Abstract
Over the past 20 years, the United States greatly expanded eligibility for public health insurance under the Medicaid and Child Health Insurance Program programs. This expansion improved children’s access to health care and their health, ultimately lowering preventable hospitalizations, chronic conditions, and mortality rates in the most vulnerable children at a cost that is 4 times lower than the average per capita cost for the elderly. They also had broader antipoverty effects, increasing economic security, children’s educational attainments, and their eventual employment and earnings opportunities. However, in recent years, this progress has been rolled back in many states. Remarkably, although income eligibility cutoffs have remained largely constant, states have reduced child coverage through a number of administrative measures ranging from increased paperwork, to reduced outreach, new parental work requirements, changes to public charge rules for immigrants, and waivers of federal requirements to provide retroactive coverage to new applicants. The number of uninsured children was rising for the first time in decades even prior to the pandemic. With rising numbers who have lost their jobs in the pandemic-induced recession, it is more important than ever to defend and restore and improve access to public health insurance for our children.
Keywords: children, coronavirus 2019, Medicaid, poverty, public health insurance access
Medicaid was adopted in 1965, at a time when only 40% to 50% of poor children had any doctor visits in a year.1 Over time, eligibility for Medicaid has been greatly expanded such that by the 2000s, half of all US births were covered.2 The fraction of children eligible for public health insurance rose from 15% to 20% to between 40% and 50%, depending on the age group, in part due to the adoption of the Child Health Insurance Program (CHIP).3 Figure 1 shows the median income eligibility cutoff for Medicaid or CHIP by child age and the cutoff for pregnant women from 2000 to 2020, while Figure 2 shows changes in the number of children enrolled in Medicaid and CHIP as well as the percentage of children who are uninsured over time. Income eligibility cutoffs initially rose but have been flat in recent years, whereas enrollments in Medicaid rose until 2016 and had been falling prior to the coronavirus 2019 (COVID-19) crisis. The fraction of children who were uninsured mirrored these trends, falling steadily until around 2016 when it began to rise. We return to these trends below.
Figure 1.
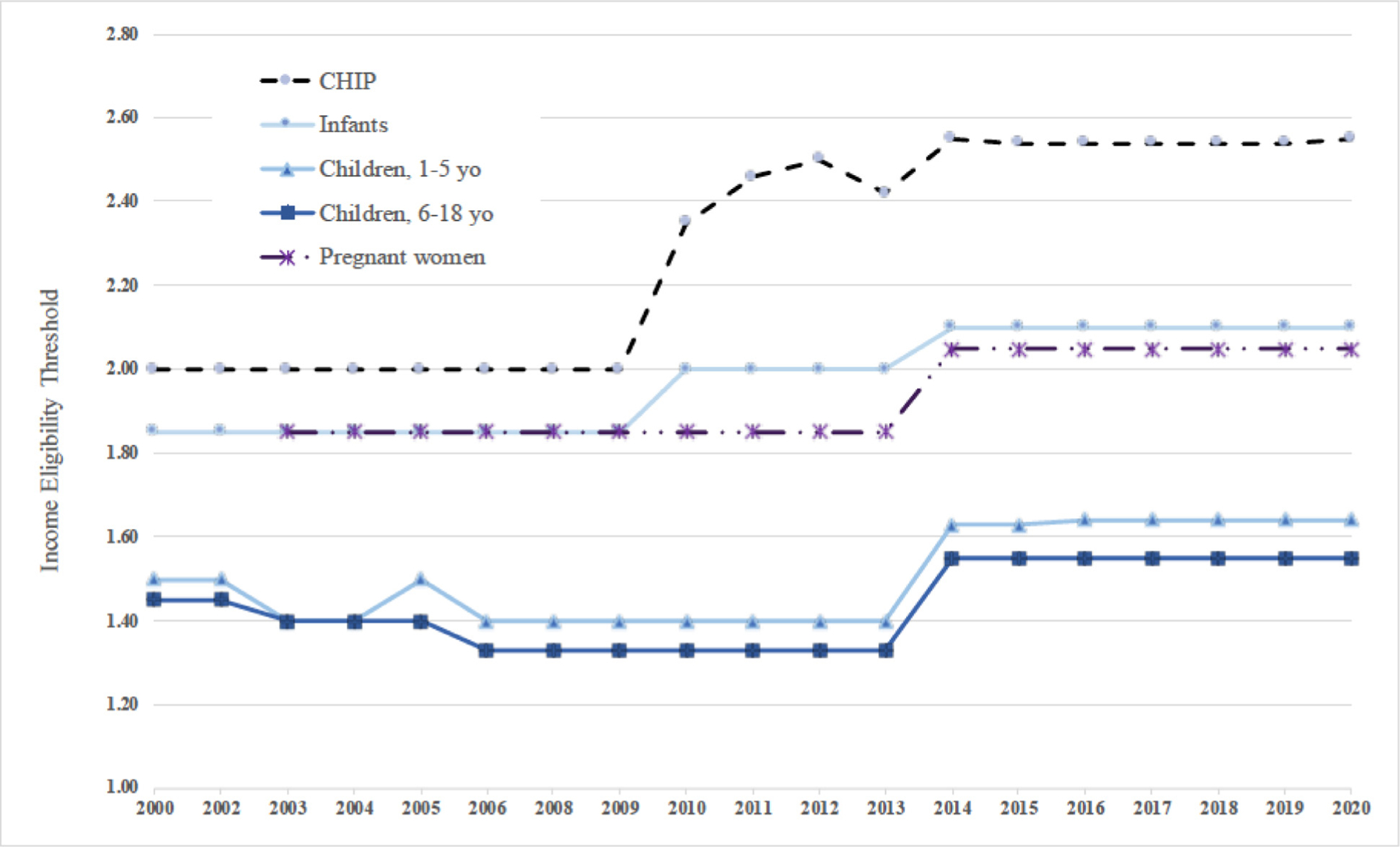
CHIP and Medicaid median income eligibility thresholds by eligibility category as a percentage of the Federal Poverty Line, 2000 to 2020. Notes: Data are from the Kaiser Family Foundation’s State Health Facts and are derived from a national survey conducted by the Kaiser Program on Medicaid and the Uninsured with the Center on Budget and Policy Priorities, 2000 to 2009; and with the Georgetown University Center for Children and Families, 2011 to 2020. Available at: https://www.kff.org/medicaid/report/annual-updates-on-eligibility-rules-enrollment-and-renewal-procedures-and-cost-sharing-practices-in-medicaid-and-chip/. CHIP indicates Child Health Insurance Program.
Figure 2.
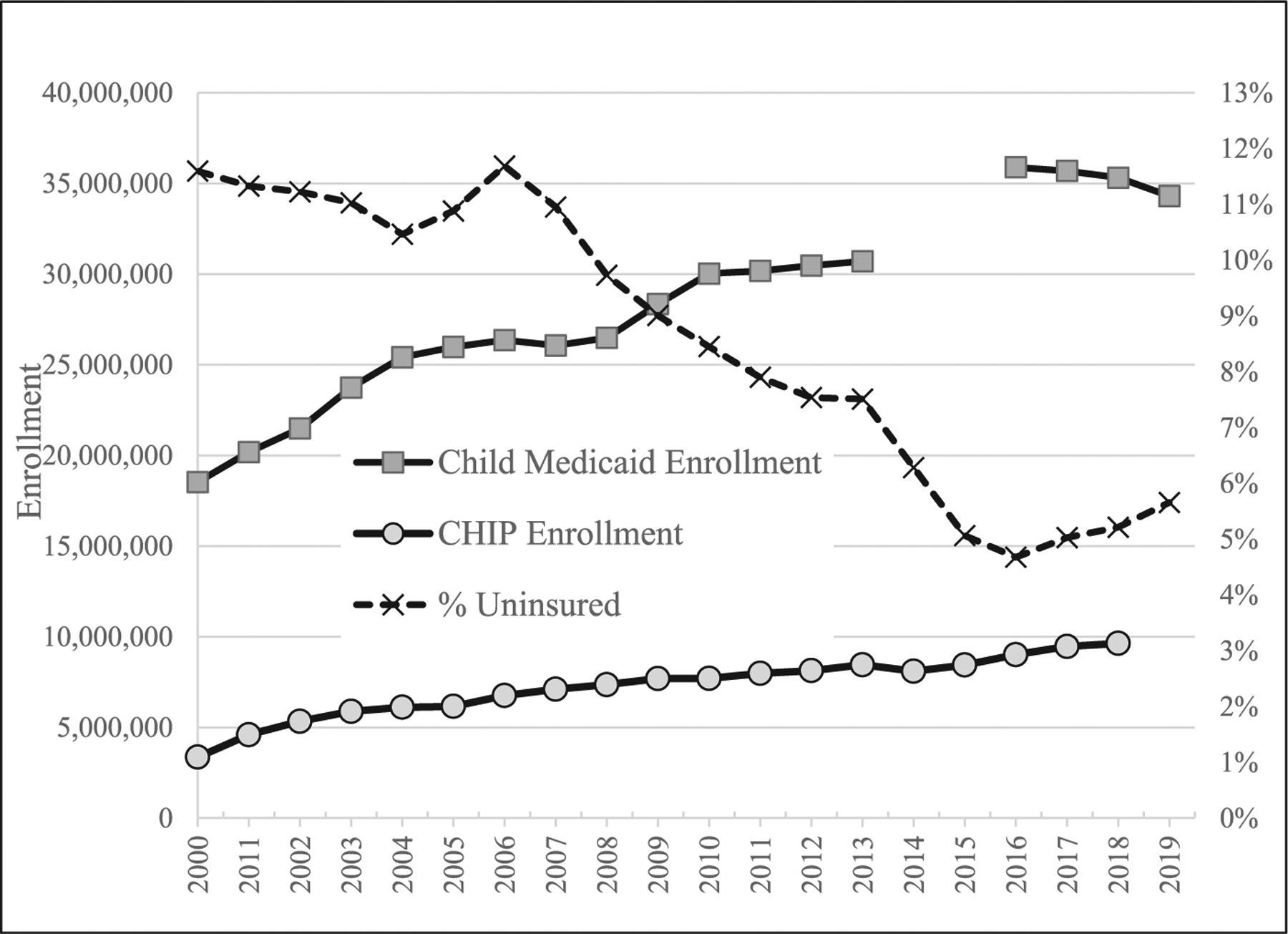
Child Medicaid and CHIP enrollments and percent of children who are uninsured. Notes: Child Medicaid enrollments come from MACStats Medicaid and CHIP data book, December 2019, Exhibit 7, https://www.macpac.gov/publication/medicaid-beneficiaries-persons-served-by-eligibility-group/. Children who qualified by reason of disability are not included in these totals. Data are missing for 2014 and 2015 because of a change in data systems. CHIP enrollment data come from the Kaiser Family Foundations State Health Facts, “Total Number of Children Ever Enrolled in CHIP Annually,” https://www.kff.org/other/state-indicator/annual-chip-enrollment. The percent uninsured are based on the author’s calculations. For 2008 to 2019, data are from the US Census’ American Community Surveys https://www.census.gov/data/tables/time-series/demo/health-insurance/acs-hi.html and refers to children less than 19. For 2000 to 2007, the data are from the US Census Bureau, Current Population Survey, Annual Social and Economic Supplements. 2000 to 2007. https://www.census.gov/data/tables/time-series/demo/health-insurance/historical-series/hia.html, and refers to children less than 18. CHIP indicates Child Health Insurance Program.
Medicaid and CHIP are administered by states. Although the cost is shared with the federal government, the state share absorbs over 15% of its total budget on average.4 This makes Medicaid vulnerable to cutbacks in the event of budget shortfalls such as state governments are currently experiencing due to the COVID-19 pandemic. Pregnant women and children make up the bulk of the Medicaid caseload. Hence, although the elderly and disabled have per capita costs over four times the average per capita cost for a child,4 children are often a more visible target for cutbacks given their sheer numbers.
Income eligibility cutoffs and administrative rules for Medicaid and CHIP vary widely from state to state. Administrative procedures can make it difficult for eligible people to enroll and stay enrolled. After rising for decades, child enrollments in public health insurance declined between 2016 and 2018 in several states, and the number of children without health insurance coverage increased. These declines can be attributed largely to changes in the program’s enrollment and re-enrollment rules. As many parents lose jobs due to the ongoing pandemic-induced recession and children lose access to private health insurance coverage, they are doing so at a time when it was already becoming increasingly difficult to enroll in public insurance in many states.
States also differ in terms of how they reimburse providers, and in terms of how many of these providers, pediatricians and other specialists, see Medicaid patients. Limited access to specialists has been an ongoing issue, which may disproportionally impact children with special health care needs (CSHCN).5 Given the copayments, lifetime maximums, and limits on covered procedures that are a feature of private health insurance, public health insurance is often the best option for these children despite difficulties initially accessing care.
This article makes three broad points. First, expansions of public health insurance since 1990 have had tremendously positive effects on child health, both in the short and long run. Second, although Medicaid is not accounted for in official poverty measures, the program has reduced poverty, especially for CSHCN. Since poverty itself has long lasting harmful effects on child health, poverty reduction enhances it.6 Third, recent changes to the Medicaid program are undermining these gains, and proposed changes are likely, if adopted, to exacerbate this trend. We end with some discussion of the current situation and some concluding recommendations about sustaining and improving public health insurance programs for pregnant women and children.
Benefits of Expanding Medicaid to Low-Income Pregnant women and Children
Expansions of public health insurance to pregnant women and children over the 1990s and 2000s had immediate positive effects. They led to declines in infant7 and child8 mortality and in preventable hospitalizations.9 As many as 6 million children began receiving preventive care as a result of the Medicaid expansions.10
Several recent studies document long-term effects of the expansions by comparing cohorts who became eligible for Medicaid in utero or in early childhood to slightly older cohorts who were ineligible. Cohorts who benefited from the Medicaid/CHIP expansions have higher educational attainment,11 12 earnings,13 self-reported health,3 and lower mortality14 and hospitalization rates15 than slightly older cohorts who did not benefit from the expansions. Recent research finds that new mothers who were covered by Medicaid as infants because of the expansions are giving birth to healthier children today.16
Using data from the introduction of Medicaid in the 1960s, we can trace out even longer-term effects. Studies that take advantage of large state-to-state variability in when Medicaid was introduced and who was eligible find that infant and child mortality fell more rapidly in states with bigger Medicaid expansions. At 20%, mortality declines were especially large among non-white children.1 Medicaid eligibility in early childhood also reduced disability and increased the probability that people were still working up to 50 years later.17,18 Careful estimates imply that for each dollar spent on children, the government saved 4 dollars in terms of future costs. If one includes not only cost savings to government, but benefits to the children themselves, then each dollar spent generates at least $12.66.19 These estimates are based on data in the appendix of Hendren and Sprung-Keyser.19 Benefits to government include cost savings from hospitalizations and emergency visits and higher future taxes paid by children. Benefits to children include the value of lives saved and the value of children’s higher future after-tax income.
Public Health Insurance Reduces Poverty
Medicaid is the largest transfer program for nonelderly, low-income Americans. Table 1 shows that Medicaid pays about $2115 per child, which is comparable to the average of $2151 in total health care spending for children who are not on Medicaid. Even prior to the Affordable Care Act, about $180 billion annually was spent on low-income children and adults in poor families annually,20 which is much more than is spent on either Supplemental Nutrition Assistance Program, formerly known as Food Stamps, or the Earned Income Tax Credit, which each cost approximately $70 billion annually.21,22
Table 1.
Health Care Expenditures and Utilization by Medicaid/CHIP and Child Special Health Care Needs (CSHCN) Status
| All Children | Not CSHCN | CSHCN | CSHCN: Severe | |||||
|---|---|---|---|---|---|---|---|---|
| Non-Medicaid | Medicaid/CHIP | Non-Medicaid | Medicaid/CHIP | Non-Medicaid | Medicaid/CHIP | Non-Medicaid | Medicaid/CHIP | |
| Demographics | ||||||||
| Age | 10 | 8 | 9 | 8 | 10 | 9 | 10 | 10 |
| Annual family income | 110,501 | 37,986 | 109,573 | 37,479 | 114,861 | 39,107 | 113,875 | 44,118 |
| Average annual health care spending per child (real 2019 dollars) | ||||||||
| Total | 2151 | 2115 | 1405 | 757 | 4518 | 5314 | 10,346 | 14,181 |
| Office | 669 | 468 | 467 | 231 | 1363 | 1054 | 3526 | 2789 |
| Emergency room | 118 | 98 | 95 | 73 | 185 | 159 | 264 | 241 |
| Hospital | 44 | 58 | 22 | 18 | 107 | 141 | 263 | 311 |
| Home Health | 27 | 188 | 4 | 12 | 110 | 628 | 363 | 3136 |
| Prescription drugs | 258 | 393 | 48 | 38 | 930 | 1280 | 2722 | 2554 |
| Share with non-zero utilization in a year | ||||||||
| Any health care | 87.3% | 85.0% | 85.2% | 81.4% | 96.6% | 95.4% | 97.3% | 98.3% |
| Office | 74.4% | 71.2% | 70.9% | 66.1% | 88.7% | 84.9% | 91.5% | 93.4% |
| Emergency room | 9.4% | 14.9% | 8.1% | 12.6% | 13.8% | 20.9% | 17.3% | 21.6% |
| Hospital | 1.7% | 2.9% | 1.2% | 1.6% | 2.7% | 5.2% | 5.4% | 9.4% |
| Home Health | 0.5% | 1.7% | 0.1% | 0.4% | 1.5% | 5.0% | 6.1% | 54.5% |
| Prescription drugs | 44.6% | 45.5% | 34.9% | 33.8% | 78.2% | 76.5% | 84.5% | 86.5% |
| Average out-of-pocket health care spending per child annually (real 2019 dollars) | ||||||||
| Total | 440.9 | 72.4 | 329.7 | 47.3 | 805.5 | 131.2 | 1463.1 | 280.7 |
| Office | 127.9 | 15.5 | 82.3 | 7.3 | 279.1 | 35.8 | 730.1 | 82.5 |
| Emergency room | 19.7 | 2.7 | 16.8 | 2.4 | 27.3 | 3.5 | 49.6 | 3.3 |
| Hospital | 15.0 | 3.2 | 10.3 | 1.7 | 20.6 | 4.7 | 28.6 | 7.2 |
| Home Health | 0.4 | 1.3 | 0.0 | 0.0 | 1.5 | 4.5 | 6.2 | 28.5 |
| Prescription drugs | 47.8 | 11.0 | 14.0 | 2.1 | 153.6 | 32.0 | 296.7 | 60.4 |
| Number children 0–17 | 52,047 | 58,238 | 36,787 | 39,145 | 10,092 | 13,779 | 718 | 1897 |
| Est. population (2008–18) | 535,414,213 | 325,898,220 | 382,913,949 | 220,990,786 | 118,379,878 | 89,641,163 | 8,765,576 | 13,591,263 |
CHIP indicates Child Health Insurance Program.
Notes: Author’s calculations based on Medical Expenditure Panel Survey, 2008 to 2018 which covers children 0 to 17. Insurance status is recorded as of December of the year before. Individual weights are applied to calculate population means. CSHCN are characterized as severe if they answer yes to 4 out of 5 qualifying questions. The questions pertain to the following: the need or use of medicines prescribed by a doctor; the need or use of more medical care, mental health, or education services than is usual for most children; being limited or prevented in doing things most children can do; the need or use of special therapy such as physical, occupational, or speech therapy; and the need or use of treatment or counseling for emotional, developmental, or behavioral problems.
It is ironic then that Medicaid benefits are excluded from the official poverty measure, which includes only cash income. The Census bureau produces a supplemental poverty measure which includes many other in-kind benefits like Supplemental Nutrition Assistance Program, but does not include Medicaid. Hence, Medicaid cannot reduce measured poverty rates because it is not included in these calculations.6
Valuing health insurance coverage is challenging. Out of pocket costs incurred by families are a poor proxy for the value of health care. Families may defer or forgo care when they cannot afford it. Furthermore, unlike food or housing, acute health care needs are episodic. However infrequent the need for health coverage, having health insurance contributes to peace of mind and prevents family financial crises.
One possible solution to including public health insurance in supplemental poverty estimates is to estimate the value of the insurance rather than the value of health care per se. Since the introduction of the Affordable Care Act in 2014, it is possible to use health insurance exchanges to calculate a market-based value of health insurance for every family. Using this approach, a supplemental poverty threshold can be defined by adding the value of health insurance to a family’s total needs along with food and shelter. Policymakers can then consider how many families would fall below this threshold without Medicaid or CHIP. This exercise suggests that Medicaid and CHIP reduced poverty from 23.7% of US children to 18.4% of US children in 2014, a decline of 22%.23
The large medical costs facing parents of CSHCN provide another perspective on the antipoverty effects of Medicaid and CHIP. Table 1 shows that for CSHCN, Medicaid and CHIP pay an average of $5314 per child, which can be compared to average income of $39,107 in their families. This payment is more than the $4518 per child paid for non-Medicaid CSHCN children most of whom have private health insurance. Among the sickest CSHCN (labeled “severe”), public insurance pays $14,181 per year, which can be compared to average family incomes of $44,118 among these children. The largest single category of expenditure ($3136) for these children is home health services which are much more generous than what is available for non-Medicaid children ($363). These supports may be essential for allowing parents to work outside the home and to care for other children.
Recent Worrying Trends in Medicaid and CHIP Enrollments
Even prior to the pandemic and pandemic-induced recession, there were ominous signs that decades of progress increasing children’s health insurance coverage was being reversed. The number of children without health insurance rose from 4.7% in 2016 to 5.7% by 2019, while among Hispanic children, this number rose to 9.2%.24 These losses were entirely accounted for by declines in public insurance, since private health insurance coverage remained constant. Twenty-nine states showed deteriorations in children’s health insurance coverage between 2016 and 2019.25
Remarkably, these swings occurred despite the stability in income eligibility cutoffs shown in Figure 1. Instead, they likely reflect changes in the way that public health insurance programs are being administered. New requirements result in eligible children being denied coverage due to administrative hurdles that appear to be designed to reduce the Medicaid rolls. Some of these changes have been implemented in response to stricter federal government audits. For example, Idaho had automatically been re-enrolling low-income people using state administrative data to verify their eligibility. The Trump administration ruled that applicants must now provide documentation of their (lack of) income.26 Texas now checks the income of children in the fifth, sixth, seventh, and eighth month of enrollment. Unless information is provided and entered into the system, the children’s cases are automatically closed.27 In Tennessee, 220,000 children were dropped from the Medicaid rolls due to incomplete or missing paperwork in 2019 alone in a system that relied on mailing paper forms.28
Other changes may be introduced in the form of “waivers” of federal rules governing administrative requirements and eligibility rules. One potentially important example has been the push to introduce work requirements for Medicaid enrollees. Although they target adults rather than children, children tend to lose coverage when parents do.29 While blocked by courts in most cases, where these waivers have been imposed they have led to dramatic reductions in Medicaid rolls: In Arkansas, 17,000 out of 65,000 people targeted lost coverage. Many of them remained eligible, but were unable to meet onerous reporting requirements which involved accessing computers and contacting the welfare office during work hours.30
Another common type of waiver limits retroactive Medicaid coverage. Normally providers can be reimbursed for services provided up to 90 days before a patient’s enrollment paperwork is approved by Medicaid. This flexibility allows providers to serve eligible but unenrolled patients and to be reimbursed as long as the patient’s application is ultimately approved. These waivers have been approved for 27 states. Some waivers of retroactive coverage requirements apply only to adults (though these may impact children indirectly), but many also include children. For example, all Delaware Medicaid enrollees in managed care are now covered only as of the date of their application, and similar limits are in place for TennCare in Tennesee.31
Anti-immigrant rhetoric and administrative changes may also have been responsible for declines in enrollment among Hispanic children, including citizen children. In 2019, the Trump administration announced that any immigrant using Medicaid for more than 12 months could be deemed a “public charge” which could lead to denial of applications for green cards. While this has been subject to much litigation, there is no doubt that the prospect of being deemed a public charge has had a chilling effect on participation in Medicaid. The Kaiser Family Foundation reports that in a recent survey of health centers, 28% reported that immigrant parents have been disenrolling their children from Medicaid.32 The Urban Institute reports that in 2018 1 in 5 Hispanic immigrant families reported that they avoided using public benefits and 42% of these respondents said that someone in their household was avoiding using Medicaid or CHIP.33 These fears may be one reason for the shockingly high rate of uninsured children in Texas in 2019: 17.5%.25
Funds for enrollment and outreach have also been slashed.34 While it is difficult to say which policies were most responsible for declines in child health insurance between 2017 and the end of 2019, the net effect was clearly to discourage enrollment.
Table 2 provides information for each state about changes in the percentage of children with Medicaid or CHIP between June 2014 to December 2016, January 2017 to December 2019, and January 2020 to August 2020. One can see that in many states, there were large gains in the first period, followed by large declines from 2017 to 2019. The first eight months of 2020 saw some increases in Medicaid and CHIP enrollments in most states as families became newly eligible due to income losses from the pandemic.
Table 2.
Percent Change in Medicaid Child and CHIP Enrollments, June 2014 to December 2016, January 2017 to December 2019, and January 2020 to June 2020
| State | June 2014–Dec 2016 | January 2017–December 2019 | January 2020–August 2020 | State | June 2014–December 2016 | January 2017–December 2019 | January 2020–August 2020 |
|---|---|---|---|---|---|---|---|
| North Carolina | 28.8% | −17.5% | 3.9% | Iowa | 4.3% | 9.5% | 3.1% |
| Missouri | 26.0% | −16.3% | 12.6% | New York | 4.1% | −3.2% | 3.3% |
| Montana | 16.1% | −4.4% | 0.3% | Oklahoma | 3.9% | −6.2% | 11.6% |
| Idaho | 15.5% | −9.9% | 6.6% | Delaware | 3.4% | −0.3% | 4.6% |
| Florida | 14.9% | −6.9% | 8.0% | Louisiana | 3.3% | −8.5% | 3.3% |
| Alaska | 14.1% | 13.8% | 0.5% | New Hampshire | 2.7% | −5.1% | 5.4% |
| Colorado | 14.0% | −11.5% | 3.9% | Nebraska | 2.6% | 2.4% | 4.4% |
| Rhode Island | 13.3% | −1.9% | 1.6% | Virginia | 2.6% | 13.8% | 4.8% |
| Washington | 13.0% | −2.8% | 2.6% | Hawaii | 1.4% | −4.0% | 6.8% |
| Massachusetts | 12.6% | 3.3% | 3.6% | Maryland | 1.0% | 1.6% | 3.6% |
| Minnesota | 11.5% | 2.0% | 4.8% | Mississippi | −1.0% | −9.6% | 5.0% |
| Nevada | 10.9% | −1.6% | 8.4% | Connecticut | −1.4% | 8.8% | 3.2% |
| Indiana | 10.5% | 1.1% | 5.1% | Georgia | −1.5% | 1.8% | 9.1% |
| Pennsylvania | 9.1% | −0.1% | 4.3% | Kansas | −1.7% | −5.6% | 8.9% |
| New Jersey | 8.9% | −4.6% | 4.7% | Alabama | −1.7% | 5.9% | 2.0% |
| West Virginia | 7.8% | −6.4% | 3.5% | Oregon | −4.8% | 0.9% | 3.9% |
| Utah | 7.3% | −15.7% | 10.2% | Ohio | −5.7% | 1.2% | 5.7% |
| Kentucky | 7.1% | 4.5% | 7.4% | Illinois | −6.3% | −7.1% | 3.9% |
| Texas | 6.4% | −7.2% | 8.7% | Maine | −8.6% | −8.6% | 6.9% |
| South Carolina | 5.6% | 0.8% | 2.2% | Michigan | −11.2% | −1.0% | 4.5% |
| Vermont | 5.5% | −5.6% | 3.3% | Wyoming | −13.4% | −3.1% | 9.3% |
| South Dakota | 4.9% | −6.5% | 6.6% |
Notes: States are sorted from largest positive to largest negative percentage changes in enrollment between June 2014 and Dec. 2016. Numbers show the authors’ calculations based on The Centers for Medicare & Medicaid Services “Monthly Medicaid & CHIP Application, Eligibility Determination, and Enrollment Reports & Data”, 2014 to 2020 available at: https://www.medicaid.gov/medicaid/national-medicaid-chip-program-information/medicaid-chip-enrollment-data/monthly-medicaid-chip-application-eligibility-determination-and-enrollment-reports-data/index.html. AR, AZ, CA, DC, ND, NM, TN, and WI are excluded from the table because their data are incomplete.
Figure 3 illustrates these patterns for four states. One can see the very sharp increases in the period following the implementation of the Affordable Care Act in 2014. This increase occurred even in states like Texas that chose not to expand Medicaid to low-income adults. This period of expansion was followed by sharp declines as the administrative measures described above came into effect. However, in the past 6 months, enrollment has climbed once again, especially in the last few months (as of this writing, data were available through August 2020).
Figure 3.
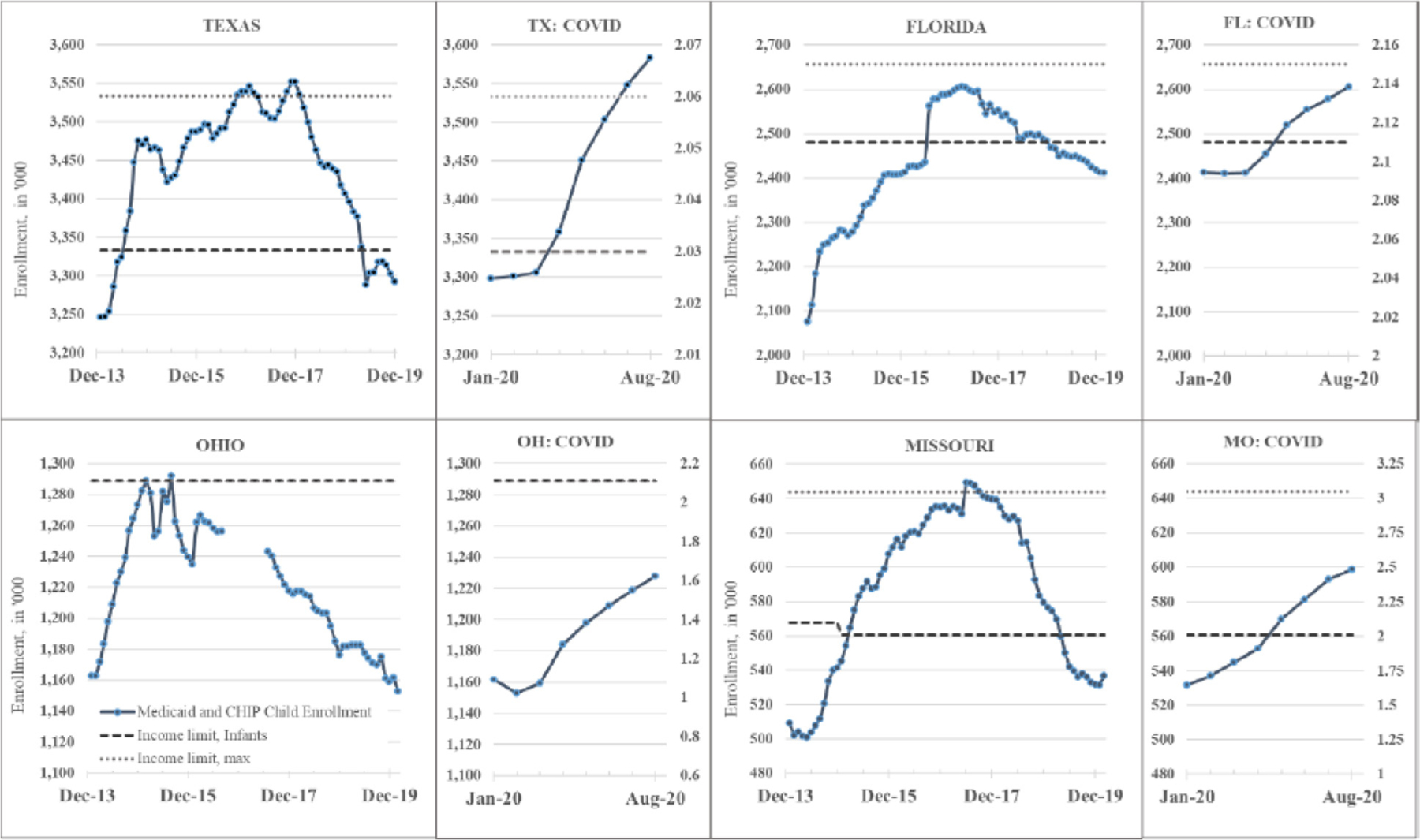
Trends in child Medicaid and CHIP enrollments in 4 states. Notes: Based on the same data as Table 2. The x-axis is expanded for January to June 2020 to show trends in the first months of the pandemic in greater detail. Dashed lines show income eligibility cutoffs as percent of the Federal Poverty Level. CHIP indicates Child Health Insurance Program.
Medicaid and COVID-19
Due to the pandemic, unemployment spiked from a historically low level of less than 4% in February 2020 to almost 15% in April, though by December 2020, it was down to 6.7%.35 The majority of US children are covered as dependents on their parent’s employer-sponsored health insurance plans. Hence, if large numbers of parents lose their jobs, many children would be left without private health insurance. However, the current recession is disproportionately affecting low-income workers, many of whom were not covered by private insurance. Some of these workers were covered by a family member’s policy, while others were already enrolled in Medicaid or had children enrolled in Medicaid or CHIP. And some employers used funds from the Paycheck Protection Program to continue to pay the health insurance premiums of furloughed workers.
The Urban Institute has used data on hundreds of thousands of individuals to simulate the effects of the increases in unemployment using the Congressional Budget Office’s projected changes in unemployment rates through the end of 2020. They estimate that 7.3 million people will lose employer sponsored health insurance coverage, that 4.3 million will become eligible for Medicaid or CHIP, and that 2.9 million will become uninsured including 300,000 children.36,,25 These numbers translate into a projected 6.1% increase in total projected Medicaid enrollments through the end of 2020. Using the monthly enrollment figures underlying Table 2, we calculate that child Medicaid and CHIP enrollments grew 5.1% between February and August 2020, and they likely continued to grow through the rest of the year.*
One reason that Medicaid has been able to fulfill its function as a safety net so far is that the federal Coronavirus Aid, Relief, and Economic Security Act (CARES Act) specified that states could not disenroll any Medicaid beneficiary until after the coronavirus national emergency declaration has been lifted. The prohibition on disenrollment even applies to pregnant women on Medicaid who are past 60 days postpartum, effectively increasing their eligibility period. Unfortunately, the prohibition does not apply to CHIP enrollees.37 The act also increased the federal share of state Medicaid costs for the duration of the public health emergency.
Recommendations
Expansions of Medicaid and CHIP have had a tremendously positive impact on children and their families. Some attempt should be made to incorporate health insurance coverage into supplemental poverty measures so that the value of these expenditures can be better understood.
Given the demonstrated success of Medicaid and CHIP, we need to reverse administrative changes that have limited access and reduced caseloads of otherwise eligible children since 2016. These changes combined with the chilling effect of anti-immigrant rhetoric all make it less likely that children will have health insurance coverage. Other proposed changes, such as work requirements, limiting federal payments to states by changing Medicaid to a “block grant,” or imposing per capita payment limits would have the same effect, and should be opposed. Mandatory 12-month continuous eligibility periods would be one way to mitigate against insurance coverage losses due to red tape.
Remarkably, the CARES Act has in fact suspended many of the actions that are leading to Medicaid disenrollments and denials of coverage. This response to the pandemic seems tantamount to an acknowledgment that current federal and state administrative policies are reducing insurance coverage by disenrolling eligible children. The prohibition should be extended to cover women and children with CHIP coverage as well as Medicaid. CHIP should also be made permanent in order to eliminate periodic re-authorization battles and uncertainty about the future of the program. Eliminating lockouts (the 90-day period when a disenrolled child is prohibited from re-enrollment) and waiting periods, and reducing premiums would all have a more immediate effect on CHIP enrollments.
Longer-standing access issues should be addressed by making Medicaid reimbursements more comparable to those of private payers. We understand the impulse to broaden the Medicaid program in order to address socioeconomic determinants of child health, but fear that could result in existing funding being spread even more thinly. Hence, while there should be enhanced coordination across programs, such as using participation in one anti-poverty program as proof of eligibility for others, income support, housing, nutrition assistance and so on should continue to be addressed through purpose-built programs that have institutional capacity rather than through Medicaid or CHIP.
Finally, given the unprecedented demands that the COVID-19 pandemic is placing on Medicaid and on state budgets, it is essential that states receive additional emergency funding earmarked for supporting their Medicaid and CHIP programs, and that children receive a fair share of any such additional funding. The CARES Acts higher federal match rate for the duration of the public health emergency is a start, but even after the immediate health crisis is past, states will likely continue to need such aid and the government could consider making a counter-cyclical increase in match rates a permanent feature of the Medicaid program.
What’s New.
This article discusses historical expansions of child Medicaid coverage and their effects on health and poverty. It reviews recent losses in child health coverage and their reasons including pandemic job losses and administrative changes to the program.
Acknowledgment
Currie acknowledges support from Princeton’s Center for Health and Wellbeing.
Financial disclosure:
This article is published as part of a supplement sponsored by the Robert Wood Johnson Foundation.
Footnotes
Although this most recent report does not break down insurance changes by age, combining these numbers with those from an earlier report suggests that about 200,000 children may be come uninsured as a result of pandemic related employment losses. See the earlier report at: Robert Wood Johnson Foundation, Twenty-five million workers or more could lose employer-based health insurance due to COVID-19-related unemployment, https://www.rwjf.org/en/library/research/2020/05/how-the-covid-19-recession-could-affect-health-insurance-coverage.html; Accessed 6 October 2020.
The authors do not have any conflicts of interest to report.
References
- 1.Goodman-Bacon A Public insurance and mortality: evidence from Medicaid implementation. J Polit Econ. 2018;126:216–262. [Google Scholar]
- 2.Markus AR, Ellie A, West KD, et al. Medicaid covered births 2008 through 2010 in the context of the implementation of health reform. Women’s Health Issues. 2013;23:e273–e280. [DOI] [PubMed] [Google Scholar]
- 3.Currie J, Decker S, Lin W. Has public health insurance for older children reduced disparities in access to care and health outcomes? J Health Econ. 2008;27:1407–1652. [DOI] [PubMed] [Google Scholar]
- 4.Currie J, Duque V. Medicaid: what does it do, and can we do it better? Ann Am Acad Pol Soc Sci. 2019;686:148–179. [Google Scholar]
- 5.Laurie E, Felland L, Amanda E, et al. Improving Access to Specialty Care for Medicaid Patients: Policy Issues and Options. The Commonwealth Fund; 2013. [Google Scholar]
- 6.National Academies of Sciences, Engineering, and Medicine. A Roadmap to Reducing Child Poverty. Washington, DC: National Academies Press; 2019. [PubMed] [Google Scholar]
- 7.Currie J, Gruber J. Saving babies: the efficacy and cost of recent changes in the Medicaid eligibility of pregnant women. J Polit Econ. 1996;104:1263–1296. [Google Scholar]
- 8.Currie J, Gruber J. Health insurance eligibility, utilization of medical care, and child health. Q J Econ. 1996;111:431–466. [Google Scholar]
- 9.Dafny L, Gruber J. Public insurance and child hospitalizations: access and efficiency effects. J Public Econ. 2005;89:109–129. [Google Scholar]
- 10.Howell E, Kenney G. The impact of the Medicaid/CHIP expansions on children: a synthesis of the evidence. Med Care Res Rev. 2012; 69:372–396. [DOI] [PubMed] [Google Scholar]
- 11.Levine P, Schanzenbach D. The impact of children’s public health insurance expansions on educational outcomes. In: Cutler D, Garber A, Goldman D, eds. Forum for Health Research and Policy. Boston, Mass: De Gruyter; 2009:1–28. [Google Scholar]
- 12.Cohodes S, Grossman D, Kleiner S, et al. The effect of child health insurance access on schooling: evidence from public insurance expansions. J Hum Resour. 2016;51:727–759. [Google Scholar]
- 13.Brown DW, Kowalski A, Lurie IZ. Long-term impacts of childhood Medicaid expansions on outcomes in adulthood. Rev Econ Stud. 2020;87:792–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wherry L, Meyer B. Saving teens: using a policy discontinuity to estimate the effects of Medicaid eligibility. J Hum Resour. 2016; 51:556–588. [Google Scholar]
- 15.Miller S, Wherry L. The long-term effects of early life Medicaid coverage. J Hum Resour. 2019;54:785–824. [Google Scholar]
- 16.East CN, Miller S, Page M, et al. Multi-Generational Impacts of Childhood Access to the Safety Net: Early Life Exposure to Medicaid and the Next Generation’s Health. Cambridge, Mass: National Bureau of Economic Research; 2017. (NBER Working Paper No. 23810). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodman-Bacon A The Long-Run Effects of Childhood Insurance Coverage: Medicaid Implementation, Adult Health, and Labor Market Outcomes. Cambridge, Mass: National Bureau of Economic Research; 2016. (NBER Working Paper No. 22899). [Google Scholar]
- 18.Boudreaux M, Golberstein E, McAlpine D. The long-term impacts of Medicaid exposure in early childhood: evidence from the program’s origin. J Health Econ. 2016;45:161–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hendren N, Sprung-Keyser B. A unified welfare analysis of government policies. Q J Econ. 2020;135:1209–1318. [Google Scholar]
- 20.Kaiser Family Foundation. Medicaid spending by eligibility group. 2014. Available at: www.kff.org/medicaid/state-indicator/medicaid-spending-by-enrollment-group/?currentTimeframe=0&sortModel”{“colId”:”Location”,”sort”:”asc”}. Accessed October 5, 2020.
- 21.US Dept of Agriculture, Supplemental Nutrition Assistance Program, Available at: https://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap. Accessed October 5, 2020.
- 22.The Joint Committee on Taxation, Estimates of federal tax expenditures for fiscal years 2016–2020, Available at: https://www.jct.gov/publications.html?func=startdown&id=4971. Accessed October 5, 2020.
- 23.Korenman S, Remler D, Hyson R. Accounting for the impact of Medicaid on child poverty Sanders Korenman, 2017, Available at: https://www.nap.edu/resource/25246/Korenman%20Remler%20and%20Hyson.pdf. Accessed October 5, 2020.
- 24.Berchick ER, Laryssa Mykyta L. Children’s public health insurance coverage lower than in 2017, 2019, Available at: https://www.census.gov/library/stories/2019/09/uninsured-rate-for-children-in-2018.html. Accessed October 5, 2020.
- 25.Alker J, Corcoran A. Georgetown University Health Policy Institute Center for Children and Families. Children’s uninsured rate rises by largest annual jump in more than a decade. Available at: https://ccf.georgetown.edu/wp-content/uploads/2020/10/ACS-Uninsured-Kids-2020_10-06-edit-3.pdf. Accessed January 15, 2021. [Google Scholar]
- 26.Center on Budget and Policy Priorities. Medicaid improper payment rates don’t measure ineligible enrollees, fraud, or abuse; 2019. Available at: https://www.cbpp.org/blog/medicaid-improper-payment-rates-dont-measure-ineligibleenrollees-fraud-or-abuse. Accessed October 5, 2020.
- 27.Georgetown University Health Policy Institute, Center for Children and Families. Families first coronovirus response act freezes disenrollment in Medicaid; 2020. Available at: https://ccf.georgetown.edu/2020/03/23/families-first-coronavirus-response-act-freezes-disenrollment-in-medicaid/. Accessed October 5, 2020.
- 28.Kelman B and Reicher M. At least 220,000 Tennessee kids faced loss of health insurance due to lacking paperwork. The Tennessean; 2019. Available at: https://www.tennessean.com/story/news/investigations/2019/07/14/tenncare-coverkids-medicaidchildren-application-insurance-denied/1387769001/. Accessed January 15, 2021. [Google Scholar]
- 29.Center on Budget and Policy Priorities. Taking away Medicaid for not meeting work requirements harms children; 2020. Available at: https://www.cbpp.org/research/health/taking-away-medicaid-for-not-meeting-workrequirements-harms-children. Accessed October 5, 2020.
- 30.Scott D 16932 people have lost Medicaid coverage under Arkansas’s work requirements; 2020. Available at: https://www.vox.com/policy-and-politics/2018/12/18/18146261/arkansas-medicaid-work-requirements-enrollment. Accessed October 5, 2020. [Google Scholar]
- 31.MACPAC, Medicaid retroactive eligibility: changes under section 1115 waivers. 2019. Available at: https://www.macpac.gov/wp-content/uploads/2019/08/Medicaid-Retroactive-Eligibility-Changes-under-Section-1115-Waivers.pdf. Accessed October 5, 2020.
- 32.Tolbert J, Artiga S, Pham O. Impact of Shifting Immigration Policy on Medicaid Enrollment and Utilization of Care Among Health Center Patients. San Francisco, Calif: Henry J. Kaiser Family Foundation; 2019. Available at: https://www.kff.org/report-section/impact-of-shifting-immigration-policy-on-medicaid-enrollment-and-utilization-of-care-among-health-center-patients-issue-brief/. [Google Scholar]
- 33.Bernstein H, Gonzalez D, Karpman M, et al. With public charge rule looming, one in seven adults in immigrant families reported avoiding public benefit programs in 2018; 2018. Available at: https://www.urban.org/urban-wire/public-charge-rule-looming-one-seven-adults-immigrant-families-reported-avoiding-public-benefit-programs-2018. Accessed January 15, 2021.
- 34.Cloud H In Latest ACA Sabotage, Administration Nearly Eliminates Marketplace Enrollment Assistance Funds. Center on Budget and Policy Priorities; 2018. Available at: https://www.cbpp.org/blog/in-latest-aca-sabotage-administration-nearly-eliminates-marketplace-enrollment-assistance-funds. Accessed October 12, 2020. [Google Scholar]
- 35.The Employment Situation—September 2020. News Release of the Bureau of Labor Statistics U.S. Department of Labor. Available at: https://www.bls.gov/news.release/pdf/empsit.pdf. Accessed October 12, 2020. [Google Scholar]
- 36.Banthin J, Simpson M, Buettgens M, Blumberg L, Wang R. Changes in Health Insurance Coverage Due to the COVID-19 Recession: Preliminary Estimates Using Microsimulation. Robert Wood Johnson Foundation; 2020. Available at: https://www.urban.org/sites/default/files/publication/102552/changes-in-health-insurance-coverage-due-to-the-covid-19-recession_4.pdf. Accessed January 15, 2021. [Google Scholar]
- 37.Georgetown University Health Policy Institute Center for Children and Families, Families first coronavirus response act freezes disenrollment in Medicaid. Available at: https://ccf.georgetown.edu/2020/03/23/families-first-coronavirus-response-act-freezes-disenrollment-in-medicaid/. Accessed October 6, 2020.


