Abstract
Aim: The 2017 Japan Atherosclerosis Society (JAS) familial hypercholesterolemia (FH) criteria adopt a cut-off value of ≥ 9 mm of Achilles tendon thickness (ATT) detected by X-ray as one of the three key items. This threshold was determined based on an old data evaluating the ATT of 36 non-FH individuals that was published in 1977. Although the specificity of these clinical criteria is extremely high due to a strict threshold, there are a significant number of patients with FH whose ATT <9 mm. We aimed to determine a cut-off value of ATT detected by X-ray to differentiate FH and non-FH based on genetic diagnosis.
Methods: The individuals (male/female=486/501) with full assessments of genetic analyses for FH-genes (LDLR andPCSK9), serum lipids, and ATT detected by X-ray at the Kanazawa University Hospital and National Cerebral and Cardiovascular Center Research Institute were included in this study. Receiver operating characteristic (ROC) analyses were conducted to determine a better cut-off value of ATT that predicts the pathogenic mutation of FH.
Results: The ROC analyses revealed that the best cut-off values of ATT are 7.6 mm for male and 7.0 mm for female, with the sensitivities/specificities of 0.83/0.83 for male and 0.86/0.85 for female, respectively. If the thresholds of ATT of 8.0/7.5 mm and 7.5/7.0 mm were applied to the diagnosis of male/female FH, the sensitivities/specificities predicting the pathogenic mutation of FH by the 2017 JAS FH clinical criteria would be 0.82/0.90 and 0.85/0.88, respectively.
Conclusions: These results suggest that the cut-off value of ATT detected by X-ray is obviously lower than 9.0 mm, which was adopted by the 2017 JAS FH clinical criteria.
Keywords: Familial hypercholesterolemia, Genetic diagnosis, Low-density lipoprotein cholesterol, Low-density lipoprotein receptor, Proprotein convertase subtilisin/kexin type 9
Hayato Tada, Mika Hori, Kota Matsuki, Masa-aki Kawashiri, and Mariko Harada-Shiba contributed equally to this work.
See editorial vol. 29: 808-810
Introduction
Familial hypercholesterolemia (FH; OMIM #143890) is a relatively common genetic disorder that is associated with coronary artery disease (CAD) 1) . Currently, the prevalence of FH is considered to be 1 in 300 individuals 2 , 3) . An early diagnosis of FH is important to prevent early cardiovascular events and death through an appropriate treatment 4 - 6) . Despite the rigorous efforts to spread awareness of FH 7 , 8) , the diagnostic rates of FH in most countries, except for some European countries, are still quite low 9) . The current Japanese Atherosclerosis Society (JAS) FH clinical criteria developed in 2017 adopt three major clinical components, namely, baseline low-density lipoprotein (LDL) cholesterol levels, existence of tendon xanthomas, and family history of FH and/or premature CAD 10) . The 2017 JAS FH criteria are unique in terms of adopting quantitative threshold of Achilles tendon thickness (ATT) (≥ 9 mm detected by X-ray), which was determined by mean ATT value plus 2 standard deviation (SD) of non-FH hypercholesterolemic subjects in 1977 11) . Thus, the threshold of ATT of the 2017 JAS FH criteria (≥ 9 mm detected by X-ray) is innately specific to differentiate FH subjects from non-FH ones. However, there are a significant number of patients with FH whose ATT <9 mm, especially among young FH patients 12) . The highly specific but less-sensitive threshold of the ATT criteria may be one of the reasons of the poor diagnostic rate of FH in Japan. In addition, it has been demonstrated that there is a gender difference in ATT, which should be taken into account to ensure an accurate diagnosis 13 - 15) . Accordingly, we aimed to determine the appropriate cut-off value of ATT that predicts the presence of pathogenic mutation in FH-genes in the two major Japanese FH-care centers (Kanazawa University and National Cerebral and Cardiovascular Center Research Institute), where the genetic testing of FH has been centrally conducted upon requests from institutes all over Japan in the past two decades.
Methods
Study Population
The data of 1,529 subjects, on whom genetic analyses were conducted for the diagnosis of FH, cascade screening, and research purpose at Kanazawa University (2006–2016) and National Cerebral and Cardiovascular Center Research Institute (2005–2018), were retrospectively analyzed. The serum LDL cholesterol levels were calculated using the Friedewald formula if the serum triglyceride levels were <400 mg/dL; otherwise, they were directly determined enzymatically. The serum LDL cholesterol levels were evaluated prior to the initiation of lipid-lowering therapies. Among 1,529 study subjects, 543 were excluded from this study due to missing values ( Fig.1 ) .
Fig.1.
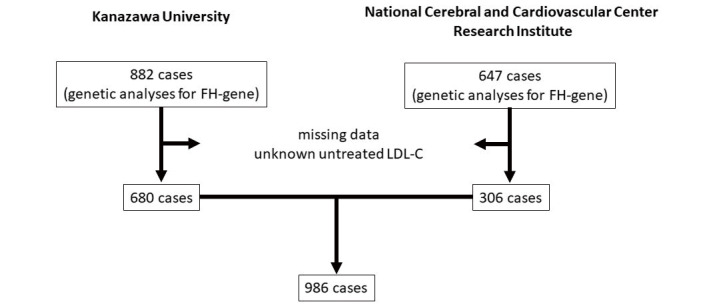
CONSORT flow diagram for study inclusion
Genetic Analysis
The coding regions of LDL receptor (LDLR) and proprotein convertase subtilisin/kexin type 9 (PCSK9) were sequenced in each institute as previously described 16 , 17) . In addition, the multiplex ligation-dependent probe amplification (MLPA) method for large rearrangement mutations was employed using the P062B LDLR MLPA Kit (MRC Holland, Amsterdam, Netherlands). At first, any variant whose minor allele frequency was 5% or greater was filtered out. Non-synonymous mutations were defined as those with any alteration(s) of the amino acid sequence of a protein as usually considered. The effects on proteins were determined using the Human Genome Variation Society (HGVS) website as reference, where we can obtain multiple sources of information from a variety of similar sources. The Human Gene Mutation Database (HGMD) Professional 2019.4 (Qiagen, Hilden, Germany) was also referred. Moreover, the American College of Medical Genetics and Genomics (ACMG) guideline was used as reference if the variants met the criteria of pathogenicity of the variants 18) . A variant was considered to be pathogenic mutation if it fulfilled any of the following criteria: 1) protein-truncated mutations; 2) registered as pathogenic in Clinvar, or HGMD, or met the criteria of the ACMG guideline; or 3) fulfilled the CADD score, which integrates diverse genome annotations using conservation matrices as well as protein-based matrices (~63 different tools) into a single measure >10 19 - 21) .
Ethical Considerations
The study was approved by the ethics committee of Kanazawa University (2019-321) and National Cerebral and Cardiovascular Center Research Institute (M17-056-20). All the procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. The informed consent for genetic analyses was obtained from all the subjects for study inclusion.
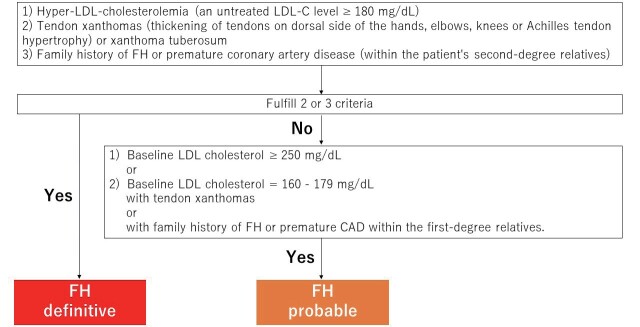
Diagnostic Flow Chart of Definitive-FH and Probable-FH
According to the JAS FH criteria, patients were diagnosed as definitive-FH if they fulfilled two or more of the clinical criteria. We defined “probable-FH” if the patients fulfilled either 1) baseline LDL cholesterol ≥ 250 mg/dL or 2) baseline LDL cholesterol ranging from 160 to 179 mg/dL with tendon xanthomas or family history of FH or premature CAD within the first-degree relatives ( Supplemental Fig.1 ) .
Supplemental Fig.1.
Diagnostic flow chart of definitive-FH and probable-FH
Statistical Analysis
The categorical variables were expressed as percentages and compared using Fisher’s exact test or the chi-squared test, whichever was appropriate. The continuous variables with a normal distribution were expressed as means±SD. The variables that were not normally distributed were expressed as median and interquartile range (IQR). The mean values of continuous variables were compared using Student’s t-test for independent data, whereas the median values were compared using the nonparametric Wilcoxon–Mann–Whitney rank-sum test; chi-squared test was also used for categorical variables, along with Fisher’s post hoc test. Receiver operating characteristic (ROC) curve analysis was conducted, and the areas under the curve (AUCs) were calculated to estimate the presence of the pathogenic mutation of FH. Pearson’s correlation coefficients were calculated between age and ATT. Statistical analysis was conducted using the R statistical package (https://www.r-project.org). P-values of <0.05 were considered statistically significant.
Results
Clinical Characteristics
The clinical characteristics of the study subjects are presented in Table 1 . Their mean age was 48 years, and the gender was balanced (male=485, 49.2%). The median total cholesterol level was 280 mg/dL (IQR, 227–332 mg/dL), and the median LDL cholesterol level was 193 mg/dL (IQR, 144–252 mg/dL). The median ATT was 7.3 mm (IQR 5.85–10.50 mm). A quarter of the study subjects had histories of prior CAD. Pathogenic FH-gene mutations were found in 485 study subjects.
Table 1. Clinical characteristics.
| All | Male | Female | P-value | |
|---|---|---|---|---|
| (N = 986) | (N = 485) | (N = 501) | ||
| Age (years) | 48±17 | 48±16 | 48±17 | NS |
| Male (%) | 485 (49.2 %) | |||
| Smoking (%) | 348 (35.2 %) | 297 (61.2 %) | 51 (10.2 %) | <0.05 |
| Total cholesterol (mg/dL) | 280 [227-332] | 263 [217-319] | 293 [237-346] | <0.05 |
| Triglyceride (mg/dL) | 114 [77-175] | 134 [90-198] | 99 [69-149] | <0.05 |
| HDL cholesterol (mg/dL) | 51 [42-62] | 45 [37-54] | 57 [48-68] | <0.05 |
| LDL cholesterol (mg/dL) | 193 [144-252] | 184 [134-240] | 203 [153-264] | <0.05 |
| Family history of FH (%) | 301 (30.5 %) | 123 (25.4 %) | 178 (35.5 %) | <0.05 |
| ATT (mm) | 7.30 [5.85-10.50] | 7.40 [6.05-10.40] | 7.20 [5.60-10.50] | <0.05 |
| FH mutation (%) | 485 (49.2 %) | 220 (45.4 %) | 265 (52.9 %) | <0.05 |
| History of prior CAD (%) | 230 (23.3 %) | 158 (32.6 %) | 72 (14.4 %) | <0.05 |
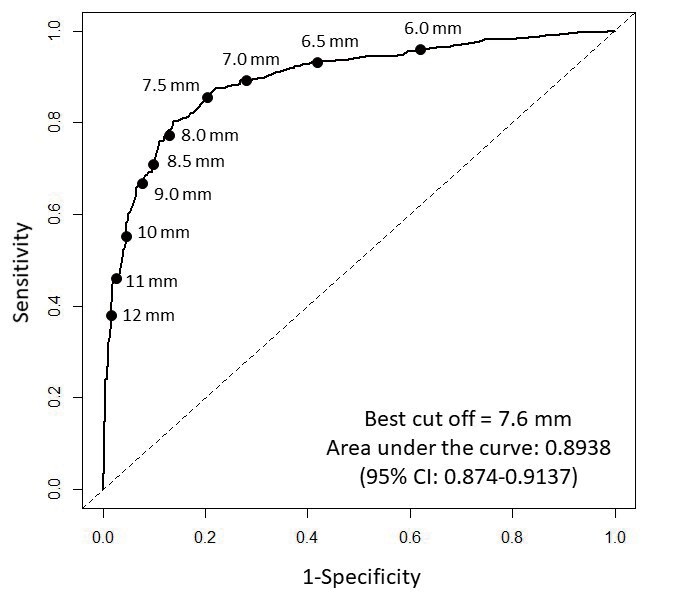
The Best Cut-Off Value Predicting the Presence of the Pathogenic Mutation of FH
First, we conducted an ROC analysis using all of the study subjects; the analysis revealed that the best cut-off value of ATT is 7.6 mm ( Fig.2 ) . The sensitivity, specificity, positive predictive value, and negative predictive value were 0.802, 0.863, 0.857, and 0.81, respectively. Second, we conducted ROC analysis to divide the men and women. The best cut-off value of ATT for men was 7.6 mm ( Fig.3 ) . The sensitivity, specificity, positive predictive value, and negative predictive value for men were 0.826, 0.825, 0.806, and 0.844, respectively. Similarly, the best cut-off value of ATT for women was 7.0 mm ( Fig.4 ) . The sensitivity, specificity, positive predictive value, and negative predictive value for women were 0.864, 0.848, 0.87, and 0.841, respectively. If the study subjects were divided into two groups (<30 years and ≥ 30 years), the best cut-off values of ATT among males ≥ 30 years, females ≥ 30 years, males <30 years, and females <30 years were 8.0, 7.5, 6.9, and 6.2 mm, respectively ( Supplemental Table 1 ) .
Fig.2. Receiver operating characteristic (ROC) curve analysis (men and women).
ROC curve analysis was conducted to determine the best cut-off value of ATT that predicts the presence of the pathogenic mutation of FH.
Fig.3. Receiver operating characteristic (ROC) curve analysis (men only).

ROC curve analysis was conducted to determine the best cut-off value of ATT that predicts the presence of the pathogenic mutation of FH.
Fig.4. Receiver operating characteristic (ROC) curve analysis (women only).
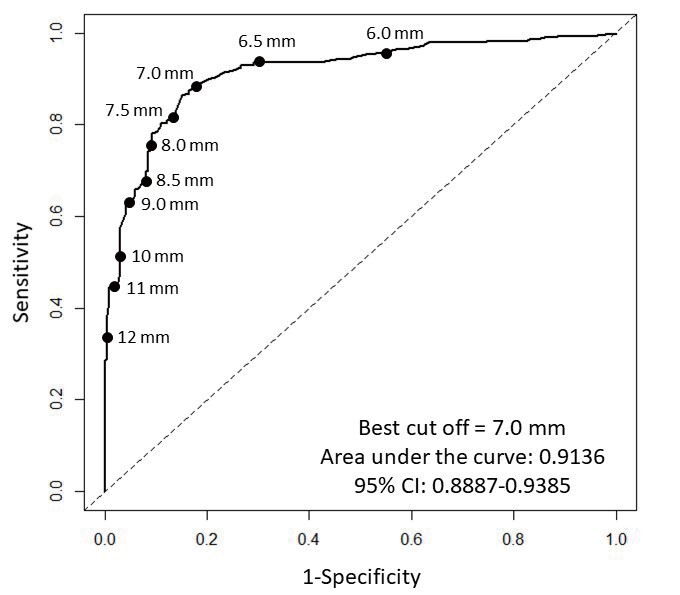
ROC curve analysis was conducted to determine the best cut-off value of ATT that predicts the presence of the pathogenic mutation of FH.
Supplemental Table 1. Best cut off point of ATT and their predictive values divided by gender, and age.
| Condition | The best cut off point of ATT (mm) | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|---|
| Male ≥ 30 years | 8.0 | 0.844 | 0.865 | 0.810 | 0.890 |
| Female ≥ 30 years | 7.5 | 0.867 | 0.904 | 0.890 | 0.883 |
| Male <30 years | 6.9 | 0.852 | 0.810 | 0.920 | 0.680 |
| Female <30 years | 6.2 | 0.870 | 0.824 | 0.952 | 0.609 |
The Proposed Best Cut-Off Value of ATT
The 2017 JAS FH criteria use three major elements for the clinical diagnosis of FH, namely, 1) LDL cholesterol ≥ 180 mg/dL, 2) tendon xanthomas (tendon xanthoma on the back of the hands, elbows, knees, etc., or Achilles tendon hypertrophy evaluated by X-ray ≥ 9 mm) or xanthoma tuberosum, and 3) family history of FH or premature CAD within the patient’s first-degree relatives. If the threshold of ATT would be revised from ≥ 9 mm to 7.5 mm (men) and 7.0 mm (women), then the sensitivity, specificity, positive predictive value, and negative predictive value would be 0.845, 0.876, 0.869, and 0.854, respectively ( Table 2 ) . Conversely, if the threshold would be increased by 0.5 mm for both genders (8.0 mm for men and 7.5 mm for women), then the sensitivity, specificity, positive predictive value, and negative predictive value would be 0.819, 0.892, 0.88, and 0.836, respectively ( Table 2 ) .
Table 2. Diagnostic accuracy predicting “definitive” FH.
| Thresholds | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| ATT ≥ 8.0/7.5 (mm) | 0.819 | 0.892 | 0.88 | 0.836 |
| ATT ≥ 7.5/7.0 (mm) | 0.845 | 0.876 | 0.869 | 0.854 |
Diagnostic Accuracy Predicting “Probable”-FH
We additionally evaluated the diagnostic accuracy predicting “probable”-FH if patients fulfilled either of the following criteria: 1) baseline LDL cholesterol ≥ 250 mg/dL or 2) baseline LDL cholesterol ranging from 160 to 179 mg/dL with tendon xanthomas or family history of FH or premature CAD within the first-degree relatives ( Supplemental Fig.1 ) . If the threshold of ATT would be lowered from ≥ 9 mm for both genders to 7.5 mm for men and 7.0 mm for women, then the sensitivity, specificity, positive predictive value, and negative predictive value would be 0.957, 0.812, 0.832, and 0.951, respectively ( Table 3 ) . Moreover, if the threshold of ATT would be lowered from ≥ 9 mm for both genders to 8.0 mm for men and 7.5 mm for women, then the sensitivity, specificity, positive predictive value, and negative predictive value would 0.957, 0.83, 0.845, and 0.952, respectively ( Table 3 ) . In addition, the predictive values by each element are presented in Supplemental Table 2 .
Table 3. Diagnostic accuracy predicting “probable” FH.
| Thresholds | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| ATT ≥ 8.0/7.5 (mm) | 0.957 | 0.83 | 0.845 | 0.952 |
| ATT ≥ 7.5/7.0 (mm) | 0.957 | 0.812 | 0.832 | 0.951 |
Supplemental Table 2. Diagnostic accuracy predicting “probable” FH by each component.
| Condition | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| Baseline LDL cholestero l ≥ 160 mg/dl with tendon xanthomas or family history of FH or premature CAD within the first-degree relatives [ATT ≥ 8.0/7.5 (mm)] | 0.798 | 0.962 | 0.953 | 0.831 |
| Baseline LDL cho lestero l ≥ 160 mg/dl with tendon xanthomas or family history of FH or premature CAD within the first-degree relatives [ATT ≥ 7.5/7.0 (mm)] | 0.942 | 0.944 | 0.942 | 0.944 |
Correlation between Age and ATT
Among patients with FH-mutation, a significant correlation between age and ATT (Pearson’s r=0.31, p <0.05, Fig.5 ) was observed but none among patients without FH-mutation (Pearson’s r=0.05, p=NS, Fig.5 ). In addition, we calculated the regression equations for ATT against age using a linear model among patients with FH-mutation. We found that the equations for both genders, male, and female were Y=7.7542+0.0885X, Y=8.3655+0.0876X, and Y=7.2055+0.0902X, respectively. Moreover, we observed a stronger correlation between age×LDL cholesterol and ATT compared with that in the simple comparison between age and ATT, suggesting that the accumulation effect of exposure to LDL cholesterol is one of the major causes of ATT (Pearson’s r=0.46, p <0.05, Fig.6 ).
Fig.5. Correlation between age and ATT.
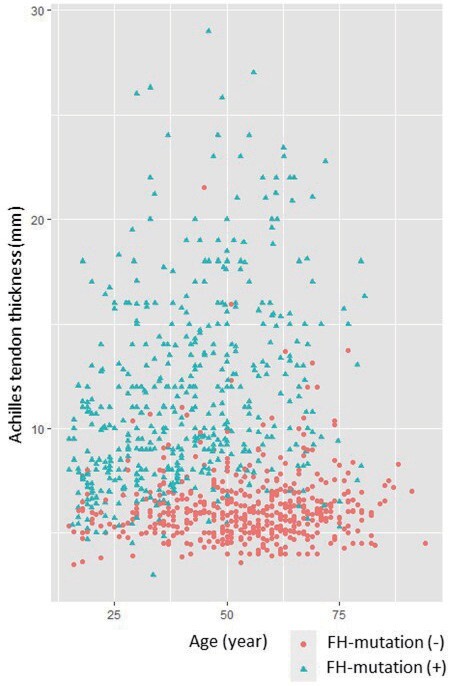
X-axis represents age. Y-axis represents ATT. Green triangles indicate patients with FH-mutation. Red circles indicate patients without FH-mutation.
Fig.6. Correlation between age×LDL cholesterol and ATT.
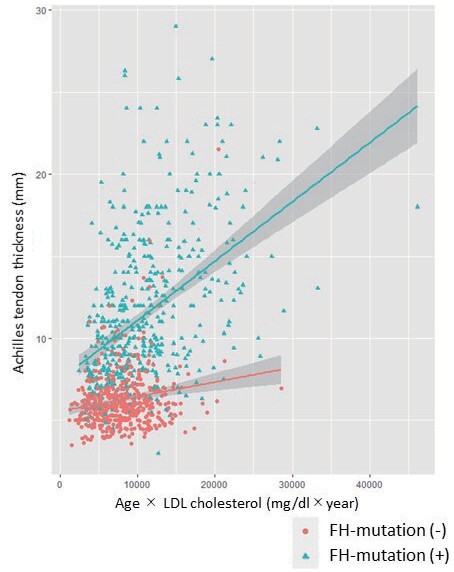
X-axis represents age×LDL cholesterol. Y-axis represents ATT. Green triangles indicate patients with FH-mutation. Red circles indicate patients without FH-mutation.
Discussion
Recent studies have repeatedly demonstrated that FH is common among the general population worldwide 2 , 3) . Importantly, the life expectancy of FH without accurate diagnosis and effective lipid-lowering therapy is limited by CAD. However, FH is still underdiagnosed in Japan, partially due to the excessively specific cut-off value of ATT 10) . In the current study, we aimed to determine a more appropriate cut-off value of ATT to clinically diagnose FH in Japan. As a result, the current cut-off value of ATT (9 mm) was found to be highly specific but poorly sensitive. Thus, the threshold of ATT seems to be lowered to increase the sensitivity. Moreover, the current threshold of ATT evaluated by X-ray (≥ 9 mm for both genders) does not account for gender difference. In this regard, there are several studies using ultrasound suggesting that the threshold of ATT to diagnose FH among males was higher than that among females 13 - 15) . In this study, we have demonstrated that the threshold of ATT evaluated by X-ray among males should also be higher than that among females. Moreover, we found that ATT was significantly associated with age among patients with FH-mutation. The age-dependent ATT cut-off values may improve the sensitivity and specificity for the diagnosis of FH. However, it is difficult to use the above equation for the diagnosis of FH as the development of ATT may not be linear with age. Furthermore, the intercepts of both equations are apparently larger than those observed among pediatric FH patients. If the study subjects were divided into two groups (<30 years and ≥ 30 years), the best cut-off values of ATT for older individuals were greater than those for younger individuals. Although the number of the study subjects <30 years is not sufficient to make conclusive results, the ATT threshold of 8.0 mm for male and 7.5 mm for female may be fine at least for older individuals (≥ 30 years). Meanwhile, our data showed that the development of ATT appears to be different between genders; thus, it would be reasonable to determine a different threshold of ATT for each gender.
Because FH is an autosomal genetic disorder, gene diagnosis is definitively essential 22 - 24) . However, there are several major hurdles that are currently under debate. First, it is sometimes quite difficult to determine the pathogenicity of the mutations. For this concern, there are many reliable publications containing the list of pathogenic mutations of FH 21 , 25) . In addition, we can defer the determination of the pathogenicity of the variants as VUS (variant of unknown significance) if the pathogenicity of the variants is unclear. These strategies are already acceptable in many other genetic disorders. Second, there is some criticism with regard to the determination of genetic backgrounds of the patients. However, the judgment of whether or not to take genetic testing is entrusted to the patients. Third, there is still a portion of FH patients without FH-mutation. In this regard, we need to keep in mind that genetic testing is important for the diagnosis of genetic disorders, whereas a negative result in genetic testing does not necessarily mean that they are free from the disorders.
In our institute, genetic analysis for FH has long been conducted not only for individuals suspected to have FH but also for those clinically diagnosed with FH. In addition, intensive cascade screening, where the patients’ relatives are screened regardless of their LDL cholesterol levels, has been performed, making it possible to assess the threshold of ATT that predicts FH-mutation by recruiting individuals whose LDL cholesterol levels are relatively low.
The current study has several limitations. First, the study was conducted within only two institutes. However, Kanazawa University and National Cerebral and Cardiovascular Center Research Institute are the top two FH-care centers in Japan, and most of the evidence in this field in Japan has been established by these two centers. Furthermore, most of the genetic testings of FH in Japan have been conducted upon requests from institutes all over Japan at these two centers in the past two decades. Thus, this study covers the largest database in Japanese FH. Second, we did not conduct functional analyses in this study to validate the pathogenicity of the genetic mutations. Third, there is at least a portion of individuals who are known/unknown FH-mutation positive FH, but we could not identify the pathogenic mutations. Fourth, we could not conduct genetic analyses and assessments of ATT in individuals with FH or those suspected to have FH from all over Japan. Moreover, we could not include all the relatives of the patients with FH or suspected to have FH despite our vigorous effort exerted toward cascade screening. This may leave room for some bias.
In conclusion, the cut-off value of ATT detected by X-ray is obviously lower than 9.0 mm, which was adopted by the 2017 JAS FH clinical criteria.
Acknowledgements
None declared.
Sources of Funding
This work has been supported by scientific research grants from the Ministry of Education, Science and Culture of Japan (19K08575), Health, Labour and Welfare Sciences Research Grant for Research on Rare and Intractable Diseases (H30-nanji-ippan-003), and Japanese Circulation Society (project for genome analysis in cardiovascular diseases) and the Japan Agency for Medical Research and Development (16ek0210075h0001).
Conflicts of Interest
Hayato Tada receives research finding from KUBIX Inc, receives scholarship grants from Bayer Yakuhin, Ltd, MSD K.K, and Sanofi K.K. Mika Hori, Kota Matsuki, Atsushi Nohara, and Masa-aki Kawashiri has nothing to disclose. Masatsune Ogura receives lecture fees from Amgen, and Astellas Pharma Inc. Mariko Harada-Shiba holds stocks of Liid Pharma, receives lecture fees from Amgen, Astellas Pharma Inc, and Sanofi, receives scholarship grants from Aegerion, Recordati, and Kaneka.
References
- 1).Mabuchi H. Half a Century Tales of Familial Hypercholesterolemia (FH) in Japan. J Atheroscler Thromb, 2017; 24: 189-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Beheshti SO, Madsen CM, Varbo A, Nordestgaard BG. Worldwide Prevalence of Familial Hypercholesterolemia: Meta-Analyses of 11 Million Subjects. J Am Coll Cardiol, 2020; 75: 2553-2566 [DOI] [PubMed] [Google Scholar]
- 3).Hu P, Dharmayat KI, Stevens CAT, Sharabiani MTA, Jones RS, Watts GF, Genest J, Ray KK, Vallejo-Vaz AJ. Prevalence of Familial Hypercholesterolemia Among the General Population and Patients With Atherosclerotic Cardiovascular Disease: A Systematic Review and Meta-Analysis. Circulation, 2020; 141: 1742-1759 [DOI] [PubMed] [Google Scholar]
- 4).Harada-Shiba M, Sugisawa T, Makino H, Abe M, Tsushima M, Yoshimasa Y, Yamashita T, Miyamoto Y, Yamamoto A, Tomoike H, Yokoyama S. Impact of statin treatment on the clinical fate of heterozygous familial hypercholesterolemia. J Atheroscler Thromb, 2010; 17: 667-674 [DOI] [PubMed] [Google Scholar]
- 5).Luirink IK, Wiegman A, Kusters DM, Hof MH, Groothoff JW, de Groot E, Kastelein JJP, Hutten BA. 20-Year Follow-up of Statins in Children with Familial Hypercholesterolemia. N Engl J Med, 2019; 381: 1547-1556 [DOI] [PubMed] [Google Scholar]
- 6).Tada H, Okada H, Nomura A, Nohara A, Yamagishi M, Takamura M, Kawashiri MA. Prognostic Impact of Cascade Screening for Familial Hypercholesterolemia on Cardiovascular Events. J Clin Lipidol, 2021 in press [DOI] [PubMed] [Google Scholar]
- 7).EAS Familial Hypercholesterolaemia Studies Collaboration, Vallejo-Vaz AJ, De Marco M, Stevens CAT, Akram A, Freiberger T, Hovingh GK, Kastelein JJP, Mata P, Raal FJ, Santos RD, Soran H, Watts GF, Abifadel M, Aguilar-Salinas CA, Al-Khnifsawi M, AlKindi FA, Alnouri F, Alonso R, Al-Rasadi K, Al-Sarraf A, Ashavaid TF, Binder CJ, Bogsrud MP, Bourbon M, Bruckert E, Chlebus K, Corral P, Descamps O, Durst R, Ezhov M, Fras Z, Genest J, Groselj U, Harada-Shiba M, Kayikcioglu M, Lalic K, Lam CSP, Latkovskis G, Laufs U, Liberopoulos E, Lin J, Maher V, Majano N, Marais AD, März W, Mirrakhimov E, Miserez AR, Mitchenko O, Nawawi HM, Nordestgaard BG, Paragh G, Petrulioniene Z, Pojskic B, Postadzhiyan A, Reda A, Reiner Ž, Sadoh WE, Sahebkar A, Shehab A, Shek AB, Stoll M, Su TC, Subramaniam T, Susekov AV, Symeonides P, Tilney M, Tomlinson B, Truong TH, Tselepis AD, Tybjærg-Hansen A, Vázquez-Cárdenas A, Viigimaa M, Vohnout B, Widén E, Yamashita S, Banach M, Gaita D, Jiang L, Nilsson L, Santos LE, Schunkert H, Tokgözoğlu L, Car J, Catapano AL, Ray KK; EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC) Investigators. Overview of the current status of familial hypercholesterolaemia care in over 60 countries - The EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Atherosclerosis, 2018; 277: 234-255 [DOI] [PubMed] [Google Scholar]
- 8).Bucholz EM, Rodday AM, Kolor K, Khoury MJ, de Ferranti SD. Prevalence and Predictors of Cholesterol Screening, Awareness, and Statin Treatment Among US Adults With Familial Hypercholesterolemia or Other Forms of Severe Dyslipidemia (1999-2014). Circulation, 2018; 137: 2218-2230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, Wiklund O, Hegele RA, Raal FJ, Defesche JC, Wiegman A, Santos RD, Watts GF, Parhofer KG, Hovingh GK, Kovanen PT, Boileau C, Averna M, Borén J, Bruckert E, Catapano AL, Kuivenhoven JA, Pajukanta P, Ray K, Stalenhoef AF, Stroes E, Taskinen MR, Tybjærg-Hansen A; European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J, 2013; 34: 3478-2490a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Harada-Shiba M, Arai H, Ishigaki Y, Ishibashi S, Okamura T, Ogura M, Dobashi K, Nohara A, Bujo H, Miyauchi K, Yamashita S, Yokote K; Working Group by Japan Atherosclerosis Society for Making Guidance of Familial Hypercholesterolemia. Guidelines for Diagnosis and Treatment of Familial Hypercholesterolemia 2017. J Atheroscler Thromb, 2018; 25: 751-770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Mabuchi H, Ito S, Haba T, Ueda K, Ueda R. Discrimination of familial hypercholesterolemia and secondary hypercholesterolemia by Achilles’ tendon thickness. Atherosclerosis, 1977; 28: 61-68 [DOI] [PubMed] [Google Scholar]
- 12).Tada H, Okada H, Nomura A, Nohara A, Usui S, Sakata K, Takamura M, Kawashiri MA. A reassessment of the Japanese clinical diagnostic criteria of familial hypercholesterolemia in a hospital-based cohort using comprehensive genetic analysis. Pract Lab Med, 2020; 22: e00180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Descamps OS, Leysen X, Van Leuven F, Heller FR. The use of Achilles tendon ultrasonography for the diagnosis of familial hypercholesterolemia. Atherosclerosis, 2001; 157: 514-518 [DOI] [PubMed] [Google Scholar]
- 14).Junyent M, Gilabert R, Zambón D, Núñez I, Vela M, Civeira F, Pocoví M, Ros E. The use of Achilles tendon sonography to distinguish familial hypercholesterolemia from other genetic dyslipidemias. Arterioscler Thromb Vasc Biol, 2005; 25: 2203-2208 [DOI] [PubMed] [Google Scholar]
- 15).Michikura M, Ogura M, Yamamoto M, Sekimoto M, Fuke C, Hori M, Arai K, Kihara S, Hosoda K, Yanagi K, Harada-Shiba M. Achilles Tendon Ultrasonography for Diagnosis of Familial Hypercholesterolemia Among Japanese Subjects. Circ J, 2017; 81: 1879-1885 [DOI] [PubMed] [Google Scholar]
- 16).Tada H, Kawashiri MA, Nomura A, Teramoto R, Hosomichi K, Nohara A, Inazu A, Mabuchi H, Tajima A, Yamagishi M. Oligogenic familial hypercholesterolemia, LDL cholesterol, and coronary artery disease. J Clin Lipidol, 2018; 12: 1436-1444 [DOI] [PubMed] [Google Scholar]
- 17).Hori M, Ohta N, Takahashi A, Masuda H, Isoda R, Yamamoto S, Son C, Ogura M, Hosoda K, Miyamoto Y, Harada-Shiba M. Impact of LDLR and PCSK9 pathogenic variants in Japanese heterozygous familial hypercholesterolemia patients. Atherosclerosis, 2019; 289: 101-108 [DOI] [PubMed] [Google Scholar]
- 18).Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL; ACMG Laboratory Quality Assurance Committee. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med, 2015; 17: 405-424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet, 2014; 46: 310-315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Tada H, Kawashiri MA, Nohara A, Saito R, Tanaka Y, Nomura A, Konno T, Sakata K, Fujino N, Takamura T, Inazu A, Mabuchi H, Yamagishi M, Hayashi K. Whole exome sequencing combined with integrated variant annotation prediction identifies asymptomatic Tangier disease with compound heterozygous mutations in ABCA1 gene. Atherosclerosis, 2015; 240: 324-329 [DOI] [PubMed] [Google Scholar]
- 21).Tada H, Hori M, Nomura A, Hosomichi K, Nohara A, Kawashiri MA, Harada-Shiba M. A catalog of the pathogenic mutations of LDL receptor gene in Japanese familial hypercholesterolemia. J Clin Lipidol, 2020; 14: 346-351 [DOI] [PubMed] [Google Scholar]
- 22).Tada H, Kawashiri MA, Nohara A, Inazu A, Mabuchi H, Yamagishi M. Impact of clinical signs and genetic diagnosis of familial hypercholesterolaemia on the prevalence of coronary artery disease in patients with severe hypercholesterolaemia. Eur Heart J, 2017; 38: 1573-1579 [DOI] [PubMed] [Google Scholar]
- 23).Sturm AC, Knowles JW, Gidding SS, Ahmad ZS, Ahmed CD, Ballantyne CM, Baum SJ, Bourbon M, Carrié A, Cuchel M, de Ferranti SD, Defesche JC, Freiberger T, Hershberger RE, Hovingh GK, Karayan L, Kastelein JJP, Kindt I, Lane SR, Leigh SE, Linton MF, Mata P, Neal WA, Nordestgaard BG, Santos RD, Harada-Shiba M, Sijbrands EJ, Stitziel NO, Yamashita S, Wilemon KA, Ledbetter DH, Rader DJ; Convened by the Familial Hypercholesterolemia Foundation. Clinical Genetic Testing for Familial Hypercholesterolemia: JACC Scientific Expert Panel. J Am Coll Cardiol, 2018; 72: 662-680 [DOI] [PubMed] [Google Scholar]
- 24).Musunuru K, Hershberger RE, Day SM, Klinedinst NJ, Landstrom AP, Parikh VN, Prakash S, Semsarian C, Sturm AC; American Heart Association Council on Genomic and Precision Medicine; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Genetic Testing for Inherited Cardiovascular Diseases: A Scientific Statement From the American Heart Association. Circ Genom Precis Med, 2020; 13: e000067 [DOI] [PubMed] [Google Scholar]
- 25).Bourbon M, Alves AC, Sijbrands EJ. Low-density lipoprotein receptor mutational analysis in diagnosis of familial hypercholesterolemia. Curr Opin Lipidol, 2017; 28: 120-129 [DOI] [PubMed] [Google Scholar]