Abstract
Introduction
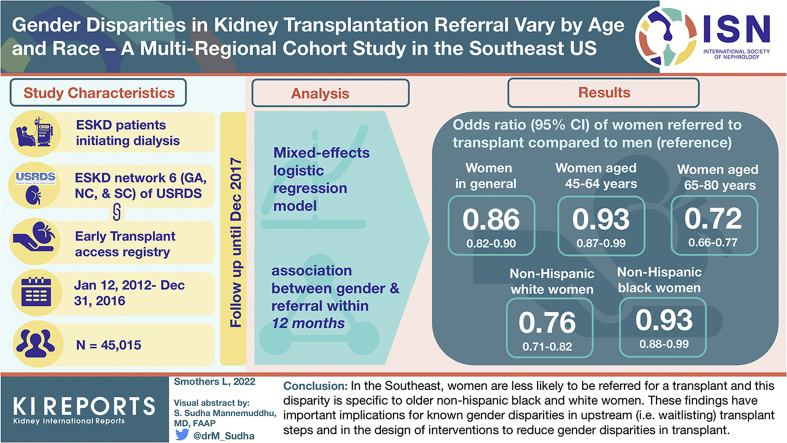
Men (vs. women) are more likely to be waitlisted or receive a kidney transplant. Whether gender disparities exist in earlier transplant steps (i.e., referral) and whether age, race, or obesity factors play a role are unknown.
Methods
Adults (18–80 years; N = 45,015) initiating dialysis in Georgia (GA), North Carolina (NC), or South Carolina (SC) (2012–2016) from the United States Renal Data System were linked to the Early Transplant Access Registry, with follow-up to December 2017. Using a mixed-effects logistic regression model adjusted for several patient characteristics, we assessed the association between gender and referral within 12 months, including interaction terms for age, race/ethnicity, and obesity.
Results
Overall, 37.0% and 41.5% of women and men, respectively, were referred within 12 months. In fully adjusted models, women (vs. men) were 14% less likely to be referred (odds ratio [OR]: 0.86; 95% CI: 0.82−0.90). Women (vs. men) aged 45 to 64 years and 65 to 80 years were 0.93 (0.87−0.99) and 0.72 (0.66−0.77) less likely to be referred, respectively. Women (vs. men) of non-Hispanic White and non-Hispanic Black race were 0.76 (0.71−0.82) and 0.93 (0.88−0.99) less likely to be referred, respectively. For other race (Hispanic, other) and age (18–44 years) subgroups, and all obesity subgroups, no gender differences in referral rates were observed.
Conclusion
In the Southeast, women are less likely to be referred for a transplant, and this disparity is specific to older non-Hispanic Black and White women. These findings have important implications for known gender disparities in upstream (i.e., waitlisting) transplant steps and in the design of interventions to reduce gender disparities in transplant.
Keywords: epidemiology, gender disparities, health services research, kidney transplant, transplant referral
Graphical abstract
See Commentary on Page 1145
For patients with end-stage kidney disease (ESKD), kidney transplantation is the preferred treatment because it provides better quality of life, longer survival, and lower hospitalization rates as compared with dialysis.1 However, a relative donor shortage means not all patients with ESKD will receive a life-saving transplant. In 2017, only 13.2% of patients with incident ESKD were placed on the deceased donor waitlist or received a transplant within 1 year of ESKD diagnosis.2 Importantly, not all eligible patients have the same chance of receiving a life-saving transplant. For example, a large body of literature now indicates that patients of lower (vs. higher) socioeconomic status,3, 4, 5 Black (vs. White) patients,6, 7, 8, 9 and obese (vs. nonobese) patients10,11 are less likely to receive a transplant.
Perhaps the most difficult disparity to explain has been that of gender: women with ESKD are 10% to 20% less likely to receive a kidney transplant compared with men even after adjustment for several demographic and clinical factors.3,4,12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 This is despite several studies demonstrating similar or better post-transplant survival in women versus men.23,25, 26, 27, 28, 29, 30, 31, 32 Emerging evidence also suggests that gender disparity may occur at downstream transplant processes (i.e., before waitlisting and transplant), such as referral and evaluation. For example, in the Southeastern United States, studies have shown that women are approximately 14% and 6% less likely to be referred and to initiate evaluation for a transplant, respectively, as compared with men,33,34 after adjustment for several individual- and system-level factors. Given that lower transplant referral rates in women are likely to lead to lower overall transplant, identifying factors that may be driving lower referral rates in women is an essential step to reducing gender disparities in transplant.
Therefore, in this study, we explore the role of age, race/ethnicity, and obesity as potential effect modifiers of gender disparities in a large Southeastern US population. Age,33,34 race/ethnicity,2,8,9,33,34 and obesity35,36 were chosen as key factors of interest in this study because they have previously been demonstrated as risk factors for reduced odds of referral and/or waitlisting.
Methods
Study Population
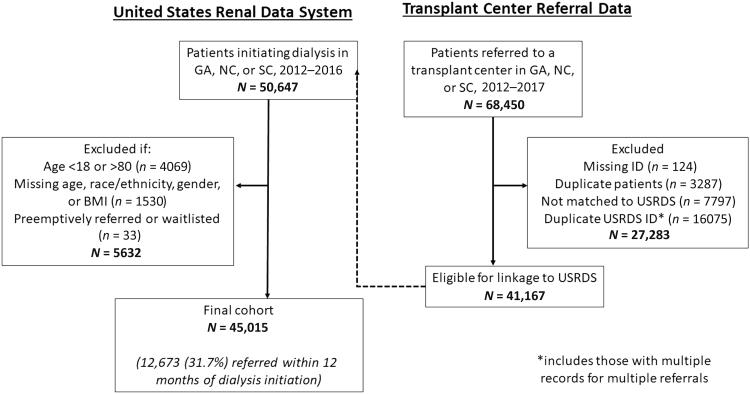
In this study, we included all adult patients with ESKD (aged 18–80 years) initiating dialysis in ESKD Network 6 (comprised GA, NC, and SC) between January 1, 2012, and December 31, 2016, from the United States Renal Data System, a national registry of all patients with ESKD in the United States initiating kidney replacement therapy.1 Individuals were linked to kidney transplant referral data obtained from the Early Transplant Access Registry37 and collected from all 9 adult transplant centers in Network 6 with follow-up until December 2017. We excluded patients who were pre-emptively waitlisted (n = 33) and those who were missing information on gender, race/ethnicity, age, or body mass index (BMI) (n = 1530). The final cohort included 45,015 people with incident ESKD between 2012 and 2016 (Figure 1).
Figure 1.
Flow diagram of study inclusion and exclusion criteria for study population. BMI, body mass index; GA, Georgia; ID, identification; NC, North Carolina; SC, South Carolina; USRDS, United States Renal Data System.
Data Collection and Measurement
The primary outcome for this study was 12-month referral, defined as the first referral from a dialysis facility for transplant evaluation within 1 year of dialysis initiation, as determined from referral forms routinely collected from the transplant centers. These data have been used in previous studies to evaluate disparities in referral rates in the Southeast.33,34,38
Primary variables of interest were ascertained from the Centers for Medicare and Medicaid Services (CMS) form 2728, which is completed by providers within 45 days of receipt of kidney replacement therapy. Gender (men or women) is assigned to each patient by their provider at initiation of kidney replacement therapy. In this study, gender is considered a social construct and a social identity, not a biological classification.39 Other key variables of interest, categorized using common groupings, included age (18–44, 45–64, and 65–80 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and “other”), and obesity as measured by BMI (underweight: <18.5 kg/m2, normal weight: 18.5–24 kg/m2, overweight: 25–29 kg/m2, obese class I: 30–34 kg/m2, obese class II: 35–40 kg/m2; and obese class III: ≥40 kg/m2). Other variables of interest included primary cause of ESKD (diabetes, hypertension, glomerulonephritis, other), access to pre-ESKD care (yes, no), comorbidities (smoking status, congestive heart failure, diabetes, atherosclerotic heart disease, other cardiac disease, cerebrovascular disease, peripheral vascular disease, and cancer), transplant education (informed of transplant yes/no; if no, why [medically unfit, patient declined, patient not assessed, other]), and insurance status (no insurance, Medicaid, Medicare, private, or other). For insurance status, where patients indicated they had >1 insurance provider, we categorized them using a hierarchy of private, Medicaid, Medicare, and other. For all nonprimary variables, <13% of data were missing.
Statistical Analysis
Differences in baseline demographic and clinical characteristics by gender, and by pre-emptive referral status, were evaluated using χ2 tests for categorical variables, independent t tests for normally distributed continuous variables, and 2-sample Mann-Whitney U tests for non-normally distributed continuous variables. The normality assumption was tested for all continuous variables using density plots. Individuals were followed from date of dialysis initiation to 12-month referral date, date of death, or end of follow-up (12 months from dialysis start), whichever occurred first. To assess the association between gender and 12-month referral, we used logistic regression models and adjusted for age, race/ethnicity, BMI, insurance, primary cause of ESKD, pre-ESKD care, transplant education, and comorbidities. To account for clustering of patients within dialysis facilities, dialysis facility was modeled as a random effect. The final model included variables significantly associated with 12-month referral in fully adjusted models with P < 0.05 and who did not violate collinearity assumptions (i.e., variance inflation factor >10).
We tested for interactions between age, BMI, and race/ethnicity with gender. Where the interaction was significant (P < 0.05), we stratified analyses by that factor. All analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC) and R version 4.0.2 (R Core Team, 2020) with “survival” (Therneau 2020). This study adheres to the STROBE guidelines for observational studies (Supplementary Table S1), adheres to the Declaration of Helsinki, and was approved by the institutional review board at Emory University (IRB00079596).
Results
Baseline Characteristics
We included 45,015 adult patients with ESKD initiating dialysis (median age 61.0 years [interquartile range: 51.0–69.0], 55.5% men) in GA, SC, and NC between January 2012 and December 2016. At dialysis initiation, women (vs. men) were more likely to be non-Hispanic Black, have a higher BMI, be Medicare insured, have diabetes as primary cause of ESKD, have pre-ESKD care, and have some comorbidities (diabetes, congestive heart failure, cerebrovascular disease) (Table 1). In contrast, men (vs. women) were more likely to have hypertension as a primary cause of ESKD and some comorbidities (current smoker, atherosclerotic disease, peripheral vascular disease, other cardiac disease, and cancer). Men and women were similarly likely to be informed of transplant as a treatment option.
Table 1.
Baseline characteristics of adult patients with incident ESKD in GA, SC, and NC, by gender, 2012 to 2016
| Characteristics | Total | Men | Women |
|---|---|---|---|
| n (%) | 45,015 (100.0) | 22,965 (55.5) | 20,050 (44.5) |
| Age in years, median (IQR) | 61.0 (51.0–69.0) | 61.0 (50.0–69.0) | 62.0 (52.0–70.0) |
| Age (%) | |||
| 18–44 | 14.7 | 15.2 | 14.1 |
| 45–64 | 44.7 | 45.6 | 43.4 |
| 65–80 | 40.6 | 39.1 | 42.5 |
| Race/ethnicity (%) | |||
| Non-Hispanic White | 42.1 | 44.8 | 39.0 |
| Non-Hispanic Black | 53.3 | 50.3 | 57.0 |
| Hispanic | 2.7 | 3.0 | 2.3 |
| Other | 1.9 | 2.0 | 1.8 |
| Insurance (%) | |||
| Private | 20.7 | 22.2 | 18.7 |
| Medicare | 39.2 | 40.1 | 38.0 |
| Medicaid | 23.9 | 18.5 | 30.6 |
| Other | 7.1 | 8.8 | 4.9 |
| No coverage | 9.2 | 10.4 | 7.7 |
| Obesity (BMI, kg/m2, median [IQR]) | 29.2 (24.6–35.0) | 28.4 (24.3–33.7) | 30.1 (25.0–36.7) |
| Obesity (BMI, kg/m2, %) | |||
| Underweight (<18.5) | 3.0 | 2.8 | 3.2 |
| Normal (18.5–24.9) | 24.5 | 26.3 | 22.4 |
| Overweight (25–29.9) | 26.6 | 29.2 | 23.4 |
| Obese class I (30–34.9) | 20.8 | 21.1 | 20.5 |
| Obese class II (35–39.9) | 12.4 | 11.1 | 13.9 |
| Obese class III (≥40) | 12.7 | 9.6 | 16.6 |
| Primary cause of ESKD (%) | |||
| Diabetes | 45.0 | 43.5 | 47.0 |
| Hypertension | 35.3 | 36.7 | 33.6 |
| Glomerulonephritis | 7.4 | 6.7 | 8.3 |
| Other | 12.3 | 13.1 | 11.2 |
| Pre-ESKD nephrology care (%) | 74.2 | 72.9 | 75.8 |
| Informed of transplant as a treatment option (%) | 88.5 | 88.7 | 88.2 |
| Reason not informed of transplant (%) | |||
| Medically unfit | 3.1 | 3.0 | 3.2 |
| Patient declined | 0.2 | 0.2 | 0.2 |
| Patient not assessed | 6.8 | 6.7 | 6.8 |
| Other | 2.0 | 1.9 | 2.2 |
| Comorbidities (%) | |||
| Current smoker | 8.7 | 10.2 | 7.0 |
| Congestive heart failure | 26.3 | 25.6 | 27.3 |
| Atherosclerotic disease | 9.7 | 10.5 | 8.7 |
| Other cardiac disease | 17.3 | 18.3 | 16.0 |
| Diabetes | 58.9 | 57.1 | 61.0 |
| Cerebrovascular disease | 9.0 | 8.7 | 9.3 |
| Peripheral vascular disease | 8.6 | 9.5 | 7.6 |
| Cancer | 6.1 | 6.5 | 5.6 |
BMI, body mass index; ESKD, end-stage kidney disease; GA, Georgia; IQR, interquartile range; NC, North Carolina, SC, South Carolina.
Of the patients, 30 (<0.1%) had missing primary cause of ESKD; 5239 (11.6%) missing pre-ESKD nephrology care, and 16 (<0.1%) missing information on comorbidities.
When comparing men and women according to pre-emptively referred status (i.e., those pre-emptively referred and those not pre-emptively referred), differences in men and women were similar, with some exceptions (Supplementary Table S2). Specifically, among pre-emptively referred patients, women (vs. men) were more likely to have glomerulonephritis as primary cause of ESKD (vs. diabetes in non–pre-emptively referred participants) and men had a higher proportion of all comorbidities as compared with women who were pre-emptively referred.
Gender and 12-Month Referral for Kidney Transplant
Overall, 37.0% and 41.5% of women and men, respectively, were referred for a transplant within 12 months of dialysis initiation. Rates of referral also differed by subgroup: 62.6%, 46.21%, and 23.7% of adults aged 18 to 44, 45 to 64, and 65 to 80 years were referred, respectively; 33.7%, 43.3%, 47.4%, and 47.8% of non-Hispanic White, non-Hispanic Black, Hispanic, and “other” race/ethnic groups were referred, respectively; and 26.9%, 36.3%, 40.8%, 43.3%, 43.3%, and 35.7% of underweight, normal, overweight, obese class I, obese class II, and obese class III were referred, respectively. In unadjusted models, women were 17% less likely (OR: 0.83 [95% CI: 0.80–0.86]) to be referred within 12 months as compared with men. In multivariable-adjusted models, women were 14% (OR: 0.86 [0.82–0.90]) less likely to be referred within 12 months as compared with men (Table 2).
Table 2.
Association between demographic and clinical characteristics and 12-month referral in the Southeastern United States in crude and multivariable models
| Characteristics | Bivariate model, OR (95% CI) | Multivariable model,a OR (95% CI) |
|---|---|---|
| Gender | ||
| Men | Reference | Reference |
| Women | 0.83 (0.80–0.86) | 0.86 (0.82–0.90) |
| Age, yr | ||
| 18–44 | Reference | Reference |
| 45–64 | 0.51 (0.48–0.54) | 0.55 (0.51–0.58) |
| 65–80 | 0.18 (0.17–0.19) | 0.21 (0.20–0.23) |
| Race/ethnicity | ||
| Non-Hispanic White | Reference | Reference |
| Non-Hispanic Black | 1.50 (1.44–1.56) | 1.27 (1.21–1.34) |
| Hispanic | 1.77 (1.57–1.99) | 1.31 (1.14–1.50) |
| Other | 1.80 (1.56–2.07) | 1.60 (1.35–1.87) |
| Insurance | ||
| Private | Reference | Reference |
| Medicare | 0.33 (0.32–0.35) | 0.63 (0.59–0.67) |
| Medicaid | 0.42 (0.39–0.44) | 0.46 (0.43–0.49) |
| Other | 0.60 (0.55–0.65) | 0.61 (0.56–0.67) |
| No coverage | 0.73 (0.68–0.79) | 0.58 (0.53–0.63) |
| Obesity (BMI, kg/m2) | ||
| Underweight (<18.5) | 0.65 (0.57–0.74) | 0.68 (0.59–0.79) |
| Normal (18.5–24.9) | Reference | Reference |
| Overweight (25–29.9) | 1.21 (1.15–1.28) | 1.16 (1.09–1.23) |
| Obese class I (30–34.9) | 1.34 (1.27–1.42) | 1.24 (1.16–1.33) |
| Obese class II (35–39.9) | 1.34 (1.26–1.44) | 1.20 (1.11–1.30) |
| Obese class III (≥40) | 0.98 (0.91–1.04) | 0.75 (0.70–0.82) |
| Primary cause of ESKD | ||
| Diabetes | Reference | Reference |
| Hypertension | 1.05 (1.01–1.10) | 1.02 (0.96–1.08) |
| Glomerulonephritis | 1.86 (1.73–2.00) | 1.23 (1.12–1.35) |
| Other | 0.78 (0.73–0.83) | 0.75 (0.69–0.82) |
| Pre-ESKD nephrology careb | 1.45 (1.38–1.52) | 1.64 (1.55–1.73) |
| Informed of transplant as a treatment optionb | 2.18 (2.04–2.33) | 1.75 (1.62–1.89) |
| Comorbiditiesb | ||
| Current smoker | 0.79 (0.74–0.84) | 0.79 (0.73–0.85) |
| Congestive heart failure | 0.54 (0.52–0.57) | 0.73 (0.69–0.77) |
| Atherosclerotic disease | 0.53 (0.49–0.57) | 0.82 (0.76–0.89) |
| Other cardiac disease | 0.54 (0.51–0.57) | 0.77 (0.72–0.81) |
| Diabetes | 0.86 (0.82–0.89) | 0.97 (0.91–1.02) |
| Cerebrovascular disease | 0.53 (0.50–0.57) | 0.71 (0.65–0.77) |
| Peripheral vascular disease | 0.55 (0.51–0.59) | 0.79 (0.72–0.86) |
| Cancer | 0.40 (0.36–0.43) | 0.57 (0.51–0.63) |
BMI, body mass index; ESKD, end-stage kidney disease; OR, odds ratio.
Adjusted for all characteristics in Table 2.
Reference group is “no” vs. yes to each specific comorbidity.
Factors significantly associated with a reduced likelihood of 12-month referral in multivariable-adjusted models included older (vs. younger) age, White (vs. all other) race/ethnicity, underweight and obese class III (vs. normal weight), Medicare, Medicaid, none, and other (vs. private) insurance, other primary cause of ESKD (vs. diabetes), and all comorbidities, excluding diabetes (vs. not having a comorbidity) (Table 2). Factors associated with a higher likelihood of 12-month referral in fully adjusted models included non-Hispanic Black, Hispanic, and “other” race/ethnicity (vs. White), overweight, obese class I, and obese class II (vs. normal weight), having pre-ESKD nephrology care (vs. not), and being informed of transplant as a treatment option (Table 2).
Gender Interaction Terms
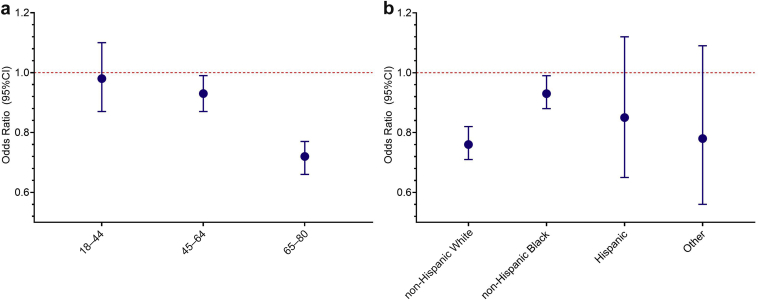
Significant interactions were found between age and gender (P < 0.001) and race/ethnicity and gender (P < 0.001), but not obesity and gender (P = 0.063). By age, women aged 45 to 64 and 65 to 80 years were 7% (OR: 0.93 [0.87–0.99]) and 28% (OR: 0.72 [0.66–0.77]) less likely to be referred within 12 months as compared with men of the same age, respectively (Figure 2a). Women aged 18 to 44 years had no difference in odds of referral as compared with men (OR: 0.98 [0.87–1.10]). By race/ethnicity, non-Hispanic Black women and non-Hispanic White women were 7% (OR: 0.93 [0.88–0.99]) and 24% (OR: 0.76 [0.71–0.82]) less likely to be referred within 12 months compared with non-Hispanic Black and non-Hispanic White men, respectively (Figure 2b). Hispanic women and women of “other race” had nonsignificant lower odds of 12-month referral compared with their male counterparts: (OR: 0.85 [0.65–1.12] and OR: 0.78 [0.56–1.09], respectively).
Figure 2.
Association between gender and 12-month referral by (a) age and (b) race/ethnicity. The reference line of 1 (dotted line) indicates no difference in referral rates between men and women.
Sensitivity Analysis
We conducted age and gender interaction terms among Black and White persons separately (Supplementary Table S3). In this analysis, significant interactions between age and gender were found for Black (P = 0.047) and White (P < 0.001) persons. In stratified analysis, White women aged 18 to 44 years had no difference in likelihood of being referred as compared with men (OR: 0.95 [0.76–1.19]), whereas women aged 45–64 and 65–80 years were 15% (OR: 0.85 [0.77–0.95]) and 36% (OR: 0.64 [0.57–0.72]) less likely to be referred compared with men of the same age, respectively. Similar findings were observed in Black women but of smaller magnitude. For example, Black women aged 18 to 44 and 45 to 64 years had no difference in likelihood of being referred as compared with men of the same age (OR: 0.99 [0.85–1.14] and OR: 0.98 [0.90–1.07], respectively), whereas Black women aged 65 to 80 years were 18% less likely to be referred as compared with men aged 65 to 80 years (OR: 0.92 [0.073–0.92]).
Discussion
In this study of Southeastern US adults initiating dialysis, women were 14% less likely to be referred for a transplant within 12 months of dialysis initiation as compared with men, after adjusting for several demographic and clinical characteristics. For the first time, we have demonstrated that this gender disparity is modified by both age and race/ethnicity, but not obesity. Specifically, older, but not younger, women were less likely to be referred as compared with men of the same age, and this disparity increased with increasing age. In addition, non-Hispanic White and non-Hispanic Black women were 24% and 7% less likely to be referred as compared with non-Hispanic Black and non-Hispanic White men, respectively. The results of this study suggest that policies and interventions designed to reduce gender disparities should consider the role age and race/ethnicity play in access to transplant referral.
The finding that age modifies gender disparities in transplant access has also been observed in studies of downstream transplant steps. For example, in a national US study between 2000 and 2005, older, but not younger, women were 29% to 59% less likely to be waitlisted or receive a living donor transplant.40 In a Canadian study, men aged 40 years and onward were 27% to 37% more likely to receive a transplant compared with women, with this disparity also increasing with increasing age.24 In the current study, we show that age and gender also interact at earlier transplant steps (i.e., referral) to significantly decrease referral rates for older women (range: 10%–24%), which likely contributes to gender disparities seen at later steps. Though more research is needed to elucidate the underlying mechanisms, it is hypothesized that these findings may be explained by the perception that women are more frail than men, and thus may not be suitable transplant candidates, despite similar or enhanced survival among female transplant recipients as compared with male transplant recipients of the same age.3,4,12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23 Indeed, a study conducted in a single dialysis facility demonstrated that nurse practitioners viewed women as more frail compared with men, and thus may be less likely to refer them for a transplant.41 Importantly, frailty is a potentially modifiable factor,42 and thus interventions to reduce gender disparities in transplant may focus on providing education and resources for physical rehabilitation in eligible female patients. Additional training to referring staff may also assist in reducing bias of perceived frailty among older women.
In this study, we also demonstrate that gender disparities in transplant referral rates are specific to certain race/ethnic groups with a 24% and 7% lower likelihood of referral in non-Hispanic White and non-Hispanic Black women as compared with men of the same race/ethnicity. A nonsignficant gender disparity was also observed for Hispanic and “other race,” though the lack of a significant finding likely reflects the smaller sample sizes (2.7% and 1.9% of the study population, respectively) rendering us underpowered to detect a significant effect in these groups. Future studies with larger Hispanic and “other race” representation should be conducted to confirm this. Though racial disparities in transplant access are well cited, how they explain gender disparities is less clear with few studies dedicated to exploring the issue. One Canadian study of transplant rates among people initiating renal replacement therapy demonstrated that the negative impact of female gender was weaker among Caucasians and persons of Eastern Asian origin and stronger among African Canadians, Inuits, and persons of Asian Indian origin.24 In another small, single-center study in Chicago, the completion of pretransplant workup was faster in men versus women in White and Hispanic patients, but not in African Americans.43 Given what we know of racial disparities in transplant access (i.e., that underrepresented minorities have lower waitlisting and transplant access as compared with White populations),44 it is perhaps a surprising finding of the current study that the gender disparity in referral rates is greatest in non-Hispanic older White populations. However, accumulating evidence suggests that racial disparities may differ at different transplant steps. For example, surveillance data on referral rates from the Southeast US show that Black patients are approximately 22% more likely to be referred compared with White patients,34 despite lower rates of waitlisting and transplant,44 and 37% less likely to be pre-emptively referred as compared with White patients.6 Lower referral rates in White versus Black patients may be explained in part by higher pre-emptive referrals in White patients, yet how this explains greater gender disparities in White versus Black populations and the mechanisms underpinning them warrant further analysis.
Also highlighting the need to evaluate barriers at each transplant step is our finding that overweight and obese class I and II persons were 16% to 24%, respectively, more likely to be referred as compared with normal weight individuals. In contrast, underweight and obese class III (BMI ≥40 kg/m2) persons were 32% and 25% less likely to be referred, respectively, as compared with normal weight individuals. This finding is somewhat inconsistent with the broader literature which demonstrates that obese people are less likely to be waitlisted for a kidney transplant, largely owing to increased risk of surgical complications in obese versus nonobese persons.45 Our differential finding may be explained by our detailed exploration of obese subclasses in contrast to most studies that only compare obese (≥30 kg/m2) with nonobese (<30 kg/m2) people. Given that we show a J-shaped association between obesity and referral, evaluating obese subclasses may be an important consideration for all future research that aims to understand the association between obesity and transplant access. Alternatively, it may be that obesity is a barrier at later steps of the transplant process, but not earlier steps. Regardless, in the current study we did not find that obesity modified gender disparities in likelihood of transplant referral, though this interaction was borderline significant (P = 0.063) and some other evidence suggests that obese women are less likely to be waitlisted as compared with obese men.10 An important future direction of our work will be to evaluate obesity and gender interactions across the spectrum of transplant steps.
Outside our own work,33,34,46, 47, 48 findings that women have reduced access to early transplant steps have been demonstrated in several other studies. For example, in a national Canadian study of >13,000 people who initiated dialysis between 2010 and 2013, female sex was associated with a 12% reduced likelihood of transplant referral.49 In a seminal 1998 paper, Alexander and Sehgal3 demonstrated that women were less likely to be considered medically suitable for a transplant, to indicate they were definitely interested in a transplant, and to complete the pretransplant workup as compared with men. Reasons for these gender disparities remain elusive, even for later transplant steps, but hypotheses include lower probability of providers discussing transplant as a treatment option with women, women’s attitudes toward transplant, both of which are upstream factors likely to significantly affect referral rates,50,51 and a lack of awareness of gender disparities.52 For example, a single-center study by Salter et al.50 among individuals who recently initiated hemodialysis treatment in Maryland showed that women were 45% more likely to not discuss kidney transplant with a medical professional compared with men. Another study by Salter et al.53 surveyed patients at dialysis centers in Maryland between 2009 and 2012 and reported that women are less likely to “want” to receive a transplant compared with men. Salter et al.53 also found that women initiating dialysis were 72% and 55% more likely to report having high health-related and psychosocial concerns about kidney transplant, respectively, compared with men. Finally, a 2012 survey conducted among 209 dialysis staff members in the Southeast United States suggested that staff were unaware of gender transplant disparities owing to limited experience and observation.52 More research is needed in this space to understand the underlying causes for why women (and their physicians) may be less likely to pursue a transplant. In the interim, prioritizing transplant education as early as possible (i.e., before initiating dialysis), increasing access to psychosocial services to reduce health-related stress, and providing and encouraging the use of implicit bias training for physicians may increase transplant referral rates among women. Finally, policies, such as the Advancing American Kidney Care Initiative, may need to consider the age and race/ethnicity interactions with gender to ensure equitable access to kidney transplants.
The key strength of this study includes the use of routinely collected referral data across 9 transplant centers in GA, NC, and SC, linked to the national United States Renal Data System registry. However, there are some limitations to be considered. First, our results are generalizable only to the Southeastern United States, which has a larger Black population, higher burden of chronic disease, and lower transplant rates compared with other regions in the United States.2,54,55 Second, patients who may have initiated dialysis in the region but were referred to transplant centers outside of GA, NC, and SC were excluded from the study population. However, based on previous literature, we expect this to be a small proportion (i.e., <10%).34 Third, this study is limited to data routinely captured in dialysis and transplant centers. We are therefore unable to adjust for several potentially important factors, such as income and education status. Furthermore, data from CMS form 2728 on pre-ESKD nephrology care are subject to misclassification,56 and comorbidity data are only captured at time of ESKD diagnosis and do not indicate severity. As a result, we cannot rule out the possibility of residual confounding in this study. Fourth, given the limitations of data captured in CMS 2728, we were not able to exclude those patients who may not have been eligible for transplant referral (e.g., someone with advanced cardiac disease), though there is a general consensus among End Stage Renal Disease Network 6 that there are no absolute contraindications for transplant referral. Fifth, for some smaller subgroups, such as Hispanic and other race/ethnicity groups, we may have been underpowered to detect significant associations. Finally, gender, as determined from CMS 2728, is assigned by the provider at kidney replacement therapy initiation and does not necessarily reflect patient self-identified gender. Therefore, findings of this study will be influenced by provider perception of gender.
In conclusion, in the Southeast, we report that women are 14% less likely to be referred for a transplant as compared with men. This disparity is specific to older and non-Hispanic Black and White women. These findings have important implications for known gender disparities in upstream (i.e., waitlisting) transplant steps and in the design of interventions to reduce gender disparities in transplant.
Disclosure
All the authors declared no competing interests.
Acknowledgments
This project and The Reducing Disparities in Access to kidNey Transplantation Regional Study was funded in part by the National Institute on Minority Health and Health Disparities award U01MD010611. Support for the preparation of this document was funded by Centers for Medicare and Medicaid Services (CMS) (an agency of the US Department of Health and Human Services) End Stage Renal Disease Network 6 contract HHSM-500-2013-NW006C. The data reported here have been supplied by the United States Data Renal System and the Southeastern Kidney Transplant Coalition. The conclusions presented are solely those of the authors and do not represent those of the Southeastern Kidney Coalition, CMS, or United States Renal Data System. The content of this publication does not necessarily reflect the policies or positions of the Department of Health and Human Services, and mention of trade names, commercial products, or organizations does not imply endorsement by the US Government. The authors assume responsibility for the accuracy and completeness of the ideas presented.
Author Contributions
LS conducted all analyses and drafted the manuscript. REP conceptualized the study, contributed to data acquisition and study design, and reviewed/edited the manuscript. SOP contributed to study design and data acquisition and reviewed/edited the manuscript. DD contributed to study design and reviewed/edited the manuscript. JLH contributed to study design, provided supervision, and reviewed/edited the manuscript.
Footnotes
Table S1. Adapted STROBE Checklist for Observational Studies.
Table S2. Baseline characteristics of men versus women in those who were and were not pre-emptively referred.
Table S3. Multivariable association between gender and 12-month referral in the Southeastern US stratified by age and race.
Supplementary Material
Table S1. Adapted STROBE Checklist for Observational Studies.
Table S2. Baseline characteristics of men versus women in those who were and were not pre-emptively referred.
Table S3. Multivariable association between gender and 12-month referral in the Southeastern US stratified by age and race.
References
- 1.Tonelli M., Wiebe N., Knoll G., et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093–2109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- 2.United States Renal Data System, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. 2019 USRDS annual data report: epidemiology of kidney disease in the United States. United States Renal Data System, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Accessed 19 April, 2022. https://www.usrds.org/annual-data-report/
- 3.Alexander G.C., Sehgal A.R. Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA. 1998;280:1148–1152. doi: 10.1001/jama.280.13.1148. [DOI] [PubMed] [Google Scholar]
- 4.Held P.J., Pauly M.V., Bovbjerg R.R., et al. Access to kidney transplantation. Has the United States eliminated income and racial differences? Arch Intern Med. 1988;148:2594–2600. doi: 10.1001/archinte.148.12.2594. [DOI] [PubMed] [Google Scholar]
- 5.Navaneethan S.D., Aloudat S., Singh S. A systematic review of patient and health system characteristics associated with late referral in chronic kidney disease. BMC Nephrol. 2008;9:3. doi: 10.1186/1471-2369-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gander J.C., Zhang X., Plantinga L., et al. Racial disparities in preemptive referral for kidney transplantation in Georgia. Clin Transpl. 2018;32 doi: 10.1111/ctr.13380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stolzmann K.L., Bautista L.E., Gangnon R.E., McElroy J.A., Becker B.N., Remington P.L. Trends in kidney transplantation rates and disparities. J Natl Med Assoc. 2007;99:923–932. [PMC free article] [PubMed] [Google Scholar]
- 8.Hall Y.N., Choi A.I., Xu P., et al. Racial ethnic differences in rates and determinants of deceased donor kidney transplantation. J Am Soc Nephrol. 2011;22:743–751. doi: 10.1681/asn.2010080819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Purnell T.S., Luo X., Cooper L.A., et al. Association of race and ethnicity with live donor kidney transplantation in the United States from 1995 to 2014. JAMA. 2018;319:49–61. doi: 10.1001/jama.2017.19152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ladhani M., Craig J.C., Wong G. Obesity and gender-biased access to deceased donor kidney transplantation. Nephrol Dial Transplant. 2019;35:184–189. doi: 10.1093/ndt/gfz100. [DOI] [PubMed] [Google Scholar]
- 11.Orandi B.J., Lewis C.E., MacLennan P.A., et al. Obesity as an isolated contraindication to kidney transplantation in the end-stage renal disease population: a cohort study. Obesity (Silver Spring) 2021;29:1538–1546. doi: 10.1002/oby.23195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kjellstrand C.M. Age, sex, and race inequality in renal transplantation. Arch Intern Med. 1988;148:1305–1309. [PubMed] [Google Scholar]
- 13.Ojo A., Port F.K. Influence of race and gender on related donor renal transplantation rates. Am J Kidney Dis. 1993;22:835–841. doi: 10.1016/s0272-6386(12)70343-8. [DOI] [PubMed] [Google Scholar]
- 14.Wolfe R.A., Ashby V.B., Milford E.L., et al. Differences in access to cadaveric renal transplantation in the United States. Am J Kidney Dis. 2000;36:1025–1033. doi: 10.1053/ajkd.2000.19106. [DOI] [PubMed] [Google Scholar]
- 15.Alexander G.C., Sehgal A.R. Transplant Task Force of The Renal Network, Inc. Variation in access to kidney transplantation across dialysis facilities: using process of care measures for quality improvement. Am J Kidney Dis. 2002;40:824–831. doi: 10.1053/ajkd.2002.35695. [DOI] [PubMed] [Google Scholar]
- 16.Biller-Andorno N. Gender imbalance in living organ donation. Med Health Care Philos. 2002;5:199–204. doi: 10.1023/a:1016053024671. [DOI] [PubMed] [Google Scholar]
- 17.Bloembergen W.E., Mauger E.A., Wolfe R.A., Port F.K. Association of gender and access to cadaveric renal transplantation. Am J Kidney Dis. 1997;30:733–738. doi: 10.1016/s0272-6386(97)90076-7. [DOI] [PubMed] [Google Scholar]
- 18.Bloembergen W.E., Port F.K., Mauger E.A., et al. Gender discrepancies in living related renal transplant donors and recipients. J Am Soc Nephrol. 1996;7:1139–1144. doi: 10.1681/ASN.V781139. [DOI] [PubMed] [Google Scholar]
- 19.Garg P.P., Furth S.L., Fivush B.A., Powe N.R. Impact of gender on access to the renal transplant waiting list for pediatric and adult patients. J Am Soc Nephrol. 2000;11:958–964. doi: 10.1681/asn.V115958. [DOI] [PubMed] [Google Scholar]
- 20.Gaylin D.S., Held P.J., Port F.K., et al. The impact of comorbid and sociodemographic factors on access to renal transplantation. JAMA. 1993;269:603–608. [PubMed] [Google Scholar]
- 21.Jindal R.M., Ryan J.J., Sajjad I., et al. Kidney transplantation and gender disparity. Am J Nephrol. 2005;25:474–483. doi: 10.1159/000087920. [DOI] [PubMed] [Google Scholar]
- 22.Kayler L.K., Meier-Kriesche H.U., Punch J.D., et al. Gender imbalance in living donor renal transplantation. Transplantation. 2002;73:248–252. doi: 10.1097/00007890-200201270-00017. [DOI] [PubMed] [Google Scholar]
- 23.Koka P., Cecka J.M. Sex and age effects in renal transplantation. Clin Transpl. 1990:437–446. [PubMed] [Google Scholar]
- 24.Schaubel D.E., Stewart D.E., Morrison H.I., et al. Sex inequality in kidney transplantation rates. Arch Intern Med. 2000;160:2349–2354. doi: 10.1001/archinte.160.15.2349. [DOI] [PubMed] [Google Scholar]
- 25.Busson M., Benoit G. Is matching for sex and age beneficial to kidney graft survival? Société Française de Transplantation and Association France Transplant. Clin Transpl. 1997;11:15–18. [PubMed] [Google Scholar]
- 26.Johnson C.D., Wicks M.N., Milstead J., et al. Racial and gender differences in quality of life following kidney transplantation. Image J Nurs Sch. 1998;30:125–130. doi: 10.1111/j.1547-5069.1998.tb01266.x. [DOI] [PubMed] [Google Scholar]
- 27.Kwon O.J., Lee H.G., Kwak J.Y. The impact of donor and recipient age on the outcome of kidney transplantation. Transplant Proc. 2004;36:2043–2045. doi: 10.1016/j.transproceed.2004.07.047. [DOI] [PubMed] [Google Scholar]
- 28.Meier-Kriesche H.U., Ojo A.O., Leavey S.F., et al. Gender differences in the risk for chronic renal allograft failure. Transplantation. 2001;71:429–432. doi: 10.1097/00007890-200102150-00016. [DOI] [PubMed] [Google Scholar]
- 29.Oh C.K., Kim S.J., Kim J.H., et al. Influence of donor and recipient gender on early graft function after living donor kidney transplantation. Transplant Proc. 2004;36:2015–2017. doi: 10.1016/j.transproceed.2004.06.049. [DOI] [PubMed] [Google Scholar]
- 30.Shibue T., Kondo K., Iwaki Y., Terasaki P.I. Effect of sex on kidney transplants. Clin Transpl. 1987:351–360. [PubMed] [Google Scholar]
- 31.Kayler L.K., Rasmussen C.S., Dykstra D.M., et al. Gender imbalance and outcomes in living donor renal transplantation in the United States. Am J Transplant. 2003;3:452–458. doi: 10.1034/j.1600-6143.2003.00086.x. [DOI] [PubMed] [Google Scholar]
- 32.Zeier M., Döhler B., Opelz G., Ritz E. The effect of donor gender on graft survival. J Am Soc Nephrol. 2002;13:2570–2576. doi: 10.1097/01.asn.0000030078.74889.69. [DOI] [PubMed] [Google Scholar]
- 33.Patzer R.E., Plantinga L.C., Paul S., et al. Variation in dialysis facility referral for kidney transplantation among patients with end-stage renal disease in Georgia. JAMA. 2015;314:582–594. doi: 10.1001/jama.2015.8897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patzer R.E., McPherson L., Wang Z., et al. Dialysis facility referral and start of evaluation for kidney transplantation among patients treated with dialysis in the Southeastern United States. Am J Transplant. 2020;20:2113–2125. doi: 10.1111/ajt.15791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Segev D.L., Simpkins C.E., Thompson R.E., et al. Obesity impacts access to kidney transplantation. J Am Soc Nephrol. 2008;19:349–355. doi: 10.1681/asn.2007050610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gill J.S., Hendren E., Dong J., et al. Differential association of body mass index with access to kidney transplantation in men and women. Clin J Am Soc Nephrol. 2014;9:951–959. doi: 10.2215/cjn.08310813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patzer R.E., Retzloff S., Buford J., et al. Community engagements to improve equity in kidney transplantation from the group up: the Southeastern Kidney Transplant Coalition. Curr Transplant Rep. 2021;8:324–332. doi: 10.1007/s40472-021-00346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patzer R.E., Gander J., Sauls L., et al. The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol. 2014;15:171. doi: 10.1186/1471-2369-15-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heidari S., Babor T.F., De Castro P., et al. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2016;1:2. doi: 10.1186/s41073-016-0007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Segev D.L., Kucirka L.M., Oberai P.C., et al. Age and comorbidities are effect modifiers of gender disparities in renal transplantation. J Am Soc Nephrol. 2009;20:621–628. doi: 10.1681/asn.2008060591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salter M.L., Gupta N., Massie A.B., et al. Perceived frailty and measured frailty among adults undergoing hemodialysis: a cross-sectional analysis. BMC Geriatr. 2015;15:52. doi: 10.1186/s12877-015-0051-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puts M.T.E., Toubasi S., Andrew M.K., et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age Ageing. 2017;46:383–392. doi: 10.1093/ageing/afw247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monson R.S., Kemerley P., Walczak D., et al. Disparities in completion rates of the medical prerenal transplant evaluation by race or ethnicity and gender. Transplantation. 2015;99:236–242. doi: 10.1097/tp.0000000000000271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patzer R.E., McClellan W.M. Influence of race, ethnicity and socioeconomic status on kidney disease. Nat Rev Nephrol. 2012;8:533–541. doi: 10.1038/nrneph.2012.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Di Cocco P., Okoye O., Almario J., et al. Obesity in kidney transplantation. Transpl Int. 2020;33:581–589. doi: 10.1111/tri.13547. [DOI] [PubMed] [Google Scholar]
- 46.McPherson L.J., Barry V., Yackley J., et al. Distance to kidney transplant center and access to early steps in the kidney transplantation process in the Southeastern United States. Clin J Am Soc Nephrol. 2020;15:539–549. doi: 10.2215/CJN.08530719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paul S., Plantinga L.C., Pastan S.O., et al. Standardized transplantation referral ratio to assess performance of transplant referral among dialysis facilities. Clin J Am Soc Nephrol. 2018;13:282–289. doi: 10.2215/CJN.04690417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harding J.L., Perez A., Snow K., et al. Non-medical barriers in access to early steps of kidney transplantation in the United States—a scoping review. Transplant Rev (Orlando) 2021;35:100654. doi: 10.1016/j.trre.2021.100654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim S.J., Gill J.S., Knoll G., et al. Referral for kidney transplantation in Canadian provinces. J Am Soc Nephrol. 2019;30:1708–1721. doi: 10.1681/ASN.2019020127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Salter M.L., McAdams-Demarco M.A., Law A., et al. Age and sex disparities in discussions about kidney transplantation in adults undergoing dialysis. J Am Geriatr Soc. 2014;62:843–849. doi: 10.1111/jgs.12801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Melk A., Babitsch B., Borchert-Mörlins B., et al. Equally interchangeable? How sex and gender affect transplantation. Transplantation. 2019;103:1094–1110. doi: 10.1097/tp.0000000000002655. [DOI] [PubMed] [Google Scholar]
- 52.Lipford K.J., McPherson L., Hamoda R., et al. Dialysis facility staff perceptions of racial, gender, and age disparities in access to renal transplantation. BMC Nephrol. 2018;19:5. doi: 10.1186/s12882-017-0800-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salter M.L., Gupta N., King E., et al. Health-related and psychosocial concerns about transplantation among patients initiating dialysis. Clin J Am Soc Nephrol. 2014;9:1940–1948. doi: 10.2215/cjn.03310414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ward B.W., Black L.I. State and regional prevalence of diagnosed multiple chronic conditions among adults aged ≥18 years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:735–738. doi: 10.15585/mmwr.mm6529a3. [DOI] [PubMed] [Google Scholar]
- 55.US Census Bureau 2008-2019 American Community Survey, 1-year estimates. US Census Bureau. https://www.census.gov/programs-surveys/acs
- 56.Kim J.P., Desai M., Chertow G.M., Winkelmayer W.C. Validation of reported predialysis nephrology care of older patients initiating dialysis. J Am Soc Nephrol. 2012;23:1078–1085. doi: 10.1681/ASN.2011080871. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.