Background:
The coronavirus disease 2019 (COVID-19) pandemic necessitated the replacement of in-person physician consultations with telemedicine. During the pandemic, Medicaid covered the cost of telemedicine visits.
Objectives:
The aim was to measure the adoption of telemedicine during the pandemic. We focus on key patient subgroups including those with chronic conditions, those living in urban versus rural areas, and different age groups.
Methods:
This study examined the universe of claims made by Florida Medicaid beneficiaries (n=2.4 million) between January 2019 and July 2020. Outpatient visits were identified as in-person or telemedicine. Telemedicine visits were classified into audio-visual or audio-only visits.
Results:
We find that telemedicine offsets much of the decline in in-person outpatient visits among Florida’s Medicaid enrollees, however, uptake differs by enrollee type. High utilizers of care and beneficiaries with chronic conditions were significantly more likely to use telemedicine, while enrollees living in rural areas and health professional shortage areas were moderately less likely to use telemedicine. Elderly Medicaid recipients (dual-eligibles) used audio-only telemedicine visits at higher rates than other age groups, and the demand for these consultations is more persistent.
Conclusions:
Telemedicine offset the decline in health care utilization among Florida’s Medicaid-enrolled population during the novel coronavirus pandemic, with particularly high uptake among those with prior histories of high utilization. Audio-only visits are a potentially important method of delivery for the oldest Medicaid beneficiaries.
Key Words: telemedicine, COVID-19, Medicaid
The ongoing coronavirus disease 2019 (COVID-19) pandemic necessitated restrictions on contact between individuals to slow the spread of the virus. One consequence was that medical consultations that would have previously taken place in-person were conducted remotely through telemedicine. This resulted in a dramatic decline in in-person outpatient visits early in the pandemic, with a corresponding surge in telemedicine visits.1–4 The use and uptake of telemedicine for particular specialties has been studied.5–8 However, only a few recent studies have focused on telemedicine adoption across all outpatient specializations and conditions.1,9–12 Even fewer studies have examined variation in telemedicine use within state Medicaid programs. These programs collectively comprise the largest public insurance program in the United States and insure diverse groups of patients, for whom the demand for care and ability to substitute to telemedicine visits varies widely, underscoring the importance of characterizing changes within Medicaid. Prior research on the uptake of telemedicine among low-income Medicaid populations has been limited and is often focused on mental health.13,14
Importantly, lower telemedicine utilization rates by Medicaid enrollees may widen existing disparities in care. Medicaid patients have generally had lower access to health care providers as compared with other insured patients,15 largely due to lower Medicaid reimbursement rates for medical services.15–17 Urban-rural disparities can exist even within Medicaid programs: one study found that asthmatic children enrolled in Medicaid filled fewer prescriptions for their medications if they lived in rural areas,18 while another found that median per-child expenditure in Colorado’s Medicaid program was $99 more in urban areas relative to rural areas.19
Early evidence from the COVID-19 pandemic documents that telemedicine adoption rates differed across populations. Data from Medicaid and the Children’s Health Insurance Program (CHIP) show that rates of services delivered through telemedicine were highest among beneficiaries between the ages of 19 and 64 across nearly all 50 states.20 Other evidence suggests that poor familiarity with technology—even for households with an Internet connection—drives low take-up of telemedicine among the elderly.21 However, there is little research on differential uptake of telemedicine services by location or mode of delivery, though there are concerns that telemedicine has the potential to exacerbate disparities in health care if a lack of broadband access (ie, the “digital divide”) makes it difficult for those in rural areas to access telemedicine services.22,23
This study uses administrative data comprising the universe of Medicaid claims for the State of Florida over the period January 2019 - July 2020 to examine variation over time in claims for different services before and after the expanded reimbursement and utilization of telemedicine during the COVID-19 pandemic. We investigate how the substitution towards telemedicine visits (overall and by mode of visit) varied across subgroups of Medicaid beneficiaries, including age, health status, prior health care use, and geography.
METHODS
Data
We use administrative data from Florida’s Medicaid program between January 2019 and July 2020. July 2020 is the most recent month of claims data that was provided by Florida’s Agency for Health Care Administration. The data include medical claims and enrollment information for the universe of Florida’s Medicaid enrollees. The claims data are granular, containing information on patient diagnoses, location of service, each procedure or drug that was billed, along with the billing physician and amount billed. Claims for dual-eligible Medicare-Medicaid enrollees are sent to Medicaid directly from Medicare and are included in our dataset even if health plan adjudication determines that there is no Medicaid liability. We define a “claim” as a unique internal control number which is a unique 13-digit number assigned to each claim. The enrollee data include all enrollees in the Medicaid system regardless of whether they submit a claim during the analysis period. The enrollee data include information on the enrollee’s county of residence, age range, and months of Medicaid enrollment.
Approach
Study Cohort
We analyze the universe of claims made by Florida Medicaid beneficiaries in 2019 and 2020. We restrict our sample to Medicaid recipients that were continuously enrolled in Medicaid between January 2019 and July 2020 to allow for the identification of patients with chronic conditions. Our sample construction is summarized in Supplemental Digital Content Figure A1 (http://links.lww.com/MLR/C454). From an original sample of 4.4 million enrollees, we are left with 2.4 million after imposing our sample restrictions with the majority (1.5 million) of the sample decrease due to dropping individuals that were not enrolled in Medicaid for all 19 months of the sample period. Nearly 90% of Medicaid beneficiaries in Florida are enrolled in Medicaid Managed Care programs.24 Approximately 0.5 million Medicaid beneficiaries who were not enrolled in Medicaid Managed Care were excluded from our analysis, as Medicaid only covers select services for many of these beneficiaries (see Appendix Section A1 for details, http://links.lww.com/MLR/C456). Florida did not expand Medicaid eligibility under the Affordable Care Act. To qualify for Medicaid in this time period, enrollees must be young (21 and under), elderly (65 and over), pregnant, blind, have a disability or a family member with a disability or be responsible for a child 18 years or younger, as well as a resident of the state of Florida, a United States national, citizen, permanent resident, or legal alien. Income eligibility standards depend on the reason for qualification but range from 27% of the federal poverty line for adults with dependent children to 206% of the federal poverty line for children under 1 year of age. Nondisabled, nonelderly adults without children are ineligible for Medicaid regardless of income.
Identifying Telemedicine Visits
Though telemedicine was utilized before the COVID-19 pandemic, reimbursement was limited to Community Behavioral Health settings,25 and therefore, prepandemic telemedicine claims were small. Because telemedicine billing was rapidly rolled out and adopted by a broader set of providers during the COVID-19 pandemic, we use a variety of approaches to identify telemedicine visits. Specifically, we define a visit as telemedicine if its place of service code, procedure code, or procedure modifier code indicate that care was provided via telemedicine. We further break this down into codes which identify audio-visual services versus those that identify audio-only services. Supplemental Digital Content Section A2 (http://links.lww.com/MLR/C456) provides the list of codes used to identify telemedicine claims, including audio-visual, audio-only, and unclassified visits. For our analysis regarding the method of telemedicine service delivery, we exclude ∼20% of visits which we are unable to classify as audio or audio-visual. A large portion of unclassified visits are for psychiatry and speech, occupational, and physical therapy; thus, we also exclude visits for these specialties from this analysis. Alternative versions of the analysis including unclassified visits, are shown in the Online Supplemental Digital Content (http://links.lww.com/MLR/C456).
We validate our methodology in 2 ways. First, as we show in Supplemental Digital Content Figure A2 (http://links.lww.com/MLR/C455), telemedicine visits (the gap between in-person and total visits) sharply increase starting in March 2020, suggesting that we are appropriately capturing telemedicine visits. Second, Supplemental Digital Content Figure A2 (http://links.lww.com/MLR/C455) shows that telemedicine visits are clustered almost entirely in the outpatient setting. These patterns agree with the expected time when access to telemedicine is expanded as well as the settings where telemedicine is used.
Identifying Enrollee Subgroups
We construct a sample of Medicaid enrollees with chronic conditions, including diabetes, psychiatric conditions (depression and anxiety), heart disease, addiction disorders, and respiratory conditions (asthma, chronic obstructive pulmonary disorder, chronic bronchitis, emphysema, bronchiectasis). We use a 1-year lookback period to determine whether individuals have each condition. If an individual had a diagnosis code for any of these conditions in 2019, we treat them as having that condition for the full sample period. Supplemental Digital Content Section A2 (http://links.lww.com/MLR/C456) includes the International Classification of Diseases, 10th Revision (ICD-10) diagnosis codes used to define each condition. We identify heavy users of health care services, or “super-utilizers” as any individual that has 12 or more emergency department visits in 2019, following the definition employed by Florida’s Agency for Health Care Administration.26
We use enrollee county of residence to determine whether the enrollee lives in a Health Professional Shortage Area (HPSA) or a rural or urban county. Counties are defined as urban or rural using the US Department of Agriculture’s Economic Research Service 2013 Rural-Urban Continuum codes.27 Counties are considered an HPSA if they are identified as a primary care geographic HPSA by the US Health Resources and Services Administration.28
Outcome Measures
Our primary variables of interest are: (1) a dichotomous variable indicating whether an enrollee utilizes any medical care or telemedicine services during our time period of interest; (2) the number of outpatient visits made by enrollees; and (3) the mode of outpatient visits—telemedicine or in-person. We also separate telemedicine visits into audio-only and audio-visual.
Measures
We first calculate the percentage of Medicaid enrollees with any telemedicine utilization in our time frame. We do this calculation separately for all Medicaid enrollees for the subset of Medicaid enrollees who have any medical claims in the March–July 2020 time frame (we refer to this group as “claimants”). We define the group of claimants separately from all enrollees to account for the fact that many enrollees did not access any health services during the early months of the pandemic. We stratify telemedicine utilization rates by patient age group (0–18, 19–64, and 65+), sex, super-utilizer status, chronic medical conditions, geographic location (urban/rural), and whether an enrollee’s county of residence is an HPSA. We measure whether differences in telemedicine utilization between different subgroups of patients are statistically different using χ2 tests of independence.
Next, we calculate the total number of outpatient visits on a monthly basis. For expository purposes, we index these values to the average monthly visits in 2019 separately for all visits (telemedicine and in-person) and for in-person visits only. We calculate this for all enrollees and separately for the subset of enrollees with chronic medical conditions and super-utilizers. While the COVID-19 pandemic led to a steep initial decrease in outpatient visits, we find that much of the decrease was mitigated by the use of telemedicine services.
Last, we subset telemedicine visits into audio-only and audio-visual visits. Excluding claims that cannot be classified as audio-only or audio-visual, we calculate the percentage of telemedicine visits that were audio-only or audio-visual for all enrollees, and separately by age group and by urban/rural and HPSA status.
RESULTS
Telemedicine Utilization
Supplemental Digital Content Figure A2 (http://links.lww.com/MLR/C455) graphs telemedicine usage over time, documenting a dramatic decrease in in-person visits and a corresponding increase in telemedicine visits beginning in March 2020. Outpatient and emergency department utilization (as well as some inpatient utilization) declined dramatically between March and April and then started to bounce back in May through July. We restrict our analysis to outpatient visits, but Supplemental Digital Content Figure A2 (http://links.lww.com/MLR/C455) shows that other claim types (emergency department visits, inpatient stays, and the pharmacy fills) also dropped dramatically at the start of the pandemic, though telemedicine was not (or could not be) adopted in those areas.
Table 1 shows the utilization of telemedicine services between March and July of 2020. Only 13.52% of all enrollees, or 23.37% of claimants, utilized any telemedicine services. Consistent with past studies, nonelderly adults were most likely to utilize telemedicine (20.06% of all enrollees or 35.26% of claimants). While only 6.01% of all elderly enrollees utilized telemedicine during this time frame, 22.69% of elderly claimants utilized telemedicine—suggesting that the elderly were significantly more likely to forego medical care during this time frame. Sex differences in telemedicine utilization were minor.
TABLE 1.
Summary Statistics of Telemedicine Usage
| Characteristics | Use Telemedicine | No Telemedicine (Nonclaimants) | No Telemedicine (Claimants) | % Telemedicine (Enrollees) | % Telemedicine (Claimants) |
|---|---|---|---|---|---|
| N | 320,648 | 1,056,827 | 994,884 | 13.52 | 24.37 |
| Age (y) | |||||
| 0–18 | 191,047 | 526,454 | 717,563 | 13.31 | 21.03 |
| 19–64 | 104,571 | 224,576 | 192,018 | 20.06 | 35.26 |
| 65+ | 25,030 | 305,797 | 85,303 | 6.01 | 22.69 |
| Sex | |||||
| Male | 141,639 | 489,109 | 445,190 | 13.16 | 24.14 |
| Female | 179,009 | 567,718 | 549,694 | 13.81 | 24.57 |
| Super-utilizers | 24,997 | 7729 | 35,010 | 36.90 | 41.66 |
| Non–super-utilizers | 295,651 | 1,049,098 | 959,874 | 12.83 | 23.55 |
| Patient subgroups | |||||
| Heart disease | 39,051 | 10,589 | 57,491 | 36.45 | 40.45 |
| Diabetes | 36,993 | 9491 | 55,120 | 36.41 | 40.16 |
| Behavioral health (depression/anxiety) | 81,559 | 20,731 | 86,248 | 43.26 | 48.60 |
| Addiction treatment | 35,498 | 17,426 | 53,554 | 33.34 | 39.86 |
| Respiratory diseases | 70,591 | 38,452 | 142,389 | 28.08 | 33.14 |
| Location | |||||
| Rural counties | 11,777 | 40,700 | 49,352 | 11.57 | 19.27 |
| Urban counties | 308,871 | 1,016,127 | 945,532 | 13.60 | 24.62 |
| HPSA counties | 5460 | 20,204 | 25,372 | 10.70 | 17.71 |
| Non-HPSA counties | 315,188 | 1,036,623 | 969,512 | 13.58 | 24.53 |
Patients are inferred to have a chronic condition if they were diagnosed or treated for the condition in 2019.
“HPSA” stands for “Health Professional Shortage Area.”27 Super-utilizers are defined as patients that make 12 or more emergency department visits in a year.25 Percentages in the final 2 columns are calculated as follows: Column 4 is column 1 divided by the sum of columns 1-3 expressed as a percentage, and column 5 is column 1 divided by column 1+column 3, expressed as a percentage. The χ2 tests were conducted to test for statistically significant differences in telehealth utilization between groups of enrollees. As each of these tests were statistically significant at the <0.01 level, we do not note significance in the table.
Source: Authors’ own calculations using Florida’s Medicaid Managed Care administrative records, January 2019–July 2020.
Super-utilizers and enrollees with chronic conditions were significantly more likely than the average patient to utilize telemedicine services. Among super-utilizers, 36.90% of enrollees, or 41.66% of claimants, accessed telemedicine services as compared with 12.83% of enrollees, or 23.55% of claimants, among non–super-utilizers. Rates of telemedicine utilization for patients with chronic conditions were similarly high, with particularly high utilization among patients with psychiatric conditions, where 43.26% of all enrollees, or 48.60% of claimants, accessed telemedicine services.
Telemedicine utilization rates were moderately different by location. Enrollees living in urban counties were somewhat more likely to access telemedicine services as compared with those living in rural counties (13.60% vs. 11.57% of all enrollees and 24.62% vs. 19.27% of claimants in urban and rural counties, respectively). Enrollees living in HPSA counties were less likely than those living in non-HPSA counties to utilize telemedicine (10.70% vs. 13.58% of all enrollees and 17.71% vs. 24.53% of claimants in HPSA and non-HPSA counties, respectively).
Telemedicine Usage by Chronic Condition
Figure 1 graphs the number of total outpatient visits by month in 2020 relative to the average monthly visits for 2019 (indexed to 100) and shows markedly different relative declines in usage. In-person outpatient visits fell by 61% between February and April 2020, though telemedicine offset much of the decline in in-person visits, with total visits falling by a lower, but still substantial, 38% during the same time period. Though large, this decline is in line with prior estimates using other data sources of the overall decline in in-person outpatient visits during the COVID-19 pandemic.4,9,29 While there were dramatic declines in overall Medicaid visits, these patterns were more muted for patients with chronic conditions. For these patients, visits almost recovered to their prepandemic levels in June 2020, with telemedicine services helping to offset much of the decline in in-person visits, particularly for patients with psychiatric conditions.
FIGURE 1.
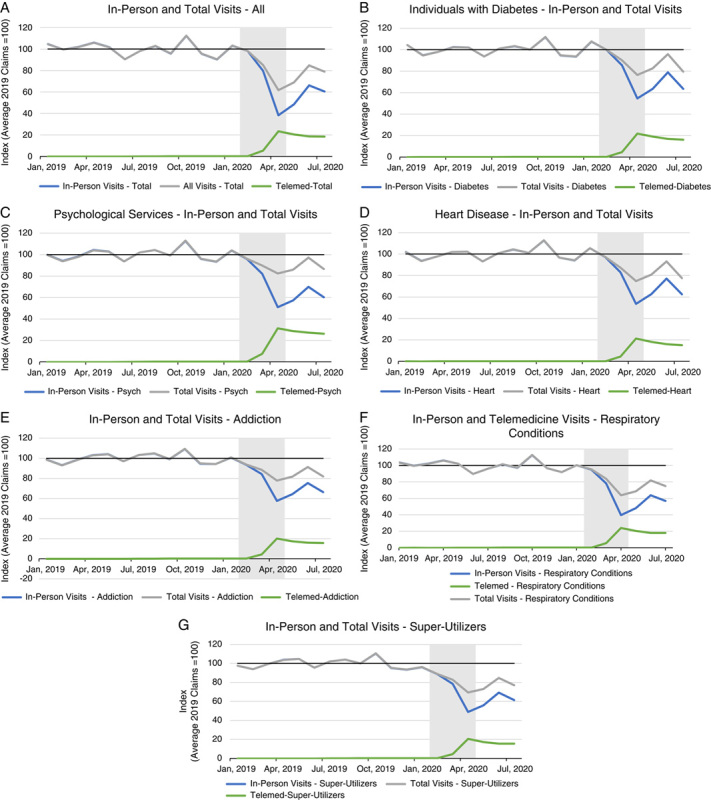
Deviations of visits, in-person and total, from 2019 average. Graph shows the indexed number of visits made by patients with chronic conditions (A–F) or super-utilizers (G) relative to the average for the year 2019, equal to 100 on the y-axis. Patients are inferred to have a chronic condition if they were diagnosed or treated for the condition in 2019. Super-utilizers are defined as patients that make 12 or more emergency department visits in a year. “Psychological Services” comprise consultations for depression and anxiety only. “Respiratory conditions” include asthma, chronic obstructive pulmonary disorder, chronic bronchitis, emphysema and bronchiectasis. Shaded regions correspond to periods in which the United States was in a recession as dated by the National Bureau of Economic Research. Source: Authors’ own calculations using Florida’s Medicaid Managed Care administrative records, January 2019–July 2020.
Audio-only Telehealth Services by Age and Location
Figure 2 shows a strong age gradient in the take-up of audio-only telemedicine. Most telemedicine visits include both audio and video. For elderly Medicaid beneficiaries, audio-only visits make up a larger share of telemedicine visits than among younger Medicaid enrollees (21% vs. 14% of telemedicine visits in July 2020 for elderly and nonelderly adult enrollees, respectively). Audio-only telemedicine visits were uncommon for children, making up only 5% of telemedicine visits in July 2020.
FIGURE 2.
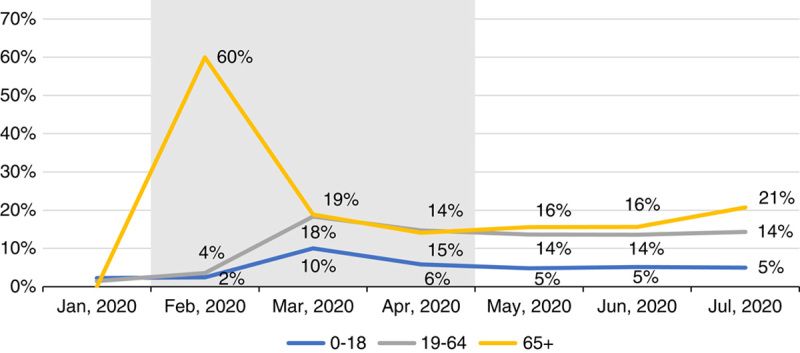
Share of audio-only telemedicine visits by age group. Graph shows the percentage of audio-only telemedicine visits split by age group made by patients enrolled in Florida’s Medicaid program between January and July 2020, excluding claims for psychological services, occupational therapy, speech therapy, and physical therapy. Shaded regions correspond to periods in which the United States was in a recession as dated by the National Bureau of Economic Research. Source: Authors’ own calculations using Florida’s Medicaid Managed Care administrative records, January 2020–July 2020.
The top panel of Figure 3 displays audio-only telemedicine usage for enrollees in rural and urban counties, while the bottom panel displays audio-only telemedicine usage for enrollees in HPSA and non-HPSA counties. Across urban-rural settings, there is little difference in take-up of video versus audio-only telemedicine. At the beginning of the pandemic, audio-only telemedicine visits were more common in non-HPSA counties (13% vs. 6% of telemedicine visits in March 2020 for non-HPSA and HPSA counties, respectively), however, there was little difference in audio-only telemedicine utilization rates by July 2020.
FIGURE 3.
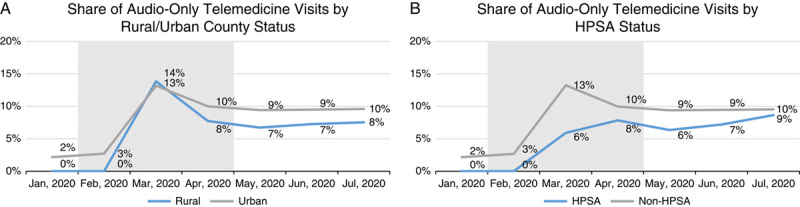
Share of audio-only telemedicine visits by geographical indicator. Graph shows the percentage of audio-only telemedicine visits split by urban-rural status and HPSA (Health Professional Shortage Area) status made by patients enrolled in Florida’s Medicaid program between January and July 2020, excluding claims excluding claims for psychological services, occupational therapy, speech therapy, and physical therapy. A, Differences in the share of audio-only telemedicine visits out of known claims between urban and rural counties. B, Differences in the share of audio-only telemedicine visits out of known claims between HPSA and non-HPSA counties. Shaded regions correspond to periods in which the United States was in a recession as dated by the National Bureau of Economic Research. Source: Authors’ own calculations using Florida’s Medicaid Managed Care administrative records for January 2020–July 2020.
DISCUSSION
Our findings shed new light on the differential value of telemedicine depending on both the method of delivery and the subgroup of Medicaid enrollees. While there is an overall decline in outpatient visits during the beginning of the COVID-19 pandemic, vulnerable subgroups with chronic conditions and super-utilizers appear to be more likely than the average Medicaid enrollee to utilize telemedicine; they were, therefore, less likely to defer contact with the health care system even in the absence of in-person consultations. Patients receiving psychiatric outpatient care were highly likely to use telemedicine. This suggests that access to telemedicine may be particularly beneficial for this high-needs group of patients, who regularly interact with the health care system. At least one large psychiatric care hospital system has found it is possible to provide almost all of their services via telemedicine.6 However, it is still unknown whether the quality of care or patient outcomes were impacted by the switch from in-person to telemedicine visits.
Medicaid enrollees living in rural and HPSA counties face a particularly stark lack of access to local health care providers18,19,30,31 and might benefit from telemedicine services through the ability to more easily access providers. Despite this, Medicaid enrollees living in these counties were slightly less likely to utilize telemedicine services. One potential explanation for this is the digital divide: access to broadband internet is less common in rural areas. Other studies have found that households outside of metropolitan areas are nearly twice as likely to have neither a personal computer nor a smartphone than households that reside within a metropolitan area.23 However, in our results, audio-only telemedicine consultations accounted for a similar proportion of visits in rural and HPSA counties to urban and non-HPSA counties in Florida, suggesting additional barriers to telemedicine access than mere lack of access to a device with an Internet connection. This is in line with results from at least one prior study,32 which found that nearly two-thirds of those who are offered audio-only telemedicine consultations have access to either a smartphone or a computer with Internet access.
Our findings highlight the importance of audio-only telemedicine, particularly for the elderly. For appropriate services, potentially lower cost phone consultations can expand access to low-income populations. This may involve less infrastructure investment than video-based telemedicine, which is also more difficult to access for older Medicaid beneficiaries,32 though other underserved populations may benefit as well.33–38 While we do not examine its effects on outcomes, a recent study found that pregnant women consuming audio-only prenatal care during 2020 had similar outcomes to pregnant women consuming in-person prenatal care in 2019.39 Creating best practices for audio-only telemedicine consultations could improve the quality of care for elderly patients who may struggle with the technology required for an audio-visual telemedicine appointment.
Policy Implications
We find that telemedicine can be an effective method of maintaining access to outpatient services for Medicaid enrollees, especially for enrollees with chronic conditions or high utilization of health care services. We posit that improved infrastructure and continued reimbursement for telemedicine consultations can expand access for Medicaid recipients beyond the COVID-19 pandemic. Our findings can be reconciled with previous studies that recommended against the use of telemedicine due to the extent of the digital divide5 because we use a broader definition of telemedicine that includes audio-only consultations which do not require broadband access. One size does not fit all; older enrollees are more likely to benefit from phone-based delivery of telemedicine, and more intensive users of health care are more likely to take-up telemedicine services more generally. Before the COVID-19 pandemic, telemedicine services were used for Medicare beneficiaries in rural areas.12 We find that there is significant uptake of telemedicine among Florida’s Medicaid beneficiaries in urban areas as well as rural areas, suggesting scope for benefits regardless of location. Further research is needed to determine the extent to which the persistent use of telemedicine expanded overall access or represents a substitution away from in-person visits.
Limitations
We acknowledge several limitations of our analysis. First, our analysis of telemedicine is solely descriptive and cannot speak to the causal impact of telemedicine on health outcomes. Second, we cannot distinguish temporary changes in outpatient visits from permanent changes that last beyond the pandemic, given that the research has been conducted before the end of the COVID-19 pandemic. This is particularly important for elderly and chronically ill patients, who are at higher risk for severe cases of COVID-19 and might otherwise have different utilization of telemedicine services. Third, we limit our analysis to the subset of beneficiaries who are continuously enrolled in Medicaid between January 2019 and July 2020, thus, we do not analyze subgroups with short-term Medicaid enrollment, including women who qualify for Medicaid solely due to pregnancy. Fourth, our data is limited to Medicaid enrollees in the state of Florida and we are unable to assess broader regional trends or compare Medicaid enrollees to patients with other forms of insurance. While our study is limited to Florida, Florida has some of the most restrictive Medicaid eligibility requirements, so we view our estimates as a lower bound on the potential adoption of telemedicine because other states are more likely to allow higher income applicants to enroll in Medicaid. There is limited research that explicitly compares telemedicine adoption among Medicaid enrollees relative to non-Medicaid populations, though at least one study finds between 1.5 and 2 times as much adoption among higher income households relative to lower income households.22 Fifth, since we do not have data beyond the end of July of 2020, we are unable to make statements regarding the trajectory of telemedicine usage between that month and the time of writing. Sixth, while our analysis will capture the majority of claims for dual-eligible enrollees, we may miss a small percentage of claims that were not sent to Medicaid for adjudication.
CONCLUSIONS
Telemedicine use in a low-income population appeared to buffer an overall decline in the use of outpatient services during the novel coronavirus pandemic. Patients with higher health care needs—such as super-utilizers or those with chronic conditions—were significantly more likely to access telemedicine services, while enrollees living in rural areas and HPSAs were moderately less likely to access these services. We find that the digital divide previously noted in the literature5,8 can be mitigated by audio-only telemedicine services, which the elderly use at higher rates than younger enrollees.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
ACKNOWLEDGMENTS
The authors thank Julia Platt for outstanding research assistance and technical and computing support from the University of Miami’s Institute for Data Science and Computing.
Footnotes
The authors declare no conflict of interest.
Contributor Information
Mallick Hossain, Email: emallickhossain@gmail.com.
Emma B. Dean, Email: exb736@miami.edu.
Daniel Kaliski, Email: d.kaliski@bbk.ac.uk.
REFERENCES
- 1. Patel SY, Mehrotra A, Huskamp HA, et al. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States: study examines variation in total US outpatient visits and telemedicine use across patient demographics, specialties, and conditions during the COVID-19 pandemic. Health Aff. 2021;40:349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cortez C, Mansour O, Qato DM, et al. Changes in short-term, long-term, and preventive care delivery in US office-based and telemedicine visits during the COVID-19 pandemic. JAMA Health Forum. 2021;2:e211529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;180:1386–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174:129–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for medicare. Health Aff. 2014;33:244–250. [DOI] [PubMed] [Google Scholar]
- 6. Kalin ML, Garlow SJ, Thertus K, et al. Rapid implementation of telehealth in hospital psychiatry in response to COVID-19. Am J Psychiatry. 2020;177:636–637. [DOI] [PubMed] [Google Scholar]
- 7. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178:745–746. [DOI] [PubMed] [Google Scholar]
- 8. Barbosa W, Zhou K, Waddell E, et al. Improving access to care: telemedicine across medical domains. Annu Rev Public Health. 2021;42:463–481. [DOI] [PubMed] [Google Scholar]
- 9. Patel SY, Mehrotra A, Huskamp HA, et al. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181:388–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zeltzer D, Einav L, Rashba J, et al. The Impact of Increased Access to Telemedicine. Cambridge, MA: National Bureau of Economic Research; 2021. [Google Scholar]
- 12. Mehrotra A, Jena AB, Busch AB, et al. Utilization of telemedicine among rural Medicare beneficiaries. JAMA. 2016;315:2015–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Uscher-Pines L, Bouskill KE, Sousa J, et al. Experiences of Medicaid programs and health centers in implementing telehealth. Rand Health Q. 2020;8:RR-2564-ASPE. [PMC free article] [PubMed] [Google Scholar]
- 14. Douglas MD, Xu J, Heggs A, et al. Assessing telemedicine utilization by using Medicaid claims data. Psychiatr Serv. 2017;68:173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff. 2012;31:1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berman S, Dolins J, Tang S-f, et al. Factors that influence the willingness of private primary care pediatricians to accept more Medicaid patients. Pediatrics. 2002;110:239–248. [DOI] [PubMed] [Google Scholar]
- 17. Zuckerman S, McFeeters J, Cunningham P, et al. Changes in Medicaid physician fees, 1998–2003: implications for physician participation: despite recent gains, the relative attractiveness of Medicaid patients has not improved much over the longer term. Health Aff. 2004;23(suppl 1):W4-374. [DOI] [PubMed] [Google Scholar]
- 18. Valet RS, Gebretsadik T, Carroll KN, et al. High asthma prevalence and increased morbidity among rural children in a Medicaid cohort. Ann Allergy Asthma Immunol. 2011;106:467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McManus BM, Lindrooth R, Richardson Z, et al. Urban/rural differences in therapy service use among Medicaid children aged 0–3 With developmental conditions in Colorado. Acad Pediatr. 2016;16:358–365. [DOI] [PubMed] [Google Scholar]
- 20. Chu RC Peters C De Lew N, et al. State Medicaid telehealth policies before and during the COVID-19 public health emergency. 2021. Available at: https://aspe.hhs.gov/reports/state-medicaid-telehealth-policies.
- 21. Cubanski J. Possibilities and Limits of Telehealth for Older Adults During the COVID-19 Emergency. San Francisco, CA: Henry J. Kaiser Family Foundation; 2020. [Google Scholar]
- 22. Poeran J, Cho LD, Wilson L, et al. Pre-existing disparities and potential implications for the rapid expansion of telemedicine in response to the coronavirus disease 2019 pandemic. Med Care. 2021;59:694–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Curtis ME, Clingan SE, Guo H, et al. Disparities in digital access among American rural and urban households and implications for telemedicine‐based services. J Rural Health. 2021. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kaiser Family Foundation. Share of Medicaid population covered under different delivery systems; 2021. Available at: www.kff.org/medicaid/state-indicator/share-of-medicaid-population-covered-under-different-delivery-systems/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D . Accessed February 1, 2022.
- 25. Center for Connected Health Policy. State Telehealth Laws and Medicaid Program Policies; 2019. Available at: https://cdn.cchpca.org/files/2019-05/cchp_report_MASTER_spring_2019_FINAL.pdf . Accessed February 25, 2022.
- 26. Florida Agency for Health Care Administration. Comprehensive quality strategy; 2020. Available at: https://ahca.myflorida.com/medicaid/policy_and_quality/quality/docs/Comprehensive_Quality_Strategy_Report.pdf . Accessed July 1, 2021.
- 27. Economic Research Service of the US Department of Agriculture. Rural-urban continuum codes; 2013. Available at: www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx . Accessed July 1, 2021.
- 28. US Health Resources and Services Administration. Health Professional Shortage Area (HPSA) Find; 2021. Available at: https://data.hrsa.gov/tools/shortage-area/hpsa-find . Accessed July 1, 2021.
- 29. Chatterji P, Li Y. Effects of the COVID-19 pandemic on outpatient providers in the United States. Med Care. 2021;59:58–61. [DOI] [PubMed] [Google Scholar]
- 30. Martino SC, Mathews M, Agniel D, et al. National racial/ethnic and geographic disparities in experiences with health care among adult Medicaid beneficiaries. Health Serv Res. 2019;54:287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Davis MM, Renfro S, Pham R, et al. Geographic and population-level disparities in colorectal cancer testing: a multilevel analysis of Medicaid and commercial claims data. Prev Med. 2017;101:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Benjenk I, Franzini L, Roby D, et al. Disparities in audio-only telemedicine use among medicare beneficiaries during the coronavirus disease 2019 pandemic. Med Care. 2021;59:1014–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Drake C, Lian T, Cameron B, et al. Understanding telemedicine’s “new normal”: variations in telemedicine use by specialty line and patient demographics. Telemed J E Health. 2022;28:51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gilson SF, Umscheid CA, Laiteerapong N, et al. Growth of ambulatory virtual visits and differential use by patient sociodemographics at one urban academic medical center during the COVID-19 pandemic: retrospective analysis. JMIR Med Inform. 2020;8:e24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hsiao V, Chandereng T, Lankton RL, et al. Disparities in telemedicine access: a cross-sectional study of a newly established infrastructure during the COVID-19 pandemic. Appl Clin Inform. 2021;12:445–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020:1357633X20963893. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schifeling CH, Shanbhag P, Johnson A, et al. Disparities in video and telephone visits among older adults during the COVID-19 pandemic: cross-sectional analysis. JMIR Aging. 2020;3:e23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Duryea EL, Adhikari EH, Ambia A, et al. Comparison between in-person and audio-only virtual prenatal visits and perinatal outcomes. JAMA Netw Open. 2021;4:e215854. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


