non-significant, Cacioppo’s proposal that chronic loneliness could contribute to hypervigilance for social threats, which would then result in a self-reinforcing pattern of social withdrawal for relief of hypervigilance, could be relevant for paranoia and other aspects of positive symptomatology (Cacioppo et al., 2006). It is also unclear whether the mechanisms contributing to loneliness in people with SZ such as barriers to social interaction and/or social anxiey are similar or different to mechanisms contributing to loneliness in other groups. There will be a need for such theory-driven and conceptual work in the near future, as researchers attempt to place the results of recent empirical studies in a broader context and begin to develop psychosis-specific interventions to target loneliness.
Several limitations are notable. First, our sample size was limited. Future work will be needed to replicate the present findings in larger samples. One particularly important future direction is the examination of sex differences the experience of loneliness in SZ. In the general population, there has been some debate regarding whether sex differences in the experience of loneliness are present (Borys & Perlman, 1985). However, we were underpowered to examine how the effects described in the current manuscript may interact with gender. Second, control participants were not included in the EMA portion of the study precluding analyses of group differences in daily social interaction and experience. However, our study aims were to examine loneliness and its relationship to social functioning in SZ. Thus, while the inclusion of a control group would have been informative for some of the reported effects, it was not essential to the main findings of the manuscript. Third, our EMA sampling period (one week) was relatively brief. Future studies conducted over longer sampling intervals may yield opportunities for characterization of loneliness across greater temporal windows (e.g., seasonal changes in the experience of loneliness). Fourth, our design was not optimized to examine the temporal unfolding of loneliness and social interaction. Thus, the current analyses do not provide information as to whether loneliness is a consequence of less social engagement with non-strangers or if feelings of loneliness might actually lead to further social isolation and withdraw. Similarly, in regard to negative affect, the current design cannot provide information about whether the temporal dynamics and direction of the association between negative affect and loneliness. It will be important for future work to determine whether loneliness is simply a proxy for negative affect, or if there is a reciprocal relationship between negative affect and loneliness that can be examined using EMA. Thus, describing these temporal dynamics using EMA designs will be important directions for future work.
In summary, the goal of the current study was to examine potential contributions of loneliness to social and occupational functioning, as well as characterize the experience of loneliness in the daily lives of people with SZ. Our finding that loneliness remained a significant predictor of functioning even when controlling for depressive and negative symptoms, suggesting that severity of depressive and negative symptoms cannot fully explain the relationship between loneliness and functioning. Further, consistent with previous literature, our EMA analyses revealed that loneliness did not significantly vary when individuals were alone versus with others, underscoring the notion that being alone is not the same as feeling lonely. However, loneliness did vary when considering particular social relationship (i.e., interactions with Family/Friend/Spouse vs. Stranger/Alone). Taken together, these findings suggest that loneliness is an important treatment target in schizophrenia. Further, the current study provides descriptive understanding for how loneliness may manifest in the lives of those with schizophrenia. Future work is needed to develop theoretical understanding of loneliness in SZ, as well as how loneliness may interact with other core facets of the disorder.
Supplementary Material
Acknowledgments
We thank the participants in this study who gave generously of their time. We also thank those that helped with all aspects of data collection including Julia Sheffeld, Maria Gehred, Lori Ingram, Anita Mahadevan, Lisa Gorham, and Callan Coghlan. Parts of this article have been reported in a presentation at the Society for Research in Psychopathology conference. The current study was funded by NIMH Grant R37MH066031 awarded to Deanna Barch.
Footnotes
Financial Disclosures
Dr. Moran and Dr. Culbreth report no conflicts of interest. Dr. Barch has consulted for Pfizer, Amgen, Roche and Takeda, and has a contract to analyze imaging data for Pfizer.
References
- Badcock JC, Adery LH, & Park S (2020). Loneliness in psychosis: A practical review and critique for clinicians. In Clinical Psychology: Science and Practice. John Wiley & Sons, Ltd. 10.1111/cpsp.12345 [DOI] [Google Scholar]
- Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, & Morgan VA (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophrenia Research, 169(1–3), 268–273. 10.1016/j.schres.2015.10.027 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the beck depression inventory The Psychological Corporation. San Antonio, TX, 1996. [Google Scholar]
- Borys S, & Perlman D (1985). Gender Differences in Loneliness. Personality and Social Psychology Bulletin, 11(1), 63–74. 10.1177/0146167285111006 [DOI] [Google Scholar]
- Buecker S, Maes M, Denissen JJA, & Luhmann M (2020). Loneliness and the Big Five Personality Traits: A Meta-analysis. European Journal of Personality, 34(1), 8–28. 10.1002/per.2229 [DOI] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Berntson GG (2003). The anatomy of loneliness. Current Directions in Psychological Science, 12(3), 71–74. 10.1111/1467-8721.01232 [DOI] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, & Spiegel D (2006). Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality, 40(6), 1054–1085. 10.1016/j.jrp.2005.11.007 [DOI] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015a). Loneliness: Clinical Import and Interventions. Perspectives on Psychological Science, 10(2), 238–249. 10.1177/1745691615570616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015b). Loneliness: Clinical Import and Interventions. Perspectives on Psychological Science, 10(2), 238–249. 10.1177/1745691615570616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childers SE, & Harding CM (1990). Gender, premorbid social functioning, and long-term outcome in DSM-III schizophrenia. Schizophrenia Bulletin, 16(2), 309–318. 10.1093/schbul/16.2.309 [DOI] [PubMed] [Google Scholar]
- Chrostek A, Grygiel P, Anczewska M, Wciórka J, & Świtaj P (2016). The intensity and correlates of the feelings of loneliness in people with psychosis. Comprehensive Psychiatry, 70, 190–199. 10.1016/j.comppsych.2016.07.015 [DOI] [PubMed] [Google Scholar]
- Davidson L, & Stayner D (1997). Loss, loneliness, and the desire for love: Perspectives on the social lives of people with schizophrenia. Psychiatric Rehabilitation Journal, 20(3), 3–12. 10.1037/h0095369 [DOI] [Google Scholar]
- Edwards CJ, Cella M, Emsley R, Tarrier N, & Wykes THM (2018). Exploring the relationship between the anticipation and experience of pleasure in people with schizophrenia: An experience sampling study. Schizophrenia Research, 202, 72–79. 10.1016/j.schres.2018.06.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eglit GML, Palmer BW, Martin AS, Tu X, & Jeste DV (2018). Loneliness in schizophrenia: Construct clarification, measurement, and clinical relevance. PLoS ONE, 13(3), e0194021. 10.1371/journal.pone.0194021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulford D, Mote J, Gonzalez R, Abplanalp S, Zhang Y, Luckenbaugh J, Onnela JP, Busso C, & Gard DE (2020). Smartphone sensing of social interactions in people with and without schizophrenia. Journal of Psychiatric Research. 10.1016/j.jpsychires.2020.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulford D, & Mueser KT (2020). The importance of understanding and addressing loneliness in psychotic disorders. In Clinical Psychology: Science and Practice. John Wiley & Sons, Ltd. 10.1111/cpsp.12383 [DOI] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, & Cacioppo JT (2003). Loneliness in Everyday Life: Cardiovascular Activity, Psychosocial Context, and Health Behaviors. Journal of Personality and Social Psychology, 85(1), 105–120. 10.1037/0022-3514.85.1.105 [DOI] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010a). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010b). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssens M, Lataster T, Simons CJP, Oorschot M, Lardinois M, van Os J, & Myin-Germeys I (2012). Emotion recognition in psychosis: No evidence for an association with real world social functioning. Schizophrenia Research, 142(1–3), 116–121. 10.1016/j.schres.2012.10.003 [DOI] [PubMed] [Google Scholar]
- Kimhy D, Delespaul P, Corcoran C, Ahn H, Yale S, & Malaspina D (2006a). Computerized experience sampling method (ESMc): Assessing feasibility and validity among individuals with schizophrenia. Journal of Psychiatric Research, 40(3), 221–230. 10.1016/j.jpsychires.2005.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhy D, Delespaul P, Corcoran C, Ahn H, Yale S, & Malaspina D (2006b). Computerized experience sampling method (ESMc): Assessing feasibility and validity among individuals with schizophrenia. Journal of Psychiatric Research, 40(3), 221–230. 10.1016/j.jpsychires.2005.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, & Marder SR (2011). The brief negative symptom scale: Psychometric properties. Schizophrenia Bulletin, 37(2), 300–305. 10.1093/schbul/sbq059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Gur RE, Blanchard JJ, Horan WP, & Reise SP (2013a). The Clinical Assessment Interview for Negative Symptoms (CAINS): Final development and validation. American Journal of Psychiatry, 170(2), 165–172. 10.1176/appi.ajp.2012.12010109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Gur RE, Blanchard JJ, Horan WP, & Reise SP (2013b). The Clinical Assessment Interview for Negative Symptoms (CAINS): Final Development and Validation. American Journal of Psychiatry, 170(2), 165–172. 10.1176/appi.ajp.2012.12010109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim MH, & Gleeson JF (2014). Social connectedness across the psychosis spectrum: Current issues and future directions for interventions in loneliness. Frontiers in Psychiatry, 5(NOV), 154. 10.3389/fpsyt.2014.00154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim MH, Gleeson JFM, Alvarez-Jimenez M, & Penn DL (2018). Loneliness in psychosis: a systematic review. In Social Psychiatry and Psychiatric Epidemiology (Vol. 53, Issue 3, pp. 221–238). Springer. 10.1007/s00127-018-1482-5 [DOI] [PubMed] [Google Scholar]
- Llerena K, Park SG, McCarthy JM, Couture SM, Bennett ME, & Blanchard JJ (2013). The Motivation and Pleasure Scale–Self-Report (MAP-SR): Reliability and validity of a self-report measure of negative symptoms. Comprehensive Psychiatry, 54(5), 568–574. 10.1016/J.COMPPSYCH.2012.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig KA, Nye LN, Simmons GL, Jarskog LF, Pinkham AE, Harvey PD, & Penn DL (2020). Correlates of loneliness among persons with psychotic disorders. Social Psychiatry and Psychiatric Epidemiology, 55(5), 549–559. 10.1007/s00127-019-01789-5 [DOI] [PubMed] [Google Scholar]
- Marder SR, & Galderisi S (2017). The current conceptualization of negative symptoms in schizophrenia. World Psychiatry, 16(1), 14–24. 10.1002/wps.20385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalska Da Rocha B, Rhodes S, Vasilopoulou E, & Hutton P (2018). Loneliness in Psychosis: A Meta-analytical Review. In Schizophrenia Bulletin (Vol. 44, Issue 1, pp. 114–125). Oxford University Press. 10.1093/schbul/sbx036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mote J, Gard DE, Gonzalez R, & Fulford D (2019). How did that interaction make you feel? The relationship between quality of everyday social experiences and emotion in people with and without schizophrenia. PLoS ONE, 14(9). 10.1371/journal.pone.0223003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myin-Germeys I, Nicolson NA, & Delespaul PAEG (2001). The context of delusional experiences in the daily life of patients with schizophrenia. Psychological Medicine, 31(3), 489–498. 10.1017/s0033291701003646 [DOI] [PubMed] [Google Scholar]
- Myin-Germeys Inez, an Os VJ, Schwartz JE, Stone AA, & Delespaul PA (2001). Emotional reactivity to daily life stress in psychosis. Archives of General Psychiatry, 58(12), 1137–1144. 10.1001/archpsyc.58.12.1137 [DOI] [PubMed] [Google Scholar]
- Overall JE, & Gorham DR (1962). The Brief Psychiatric Rating Scale. Psychological Reports, 10(3), 799–812. 10.2466/pr0.1962.10.3.799 [DOI] [Google Scholar]
- Russell D, Peplau LA, & Cutrona CE (1980a). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. 10.1037/0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, & Cutrona CE (1980b). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. 10.1037/0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Schneider LC, & Struening EL (1983). SLOF: a behavioral rating scale for assessing the mentally ill. Social Work Research & Abstracts, 19(3), 9–21. 10.1093/swra/19.3.9 [DOI] [PubMed] [Google Scholar]
- Schneider M, Reininghaus U, Van Nierop M, Janssens M, Myin-Germeys I, Alizadeh B, Bartels-Velthuis AA, Bruggeman R, Cahn W, De Haan L, Delespaul P, Kahn RS, Meijer CJ, Myin-Germeys I, Simons C, Van Haren N, Van Os J, & Van Winkel R (2017). Does the Social Functioning Scale reflect real-life social functioning? An experience sampling study in patients with a non-affective psychotic disorder and healthy control individuals. Psychological Medicine, 47(16), 2777–2786. 10.1017/S0033291717001295 [DOI] [PubMed] [Google Scholar]
- Trémeau F, Antonius D, Malaspina D, Goff DC, & Javitt DC (2016). Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Research, 246, 211–217. 10.1016/J.PSYCHRES.2016.09.043 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


