Abstract
The advent of COVID-19 and the persistent threat of infectious diseases such as tuberculosis, malaria, influenza and HIV/AIDS remind us of the marked impact that infections continue to have on public health. Some of the most effective protective measures are vaccines but these have been difficult to develop for some of these infectious diseases even after decades of research. The development of drugs and immunotherapies acting directly against the pathogen can be equally challenging, and such pathogen-directed therapeutics have the potential disadvantage of selecting for resistance. An alternative approach is provided by host-directed therapies, which interfere with host cellular processes required for pathogen survival or replication, or target the host immune response to infection (immunotherapies) to either augment immunity or ameliorate immunopathology. Here, we provide a historical perspective of host-directed immunotherapeutic interventions for viral and bacterial infections and then focus on SARS-CoV-2 and Mycobacterium tuberculosis, two major human pathogens of the current era, to indicate the key lessons learned and discuss candidate immunotherapeutic approaches, with a focus on drugs currently in clinical trials.
Subject terms: Infectious diseases, Immunotherapy
In this Perspective, the authors reflect on the historical development of host-directed immunotherapeutic interventions for viral and bacterial infections, and then focus on how historical insights can be applied to current approaches to therapy of SARS-CoV-2 and Mycobacterium tuberculosis infections.
Introduction
Infectious disease immunotherapies are broadly defined as host-directed interventions that modify aspects of intracellular, innate or adaptive immune responses to microbial pathogens to promote the anti-pathogen immune response or to prevent immunopathology. Renewed interest in this area of research is being driven by the growing global burden of drug-resistant pathogens and, with the exception of the ongoing COVID-19 pandemic, by the declining involvement of the pharmaceutical industry in antimicrobial research and development. Although the emergence of drug resistance can be countered in some cases by the use of drug combinations, for example for HIV-1 infection, host-directed immunotherapies should, in principle, remain fully effective against microorganisms with high-level antimicrobial drug resistance. Furthermore, immunotherapies hold promise for those cases where drugs are not available against the pathogen, as is the case for many viral infections such as hepatitis B, or where sterile cure is not achieved by drug treatment such as in people living with HIV-1. Moreover, in the case of tuberculosis (TB), where poorly tolerated antimicrobial drugs need to be delivered for many months, leading to poor compliance, host-directed therapies administered on their own or adjunctively may contribute to shorter and more effective treatment. In contrast to antimicrobial drugs, resistance to host-directed therapies is unlikely to be a major problem, particularly for those that target multiple cellular mechanisms essential for microbial pathogenesis. Thus, the potential of immunotherapies to ameliorate pathology, prevent permanent functional impairment and improve long-term survival from infectious disease should be key to their adoption into clinical practice, spurred on by the striking successes achieved during the past decade with cancer immunotherapies1,2.
Here, we examine the use and promise of host-directed immunotherapies in viral and bacterial infectious disease (key approaches summarized in Box 1), first from a general historical perspective (Fig. 1), then focusing on two major killers in infectious disease — COVID-19, caused by SARS-CoV-2 infection, and TB, caused by Mycobacterium tuberculosis infection — with emphasis on drugs currently in clinical trials, and finally indicating the key issues that need to be addressed in future studies. We do not discuss passive immunotherapies or therapeutic vaccines owing to space considerations.
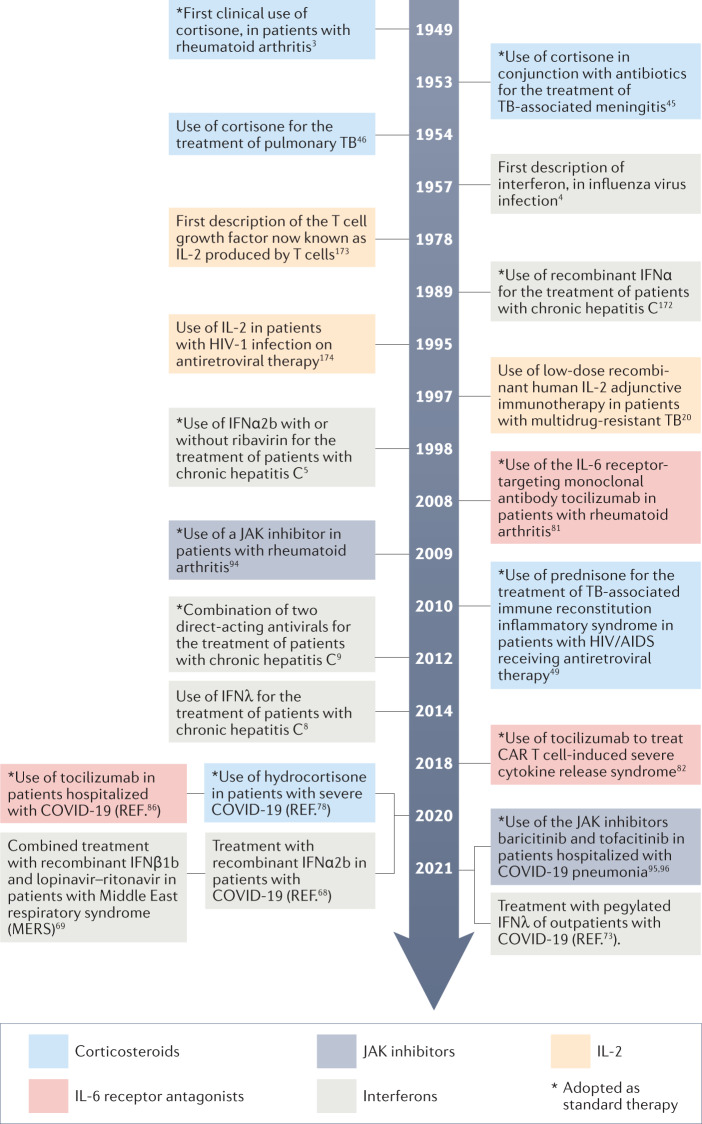
Fig. 1. Timeline of key developments in host-directed immunotherapeutic interventions for infectious disease.
Indicated are the time of discovery or first description for corticosteroids, interferons, IL-2, IL-6 receptor antagonists and Janus kinase (JAK) inhibitors, together with their successful uses in humans as immunotherapies for the indicated non-infectious and infectious diseases. Asterisks indicate therapies that were ultimately adopted into routine clinical use172–174. TB, tuberculosis.
Box 1 Key approaches to host-directed immunotherapy for infectious disease.
Augmenting immunity
Recombinant cytokines (for example, interferon treatment of chronic hepatitis C)
Cytokine administration by RNA or DNA application (experimental)
Macrophage-targeting strategies (for example, tyrosine kinase inhibitors and mechanistic target of rapamycin (mTOR) inhibitors in tuberculosis)
Cell-based immunotherapies (for example, CAR T cells in HIV-1; not discussed here)
Passive infusion of anti-pathogen antibodies (used for COVID-19 and respiratory syncytial virus infection, for example; not discussed here)
Vaccination (all infectious diseases; not discussed here)
Ameliorating immunopathology
Anti-cytokine antibodies (for example, IL-6 receptor blockade in COVID-19; anti-tumour necrosis factor treatment of paradoxical reactions to antimycobacterial therapy in tuberculous meningitis)
Cytokine modulators (for example, Janus kinase (JAK) inhibitors in COVID-19; phosphodiesterase inhibitors such as CC-11050 in tuberculosis; high-dose corticosteroids)
DNAse treatment or elastase inhibitors for removal of neutrophil extracellular traps (COVID-19)
Complement inhibitors (COVID-19)
Anticoagulants (COVID-19)
Anti-oxidants (for example, N-acetylcysteine in tuberculosis)
Anti-inflammatory drugs (for example, statins and cyclooxygenase 2 inhibitors in tuberculosis)
Historical perspectives
The largest relevant body of historical clinical experience comes from clinical trials of immunotherapies for influenza, viral hepatitis, TB and HIV/AIDS. These studies generally fall into two categories: cytokine-based therapies for augmenting immunity to eradicate infection and strategies for ameliorating pathology to prevent permanent tissue injury. In the past 20 years, animal studies and clinical trials have helped to identify circumstances in which cytokine therapy can be beneficial and have also contributed to current thinking regarding optimal timing of these interventions (Fig. 1). Similarly, studies of corticosteroids, showing both benefits and limitations3, have guided subsequent research targeting specific pathogenic mechanisms responsible for tissue destruction.
Cytokine-based strategies to augment immunity
Historically, most immunotherapeutic interventions to improve antiviral immunity have been applied in the setting of chronic infections such as viral hepatitis and HIV/AIDS. Acute viral infections may leave only a short time-window for enhancing the immune response; the practical challenges for rapid diagnosis and therapeutic intervention have historically limited clinical research in this setting, although these now seem to have substantial promise.
An early example of the development of cytokine-based therapies to augment the host antiviral response was the use of type I interferons (Fig. 1). Although the first studies demonstrating their ability to induce an antiviral state in cells were carried out in the late 1950s4, randomized controlled trials of the use of interferons to treat viral infections awaited their production to pharmaceutical standards in the late 1980s. These trials ultimately showed that polyethylene glycol (PEG)-conjugated IFNα (to increase plasma half-life) plus the antiviral agent ribavirin could induce sustained antiviral responses in about half of patients with chronic hepatitis C virus (HCV) infection5, providing the first curative treatment for this disease. However, the success of these interferon regimens depended on virus genotype, patient race and pre-treatment levels of IP-10, an interferon-induced protein6,7. Moreover, the interferon regimens had significant disadvantages, requiring injections for up to 6 months and often causing adverse effects that were poorly tolerated, including flu‐like symptoms, bone marrow depression, neuropsychiatric disorders and autoimmune syndromes. More recently, IFNλ has also been tested with some success in HCV infection8, but with the introduction during the past decade of antiviral regimens for HCV9, including oral inhibitors of NS3/4A, NS5A and NS5B, the era of interferon-based treatment of this virus was brought to a close6.
Furthermore, interferon administration has not been successful as a therapeutic for other chronic viral infections such as hepatitis B virus (HBV) and HIV/AIDS10. Indeed, in the case of HIV/AIDS, host-derived type I interferons may cause pathology in the chronic phase11,12. Similarly, influenza virus infections are not routinely treated with interferons. Although there is general agreement that prophylaxis and early treatment with type I or type III interferons are effective against influenza, preclinical studies show that the therapeutic treatment window is small in terms of dosage and timing, particularly for type I interferons13,14. Treatment later during severe influenza may lead to enhanced inflammation and impaired epithelial repair13–17. These early conclusions regarding the feasibility of interferon-based immunotherapies have recently been reiterated in the case of COVID-19, for which therapeutic success also seems to depend strongly on the timing of administration. Thus, the historical experience indicates that interferons may be an effective treatment for viral infections if given early, but that clinical administration late in persistent or chronic viral infection is successful only in some cases and may be poorly tolerated.
Much has also been learnt from clinical trials examining the therapeutic potential of IL-2, which is required for T cell proliferation, in individuals with HIV-1 infection (Fig. 1). Twenty-five therapeutic trials of IL-2 in HIV-1 infection were published between 1998 and 2009, including six studies with a total of 6,565 participants reporting mortality as an end point. A meta-analysis of these studies concluded that periodic IL-2 infusion combined with antiretroviral therapy (ART) increased the CD4+ T cell count but simultaneously increased the risk of high-grade adverse events (including gastrointestinal disorders, psychiatric disorders and deep venous thrombosis) without reducing mortality or the incidence of opportunistic infection18. It has been speculated that the absence of protection was due to the expansion of regulatory (FOXP3+) T cells18. The studies also prompted a reassessment of CD4+ T cell enumeration for measuring the success of immunotherapeutic drug development in HIV/AIDS.
Pro-inflammatory cytokines, such as IL-2 and IFNγ, have also been studied for their ability to increase immunity to mycobacterial infection often together with antibacterial drug therapy, mostly with limited success19. The proliferation of M. tuberculosis-specific T cells producing IFNγ depends on local production of IL-2, and adjunctive therapies using IL-2 to augment the immune response in TB were first considered in small trials conducted in the late 1990s and early 2000s20. However, a randomized, placebo-controlled trial of adjunctive recombinant IL-2 immunotherapy in patients with TB reported in 2003 failed to show statistically significant improvement in bacterial clearance at 1 or 2 months after treatment21. The most likely explanation is that IL-2 supports the proliferation not only of IFNγ-producing effector T cells but also of regulatory T cells that dampen the protective response22 although, in one preclinical study in non-human primates, some protection against TB pathology was observed despite the dual expansion of both T cell subsets in response to treatment with the cytokine23.
IFNγ is essential for the full activation of macrophages, which is crucial for controlling M. tuberculosis growth24–26. In patients with Mendelian susceptibility to mycobacterial disease, which is associated with IFNγ deficiency resulting from IL-12Rβ1 mutation, adjunctive treatment with IFNγ and antibiotics has proven efficacious27. These observations led to several therapeutic trials of adjunctive IFNγ in patients without apparent defects in interferon production or action, with the goals of accelerating eradication of M. tuberculosis infection and preventing relapse. However, the initial positive findings of safety and efficacy for IFNγ in a 1997 pilot study28 failed to be confirmed by larger, more definitive trials (summarized in ref.29). The most rigorous trial of IFNγ therapy in TB compared the use of aerosolized IFNγ to placebo in 80 patients with multidrug-resistant TB, all of whom also received therapy with second-line drugs. The study was halted in 2003 because of a trend towards increased mortality in the experimental arm, without evidence of clinical or microbiological benefit. The study findings were never published but appear in an online supplement to an inconclusive subsequent trial30. It has since been reported that most IFNγ-induced genes are already maximally upregulated in the lung in TB and that aerosolized IFNγ therefore has little additional effect31.
Thus, two historical lessons are apparent regarding immunotherapy of viral or mycobacterial infections. In patients with chronic infections who do not have distinct defects in cytokine production or signalling, therapy with interferons or IL-2 risks causing immunopathology with mixed microbiological benefit. By contrast, at least in preclinical models, a potential benefit was demonstrated for cytokine treatment of early infection. The pleiotropic effects of these potent immunostimulators and insufficient knowledge of how to limit their effects in terms of timing, space and target cells are likely to explain the mixed success of these approaches in the clinic. Future developments should factor in the multitude and dynamic nature of cytokine effects and find more precise ways to target these.
Strategies to ameliorate immunopathology
Immune activation aimed at pathogen elimination can cause significant collateral tissue damage in acute infection. For example, in both HCV and HBV infection, the immune response can lead to liver cirrhosis, hepatic failure and malignancy. In pulmonary TB, IFNγ production contributes to lung necrosis, cavitation, fibrosis and bronchiectasis32–34, and studies in experimental models show that high-level induction of type I interferon-inducible genes can lead to myeloid cell-mediated tissue necrosis and release of neutrophil extracellular traps (NETs) in TB35–41. In humans, these permanent effects impair lung function and reduce long-term survival despite microbiological cure42,43.
Historically, corticosteroids have been the most successful therapeutics for the treatment of infection-related immunopathology. Corticosteroids have dose-dependent anti-inflammatory and immunosuppressive effects on nearly all immune cells, reducing the production of pro-inflammatory cytokines and inhibiting cellular microbicidal responses44. Although corticosteroids can increase the risk of acquiring many bacterial, fungal and viral infections, including TB44, multiple randomized controlled trials of the use of adjunctive corticosteroids together with drug therapies against M. tuberculosis were started in the 1950s45,46 (Fig. 1). A systematic review in 1997 and a formal meta-analysis in 2013 concluded that corticosteroids conferred a survival advantage in patients with central nervous system and pericardial TB, and that they hastened the resolution of pulmonary abnormalities but did not affect end-of-treatment outcomes47,48. More recent studies indicate that corticosteroids are also effective in treating or preventing immune reconstitution inflammatory syndrome in patients with both HIV/AIDS and TB49,50, which most often manifests as a clinical worsening shortly after patients start combined TB therapy and ART. Based on a meta-regression analysis of 12 trials carried out in 2014 (ref.51), high-dose adjunctive corticosteroids also seem to accelerate the conversion of sputum culture from positive to negative in patients with TB. This apparent indirect antimicrobial effect of high-dose corticosteroids has been attributed to impaired integrity of granulomas, with resulting improved lesional penetration of anti-TB drugs. This process also likely allows a return of aerobic metabolism and replication to previously semi-dormant bacilli owing to the return of oxygen and nutrients to central regions of the granuloma, which increases their susceptibility to anti-TB drugs. In addition, multiple randomized controlled trials carried out in the 1990s found that early adjunctive treatment with corticosteroids substantially improves oxygenation and survival in patients with pneumonia caused by the fungus Pneumocystis jirovecii, particularly in patients with HIV/AIDS who are not yet on ART, in other words, those with the most profound immune dysregulation52–54.
Severe influenza is also characterized by cytokine excess55 but, in contrast to TB, retrospective studies of the use of corticosteroids in severe influenza have shown no benefit56; indeed, two meta-analyses of mainly retrospective series found that they increased mortality risk57,58. As severe influenza is often accompanied by secondary bacterial infections, it is possible that the deleterious effects of corticosteroids on mucosal defences account for their increased mortality risk15. Agents with greater specificity that are currently under investigation to control the hyperinflammatory response in severe influenza include non-steroidal anti-inflammatory drugs, statins, macrolides (antibiotics with additional anti-inflammatory effects), antibodies to complement factor C5a and N-acetylcysteine (a non-prescription medicine used to prevent death owing to hepatic necrosis after paracetamol acetaminophen poisoning) (reviewed in ref.56).
In summary, historical studies have shown a potentially important role for corticosteroids in reducing infectious immunopathology although, in some circumstances, more specific anti-inflammatory adjunctive treatments are warranted. At the same time, the use of cytokines to augment immunity during chronic infection has been limited by their exacerbation of immunopathology; immune induction seemed to be most promising during early viral infection although its use was limited by practical measures of prompt detection and intervention. How can the lessons learnt from these historical investigations be applied to current approaches? We discuss these questions in the context of COVID-19 and TB, currently two of the most deadly viral and bacterial diseases, respectively.
Current approaches to COVID-19
The extraordinary global impact of COVID-19 has placed it at the focus of extensive original research and critical review59,60 and provides an opportunity to examine current thinking regarding the immunotherapeutic approaches that have evolved across a wide spectrum of infectious and non-infectious diseases. The current view of SARS-CoV-2 pathogenesis in humans is that it can be divided into two phases: an early phase characterized by high-level viral replication and reduced or absent immune responsiveness, and a second phase in which this balance is reversed. Both phases can be targeted by immunotherapeutic strategies — to augment immunity in the first phase or reduce immunopathology in the second (Fig. 2). Two major lessons from the historic experiences outlined above were rapidly translated into treatment design: first, that the therapeutic window for antiviral immune intervention may be small and early; and second, that cytokines can be harmful as well as beneficial and, therefore, that cytokine responses might need to be inhibited in order to reduce immunopathology.
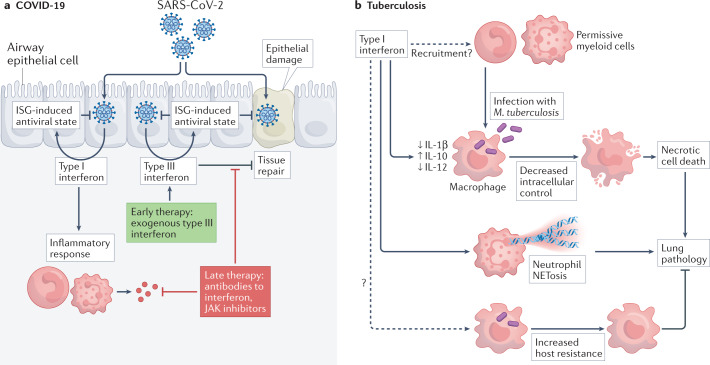
Fig. 2. Host-directed immunotherapeutic intervention points for severe COVID-19.
If the initial interferon and inflammatory responses are insufficient to control SARS-CoV-2 infection, the inflammatory cascade may persist and become hyperactivated. This can lead to monocyte and neutrophil infiltration into the lung, high local and systemic levels of cytokines, tissue damage in the lung, formation of neutrophil extracellular traps (NETosis), complement hyperactivation, coagulation, and the formation of microthrombi. Immunotherapeutic interventions aim to improve virus control early in infection (indicated in green) or to limit immune-mediated tissue damage owing to uncontrolled inflammation (indicated in red). JAK, Janus kinase.
Interferon-based strategies to augment immunity
Building on the historical knowledge of the antiviral effect of interferons in HCV and influenza, and based on retrospective studies showing that type I interferon is essential for protection against SARS-CoV-2 (refs61,62), the therapeutic use of type I interferon in early SARS-CoV-2 infection was rapidly proposed in the early stages of the ongoing pandemic63 although other studies showed that interferon levels strongly correlate with COVID-19 disease severity64–67. Thus, the timing of the interferon response seems to be a crucial factor63 as has been shown for influenza and, more recently, in preclinical studies of severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and COVID-19 (refs59,63). A retrospective multicohort study published early in the pandemic suggested that the likelihood of survival was increased by early IFNα treatment (within 5 days of hospitalization), whereas it was reduced if interferon therapy was started later68, findings that are reminiscent of earlier data obtained from patients with MERS69. Several prospective studies of hospitalized patients with COVID-19 followed, showing that the effects of interferon therapy relate to the timing of intervention and severity of illness. In the WHO Solidarity trial, in which hospitalized patients at different stages of disease were randomly assigned to receive subcutaneous IFNβ1a or other repurposed drugs, IFNβ1a tended to slightly increase mortality risk in patients requiring supplemental oxygen therapy compared with controls, suggesting that these patients were too advanced in the course of disease to benefit from interferon treatment70. However, a small randomized controlled trial in a similar population of hospitalized patients with COVID-19 found that treatment with aerosolized IFNβ1a led to more rapid recovery compared with placebo71. In another randomized controlled trial of 127 hospitalized patients, only 13% of whom required supplemental oxygen, the addition of INFβ1b plus ribavirin to lopinavir–ritonavir ART yielded a shorter time to resolution of symptoms72. Lastly, in a trial of 60 outpatients with COVID-19, none of whom required supplemental oxygen, a single dose of PEG-IFNλ increased the likelihood of having undetectable virus by day 7 of infection73. Together with results from hamster and mouse infection models59,63, these studies suggested greater clinical and virological benefit when interferon treatment is started early in the course of SARS-CoV-2 infection.
The assumption is that, in early treatment, the antiviral effects of interferons contribute to protection, whereas later in infection, interferon treatment may enhance immunopathology14,74 (Fig. 3). The cellular specificity of interferon receptors may also be a significant factor. The receptor for type I interferon is ubiquitous, allowing for effects on immune cells to drive inflammation and immunopathology, particularly late in infection75. By contrast, the receptor for type III interferon is mainly expressed on epithelial cells; IFNλ therefore lacks some of the immunopathogenic potential of type I interferons and has been proposed as the interferon treatment of choice76,77. Although it is generally less pro-inflammatory, IFNλ impaired epithelial repair when administered late in respiratory infection, which suggests that its use should also be restricted to early intervention in COVID-19 (refs16,17). Further trials using subtypes of the IFNα, IFNβ or IFNλ families are under way to bring more clarity to this complex issue75.
Fig. 3. Interferons and immunotherapeutic intervention: COVID-19 and tuberculosis.
Interferons are thought to have both protective and detrimental effects in COVID-19 and in tuberculosis. a | COVID-19. Lung epithelial cells produce type I interferon and type III interferon upon infection with SARS-CoV-2. Both types of interferon contribute to the establishment of an antiviral state in infected and adjacent cells through the induction of interferon-stimulated genes (ISGs). Immunotherapeutic intervention early after infection includes treatment with interferons, in particular with type III interferon, to reduce virus replication. Later in infection, type I interferon drives sustained inflammation, and type III interferon may contribute to impaired tissue repair. Therefore, late treatment with interferons should be avoided. Instead, monoclonal antibody-mediated interferon blockade may be considered, and treatment with Janus kinase (JAK) inhibitors may exert its beneficial effect partly through blocking the deleterious effects of interferons. b | In tuberculosis, type I interferon can promote disease by recruiting infection-permissive myeloid cells, by inhibiting intracellular control of bacterial growth in macrophages and by promoting immunopathology through necrosis of infected macrophages as well as neutrophils through the release of neutrophil extracellular traps (NETosis). By contrast, there is also evidence that type I interferon, under certain conditions, can enhance host resistance to Mycobacterium tuberculosis. The basis of these divergent effects of type I interferon on M. tuberculosis is poorly understood. As yet, there have been no published clinical trials that directly target this pathway in tuberculosis.
Strategies to ameliorate immunopathology
Corticosteroid treatment leads to clear improvement in seriously ill patients with COVID-19 (ref.78) (Fig. 1). In one trial, corticosteroids reduced the risk of death from 41% to 29% in patients receiving invasive mechanical ventilation and from 26% to 23% in those receiving oxygen without mechanical ventilation79. No benefit was found for patients not receiving respiratory support at randomization. The basis for this distinct difference from influenza — in which corticosteroids were ineffective at preventing immunopathology and were harmful in patients with severe disease — is uncertain but may relate to the markedly lower frequency of secondary bacterial infections in COVID-19, which in turn may be linked to SARS-CoV-2 inducing high levels of IL-6, a cytokine that has strong pro-inflammatory but also potent antibacterial effects.
One of the defining features of severe COVID-19 is a high-level cytokine response that contributes to immunopathology, although the absolute cytokine levels are only a fraction of those in other potentially lethal syndromes unrelated to COVID-19 (ref.80). How to control the virus-induced hyperinflammatory response has remained an open question despite ongoing trials in severe influenza, and the issue is now receiving increased attention as a result of the COVID-19 pandemic. Several anti-cytokine approaches are currently being studied. In particular, IL-6 was targeted early in the pandemic based on the use of anti-IL-6 therapy in immune-mediated inflammatory diseases, such as rheumatoid arthritis81, and on the successful therapy experience in hyperinflammatory complications associated with CAR T cell therapy82 (Fig. 1). Two classes of anti-IL-6 reagents have been studied, targeting either the IL-6 receptor (tocilizumab and sarilumab) or IL-6 itself (siltuximab). Tocilizumab has had the most extensive evaluation in COVID-19. Although an early study (COVACTA) found no benefit83, two others (RECOVERY and REMAP-CAP) found that IL-6 receptor blockade improved the clinical outcomes of COVID-19, including progression to invasive mechanical ventilation and death84–86. The contrary findings of these studies may be due to the concomitant use of corticosteroids, which were given more often and earlier in RECOVERY and REMAP-CAP. It seems that the two treatments target complementary inflammatory pathways and that the benefit of IL-6 blockade becomes more evident when corticosteroids are co-administered87.
Therapies that block signalling by granulocyte–macrophage colony stimulating factor (GM-CSF), IL-1 or other cytokines are also being tested for COVID-19. Early reports of treatment with the IL-1 receptor antagonist anakinra and with antibodies to GM-CSF indicate improved outcomes88–90 but larger-scale trials are necessary to demonstrate this conclusively. As all of these cytokines are potent immunomodulators with pleiotropic functions, understanding their effects in severe COVID-19 and learning from this which patient groups may benefit the most from cytokine-directed therapies are of crucial importance. For example, GM-CSF has been shown to improve the outcome of influenza infection in animal models by improving alveolar epithelial repair91,92 and, therefore, clinical trials have been carried out either adding or blocking GM-CSF93.
Cytokine-mediated signalling can alternatively be blocked further downstream by pharmacological inhibition. Inhibitors of the Janus kinases (JAKs) that signal downstream of many cytokine receptors were originally developed for use in patients with chronic inflammatory conditions such as rheumatoid arthritis and inflammatory bowel diseases94 (Fig. 1). As orally bioavailable small molecules, they presented an attractive alternative to large molecule therapeutics requiring injection such as anti-tumour necrosis factor (TNF) agents. The combination of baricitinib (a JAK inhibitor) plus remdesivir (a direct antiviral) has been shown to shorten recovery time and reduce mortality in patients with COVID-19 compared with remdesivir alone95. A similar trial of the JAK inhibitor tofacitinib in patients with COVID-19 found improved survival despite a relatively small sample size96. How much of this effect is due to the blockade of multiple cytokine signalling pathways or to apparent direct antiviral activity is not yet clear97. For practical reasons, these oral therapies are more likely to be suitable for widespread use than intravenous application of monoclonal antibodies and should therefore continue to be investigated as a priority. Similarly, two small studies of the serotonin reuptake inhibitor fluvoxamine found that it prevented clinical deterioration in patients with early COVID-19 (refs98,99). Fluvoxamine dampens pro-inflammatory cytokine production100, but the relationship of this effect to the clinical findings in COVID-19 is uncertain.
Novel strategies for immunotherapy
Excessive coagulation and thrombosis are found together with hyperinflammation in severe COVID-19 (ref.101). Endothelial dysfunction and damage, coagulopathy, and excessive complement activation combine with inflammation to cause thrombotic complications that likely contribute to the acute respiratory distress syndrome. Although the above-mentioned anti-inflammatory interventions can contribute to alleviating this pathogenic process, additional therapies, including antithrombotic drugs, such as heparin, garadacimab, nafamostat mesylate and tissue-type plasminogen activator, and inhibitors of the complement cascade, such as the C5 inhibitors eculizumab and ravulizumab and the inhibitor of C3 cleavage AMY-101, may synergize with anti-inflammatory treatment.
Another unmet therapeutic need — with some analogies to post-TB lung disease, as discussed below — is for ‘Long COVID’, which is characterized by persistent fatigue, anhedonia, muscle weakness, concentration deficits, anxiety or even depression, myalgia and arthralgia102. As the underlying mechanisms of Long COVID are unclear, no immunotherapeutic strategies have been developed so far, but persistent inflammation and the prothrombotic state often found in these patients will likely require anti-inflammatory and antithrombotic therapy similar to that described above for acute COVID-19 (ref.103). Neutrophil activation and release of NETs (NETosis) have also been observed in patients with COVID-19 (ref.104), and several clinical trials are under way (among others, ClinicalTrials.gov: NCT04402944, NCT04355364, NCT04432987, NCT04359654, NCT04445285 and NCT04402970) to confirm initial observations of the beneficial effects of dissolving NETs by treatment with DNAse105.
In summary, greater success has been achieved so far in ameliorating the immunopathology of severe COVID-19 using cytokine and signalling pathway inhibitors than in boosting immunity as the latter must occur early during infection, when the pathogen burden is low, to be successful. The same themes are evident in studies of TB as described below.
Current approaches to TB
As is the case for COVID-19, it is convenient to categorize host-directed immunotherapies for TB on the basis of their original intended use: either to ameliorate immunopathology or to augment immune control of the bacteria, although therapeutic interventions affecting one of these processes may have unanticipated effects on the other (Fig. 4). With few exceptions, the agents that have entered testing so far are re-purposed drugs that were originally approved for other wide-ranging indications, most of which are unrelated to the treatment of infectious disease106. This strategy reflects the economic reality that TB case numbers in North America and Europe are insufficient to support the costs of development and licensing of new drugs for TB. In most clinical trials, these host-directed therapies are administered adjunctly with standard antibiotics targeting M. tuberculosis, either for rifampin-susceptible or rifampin-resistant infection. In some cases, alternative antibiotics, such as rifabutin, have been used to avoid deleterious pharmacokinetic interactions between drugs.
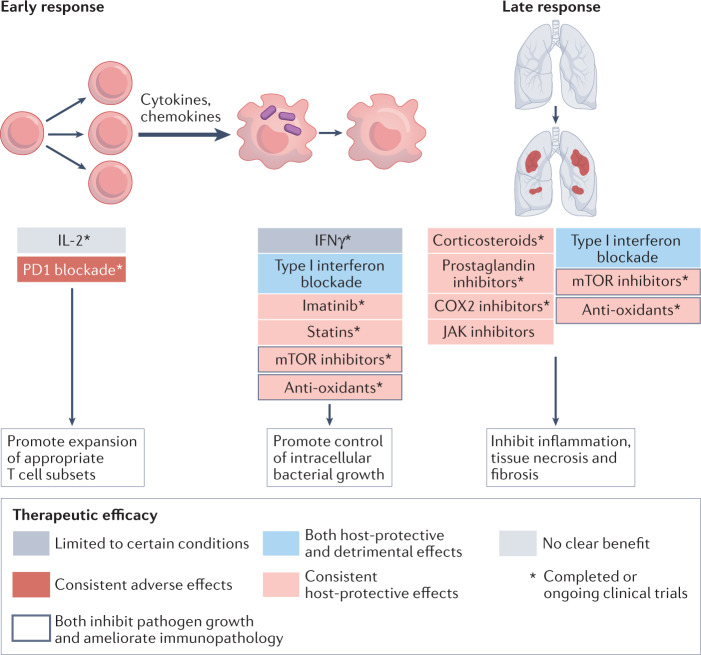
Fig. 4. Major candidates for host-directed immunotherapies and their targets in tuberculosis.
Host-directed immunotherapies for Mycobacterium tuberculosis infection can act early in the response to augment immunity or later in the response to reduce immunopathology. Although the control of M. tuberculosis infection clearly depends on both interferon-γ (IFNγ) production and T cell responses, immunotherapies targeting these elements — through IFNγ administration or PD1 blockade — have shown only limited promise in certain conditions or have proven detrimental, respectively. Administration of IL-2 to enhance T cell responses showed no clear benefit in clinical trials. Type I interferon blockade, despite having potent preclinical effects in ameliorating immunopathology, has unexplained effects on increasing the mycobacterial load in certain models. Also of note is that some interventions (such as mechanistic target of rapamycin (mTOR) inhibitors and anti-oxidants) have host-protective effects by both inhibiting pathogen growth and ameliorating immunopathology despite their original intended target being to augment immunity. Nearly all clinical trials of candidates for host-directed immunotherapy of tuberculosis are carried out adjunctively with antibiotics. COX2, cyclooxygenase 2; JAK, Janus kinase.
Strategies to modulate the effects of interferons
The role of interferon signalling in M. tuberculosis infection and disease is complex. As in COVID-19, interferon is a key element in the early protective antimycobacterial response but, in the case of TB, type II interferon (IFNγ) rather than type I or type III interferons seems to have a dominant role. Unlike in COVID-19, immune success in TB is most often non-sterilizing, resulting in containment of a latent infection rather than eradication of M. tuberculosis, and active tuberculosis most often results from progression of latent infection. In such cases, interferon signalling is detrimental, promoting the formation of lung cavities in which bacilli replicate to high numbers, thereby facilitating aerosol transmission. Indeed, the lack of genetic diversity in major M. tuberculosis antigens has been interpreted as evidence of an evolutionary strategy to provoke a host immune response107,108. Patients with TB and advanced AIDS, in whom interferon responses are reduced or absent, often lack radiographic evidence of lung disease, have reduced numbers of bacilli in sputum and are less likely to transmit M. tuberculosis infection109.
Additional data from patients and experimental infection models also show that type I interferon signalling has a major role in TB pathogenesis and exacerbation35–41,110–125. For example, antibody to type I interferon receptor (IFNAR1) blocks disease progression in infected TB-susceptible mice, even when applied 7 days after infection118. However, in genetically resistant mice infected with a lab strain of M. tuberculosis, an absence of IFNαβ signalling resulted in either an increased or unchanged bacterial load38,121,126,127, which highlights the complexities of interferon responses in different host genetic backgrounds38 and, possibly, the pleiotropic effects of interferons in the immune system. Human data support this complexity, also documenting situations in which type I interferon seems to be protective rather than disease promoting. For example, several clinical case reports have described improved clinical symptoms and decreased bacterial burden after co-administration of IFNα together with antimycobacterial chemotherapy. It is imperative to better understand the circumstances in which type I interferons induce exacerbation of TB rather than protection from disease and the mechanisms underlying these effects. Several mechanisms have been proposed for the pathogenic effects, including pulmonary recruitment of a pathogen-permissive monocyte and/or macrophage population based on findings in a model of TB exacerbated by intranasal treatment with poly(I:C)41, induction of the immunoregulatory cytokine IL-10, and suppression of IL-12 (refs38,128) (a major inducer of IFNγ synthesis) and/or IL-1 production by myeloid subsets37,118 (Fig. 3). IL-1 was reported to promote host resistance and mycobacterial control through the induction of eicosanoids that limit excessive type I interferon production (discussed later)37. Type I interferon signalling was also shown to trigger immunopathology in TB-susceptible mice by modulating lung phagocyte dynamics, with increased migration of inflammatory monocytes and neutrophils to the lung, and increased death of alveolar macrophages36. In TB-susceptible mice, type I interferon induces neutrophil-mediated lung inflammation and NETosis and promotes both bacterial growth and disease severity39, and blockade of IFNAR1 signalling or depletion of neutrophils in these mice abrogated lung pathology36,39. More recently, a role for autocrine or paracrine signalling by macrophage-derived type I interferon in the death of M. tuberculosis-infected macrophages in vitro has also been shown125.
Further knowledge of the pathways of type I interferon-driven lung pathology and disease in vivo may lead to the discovery of small-molecule inhibitors amenable for the development of affordable host-directed therapies125. In this regard, the JAK inhibitor tofacitinib has been studied in mouse models of TB. During early or latent M. tuberculosis infection, tofacitinib reduces host containment of infection and promotes bacterial replication in the lungs129. During late or active infection, tofacitinib reduces the production of pro-inflammatory mediators and enhances the effects of antimycobacterial chemotherapy130. These observations of a two-phase response, in which interferons might switch from augmenting immunity to mediating immunopathology, are very similar to those in SARS-CoV-2 infection.
Novel strategies to ameliorate immunopathology
Oxidative stress is a major sequela of M. tuberculosis infection that contributes to necrotic tissue damage as well as bacterial spread, in part through lipid peroxidation-induced damage to host cell membranes. As such, it is a logical target for host-directed therapy to ameliorate immunopathology. N-acetylcysteine, which functions by restoring cellular levels of the reduced form of glutathione, a major anti-oxidant that protects cells from oxidative damage, has been shown to reduce lung pathology and M. tuberculosis bacterial burden in several animal model studies and to inhibit tolerance to the antibiotic isoniazid in vitro131. It is currently being tested in three clinical trials for its effects in patients with TB (Table 1). In separate work, ferrostatin, a radical-trapping anti-oxidant that inhibits lipid peroxidation-induced membrane damage and cell death, has been shown to reduce pulmonary necrosis and bacterial burden in mice infected with M. tuberculosis132.
Table 1.
Ongoing clinical trials of host-directed immunotherapies for tuberculosis
| Immunotherapy | Mechanism | Trial acronym | Patient population | Main end points | Clinical trial number |
|---|---|---|---|---|---|
| CC-11050 | Phosphodiesterase inhibitor; inhibits cytokine production | DRTB-HDT | Rifampin-resistant TB | Sputum culture conversion and lung function | Horizon 2020: project 847465 |
| N-acetylcysteine (NAC) | Restores reduced form of glutathione; anti-oxidant | NAC-TB sub-study of TB-SEQUEL | Rifampin-susceptible TB | Sputum culture conversion and lung function | ClinicalTrials.gov: NCT03702738 |
| PanTB-HM | Rifampin-susceptible TB | Durable cure, drug-induced liver injury, lung function | EDCTP: RIA2019AMR-2647 | ||
| NAC TRIAL | Rifampin-resistant TB | Adverse drug reactions | PACTR: 202007736854169 | ||
| Metformin | AMPK activator; inhibits mTOR | METHOD | HIV-1-infected plus rifampin-susceptible TB | Sputum culture conversion and lung function | ClinicalTrials.gov: NCT04930744 |
| DRTB-HDT | Rifampin-resistant TB | Sputum culture conversion and lung function | Horizon 2020: project 847465 | ||
| Statins | Lipid-lowering and anti-inflammatory | STAT-TB | Rifampin-susceptible TB | Safety and pharmacokinetics | ClinicalTrials.gov: NCT03882177 |
| ATOR-TUB | Rifampin-susceptible TB | Sputum culture conversion | ClinicalTrials.gov: NCT04721795 | ||
| Statin-TB | Post-TB treatment | PET-CT glycolytic activity | ClinicalTrials.gov: NCT04147286 | ||
| Imatinib | Tyrosine kinase inhibitor | IMPACT-TB | Healthy volunteers | Pharmacokinetics, myeloid cell numbers, whole blood mycobactericidal activity | ClinicalTrials.gov: NCT03891901 |
| Cyclooxygenase inhibitors | Inhibit prostaglandin synthesis | SMA-TB | Adult TB | Composite symptom score | ClinicalTrials.gov: NCT04575519 |
Eicosanoids, which are lipid mediators derived from the catabolism of arachidonic acid, have been shown in vivo and in vitro to have an important role in regulating M. tuberculosis infection; products of the cyclooxygenase pathway (for example, prostaglandins) limit acute infection and disease, whereas products of the lipoxygenase pathway (for example, lipoxins) promote infection and disease. The pathogenic effects of type I interferon on M. tuberculosis infection seem to be caused, in part, by modulation of these pathways, and experimental administration of either prostaglandin E2 or a clinically approved 5-lipoxygenase inhibitor protected mice against the disease-promoting effects of type I interferon37. Other studies, by contrast, have noted that prostaglandins have disease-promoting effects in late infection, which suggests that cyclooxygenase 2 inhibitors, such as aspirin, might be effective in TB therapy. Trials testing the effects of aspirin on tuberculous meningitis in adults have yielded encouraging results but the benefit in terms of preventing strokes may be due to anti-platelet effects19,133,134. One trial of aspirin in children with tuberculous meningitis showed no benefit135. Additional clinical studies using newer-generation, more-selective cyclooxygenase 2 inhibitors for both drug-sensitive and drug-resistant M. tuberculosis strains are in progress (Table 1).
Another class of anti-inflammatory drugs currently undergoing clinical trials in patients with TB are the statins (Table 1). These HMG-CoA reductase inhibitors, which are widely used to reduce the risk of cardiovascular disease, function by lowering lipid levels but also have immunomodulatory activity. In the mouse model of TB, statins accelerate the clearance of mycobacteria and facilitate shortening of treatment136,137. Interestingly, statins can also promote bacterial control by reducing macrophage lipids that promote the growth of M. tuberculosis and by enhancing phagosome–lysosome fusion.
Even after mycobacterial cure, most patients with TB are left with bronchiectasis and fibrosis, permanent conditions that impair lung function and have profound long-term health consequences associated with excess mortality risk43,138–142. Addressing these long-term effects has become a major focus for studies of adjunctive host-directed therapies for TB. Phosphodiesterase inhibitors can inhibit pro-inflammatory cytokine production by preventing the degradation of cAMP. Several such inhibitors have shown promise in animal models of TB. Perhaps the best studied is CC-11050, which, when used adjunctively with the antibiotic isoniazid in mice and rabbits, ameliorated pulmonary pathology and decreased M. tuberculosis bacterial load in the lung to a greater extent than isoniazid alone143,144. In patients given CC-11050 as an adjunct for the first 112 days of rifabutin-substituted standard TB treatment, the results suggested that CC-11050 may interrupt mechanisms responsible for the irreversible loss of lung function145. A trial of CC-11050 in patients with rifampin-resistant TB is currently under way145 (Table 1).
Strategies to augment immunity
The induction of phagosome acidification and autophagy in M. tuberculosis-infected macrophages are important effector mechanisms of host resistance to infection and, accordingly, have become major targets of host-directed immunotherapeutic approaches for this pathogen. Unlike strategies to augment immunity in COVID-19, none of the agents for TB is a cytokine-based therapy. Tyrosine kinase inhibitors are one class of drugs that promote the macrophage phagocytic response. For example, in preclinical studies in M. tuberculosis-infected macrophages and mice, low doses of the tyrosine kinase inhibitor imatinib (an anticancer agent) were shown to reduce mycobacterial viability by promoting phagosome–lysosome fusion as well as increasing myelopoiesis146,147. This approach is currently being assessed in a phase I clinical trial (Table 1). Inhibitors of mechanistic target of rapamycin (mTOR) are a second group of agents thought to promote macrophage-mediated control of M. tuberculosis, in this case through the induction of autophagy111. In addition, mTOR inhibitors have been described to have anti-inflammatory and anti-fibrotic effects that could have a role in reducing immunopathology148,149. In a recent trial, the mTOR inhibitor everolimus had similar effects to CC-11050 on the recovery of lung function in patients with TB106. The AMPK activator metformin, which also inhibits mTOR, has been shown to promote macrophage control of M. tuberculosis, an effect associated with the induction of autophagy and reactive oxygen species, and to reduce pulmonary immune pathology, accelerate the resolution of lung fibrosis and enhance the efficacy of conventional antimicrobials in M. tuberculosis-infected mice150. Multiple studies in patients with diabetes found that metformin reduced the risk of TB compared with other diabetes treatments151–153 and improved outcomes in persons with diabetes and TB150,154,155. These findings do not seem to be due to superior glucose control. One recently reported phase II trial of metformin in TB found enhanced resolution of lung cavities but no effect on sputum culture conversion156. Other trials of metformin in patients with TB and without diabetes are presently under way (Table 1).
Given the markedly increased risk of TB caused by loss of CD4+ T cells157, enhancing T cell function would seem to be an obvious approach for host-directed therapy of TB. However, several studies involving PD1 blockade or deficiency in mice and rhesus monkeys and in a 3D in vitro granuloma model concur that checkpoint inhibition through PD1 markedly increases rather than decreases TB susceptibility30–32. These findings are consistent with a growing number of case reports of TB reactivation in patients with cancer who are treated with checkpoint inhibitors158–160. In experimental models, the exacerbation of TB resulting from PD1 blockade was associated with increased granulomatous inflammation as well as increased production of TNF and IFNγ and increased caspase 1 activity. Similarly, absence of cyclophilin in T cells, which directly increases T cell activity independently of checkpoint receptors, did not reduce bacterial burden but increased mortality in mouse models of TB161. Together, these observations highlight the potential negative consequences of interventions designed to augment T cell function in TB. Nonetheless, they should not discourage the investigation of other checkpoint-inhibition strategies that might have a therapeutic rather than a disease-promoting outcome.
The future of infection immunotherapy
Several themes have emerged from past and recent studies of infection immunotherapy. First, across a wide range of infecting organisms, there has been greater success in reducing immunopathology than in boosting immunity. This, in part, is a reflection of the importance of the timing of intervention as the ‘early’ phase of an acute infection, where enhancing anti-pathogen responses holds promise, may be over by the time of symptom onset. There may, however, be unexplored opportunities for early cytokine therapy of latent TB infection, for example, in household contacts of TB index cases. The potential advantage of using immunotherapy to augment immunity in this setting is that knowledge of microbial drug susceptibility would not be required; in addition, the low pathogen burden may decrease the risk of inducing immunopathology.
Factors other than cytokines have become recognized as important in modulating the host response. It has also become apparent that there is sizeable individual-to-individual variation in the response to pathogens such as M. tuberculosis and SARS-CoV-2. Therefore, the success of any host-directed therapy may depend heavily on both knowledge of disease as well as baseline parameters for each patient receiving treatment. Endotypes, which are defined as distinct molecular profiles based on metabolism, epigenetics, transcription or immune function, have been proposed to guide the application of personalized immunotherapies162. However, specific endotypes remain to be defined for most infections, even for those with ostensibly similar clinical phenotypes163. A particular challenge exists for diseases of global public health impact such as TB and now COVID-19, for which individualized therapies are considered impractical. Nevertheless, it will be particularly important to identify clinical correlates of specific endotypes (for example, far-advanced cavitary TB164 or cases with post-TB severe loss of lung function) to assist in the selection of appropriate immunotherapies for specific patients. The role of specific endotypes in acute viral infections, including with SARS-CoV-2, is also poorly understood. The wide diversity of outcomes has long been known for influenza165 but is now particularly apparent for SARS-CoV-2 infection as the virus spreads through an immunologically naive population.
Improved immunotherapies for COVID-19 will depend on a better understanding of the mechanisms of immunopathology and of the highly dynamic nature of the course of infection. Interventions with greater specificity may be possible, for example preserving the beneficial effects of IL-6 on epithelial repair166 and B cell responses while minimizing its pro-inflammatory signals167. As several members of the IL-6 family have similar effects on immune responses, inhibition of additional family members, such as oncostatin M, which has been implicated in driving excessive inflammation in COVID-19 (ref.168), or specific targeting of the receptor chain gp130 that is used by most IL-6 family members may be considered169. Similarly, the mixed effects of a broad-range JAK inhibitor, such as baricitinib, may be improved by more specific inhibition of TYK2, which blocks signals downstream of type I interferon but not of type III interferon. Such an approach would prevent the pro-inflammatory effects driven by type I interferon and other pro-inflammatory cytokines, while preserving mucosal antiviral effects downstream of type III interferon170.
New therapeutics to enhance immunity without worsening immunopathology are needed. Alternatively, host-directed therapies that correct underlying pathogenic mechanisms in infected cells, rather than targeting immune cells, may make it possible to both enhance immunity and lessen immunopathology with a single intervention, as is thought to occur with imatinib. In this regard, the burgeoning field of immunometabolism may reveal new insights and approaches to achieve this dual therapeutic aim.
Finally, a compelling cost–benefit analysis must be advanced if immunotherapies are to become part of a new standard of care as either adjunctive or stand-alone therapies. This is particularly true for biotherapeutics such as cytokines and antibodies, which are typically substantially more expensive to produce at large scale than antimicrobial drugs. The remarkable success of mRNA-mediated delivery of vaccine antigens may stimulate similar methods for immunotherapy such as the delivery of cytokine-encoding genes. In the case of TB, one may estimate that the added recovery of lung function afforded by treatment with CC-11050 could be quite favourable in terms of cost per disability-adjusted life year, but it nonetheless will require that public health programmes begin to include post-TB morbidity and mortality in estimates of national and global health burdens171. Similar cost–benefit and ‘quality of life’ analyses will be required for patients with Long COVID. Combining host-directed therapies for TB with new antimicrobial regimens and adjusting treatment duration based on a simple measure at diagnosis is a strategy that could add substantial value both to patients and health programmes and promote uptake of these new therapies.
Acknowledgements
The authors thank E. Wall and W. Blanchett for helpful suggestions on the manuscript. The contribution of R.S.W. was partially supported by Horizon 2020 grant 847465 for Research and Innovation (DRTB-HDT) and project RIA2019AMR-2647 (panTB-HM) of the EDCTP2 programme of the European Union. The contribution of A.W. was funded by The Francis Crick Institute, which receives its core funding from Cancer Research UK (FC001206), the UK Medical Research Council (FC001206) and the Wellcome Trust (FC001206). A.O’G. is funded by The Francis Crick Institute, which receives its core funding from Cancer Research UK (FC001126), the UK Medical Research Council (FC001126) and the Wellcome Trust (FC001126). A.S. is supported by the intramural research program of the National Institute of Allergy and Infectious Diseases, US National Institutes of Health.
Author contributions
The authors contributed equally to all aspects of the article.
Peer review
Peer review information
Nature Reviews Immunology thanks T. Decker, R. Mahon and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinicalTrials.gov: https://clinicaltrials.gov/
EDCTP: https://www.edctp.org/
PACTR: https://pactr.samrc.ac.za/
Contributor Information
Robert S. Wallis, Email: rwallis@auruminstitute.org
Andreas Wack, Email: andreas.wack@crick.ac.uk.
References
- 1.Ellis GI, Sheppard NC, Riley JL. Genetic engineering of T cells for immunotherapy. Nat. Rev. Genet. 2021;22:427–447. doi: 10.1038/s41576-021-00329-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wykes MN, Lewin SR. Immune checkpoint blockade in infectious diseases. Nat. Rev. Immunol. 2018;18:91–104. doi: 10.1038/nri.2017.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boland EW, Headley NE. Effects of cortisone acetate on rheumatoid arthritis. J. Am. Med. Assoc. 1949;141:301–308. doi: 10.1001/jama.1949.02910050001001. [DOI] [PubMed] [Google Scholar]
- 4.Isaacs A, Lindenmann J. Virus interference. I. The interferon. Proc. R. Soc. Lond. B. Biol. Sci. 1957;147:258–267. doi: 10.1098/rspb.1957.0048. [DOI] [PubMed] [Google Scholar]
- 5.Reichard O, et al. Randomised, double-blind, placebo-controlled trial of interferon alpha-2b with and without ribavirin for chronic hepatitis C. The Swedish Study Group. Lancet. 1998;351:83–87. doi: 10.1016/S0140-6736(97)06088-1. [DOI] [PubMed] [Google Scholar]
- 6.Heim MH. 25 years of interferon-based treatment of chronic hepatitis C: an epoch coming to an end. Nat. Rev. Immunol. 2013;13:535–542. doi: 10.1038/nri3463. [DOI] [PubMed] [Google Scholar]
- 7.Neesgaard B, Ruhwald M, Weis N. Inducible protein-10 as a predictive marker of antiviral hepatitis C treatment: a systematic review. World J. Hepatol. 2017;9:677–688. doi: 10.4254/wjh.v9.i14.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muir AJ, et al. A randomized phase 2b study of peginterferon lambda-1a for the treatment of chronic HCV infection. J. Hepatol. 2014;61:1238–1246. doi: 10.1016/j.jhep.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 9.Lok AS, et al. Preliminary study of two antiviral agents for hepatitis C genotype 1. N. Engl. J. Med. 2012;366:216–224. doi: 10.1056/NEJMoa1104430. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann SHE, Dorhoi A, Hotchkiss RS, Bartenschlager R. Host-directed therapies for bacterial and viral infections. Nat. Rev. Drug Discov. 2018;17:35–56. doi: 10.1038/nrd.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrat FJ, Su L. A pathogenic role of plasmacytoid dendritic cells in autoimmunity and chronic viral infection. J. Exp. Med. 2019;216:1974–1985. doi: 10.1084/jem.20181359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Su L. Pathogenic role of type i interferons in HIV-induced immune impairments in humanized mice. Curr. HIV/AIDS Rep. 2019;16:224–229. doi: 10.1007/s11904-019-00444-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beilharz MW, Cummins JM, Bennett AL. Protection from lethal influenza virus challenge by oral type 1 interferon. Biochem. Biophys. Res. Commun. 2007;355:740–744. doi: 10.1016/j.bbrc.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 14.Davidson S, et al. IFNlambda is a potent anti-influenza therapeutic without the inflammatory side effects of IFNalpha treatment. EMBO Mol. Med. 2016;8:1099–1112. doi: 10.15252/emmm.201606413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson S, Maini MK, Wack A. Disease-promoting effects of type I interferons in viral, bacterial, and coinfections. J. Interferon Cytokine Res. 2015;35:252–264. doi: 10.1089/jir.2014.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Major J, et al. Type I and III interferons disrupt lung epithelial repair during recovery from viral infection. Science. 2020;369:712–717. doi: 10.1126/science.abc2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Broggi A, et al. Type III interferons disrupt the lung epithelial barrier upon viral recognition. Science. 2020;369:706–712. doi: 10.1126/science.abc3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Onwumeh J, Okwundu CI, Kredo T. Interleukin-2 as an adjunct to antiretroviral therapy for HIV-positive adults. Cochrane Database Syst. Rev. 2017;5:CD009818. doi: 10.1002/14651858.CD009818.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Young C, Walzl G, Du Plessis N. Therapeutic host-directed strategies to improve outcome in tuberculosis. Mucosal Immunol. 2020;13:190–204. doi: 10.1038/s41385-019-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson BJ, et al. rhuIL-2 adjunctive therapy in multidrug resistant tuberculosis: a comparison of two treatment regimens and placebo. Tuber. Lung Dis. 1997;78:195–203. doi: 10.1016/S0962-8479(97)90026-5. [DOI] [PubMed] [Google Scholar]
- 21.Johnson JL, et al. Randomized trial of adjunctive interleukin-2 in adults with pulmonary tuberculosis. Am. J. Respir. Crit. Care Med. 2003;168:185–191. doi: 10.1164/rccm.200211-1359OC. [DOI] [PubMed] [Google Scholar]
- 22.Larson RP, Shafiani S, Urdahl KB. Foxp3+ regulatory T cells in tuberculosis. Adv. Exp. Med. Biol. 2013;783:165–180. doi: 10.1007/978-1-4614-6111-1_9. [DOI] [PubMed] [Google Scholar]
- 23.Chen CY, et al. IL-2 simultaneously expands Foxp3+ T regulatory and T effector cells and confers resistance to severe tuberculosis (TB): implicative Treg-T effector cooperation in immunity to TB. J. Immunol. 2012;188:4278–4288. doi: 10.4049/jimmunol.1101291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper AM. Cell-mediated immune responses in tuberculosis. Annu. Rev. Immunol. 2009;27:393–422. doi: 10.1146/annurev.immunol.021908.132703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flynn JL, Chan J. Immunology of tuberculosis. Annu. Rev. Immunol. 2001;19:93–129. doi: 10.1146/annurev.immunol.19.1.93. [DOI] [PubMed] [Google Scholar]
- 26.Kristensen IA, Veirum JE, Moller BK, Christiansen M. Novel STAT1 alleles in a patient with impaired resistance to mycobacteria. J. Clin. Immunol. 2011;31:265–271. doi: 10.1007/s10875-010-9480-8. [DOI] [PubMed] [Google Scholar]
- 27.Alangari AA, et al. Treatment of disseminated mycobacterial infection with high-dose IFN-gamma in a patient with IL-12Rbeta1 deficiency. Clin. Dev. Immunol. 2011;2011:691956. doi: 10.1155/2011/691956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Condos R, Rom WN, Schluger NW. Treatment of multidrug-resistant pulmonary tuberculosis with interferon- gamma via aerosol. Lancet. 1997;349:1513–1515. doi: 10.1016/S0140-6736(96)12273-X. [DOI] [PubMed] [Google Scholar]
- 29.Wallis RS. Lack of a therapeutic role for interferon gamma in patients with tuberculosis. J. Infect. Dis. 2014;209:627–628. doi: 10.1093/infdis/jit555. [DOI] [PubMed] [Google Scholar]
- 30.Dawson R, et al. Immunomodulation with recombinant interferon-gamma1b in pulmonary tuberculosis. PLoS One. 2009;4:e6984. doi: 10.1371/journal.pone.0006984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raju B, et al. Aerosolized gamma interferon (IFN-gamma) induces expression of the genes encoding the IFN-gamma-inducible 10-kilodalton protein but not inducible nitric oxide synthase in the lung during tuberculosis. Infect. Immun. 2004;72:1275–1283. doi: 10.1128/IAI.72.3.1275-1283.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guirado E, Schlesinger LS, Kaplan G. Macrophages in tuberculosis: friend or foe. Semin. Immunopathol. 2013;35:563–583. doi: 10.1007/s00281-013-0388-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tan BH, et al. Macrophages acquire neutrophil granules for antimicrobial activity against intracellular pathogens. J. Immunol. 2006;177:1864–1871. doi: 10.4049/jimmunol.177.3.1864. [DOI] [PubMed] [Google Scholar]
- 34.Gopal R, et al. S100A8/A9 proteins mediate neutrophilic inflammation and lung pathology during tuberculosis. Am. J. Respir. Crit. Care Med. 2013;188:1137–1146. doi: 10.1164/rccm.201304-0803OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berry MP, et al. An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature. 2010;466:973–977. doi: 10.1038/nature09247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dorhoi A, et al. Type I IFN signaling triggers immunopathology in tuberculosis-susceptible mice by modulating lung phagocyte dynamics. Eur. J. Immunol. 2014;44:2380–2393. doi: 10.1002/eji.201344219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mayer-Barber KD, et al. Host-directed therapy of tuberculosis based on interleukin-1 and type I interferon crosstalk. Nature. 2014;511:99–103. doi: 10.1038/nature13489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moreira-Teixeira L, Mayer-Barber K, Sher A, O’Garra A. Type I interferons in tuberculosis: foe and occasionally friend. J. Exp. Med. 2018;215:1273–1285. doi: 10.1084/jem.20180325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moreira-Teixeira L, et al. Type I IFN exacerbates disease in tuberculosis-susceptible mice by inducing neutrophil-mediated lung inflammation and NETosis. Nat. Commun. 2020;11:5566. doi: 10.1038/s41467-020-19412-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moreira-Teixeira L, et al. Mouse transcriptome reveals potential signatures of protection and pathogenesis in human tuberculosis. Nat. Immunol. 2020;21:464–476. doi: 10.1038/s41590-020-0610-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Antonelli LR, et al. Intranasal Poly-IC treatment exacerbates tuberculosis in mice through the pulmonary recruitment of a pathogen-permissive monocyte/macrophage population. J. Clin. Invest. 2010;120:1674–1682. doi: 10.1172/JCI40817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Romanowski K, et al. Long-term all-cause mortality in people treated for tuberculosis: a systematic review and meta-analysis. Lancet Infect. Dis. 2019;19:1129–1137. doi: 10.1016/S1473-3099(19)30309-3. [DOI] [PubMed] [Google Scholar]
- 43.Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir. Med. 1989;83:195–198. doi: 10.1016/S0954-6111(89)80031-9. [DOI] [PubMed] [Google Scholar]
- 44.Youssef J, Novosad SA, Winthrop KL. Infection risk and safety of corticosteroid use. Rheum. Dis. Clin. North. Am. 2016;42:157–176. doi: 10.1016/j.rdc.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barnard C. Tuberculous meningitis; cortisone treatment as an adjunct to the antibiotics; the effect on the clinical features and the cerebrospinal fluid. S. Afr. Med. J. 1953;27:219–220. [PubMed] [Google Scholar]
- 46.Cochran JB. Cortisone in the treatment of pulmonary tuberculosis. Edinb. Med. J. 1954;61:238–249. [PMC free article] [PubMed] [Google Scholar]
- 47.Dooley DP, Carpenter JL, Rademacher S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin. Infect. Dis. 1997;25:872–887. doi: 10.1086/515543. [DOI] [PubMed] [Google Scholar]
- 48.Critchley JA, Young F, Orton L, Garner P. Corticosteroids for prevention of mortality in people with tuberculosis: a systematic review and meta-analysis. Lancet Infect. Dis. 2013;13:223–237. doi: 10.1016/S1473-3099(12)70321-3. [DOI] [PubMed] [Google Scholar]
- 49.Meintjes G, et al. Randomized placebo-controlled trial of prednisone for paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome. AIDS. 2010;24:2381–2390. doi: 10.1097/QAD.0b013e32833dfc68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meintjes G, et al. Prednisone for the prevention of paradoxical tuberculosis-associated IRIS. N. Engl. J. Med. 2018;379:1915–1925. doi: 10.1056/NEJMoa1800762. [DOI] [PubMed] [Google Scholar]
- 51.Wallis RS. Corticosteroid effects on sputum culture in pulmonary tuberculosis: a meta-regression analysis. Open Forum Infect. Dis. 2014;1:ofu020. doi: 10.1093/ofid/ofu020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The National Institutes of Health-University of California Expert Panel for Corticosteroids as Adjunctive Therapy for Pneumocystis Pneumonia. Consensus statement on the use of corticosteroids as adjunctive therapy for pneumocystis pneumonia in the acquired immunodeficiency syndrome. N. Engl. J. Med. 1990;323:1500–1504. doi: 10.1056/NEJM199011223232131. [DOI] [PubMed] [Google Scholar]
- 53.Fujikura Y, Manabe T, Kawana A, Kohno S. Adjunctive corticosteroids for Pneumocystis jirovecii pneumonia in non-HIV-infected patients: a systematic review and meta-analysis of observational studies. Arch. Bronconeumol. 2017;53:55–61. doi: 10.1016/j.arbres.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 54.Ewald H, et al. Adjunctive corticosteroids for Pneumocystis jiroveci pneumonia in patients with HIV infection. Cochrane Database Syst. Rev. 2015;2015:CD006150. doi: 10.1002/14651858.CD006150.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.de Jong MD, et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 2006;12:1203–1207. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hui DS, Lee N, Chan PK, Beigel JH. The role of adjuvant immunomodulatory agents for treatment of severe influenza. Antivir. Res. 2018;150:202–216. doi: 10.1016/j.antiviral.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhou Y, et al. Use of corticosteroids in influenza-associated acute respiratory distress syndrome and severe pneumonia: a systemic review and meta-analysis. Sci. Rep. 2020;10:3044. doi: 10.1038/s41598-020-59732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ni YN, Chen G, Sun J, Liang BM, Liang ZA. The effect of corticosteroids on mortality of patients with influenza pneumonia: a systematic review and meta-analysis. Crit. Care. 2019;23:99. doi: 10.1186/s13054-019-2395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wong LR, Perlman S. Immune dysregulation and immunopathology induced by SARS-CoV-2 and related coronaviruses - are we our own worst enemy? Nat. Rev. Immunol. 2022;22:47–56. doi: 10.1038/s41577-021-00656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Diamond MS, Kanneganti TD. Innate immunity: the first line of defense against SARS-CoV-2. Nat. Immunol. 2022;23:165–176. doi: 10.1038/s41590-021-01091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang Q, et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370:eabd4570. doi: 10.1126/science.abd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bastard P, et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020;370:eabd4585. doi: 10.1126/science.abd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Park A, Iwasaki A. Type I and type III interferons- induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020;27:870–878. doi: 10.1016/j.chom.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Laing AG, et al. A dynamic COVID-19 immune signature includes associations with poor prognosis. Nat. Med. 2020;26:1623–1635. doi: 10.1038/s41591-020-1038-6. [DOI] [PubMed] [Google Scholar]
- 65.Lucas C, et al. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. 2020;584:463–469. doi: 10.1038/s41586-020-2588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Galani IE, et al. Untuned antiviral immunity in COVID-19 revealed by temporal type I/III interferon patterns and flu comparison. Nat. Immunol. 2021;22:32–40. doi: 10.1038/s41590-020-00840-x. [DOI] [PubMed] [Google Scholar]
- 67.Zhou Z, et al. Heightened innate immune responses in the respiratory tract of COVID-19 patients. Cell Host Microbe. 2020;27:883–890.e2. doi: 10.1016/j.chom.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang N, et al. Retrospective multicenter cohort study shows early interferon therapy is associated with favorable clinical responses in COVID-19 patients. Cell Host Microbe. 2020;28:455–464.e2. doi: 10.1016/j.chom.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arabi YM, et al. Interferon beta-1b and Lopinavir-Ritonavir for middle east respiratory syndrome. N. Engl. J. Med. 2020;383:1645–1656. doi: 10.1056/NEJMoa2015294. [DOI] [PubMed] [Google Scholar]
- 70.WHO Solidarity Trial Consortium. et al. Repurposed antiviral drugs for Covid-19 - interim WHO solidarity trial results. N. Engl. J. Med. 2021;384:497–511. doi: 10.1056/NEJMoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Monk PD, et al. Safety and efficacy of inhaled nebulised interferon beta-1a (SNG001) for treatment of SARS-CoV-2 infection: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Respir. Med. 2021;9:196–206. doi: 10.1016/S2213-2600(20)30511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hung IF, et al. Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet. 2020;395:1695–1704. doi: 10.1016/S0140-6736(20)31042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Feld JJ, et al. Peginterferon lambda for the treatment of outpatients with COVID-19: a phase 2, placebo-controlled randomised trial. Lancet Respir. Med. 2021;9:498–510. doi: 10.1016/S2213-2600(20)30566-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Channappanavar R, et al. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Garcia-Del-Barco D, Risco-Acevedo D, Berlanga-Acosta J, Martos-Benitez FD, Guillen-Nieto G. Revisiting pleiotropic effects of type I interferons: rationale for its prophylactic and therapeutic use against SARS-CoV-2. Front. Immunol. 2021;12:655528. doi: 10.3389/fimmu.2021.655528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Prokunina-Olsson L, et al. COVID-19 and emerging viral infections: the case for interferon lambda. J. Exp. Med. 2020;217:e20200653. doi: 10.1084/jem.20200653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Davidson S, Crotta S, McCabe TM, Wack A. Pathogenic potential of interferon alphabeta in acute influenza infection. Nat. Commun. 2014;5:3864. doi: 10.1038/ncomms4864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Angus DC, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA. 2020;324:1317–1329. doi: 10.1001/jama.2020.17022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Recovery Collaborative Group. et al. Dexamethasone in hospitalized patients with Covid-19. N. Engl. J. Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Leisman DE, et al. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir. Med. 2020;8:1233–1244. doi: 10.1016/S2213-2600(20)30404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Smolen JS, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet. 2008;371:987–997. doi: 10.1016/S0140-6736(08)60453-5. [DOI] [PubMed] [Google Scholar]
- 82.Le RQ, et al. FDA approval summary: tocilizumab for treatment of chimeric antigen receptor T cell-induced severe or life-threatening cytokine release syndrome. Oncologist. 2018;23:943–947. doi: 10.1634/theoncologist.2018-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rosas IO, et al. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N. Engl. J. Med. 2021;384:1503–1516. doi: 10.1056/NEJMoa2028700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Recovery Collaborative Group. et al. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397:1637–1645. doi: 10.1016/S0140-6736(21)00676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Remap-Cap Investigators. et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N. Engl. J. Med. 2021;384:1491–1502. doi: 10.1056/NEJMoa2100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Stone JH, et al. Efficacy of tocilizumab in patients hospitalized with Covid-19. N. Engl. J. Med. 2020;383:2333–2344. doi: 10.1056/NEJMoa2028836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rubin EJ, Longo DL, Baden LR. Interleukin-6 receptor inhibition in Covid-19-cooling the inflammatory soup. N. Engl. J. Med. 2021;384:1564–1565. doi: 10.1056/NEJMe2103108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cremer PC, et al. Mavrilimumab in patients with severe COVID-19 pneumonia and systemic hyperinflammation (MASH-COVID): an investigator initiated, multicentre, double-blind, randomised, placebo-controlled trial. Lancet Rheumatol. 2021;3:e410–e418. doi: 10.1016/S2665-9913(21)00070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.De Luca G, et al. GM-CSF blockade with mavrilimumab in severe COVID-19 pneumonia and systemic hyperinflammation: a single-centre, prospective cohort study. Lancet Rheumatol. 2020;2:e465–e473. doi: 10.1016/S2665-9913(20)30170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cavalli G, et al. Interleukin-1 and interleukin-6 inhibition compared with standard management in patients with COVID-19 and hyperinflammation: a cohort study. Lancet Rheumatol. 2021;3:e253–e261. doi: 10.1016/S2665-9913(21)00012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cakarova L, et al. Macrophage tumor necrosis factor-alpha induces epithelial expression of granulocyte-macrophage colony-stimulating factor: impact on alveolar epithelial repair. Am. J. Respir. Crit. Care Med. 2009;180:521–532. doi: 10.1164/rccm.200812-1837OC. [DOI] [PubMed] [Google Scholar]
- 92.Rosler B, Herold S. Lung epithelial GM-CSF improves host defense function and epithelial repair in influenza virus pneumonia-a new therapeutic strategy? Mol. Cell. Pediatr. 2016;3:29. doi: 10.1186/s40348-016-0055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mehta P, Chambers RC, Dagna L. Granulocyte-macrophage colony stimulating factor in COVID-19: friend or foe? Lancet Rheumatol. 2021;3:e394–e395. doi: 10.1016/S2665-9913(21)00078-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kremer JM, et al. The safety and efficacy of a JAK inhibitor in patients with active rheumatoid arthritis: results of a double-blind, placebo-controlled phase IIa trial of three dosage levels of CP-690,550 versus placebo. Arthritis Rheum. 2009;60:1895–1905. doi: 10.1002/art.24567. [DOI] [PubMed] [Google Scholar]
- 95.Kalil AC, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N. Engl. J. Med. 2021;384:795–807. doi: 10.1056/NEJMoa2031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Guimaraes PO, et al. Tofacitinib in patients hospitalized with Covid-19 pneumonia. N. Engl. J. Med. 2021;385:406–415. doi: 10.1056/NEJMoa2101643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stebbing J, et al. JAK inhibition reduces SARS-CoV-2 liver infectivity and modulates inflammatory responses to reduce morbidity and mortality. Sci. Adv. 2021;7:eabe4724. doi: 10.1126/sciadv.abe4724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Seftel D, Boulware DR. Prospective cohort of fluvoxamine for early treatment of coronavirus disease 19. Open Forum Infect. Dis. 2021;8:ofab050. doi: 10.1093/ofid/ofab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lenze EJ, et al. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial. JAMA. 2020;324:2292–2300. doi: 10.1001/jama.2020.22760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rosen DA, et al. Modulation of the sigma-1 receptor–IRE1 pathway is beneficial in preclinical models of inflammation and sepsis. Sci. Transl. Med. 2019;11:eaau5266. doi: 10.1126/scitranslmed.aau5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bonaventura A, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat. Rev. Immunol. 2021;21:319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gusev E, Sarapultsev A, Solomatina L, Chereshnev V. SARS-CoV-2-Specific immune response and the pathogenesis of COVID-19. Int. J. Mol. Sci. 2022;23:1716. doi: 10.3390/ijms23031716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Acanfora D, et al. The cross-talk between thrombosis and inflammatory storm in acute and long-COVID-19: therapeutic targets and clinical cases. Viruses. 2021;13:1904. doi: 10.3390/v13101904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Middleton EA, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Weber AG, Chau AS, Egeblad M, Barnes BJ, Janowitz T. Nebulized in-line endotracheal dornase alfa and albuterol administered to mechanically ventilated COVID-19 patients: a case series. Mol. Med. 2020;26:91. doi: 10.1186/s10020-020-00215-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zumla A, et al. Towards host-directed therapies for tuberculosis. Nat. Rev. Drug Discov. 2015;14:511–512. doi: 10.1038/nrd4696. [DOI] [PubMed] [Google Scholar]
- 107.Musser JM, Amin A, Ramaswamy S. Negligible genetic diversity of mycobacterium tuberculosis host immune system protein targets: evidence of limited selective pressure. Genetics. 2000;155:7–16. doi: 10.1093/genetics/155.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ernst JD. Antigenic variation and immune escape in the MTBC. Adv. Exp. Med. Biol. 2017;1019:171–190. doi: 10.1007/978-3-319-64371-7_9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Drain PK, et al. Incipient and subclinical tuberculosis: a clinical review of early stages and progression of infection. Clin. Microbiol. Rev. 2018;31:e00021-18. doi: 10.1128/CMR.00021-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ottenhoff TH, et al. Genome-wide expression profiling identifies type 1 interferon response pathways in active tuberculosis. PLoS One. 2012;7:e45839. doi: 10.1371/journal.pone.0045839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Scriba TJ, et al. Sequential inflammatory processes define human progression from M. tuberculosis infection to tuberculosis disease. PLoS Pathog. 2017;13:e1006687. doi: 10.1371/journal.ppat.1006687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Singhania A, et al. A modular transcriptional signature identifies phenotypic heterogeneity of human tuberculosis infection. Nat. Commun. 2018;9:2308. doi: 10.1038/s41467-018-04579-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bloom CI, et al. Detectable changes in the blood transcriptome are present after two weeks of antituberculosis therapy. PLoS One. 2012;7:e46191. doi: 10.1371/journal.pone.0046191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cliff JM, et al. Distinct phases of blood gene expression pattern through tuberculosis treatment reflect modulation of the humoral immune response. J. Infect. Dis. 2013;207:18–29. doi: 10.1093/infdis/jis499. [DOI] [PubMed] [Google Scholar]
- 115.Zhang X, et al. Human intracellular ISG15 prevents interferon-alpha/beta over-amplification and auto-inflammation. Nature. 2015;517:89–93. doi: 10.1038/nature13801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gideon HP, Skinner JA, Baldwin N, Flynn JL, Lin PL. Early whole blood transcriptional signatures are associated with severity of lung inflammation in cynomolgus macaques with mycobacterium tuberculosis infection. J. Immunol. 2016;197:4817–4828. doi: 10.4049/jimmunol.1601138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bogunovic D, et al. Mycobacterial disease and impaired IFN-gamma immunity in humans with inherited ISG15 deficiency. Science. 2012;337:1684–1688. doi: 10.1126/science.1224026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ji DX, et al. Type I interferon-driven susceptibility to Mycobacterium tuberculosis is mediated by IL-1Ra. Nat. Microbiol. 2019;4:2128–2135. doi: 10.1038/s41564-019-0578-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Manca C, et al. Virulence of a Mycobacterium tuberculosis clinical isolate in mice is determined by failure to induce Th1 type immunity and is associated with induction of IFN-alpha /beta. Proc. Natl Acad. Sci. USA. 2001;98:5752–5757. doi: 10.1073/pnas.091096998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Manca C, et al. Hypervirulent M. tuberculosis W/Beijing strains upregulate type I IFNs and increase expression of negative regulators of the Jak-Stat pathway. J. Interferon Cytokine Res. 2005;25:694–701. doi: 10.1089/jir.2005.25.694. [DOI] [PubMed] [Google Scholar]
- 121.McNab FW, et al. TPL-2-ERK1/2 signaling promotes host resistance against intracellular bacterial infection by negative regulation of type I IFN production. J. Immunol. 2013;191:1732–1743. doi: 10.4049/jimmunol.1300146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ordway D, et al. The hypervirulent Mycobacterium tuberculosis strain HN878 induces a potent TH1 response followed by rapid down-regulation. J. Immunol. 2007;179:522–531. doi: 10.4049/jimmunol.179.1.522. [DOI] [PubMed] [Google Scholar]
- 123.Redford PS, et al. Influenza A virus impairs control of Mycobacterium tuberculosis coinfection through a type I interferon receptor-dependent pathway. J. Infect. Dis. 2014;209:270–274. doi: 10.1093/infdis/jit424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Stanley SA, Johndrow JE, Manzanillo P, Cox JS. The type I IFN response to infection with Mycobacterium tuberculosis requires ESX-1-mediated secretion and contributes to pathogenesis. J. Immunol. 2007;178:3143–3152. doi: 10.4049/jimmunol.178.5.3143. [DOI] [PubMed] [Google Scholar]
- 125.Zhang L, Jiang X, Pfau D, Ling Y, Nathan CF. Type I interferon signaling mediates Mycobacterium tuberculosis-induced macrophage death. J. Exp. Med. 2021;218:e20200887. doi: 10.1084/jem.20200887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cooper AM, Pearl JE, Brooks JV, Ehlers S, Orme IM. Expression of the nitric oxide synthase 2 gene is not essential for early control of Mycobacterium tuberculosis in the murine lung. Infect. Immun. 2000;68:6879–6882. doi: 10.1128/IAI.68.12.6879-6882.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Moreira-Teixeira L, et al. Type I IFN inhibits alternative macrophage activation during Mycobacterium tuberculosis infection and leads to enhanced protection in the absence of IFN-gamma signaling. J. Immunol. 2016;197:4714–4726. doi: 10.4049/jimmunol.1600584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.McNab F, Mayer-Barber K, Sher A, Wack A, O’Garra A. Type I interferons in infectious disease. Nat. Rev. Immunol. 2015;15:87–103. doi: 10.1038/nri3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Maiga M, et al. Risk of tuberculosis reactivation with tofacitinib (CP-690550) J. Infect. Dis. 2012;205:1705–1708. doi: 10.1093/infdis/jis269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Maiga M, et al. Efficacy of adjunctive tofacitinib therapy in mouse models of tuberculosis. EBioMedicine. 2015;2:868–873. doi: 10.1016/j.ebiom.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Vilcheze C, Jacobs WR., Jr The promises and limitations of N-acetylcysteine as a potentiator of first-line and second-line tuberculosis drugs. Antimicrob. Agents Chemother. 2021;65:e01703-20. doi: 10.1128/AAC.01703-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Amaral et al. A major role for ferroptosis in Mycobacterium tuberculosis-induced cell death and tissue necrosis. J. Exp Med.216, 556–570 (2019). [DOI] [PMC free article] [PubMed]
- 133.Mai NT, et al. A randomised double blind placebo controlled phase 2 trial of adjunctive aspirin for tuberculous meningitis in HIV-uninfected adults. eLife. 2018;7:e33478. doi: 10.7554/eLife.33478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Misra UK, Kalita J, Nair PP. Role of aspirin in tuberculous meningitis: a randomized open label placebo controlled trial. J. Neurol. Sci. 2010;293:12–17. doi: 10.1016/j.jns.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 135.Schoeman JF, Janse van Rensburg A, Laubscher JA, Springer P. The role of aspirin in childhood tuberculous meningitis. J. Child Neurol. 2011;26:956–962. doi: 10.1177/0883073811398132. [DOI] [PubMed] [Google Scholar]
- 136.Skerry C, et al. Simvastatin increases the in vivo activity of the first-line tuberculosis regimen. J. Antimicrob. Chemother. 2014;69:2453–2457. doi: 10.1093/jac/dku166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Dutta NK, et al. Statin adjunctive therapy shortens the duration of TB treatment in mice. J. Antimicrob. Chemother. 2016;71:1570–1577. doi: 10.1093/jac/dkw014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ralph AP, et al. High morbidity during treatment and residual pulmonary disability in pulmonary tuberculosis: under-recognised phenomena. PLoS One. 2013;8:e80302. doi: 10.1371/journal.pone.0080302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Meghji J, Simpson H, Squire SB, Mortimer K. A systematic review of the prevalence and pattern of imaging defined post-TB lung disease. PLoS One. 2016;11:e0161176. doi: 10.1371/journal.pone.0161176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ross J, Ehrlich RI, Hnizdo E, White N, Churchyard GJ. Excess lung function decline in gold miners following pulmonary tuberculosis. Thorax. 2010;65:1010–1015. doi: 10.1136/thx.2009.129999. [DOI] [PubMed] [Google Scholar]
- 141.Ehrlich RI, et al. Predictors of chronic bronchitis in South African adults. Int. J. Tuberc. Lung Dis. 2004;8:369–376. [PubMed] [Google Scholar]
- 142.Byrne AL, Marais BJ, Mitnick CD, Lecca L, Marks GB. Tuberculosis and chronic respiratory disease: a systematic review. Int. J. Infect. Dis. 2015;32:138–146. doi: 10.1016/j.ijid.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 143.Subbian S, et al. Pharmacologic inhibition of host phosphodiesterase-4 improves isoniazid-mediated clearance of Mycobacterium tuberculosis. Front. Immunol. 2016;7:238. doi: 10.3389/fimmu.2016.00238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Subbian S, et al. Adjunctive phosphodiesterase-4 inhibitor therapy improves antibiotic response to pulmonary tuberculosis in a rabbit model. EBioMedicine. 2016;4:104–114. doi: 10.1016/j.ebiom.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wallis RS, et al. Adjunctive host-directed therapies for pulmonary tuberculosis: a prospective, open-label, phase 2, randomised controlled trial. Lancet Respir. Med. 2021;9:897–908. doi: 10.1016/S2213-2600(20)30448-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Napier RJ, et al. Low doses of imatinib induce myelopoiesis and enhance host anti-microbial immunity. PLoS Pathog. 2015;11:e1004770. doi: 10.1371/journal.ppat.1004770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Napier RJ, et al. Imatinib-sensitive tyrosine kinases regulate mycobacterial pathogenesis and represent therapeutic targets against tuberculosis. Cell Host Microbe. 2011;10:475–485. doi: 10.1016/j.chom.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Han Q, Lin L, Zhao B, Wang N, Liu X. Inhibition of mTOR ameliorates bleomycin-induced pulmonary fibrosis by regulating epithelial-mesenchymal transition. Biochem. Biophys. Res. Commun. 2018;500:839–845. doi: 10.1016/j.bbrc.2018.04.148. [DOI] [PubMed] [Google Scholar]
- 149.Cabahug VLO, Uy HS, Yu-Keh E, Sapno KJD. Outcomes of treatment with sirolimus for non-infectious uveitis: a meta-analysis and systematic review. Clin. Ophthalmol. 2019;13:649–669. doi: 10.2147/OPTH.S198401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Singhal A, et al. Metformin as adjunct anti-tuberculosis therapy. Sci. Transl. Med. 2014;6:263ra159. doi: 10.1126/scitranslmed.3009885. [DOI] [PubMed] [Google Scholar]
- 151.Pan SW, et al. The risk of TB in patients with type 2 diabetes initiating metformin vs sulfonylurea treatment. Chest. 2018;153:1347–1357. doi: 10.1016/j.chest.2017.11.040. [DOI] [PubMed] [Google Scholar]
- 152.Lin SY, et al. Metformin is associated with a lower risk of active tuberculosis in patients with type 2 diabetes. Respirology. 2018;23:1063–1073. doi: 10.1111/resp.13338. [DOI] [PubMed] [Google Scholar]
- 153.Marupuru S, et al. Protective effect of metformin against tuberculosis infections in diabetic patients: an observational study of south Indian tertiary healthcare facility. Braz. J. Infect. Dis. 2017;21:312–316. doi: 10.1016/j.bjid.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Degner NR, Wang JY, Golub JE, Karakousis PC. Metformin use reverses the increased mortality associated with diabetes mellitus during tuberculosis treatment. Clin. Infect. Dis. 2018;66:198–205. doi: 10.1093/cid/cix819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ma Y, et al. Metformin reduces the relapse rate of tuberculosis patients with diabetes mellitus: experiences from 3-year follow-up. Eur. J. Clin. Microbiol. Infect. Dis. 2018;37:1259–1263. doi: 10.1007/s10096-018-3242-6. [DOI] [PubMed] [Google Scholar]
- 156.Padmapriydarsini C, et al. Randomized trial of metformin with Anti-tuberculosis drugs for early sputum conversion in adults with pulmonary tuberculosis. Clin. Infect. Dis. 2021 doi: 10.1093/cid/ciab964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Badri M, Wilson D, Wood R. Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: a cohort study. Lancet. 2002;359:2059–2064. doi: 10.1016/S0140-6736(02)08904-3. [DOI] [PubMed] [Google Scholar]
- 158.Tezera LB, et al. Anti-PD-1 immunotherapy leads to tuberculosis reactivation via dysregulation of TNF-alpha. eLife. 2020;9:e52668. doi: 10.7554/eLife.52668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Barber DL, et al. Tuberculosis following PD-1 blockade for cancer immunotherapy. Sci. Transl. Med. 2019;11:eaat2702. doi: 10.1126/scitranslmed.aat2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Fujita K, Terashima T, Mio T. Anti-PD1 antibody treatment and the development of acute pulmonary tuberculosis. J. Thorac. Oncol. 2016;11:2238–2240. doi: 10.1016/j.jtho.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 161.Tzelepis F, et al. Mitochondrial cyclophilin D regulates T cell metabolic responses and disease tolerance to tuberculosis. Sci. Immunol. 2018;3:eaar4135. doi: 10.1126/sciimmunol.aar4135. [DOI] [PubMed] [Google Scholar]
- 162.DiNardo AR, et al. Tuberculosis endotypes to guide stratified host-directed therapy. Med. 2021;2:217–232. doi: 10.1016/j.medj.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Manion M, et al. To induce immune reconstitution inflammatory syndrome or suppress it: the spectrum of Mycobacterium genavense in the antiretroviral era. Clin. Infect. Dis. 2020;72:315–318. doi: 10.1093/cid/ciaa753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.National Tuberculosis Association. Diagnostic Standards and Classification of Tuberculosis (NTA, 1940).
- 165.Albright FS, Orlando P, Pavia AT, Jackson GG, Cannon Albright LA. Evidence for a heritable predisposition to death due to influenza. J. Infect. Dis. 2008;197:18–24. doi: 10.1086/524064. [DOI] [PubMed] [Google Scholar]
- 166.Tadokoro T, et al. IL-6/STAT3 promotes regeneration of airway ciliated cells from basal stem cells. Proc. Natl Acad. Sci. USA. 2014;111:E3641–E3649. doi: 10.1073/pnas.1409781111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Garbers C, Heink S, Korn T, Rose-John S. Interleukin-6: designing specific therapeutics for a complex cytokine. Nat. Rev. Drug Discov. 2018;17:395–412. doi: 10.1038/nrd.2018.45. [DOI] [PubMed] [Google Scholar]
- 168.Arunachalam PS, et al. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science. 2020;369:1210–1220. doi: 10.1126/science.abc6261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rose-John S. Interleukin-6 family cytokines. Cold Spring Harb. Perspect. Biol. 2017;10:a028415. doi: 10.1101/cshperspect.a028415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Schnepf D, et al. Selective Janus kinase inhibition preserves interferon-lambda-mediated antiviral responses. Sci. Immunol. 2021;6:eabd5318. doi: 10.1126/sciimmunol.abd5318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Allwood BW, et al. Post-tuberculosis lung health: perspectives from the first international symposium. Int. J. Tuberc. Lung Dis. 2020;24:820–828. doi: 10.5588/ijtld.20.0067. [DOI] [PubMed] [Google Scholar]
- 172.Davis GL, et al. Treatment of chronic hepatitis C with recombinant interferon alfa. A multicenter randomized, controlled trial. N. Engl. J. Med. 1989;321:1501–1506. doi: 10.1056/NEJM198911303212203. [DOI] [PubMed] [Google Scholar]
- 173.Gillis S, Ferm MM, Ou W, Smith KA. T cell growth factor: parameters of production and a quantitative microassay for activity. J. Immunol. 1978;120:2027–2032. doi: 10.4049/jimmunol.120.6.2027. [DOI] [PubMed] [Google Scholar]
- 174.Kovacs JA, et al. Increases in CD4 T lymphocytes with intermittent courses of interleukin-2 in patients with human immunodeficiency virus infection. A preliminary study. N. Engl. J. Med. 1995;332:567–575. doi: 10.1056/NEJM199503023320904. [DOI] [PubMed] [Google Scholar]