Abstract
Aims/hypothesis
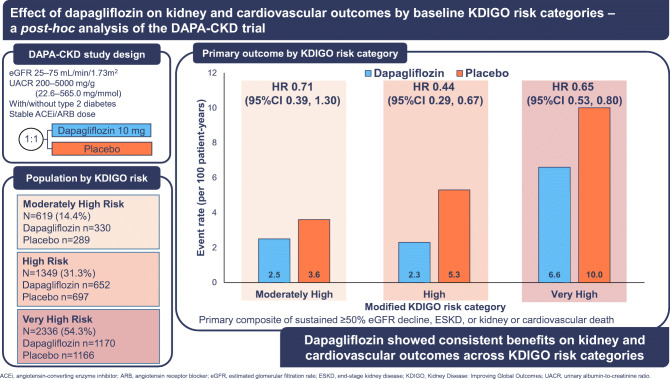
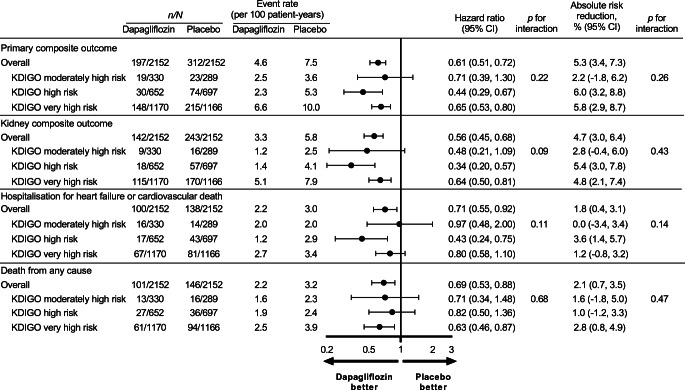
In the Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) trial, dapagliflozin reduced the risks of progressive kidney disease, hospitalised heart failure or cardiovascular death, and death from all causes in patients with chronic kidney disease (CKD) with or without type 2 diabetes. Patients with more severe CKD are at higher risk of kidney failure, cardiovascular events and all-cause mortality. In this post hoc analysis, we assessed the efficacy and safety of dapagliflozin according to baseline Kidney Disease Improving Global Outcomes (KDIGO) risk categories.
Methods
DAPA-CKD was a double-blind, placebo-controlled trial that randomised patients with an eGFR of 25–75 ml min−1 [1.73 m]−2 and urinary albumin/creatinine ratio (UACR) of ≥22.6 and <565.0 mg/mmol (200–5000 mg/g) to dapagliflozin 10 mg/day or placebo. The primary endpoint was a composite of ≥50% reduction in eGFR, end-stage kidney disease (ESKD), and death from a kidney or cardiovascular cause. Secondary endpoints included a kidney composite (≥50% reduction in eGFR, ESKD and death from a kidney cause), a cardiovascular composite (heart failure hospitalisation or cardiovascular death), and death from all causes. We used Cox proportional hazards regression analyses to assess relative and absolute effects of dapagliflozin across KDIGO risk categories.
Results
Of the 4304 participants in the DAPA-CKD study, 619 (14.4%) were moderately high risk, 1349 (31.3%) were high risk and 2336 (54.3%) were very high risk when categorised by KDIGO risk categories at baseline. Dapagliflozin reduced the hazard of the primary composite (HR 0.61; 95% CI 0.51, 0.72) and secondary endpoints consistently across KDIGO risk categories (all p for interaction >0.09). Absolute risk reductions for the primary outcome were also consistent irrespective of KDIGO risk category (p for interaction 0.26). Analysing patients with and without type 2 diabetes separately, the relative risk reduction with dapagliflozin in terms of the primary outcome was consistent across subgroups of KDIGO risk categories. The relative frequencies of adverse events and serious adverse events were also similar across KDIGO risk categories.
Conclusion/interpretations
The consistent benefits of dapagliflozin on kidney and cardiovascular outcomes across KDIGO risk categories indicate that dapagliflozin is efficacious and safe across a wide spectrum of kidney disease severity.
Trial registration
Funding
The study was funded by AstraZeneca.
Graphical abstract
Supplementary Information
The online version contains peer-reviewed but unedited supplementary material available at 10.1007/s00125-022-05694-6.
Keywords: Albuminuria, Dapagliflozin, eGFR, KDIGO risk categories, Kidney outcome, SGLT2 inhibitor
Introduction
Sodium–glucose cotransporter 2 (SGLT2) inhibitors were originally developed as oral glucose-lowering drugs. Previous studies showed that the HbA1c-lowering efficacy of SGLT2 inhibitors is attenuated or absent in patients with reduced eGFR [1, 2]. Due to the lack of glycaemic efficacy, it was assumed that SGLT2 inhibitors would not prevent micro- and macrovascular complications in patients with diabetes and reduced eGFR [2]. However, several clinical trials demonstrated that SGLT2 inhibitors prevent progression of chronic kidney disease (CKD), kidney failure, and cardiovascular events in patients with CKD [3–5]. The Canagliflozin and Renal Events in Diabetes With Established Nephropathy Clinical Evaluation (CREDENCE) trial demonstrated these clinical benefits in patients with type 2 diabetes and CKD [3]. The Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) trial extended these findings to a broader population of patients with CKD, with or without type 2 diabetes, and the results were independent of the degree of glycaemic control [4, 6, 7].
Higher albuminuria and lower eGFR are well-established predictors of kidney failure and cardiovascular events, and form the foundation of the Kidney Disease Improving Global Outcomes (KDIGO) CKD disease classification system [8]. The inclusion of both albuminuria and eGFR in the KDIGO CKD classification system allows cardiovascular and kidney risk categorisation based on combined albuminuria and eGFR assessment. Whether the clinical benefits of the SGLT2 inhibitor dapagliflozin in patients with CKD are generalisable to patients at various stages of CKD as defined by baseline KDIGO classification is unknown. In addition, whether the KDIGO CKD classification can be used to identify patients who may derive greater absolute benefit from dapagliflozin, or whether there are subpopulations without such benefits, has not been determined, but may guide treatment decisions in clinical practice.
In this post hoc analysis of the DAPA-CKD trial, we examined the efficacy and safety of dapagliflozin according to baseline KDIGO risk categories among patients with and without type 2 diabetes.
Methods
Study design and participants
DAPA-CKD was a randomised, double-blind, placebo-controlled multicentre, international trial conducted in 21 countries at 386 study sites. The study design and the primary results have been published previously [4, 9]. Briefly, we enrolled adult patients with CKD with and without type 2 diabetes who were ≥18 years of age with eGFR ≥25 and <75 ml min−1 [1.73 m]−2 and urinary albumin/creatinine ratio (UACR) ≥22.6 and <565.0 mg/mmol (≥200 and <5000 mg/g). Patients with type 1 diabetes, polycystic kidney disease, lupus nephritis or anti-neutrophil cytoplasm antibodies (ANCA)-associated vasculitis, as well as those receiving immunotherapy for primary or secondary kidney disease within 6 months prior to enrolment, were excluded. All eligible patients were receiving treatment with a stable dose of an ACE inhibitor or angiotensin receptor blocker for ≥4 weeks prior to randomisation unless there was a documented intolerance to these drugs. The trial protocol was approved by a central or local ethics committee at each trial site, and all participants provided written informed consent. This study was registered on ClinicalTrials.gov (NCT03036150) and posted online on 30 January 2017, prior to enrolment of the first participant.
Randomisation and follow-up
We randomly assigned eligible participants to receive dapagliflozin 10 mg once daily or matching placebo. The study drug was to be continued until the occurrence of diabetic ketoacidosis, pregnancy, receipt of disallowed therapy, or study completion. Following randomisation, in-person study visits were performed after 2 weeks, at 2, 4 and 8 months, and at 4-month intervals thereafter. At each follow-up visit, we recorded vital signs, sent blood and urine samples for laboratory assessment, and collected information on potential study endpoints, adverse events, concomitant therapies and study drug adherence.
Classification of KDIGO risk categories
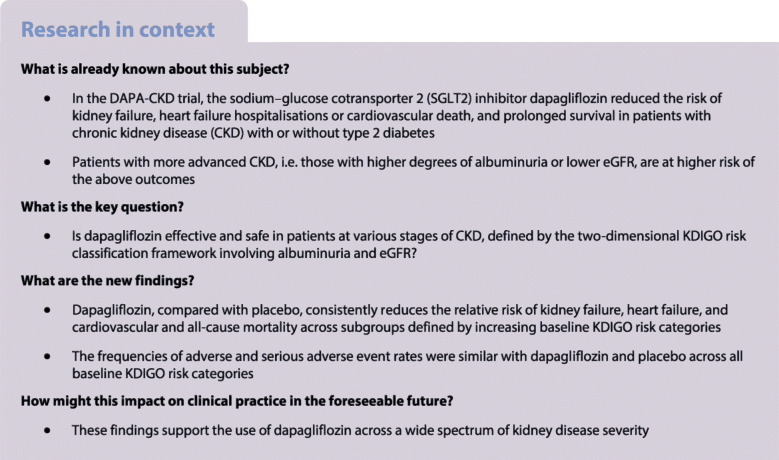
We categorised patients according KDIGO risk categories based on their eGFR and albuminuria level. As many DAPA-CKD participants were categorised in the original very high KDIGO risk category, we created an additional category in order to stratify the cohort across three subgroups with approximately equal sample sizes. We therefore defined the following categories in this study (Fig. 1): moderately high risk (baseline eGFR 30–44 ml min−1 [1.73 m]−2 and UACR <3.4 mg/mmol [<30 mg/g]; or baseline eGFR 45–89 ml min−1 [1.73 m]−2 and UACR 3.4–33.9 mg/mmol [30–300 mg/g]; or baseline eGFR >60 ml min−1 [1.73 m]−2 and UACR >33.9 mg/mmol [>300 mg/g]); high risk (baseline eGFR 30–44 ml min−1 [1.73 m]−2 and UACR 3.4–33.9 mg/mmol [30–300 mg/g]; or baseline eGFR 45–59 ml min−1 [1.73 m]−2 and UACR >33.9 mg/mmol [>300 mg/g]); and very high risk (baseline eGFR <30 ml min−1 [1.73 m]−2 and UACR 3.4–33.9 mg/mmol [30–300 mg/g]; or baseline eGFR <45 ml min−1 [1.73 m]−2 and UACR >33.9 mg/mmol [>300 mg/g]). The term ‘KDIGO risk categories’ used in this manuscript refers to this modified categorisation.
Fig. 1.
Number of patients by modified KDIGO risk categories. The KDIGO risk categories refer to a modified categorisation that includes an additional category of moderately high risk
Outcomes
The primary endpoint was a composite of a sustained ≥50% decline in eGFR (confirmed by a second serum creatinine measurement after at least 28 days), onset of end-stage kidney disease (ESKD, defined as maintenance dialysis for more than 28 days, kidney transplantation, or eGFR <15 ml min−1 [1.73 m]−2 confirmed by a second measurement after at least 28 days), or death from a kidney or cardiovascular cause. Secondary outcomes were, in hierarchical order: (1) a kidney-specific endpoint defined in the same way as the primary outcome but excluding death from a cardiovascular cause; (2) a cardiovascular composite endpoint of cardiovascular death or hospitalisation for heart failure; and (3) all-cause mortality. An independent blinded event adjudication committee assessed all clinical endpoints using rigorous pre-specified endpoint definitions.
Statistical analysis
The overall analytic approach, power calculation, and pre-specified statistical analysis plan have been published previously [9]. Briefly, we performed time-to-event analyses using a Cox proportional hazards regression stratified for randomisation factors (diabetes status and UACR) and adjusted for baseline eGFR. We calculated the HRs and 95% CI from the model parameter coefficients and standard errors, respectively. All analyses presented here followed the intention-to-treat principle. For the purpose of the current analysis, we evaluated the primary and secondary efficacy endpoints in patients stratified by the modified KDIGO risk categories. The effects of dapagliflozin by KDIGO risk categories were separately assessed in patients with and without type 2 diabetes. We avoided including redundant terms for the randomisation strata and subgroup factors in the statistical models when the two coincided. We compared results across KDIGO risk groups by including a multiplicative interaction term between randomised treatment group and KDIGO risk categories. We also performed exploratory analyses stratified by UACR and eGFR separately. In these analyses, we categorised patients based on baseline UACR into three categories (≤113.0 mg/mmol [≤1000 mg/g], >113.0 to ≤395.5 mg/mmol [>1000 to ≤3500 mg/g] and >395.5 mg/mmol [>3500 mg/g]) and categorised patients based on eGFR into subgroups (<30 ml min−1 [1.73 m]−2; ≥30 to <45 ml min−1 [1.73 m]−2; ≥45 ml min−1 [1.73 m]−2). In additional analyses, to investigate whether the effect of treatment varies by levels of baseline UACR, interaction was tested between treatment and UACR (continuous) separately in patients with and without type 2 diabetes. To allow for non-linearity of the effect of treatment across levels of baseline UACR, UACR was transformed by fractional polynomials. For the time-to-event analyses, we assessed the proportional hazards assumption using the Akaike’s information criterion and Schoenfeld residuals test.
We analysed the effects of dapagliflozin on the mean on-treatment eGFR slope by fitting a two-slope mixed effects linear spline model (with a knot at week 2) with a random intercept and random slopes for treatment. The model included fixed effects for treatment, baseline KDIGO category, stratification factors (diabetes status) and a continuous, fixed covariate for time-to-visit. To determine eGFR slopes for the KDIGO risk subgroup, we added to the model all possible interaction terms for treatment effect, KDIGO risk subgroup and time-to-visit, assuming an unstructured variance/covariance matrix. The mean total slope was computed as a weighted combination of the acute and chronic slopes, to reflect the mean rate of eGFR change until the last on-treatment visit. We also presented the pattern of change in mean eGFR using a restricted maximum-likelihood repeated-measures approach. This latter analysis included fixed effects of treatment, visit, treatment-by-visit interaction and treatment-by-KDIGO risk subgroup interaction. We added interaction terms among KDIGO risk subgroup, visit and treatment assignment to assess the change in eGFR within each subgroup. We considered p values <0.05 to be statistically significant, and all analyses were performed using Stata version 14.2 (StataCorp, USA) or R version 4.0.2 (R Foundation).
Results
The DAPA-CKD trial included 4304 patients, who were randomly assigned to dapagliflozin (n = 2152) or placebo (n = 2152). The mean age at baseline was 61.8 years (SD 12.1), 1425 patients were female (33.1%), the mean eGFR was 43.1 ml min−1 [1.73 m]−2 (SD 12.4), and the median UACR was 107.2 mg/mmol (IQR 53.9–213.0) (949 mg/g [IQR 477–1885]); 2906 patients had type 2 diabetes (67.5%) and 1398 patients did not have diabetes (32.5%).
When categorised by baseline KDIGO risk categories, 619 patients (14.4%) were moderately high risk, 1349 (31.3%) were at high risk, and 2336 (54.3%) were very high risk (Fig. 1). Patients in the highest KDIGO risk category were more likely to have higher systolic blood pressure and lower HbA1c compared with those with lower KDIGO risk (Table 1).
Table 1.
Baseline characteristics by baseline KDIGO risk category
| KDIGO risk categories | p valuea | |||
|---|---|---|---|---|
| Moderately high risk | High risk | Very high risk | ||
| Number of participants, n (%) | 619 (14.4) | 1349 (31.3) | 2336 (54.3) | |
| Mean age, years (SD) | 61.4 (11.6) | 62.0 (12.0) | 61.9 (12.3) | 0.54 |
| Female sex, n (%) | 203 (32.8) | 417 (30.9) | 805 (34.5) | 0.09 |
| Race, n (%) | 0.001 | |||
| White | 355 (57.3) | 698 (51.7) | 1237 (52.9) | |
| Black | 32 (5.2) | 55 (4.1) | 104 (4.4) | |
| Asian | 164 (26.5) | 490 (36.3) | 813 (34.8) | |
| Other | 68 (11.0) | 106 (7.9) | 182 (7.8) | |
| Mean BMI, kg/m2 (SD) | 29.9 (6.1) | 29.4 (6.0) | 29.5 (6.2) | 0.17 |
| Current smoker, n (%) | 86 (13.9) | 192 (14.2) | 306 (13.1) | 0.86 |
| BP, mmHg | ||||
| Systolic | 136.4 (16.2) | 136.3 (16.9) | 137.7 (17.9) | 0.047 |
| Diastolic | 77.6 (9.7) | 77.8 (10.4) | 77.3 (10.7) | 0.47 |
| eGFR, ml min−1 [1.73 m]−2 | 62.7 (8.6) | 49.5 (6.3) | 34.2 (5.9) | <0.001 |
| HbA1c, mmol/mol | 57 (20.8) | 54 (19.7) | 52 (17.5) | <0.001 |
| HbA1c, % | 7.4 (1.9) | 7.1 (1.8) | 6.9 (1.6) | <0.001 |
| Haemoglobin, g/l (SD) | 134 (18) | 132 (18) | 125 (18) | <0.001 |
| Median UACR, mg/mmol (IQR) | 58.4 (30.0–147.4) | 93.1 (47.0–193.1) | 126.9 (68.6–242.8) | <0.001 |
| Median UACR, mg/g (IQR) | 517 (265–1304) | 824 (416–1709) | 1123 (607–2149) | <0.001 |
| Type 2 diabetes, n (%) | 470 (75.9) | 915 (67.8) | 1521 (65.1) | <0.001 |
| Cardiovascular disease, n (%) | 248 (40.1) | 492 (36.5) | 870 (37.2) | 0.30 |
| Medications | ||||
| ACE inhibitor/ARB, n (%) | 613 (99.0) | 1314 (97.4) | 2247 (96.2) | 0.001 |
| Diuretics, n (%) | 234 (37.8) | 538 (39.9) | 1110 (47.5) | <0.001 |
| GLP-1 receptor agonistsb, n (%) | 20 (4.3) | 31 (3.4) | 71 (4.7) | 0.31 |
| Mineralocorticoid receptor antagonists, n (%) | 24 (3.9) | 78 (5.8) | 127 (5.4) | 0.20 |
| Statin, n (%) | 245 (39.6) | 467 (34.6) | 886 (37.9) | 0.05 |
aStatistically significant differences across the three baseline KDIGO risk categories
bOnly in patients with diabetes (n = 2906)
ARB, angiotensin receptor blocker; GLP-1, glucagon-like peptide 1
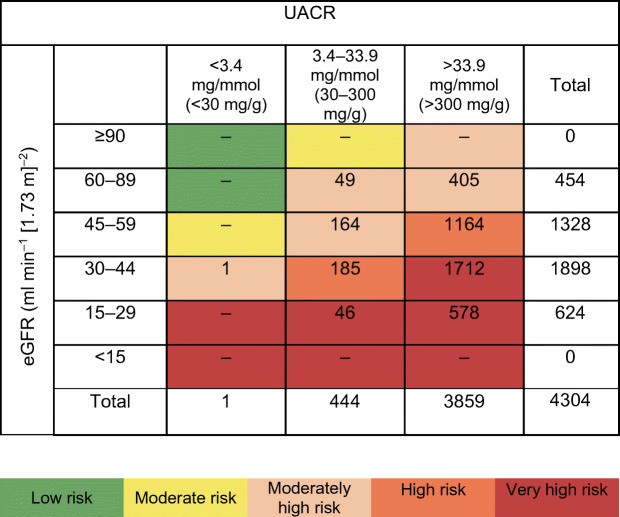
Rates of the primary and secondary endpoints by baseline KDIGO risk
Patients with a higher KDIGO risk category experienced a higher event rate for kidney and cardiovascular events, in both the placebo and dapagliflozin treatment groups. For example, patients randomised to placebo with a very high KDIGO risk experienced an event rate of 10.0 events (95% CI 8.7, 11.4) per 100 patient-years for the primary composite endpoint, while the event rate among patients with moderately high risk was 3.6 (95% CI 2.4, 5.4) (Fig. 2). The rate of heart failure hospitalisation or cardiovascular death among patients randomised to placebo with very high KDIGO risk was 3.4 events (95% CI 2.8, 4.3) per 100 patient-years compared with 2.0 (95% CI 1.2, 3.5) in patients with a moderately high KDIGO risk (Fig. 2).
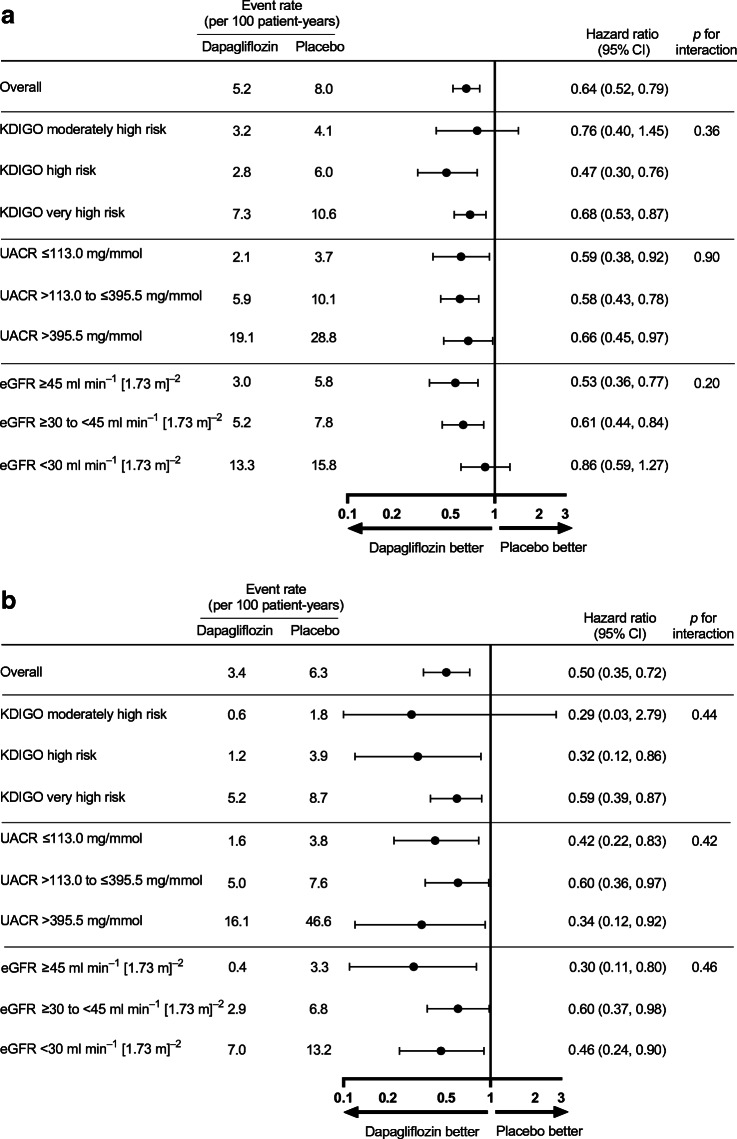
Fig. 2.
Relative effect and absolute risk reduction for dapagliflozin on the primary and secondary outcomes across different subgroups of KDIGO risk categories. The primary composite outcome is a composite of an eGFR decline of ≥50%, ESKD or death from kidney or cardiovascular causes. The kidney composite outcome is a composite of an eGFR decline of ≥50%, ESKD or death from kidney causes
Relative risk reduction by KDIGO risk categories
Compared with placebo, there was no evidence of heterogeneity by KDIGO risk categories when considering relative effects of dapagliflozin on the primary composite endpoint (HR 0.61; 95% CI 0.51, 0.72). The HR with dapagliflozin compared with placebo was 0.65 (95% CI 0.53, 0.80) in patients in the very high KDIGO risk category, 0.44 (95% CI 0.29, 0.67) among patients in the high KDIGO risk category, and 0.71 (95% CI 0.39, 1.30) among patients in the moderately high KDIGO risk category (Fig. 2, p for interaction 0.22). Similarly, there was no evidence of heterogeneity by KDIGO risk categories when considering relative effects of dapagliflozin on secondary endpoints by KDIGO risk categories (Fig. 2). There was no evidence against the proportional hazards assumption.
Absolute risk reduction by KDIGO risk categories
Although there was no evidence of heterogeneity by KDIGO risk categories when considering the absolute effects of dapagliflozin (p for interaction 0.26), the absolute benefits for the primary endpoint were numerically higher in patients with very high KDIGO risk (5.8%; 95% CI 2.9, 8.7) compared with patients with moderately high KDIGO risk (2.2%; 95% CI −1.8, 6.2). Absolute benefits of dapagliflozin on the secondary kidney endpoint, hospitalisation for heart failure or cardiovascular death endpoint and all-cause death were consistent across KDIGO risk categories (all p for interaction >0.14; Fig. 2).
Efficacy in patients with and without type 2 diabetes in various KDIGO risk categories
Analysing patients with and without type 2 diabetes separately, the effect of dapagliflozin compared with placebo on the primary composite endpoint was consistent across subgroups of baseline KDIGO risk categories in patients with and without type 2 diabetes (all p for interaction >0.36; Fig. 3). The effects of dapagliflozin on the three secondary endpoints were also consistent across KDIGO risk categories in patients with and without type 2 diabetes (electronic supplementary material [ESM] Fig. 1).
Fig. 3.
Effects of dapagliflozin on the primary composite outcomes across KDIGO risk categories and subgroups of UACR and eGFR in patients with diabetes (a) and without diabetes (b). The primary composite outcome is a composite of an eGFR decline of ≥50%, ESKD or death from kidney or cardiovascular causes
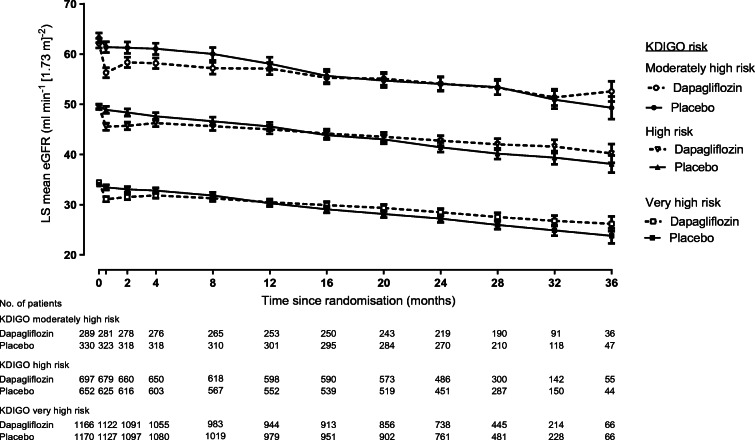
Effects on eGFR slope by KDIGO risk category
The relative effect of dapagliflozin on eGFR slope was consistent across all subgroups of KDIGO risk categories (Fig. 4; ESM Fig. 2). For example, across KDIGO risk categories, initiation of dapagliflozin led to an acute drop in eGFR at week 2 that was consistent in moderately high, high and very high KDIGO risk categories. Placebo-subtracted differences in these groups were −2.7, −2.5 and −2.2 ml min−1 [1.73 m]−2, respectively (p for interaction 0.49). Thereafter, treatment with dapagliflozin compared with placebo led to a reduction in eGFR decline in all KDIGO risk categories with corresponding placebo-subtracted differences in chronic slope of 1.8 ml min−1 [1.73 m]−2 per year (95% CI 1.3, 2.2) in the very high risk category, 2.1 (95% CI 1.6, 2.7) in the high risk category, and 2.1 (95% CI 1.3, 2.9) in the moderately high risk category (p for interaction 0.34; Fig. 4; ESM Fig. 2). The effect of dapagliflozin on total slope was also consistent across KDIGO risk categories (ESM Fig. 2).
Fig. 4.
Effect of dapagliflozin on eGFR slope across KDIGO risk categories. LS, least squares. Data reported with 95% CI
Primary endpoint and secondary endpoints by baseline UACR and eGFR
Baseline characteristics for each baseline subgroup of UACR and eGFR are presented in ESM Table 1. The event rate for the primary endpoint was higher in patients with a lower baseline eGFR or higher UACR. For example, in patients randomised to placebo with an eGFR <30 ml min−1 [1.73 m]−2, the event rate per 100 patient-years for the primary endpoint was 14.9 (95% CI 12.1, 18.4) compared with 5.1 (95% CI 4.2, 6.2) in patients with an eGFR ≥45 ml min−1 [1.73 m]−2 (ESM Fig. 3).
Dapagliflozin consistently reduced the relative risks for the primary and all secondary endpoints across subgroups of UACR and eGFR (all p for interaction >0.10). Although the relative effects on the primary and kidney-specific secondary endpoint were consistent across baseline UACR subgroups, the absolute benefit on the primary and kidney-specific secondary endpoints was greater in subgroups with higher levels of albuminuria. The absolute effects of dapagliflozin on the primary composite and secondary endpoints were consistent across subgroups of eGFR (all p for interaction >0.36, ESM Fig. 3).
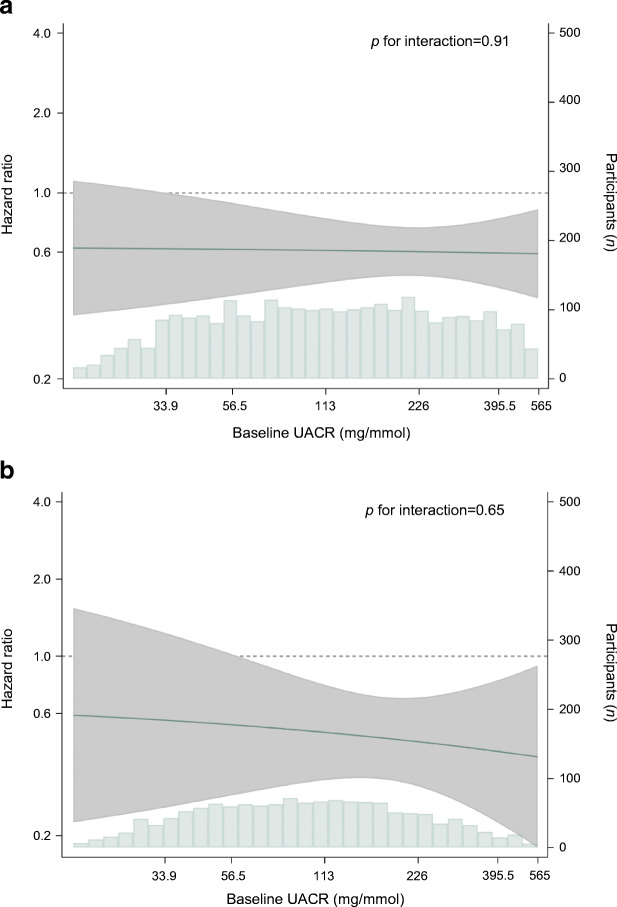
When we analysed UACR as a continuous measure in patients with and without type 2 diabetes separately, we observed the benefit of dapagliflozin on the primary composite endpoint across a range of UACR levels (Fig. 5; p value heterogeneity 0.91 and 0.65, respectively).
Fig. 5.
Effect of dapagliflozin on the primary composite outcome across baseline UACR levels in patients with diabetes (a) and without diabetes (b). The solid line indicates the HR for the primary outcome across baseline UACR, on the left y-axis plotted on a natural log scale; the shaded area indicates the 95% CI. The histogram shows the distribution of UACR at baseline, by number of participants on the right y-axis
There were 454 patients with an eGFR ≥60 ml min−1 [1.73 m]−2, of whom 33 experienced a primary composite endpoint. A total of 445 patients had UACR ≤33.9 mg/mmol (≤300 mg/g), of whom 18 experienced a primary composite endpoint. Although the number of patients and events in the groups with eGFR ≥60 ml min−1 [1.73 m]−2 or UACR ≤33.9 mg/mmol (≤300 mg/g) was low, there was no indication that the efficacy of dapagliflozin differed in these subgroups compared with the overall population (p for interaction >0.38; ESM Fig. 4).
Safety outcomes
The incidence of discontinuation due to adverse events and serious adverse events was similar in patients treated with dapagliflozin and placebo, and did not vary across subgroups of UACR, eGFR and KDIGO risk categories (all p for interaction >0.20, Table 2).
Table 2.
Safety and adverse events of special interest by baseline KDIGO risk categories and subgroups of UACR and eGFR
| n/N | OR (95% CI) | p for interaction | ||
|---|---|---|---|---|
| Dapagliflozin | Placebo | |||
| Discontinuation due to adverse event | ||||
| Overall | 118/2149 | 123/2149 | 0.97 (0.74, 1.26) | |
| KDIGO risk category | ||||
| Moderately high risk | 8/330 | 12/289 | 0.56 (0.22, 1.38) | 0.41 |
| High risk | 31/651 | 32/696 | 1.03 (0.62, 1.71) | |
| Very high risk | 79/1168 | 79/1164 | 1.03 (0.74, 1.42) | |
| UACR subgroup | ||||
| UACR ≤113.0 | 55/1102 | 50/1119 | 1.12 (0.76, 1.66) | 0.48 |
| UACR >113.0 to ≤395.5 | 47/881 | 54/882 | 0.87 (0.58, 1.30) | |
| UACR >395.5 | 16/166 | 19/148 | 0.71 (0.35, 1.46) | |
| eGFR subgroup | ||||
| eGFR ≥45 | 30/879 | 42/901 | 0.73 (0.45, 1.19) | 0.20 |
| eGFR ≥30 to <45 | 60/977 | 45/917 | 1.26 (0.84, 1.87) | |
| eGFR <30 | 28/293 | 36/331 | 0.84 (0.50, 1.43) | |
| Any serious adverse event | ||||
| Overall | 633/2149 | 729/2149 | 0.81 (0.72, 0.93) | |
| KDIGO risk category | ||||
| Moderately high risk | 89/330 | 106/289 | 0.64 (0.45, 0.90) | 0.26 |
| High risk | 176/651 | 205/696 | 0.89 (0.70, 1.12) | |
| Very high risk | 368/1168 | 418/1164 | 0.83 (0.70, 0.98) | |
| UACR subgroup | ||||
| UACR ≤113.0 | 284/1102 | 344/1119 | 0.78 (0.65, 0.95) | 0.79 |
| UACR >113.0 to ≤395.5 | 279/881 | 313/882 | 0.85 (0.69, 1.03) | |
| UACR >395.5 | 70/166 | 72/148 | 0.77 (0.49, 1.22) | |
| eGFR subgroup | ||||
| eGFR ≥45 | 237/879 | 289/901 | 0.78 (0.63, 0.96) | 0.54 |
| eGFR ≥30 to <45 | 295/977 | 302/917 | 0.88 (0.72, 1.07) | |
| eGFR <30 | 101/293 | 138/331 | 0.72 (0.52, 1.00) | |
Data are based on the safety population of 4298
Cut-off values for UACR are mg/mmol (in mg/g: ≤1000 mg/g, >1000 to ≤3500 mg/g, >3500 mg/g); cut-off values for eGFR are ml min−1 [1.73 m]−2
Discussion
The benefits of dapagliflozin on kidney and cardiovascular endpoints in patients with CKD are present across all assessed KDIGO risk categories, as defined by UACR and/or eGFR, without evidence of heterogeneity. The absolute benefits of dapagliflozin were consistent across KDIGO risk categories, but markedly increased among patients with higher levels of UACR. These findings are evident among participants with and without type 2 diabetes. Together, these findings support the initiation of dapagliflozin treatment in a wide group of patients with CKD irrespective of baseline KDIGO risk or presence of diabetes.
The DAPA-CKD trial was preceded by a cardiovascular endpoint trial, Dapagliflozin Effect on Cardiovascular Events –Thrombolysis in Myocardial Infarction 58 (DECLARE-TIMI 58), which randomised 17,160 patients with type 2 diabetes at high cardiovascular risk and early-stage CKD. In this trial, dapagliflozin significantly reduced the risk of the co-primary endpoint of heart failure hospitalisation or cardiovascular death and the secondary kidney endpoint [10]. Post hoc analyses from DECLARE-TIMI 58 demonstrated that patients with lower eGFR and higher albuminuria experienced a higher rate of progressive kidney disease, but the benefits of dapagliflozin in reducing the risk of kidney and heart failure outcomes were evident irrespective of baseline UACR and eGFR [11–13]. In the current study, we extend these observations from DECLARE-TIMI 58, and show that the risk of kidney failure and cardiovascular outcomes continues to increase in patients with albuminuria levels well above 300 mg/g and in patients without type 2 diabetes. Taken together, the data from the DECLARE-TIMI 58 and DAPA-CKD trials provide compelling evidence to initiate treatment with SGLT2 inhibitors to prevent kidney failure, heart failure hospitalisations or cardiovascular death in patients with type 2 diabetes regardless of kidney function or albuminuria status.
Other outcome trials comparing SGLT2 inhibitors to placebo also reported no effect modification by baseline KDIGO risk classification on kidney and cardiovascular benefits of SGLT2 inhibitors. These trials, Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME), Canagliflozin Cardiovascular Assessment Study and CANVAS-Renal (CANVAS Program) and Evaluation of Ertugliflozin Efficacy and Safety Cardiovascular Outcomes Trial (VERTIS CV), enrolled patients with type 2 diabetes who were at high risk for cardiovascular disease, most of whom had normal, or near normal, kidney function [14–16]. In line with our results, these trials demonstrated that the relative effects of SGLT2 inhibitors were consistent regardless of KDIGO risk category [17–19]. In conjunction with the results from the current study, these data indicate that the benefit of SGLT2 inhibitors is not affected by kidney disease severity.
The DAPA-CKD trial enrolled patients with CKD with and without type 2 diabetes [4]. Previous studies reported that dapagliflozin consistently reduced the risk of kidney and cardiovascular endpoints in patients with and without type 2 diabetes irrespective of the underlying cause of kidney disease [6]. In the current study, we demonstrated that, in patients without type 2 diabetes, the effect of dapagliflozin on kidney and cardiovascular outcomes is consistent across KDIGO risk categories and the spectrum of UACR and eGFR values included. Specifically, the consistent effects of dapagliflozin across the spectrum of baseline UACR values indicate that, even in patients without diabetes and microalbuminuria (UACR 3.4–33.9 mg/mmol [30–300 mg/g]), dapagliflozin slows progressive kidney function decline. These data thus further support the use of dapagliflozin in a broad range of patients with and without type 2 diabetes to prevent clinically important outcomes.
We also analysed the effect of dapagliflozin on eGFR trajectories according to KDIGO CKD risk categories. By definition, patients with a very high risk score had the lowest eGFR values at baseline. During placebo treatment, eGFR decline during the trial was less pronounced in the highest risk category (−3.5 ml min−1 [1.73 m]−2 per year) compared with the high risk patients (−4.0 ml min−1 [1.73 m]−2 per year) or moderately high risk patients (−4.6 ml min−1 [1.73 m]−2 per year). However, the benefit of dapagliflozin in slowing the progression of eGFR decline was similar across KDIGO risk categories. Consistent with the mechanism of action and prior clinical trials, dapagliflozin reduced eGFR during the first 2 weeks of treatment in all KDIGO risk categories [20]. During chronic treatment, dapagliflozin stabilised the mean eGFR decline in each KDIGO risk category.
More than 300 participants in the DAPA-CKD trial had a UACR above 395.5 mg/mmol (3500 mg/g) at baseline. This subgroup represents highly vulnerable patients in whom blood pressure and HbA1c was significantly higher, while their eGFR was markedly lower than those with less severe albuminuria. The prognosis of these participants was generally poor. Specifically, the event rates for the kidney-specific endpoints and heart failure hospitalisation or cardiovascular death endpoint were approximately ten- and threefold higher, respectively, compared with patients with UACR below 113.0 mg/mmol (1000 mg/g). These data are consistent with the well-known association between UACR and kidney outcomes [8, 21–24]. Similar results were also observed in the CREDENCE trial, with substantially increased rates of kidney and cardiovascular events among patients with type 2 diabetes and CKD and a UACR above 339.0 mg/mmol (3000 mg/g) [25]. Despite the advanced stage of kidney disease and vulnerable population included in the DAPA-CKD trial, adverse and serious adverse event rates were similar with dapagliflozin compared with placebo across all categories of baseline UACR. These data provide reassurance that dapagliflozin treatment may be safely initiated in high-risk patients with severely increased albuminuria.
The results of this study should be interpreted in the context of its limitations. First, the trial was discontinued prematurely at the recommendation of the independent data monitoring committee due to clear efficacy on the primary outcome and survival [4]. This led to a shorter follow-up time and lower number of events than originally planned, limiting the statistical power in certain subgroups, such as patients with albuminuria <33.9 mg/mmol (<300 mg/g) or eGFR > 60 ml min−1 [1.73 m]−2. However, the consistent benefit for kidney and cardiovascular outcome observed with dapagliflozin in previous cardiovascular outcome trials and in the DAPA-CKD trial suggest that benefits will accrue during prolonged treatment as would occur in clinical practice. The subgroup of patients without diabetes enrolled in the DAPA-CKD trial had CKD with micro- or macroalbuminuria. Whether dapagliflozin reduces the risk of kidney and cardiovascular endpoints in people without diabetes and without albuminuria requires further study. The Study of Heart and Kidney Protection with Empagliflozin (EMPA-KIDNEY) trial is assessing the efficacy of empagliflozin in CKD patients with and without diabetes, and permits inclusion of patients with any level of UACR with an eGFR between 20–45 ml min−1 [1.73 m]−2 [26].
In conclusion, these findings demonstrate that dapagliflozin reduces the relative risk of kidney and cardiovascular outcomes to a similar extent across subgroups of KDIGO risk categories. These results were consistent in patients with and without type 2 diabetes. Together, these findings support the initiation of dapagliflozin treatment across a wide range of patients with CKD, with and without diabetes, who are at high risk of progressive kidney and cardiovascular disease.
Supplementary information
(PDF 945 kb)
Acknowledgements
The authors thank all investigators, trial teams and patients for their participation in the trial. The authors would also like to acknowledge Marco Favretto and Nicola Truss, inScience Communications, London, UK, for assistance in preparation of figures and editing the manuscript. This support was funded by AstraZeneca.
Authors’ relationships and activities
SWW, PV and NJ have no disclosures. DZIC has received consulting fees or speaking honoraria, or both, from Bristol Myers Squibb, Novo Nordisk, Mitsubishi Tanabe, MAZE, Janssen, Bayer, Boehringer Ingelheim/Eli Lilly, AstraZeneca, Merck & Co., Prometic and Sanofi, and has received operating funds from Janssen, Boehringer Ingelheim/Eli Lilly, Sanofi, AstraZeneca, Novo Nordisk and Merck & Co. GMC has received fees from AstraZeneca for the DAPA-CKD trial steering committee, research grants from NIDDK and Amgen; he is on the board of directors for Satellite Healthcare, has received fees for advisory boards for Baxter, Cricket, DiaMedica and Reata, holds stock options for Ardelyx, CloudCath, Durect, DxNow and Outset, has received fees from Akebia, Sanifit and Vertex for trial steering committees, and has received fees for data and safety monitoring board service from Angion, Bayer and ReCor. AML and BVS are employees and stockholders of AstraZeneca. JFEM reports receipt of speaker honoraria from AstraZeneca, Boehringer Ingelheim, Bayer, Fresenius, Medice, Novo Nordisk, Relypsa and Roche, research support from the European Union, the Canadian Institutes Health Research, Boehringer Ingelheim, Celgene, Idorsia, Novo Nordisk, Roche and Sandoz, and consultation fees from AstraZeneca, Bayer, Celgene, Novo Nordisk and Vifor Pharma. OM has received grants and personal fees from AstraZeneca, Bristol Myers Squibb and Novo Nordisk, and personal fees from Eli Lilly, Sanofi, Merck Sharp & Dohme, Boehringer Ingelheim, Johnson & Johnson and Novartis. JJVM reports payments to his employer, Glasgow University, for his work on clinical trials, consulting and other activities from Alnylam, Amgen, AstraZeneca, Bayer, BMS, Cardurion, Cytokinetics, GSK, Novartis, Pfizer and Theracos and personal lecture fees from the Corpus, Abbott, Hickma, Sun Pharmaceuticals and Medsca. PR has received honoraria to Steno Diabetes Center Copenhagen for steering group membership and/or lectures and advice from AstraZeneca, Novo Nordisk, Bayer and Eli Lilly, for advisory board participation from Sanofi Aventis and Boehringer Ingelheim, and for steering group participation from Gilead. RC-R has received honoraria from AstraZeneca, GlaxoSmithKline, Medtronic and Boehringer Ingelheim, has lectured for Amgen, Janssen and Boehringer Ingelheim, and has received research support from GlaxoSmithKline, Novo Nordisk and AstraZeneca. RDT received funding from AstraZeneca for participating in the steering committee for the DAPA-CKD trial. He has received fees for consultancy from Boehringer Ingelheim, Reata Pharma and Chinook Pharma. He has received honoraria for lectures from Medscape and Medical Education Resources. He has participated in data and safety monitoring or advisory boards for Bayer, Viofor, Akebia and Otsuka. DCW provides ongoing consultancy services to AstraZeneca and has received honoraria and/or consultancy fees from Amgen, Astellas, AstraZeneca, Boehringer Ingelheim, Bayer, GlaxoSmithKline, Janssen, Napp, Mundipharma, Merck Sharp and Dohme, Reata, Tricida and Vifor Fresenius. HJLH is a consultant for AstraZeneca, Bayer, Boehringer Ingelheim, Chinook, CSL Pharma, Gilead, Janssen, Merck, Mundipharma, Mitsubishi Tanabe, Novo Nordisk and Retrophin. He received research support from Abbvie, AstraZeneca, Boehringer Ingelheim and Janssen.
Abbreviations
- CKD
Chronic kidney disease
- CREDENCE
Canagliflozin and Renal Events in Diabetes With Established Nephropathy Clinical Evaluation
- DAPA-CKD
Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease
- DECLARE-TIMI 58
Dapagliflozin Effect on Cardiovascular Events –Thrombolysis in Myocardial Infarction 58
- ESKD
End-stage kidney disease
- KDIGO
Kidney Disease Improving Global Outcomes
- SGLT2
Sodium–glucose cotransporter 2
- UACR
Urinary albumin/creatinine ratio
Contribution statement
SW, PV and HJLH analysed and interpreted the data. SW and HJLH wrote the first draft of the manuscript. All other authors were involved in data interpretation and contributed to revisions for important intellectual content. All authors read and approved the manuscript. HJLH is responsible for the integrity of the work as a whole.
Funding
The DAPA-CKD trial was funded by AstraZeneca. The sponsor of the study was involved in the study design, analysis, interpretation of data, writing of the report and the decision to submit the paper for publication.
Data availability
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at: https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yamout H, Perkovic V, Davies M, et al. Efficacy and safety of canagliflozin in patients with type 2 diabetes and stage 3 nephropathy. Am J Nephrol. 2014;40(1):64–74. doi: 10.1159/000364909. [DOI] [PubMed] [Google Scholar]
- 2.Kohan DE, Fioretto P, Tang W, List JF. Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int. 2014;85(4):962–971. doi: 10.1038/ki.2013.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 4.Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–1446. doi: 10.1056/NEJMoa2024816. [DOI] [PubMed] [Google Scholar]
- 5.Bhatt DL, Szarek M, Pitt B, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med. 2021;384(2):129–139. doi: 10.1056/NEJMoa2030186. [DOI] [PubMed] [Google Scholar]
- 6.Wheeler DC, Stefánsson BV, Jongs N, et al. Effects of dapagliflozin on major adverse kidney and cardiovascular events in patients with diabetic and non-diabetic chronic kidney disease: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9(1):22–31. doi: 10.1016/S2213-8587(20)30369-7. [DOI] [PubMed] [Google Scholar]
- 7.Persson F, Rossing P, Vart P, et al. Efficacy and safety of Dapagliflozin by baseline glycemic status: a Prespecified analysis from the DAPA-CKD trial. Diabetes Care. 2021;44(8):1894–1897. doi: 10.2337/dc21-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group KDIGO 2012 clinical practice guideline for the evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2013;3(1):1–150. doi: 10.1038/kisup.2012.73. [DOI] [Google Scholar]
- 9.Heerspink HJL, Stefansson BV, Chertow GM, et al. Rationale and protocol of the Dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) randomized controlled trial. Nephrol Dial Transplant. 2020;35(2):274–282. doi: 10.1093/ndt/gfz290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–357. doi: 10.1056/NEJMoa1812389. [DOI] [PubMed] [Google Scholar]
- 11.Mosenzon O, Wiviott SD, Cahn A, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE–TIMI 58 randomised trial. Lancet Diabetes Endocrinol. 2019;7(8):606–617. doi: 10.1016/S2213-8587(19)30180-9. [DOI] [PubMed] [Google Scholar]
- 12.Zelniker TA, Raz I, Mosenzon O et al (2021) Effect of dapagliflozin on cardiovascular outcomes according to baseline kidney function and albuminuria status in patients with type 2 diabetes: a prespecified secondary analysis of a randomized clinical trial. JAMA Cardiol 6(7):801–810 [DOI] [PMC free article] [PubMed]
- 13.Mosenzon O, Wiviott SD, Heerspink HJL, et al. The effect of Dapagliflozin on albuminuria in DECLARE-TIMI 58. Diabetes Care. 2021;44(8):1805–1815. doi: 10.2337/dc21-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–657. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
- 15.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 16.Cannon CP, Pratley R, Dagogo-Jack S, et al. Cardiovascular outcomes with Ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383(15):1425–1435. doi: 10.1056/NEJMoa2004967. [DOI] [PubMed] [Google Scholar]
- 17.Levin A, Perkovic V, Wheeler DC, et al. Empagliflozin and cardiovascular and kidney outcomes across KDIGO risk categories: post hoc analysis of a randomized, double-blind, placebo-controlled, multinational trial. Clin J Am Soc Nephrol. 2020;15(10):1433–1444. doi: 10.2215/CJN.14901219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neuen BL, Ohkuma T, Neal B, et al. Relative and absolute risk reductions in cardiovascular and kidney outcomes with Canagliflozin across KDIGO risk categories: findings from the CANVAS program. Am J Kidney Dis. 2021;77(1):23–34. doi: 10.1053/j.ajkd.2020.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Cherney DZI, McGuire DK, Charbonnel B, et al. Gradient of risk and associations with cardiovascular efficacy of Ertugliflozin by measures of kidney function. Circulation. 2021;143(6):602–605. doi: 10.1161/CIRCULATIONAHA.120.051901. [DOI] [PubMed] [Google Scholar]
- 20.Heerspink HJL, Cherney DZI. Clinical implications of an acute dip in eGFR after SGLT2 inhibitor initiation. Clin J Am Soc Nephrol. 2021;16(8):1278–1280. doi: 10.2215/CJN.02480221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halbesma N, Kuiken DS, Brantsma AH, et al. Macroalbuminuria is a better risk marker than low estimated GFR to identify individuals at risk for accelerated GFR loss in population screening. J Am Soc Nephrol. 2006;17(9):2582–2590. doi: 10.1681/ASN.2005121352. [DOI] [PubMed] [Google Scholar]
- 22.Gansevoort RT, Matsushita K, van der Velde M, et al. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int. 2011;80(1):93–104. doi: 10.1038/ki.2010.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoefield RA, Kalra PA, Baker PG, et al. The use of eGFR and ACR to predict decline in renal function in people with diabetes. Nephrol Dial Transplant. 2011;26(3):887–892. doi: 10.1093/ndt/gfq526. [DOI] [PubMed] [Google Scholar]
- 24.Modification of Diet in Renal Disease Study Group. Hunsicker LG, Adler S, et al. Predictors of the progression of renal disease in the modification of diet in renal disease study. Kidney Int. 1997;51(6):1908–1919. doi: 10.1038/ki.1997.260. [DOI] [PubMed] [Google Scholar]
- 25.Jardine M, Zhou Z, Lambers Heerspink HJ, et al. Kidney, cardiovascular, and safety outcomes of Canagliflozin according to baseline albuminuria: a CREDENCE secondary analysis. Clin J Am Soc Nephrol. 2021;2:1–12. doi: 10.2215/CJN.15260920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herrington WG, Preiss D, Haynes R, et al. The potential for improving cardio-renal outcomes by sodium-glucose co-transporter-2 inhibition in people with chronic kidney disease: a rationale for the EMPA-KIDNEY study. Clin Kidney J. 2018;11(6):749–761. doi: 10.1093/ckj/sfy090. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 945 kb)
Data Availability Statement
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at: https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure