Abstract
Background
Cerebral palsy (CP) in children is a predominantly congenital developmental disease with complex causes and diverse symptoms. Chinese medicine mainly uses acupuncture for the treatment of CP; as the disease site is in the brain, emphasis is placed on scalp acupuncture therapy. There were studies about the treatment but different studies had very different results. In this study, we performed a systematic review and meta-analysis of the recent reports on scalp acupuncture in the treatment of CP in children, providing evidence for clinical diagnosis and treatment.
Methods
The databases of PubMed, Chinese Biomedical Literature (CBM), China National Knowledge Infrastructure (CNKI), and VIP were searched for randomized controlled trials (RCTs) on scalp acupuncture treatment of pediatric CP published from January 2000 to December 2021. The inclusion criteria of studies were made according to the Participants, Intervention, Control, Outcomes, Study design (PICOS) principles. The Cochrane risk of bias 2.0 was used to evaluate the bias of the included literature. Meta-analysis was performed using the effective rate, Mental Development Index (MDI), Psychological Development Index (PDI), and Gross Motor Function Measure (GMFM-88 scale) as outcome indicators for the efficacy, and the safety of scalp acupuncture was assessed.
Results
Initially, 332 articles were retrieved; after screening, 11 articles were included in the selection, including a total of 731 children, with 369 and 362 children for the experimental group and control group respectively. Meta-analysis showed that scalp acupuncture significantly improved the symptoms of children with CP [odds ratio (OR) =3.73, 95% confidence interval (CI): 2.49–5.58, Z=6.41, P<0.00001], could significantly improve their mental development [mean difference (MD) =15.58, 95% CI: 11.74–19.43, Z=7.95, P<0.00001] and psychological development (MD =13.23, 95% CI: 6.17–20.28, Z=3.67, P=0.0002) of children, and significantly improved the motor ability of CP children (MD =17.45, 95% CI: 8.19–26.72, Z=3.69, P=0.0002).
Discussion
The curative effect of scalp acupuncture is better than that of conventional rehabilitation. Scalp-based acupuncture therapy can effectively improve the symptoms of pediatric CP, promote the mental and psychological development of children, and improve their gross motor function, the treatment is safe.
Keywords: Scalp acupuncture, acupuncture, cerebral palsy (CP), meta-analysis
Introduction
Pediatric cerebral palsy (CP) refers to the situation when within 1 month after birth, internal brain development does not reach the normal level, and various symptoms of central nervous system disorders occur, such as intellectual disability, epilepsy, behavioral abnormalities, mental disorders, and visual, auditory, and language disorders (1). The causes of pediatric CP are ascribed to a variety of factors before, during, and after delivery. Alcoholism, drug abuse, and mental illness while pregnant; diabetes, hypertension, placenta previa, threatened abortion, placental dysplasia, and other diseases during pregnancy; or postpartum pneumonia infection, hypoxic-ischemic encephalopathy, and malnutrition may lead to pediatric CP (termed simply CP from here on) (2). Drug treatment of this disease usually involves cranial neurotrophic drugs, muscle relaxants, and blood-activating drugs to supply various amino acids required for brain tissue repair and regeneration, reconstruct and repair brain tissue, protect nerve cells, promote the consumption of oxygen by brain cells, improve brain cell energy metabolism, accelerate nerve excitation conduction, and improve learning and memory function (3). However, because CP is a congenital developmental disease, the causes of the disease are complex and the symptoms are diverse; there is still no specific drug treatment, and it remains necessary to incorporate rehabilitation training in comprehensive treatment, including exercise therapy, massage, language training, hydrotherapy, acupuncture, and so on. Traditionally, Chinese medicine for the treatment of CP is mainly based on acupuncture, and as the site of disease is in the brain, scalp acupuncture therapy is the most important, with different local parts of the body incorporated into acupuncture treatment according to the different symptoms of children (4). A study by Luo et al. (5) showed that scalp acupuncture can improve balance function of children with spastic hemiplegia better than routine rehabilitation training alone. However, another randomized controlled trial (RCT) by Wu et al. (6) showed that acupuncture treatment for cerebral palsy could not change the seizure frequency during intervention. To evaluate the clinical efficacy and safety of acupuncture and moxibustion in the treatment of pediatric CP, we conducted this meta-analysis to fully explore this topic. We present the following article in accordance with the PRISMA reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-85/rc).
Methods
Inclusion criteria
We established the inclusion criteria according to the Participants, Intervention, Control, Outcomes, Study design (PICOS) standard: (I) study type: all included studies were RCTs, unrestricted by the number of centers involved, there was no limitation on the allocation concealment method and blind method of the study (although all studies were subjected to quality and bias evaluation), and language was restricted to Chinese and English; (II) participants: all study participants were children under 10 years of age, with a clinical diagnosis of CP, and the clinical classification could be divided into spastic type, hypotonia type, balance ability disorder type, and mixed type, with combined symptoms including motor dysfunction and postural abnormalities, intellectual disability, convulsions, behavioral abnormalities, salivation, and language impairment. We excluded studies of an experimental nature (non-clinical) in which scalp acupuncture was applied to animals such as rats and dogs; (III) intervention measures: all studies were divided into a control group and experimental group for intervention. The 2 groups of children needed to have received the same basic treatment, including drug treatment (brain activin, growth and development promoting factor) and educational methods. The control group was given conventional rehabilitation therapy, including active or passive limb movement, language training, perception guidance, and limb coordination training. The experimental group was given scalp acupoint acupuncture treatment on the basis of control group interventions. We did not exclude cases where acupuncture was supplemented with other treatment means (such as massage, moxibustion, tongue acupuncture, body acupuncture), but scalp acupuncture was the main intervention; we did not exclude literature that contained other cohorts or groups (such as muscle acupoint injection drug treatment), but such interventions were not included in the final data statistics and analysis. (IV) Outcome indicators: (i) efficacy indicators: we interpreted the treatment response rate as the efficacy index, response rate = (significantly effective number + effective number)/total number of cases. There is no fixed cure standard for CP disease, so clinical studies mostly evaluate the efficacy with the improvement of symptoms (some studies also use the improvement of children’s intelligence as the significant effect standard), but the complications of CP are diverse, so the significant effect standard is also different, which could produce heterogeneity. If the final results showed heterogeneity, we tried to investigate the source of heterogeneity; (ii) intelligence improvement: the Mental Development Index (MDI) and Psychological Development Index (PDI) were used as the evaluation criteria for children’s intellectual improvement; (iii) motor ability: the Gross Motor Function Measure [GMFM-88 Scale (7)] was used as the evaluation criteria for children’s motor ability, which has a total of 88 items. The motor ability of the children was assessed from the perspectives of movement, reflex, balance, climbing, and hand-eye coordination, with a maximum score of 264 points, the higher the score, the better the motor function; (iv) safety: we used adverse events rate as the safety indicator including bleeding, subcutaneous hematoma, tendon, muscle strain, fever, secondary infection, organ injury. (V) Observation time: 3–6 courses of treatment were used as the criterion.
Literature search
(I) Search strategy: a broad range keyword search was performed with the search terms “Scalp acupuncture” AND “cerebral palsy”; (II) databases: we searched the databases of search PubMed, China Biomedical Literature (CBM), China National Knowledge Infrastructure (CNKI), and VIP; (III) filter setting: we performed a computer search for the database with filter settings on the search website, literature type (RCT).
Selection of literatures
After 2 researchers had independently completed the retrieval, data were entered into EndNote X9 software (Clarivate Analytics, Spring Garden, PA, USA) for subsequent management. Using the de-duplication function of the software, duplicate documents were eliminated, and the title, abstract, and full text of the articles were read. The unqualified articles were excluded. In case of any dispute in this process, a third person was invited to arbitrate after discussion.
Data extraction and conversion
After completing the literature screening, 2 researchers read the full texts again; the characteristic information of articles (author, publication time, study site), participant information (gender, age, weight, height), information of intervention measures (number of patients in groups, intervention methods), and outcome information (outcome indicators) were extracted.
Literature risk of bias assessment
The risk of bias assessment was performed by Cochrane RoB 2.0 for each study from 5 aspects: (I) randomization process; (II) deviations from intended interventions; (III) missing outcome data; (IV) measurement of the outcome; (V) selection of the reported result. Each aspect was given an assessment result of 3 levels: “low risk of bias”, “some concerns”, and “high risk of bias”. The overall bias was assessed with also the 3 levels.
Statistical methods
(I) The software RevMan 5.4 was used for statistical analysis; (II) standardized mean difference (SMD) effect size and 95% confidence interval (CI) were used for continuous indicators, and odds ratio (OR) effect size and 95% CI were used for discrete indicators (dichotomization), with P<0.05 indicating statistical significance; (III) Mantel-Haenszel model was used for each primary outcome indicator (response rate, MDI, PDI, PMFM-88 Score); (IV) forest plot was used to display the effect size; (V) I2 analysis and Q were used to check the heterogeneity of literatures. Where I2>50% or P<0.1, heterogeneity was indicated, and the random effects model was used; otherwise the fixed effects model was used. Mantel-Haenszel model was used for OR effect size, and inverse model was used for SMD effect size; (VI) if heterogeneity was detected between articles, the heterogeneity was investigated, and if the source of heterogeneity could not be determined, only descriptive analysis was conducted; perform subgroup analysis; (VII) sensitivity analysis was performed on the results; if there was no heterogeneity between articles, the results of fixed effects and random effects models were compared to judge whether the results of meta-analysis were stable; (VIII) funnel plot was used to represent publication bias.
Results
Literature screening process and results
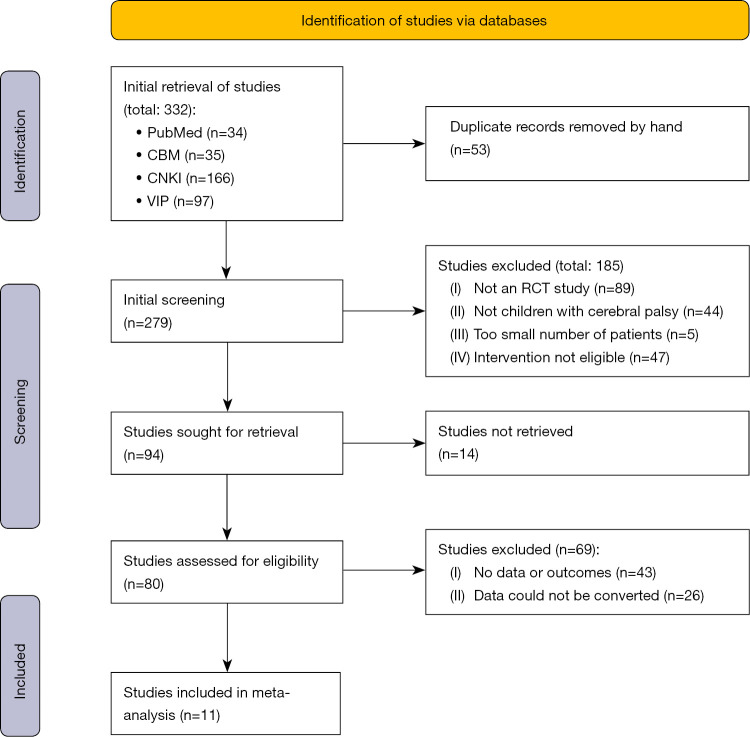
The retrieval flow chart is shown in Figure 1. A total of 332 articles were initially retrieved, and 11 remaining articles were included after screening, comprising a total of 731 children.
Figure 1.
Literature selection flow chart. CBM, Chinese Biomedical Literature; CKNI, China National Knowledge Infrastructure; RCT, randomized controlled trial.
Basic characteristics of articles
The basic characteristics, intervention measures, outcome indicators the included articles are shown in Table 1. The age range of participants was 0.5 to 10 years. The minimum number of cases in the grouping was 25 and the maximum was 60. According to different intervention methods, there were 6 articles involving simple scalp acupuncture, 1 involving scalp acupuncture + acupoint injection, 1 involving acupuncture + tongue acupuncture, 1 involving scalp acupuncture + massage, 1 involving scalp acupuncture + acupuncture, and 1 article involving scalp acupuncture + language training.
Table 1. Basic characteristics, intervention measures, outcome indicators, and quality scores of the included articles.
| Author | Year | Mean age (years) | Gender ratio | Major comorbidities | Population (E/C) |
Intervention methods | Outcome indicators | |
|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | |||||||
| Gao et al. (8) | 2019 | 3.6±1.5 | 27/25 | N/A | 23/29 | SA | CRT | ④⑤ |
| Li et al. (9) | 2011 | 0.5–3 | 46/22 | Intellectual disability | 34/34 | SA | CRT | ①② |
| Xing et al. (10) | 2012 | 1–10 | 38/22 | Intellectual disability | 30/30 | SA | CRT | ① |
| Li et al. (11) | 2010 | 0.5–2 | 38/34 | Intellectual disability | 36/36 | SA | CRT | ① |
| Qi et al. (12) | 2015 | 0.5–7 | 40/20 | Intellectual disability | 34/34 | SA | CRT | ①② |
| Tao et al. (13) | 2012 | 1–10 | 38/22 | N/A | 30/30 | SA | CRT | ① |
| Li et al. (14) | 2019 | 2.2±0.5 | 34/26 | N/A | 30/30 | SA + AJ | CRT | ①②③⑥ |
| Xian et al. (15) | 2019 | 0.5–5 | 68/52 | Intellectual disability | 60/60 | SA + latch needle | CRT | ①④ |
| Li et al. (16) | 2019 | 3.5±1.2 | 29/31 | Strabismus | 30/30 | SA + massage | Massage + CRT | ① |
| Li et al. (17) | 2014 | 4.4±2.7 | 29/21 | Speech dysfunction | 25/25 | SA + moxibustions | CRT | ①③ |
| Jin et al. (18) | 2014 | 1–6 | 67/46 | Speech dysfunction | 60/53 | SA + LT | CRT | ① |
Outcomes: ① effective rate; ② MDI score; ③ PDI score; ④ GMFM-88 score; ⑤ ADL score; ⑥ advert events. E, Experimental group; C, Control group; N/A, not available; SA, scalp acupuncture; AJ, acupoint injection; LT, language training; CRT, conventional rehabilitation training; MDI, Mental Development Index; PDI, Psychological Development Index; GMFM, Gross Motor Function Measure; ADL, activities of daily living.
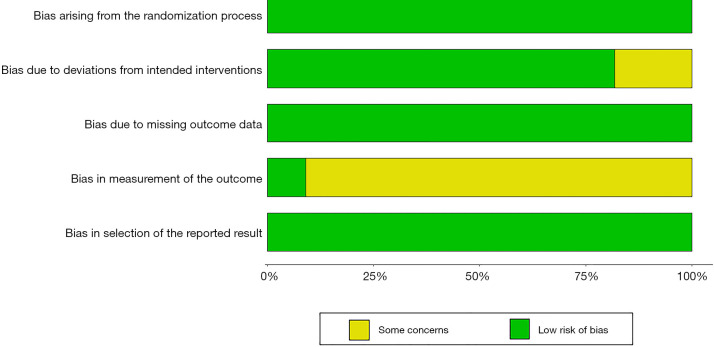
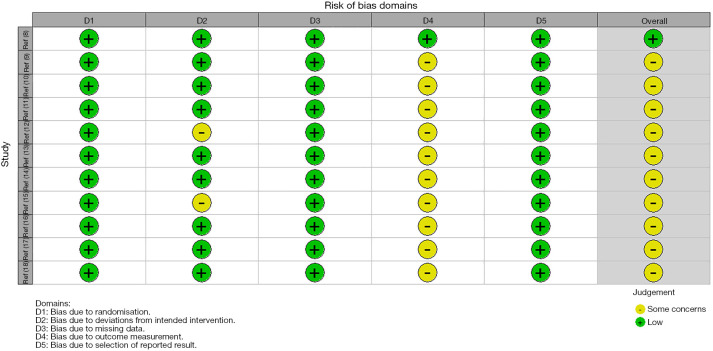
Literature bias assessment
In this study, all articles indicated that a randomization method was used; however, two articles (12,15) indicated no blinding methods which resulted in deviations from intended interventions; studies (9-18) had some concerns about the measurement of the outcome (Figures 2,3).
Figure 2.
Risk of bias summary.
Figure 3.
Risk of bias graph.
Meta-analysis results
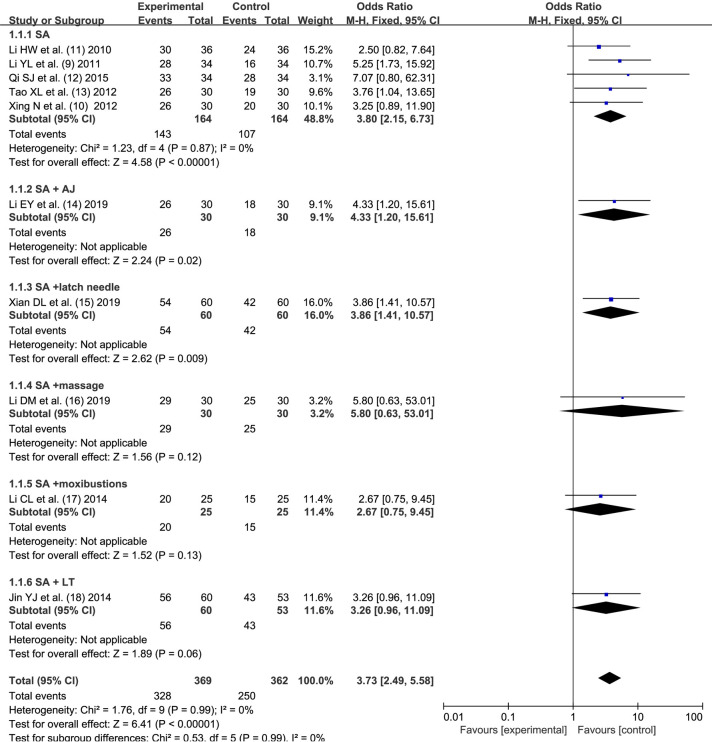
Effective rate
The effective rate of scalp acupuncture treatment was reported in all articles except (8). The experimental group included 369 children and the control group included 363 children. There was no statistical heterogeneity between the articles (I2=0%, P=0.99). The fixed-effects model analysis was used to obtain the pooled size (OR =3.73, 95% CI: 2.49–5.58), indicating that scalp acupuncture had a significant effect on the improvement of symptoms in children with CP (Z=6.41, P<0.00001). The patients were further divided into simple scalp acupuncture group (SA), scalp acupuncture + acupoint injection group (SA + AJ), scalp acupuncture + tongue acupuncture group (SA + tongue acupuncture), scalp acupuncture + massage group (SA + massage), scalp acupuncture + moxibustion (SA + moxibustion), and scalp acupuncture + language training (SA + LT) according to the type of intervention, and there was no statistical heterogeneity between each internal article, as shown in Figure 4.
Figure 4.
Combined analysis of the therapeutic effect of acupuncture based on scalp acupuncture on children with cerebral palsy. SA, scalp acupuncture; AJ, acupoint injection; LT, language trainin; CI, confidence interval; df, degrees of freedom.
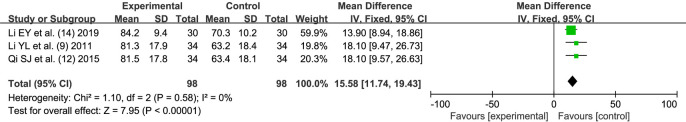
MDI score
A total of 3 articles (9,12,14) reported the improvement of MDI score by scalp acupuncture. Both the experimental group and the control group included 98 children. There was no statistical heterogeneity between the articles (I2=0%, P=0.58). The fixed effects model analysis was used to obtain the pooled size (MD =15.58, 95% CI: 11.74–19.43), indicating that scalp acupuncture had a significant effect on improving the mental development of children (Z=7.95, P<0.00001) (Figure 5).
Figure 5.
Combined analysis of effect on mental development by acupuncture treatment based on scalp acupuncture for children with cerebral palsy. SD, standard deviation; CI, confidence interval; df, degrees of freedom.
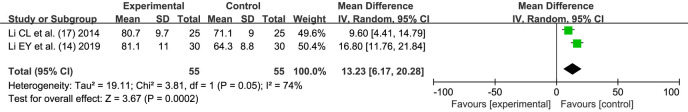
PDI score
A total of 2 articles (14,17) reported the improvement of PDI score by scalp acupuncture. Both the experimental group and the control group included 55 children, with statistical heterogeneity between the articles (I2=74%, P=0.05). The random-effects model analysis was used to obtain the combined size (MD =13.23, 95% CI: 6.17–20.28), indicating that scalp acupuncture had a significant effect on improving the psychological development of the children (Z=3.67, P=0.0002) (Figure 6).
Figure 6.
Combined analysis of psychological development of acupuncture treatment based on scalp acupuncture for children with cerebral palsy. SD, standard deviation; CI, confidence interval; df, degrees of freedom.
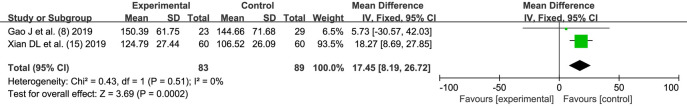
GMFM-88 score
A total of 2 articles (8,15) reported on the improvement of GMFM-88 score by scalp acupuncture. The experimental group included 83 children and the control group included 89 children. There was statistical heterogeneity between the literatures (I2=0%, P=0.51). Fixed-effects model analysis was used to obtain the combined size (MD =17.45, 95% CI: 8.19–26.72), that indicating that scalp acupuncture had a significant effect on improving the motor ability of the children (Z=3.69, P=0.0002) (Figure 7).
Figure 7.
Combined analysis of motor ability of acupuncture treatment based on scalp acupuncture for children with cerebral palsy. SD, standard deviation; CI, confidence interval; df, degrees of freedom.
Safety
Only study (14) reported the adverse events for both groups. In the intervention group, there were some cases of slight bleeding at acupuncture points, which could be easily treated, while there were no cases of adverse events for the control group.
Heterogeneity investigation
In the meta-analysis of response rate indicators, there was no statistically significant heterogeneity between the articles. We tried to analyze the articles according to different intervention methods, and there was still no statistically significant heterogeneity among them.
Sensitivity analysis
In the analysis of response rate indicators, if the random effects model was used for analysis, the pooled effect size (OR =3.69, 95% CI: 2.46–5.53) was obtained, which was not significantly different from the results of the analysis using the fixed effects model, so the results could be considered stable.
Publication bias analysis
In the analysis of the effective rate index, the 10 included articles were evenly distributed on the left and right sides in the funnel plot, suggesting that the possibility of publication bias was small, as shown in Figure 8.
Figure 8.
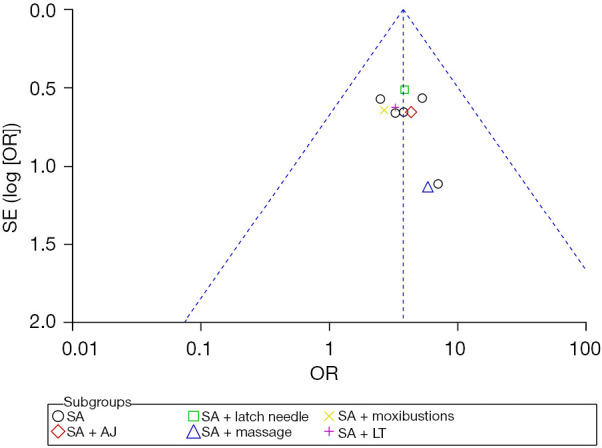
Funnel plot. SA, scalp acupuncture; AJ, acupoint injection; LT, language training.
Discussion
In traditional Chinese medicine (TCM), pediatric CP belongs to the category of “dementia”. Its etiology mainly stems from embryonic dysplasia caused by congenital endowment deficiency, liver and kidney deficiency, lack of source of qi and blood, or intrapartum brain damage, and developmental impairment caused by trauma (19). In TCM, the brain is the medullary sea, the house of Yuan Shen, and in CP the kidney source is depleted, and the brain marrow is lost, so it is stunted and results in intellectual disability. Acupoint selection through scalp acupuncture can be adjusted to Zhuyang, transporting qi and blood, tonifying Qingqiao, playing a role in enriching the medullary sea, and strengthening the brain and cognition (20).
In this meta-analysis, a total of 11 clinical RCTs published in recent years were retrieved, and 731 children with CP were included. The main symptoms of the children were intellectual disability, limb disorders, poor speech function, and strabismus. After comprehensive rehabilitation treatment based on scalp acupuncture, the symptoms of the children were significantly improved, the treatment efficiency was higher than that of conventional rehabilitation treatment, and the mental development, psychological development, and motor function of the children after treatment were superior to those who received conventional rehabilitation treatment alone, which indicated that scalp acupuncture had a superior effect in the treatment of CP. There was no report of serious adverse event, the treatment was safe. An experimental study on rats (21) has indicated that scalp acupuncture methods promote the rehabilitation of neurological impairment in CP, and these effects may be related to scalp acupuncture improving the expression of nerve growth related proteins, enhancing ATPase activity, and regulating the brain microenvironment. Zhang et al.’s study (22) reported that the effect of scalp acupuncture targeting the PI3K/Akt signaling pathway may be one of the mechanisms to inhibit hippocampal neuronal apoptosis and ameliorate defects associated with pediatric CP in a rat model. In another study (14), the cerebral hemodynamics of the children were monitored and it was shown that the cerebral hemodynamic parameters of the children treated with scalp acupuncture were significantly better than those of the control group, while the serum neuron-specific enolase content was lower than that of the control group, indicating that the degree of cranial nerve function impairment was lower. Scalp acupuncture treatment can not only regulate vascular tone, significantly increase cerebral blood flow in children with CP, improve cerebral blood supply efficiency, but also improve brain cell metabolism, promote partial or complete compensation of brain function, and promote the repair of brain tissue and functional plasticity to some extent (23).
Among the 11 articles included this meta-analysis, the needle application site of scalp acupuncture was not exactly the same, but all included Baihui, Sishen, Zhi San, Temporal San, motor area, foot transport sensory area, sensory area, balance area, and language area. The Baihui point is an important point to regulate brain function, as it can influence the venation of yin and yang and connect the whole body meridians, and plays an important role in regulating the balance of yin and yang in the body, so acupuncture at Baihui point can generate qi and blood, replenish the brain marrow, and open the mind to achieve the function of Xingnao Ningshen Kaiqiao. The Sishen acupoint is an important point for Jin 3 acupuncture to treat the mind, which can adjust the brain meridians and qi, and benefit the mind and strengthen the brain. Acupuncture at Zhi San can promote brain development and improve intelligence. The motor area, foot transport sensory area, sensory area, balance area, and language area correspond to the anatomical position of brain function, which can improve brain-blood circulation, increase brain oxygen supply, promote brain development, and improve intelligence (24). A study by Wang et al. (21) showed that scalp acupuncture methods promoted the rehabilitation of nerve function damaged by CP, and these effects were likely related to the improved expression of nerve growth-related proteins, enhancement of ATPase activities, and regulation of the brain microenvironment.
For the treatment of children with CP, scalp acupuncture is typically combined with body acupuncture treatment. One article (15) explored the combination of scalp acupuncture and tongue acupuncture, and showed that that tongue acupuncture can reflexively regulate the viscera and body. Selection of the heart point, spleen point, kidney point, liver point, tongue column has the effect of invigorating the spleen and tonifying the liver, can replenish qi and strengthen tendons and bones, and can be used for resuscitation. One article (17) adopted the method of scalp acupuncture combined with moxibustion, and concluded that moxibustion at the Baihui point in healthy individuals can significantly accelerate the blood flow velocity of the common carotid artery and left and right middle and posterior cerebral arteries, significantly reduce the peripheral vascular resistance of the brain, and significantly improve blood supply of the brain. The method of scalp acupuncture combined with acupoint injection in an article (14) was found to enhance the effect of acupuncture, repair brain injury, and promote neural cell development in the brain.
In this meta-analysis, 10 articles reported the effectiveness of scalp acupuncture treatment. Although no heterogeneity was detected among the articles, we still performed subgroup analysis. The results showed that there was no significant difference in the efficacy between scalp acupuncture combined with massage, scalp acupuncture combined with moxibustion, and scalp acupuncture combined with language training and the conventional control group. However, since there was only 1 article in these few literatures, we could not consider that the effect of combined rehabilitation training was inferior to that of scalp acupuncture treatment alone. The efficacy of combined rehabilitation training still needs to be explored in more clinical RCTs.
This study had some limitations, including the following: (I) the number of included articles was small, the number of participants was small, and there was a lack of multi-center, large-sample RCTs; (II) regarding the quality of included studies, only one study with low risk of bias and 10 of them with some concerns of bias; (III) the symptoms of included children with CP were diverse, so the foci of acupuncture treatment were different. Some studies focused on the treatment of limb hemiplegia in children, and some focused on the treatment of speech disorders in children, which made the effectiveness evaluation quite different.
Conclusions
Comprehensive rehabilitation incorporating scalp acupuncture is more effective than conventional rehabilitation, which can effectively improve the symptoms of CP, promote the mental and psychological development of children, and improve their motor function. The treatment was safe because no serious adverse event was reported. However, more high-quality, multicenter, large-sample RCTs need to be conducted in clinical practice to provide stronger evidence.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This work was supported by grants from the Heilongjiang University of Traditional Chinese Medicine Research Fund Project (No. 201730); Heilongjiang Province Traditional Chinese Medicine Research Project (No. ZHY2020-162); and the Sichuan Provincial Department of Education Humanities and Social Sciences Key Research Base-Sichuan Hospital Management and Development Research Center (No. SCYG2021-35); and conducted by the second batch of provincial-level famous Chinese medicine practitioners in Heilongjiang Province (No. 2021-2023).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-85/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-85/coif). The authors have no conflicts of interest to declare.
References
- 1.Mathewson MA, Lieber RL. Pathophysiology of muscle contractures in cerebral palsy. Phys Med Rehabil Clin N Am 2015;26:57-67. 10.1016/j.pmr.2014.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aisen ML, Kerkovich D, Mast J, et al. Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol 2011;10:844-52. 10.1016/S1474-4422(11)70176-4 [DOI] [PubMed] [Google Scholar]
- 3.Chin EM, Gwynn HE, Robinson S, et al. Principles of Medical and Surgical Treatment of Cerebral Palsy. Neurol Clin 2020;38:397-416. 10.1016/j.ncl.2020.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elbasan B, Bezgin S. The effects of reflexology on constipation and motor functions in children with cerebral palsy. Pediatr Neonatol 2018;59:42-7. 10.1016/j.pedneo.2017.01.005 [DOI] [PubMed] [Google Scholar]
- 5.Luo W, Wang PQ, Liu CL, et al. Therapeutic effect of scalp acupuncture combined with rehabilitation training on balance dysfunction in children with spastic hemiplegia. Chinese Journal of acupuncture and moxibustion. 2020;45:662-6. [DOI] [PubMed]
- 6.Wu Y, Zou LP, Han TL, et al. Randomized controlled trial of traditional Chinese medicine (acupuncture and tuina) in cerebral palsy: part 1--any increase in seizure in integrated acupuncture and rehabilitation group versus rehabilitation group? J Altern Complement Med 2008;14:1005-9. 10.1089/acm.2007.0756 [DOI] [PubMed] [Google Scholar]
- 7.Alotaibi M, Long T, Kennedy E, et al. The efficacy of GMFM-88 and GMFM-66 to detect changes in gross motor function in children with cerebral palsy (CP): a literature review. Disabil Rehabil 2014;36:617-27. 10.3109/09638288.2013.805820 [DOI] [PubMed] [Google Scholar]
- 8.Gao J, He L, Yu X, et al. Rehabilitation with a combination of scalp acupuncture and exercise therapy in spastic cerebral palsy. Complement Ther Clin Pract 2019;35:296-300. 10.1016/j.ctcp.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 9.Li YL. Scalp acupuncture for 68 cases of cerebral palsy complicated with mental retardation in children. China Rehabilitation 2011;26:45-6. [Google Scholar]
- 10.Xing N, Chen YG. Clinical study of scalp acupuncture on improving cerebral palsy complicated with mental retardation in children. Journal of Liaoning University of Traditional Chinese Medicine 2012;14:191-2. [Google Scholar]
- 11.Li HW, Ma BX. Clinical observation on scalp acupuncture in the treatment of cerebral palsy complicated with mental retardation in children. China Pediatrics of Integrated Traditional Chinese and Western Medicine 2010;2:23-4. [Google Scholar]
- 12.Qi SJ. Effect of scalp acupuncture on children with cerebral palsy and mental retardation. Henan Medical Research 2015;24:88-9. [Google Scholar]
- 13.Tao XL, Ma LX. 60 cases of infantile cerebral palsy treated with scalp acupuncture. Shaanxi Traditional Chinese Medicine 2012;33:88-9. [Google Scholar]
- 14.Li EY, Teng JF, Zhao PJ, et al. Clinical study on head water acupuncture combined with routine rehabilitation to improve intellectual impairment in children with cerebral palsy. Chinese Journal of Rehabilitation Medicine 2019;34:165-71. [Google Scholar]
- 15.Xian DL. Effect of scalp acupuncture combined with tongue acupuncture on children with cerebral palsy and mental retardation and its effect on damaged brain tissue. Sichuan Traditional Chinese Medicine 2019;37:177-80. [Google Scholar]
- 16.Li DM, Xiao YS, Zhang L, et al. Preliminary clinical study on massage and scalp acupuncture in the treatment of infantile cerebral palsy strabismus. Chinese Journal of Ophthalmology of Traditional Chinese Medicine 2019;29:35-8. [Google Scholar]
- 17.Li CL, Liu XL. Scalp acupuncture combined with moxibustion Baihui in the treatment of 50 cases of speech dysfunction in children with cerebral palsy. Journal of integrated traditional Chinese and Western Medicine on Cardiovascular and Cerebrovascular Diseases 2014;12:124-5.
- 18.Jin YJ, Huang M, Li HX, et al. Effect of scalp acupuncture combined with speech training on cognitive impairment in children with cerebral palsy. Journal of Hebei Traditional Chinese Medicine 2014;29:34-6. [Google Scholar]
- 19.Hao JJ, Hao LL. Review of clinical applications of scalp acupuncture for paralysis: an excerpt from chinese scalp acupuncture. Glob Adv Health Med 2012;1:102-21. 10.7453/gahmj.2012.1.1.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zanella AK, Gutierres JM, Stigger F. Effects of Scalp Acupuncture on Functional Deficits Induced by Early Sensorimotor Restriction. J Acupunct Meridian Stud 2019;12:77-83. 10.1016/j.jams.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 21.Wang Z, Fan X, Chen K, et al. Effects of three kinds of head acupuncture therapies on regulation of brain microenvironment and rehabilitation of nerve function in rats with cerebral palsy. J Tradit Chin Med 2021;41:276-83. [PubMed] [Google Scholar]
- 22.Zhang H, Gao J, Wang M, et al. Effects of scalp electroacupuncture on the PI3K/Akt signalling pathway and apoptosis of hippocampal neurons in a rat model of cerebral palsy. Acupunct Med 2018;36:96-102. 10.1136/acupmed-2016-011335 [DOI] [PubMed] [Google Scholar]
- 23.Kim HN, Pak ME, Shin MJ, et al. Comparative analysis of the beneficial effects of treadmill training and electroacupuncture in a rat model of neonatal hypoxia-ischemia. Int J Mol Med 2017;39:1393-402. 10.3892/ijmm.2017.2970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Di Wang, Yu Cheng, Ma Shuangyu, et al Research progress of acupuncture and moxibustion in the treatment of cervical headache. Journal of Guangzhou University of Traditional Chinese Medicine 2021;38:6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as