Abstract
Background
Older patients with chronic renal failure (CRF) which currently is referred to as end-stage renal disease (ESRD) are associated with higher mortality. In-center nocturnal dialysis (INHD) is a new blood purification model, which is characterized by longer sessions and nighttime administration. However, no data for the efficacy of INHD in older patients with ESRD are available. This study is to analyze the effect of INHD in the treatment of older patients with ESRD.
Methods
A retrospective, observational study was conducted in a university teaching hospital. Seventy-two patients with ESRD receiving INHD were enrolled. They were divided into the older ESRD patients (age ≥60) group (n = 22) and the non-older ESRD patients (age <60) group (n = 50). The causes of older ESRD patients and non-older ESRD patients receiving INHD were analyzed. Differences of laboratory test indicators of older patients with ESRD before INHD and after INHD were compared. Quality of life for older ESRD patients receiving INHD was assessed by using the Kidney Disease Quality of Life-36 Instrument (KDQOL-36).
Results
Serum concentration of hemoglobin and serum concentration of albumin of older patients with ESRD increased significantly after INHD (p < 0.05). There were similar results in the non-older cohort (p ≤ 0.05). Scores of five KDQOL-36 subscales increased significantly after INHD (p ≤ 0.001) indicated that the quality of life for old patients with ESRD was significantly improved after INHD.
Conclusion
INHD is an effective blood purification therapy that can improve the condition of renal anemia, and it may provide a potential positive impact in the malnutrition of older and non-older patients with ESRD. INHD can improve the quality of life of older patients with ESRD. The results will provide a basis for formulating new policies of blood purification therapy for older patients.
Keywords: older patients, chronic renal failure, CRF, end-stage renal disease, ESRD, in-center nocturnal hemodialysis, INHD, quality of life, nocturnal home hemodialysis, NHHD
Introduction
Older patients with chronic renal failure (CRF), which currently is referred to as end-stage renal disease (ESRD), are associated with higher mortality. Hemodialysis (HD) is one of the main methods of treatment for patients with ESRD, in which conventional hemodialysis (CHD; 3–4 hours per session, three times per week) is the most widely used hemodialysis treatment mode. In clinical practice, it is found that there are some defects in this hemodialysis treatment mode. In-center nocturnal hemodialysis (INHD; 7–8 hours per session, three times per week) is a new blood purification model, which is characterized by longer sessions and nighttime administration and may lead to better outcomes for some patients.1 INHD has been applied in the treatment of patients with ESRD. Owing to its longer treatment duration-up to 7.5 hours per dialysis treatment-in-center thrice-weekly, INHD is receiving greater attention,2 and scholars have conducted relevant researches on this new blood purification mode.3–6 It has been found that INHD was associated with improvements in several clinically relevant outcomes compared to that of CHD and no pre-specified outcome was worse with INHD.7 However, most clinical studies of INHD are aimed at patients of all age groups and clinical research on older patients with ESRD receiving INHD has not been reported. The older patients with ESRD receiving INHD are a special patient group whose health status, nutritional status, immunity and organs’ function are significantly different from that of patients from other age groups. Human society has entered the age of aging, and the number of older patients with ESRD receiving HD treatment is increasing significantly. However, no data for the efficacy of INHD in older patients with ESRD is available. Therefore, it is necessary to study the effect of INHD in older patients with ESRD. This study is to analyze the effect of INHD in the treatment of older patients with ESRD.
Methods
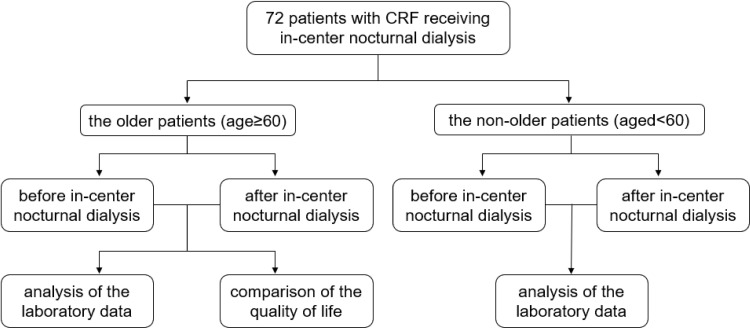
A retrospective, observational study was conducted in a university teaching hospital. 72 patients with ESRD receiving INHD at a large hemodialysis center with more than 100 hemodialysis machines were enrolled into this study. They were divided into the older patients (age≥60) with ESRD group and the non-older patients (age<60) with ESRD group. The flow diagram of enrollment and grouping of older patients with ESRD receiving INHD are shown in Figure 1. INHD was performed 7.5 hours a time, three times a week. The starting time of INHD is 22:00–22:30. The end time of INHD is 5:30–6:00. CHD was performed regularly 4 hours a time, three times a week. Mean dialysis duration of CHD was 12 hours per week. Mean dialysis duration of INHD was 22.5 hours per week. Patients who interrupted INHD treatment and then continued INHD were excluded. The blood samples were taken before hemodialysis and the timing of the sample collections were 84.58±23.57 months. Renal anemia,8 hypertension9 and bone mineral metabolism disorder10 were defined according to various international standards. Clinical characteristics and laboratory test results of the older patients with ESRD and non-older patients with ESRD are shown in Table 1.
Figure 1.
The flow diagram of enrollment and grouping of older patients with end stage renal disease receiving in-center nocturnal dialysis.
Abbreviation: INHD, in-center nocturnal dialysis.
Table 1.
Clinical Characteristics and Laboratory Test Results of the Older Patients with End-Stage Renal Disease (Age≥60) and Non-Older Patients with End-Stage Renal Disease (Age<60)
| Variables | All Patients | Older Patients (Age≥60, n=22) | Non-Older Patients (Age<60, n=50) | t/z/χ2 | p value |
|---|---|---|---|---|---|
| Mean ages (yr) (±SD) | 52.71±12.194 | 66.59±4.72 | 46.60±9.02 | 0.0000 | |
| Gender (male/female) | 55/17 | 17/5 | 38/12 | 0.014 | 0.907 |
| Duration of HD (month) | 134.96±64.59 | 149.64±64.43 | 128.50±64.24 | 1.285 | 0.203 |
| Duration of INHD (month) | 84.58±23.57 | 86.95±24.58 | 83.54±23.29 | 0.564 | 0.575 |
| Complications | |||||
| Renal anemia (n) | 59(81.9%) | 21(95.5) | 38(76.0) | 2.704 | 0.100 |
| Hypertension (n) | 14(19.4) | 2(9.1) | 12(24.0) | 1.321 | 0.250 |
| Bone mineral metabolism disorder (n) | 3(4.2) | 0(0.0) | 3(6.0) | 0.285 | 0.594 |
| Hemoglobin (g/L) | 96.19±25.939 | 99.91±25.677 | 94.56±26.143 | 0.804 | 0.424 |
| Platelet (*10^9/L) | 176.33±62.958 | 175.45±71.638 | 176.72±59.526 | 0.078 | 0.938 |
| Serum calcium (umol/L) | 2.305±0.326 | 2.351±0.282 | 2.286±0.345 | 0.774 | 0.441 |
| Serum phosphorus (umol/L) | 1.762±0.611 | 1.843±0.62 | 1.727±0.61 | 0.74 | 0.462 |
| Parathyroid hormone (pg/mL) | 384.285±544.901 | 412.268±710.141/248(111.7075,388.8250) | 371.972±462.16/251.8(128.025,438.475) | 0.037 | 0.971 |
| Ferritin (ug/L) | 371.152±444.647 | 316.98±346.848/209.75(99.89,405.4) | 394.987±482.725/225.0(78.5475,504.625) | 0.416 | 0.678 |
| Albumin (g/L) | 39.625±5.65 | 38.5±5.655 | 40.12±5.634 | 1.123 | 0.265 |
| KT/V | 2.276±0.892 | 2.394±0.869 | 2.223±0.906 | 0.725 | 0.471 |
| Volume of blood flow of INHD (mL/min) | 213.889±23.229 | 216.818±16.442/220 (200,220) | 212.6±25.699/215 (200,220) | 0.853 | 0.394 |
Abbreviations: INHD, in-center nocturnal dialysis; HD, hemodialysis; KT/V, (K: effective urea clearance; T: effective dialysis time; V: volume of distribution of urea).
The causes of the older patients with ESRD receiving INHD and non-older patients with ESRD receiving INHD are shown in Table 2. Differences of some important laboratory test indicators of older patients with ESRD before INHD and after INHD were compared.
Table 2.
Causes of the Older Patients with End-Stage Renal Disease and the Non-Older Patients with End-Stage Renal Disease
| Causes of Chronic Renal Failure | All Patients | Older Patients (Age≥60, n=22) | Non-Older Patients (Age<60, n=50) |
|---|---|---|---|
| Chronic glomerulonephritis n (n%) | 48(66.7%) | 37(74%) | 11(50%) |
| Polycystic kidney disease | 10(13.9%) | 7(14%) | 3(13.6%) |
| Diabetic nephropathy | 3(4.2%) | 1(2%) | 2(9.1%) |
| Hypertensive nephropathy | 5(6.9%) | 0(0%) | 5(22.7%) |
| Chronic pyelonephritis | 1(1.4%) | 0(0%) | 1(4.5%) |
| Hepatitis B virus associated glomerulonephritis | 1(1.4%) | 1(2%) | 0(0%) |
| Cause of chronic renal insufficiency is unknown | 4(5.6%) | 4(8%) | 0(0%) |
Quality of life for older ESRD patients receiving INHD was assessed by using Kidney Disease Quality of Life-36 Instrument (KDQOL-36).11 Kidney Disease Quality of Life-36 (KDQOL-36) is a 36-item health-related quality of life scale, mainly used to measure the quality of life of dialysis patients. Since there is no recognized KDQOL-36 overall score that includes all KDQOL-36 subscales, we calculated the scores of five KDQOL-36 subscales, respectively, including symptoms of kidney disease, effects of kidney disease, burden of kidney disease, 12-item Short Form Health Survey (SF-12) Summary of Physical Component and 12-item Short Form Health Survey (SF-12) Summary of Psychological Component. The raw scores were transformed linearly to a range of 0 to 100. This scale was then translated by RAND Corporation according to the basic guidelines and specifications on using forward and back translation. See: http://www.rand.org/health/surveys_tools/about_translations.html
The protocol for this research project has been approved by the Ethics Committee of Shanghai Changzheng Hospital (No. 201106-3) and it conforms to the provisions of the Declaration of Helsinki in 1975 (as revised in Edinburgh 1983). Informed, written informed consent was obtained from every participant and no participants received any stipend.
Statistical analysis of the study data was performed by using the IBM SPSS Statistics Version 20.0 (IBM Inc., Chicago, USA). Continuous variables were analyzed by t-test, the Wilcoxon signed-rank test or two-way analysis of variance (ANOVA). Normally distributed variables were expressed as the mean ± standard deviation (x±s) and non-normally distributed variables were expressed as median and interquartile range. Categorical variables were analyzed by chi-square test or Fisher’s exact test. p value < 0.05 was considered statistically significant.
Results
In this study, no significant differences were found between the older patients with ESRD (n = 22, mean ages = 66.59±4.72 years old) and the non-older patients with ESRD (n=50, mean ages=46.60±9.02 years old) in the following categories: the duration of patients with ESRD treated by CHD, duration of patients with ESRD treated by INHD, renal anemia, hypertension, bone mineral metabolism disorder, metastatic calcification, hemoglobin, serum calcium, serum phosphorus, parathyroid hormone, albumin, KT/V (K: Effective Urea Clearance; T: Effective Dialysis Time; V: Volume of Distribution of Urea), volume of blood flow, etc. 72 patients with ESRD receiving INHD were enrolled. 55 were male and 17 were female (mean ages=52.71±12.194 years old). Duration of the older patients with ESRD treated by CHD before INHD was 149.64±64.43 months. Duration of the non-older patients with ESRD treated by CHD before INHD was 128.50±64.24 months. Duration of the older patients with ESRD treated by INHD was 86.95±24.58 months. Duration of the non-older patients with ESRD treated by INHD was 83.54±23.29 months. Please see Table 1.
In this study, chronic glomerulonephritis (74%) was the primary cause for the older patients with ESRD receiving INHD and polycystic kidney disease (14%) was the second. Chronic glomerulonephritis (50%) was also the primary cause for the non-older patients with ESRD receiving INHD, and hypertensive nephropathy (22.7%) was the second. Please see Table 2.
Additionally, it was found that serum concentration of hemoglobin of older patients with ESRD increased significantly after INHD treatment (p=0.012) and serum concentration of albumin of older patients with ESRD also increased significantly after INHD treatment (p= 0.022). Serum calcium and the platelet count increased after INHD treatment. Serum phosphorus, parathyroid hormone and serum ferritin decreased after INHD treatment, but there were no significant differences (p>0.05). The differences of the laboratory data of the older patients with ESRD before and after INHD were shown in Table 3.
Table 3.
Analysis of the Laboratory Data of the Older Patients with End-Stage Renal Disease Before and After In-Center Nocturnal Dialysis
| Laboratory Test Indicators | Before INHD | After INHD | t/z | p value |
|---|---|---|---|---|
| Hemoglobin | 99.91±25.677 | 116.95±13.906 | 2.738 | 0.012 |
| Platelet | 175.45±71.638 | 186.773±60.693 | 0.976 | 0.34 |
| Serum calcium | 2.351±0.282 | 2.45±0.204 | 1.424 | 0.169 |
| Serum phosphorus | 1.843±0.62 | 1.667±0.531 | 1.135 | 0.269 |
| Parathyroid hormone | 412.268±710.141/248 (111.7075,388.8250) | 313.149±199.806/267.3 (165.85,377.4) | 0.243 | 0.808 |
| Serum ferritin | 316.98±346.848 | 162.996±126.24 | 2.01 | 0.058 |
| Albumin | 38.5±5.655 | 42.091±4.208 | 2.469 | 0.022 |
Abbreviation: INHD, in-center nocturnal dialysis.
We observed a significant decrease in serum concentrations of hemoglobin (p<0.001), serum calcium (p= 0.031) and serum ferritin (p= 0.013) of non-older patients with ESRD after INHD. There were no significant differences found in the total blood count of platelet, serum phosphorus, parathyroid hormone, serum ferritin and albumin of non-older patients with ESRD after INHD (p≥0.05). However, it is worth noting that there were some similar results between the older and non-older patients with ESRD cohort. The differences of the laboratory data of the non-older patients with ESRD before and after INHD are shown in Table 4.
Table 4.
Analysis of the Laboratory Data of the Non-Older Patients with End-Stage Renal Disease Before and After In-Center Nocturnal Dialysis
| Laboratory Test Indicators | Before INHD | After INHD | t/z | p value |
|---|---|---|---|---|
| Hemoglobin | 94.56±26.143 | 121.38±16.373 | 6.254 | 0.000 |
| Platelet | 176.72±59.526 | 168.5±52.875 | 1.042 | 0.303 |
| Serum calcium | 2.286±0.345 | 2.433±0.272 | 2.227 | 0.031 |
| Serum phosphorus | 1.727±0.61 | 1.569±0.666 | 1.23 | 0.224 |
| Parathyroid hormone | 371.972±462.16 251.8 (128.025,438.475) |
378.922±369.627/300.2(138.3,471.475) | 0.941 | 0.347 |
| Serum ferritin | 394.987±482.725/225(78.5475,504.625) | 189.575±176.018/123.55(50.7425,267.275) | 2.472 | 0.013 |
| Albumin | 40.12±5.634 | 41.8±3.057 | 1.993 | 0.052 |
Abbreviation: INHD, in-center nocturnal dialysis;
Furthermore, KDQOL-36 subscales were applied to assess the quality of life for old patients with ESRD before and after INHD. It was found that the scores of five KDQOL-36 subscales (Symptoms of kidney disease, effects of kidney disease, Burden of kidney disease, 12-item Short Form Health Survey (SF-12) Summary of Physical Component and 12-item Short Form Health Survey (SF-12) Summary of Psychological Component) increased significantly after INHD (p≤0.001) which indicated that the quality of life of old patients with ESRD was significantly improved after INHD. The scores of Symptom/problem list before and after INHD was 69.79±9.74 and 81.56±7.56, respectively. The scores of effects of kidney disease before and after INHD was 59.69±15.09 and 73.75±12.02, respectively. The scores of Burden of kidney disease before and after INHD was 16.88±14.45 and 35.63±12.66, respectively. The scores of SF-12 Physical Composite before and after INHD was 29.35±5.97 and 32.89±7.21, respectively. The scores of SF-12 Mental Composite before and after INHD was 32.27±7.69 and 43.72±5.03, respectively (see Table 5).
Table 5.
Comparison of the Quality of Life for Older Patients with End-Stage Renal Disease Before and After In-Center Nocturnal Hemodialysis
| Items | Before INHD | After INHD | t | p value | df |
|---|---|---|---|---|---|
| Symptom/problem list | 69.79±9.74 | 81.56±7.56 | −14.064 | 0.000 | 21 |
| Effects of kidney disease | 59.69±15.09 | 73.75±12.02 | −15.108 | 0.000 | 21 |
| Burden of kidney disease | 16.88±14.45 | 35.63±12.66 | −13.748 | 0.000 | 21 |
| SF-12 Physical Composite | 29.35±5.97 | 32.89±7.21 | −3.682 | 0.001 | 21 |
| SF-12 Mental Composite | 37.27±7.69 | 43.72±5.03 | −5.408 | 0.000 | 27 |
Abbreviations: INHD, in-center nocturnal dialysis; SF-12 Physical Composite, 12-item Short Form Health Survey Summary of Physical Component from the Kidney Disease Quality of Life-36; SF-12 Mental Composite, 12-item Short Form Health Survey Summary of Psychological Component from the Kidney Disease Quality of Life-36.
Discussion
INHD is an innovation of HD treatment mode with the characteristics of low treatment cost, positive treatment outcomes, higher cost performance, longer sessions and nighttime administration in HD center. Compared with CHD in this study, we found that INHD can improve the condition of renal anemia and has potential positive impact in the malnutrition of older and non-older patients with ESRD, especially in improving the quality of life of older patients with ESRD.
Previous clinical studies related to INHD have been carried out since INHD was applied in the treatment of patients with ESRD. In the study of Lacson et al, it was found that INHD was associated with favorable clinical features, laboratory biomarkers, and improved survival compared with propensity score-matched controls.12 INHD is on the increase all over the world, and enables patients to both work and live normally during the daytime without the interference of hemodialysis treatment. It also provides a new hemodialysis mode for patients who need to extend the dialysis duration for various medical reasons.13
In developed countries, nocturnal hemodialysis, also called nocturnal home hemodialysis (NHHD), is mainly carried out in a patient’s home. Although it is easy for older patients with ESRD to receive HD treatment within their own homes, NHHD cannot guarantee the quality of hemodialysis due to it being affected by several environmental factors as well as conditions in the homes of older patients. Our study is about INHD which is conducted in hemodialysis centers at night which is different from NHHD. We can conclude that INHD conducted at night had no significant effect on the normal work life of older patient with ESRD during the daytime. In our study, INHD was conducted in the hemodialysis center of a large general hospital at night and adopted the same standard of hemodialysis quality control, standard of treatment, and dialysate as the daytime hemodialysis treatment. These characteristics ensured that all the older patients with ESRD receiving INHD have the same quality control standards of hemodialysis.
The main advantage of INHD is that it takes 8 hours for each hemodialysis treatment compared to just 3–4 hours for CHD, which cannot fully remove enough toxins and excess water from patients’ blood in such a short amount of time. INHD allows patients to have sufficient time for long-term hemodialysis treatment and while removing harmful metabolic substances such as creatinine and metabolized waste. It also maintains electrolyte and acid-base balance and removes excessive water from patients’ blood. Due to the prolonged dialysis time, INHD was accompanied with some dietary restrictions for patients with ESRD. For example, patients had restrictions on drinking water and required tightly regulated protein intake. Overall, INHD can improve the nutritional status of patients and patients’ quality of life.
In terms of the efficacy of HD treatment, the effect of INHD and NHHD on patients with ESRD is comparable. In a retrospective analysis of NHHD in four European centers for a minimum of 12 months, it was found that NHHD was both effective and safe at improving long-term patient outcomes.14 In the study of Wong et al, INHD was associated with increased hemoglobin levels and lower serum phosphate levels. These results are the same as those represented in our study, which found a significant increase in the serum hemoglobin concentration (p < 0.05) in the older patients with ESRD after INHD treatment. Serum hemoglobin concentration of patients with ESRD is an important index to judge the improvement of renal anemia in ESRD patients receiving hemodialysis. An increase of serum hemoglobin concentration in older patients with ESRD after INHD indicated that INHD can improve renal anemia of older ESRD patients. Also, observed a significant increase in the serum albumin concentration (p < 0.05) of older patients with ESRD after INHD. In the setting of CKD, some studies have shown that reduced serum albumin concentrations are often a manifestation of protein-energy wasting - a state of metabolic and nutritional alterations resulting in reduced protein and energy stores.15 Although anemia and malnutrition are associated with higher cardiovascular morbidity and mortality. The role of albumin as a direct marker of nutrition remains a contentious issue. Since albumin loss into the dialysate through the dialyzer appears to be a potentially modifiable cause of hypoalbuminemia in some patients, the results of our study support the notion that INHD has potential positive impact in malnutrition of older patients with ESRD.
There are also some different conclusions about the therapeutic effect of INHD. In the study of Gangaram et al, it was found that there were a trend for improvement in standardized Kt/V, phosphate, hemoglobin, and albumin, along with a significant reduction in phosphate binder usage after NHHD.14 The improvement in hemoglobin and albumin in their study was similar to that of our study. The difference between their research and our research results is (re-phrase for punctuality) is that we found serum phosphorus and parathyroid hormone to be decreased after INHD without significant differences (p>0.05). This may be attributed to the relatively small patient sample size and the shorter duration time all patients with ESRD treated by INHD, which was 84.58±23.57 months. Therefore, the therapeutic effect of INHD in the older patients with ESRD may have been present, but there was no significant statistical difference since the relatively shorter observation time of the older patients with ESRD receiving INHD in our study.
INHD has been applied in some countries for the treatment of older patients with ESRD. At the same time, NHHD has also been used in other regions. Some clinical studies on NHHD have been carried out, and several benefits of frequent NHHD have been reported.16 In the study by Tennankore et al, it was found that those receiving NHHD had similar patient survival compared to patients receiving short daily HD and conventional home HD.17 In another study by Li et al, it was concluded that NHHD appeared to offer higher employment rate, lower dosage of aluminum-based phosphate binder and mineral metabolic markers at 1 year compared with CAPD in Hong Kong.18 Pnnn et al found that NHHD with an alternate night schedule improves anemia and reduces ESA requirement because of enhanced uremic clearance, and this benefit extended beyond the first year of NHHD.19 This is similar to the results of our study, which found that serum concentration of hemoglobin of older patients with ESRD increased significantly after INHD. It was found that NHHD leads to favorable cardiovascular remodeling with a reduction in cavity dimensions, regression of left ventricular hypertrophy, and an improvement in diastolic function.20 Thomson et al found hemodialysis modalities of longer duration were associated with improvements in electrocardiographic parameters associated with sudden cardiac death.21 However, prospective trials are required to determine whether dialysis prescription reduces sudden cardiac death, cardiovascular morbidity, and mortality in hemodialysis patients. In regards to the cost-utility analysis of NHHD, there have also been studies done in support of our findings. Klarenbach et al performed a cost-utility analysis of frequent NHHD compared with CHD and found that frequent NHHD is superior to CHD.22
Nocturnal hemodialysis is an underutilized way of offering extended-hour hemodialysis to patients in both home and in-center environments. NHHD was developed because it was less expensive than INHD, thus allowing more patients to be treated with the limited medical care funds.23 NHHD has several additional advantages. For example, it can save time for patients to go to the hospital. But patients receiving NHHD requiring caregiver assistance for dialysis may be at higher risk for poor outcomes. However, it was found that the need for caregiver assistance alone was not a deterrent to NHHD.24 INHD can guarantee the quality of HD for the older patients. Since INHD was performed in the hemodialysis center, doctors can monitor patients’ conditions through a duration of time, while providing corresponding treatment. Another point to bring up is that the quality of dialysate was also fully guaranteed. Based on the data we found in our study, along with findings from other studies regarding hemodialysis, INHD is considered superior to NHHD. Ultimately, we should find a balance between the advantages and disadvantages of INHD and NHHD to then choose the appropriate hemodialysis treatment mode according to the specific situation of older patients with ESRD. Why did we choose INHD instead of NHHD for the older patients with ESRD in the hemodialysis center? The first reason was to ensure the dialysis quality of older patients with ESRD in the hemodialysis center. The second reason was that the older patients with ESRD believed it was safer to receive dialysis treatment in the hemodialysis center in the hospital (INHD) than at home (NHHD).
INHD is a kind of blood purification method, which is not widely used to provide long-term hemodialysis for older patients. With the development of nocturnal hemodialysis, clinicians and dialysis providers are becoming increasingly obliged to investigate implementation strategies for nocturnal hemodialysis services to improve patient outcomes.25 INHD has been associated with variable clinical benefits. For example, it has been found that phosphate had been removed in a consistent manner during the whole duration of nocturnal HD as assessed through dialysate and the total removed phosphate was higher than previously reported and exceeded the normal phosphate food intake.26 To some extent, this conclusion is similar to that of our study, which demonstrated that serum phosphorus of the older patients with ESRD decreased after INHD. In the study of Noori et al, it was demonstrated that INHD can improve the nutritional status of patients with ESRD and prolongation of sessions with INHD may improve clinical outcomes by enhancement of ultrafiltration and uremic toxin removal.27 This conclusion is like that of our study which demonstrated that serum concentration of albumin of older patients with ESRD also increased significantly after INHD treatment (p= 0.022).
With the focus of health changing from biological health to bio-psycho-social health, the treatment of end-stage renal disease is no longer limited to life maintenance and symptom relief. Rather, it has evolved to comprehensively improve and restore patients’ physical, psychological, and social activities. The quality of life of patients with ESRD has become a reliable index for comprehensive evaluation of HD treatment. In our study, it was found that INHD can improve the quality of life for elderly patients with ESRD. This may be due to the extended dialysis time of INHD, which led to a significant increase in the clearance of toxic substances in older patients with ESRD. The ultrafiltration rate per unit time was decreased during INHD and the hemodynamic, and changes were relatively stable during INHD. This resulted in a decrease in the incidence of adverse events.28 Likewise, it has been found that Continuous renal replacement therapy (CRRT) was beneficial in cutting the peaks of the concentrations of both pro- and anti-inflammatory mediators, restoring a situation of immuno-homeostasis due to their continuity and unspecific capacity of removal.29 Like CRRT, INHD may eliminate pro-inflammatory mediators to restore immune homeostasis by prolonging dialysis time, which will enhance the immunity of older patients with ESRD. As infection is one of the main risk factors leading to death of older patients with ESRD, INHD is also seen to reduce the risk of infectious diseases. Thus, INHD may prolong the survival time of older patients with ESRD and improve the quality of life of older patients with ESRD.
Sleep disturbances are common in ESRD patients, and its treatment is an area that requires further study. At present, some researchers found that overall subjective sleep quality on both dialysis and off-dialysis nights were improved after a switch from CHD to NHD, especially in the patients with sleep disorders.30,31
It is worth noting that the results between the two cohorts (≥60 years old and <60 years old) are similar. This suggests that INHD is a potential renal replacement therapy for adults with end-stage kidney disease and that age cut-offs may not apply to dialysis modalities when renal replacement therapy is clinically appropriate for the individual.
There are some limitations in this study. This study is a single-center study with a relatively small number of patients and a relatively short observation time. More patients of multiple centers and longer observation time will be needed in the future. A prospective randomized controlled study will be conducted in the future to compare the difference in treatment effect between older patients receiving INHD and CHD.
Conclusions
INHD is an effective blood purification therapy for older patients with ESRD. INHD can improve the condition of renal anemia and may take potential positive impact in malnutrition of older and non-older patients with ESRD. INHD can improve the quality of life of older patients with ESRD. The results will provide a basis for formulating new policies of blood purification therapy for older patients.
Acknowledgments
We thank Felix Yang from University of Missouri – Kansas City School of Medicine, USA, for the guidance of grammar, style and choice of words of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wilk AS, Tang Z, Hoge C, Plantinga LC, Lea JP. Association between patient psychosocial characteristics and receipt of in-center nocturnal hemodialysis among prevalent dialysis patients. Hemodial Int. 2019;23(4):479–485. doi: 10.1111/hdi.12782 [DOI] [PubMed] [Google Scholar]
- 2.Jakubovic BD, Yan AT, Wald R. In-center nocturnal hemodialysis. Semin Dial. 2014;27(2):179–187. doi: 10.1111/sdi.12184 [DOI] [PubMed] [Google Scholar]
- 3.Karur GR, Wald R, Goldstein MB, et al. Association between conversion to in-center nocturnal hemodialysis and right ventricular remodeling. Nephrol Dial Transplant. 2018;33(6):1010–1016. doi: 10.1093/ndt/gfx232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin X, Rong S, Mei C, Ye C, Chen J, Chen X. Effects of thrice-weekly in-center nocturnal vs. conventional hemodialysis on integrated backscatter of myocardial tissue. Hemodial Int. 2011;15(2):200–210. doi: 10.1111/j.1542-4758.2011.00537.x [DOI] [PubMed] [Google Scholar]
- 5.McFarlane PA, Bayoumi AM, Pierratos A, Redelmeier DA. The quality of life and cost utility of home nocturnal and conventional in-center hemodialysis. Kidney Int. 2003;64(3):1004–1011. doi: 10.1046/j.1523-1755.2003.00157.x [DOI] [PubMed] [Google Scholar]
- 6.Munoz Mendoza J, Bayes LY, Sun S, Doss S, Schiller B. Effect of lowering dialysate sodium concentration on interdialytic weight gain and blood pressure in patients undergoing thrice-weekly in-center nocturnal hemodialysis: a quality improvement study. Am J Kidney Dis. 2011;58(6):956–963. doi: 10.1053/j.ajkd.2011.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong B, Collister D, Muneer M, et al. In-center nocturnal hemodialysis versus conventional hemodialysis: a systematic review of the evidence. Am J Kidney Dis. 2017;70(2):218–234. doi: 10.1053/j.ajkd.2017.01.047 [DOI] [PubMed] [Google Scholar]
- 8.Babitt JL, Eisenga MF, Haase VH, et al. Controversies in optimal anemia management: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Conference. Kidney Int. 2021;99(6):1280–1295. doi: 10.1016/j.kint.2021.03.020 [DOI] [PubMed] [Google Scholar]
- 9.Kidney Disease: Improving Global Outcomes Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for management of blood pressure in chronic kidney disease. Kidney Int. 2021;2021(99):S1–S87. [DOI] [PubMed] [Google Scholar]
- 10.Kidney Disease: Improving Global Outcomes CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2017;7(1):1–59. doi: 10.1016/j.kisu.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB. Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res. 1994;3(5):329–338. doi: 10.1007/BF00451725 [DOI] [PubMed] [Google Scholar]
- 12.Lacson E Jr., Xu J, Suri RS, et al. Survival with three-times weekly in-center nocturnal versus conventional hemodialysis. J Am Soc Nephrol. 2012;23(4):687–695. doi: 10.1681/ASN.2011070674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doss S, Schiller B. Dialysis overnight: in-center nocturnal hemodialysis programs showing growth. Nephrol News Issues. 2011;25(8):22, 4, 6. [PubMed] [Google Scholar]
- 14.Gangaram V, Vilpakka M, Goffin E, Weinhandl ED, Kubisiak KM, Borman N. Nocturnal home hemodialysis with low-flow dialysate: retrospective analysis of the first European patients. Hemodial Int. 2019;24(2):175–181. doi: 10.1111/hdi.12808 [DOI] [PubMed] [Google Scholar]
- 15.Kalantar-Zadeh K, Ficociello LH, Bazzanella J, et al. Slipping through the pores: hypoalbuminemia and albumin loss during hemodialysis. Int J Nephrol Renovasc Dis. 2021;14:11–21. doi: 10.2147/IJNRD.S291348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Misra M, Twardowski ZJ. Benefits of frequent nocturnal home hemodialysis. Kidney Int. 2012;82(1):114–5;author reply 5. doi: 10.1038/ki.2012.90 [DOI] [PubMed] [Google Scholar]
- 17.Tennankore KK, Na Y, Wald R, Chan CT, Perl J. Short daily-, nocturnal- and conventional-home hemodialysis have similar patient and treatment survival. Kidney Int. 2018;93(1):188–194. doi: 10.1016/j.kint.2017.06.014 [DOI] [PubMed] [Google Scholar]
- 18.Li JW, Wong JHS, Chak WL, Chau KF. Effect of incident nocturnal home hemodialysis versus incident continuous ambulatory peritoneal dialysis on employment rate, clinical, and laboratory outcomes: a 1-year retrospective observation study. Hemodial Int. 2018;22(3):308–317. doi: 10.1111/hdi.12616 [DOI] [PubMed] [Google Scholar]
- 19.Poon CK, Tang HL, Wong JH, et al. Effect of alternate night nocturnal home hemodialysis on anemia control in patients with end-stage renal disease. Hemodial Int. 2015;19(2):235–241. doi: 10.1111/hdi.12227 [DOI] [PubMed] [Google Scholar]
- 20.Friesen T, Jassal DS, Zhu M, et al. Cardiovascular remodeling during long-term nocturnal home hemodialysis. Clin Exp Nephrol. 2015;19(3):514–520. doi: 10.1007/s10157-014-0992-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomson BK, Huang SH, Chan C, Urquhart B, Skanes A, Lindsay RM. Nocturnal home hemodialysis associates with improvement of electrocardiographic features linked to sudden cardiac death. ASAIO J. 2014;60(1):99–105. doi: 10.1097/MAT.0000000000000023 [DOI] [PubMed] [Google Scholar]
- 22.Klarenbach S, Tonelli M, Pauly R, et al. Economic evaluation of frequent home nocturnal hemodialysis based on a randomized controlled trial. J Am Soc Nephrol. 2014;25(3):587–594. doi: 10.1681/ASN.2013040360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blagg CR. Dialysis composite rate bundling: potential effects on the utilization of home hemodialysis, daily and nocturnal hemodialysis, and peritoneal dialysis. Semin Dial. 2011;24(6):674–677. doi: 10.1111/j.1525-139X.2011.00993.x [DOI] [PubMed] [Google Scholar]
- 24.Tennankore KK, Kim SJ, Chan CT. The feasibility of caregiver-assisted home nocturnal hemodialysis. Nephron Clin Pract. 2012;122(1–2):17–23. doi: 10.1159/000348419 [DOI] [PubMed] [Google Scholar]
- 25.Burton JO, Graham-Brown MPM. Nocturnal hemodialysis: an underutilized modality? Curr Opin Nephrol Hypertens. 2018;27(6):472–477. doi: 10.1097/MNH.0000000000000450 [DOI] [PubMed] [Google Scholar]
- 26.Zupancic T, Ponikvar R, Gubensek J, Buturovic-Ponikvar J. Phosphate removal during long nocturnal hemodialysis/hemodiafiltration: a study with total dialysate collection. Ther Apher Dial. 2016;20(3):267–271. doi: 10.1111/1744-9987.12435 [DOI] [PubMed] [Google Scholar]
- 27.Noori N, Yan AT, Kiaii M, et al. Nutritional status after conversion from conventional to in-centre nocturnal hemodialysis. Int Urol Nephrol. 2017;49(8):1453–1461. doi: 10.1007/s11255-017-1595-x [DOI] [PubMed] [Google Scholar]
- 28.Palmer BF, Henrich WL. Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol. 2008;19(1):8–11. doi: 10.1681/ASN.2007091006 [DOI] [PubMed] [Google Scholar]
- 29.Ronco C, Bonello M, Bordoni V, et al. Extracorporeal therapies in non-renal disease: treatment of sepsis and the peak concentration hypothesis. Blood Purif. 2004;22(1):164–174. [DOI] [PubMed] [Google Scholar]
- 30.Bugeja A, Dacouris N, Thomas A, et al. In-center nocturnal hemodialysis: another option in the management of chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(4):778–783. doi: 10.2215/CJN.05221008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li L, Tang X, Kim S, et al. Effect of nocturnal hemodialysis on sleep parameters in patients with end-stage renal disease: a systematic review and meta-analysis. PLoS One. 2018;13(9):e0203710. doi: 10.1371/journal.pone.0203710 [DOI] [PMC free article] [PubMed] [Google Scholar]