To the Editor:
The vaccine mRNA is sensed by multiple pattern recognition receptors of dendritic cells, leading to type I interferon secretion. This interferon response promotes the adaptive immune reaction to provoke antiviral response and probably interferonopathy including type 1 diabetes mellitus (T1DM), lupus, and thyroiditis.1 Indeed, not merely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection but also vaccination induces disease flare-up in patients with rheumatoid arthritis (RA).2, 3, 4 We here report an elderly woman with autoimmune background who received the Pfizer BioNTech vaccine BNT162b2, resulting in new-onset autoimmune polyarthritis-like RA.
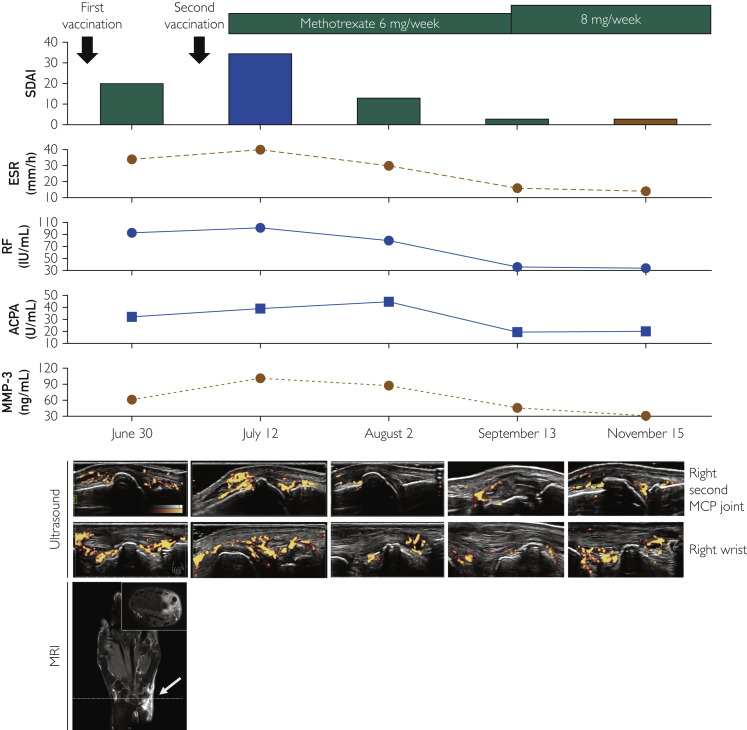
A 77-year-old nonsmoking woman manifested bilateral arthritis of wrists, fingers, and toes in late June 2021. She was diagnosed with slowly progressive insulin-dependent diabetes mellitus and Hashimoto thyroiditis in 2015. In May 2021, she developed fatigue, and the SARS-CoV-2 polymerase chain reaction test using a nasopharyngeal specimen was positive. Fortunately, her SARS-CoV-2 infection resulted in only fatigue without any febrile and respiratory symptoms. Then, she received the first BNT162b2 vaccination per her wishes in early June; subsequently, she developed peripheral polyarthritis. Laboratory findings showed an elevated level of C-reactive protein (3.2 mg/L, reference: <1.4 mg/L) and matrix metalloprotease-3 (MMP-3), and positivity of rheumatoid factor (RF) and anti-citrullinated protein antibody (ACPA) (22.7 U/mL). Ultrasound and magnetic resonance imaging showed synovitis in the fingers and wrists. We considered the mRNA vaccination-induced transient autoimmune phenomenon and provided supportive care using analgesics. However, she wished to finish the second BNT162b2 vaccination in July, resulting in symptomatic worsening with elevated levels of C-reactive protein (12.8 mg/L), RF, MMP-3, and ACPA titer (39.1 U/mL). We diagnosed the patient with BNT162b2-induced new-onset autoimmune arthritis-like RA and administered methotrexate. A month later, her arthritis was dramatically ameliorated with decreased inflammation. However, the RF and ACPA titers maintained high levels with active synovitis (Figure ).
Figure.
Clinical course of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination-induced autoimmune polyarthritis. Clinical course shown by disease activity of rheumatoid arthritis including Simplified Disease Activity Index (SDAI); laboratory findings including erythrocyte sedimentation rate (ESR), rheumatoid factor (RF), anti-citrullinated protein antibody (ACPA), and matrix metalloprotease-3 (MMP-3); and imaging studies such as joint ultrasound and magnetic resonance imaging (MRI). In ultrasound studies, the right metacarpophalangeal (MCP) joint of forefinger and wrist were focused. The MRI studies revealed synovitis as gadolinium-enhanced high intensity area in the right wrist (arrow). The upper right panel shows coronal slice directed by a broken reference line.
We believe that this patient with autoimmune background newly developed RA-like autoimmune arthritis, which was perhaps mRNA vaccination-induced interferonopathy. Autoimmune diseases including T1DM and RA share several common genetic variants deciding disease risk and autoimmune mechanisms. Similar molecular signatures at the target tissues in T1DM and RA are confluent with type I interferon signaling.5 It is biologically plausible that SARS-CoV-2 mRNA vaccination developed new-onset RA-like arthritis. This case reiterates the importance of interferon signaling for developing autoimmune diseases in predisposed individuals.
Available mRNA vaccines are reported to rarely, but rationally induce autoimmune flare-up.2, 3, 4 The reported percentage of flare-up ranges from 3% to 14%, but this might be overestimated because the definition of flare-up includes fever and musculoskeletal symptoms similar to adverse effects of vaccination, and the flare-up decision depends on patient self-reports.3 However, cases of mRNA vaccination-induced autoimmunity do exist. Nonetheless, there is established treatment for many autoimmune diseases. Therefore, we advocate that vaccination outweighs possible risks for autoimmune developments to end the unjustifiable threat by coronavirus disease 2019.
Acknowledgments
The authors thank Megumi Tachikawa and Shizuko Ishikida for their contribution to the ultrasound studies of the patient. Written consent was obtained from the patient. The Institutional Research Ethics Board does not require board review for a single case report when the patient’s privacy is protected.
References
- 1.Sprent J., King C. COVID-19 vaccine side effects: the positives about feeling bad. Sci Immunol. 2021;6(60) doi: 10.1126/sciimmunol.abj9256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Terracina K.A., Tan F.K. Flare of rheumatoid arthritis after COVID-19 vaccination. Lancet Rheumatol. 2021;3(7):e469–e470. doi: 10.1016/S2665-9913(21)00108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barbhaiya M., Levine J.M., Bykerk V.P., Jannat-Khah D., Mandl L.A. Systemic rheumatic disease flares after SARS-CoV-2 vaccination among rheumatology outpatients in New York City. Ann Rheum Dis. 2021;80(10):1352–1354. doi: 10.1136/annrheumdis-2021-220732. [DOI] [PubMed] [Google Scholar]
- 4.Watad A., De Marco G., Mahajna H., et al. Immune-mediated disease flares or new-onset disease in 27 subjects following mRNA/DNA SARS-CoV-2 vaccination. Vaccines (Basel) 2021;9(5):435. doi: 10.3390/vaccines9050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szymczak F., Colli M.L., Mamula M.J., Evans-Molina C., Eizirik D.L. Gene expression signatures of target tissues in type 1 diabetes, lupus erythematosus, multiple sclerosis, and rheumatoid arthritis. Sci Adv. 2021;7(2) doi: 10.1126/sciadv.abd7600. [DOI] [PMC free article] [PubMed] [Google Scholar]