Introduction
Puncture of the cisterna magna has recently been proposed as a promising new avenue for intrathecal gene therapy, as intracisternally injected viral vectors transduce cells of the CNS of non-human primates far more efficiently than vectors administered by the lumbar route (Hinderer et al., 2014). To facilitate the translation of intrathecal gene therapy from bench to bedside, several authors have stressed the need for the development of a safe means of performing cisterna magna puncture in human patients (Hinderer et al., 2014).
Cisterna magna puncture—also referred to as cistern, cisternal of suboccipital puncture—was introduced into clinical practice by American neurologist James Bourne Ayer (1882–1963) in 1920 (Ayer, 1920). Whereas the procedure held promising therapeutic and diagnostic applications, the notion of inserting a needle in proximity to the vital centres of the medulla oblongata was met with considerable apprehension. From the start, then, attitudes towards cistern puncture were based on individual trade-offs between the potential risks and benefits associated with the procedure: some authors were convinced of the safety and efficacy of cistern puncture and advocated its routine use in favour of lumbar puncture, while others only resorted to the procedure when other means of CSF access were inadequate. As experience with cistern puncture accumulated and new diagnostic and therapeutic entities were developed, indications gradually declined until the procedure was largely abandoned by the last quarter of the 20th century.
In this article, we commemorate the centenary of cisterna magna puncture, a clinical procedure that, despite evident dangers, had a significant impact on the treatment and diagnosis of various neurological disorders and continues to inspire novel applications.
The advent of cisterna magna puncture
Puncture of the cisterna magna had been used in animal studies for several years prior to its clinical introduction. In laboratory animals, narrow intervertebral spaces often made it difficult to reach the spinal canal via lumbar puncture, prompting the search for alternative routes of CSF access. In 1913, British scientists Walter Dixon (1871–1931) and William Halliburton (1860–1931) first described the technique of cistern puncture in animals, which proved to be more practical than lumbar puncture on account of the absence of bony coverage between the atlas and the occiput. The technique was adopted by American neuropathologist Lewis Weed (1886–1952), who headed the Army Neurosurgical Laboratory at Johns Hopkins. Weed’s extensive use of cistern puncture for the study of CSF dynamics in animals inspired James Ayer, a talented young Boston neurologist who had come to the Army Neurosurgical Laboratory during World War I, to develop a similar method in humans (Wegeforth et al., 1919).
Together with colleagues Paul Wegeforth (1887–1923) and Charles Essick (1883–1954), Ayer set out to practice the use of cistern puncture on human cadavers (Wegeforth et al., 1919). The needle was inserted in the midline at the back of the neck just above the spine of the axis and carefully advanced in a plane with the external auditory meatus and the glabella. At an average depth of 4–5 cm, the occipito-atlantoid ligament and, subsequently, the dura were pierced, characterized by a sudden loss of resistance as the needle entered the cisterna magna. Upon removal of the brain, the authors found that the needle never projected far enough into the cisterna magna ‘to cause any great anxiety that the medulla would be injured’ (Wegeforth et al., 1919). Feeling confident about the safety and potential merits of cistern puncture, the authors felt that the procedure was ready to be performed on living patients.
In 1920, Ayer reported the results of his first 20 patients undergoing cistern puncture, thereby effectively introducing the technique to the medical community (Ayer, 1920). According to Ayer, the procedure—done with the patient lying on either side—had not only been easy to perform and unaccompanied by adverse events, but had also revealed many promising therapeutic and diagnostic applications (Ayer, 1920).
Therapeutic applications
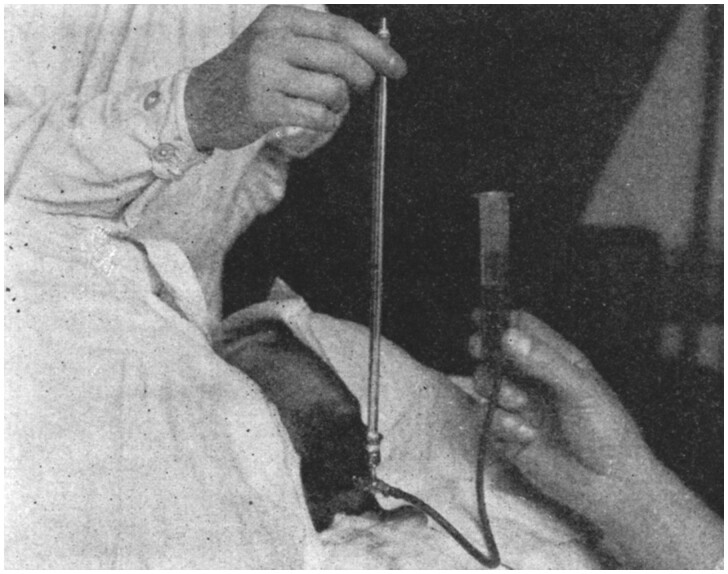
Cistern puncture was rapidly taken up for therapeutic purposes, particularly in the treatment of neurosyphilis and meningococcal meningitis. In neurosyphilis, patients with general paresis had a poor prognosis, despite recent advances brought about by the introduction of arsphenamine (salvarsan) and malarial fever therapy. By the early 1920s, treatment typically consisted of a combined regimen of malaria inoculation, mercury, salvarsan and salvarsanized serum, the latter being directly injected into the CSF by ventricular or lumbar puncture (Purves-Stewart, 1924). Compared to these procedures, the administration of salvarsanized serum via cistern puncture offered a clear advantage, as the serum could be delivered in high concentrations near the brain without requiring invasive intraventricular injections (Fig. 1).
Figure 1.
Method of administering serum by cistern puncture. From Ayer (1920).
The use of cistern puncture in meningococcal meningitis was based on a similar rationale. At the time, the intrathecal administration of anti-meningococcal serum constituted the main therapy. Based on experimental meningitis studies, meningococcal meningitis was believed to begin primarily as an infection of the cerebral meninges, only spreading to the spinal meninges as the disease progressed, making intracistern serum injections appear more logical than serum administration by the lumbar route. Moreover, lumbar puncture was not always feasible in patients with meningitis, as meningeal adhesions occasionally blocked the spinal canal, resulting in a so-called ‘dry tap’ and preventing serum from reaching the upper CNS. By alternating lumbar and cistern puncture, it was thought that the formation of such adhesions could be prevented. Combined cistern and lumbar punctures were also used to flush the spinal canal with Ringer’s solution (either with or without anti-meningococcal serum) in cases of purulent meningitis.
Early adopters of cistern puncture for serum therapy, Ayer included, did not just highlight the potential benefits of injecting serum near the brain, but also conceptualized the cisterna magna as ‘the distributing center of the cerebrospinal fluid system’ (Ayer, 1920). Strategically positioned between the brain and spinal cord, the cisterna magna was seen as capable of directing CSF to both the cerebral and spinal subarachnoid space, effectively disseminating therapeutic substances throughout the CNS. Indeed, experiments with intrathecal ink by Ayer and his colleagues had shown that ink injected via lumbar puncture resulted in little staining beyond the base of the brain, whereas intracistern ink injections stained the entire CNS, including cerebral convexities (Wegeforth et al., 1919). In this line of thought, the use of cistern puncture in the treatment of neurosyphilis and meningococcal meningitis seemed of such obvious advantage that it far outweighed the potential dangers associated with the procedure. In addition to these indications, cistern puncture was also adopted in the treatment of other disorders, most notably for therapeutic CSF withdrawal in intracranial haemorrhage in infants.
Diagnostic applications
Besides its therapeutic applications, cistern puncture proved to be a valuable aid in the diagnosis and localization of obstructive spinal cord lesions. In the first two decades of the 20th century, the diagnosis of spinal cord lesions often provided a clinical challenge. Based on neurological examination, it was often impossible to differentiate between obstructive spinal cord lesions amenable to surgery and inoperable degenerative pathology, frequently resulting in negative explorative laminectomies. Whereas a yellowish colour, increased protein levels and marked coagulation of CSF obtained via lumbar puncture (Froin syndrome) suggested the presence of an obstructive spinal cord lesion, such changes were only found at a late stage, when the spinal cord had already been permanently damaged.
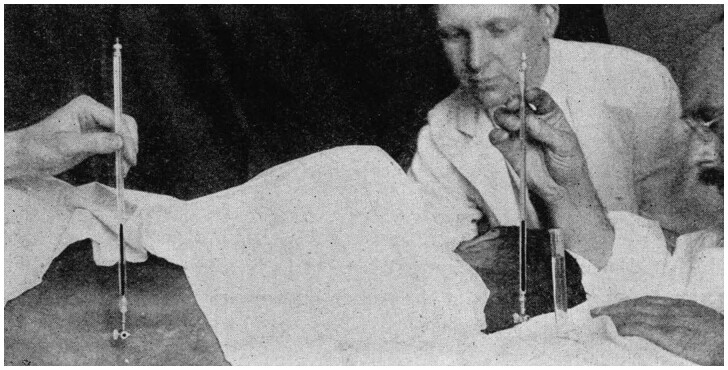
By combining cistern and lumbar puncture—with the patient lying on either side—CSF composition and pressure dynamics could be compared between the two puncture sites (Fig. 2) (Ayer, 1920). In contrast to the absolute increase in CSF protein in Froin’s syndrome, combined cistern-lumbar puncture revealed a more subtle, relative increase in CSF protein below the point of obstruction. In addition, relative differences in CSF pressure dynamics could be detected. When the spinal canal was patent, CSF pressure responses would be similar for both puncture sites. In case of obstruction, however, physiological pressure oscillations were diminished below the point of obstruction, as were the effects of jugular compression and cisternal CSF withdrawal (Ayer, 1920). By providing both chemical and mechanical evidence of obstruction, combined cistern-lumbar puncture proved a valuable aid in the diagnosis of spinal cord compression, and was rapidly adopted into clinical practice.
Figure 2.
Method of combined cistern-lumbar puncture with manometers for pressure reading. From Ayer (1920).
Cistern puncture was not just valuable in the diagnosis, but also in the precise localization of spinal cord lesions. In 1921, French physicians Jean-Athanase Sicard (1872–1929) and Jacques Forestier (1890–1978) developed the technique of contrast myelography, which involved the intrathecal injection of the radiopaque substance lipiodol. Following injection via cistern puncture with the patient in upright position, lipiodol would flow down the spinal canal until an obstructive lesion was encountered and the contrast substance would come to a halt. Using this method, the upper margin of the lesion could clearly be located on the radiogram. The lower margin of the lesion could subsequently be visualized by lumbar lipiodol injections with the patient in the Trendelenburg position. In practice, most authors only used the cisternal route, as the lumbar procedure was uncomfortable for patients and prone to misinterpretation.
In addition to these new diagnostic techniques, cistern puncture was also adopted for diagnostic procedures that had previously been performed using lumbar puncture, including pneumoencephalography and routine CSF withdrawal. Indeed, several physicians held that cistern puncture should replace lumbar puncture altogether, arguing that it was easier to perform, required less recovery time, was better tolerated by patients and was less frequently accompanied by post-dural puncture headache. According to American psychiatrist Franklin Ebaugh (1895–1972), for example, his patients often “spontaneously asked for ‘neck punctures’ in preference to the ‘back punctures’” and ‘got off the table unassisted and walked to the ward’ when the procedure was done (Ebaugh, 1922).
A procedure for the stout hearted
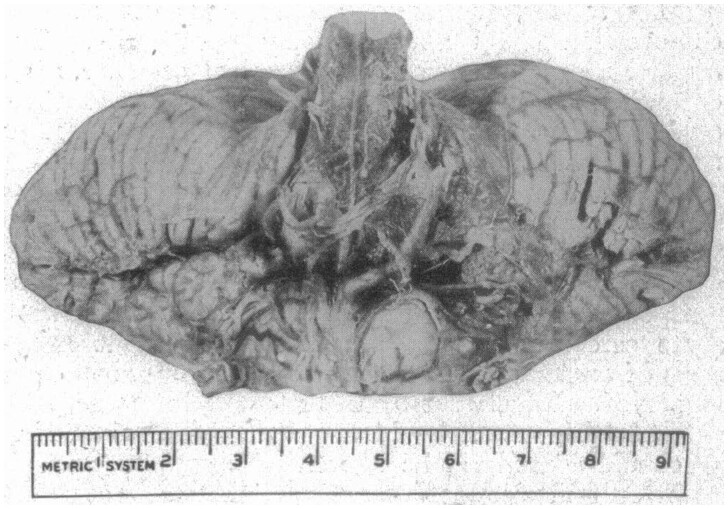
Notwithstanding the advantages of cistern puncture, most physicians were well aware of the potential dangers of inserting a needle in close proximity to the medulla oblongata. While introducing the procedure, Ayer already stated that ‘in spite of the simplicity of the technic it would … be unfair to the patient to perform cisterna puncture without previous experience at the necropsy table’ (Ayer, 1920), and even Ebaugh advised a certain degree of caution in the clinical application of cistern puncture ‘owing to the proximity of the medulla oblongata’ (Ebaugh, 1922). Such perceived dangers were hypothetical at first, but as experience with cistern puncture accumulated, incidental reports of adverse events—including subarachnoid haemorrhage, temporary cessation of respiration and death—began to appear in the literature (Fig. 3). These complications were, however, typically attributed to faulty technique or ignorance of relevant contraindication; cistern puncture generally being considered safe in experienced hands. Nevertheless, views regarding the precautions necessary to warrant the safety of the procedure diverged. While some authors argued that cistern puncture could safely be performed by any physician after preliminary practice on the cadaver, others, including the London neurologist James Purves-Stewart, held that the procedure was only safe in the hands of a select group of specialists with ‘a knowledge of [cerebral] anatomy, a steady hand, and a stout heart’ (Purves-Stewart, 1924).
Figure 3.
Post-mortem brain revealing haemorrhage surrounding the brainstem following cistern puncture. From Ebaugh (1925).
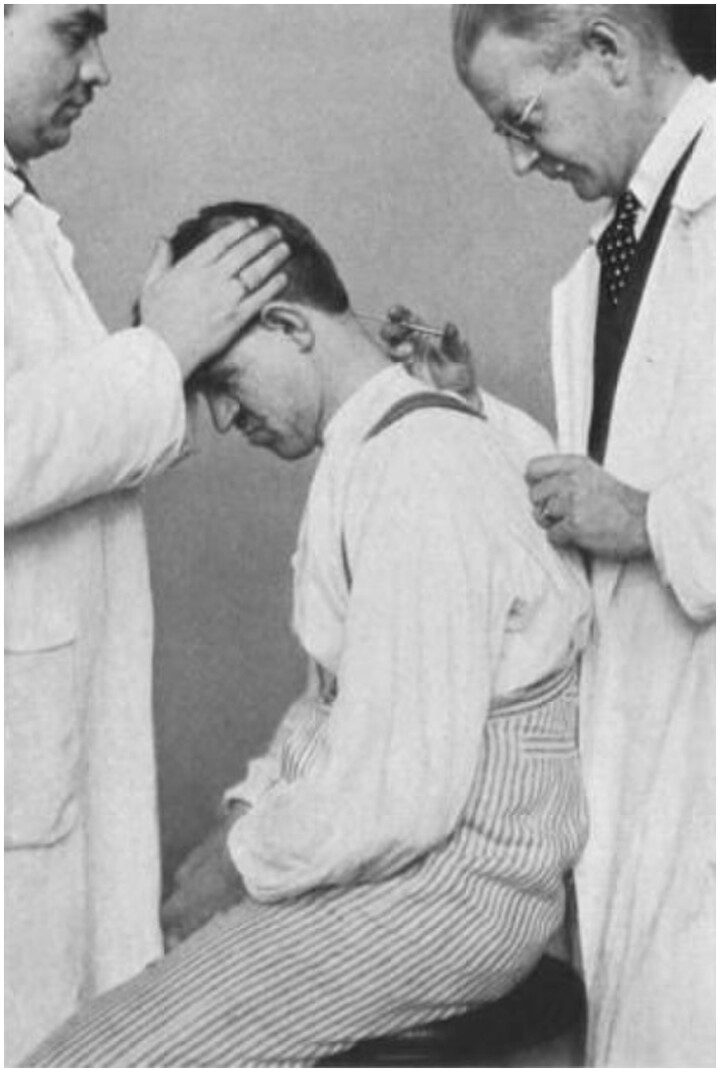
Besides the question of who was to perform cistern puncture, different attitudes towards to safety of the procedure were also reflected in the technical performance itself. In 1923, German internist Karl Eskuchen (1885–1955), who was unaware of Ayer’s work, introduced an alternative technique for puncturing the cisterna magna (Fig. 4). In contrast to Ayer’s technique—in which the direction and depth of the needle was based on external anatomical landmarks and tactile feedback upon puncturing the occipito-atlantoid ligament, respectively—Eskuchen used the occipital bone as an ‘orientation point’ (Eskuchen, 1928). In Eskuchen’s technique, the puncture needle was directed obliquely towards the posterior edge of the foramen magnum. Once the occipital bone was encountered, the needle was slightly retracted and subsequently pushed forward at a somewhat declined angle, thereby entering the relatively spacious upper region of the cisterna magna. According to Eskuchen, his technique was much safer to that of Ayer’s, as the unreliability of tactile feedback supposedly caused physicians to be ‘in the dark when there is any deviation from the norm’ (Eskuchen, 1928). This view was shared by most German-speaking authors, who widely adopted Eskuchen’s technique, whereas Ayer’s technique remained the method of choice in the USA.
Figure 4.
Cistern puncture performed by Karl Eskuchen (1885–1955). From Eskuchen (1928).
Concerning the contraindications of cistern puncture, there tended to be more agreement. Similar to lumbar puncture, cistern puncture was not to be performed when increased intracranial pressure was present or suspected, particularly in patients with a suspected brain tumour, as puncture could result in herniation of the brain through the foramen magnum and brainstem compression. Moreover, the procedure was contraindicated when abnormal anatomical relations or obliteration of the cisterna magna was suspected, since dislocated vascular or neuronal structures could potentially be damaged by the puncture needle. Such anatomical aberrations were relatively common in patients with atherosclerosis, meningeal adhesions and congenital or acquired skeletal malformations of the occipito-cervical region, causing physicians to be somewhat reluctant to perform cistern puncture on these patients.
Developments in the 20th century
As the 20th century progressed, indications for cistern puncture gradually declined. In the 1940s, the introduction of penicillin revolutionized the treatment of infectious diseases, including syphilis and meningitis. In neurosyphilis, intramuscular and intravenous penicillin injections—either with or without fever therapy or salvarsan—showed such good results that additional intrathecal injections increasingly seemed unnecessary. Whereas, in severe cases, intrathecal penicillin was still sporadically resorted to, the cistern route was considered too dangerous on account of potential adverse reactions to the drug when it was delivered in high concentrations near the syphilitic brain (Worster-Drought, 1947). Interestingly, while efficient drug delivery to the brain had been an important rationale behind the therapeutic use of cistern puncture in earlier decades, it now provided a powerful argument against the procedure.
The treatment of meningitis was characterized by similar developments, even though intrathecal drug administration—first sulphamides and later penicillin and other antibiotics—remained relatively common until the 1960s. Although cistern puncture was still occasionally referred to as the best route available ‘from the standpoint of drug dispersion’, it was generally considered ‘wise to sacrifice the somewhat better distribution of the drug, for the greater safety of lumbar injection’ (Walker and Johnson, 1945). A notable exception was American infectiologist William Winn (1903–69), who, in 1964, advocated the use of intracistern amphotericin B injections, as ‘it offered a more direct approach to the usual site of coccidioidal infection at the base of the brain’ (Winn, 1964). This approach was eventually discarded because of persistent reports of serious complications associated with cistern puncture.
For diagnostic purposes, cistern puncture remained relatively common until the last quarter of the 20th century, even though, in contrast myelography, the lumbar route was increasingly favoured over the cistern route. Moreover, in the late 1960s, the technique of lateral C1–C2 puncture was introduced as a safer and easier alternative to cistern puncture in cases where examination of the upper spinal canal or craniocervical junction were imperative (Kelly and Alexander, 1968). When non-invasive imaging modalities eventually replaced myelography in the diagnosis and localization of spinal lesions, cistern puncture had become an exceedingly rare procedure, no longer part of the armamentarium of the neurologist and neurosurgeon.
Conclusion
During the first half of the 20th century, cisterna magna puncture held several important therapeutic and diagnostic applications and offered some distinct advantages over lumbar puncture. These advantages led some authors to advocate the cistern over the lumbar route for routine CSF access. Nevertheless, cistern puncture always remained a road less travelled, the potential dangers associated with the procedure ultimately outweighing its benefits, despite various technical adaptations aimed at reducing the risk of damaging the medulla oblongata. The renewed interest in cistern puncture for intrathecal gene therapy, however, shows that the procedure and the rationale behind its therapeutic use have not faded into oblivion. Indeed, it has been suggested that the widespread cell transduction following intracistern viral vector administration may be caused by the ‘rapidly dispersing cisternal CSF’, revealing a striking parallel with Ayer’s characterization of the cisterna magna as a central distributing centre precisely 100 years ago. Whether the potential clinical advantages of intracistern gene therapy will outweigh its potential dangers remains for future investigators to discover.
Funding
No funding was received towards this work.
Competing interests
The authors report no competing interests.
References
- Ayer JB. Puncture of the cisterna magna. Arch Neurol Psychiatr 1920; 4: 529–41. [Google Scholar]
- Ebaugh FG. The treatment of general paresis by the intracistern route. Arch Neurol Psychiatr 1922; 7: 325–31. [Google Scholar]
- Ebaugh FG. Puncture of the cisterna magna: a summary of five years’ experience. JAMA 1925; 85: 184–6. [Google Scholar]
- Eskuchen K. Die Zisternenpunktion. In: Langstein L, Schittenhelm A, editors. Ergebnisse der inneren Medizin und Kinderheilkunde. 34er band. Berlin: Verlag von Julius Springer; 1928. [Google Scholar]
- Hinderer C, Bell P, Vite CH, Loubtin J, Grant R, Bote E, et al. Widespread gene transfer in the central nervous system of cynomolgus macaques following delivery of AAV9 into the cisterna magna. Mol Ther Methods Clin Dev 2014; 1: 14051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly DL, Alexander E.. Lateral cervical puncture for myelography. J Neurosurg 1968; 29: 106–10. [DOI] [PubMed] [Google Scholar]
- Purves-Stewart J. The treatment of general paralysis. Br Med J 1924; 1: 508–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker AE, Johnson HC.. Principles and practice of penicillin therapy in diseases of the nervous system. Ann Surg 1945; 122: 1125–35. [PubMed] [Google Scholar]
- Wegeforth P, Ayer JB, Essick CR.. The method of obtaining cerebrospinal fluid by puncture of the cisterna magna (cistern puncture). Am J Med Sci 1919; 157: 789–97. [Google Scholar]
- Winn WA. The treatment of coccidioidal meningitis—the use of amphotericin B in a group of 25 patients. Calif Med 1964; 101: 78–89. [PMC free article] [PubMed] [Google Scholar]
- Worster-Drought C. Penicillin in neurosyphilis. Br Med J 1947; 2: 559–64. [DOI] [PMC free article] [PubMed] [Google Scholar]