Abstract
In this study, we analyzed GPC family genes in colorectal cancer (CRC) and the possible mechanism of action of GPC1 in CRC. CRC patient data were extracted from The Cancer Genome Atlas, and the prognostic significance of GPC1 expression and its association with clinicopathological features were identified by Kolmogorov–Smirnov test. CRC patients with high GPC1 expression had poor overall survival compared with patients with low GPC1 expression. In vitro experiments demonstrated that knockdown of GPC1 significantly inhibited the proliferation and migration and promoted cell apoptosis in CRC cell lines. Gene Ontology analysis of differential genes indicated that GPC1 may influence the TGF-β1 signaling pathway. Additional experiments revealed that silencing GPC1 suppressed the levels of TGF-β1 and p-SMAD2 but increased the expression of SMAD2. Taken together, these findings suggest that GPC1 may function as a tumor promoter in CRC cells through promoting TGF-β signaling pathway. Our results also indicate that GPC1 may serve as a critical effector in CRC progression and a new potential target for CRC therapy.
Introduction
Colorectal cancer (CRC) is one of the most common cancers in the United States, with an estimated 147,950 and 53,200 new cases and deaths each year, respectively [1]. In 2015, an estimated 376,300 cases and 150,000 deaths occurred in China [2]. Approximately 20% of patients with CRC have metastatic CRC [3], and 40% of CRC patients exhibit recurrence after treated localized disease [4]. The prognosis of metastatic CRC is poor, with a 5-year survival rate of less than 20% [3]. Therefore, the identification of new markers and novel treatment methods for CRC is critical.
Glypicans (GPCs) are a family of heparan sulfate proteoglycans (HSPGs) that interact with the plasma membrane through a glycosylphosphatidyl inositol anchor [5]. In humans, six GPC family members have been identified, including GPC1, GPC2, GPC3, GPC4, GPC5 and GPC6 [6]. Melo et al. studied GPC1 expression in the peripheral blood of 190 patients with pancreatic ductal adenocarcinoma and 100 healthy volunteers and found that GPC1 was highly expressed in patients with cancer compared with the healthy volunteers; furthermore, larger tumors showed a higher positive rate of GPC1. Li et al. found that GPC1 regulates the occurrence of esophageal cancer through the PTEN/Akt/β-catenin signaling pathway [7]. In addition, the authors found that GPC1 can be used as a biomarker for the recurrence of stage III CRC, and GPC1 may be involved in EMT activation, invasion and migration of CRC cells [8]. Further studies revealed the increased expression of GPC1 in prostate cancer, endometrial cancer, lung cancer and other cancers [9–11]. However, the mechanism by which GPC1 regulates the occurrence and progression of CRC is still unclear.
In this study, we analyzed the influence of GPC family proteins in CRC and the possible mechanism of action. Our findings indicate that GPC1 expression was associated with prognosis in CRC patients and reveal that GPC1 promotes the TGF-β signaling pathway in CRC cells.
Materials and methods
Patients and specimens
Between January and February 2022, we collected 4 pairs of cancer and paracarcinoma tissues from patients with CRC at the Gastrointestinal Surgery Department of the First Affiliated Hospital of Bengbu Medical College. Our study was approved by the ethics committee of Bengbu Medical College. We obtained informed consent from every patient. All specimens were stored at − 80°C.
Data source
The expression profiles and clinicopathological data of CRC and non-tumor tissues were obtained from The Cancer Genome Atlas (TCGA, https://portal.gdc.cancer.gov/) [12]. The inclusion criteria for clinical information were set as follows: (1) patients had complete clinical information; and (2) the follow-up time of samples exceeded 30 days.
Analysis of TCGA mRNA profiles
We used the “limma” package to identify differentially expressed mRNAs between 473 CRC tissues and 41 non-tumor tissues from TCGA (|FDR|>1, P<0.05) [13]. The Kaplan–Meier method was used for univariate analysis, followed by log-rank test for assessing the differences of overall survival (OS) among different groups (P<0.05). Next, we assessed the correlation between GPC1 and clinicopathological information using Kolmogorov–Smirnov test (P<0.05). Finally, we identified the GPC1-related genes using Pearson’s correlation test (P<0.05, |R|>0.5). The STRING database (https://string-db.org/), a publicly available comprehensive resource, was used to predict the relationships between target genes.
Functional enrichment analysis
Gene Ontology (GO) enrichment analysis was performed using “clusterProfiler” package in R (4.1.0), and the “org.Hs.eg.db” package was used as the reference data. The P value was corrected by the Benjamin–Hochberg method, with a P value <0.05 and a q value <0.05 being the cut-off criteria.
Immunohistochemistry
Colorectal cancer and paracarcinoma tissues were dewaxed in xylene and rehydrated through different gradients of alcohol. Then, we placed paraffin in 3% H2O2 for 15 min at 22°C. Next, the slide was heated in citrate buffer. After washing several times with PBS (pH = 7.2), the slide was placed into the solution with a primary antibody against GPC1 (dilution 1:200, 16700-1-AP, Proteintech, China) at 4°C for more than 12 h. Then, we added secondary antibody at 22°C for 10 min. Finally, the slide was stained after the addition of 3,3′-diaminobenzidine (DAB) solution.
Cell culture and reagents
HCT116, SW480 cell lines were obtained from Cell Bank, Type Culture Collection, Chinese Academy of Sciences (Shanghai, China). All cells were cultured in DMEM (Gibco, USA) supplemented with 10% fetal bovine serum (Sigma-Aldrich, Australia) and penicillin-streptomycin (Invitrogen, USA) in a 90%–95% humidified atmosphere of 5% CO2 at 37°C.
siRNA-mediated gene silencing
SW480 and HCT116 cells were seeded in 6-well plates (2×105 cells/well) or 96-well plates (2×103 cells/well) 24 h before transfection. Two siRNAs designed to silence GPC1 and a control siRNA were obtained from Genepharma (Shanghai, China). The siRNA sequences are as follows: Control siRNA: 5′-UUCUCCGAACGUGUCACGUTT-3′; siGPC1#1: 5′-CCUGGAUAGUUAAGGGCUUTT-3′; and siGPC1#2: 5′-CCUUUCUGCCUUUUAAUUUTT-3′. siRNAs were transiently transfected into cells with Lipofectamine 8000 transfection reagent (Beyotime, Shanghai, China) according to the manufacturer’s instructions.
Cell proliferation assay
The CCK-8 Cell Counting Kit (Beyotime) was used to assess the proliferation of HCT116 and SW480 cells. Transfected cells were seeded in 96-well plates at a density of 2×104 cells/mL (100 μL/well) and incubated at 37°C with 5% CO2. On days 0 (at 48 h after transfection), 1, 2 and 3, CCK-8 reagent (10 μL) was added to cells and cells were incubated for 4–6 h. The optical density of the solution (OD450) in each well was measured by spectrophotometry (BioTek).
Apoptosis assay
The Annexin V-FITC Apoptosis Detection Kit (Beyotime, Shanghai, China) and a flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA) were used to evaluate the apoptosis of SW480 or HCT116 cells after transfection for 48 h. Briefly, cells were prepared into a 1×106 cells/mL cell suspension with 1 mL 1× Binding Buffer. Next, 200 μL of the cell suspension was mixed with 5 μL of Annexin V-FITC reagent in a centrifuge tube and the sample was mixed for 10 min in the dark at room temperature. PI reagent (5 μL) was then added to the centrifuge tube and samples were incubated in the dark at room temperature for 5 min. PBS was added to adjust the mixture to a final volume of 500 μL. After 30 min, the cells were evaluated by flow cytometry and the data were evaluated using CytoFLEX (Beckman Coulter) to calculate the number of apoptotic cells.
Cell cycle analysis
At 48 h after transfection, SW480 and HCT116 cells (2×106/ml) were collected, washed twice with PBS buffer and centrifuged at 1,000 × g for 5 min at 4°C. The supernatant was discarded and cells were fixed with ice-cold 70% ethanol for at 2 h at 4°C. The cells were centrifuged at 1,000 × g for 5 min at 4°C, washed twice with PBS and centrifuged again at 1,000 × g for 5 min at 4°C. The supernatant was discarded and cells were incubated with 50 μl RNase I (1 μg/ml; Beyotime, Shanghai, China) at 37°C for 1 h in the dark. Next, 200 μl propidium iodide (20 μg/ml) was added and the samples were held at room temperature for 20 min according to the manufacturer’s protocol.
Wound-healing assay
At 48 h after transfection, a sterilized 10-μL pipette tip was used to create a scratch in the monolayer of transfected CRC cells cultured in 6-well plates. After removing cell debris by washing with phosphate buffer saline (PBS), DMEM containing 2% FBS was added to each well and cells were cultured under 5% CO2 and 37°C for 48 h. The scratch width was measured at 0 h and 48 h using ImageJ software and an inverted optical microscope. The relative scratch width was calculated as the ratio of the scratch width at 48 h to the width at 0 h.
Transwell assay
At 24 h after transfection of CRC cells, 100 μL of cells (1×105 cells) were plated in serum-free DMEM medium in the top of a transwell chamber, and 600 μL of 20% DMEM medium was included in the bottom chamber. After 72 h of incubation under 37°C and 5% CO2, 99.99% methanol was used to fix the chamber, and 0.1% crystal violet was used for staining. A cotton swab was used to remove cells from the top chamber. Migrated cells were photographed and counted with an inverted optical microscope.
Real-time quantitative polymerase chain reaction (RT-qPCR)
Total RNA was isolated from CRC cells using TRizol reagent (Invitrogen, USA) according to the manufacturer’s instruction. Total RNAs were quantitatively analyzed and reverse-transcribed using a reverse transcription kit (PrimeScript RT Reagent Kit, RR047A, TaKaRa, Japan) to synthesize cDNAs. RT-qPCR was performed using a real-time quantitative PCR kit (A46113, Applied Biosystems, USA) on a QuantStudio 3 Real-Time PCR System (Thermo Fisher, USA). Each sample was run in triplicate. The sequences of primers used are listed in Table 1. The expression of target genes was calculated by the 2−ΔΔCt method [10]. GAPDH mRNA was used as a housekeeping gene for normalization of gene expression.
Table 1. Sequences of primers for qRT-PCR.
| ID | Forward sequence(5′-3′) | Reverse sequence(5′-3′) |
|---|---|---|
| GPC1 | TGAAGCTGGTCTACTGTGCTC | CCCAGAACTTGTCGGTGATGA |
| GAPDH | AGATCCCTCCAAAATCAAGTGG | GGCAGAGATGATGACCCTTTT |
| TGF-β1 | CTAATGGTGGAAACCCACAACG | TATCGCCAGGAATTGTTGCTG |
| SMAD2 | TCATAGCTTGGATTTACAGCCAG | TTCTACCGTGGCATTTCGGTT |
| SMAD3 | TGGACGCAGGTTCTCCAAAC | CCGGCTCGCAGTAGGTAAC |
Western blotting
SW480, and HCT116 cells were lysed using RIPA buffer (Beyotime, Shanghai, China). Equal amounts of protein were separated by 10% SDS–PAGE and electrophoretically transferred to a PVDF membrane (Millipore, Billerica, MA, USA). The membrane was blocked with 5% non-fat milk for 2 h of blocking and then incubated with primary antibodies for 12 h at 4°C. After three washes, the membranes were incubated with secondary antibodies (1:5000) for 4 h followed by washing with TBST washing buffer. The protein bands were visualized using BeyoECL Star (Beyotime) and BIO-RAD Gel Doc XR+ (USA) and Image J software were used to analyze protein bands. The primary antibodies used are as follows: primary antibodies against GPC1 (1:1000, 16700-1-AP, Proteintech); TGF-β1 (1:1000, 21898-1-AP, Proteintech); SMAD2 (1:1000, 12570-1-AP, Proteintech); and p-SMAD2 (1:1000, ABP50459, abbkine).
Statistical analysis
Log-rank test was used to compare the Kaplan–Meier survival curves between high and low expression of GPC1, and the median was used as cutoff. P<0.05 indicated statistical significance.
Results
Elevated expression of GPC1 is positively associated with the survival, disease stage and TNM stage of CRC patients
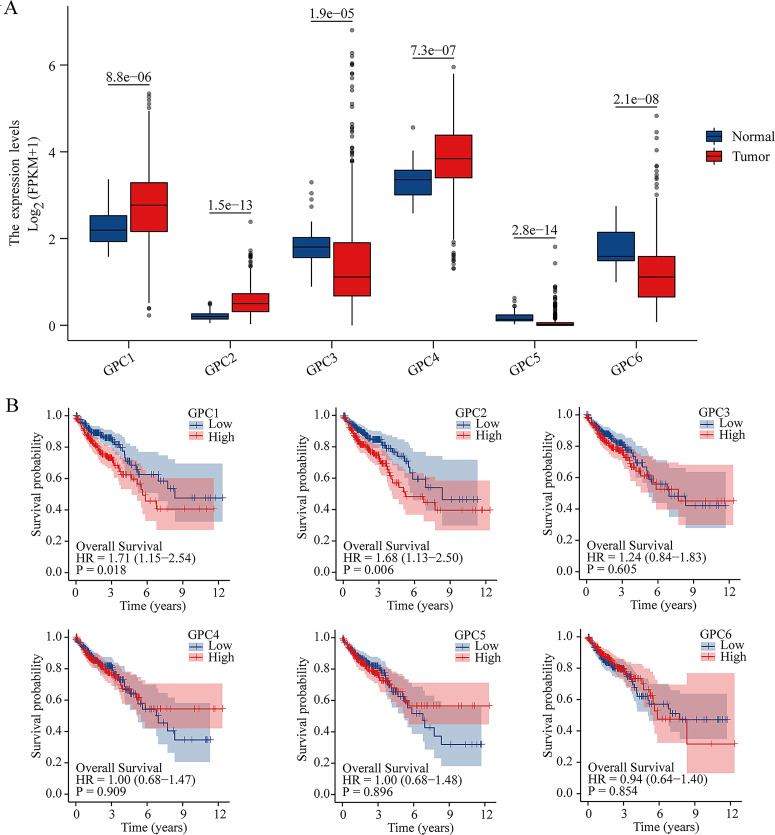
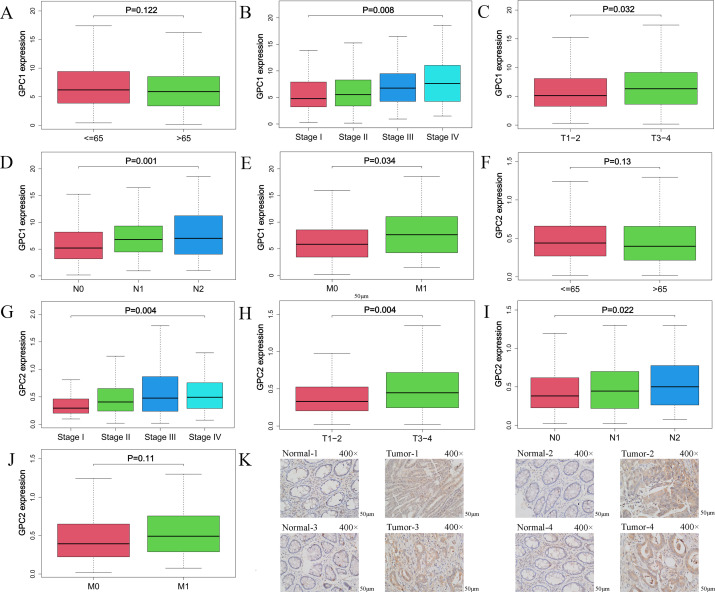
We analyzed the mRNA expression of GPCs in CRC and non-tumor tissues from TCGA database using the “limma” and “survival” program packages of R software. The results showed that the expressions of GPC1 and GPC2 were higher (P<0.001) in CRC tissues than non-tumor tissues (Fig 1A). Furthermore, Kaplan–Meier analysis revealed that high expression of GPC1 and GPC2 were associated with shorter (P<0.01) overall survival in CRC patients (log-rank test) (Fig 1B). We also found that GPC1 expression was lower (P<0.01) in early stage tumors (stage I or II, T1–2, N0 or N1, M0) than in late stage tumors (stage III or IV, T3–4, N2, M1) (Fig 2A–2E) (S1 Table). GPC2 expression was lower (P<0.05) in early stage tumors (stage I or II, T1–2, N0 or N1) than in late stage tumors (stage III or IV, T3–4, N2). There were significant differences of GPC2 expression in M0 and M1 stage (P>0.05) (Fig 2F–2J and S1 Table). In addition, compared with that in paracarcinoma tissues, the protein expression of GPC1 in tumour tissues was elevated (Fig 2K). These results indicate that CRC patients with a high expression of GPC1 had a poor prognosis. Furthermore, GPC1 may function as an oncogene in the tumorigenesis and development of CRC and may also serve as a potential molecular marker for diagnosis and prognosis prediction for CRC.
Fig 1. Differential expression of GPC family genes in colorectal cancer (CRC) patients.
(A). Gene expression of six GPC family members in cancer tissues (473 samples) and non-tumor tissues (41 samples) in CRC patients (TCGA) using Student’s t test. Blue indicates non-tumor tissues, and red indicates CRC tissues. (B). Kaplan–Meier analysis revealed that CRC patients (453 samples, TCGA) with high GPC1 expression (225 samples, TCGA) and high GPC2 expression (225 samples, TCGA) had a poor prognosis compared with patients with low GPC1 and GPC2 expression.
Fig 2. Elevated expression of GPC1 is associated with clinicopathological features of CRC.
(A–J). GPC1 and GPC2 mRNA expression analysis in TCGA CRC samples (453 samples) by age, stage, T, N and M using Kolmogorov–Smirnov test. (K). Immunohistochemical staining for GPC1 in CRC tissues and normal tissues.
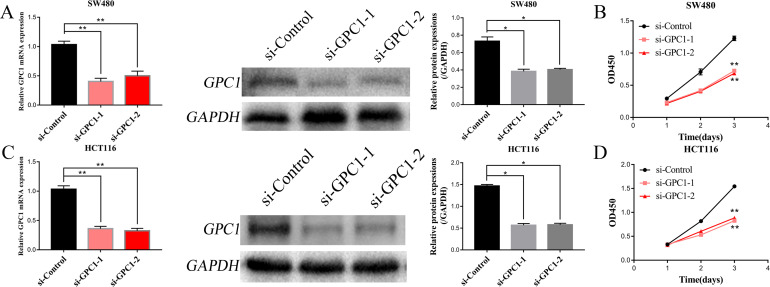
SiRNA-mediated GPC1 gene silencing significantly inhibits cell growth, induces cell cycle arrest, and promotes apoptosis of CRC cells
To explore the role of GPC1 in CRC cells, we performed siRNA-mediated gene silencing of GPC1 (si-GPC1-1 and si-GPC1-2). qRT-PCR and western blot analysis were conducted to measure GPC1 mRNA and protein expression in HCT116 and SW480 cell lines at 48 and 72 h after transfection. GPC1 mRNA expression levels were knocked down by up to 60% with si-GPC-1-1 and si-GPC1-2. We then evaluated the effects of GPC1 silencing on cell proliferation using the CCK-8 assay. The results showed that silencing GPC1 significantly (P<0.05) inhibited the proliferation of HCT116 and SW480 CRC cells compared with cells transfected with control siRNA (Fig 3A–3D).
Fig 3. Silencing GPC1 inhibits CRC cell proliferation.
(A, C). CRC cell lines were transfected with siRNA targeting GPC1, and silencing efficiency at the mRNA and protein levels was determined. (B, D). Cell proliferation was inhibited in SW480 and HCT116 cells by silencing GPC1. * p<0.05, ** p<0.01.
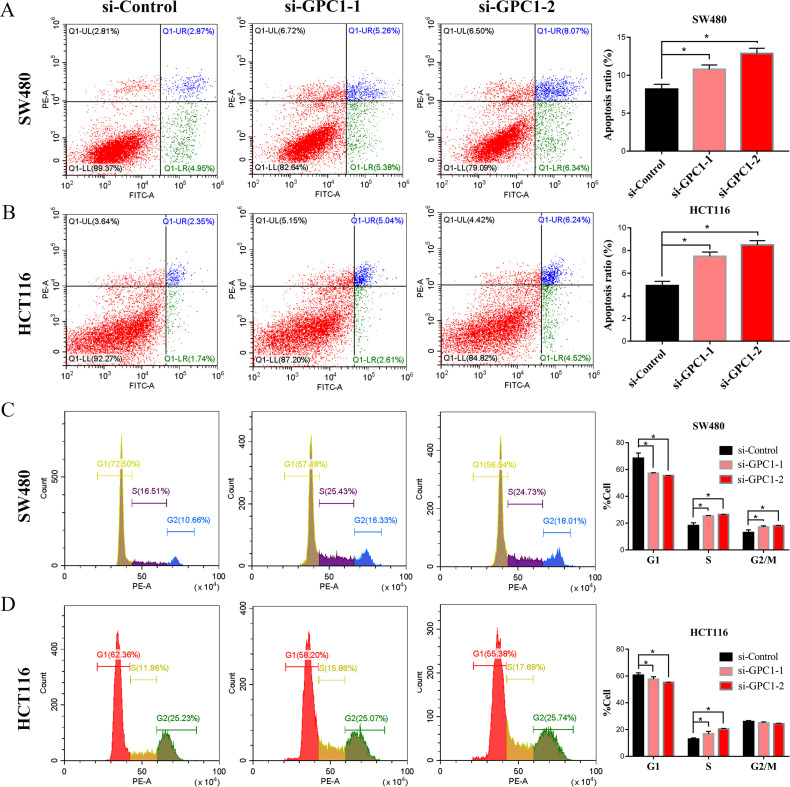
To further study the biological function of GPC1 in the development of CRC, we evaluated the effect of GPC1 silencing on the cell cycle and apoptosis of CRC cells by flow cytometry assay. Knockdown of GPC1 significantly (P<0.05) induced apoptosis and cell cycle arrest at the S phase in SW480 and HCT116 cells (Fig 4A–4D). These results indicated that silencing GPC1 inhibits cell growth, induces S phase arrest and promotes apoptosis of CRC cells.
Fig 4. Knockdown of GPC1 induces apoptosis and S phase cell cycle arrest in CRC cells.
(A, B). GPC1 silencing promoted SW480 and HCT116 cell apoptosis. (C, D). Knockdown of GPC1 induced S cell cycle arrest in SW480 and HCT116 cells. * p<0.05.
Silencing GPC1 significantly reduces cell migration ability in CRC cells in vitro
To further investigate the role of GPC1 in CRC, cell motility was assessed by wound healing and transwell migration assays. In wound healing assays, cells with GPC1 knockdown showed reduced migration compared with control cells in SW480 and HCT116 cell lines (Fig 5A and 5B). Similarly, transwell migration assay indicated that GPC1 knockdown significantly (P<0.01) impaired cell migration ability in SW480 and HCT116 cells (Fig 5C and 5D). These results showed that silencing GPC1 impairs cell migration activity in CRC cells, further implying an important role for GPC1 in the progression of CRC.
Fig 5. Silencing GPC1 significantly reduces cell migration ability in CRC cells.
(A, B). Knockdown of GPC1 significantly inhibited wound healing in SW480 and HCT116 cell lines. (C, D). Silencing GPC1 significantly impaired the cell migration in SW480 and HCT116 cell lines. ** p<0.01.
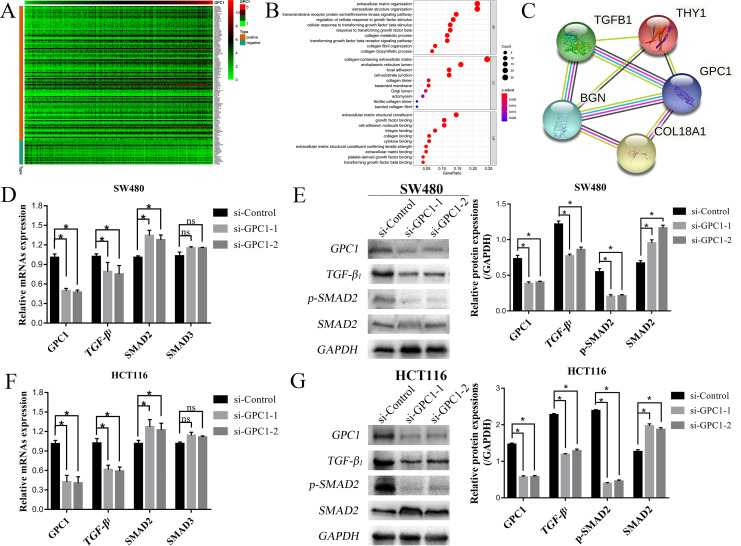
GPC1 regulates the TGF-β1/SMAD2 signaling pathway
To explore the mechanism underlying the involvement of GPC1 in CRC, we first analyzed the possible signaling pathways mediated by GPC1 by bioinformatics assay using “limma” bioconductor to identify the RNAs related to GPC1. The GPC1-related RNAs are shown in a heatmap in Fig 6A. Next, we used GO enrichment analysis on the target genes that were screened (Fig 6B). We then predicted the relationships between GPC1-related target genes (Fig 6C). Two different bioinformatics analyses indicated that GPC1 may regulate the TGF-β1 signaling pathway in CRC cells (Fig 6B and 6C), which is consistent with our previous findings [14]. Notably, previous studies showed that the TGF-β signaling pathway is involved in the occurrence and development of CRC [15].
Fig 6. Pathway enrichment analysis and TGF-β signaling pathway identification in CRC.
(A). Correlations between GPC1 and target genes in CRC. (B). GO analysis showed that the TGF-β signaling pathway was enriched in CRC. (C). The correlation-target network for GPC1. (D–G). GPC1-associated mRNAs and proteins were examined by qRT-PCR and western blot analysis in SW480 and HCT116 cell lines after silencing GPC1.
To confirm the results of the bioinformatics analysis, we explored the effect of GPC1 silencing on the expression of TGF-β1 signaling pathway–related molecules such as SMAD1 and SMAD2 by qRT-PCR. TGF-β1 and SMAD2 mRNAs were significantly down-regulated and up-regulated, respectively, in HCT116 and SW480 cells after the silencing of GPC1 expression (Fig 6D and 6F). We then evaluated the effects of GPC1 silencing on the protein levels of TGF-β1, SMAD2 and p-SMAD2 by western blot assay. The results showed that the levels of TGF-β1 and p-SMAD2 proteins were significantly down-regulated, and the expression of SMAD2 protein was significantly up-regulated in HCT116 and SW480 cells following the silencing of GPC1 expression (Fig 6E and 6G). Together these results suggest that GPC1 may be involved in the proliferation, apoptosis and migration of CRC cells through regulating the TGF-β1/SMAD2 signaling pathway.
Discussion
With the development of bioinformatics, several key genes that play an important role in the occurrence and development of CRC have been identified [16]. In this study, we analyzed the gene expression of the GPC family in CRC. GPCs belong to the HSPG family and interact with a variety of protein ligands, proteases, cytokines, chemokines, adhesion molecules and ECM proteins, thereby producing a variety of structures and signal transduction functions [17]. HSPG proteins exhibit functions in a wide range of biological processes, such as development, hemostasis control, and inflammation, and are associated with cell survival [18]. In addition, HSPG proteins are involved in cell adhesion, movement, proliferation, differentiation and apoptosis [14] and thus have been linked to the enhancement of malignant diseases.
In this study, we found that high expression of GPC1 was significantly related to the poor prognosis of patients with CRC. This finding is consistent with previous reports [19]. Several studies demonstrated that GPC1 is involved in the formation and development of different types of tumors [20, 21]. Experimental studies revealed that the expression of GPC1 was significantly increased in the extracellular vesicles released by the mouse MC38 CRC cell line [22]. In addition, TMT-MS methods to study crEV in patients with CRC found that GPC1 can be used as a biomarker for the detection of early CRC [23].
A previous study using bioinformatics analysis showed that GPC1 may participate in the occurrence and development of CRC through the glycolytic pathway [23]. Other analyses found that GPC1 may be involved in CRC development through influencing intestinal tumor hypoxia on immune cells in the tumor microenvironment [24]. However, these findings have not been verified by experiments and the precise mechanism by which GPC1 participates in the regulation of CRC is still unclear. In this study, our in vitro experiments revealed that GPC1 gene silencing in the HCT116 and SW480 CRC cell lines resulted in inhibition of cell proliferation, S phase cycle arrest, induction of apoptosis and reduced migration of CRC cells. We further showed that GPC1 may be involved in the occurrence and development of CRC by activating the TGF-β/SMAD2 signaling pathway. Decreased GPC1 expression suppresses pancreatic cancer cell growth by modifying TGF-β signaling [25]. GPC1 has been shown to interact with TGF-β and its receptors to stabilize their assembly for enhanced Smad signaling. Downregulation of GPC1 expression resulted in a slightly altered response toward TGF-β1, activin-A, and BMP2 in terms of growth, p21 induction, and Smad2 phosphorylation, ultimately leading to decreased anchorage-independent growth of T3M4 and PANC-1 cells.
GPC3 also promotes the growth of liver cancer cells and may regulate the TGF-β signaling pathway [26]. The human TGF-β family includes 33 genes that encode for homodimeric or heterodimeric secreted cytokines [27, 28]. These proteins are involved in a variety of biological processes, including proliferation, differentiation, migration, apoptosis and adhesion [29]. Dysregulation of TGF-β signaling frequently occurs in CRC [30]. TGF-β signaling is initiated through binding of the TGF-β ligand to the receptor, which in turn phosphorylates the downstream target SMAD2/3 [31, 32]. Phosphorylated SMAD2/3 enters the nucleus with the help of SMAD4 and cofactors and acts as a transcription factor to induce gene expression, including the expression of EMT-related genes [33, 34]. EMT has been shown to affect cancer cell migration [31]. The TGF-β/SMAD2/3 signaling pathway has been shown to affect the cell proliferation, survival, differentiation, apoptosis and migration of CRC [35–37]. The mechanism of S phase arrest and apoptosis induced by GPC1 silencing requires further investigation.
Future studies should verify our results using larger numbers of clinical specimen and more in-depth research is required into the mechanism by which GPC1 functions in CRC. In addition, animal models will be required to elucidate how GPC1 affects the occurrence and development of CRC in vivo. Our results suggest that GPC1 may be a prognostic marker and a new therapeutic target for CRC.
Supporting information
(A) Significantly high expression of GPC1 mRNA in colon adenocarcinoma (COAD), breast invasive carcinoma (BRCA), cholangiocarcinoma (CHOL), esophageal carcinoma (ESCA), head and neck squamous cell carcinoma (HNSC), kidney renal papillary cell carcinoma (KIRP), lung squamous cell carcinoma (LUSC), skin cutaneous melanoma (SKCM), stomach adenocarcinoma (STAD). (B) GPC1 mRNA expression levels in different cancer cell lines.
(TIF)
GPC1 is significantly enriched in the TGF-β signaling pathway.
(TIF)
(DOCX)
Note: Survival analysis was performed by Kaplan–Meier test, and correlation analysis of clinicopathological characteristics was performed by Kolmogorov-Smirnov test; the numbers in the table represent the P value of the correlation analysis.
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank Gabrielle White Wolf, PhD, from Liwen Bianji (Edanz) (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
LF and LM both are funded by the following: Anhui Natural Science Foundation under Grand (No. 2108085MH291), and the 512 Talent Cultivation Plan for subject leader of Bengbu Medical College (by51201107). LF and WH both are funded by the following: Anhui Natural Science Foundation under Grand (1908085MH257). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2.Zheng RS, Sun KX, Zhang SW, Zeng HM, Zou XN, Chen R, et al. [Report of cancer epidemiology in China, 2015]. Zhonghua zhong liu za zhi [Chinese journal of oncology]. 2019;41(1):19–28. [DOI] [PubMed] [Google Scholar]
- 3.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. doi: 10.3322/caac.21654 [DOI] [PubMed] [Google Scholar]
- 4.Kahi CJ, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, et al. Colonoscopy Surveillance After Colorectal Cancer Resection: Recommendations of the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2016;150(3):758-68.e11. [DOI] [PubMed] [Google Scholar]
- 5.Li N, Gao W, Zhang YF, Ho M. Glypicans as Cancer Therapeutic Targets. Trends in cancer. 2018;4(11):741–54. doi: 10.1016/j.trecan.2018.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fransson LA. Glypicans. The international journal of biochemistry & cell biology. 2003;35(2):125–9. doi: 10.1016/s1357-2725(02)00095-x [DOI] [PubMed] [Google Scholar]
- 7.Li J, Chen Y, Zhan C, Zhu J, Weng S, Dong L, et al. Glypican-1 Promotes Tumorigenesis by Regulating the PTEN/Akt/β-Catenin Signaling Pathway in Esophageal Squamous Cell Carcinoma. Digestive diseases and sciences. 2019;64(6):1493–502. doi: 10.1007/s10620-019-5461-9 [DOI] [PubMed] [Google Scholar]
- 8.Li J, Chen Y, Guo X, Zhou L, Jia Z, Peng Z, et al. GPC1 exosome and its regulatory miRNAs are specific markers for the detection and target therapy of colorectal cancer. Journal of cellular and molecular medicine. 2017;21(5):838–47. doi: 10.1111/jcmm.12941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang ZH, Zhang YZ, Wang YS, Ma XX. Identification of novel cell glycolysis related gene signature predicting survival in patients with endometrial cancer. Cancer cell international. 2019;19:296. doi: 10.1186/s12935-019-1001-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiong L, Li X, Chen D, Li S, Luo L. GPC1-ALK: A novel ALK fusion in a patient with pulmonary sarcomatoid carcinoma. Lung cancer (Amsterdam, Netherlands). 2021;151:104–5. [DOI] [PubMed] [Google Scholar]
- 11.Quach ND, Kaur SP, Eggert MW, Ingram L, Ghosh D, Sheth S, et al. Paradoxical Role of Glypican-1 in Prostate Cancer Cell and Tumor Growth. Sci Rep. 2019;9(1):11478. doi: 10.1038/s41598-019-47874-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choe EK, Lee S, Kim SY, Shivakumar M, Park KJ, Chai YJ, et al. Prognostic Effect of Inflammatory Genes on Stage I-III Colorectal Cancer-Integrative Analysis of TCGA Data. Cancers (Basel). 2021;13(4). doi: 10.3390/cancers13040751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu CY, Uen YH, Tsai HL, Chuang SC, Hou MF, Wu DC, et al. Molecular detection of persistent postoperative circulating tumour cells in stages II and III colon cancer patients via multiple blood sampling: prognostic significance of detection for early relapse. Br J Cancer. 2011;104(7):1178–84. doi: 10.1038/bjc.2011.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu F., Shi WJ., Wen HX., Wu HZ. & Liu Ml. Bioinformatics analysis of GPC1 regulating the progression and prognosis of colorectal cancer. Journal of gannan medical university. 2021;41(03):241–50. [Google Scholar]
- 15.Wu N, Jiang M, Liu H, Chu Y, Wang D, Cao J, et al. LINC00941 promotes CRC metastasis through preventing SMAD4 protein degradation and activating the TGF-β/SMAD2/3 signaling pathway. Cell Death Differ. 2021;28(1):219–32. doi: 10.1038/s41418-020-0596-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Nicolantonio F, Vitiello PP, Marsoni S, Siena S, Tabernero J, Trusolino L, et al. Precision oncology in metastatic colorectal cancer—from biology to medicine. Nature reviews Clinical oncology. 2021;18(8):506–25. doi: 10.1038/s41571-021-00495-z [DOI] [PubMed] [Google Scholar]
- 17.Christianson HC, Belting M. Heparan sulfate proteoglycan as a cell-surface endocytosis receptor. Matrix biology: journal of the International Society for Matrix Biology. 2014;35:51–5. doi: 10.1016/j.matbio.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 18.Rosen SD, Lemjabbar-Alaoui H. Sulf-2: an extracellular modulator of cell signaling and a cancer target candidate. Expert opinion on therapeutic targets. 2010;14(9):935–49. doi: 10.1517/14728222.2010.504718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu J, Wang S, Bai H, Wang K, Hao J, Zhang J, et al. Identification of Five Glycolysis-Related Gene Signature and Risk Score Model for Colorectal Cancer. Front Oncol. 2021;11:588811. doi: 10.3389/fonc.2021.588811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li X, Nie S, Lv Z, Ma L, Song Y, Hu Z, et al. Overexpression of Annexin A2 promotes proliferation by forming a Glypican 1/c-Myc positive feedback loop: prognostic significance in human glioma. Cell Death Dis. 2021;12(3):261. doi: 10.1038/s41419-021-03547-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grillo PK, Győrffy B, Götte M. Prognostic impact of the glypican family of heparan sulfate proteoglycans on the survival of breast cancer patients. Journal of cancer research and clinical oncology. 2021;147(7):1937–55. doi: 10.1007/s00432-021-03597-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papiewska-Pająk I, Krzyżanowski D, Katela M, Rivet R, Michlewska S, Przygodzka P, et al. Glypican-1 Level Is Elevated in Extracellular Vesicles Released from MC38 Colon Adenocarcinoma Cells Overexpressing Snail. Cells. 2020;9(7). doi: 10.3390/cells9071585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen S, Cao G, Wu W, Lu Y, He X, Yang L, et al. Mining novel cell glycolysis related gene markers that can predict the survival of colon adenocarcinoma patients. Biosci Rep. 2020;40(8). doi: 10.1042/BSR20201427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang L, Wang S, Wang Y, Zhao W, Zhang Y, Zhang N, et al. Effects of Hypoxia in Intestinal Tumors on Immune Cell Behavior in the Tumor Microenvironment. Frontiers in immunology. 2021;12:645320. doi: 10.3389/fimmu.2021.645320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kayed H, Kleeff J, Keleg S, Jiang X, Penzel R, Giese T, et al. Correlation of glypican-1 expression with TGF-beta, BMP, and activin receptors in pancreatic ductal adenocarcinoma. International journal of oncology. 2006;29(5):1139–48. [PubMed] [Google Scholar]
- 26.Sun CK, Chua MS, He J, So SK. Suppression of glypican 3 inhibits growth of hepatocellular carcinoma cells through up-regulation of TGF-β2. Neoplasia (New York, NY). 2011;13(8):735–47. doi: 10.1593/neo.11664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Derynck R, Budi EH. Specificity, versatility, and control of TGF-β family signaling. Science signaling. 2019;12(570). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heldin CH, Moustakas A. Signaling Receptors for TGF-β Family Members. Cold Spring Harbor perspectives in biology. 2016;8(8). doi: 10.1101/cshperspect.a022053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jung B, Staudacher JJ, Beauchamp D. Transforming Growth Factor β Superfamily Signaling in Development of Colorectal Cancer. Gastroenterology. 2017;152(1):36–52. doi: 10.1053/j.gastro.2016.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chittenden TW, Howe EA, Culhane AC, Sultana R, Taylor JM, Holmes C, et al. Functional classification analysis of somatically mutated genes in human breast and colorectal cancers. Genomics. 2008;91(6):508–11. doi: 10.1016/j.ygeno.2008.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shi Y, Massagué J. Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell. 2003;113(6):685–700. doi: 10.1016/s0092-8674(03)00432-x [DOI] [PubMed] [Google Scholar]
- 32.Souchelnytskyi S, Rönnstrand L, Heldin CH, ten Dijke P. Phosphorylation of Smad signaling proteins by receptor serine/threonine kinases. Methods in molecular biology (Clifton, NJ). 2001;124:107–20. doi: 10.1385/1-59259-059-4:107 [DOI] [PubMed] [Google Scholar]
- 33.Massagué J. TGFβ signalling in context. Nature reviews Molecular cell biology. 2012;13(10):616–30. doi: 10.1038/nrm3434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhu S, Zhang J, Xu F, Xu E, Ruan W, Ma Y, et al. IGFBP-rP1 suppresses epithelial-mesenchymal transition and metastasis in colorectal cancer. Cell Death Dis. 2015;6(3):e1695. doi: 10.1038/cddis.2015.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horbelt D, Denkis A, Knaus P. A portrait of Transforming Growth Factor β superfamily signalling: Background matters. The international journal of biochemistry & cell biology. 2012;44(3):469–74. doi: 10.1016/j.biocel.2011.12.013 [DOI] [PubMed] [Google Scholar]
- 36.Kitisin K, Saha T, Blake T, Golestaneh N, Deng M, Kim C, et al. Tgf-Beta signaling in development. Science’s STKE: signal transduction knowledge environment. 2007;2007(399):cm1. doi: 10.1126/stke.3992007cm1 [DOI] [PubMed] [Google Scholar]
- 37.Ikushima H, Miyazono K. TGFbeta signalling: a complex web in cancer progression. Nat Rev Cancer. 2010;10(6):415–24. doi: 10.1038/nrc2853 [DOI] [PubMed] [Google Scholar]