Abstract
Introduction
Patellar tendinopathy is one of the most common musculoskeletal problems associated with sport. While commonly perceived as a predominantly male problem, recent epidemiological studies revealed that it also affects a large number of sport-active women. The aim of this systematic review was to understand how the available treatments apply to women affected by patellar tendinopathy.
Methods
We analysed the available literature with a systematic review on three databases (PubMed, Cochrane, Web of Science) on February 2021, retrieving a total of 136 studies published from 1983.
Results
The overall scientific field offers an astonishingly low number of data on treatment results referring to only 78 women (2%) in the entire literature. Only 5% of the retrieved articles considered focusing only or mostly on men to be a limitation.
Conclusions
Women represent only a minority of patients studied for this topic. The few documented cases are further fragmented by being related to different treatments, thus basically offering no solid evidence for results and limitations of any therapeutic approach in women. This literature analysis showed a greater gender gap than what is recognized in science and general medicine; it showed a gender blindness in sports medicine when investigating a common problem like patellar tendinopathy.
Keywords: Patellar tendinopathy, Gender bias, Sports medicine, Tendinopathy
Key Points
Patellar tendinopathy is a common pathology with a high prevalence among athletes, for which several conservative therapies have been developed.
Women are at great risk of sustaining tendon and ligament injuries during physical activities due to several factors including hormonal fluctuation.
Analysis of sex-specific data is a simple yet critical step towards gender equality, which is too often omitted despite the many indications provided by different authorities.
There are no data available in the current literature to support the potential and limitations of the available treatments of patellar tendinopathy in women.
Introduction
Awareness of the need for gender equality is growing in every field, including sports medicine. In fact, sex and gender disparity encompasses many aspects of our societies, including science and medical treatments. Regarding sex, current literature refers to the biological and physiological features characterizing male and female individuals, while gender represents socially constructed roles, behaviours and identities of female, male, and gender-diverse people [1, 2]. In this context, gender bias refers to the lack of scientific data concerning half of the human population, due to the fact that for cultural reasons women are often not taken into account [3].
The gender data gap is in this context a consequence of the tendency to consider males (Caucasian males, usually) the norm or the standard and females as deviant [4]. In 1986, the NIH (National Institute of Health) encouraged increased female inclusion in clinical research, calling for justification in cases of exclusion [5, 6]. This resulted in the 1993 Revitalization Act that required female participation in NIH-funded clinical research [7]. In 1997, the FDA (Food and Drug Administration) upheld the analysis of clinical data by sex [8] and in 2001 a report affirming that sex is an important variable that must be considered in all aspects and at all levels of biomedical research was published by the Institute of Medicine [9]. Between 2005 and 2008, the GenderBasic project in Europe supported scientific studies focusing on sex and gender and the importance of distinguishing outcomes by sex [10]. A few years later, the European Association of Science Editors (EASE) established a Gender Policy Committee with the aim to develop a set of guidelines for reporting of Sex and Gender Equity in Research (SAGER) [2]. During the same period, the Canadian Institute of Health mandated a justification for any article if only one sex was considered [11], and in 2014 the NIH started promoting the use of both sexes also for preclinical animal research [12].
Sports medicine research should also identify factors that may affect risk or prognosis, including patient sex. Up to the 1970s, the suitability of sports competition for girls and women was still being questioned in some circles, exemplified by publications titled “Women in Sports: Some Misconceptions” [13] and “Inferiority of Female Athletes: Myth or Reality?” [14]. Some of the myths surrounding female athletic participation have been challenged, and now there are studies that do examine dissimilarities between the sexes focusing on differences in injury risk or prognosis of conditions such as concussions and ACL injuries [15]. The aforementioned gender equity indications have also been proposed with the aim to decrease female underrepresentation and underline the importance of sex-disaggregated data in order to provide women “benefits of care based on good, applicable evidence” [16].
Patellar tendinopathy is a common musculoskeletal problem associated with sport [17–19]. Often referred to as “jumper’s knee”, it results from overuse in activities that require jumping, running, squatting, or rapid changes in direction. This disorder affects athletes in many sports. The prevalence of jumper's knee has been estimated to be up to one-third among elite basketball players and between 40 and 50% among high-level volleyball players [18], and there is a high prevalence among soccer players, sprinters, and jumpers as well [20]. Prominent features include histopathological changes such as disorganization of collagen fibres, an increase in the number of vessels and sensory nerves, an increase in hydrated components of the extracellular matrix and [21], ultimately, apoptotic death of tenocytes leading to an overall breakdown of tissue organization [22]. Characterized by microscopic ruptures with degenerative changes in the patellar tendon, most frequently in its origin on the inferior pole of the patella, this condition results in substantial pain and reduced performance in sports. Most patients report persistent pain and disability, with some experiencing long-term limitations. There is evidence showing that the average duration of pain and reduced function can be nearly 3 years, and that at 15 years follow-up 53% of patients reported having to quit their sports career because of their knee problem [23]. Thus, patellar tendinopathy can severely affect patients even to the point of abandoning their athletic career. Moreover, it is also common as a work-related condition and even in the sedentary population causes pain and dysfunction that impair activities of daily living [24]. While commonly perceived as a predominantly male problem, recent epidemiological studies revealed that it also affects a large number of sport-active women [20, 25–31].
The purpose of this article was to systematically review the literature to determine if the available treatments have been studied considering gender-related differences and thus apply to women affected by patellar tendinopathy.
Methods
Literature Research
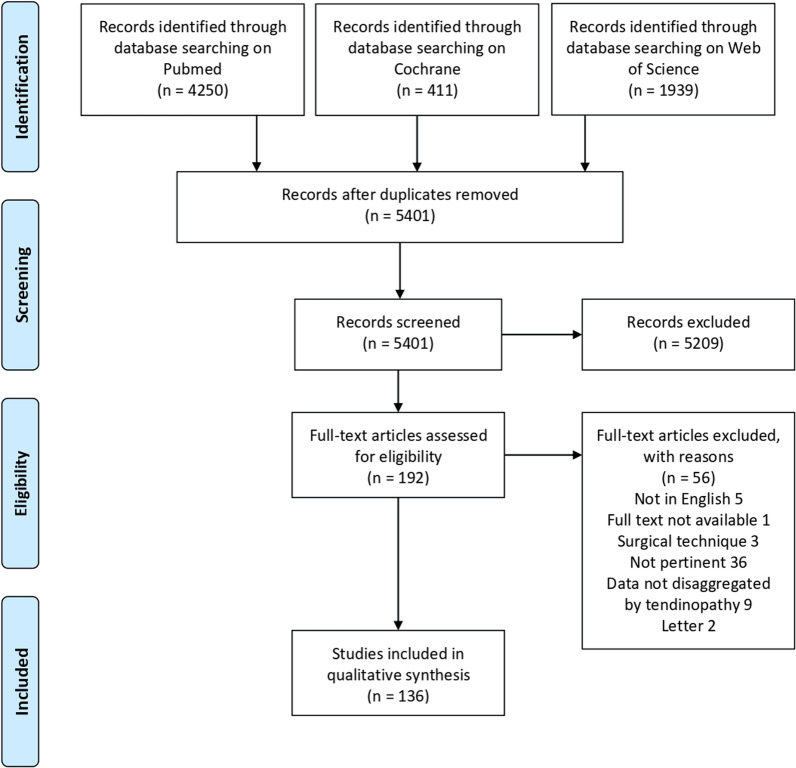
A systematic review of the literature was performed on February 1, 2021, using three bibliographic databases: PubMed, Web of Science, and Wiley Cochrane Library. The following search terms were used for initial screening “((patellar) AND ((tendinopathy) OR (tendinitis) OR (tendon pathology))) AND (treatment))”. No limitations based on the publication time were made. The guidelines for Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) were used. A flow chart of the articles’ selection for the qualitative data synthesis is reported in Fig. 1.
Fig. 1.
PRISMA (Preferred Reporting Item for Systematic Meta-Analyses) flow chart of the article selection process
Articles Selection and Data Extraction
Two authors (CMTDL, EA) performed the article selection independently, and duplicate articles were removed. Articles were included if they met the following criteria: clinical reports of any level of evidence, written in English language, with no time limitation, on therapies used to treat patients affected by patellar tendinopathy. Articles written in other languages, animal studies, and reviews were excluded. After screening titles and abstract, full text for the articles that met inclusion criteria were reviewed. In case of disagreement between the two reviewers, a third author was consulted (MPL).
An electronic table for data extraction was created prior to the article using Excel (Microsoft). The relevant data were then extracted: title, first author, year of publication, journal, type of article, level of evidence, population characteristics, type of treatment, article limitations, outcomes, and outcomes disaggregated by sex.
The included articles were further divided into three different groups based on the treatment: conservative treatment, injectable treatment, and surgical treatment. If an article compared two distinct approaches, they were counted individually.
Statistical Analysis
Absolute numbers and percentages were used to report the number of articles and the sex of patients enrolled.
For each article, sex matching was calculated as the ratio of the two sexes, multiplied by 100, using the lesser number of subjects (male or female) in an individual article as the numerator and the greater number of subjects (male or female) as the denominator. For instance, an article with 50 women and 50 men would result in a 100% sex matching, as 50/50 × 100 = 100% [32].
Institutional Board Review and Funding Source
IRB approval was not required because all data were extracted from previously published studies. No external funding was received for the initiation or completion of this article.
Results
Article Selection
The database search identified 6600 records, of which 1199 were identified as duplicates and removed. Of the remaining 5401 records, 192 full-text articles considered suitable for inclusion were assessed for eligibility. Fifty-six articles did not meet the inclusion criteria and were excluded, leading to a total of 136 studies used for the analysis. The articles were all published between 1983 and 2020 with most of the studies being published in the last two decades (116/136 articles, 85%).
Clinical Articles
Article Characteristics
Of the 136 clinical articles, six (4%) did not specify the sex of the enrolled patients. The remaining 130 articles (96%) stated the sex of the patients, two (1%) of which included only women, 25 (19%) articles included only men and 103 (80%) included both sexes. Of the 103 articles including both sexes, only one separated data by sex [33] and two referred to a general outcome for women, but without specifying their data [34, 35]. Seven other articles did perform sex-specific analysis, but without specifically discussing their data [36–42].
Only six (5%) articles considered enrolling only or mostly men as a limitation [43–48].
Representation of Women
Overall, 4142 patients were studied. Besides the 6% of patients for whom sex was not specified, the remaining 3894 patients were represented by 78% men (3022), while women accounted for 22% (872) of the patients. This percentage did not increase when evaluating only the high-level studies: the 41 randomized controlled trials enrolled a total of 310 women (22%) and 1121 men (78%).
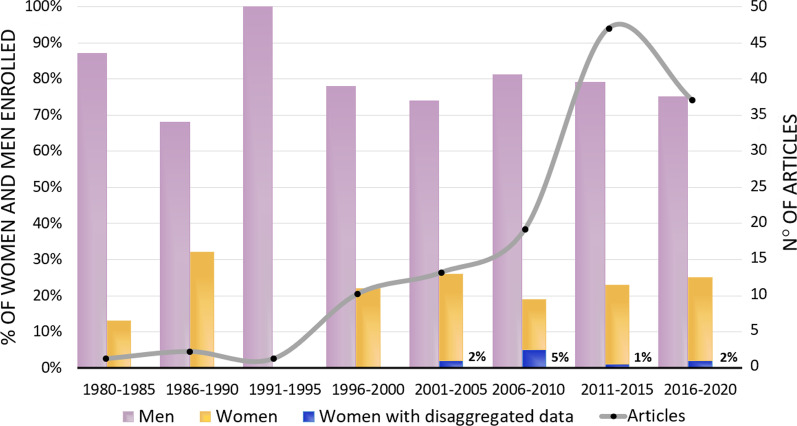
Analysis of the available data on the treatment of patellar tendinopathy was specified for 78 women, which represents 9% of all the enrolled women, and 2% of all patients studied in the literature on this topic. While the number of articles increased over the years, the percentage of female inclusion did not, since the highest value (32%) was reached between 1985 and 1990. In the last five years, between 2016 and 2020, 37 articles on the treatment of patellar tendinopathy were published, including 25% women (Fig. 2).
Fig. 2.
Percentage of women and men enrolled in patellar tendinopathy related research retrieved in this systematic review, and corresponding number of articles published from 1980 to 2020
Women were represented more in conservative treatments (50%), while they were less present in the injectable (28%) and surgical treatments (22%). The results of conservative, injectable, and surgical treatment in women were reported in 50, 7, and 21 cases, respectively.
Sex-matching
Of the 103 studies enrolling both sexes, 11% had less than 10% women, 42% had less than 20% women, 16% had less than 30% women, and 23% had less than 50% women. Only 8 articles (8%) included more than 50% women.
Sex-matched analysis demonstrated that only 17/103 studies (16%) matched the sex of more than 50%, only 6/103 studies (6%) had a sex matching of more than 80%, and only 2/103 studies (1%) had a sex-matching of 100%, enrolling the same number of women and men.
Discussion
The main finding of this systematic review is that there is a large gender gap in articles focused on the treatment and outcome of patellar tendinopathy in women.
A plethora of therapeutic strategies have been developed to address patellar tendinopathy, including physical therapy, and other conservative approaches independently or concurrently applied to favour healing of this challenging pathological condition, such as electrotherapy, massage, taping, anti-inflammatory medication, extra-corporeal shock-wave therapy, and different types of injections (platelet-rich plasma, autologous plasma, cells derived from dermal fibroblasts, bone marrow-derived stem cells). In cases where conservative treatment fails, surgery may be considered [49].
To understand how these treatments apply to women affected by patellar tendinopathy, we analysed the available literature, looking at female representation and if data disaggregation allows for a proper understanding of indications and results of these treatments in women. This systematic review of the literature was performed to retrieve data related to women by including all studies focusing only on women and those separating data by sex: only 78 women (from 10 studies) in the entire literature. This represents less than 2% of all patients studied for this topic. These cases are further fragmented by being related to different treatments, thus basically offering no solid evidence for results and limitations of any therapeutic approach in women. Even though evaluating the treatment of patellar tendinopathy has increased over the past several years, the attention towards proper gender representation has not (Fig. 2). Even worse, this has not even been perceived as an issue, as only 5% of the retrieved articles considered focusing only or mostly on men to be a limitation. Sport participation of women has increased substantially in the last few decades and therefore the number of women affected by patellar tendinopathy has also increased [50]. Women are at greater risk of sustaining tendon and ligament injuries during physical activities [17, 51–54], which has been partially explained by the potential effect of hormones, since it has been demonstrated that both ligaments [55] and tendons contain oestrogen receptors [56]. Increased concentration of oestrogen can lead to the inhibition of collagen synthesis in women [57, 58], as confirmed by the lower patellar tendon collagen synthesis rate compared to men, both at rest and after exercise [59]. In the patellar tendon of women, a higher mRNA expression of collagen type III was found. This is considered a marker of injured tissue implying smaller and less organized fibrils which could easily lead to damage and rupture [60]. In addition, lower tendon stiffness has been reported in women [61], leading to a worse adaptation to mechanical loading and a reduced tendon hypertrophy response after habitual training [62, 63]. The concept that sex hormones have a role in relation to injury is further supported by research showing a lower tendon collagen synthesis in patients taking oral contraceptives [64], while in post-menopausal women tendon stiffness matches that of men [65]. These sex-related differences can affect the likelihood of developing a tendon injury, as well as the response to available treatments, in terms of success rates and adverse effects. Additionally, hormones can affect pain perception, which further complicates the assessment of tendinopathy and treatment results, and further research is necessary to better understand the impact of patient sex on tendon, treatment options, and outcomes [66–69].
Differences in pharmacokinetics between men and women can make women more prone to experience adverse drug reactions, as evidenced and exemplified by the Zolpidem case [70]. This drug was approved and commercialized with the same dosage for both sexes. Ten years later, researchers pointed out that levels in women were high enough to cause next-morning impairment lowering their performance in tasks that require alertness, including driving, and therefore the FDA started recommending women take half the dose [71, 72]. Besides the side effects, male overrepresentation can lead to the production of drugs with less or no effect at all in women [73]. Women and men can differ in terms of outcomes, re-admission rates, and post-operative complications [74, 75]. In this light, reporting data stratified by sex is necessary to understand the risks of the different treatment options. However, it is not enough to enroll women within clinical studies to overcome the risk of gender inequality. For example, in the orthopaedic field Kalliainen et al. analysed hand surgery research: 47% of the enrolled patients were women but still, only 23% of the studies calculated statistics by sex [76]. Even though a 19% to 30% increase in sex-specific analyses has been reported between 2000 and 2010 in five high-impact orthopaedic journals [8], another analysis of the surgical literature found that only 38% reported data by sex, 33% analysed data by sex, and 23% included a discussion of sex-based results [32]. Moreover, only 2% of these articles matched the sex of included subjects by 100%, having the same number of enrolled men and women, and only 18% of the studies were able to reach an 80% match between male and female patients.
There are limitations to this review. First, this analysis is focused only on one pathology in the orthopaedic field, and thus it cannot be assumed that these findings are consistent for all orthopaedic research. Second, the data we extracted are limited to the phenotypic concept of sex with no regard to the gender issue, since no mention of it can be found in the articles analysed. Also, it should not be forgotten that a binary representation of sex/gender can lead to the exclusion of transgender, gender-fluid, and intersex individuals and that a simple disaggregation by sex could mask other subtleties, such as socioeconomic status, ability, and ethnic background, thus not adequately addressing the needs of different groups of people.
From 1983 to the present day, the number of women enrolled in studies on patellar tendinopathy has not increased, and even though most studies included both sexes, there is a persisting lack of awareness of the importance of disaggregating data by sex. This is not to say that an equal number of men and women must be enrolled in every study. It might not always be feasible, but it is important to provide sufficient data granularity recording the sex-specific outcomes to allow the data to be abstracted for use in a subsequent meta-analysis. In this way, it will be possible to understand if different treatments need to be considered for women and men. Disaggregating data is a simple yet critical step towards gender equality, which is too often omitted despite the many indications provided by different authorities. Research progresses, but gender bias persists, and we keep addressing only half the population. Gender bias persists in orthopaedics and sports medicine and can no longer be ignored. More women should be enrolled in scientific studies and sex-based analysis should be implemented systematically to guarantee women a high level of care and better outcomes in the management of patellar tendinopathy. We have the duty to offer women appropriate treatments that are no longer based on male data.
Conclusions
Women represent only a minority of patients studied for patellar tendinopathy. The few documented cases are further fragmented by being related to different treatments, thus basically offering no solid evidence for results and limitations of any therapeutic approach in women. This literature analysis showed a greater gender gap than what is recognized in science and general medicine; it showed a gender blindness in sports medicine when investigating a common problem like patellar tendinopathy.
Acknowledgements
Not applicable.
Author Contributions
The idea for the systematic review and meta-analysis was developed by GF. The article selection was independently performed by CMTDL and EA with disagreement solved by consensus or by the intervention of MPL. The statistical analysis and data interpretation were performed by CMTDL and supervised by GF. CMTDL drafted the Introduction, Materials and Methods, Results and Discussion section of the initial manuscript, which was reviewed by GF and agreed upon by all authors. MPL and GF reviewed the final version of the manuscript. All authors read and approved the final manuscript.
Funding
No sources of funding were used to assist in the preparation of this article.
Availability of Data and Materials
The datasets used and/or analysed during the current systematic review are available from the corresponding author on reasonable request.
Declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing interests
Camilla Mondini Trissino da Lodi, Maria Paola Landini, Emanuela Asunis and Giuseppe Filardo declare that they have no competing interests relevant to the content of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Maria Paola Landini, Email: mariapaola.landini@ior.it, Email: dirscien@ior.it.
Emanuela Asunis, Email: asunis.emanuela@gmail.com.
References
- 1.Gender, Equity and Human Rights. Available from: https://www.euro.who.int/en/health-topics/health-determinants/gender/gender-definitions
- 2.Heidari S, Babor TF, De Castro P, Tort S, Curno M. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2016;1:2. doi: 10.1186/s41073-016-0007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Criado Perez Caroline. Invisible Women: Exposing Data Bias in a World Designed for Men. 2019.
- 4.Nicolette J. Searching for Women’s Health: a resident’s perspective. Journal of Women’s Health & Gender-Based Medicine. Mary Ann Liebert, Inc., publishers; 2000;9:697–701. [DOI] [PubMed]
- 5.1986_10_24_Vol_15_No_22.pdf [Internet]. [cited 2021 Dec 3]. Available from: https://grants.nih.gov/grants/guide/historical/1986_10_24_Vol_15_No_22.pdf
- 6.Timeline [Internet]. SWHR. [cited 2021 Dec 3]. Available from: http://swhr.org/about/history/timeline/
- 7.Studies I of M (US) C on E and LIR to the I of W in C, Mastroianni AC, Faden R, Federman D. NIH Revitalization Act of 1993 Public Law 103–43 [Internet]. Women and Health Research: Ethical and Legal Issues of Including Women in Clinical Studies: Volume I. National Academies Press (US); 1994. Available from: https://www.ncbi.nlm.nih.gov/books/NBK236531/ [PubMed]
- 8.Hettrich CM, Hammoud S, LaMont LE, Arendt EA, Hannafin JA. Sex-specific analysis of data in high-impact orthopaedic journals: how are we doing? Clin Orthop Relat Res. 2015;473:3700–3704. doi: 10.1007/s11999-015-4457-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine (US) Committee on Understanding the Biology of Sex and Gender Differences. Exploring the Biological Contributions to Human Health: Does Sex Matter? [Internet]. Wizemann TM, Pardue M-L, editors. Washington (DC): National Academies Press (US); 2001. Available from: http://www.ncbi.nlm.nih.gov/books/NBK222288/ [PubMed]
- 10.Klinge I. Gender perspectives in European research. Pharmacol Res. 2008;58:183–189. doi: 10.1016/j.phrs.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 11.Canada H. Health Portfolio Sex and Gender-Based Analysis Policy [Internet]. aem. 2017. Available from: https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/heath-portfolio-sex-gender-based-analysis-policy.html
- 12.Clayton JA, Collins FS. Policy: NIH to balance sex in cell and animal studies. Nature. 2014;509:282–283. doi: 10.1038/509282a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris DV. Women in sports: some misconceptions. J Sports Med. 1973;1:15–17. doi: 10.1177/036354657300100303. [DOI] [PubMed] [Google Scholar]
- 14.Wilmore JH. Inferiority of female athletes: myth or reality. J Sports Med. 1975;3:1–6. doi: 10.1177/036354657500300101. [DOI] [PubMed] [Google Scholar]
- 15.Reider B. Sex in sports medicine. Am J Sports Med. 2012;40:1231–1233. doi: 10.1177/0363546512449812. [DOI] [PubMed] [Google Scholar]
- 16.Leopold SS, Beadling L, Dobbs MB, Gebhardt MC, Lotke PA, Manner PA, et al. Editorial: Fairness to all: Gender and sex in scientific reporting. Clin Orthop Relat Res. 2014;472:391–392. doi: 10.1007/s11999-013-3397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deitch JR, Starkey C, Walters SL, Moseley JB. Injury risk in professional basketball players: A comparison of women’s National Basketball Association and National Basketball Association Athletes. Am J Sports Med. 2006;34:1077–1083. doi: 10.1177/0363546505285383. [DOI] [PubMed] [Google Scholar]
- 18.Lian ØB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 19.Taunton JE. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zwerver J, Bredeweg SW, van den Akker-Scheek I. Prevalence of Jumper’s Knee among nonelite athletes from different sports: a cross-sectional survey. Am J Sports Med. SAGE Publications Inc STM; 2011;39:1984–8. [DOI] [PubMed]
- 21.Scott A, Backman LJ, Speed C. Tendinopathy: update on pathophysiology. J Orthop Sports Phys Ther. 2015;45:833–841. doi: 10.2519/jospt.2015.5884. [DOI] [PubMed] [Google Scholar]
- 22.Lian Ø, Scott A, Engebretsen L, Bahr R, Duronio V, Khan K. Excessive apoptosis in patellar tendinopathy in athletes. Am J Sports Med USA. 2007;35:605–611. doi: 10.1177/0363546506295702. [DOI] [PubMed] [Google Scholar]
- 23.Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper’s knee in male athletes: a prospective follow-up study. Am J Sports Med. 2002;30:689–692. doi: 10.1177/03635465020300051001. [DOI] [PubMed] [Google Scholar]
- 24.Albers IS, Zwerver J, Diercks RL, Dekker JH, Van den Akker-Scheek I. Incidence and prevalence of lower extremity tendinopathy in a Dutch general practice population: a cross sectional study. BMC Musculoskelet Disord. 2016;17:16. doi: 10.1186/s12891-016-0885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ito E, Iwamoto J, Azuma K, Matsumoto H. Sex-specific differences in injury types among basketball players. Open Access J Sports Med. 2014;6:1–6. doi: 10.2147/OAJSM.S73625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Vries AJ, van der Worp H, Diercks RL, van den Akker-Scheek I, Zwerver J. Risk factors for patellar tendinopathy in volleyball and basketball players: A survey-based prospective cohort study. Scand J Med Sci Sports. 2015;25:678–684. doi: 10.1111/sms.12294. [DOI] [PubMed] [Google Scholar]
- 27.Cassel M, Stoll J, Mayer F. Tendinopathies of the Lower Extremities in Sport - Diagnostics and Therapy. Sportverletzung-Sportschaden. 2015;29:87–98. [DOI] [PubMed]
- 28.Backman LJ, Danielson P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study. Am J Sports Med. 2011;39:2626–2633. doi: 10.1177/0363546511420552. [DOI] [PubMed] [Google Scholar]
- 29.Cook JL, Khan KM, Kiss ZS, Griffiths L. Patellar tendinopathy in junior basketball players: a controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14–18 years. Scand J Med Sci Sports. 2000;10:216–220. doi: 10.1034/j.1600-0838.2000.010004216.x. [DOI] [PubMed] [Google Scholar]
- 30.Morton S, Williams S, Valle X, Diaz-Cueli D, Malliaras P. Patellar tendinopathy and potential risk factors: an international database of cases and controls. Clin J Sport Med. 2017;0:7. [DOI] [PubMed]
- 31.van der Worp H, Zwerver J, Kuijer PPFM, Frings-Dresen MHW, van den Akker-Scheek I. The impact of physically demanding work of basketball and volleyball players on the risk for patellar tendinopathy and on work limitations. J Back Musculoskelet Rehabil Netherlands. 2011;24:49–55. doi: 10.3233/BMR-2011-0274. [DOI] [PubMed] [Google Scholar]
- 32.Mansukhani NA, Yoon DY, Teter KA, Stubbs VC, Helenowski IB, Woodruff TK, et al. Determining if sex bias exists in human surgical clinical research. JAMA Surg. 2016;151:1022. doi: 10.1001/jamasurg.2016.2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng L, Chang S, Qian L, Wang Y, Yang M. Extracorporeal shock wave therapy for isokinetic muscle strength around the knee joint in athletes with patellar tendinopathy. J Sports Med Phys Fitness [Internet]. 2019 [cited 2021 Mar 4];59. Available from: https://www.minervamedica.it/index2.php?show=R40Y2019N05A0822 [DOI] [PubMed]
- 34.de Vries A, Zwerver J, Diercks R, Tak I, van Berkel S, van Cingel R, et al. Effect of patellar strap and sports tape on pain in patellar tendinopathy: a randomized controlled trial: effect strap and tape jumper’s knee symptoms. Scand J Med Sci Sports. 2016;26:1217–1224. doi: 10.1111/sms.12556. [DOI] [PubMed] [Google Scholar]
- 35.Hoksrud A, Öhberg L, Alfredson H, Bahr R. Ultrasound-guided sclerosis of neovessels in painful chronic patellar tendinopathy: a randomized controlled trial. Am J Sports Med. 2006;34:1738–1746. doi: 10.1177/0363546506289168. [DOI] [PubMed] [Google Scholar]
- 36.Alaseirlis DA, Konstantinidis GA, Malliaropoulos N, Nakou LS, Korompilias A, Maffulli N. Arthroscopic treatment of chronic patellar tendinopathy in high-level athletes. :6. [PMC free article] [PubMed]
- 37.Alfredson H, Ohberg L. Neovascularisation in chronic painful patellar tendinosis? promising results after sclerosing neovessels outside the tendon challenge the need for surgery. Knee Surg Sports Traumatol Arthrosc. 2005;13:74–80. doi: 10.1007/s00167-004-0549-x. [DOI] [PubMed] [Google Scholar]
- 38.Ferretti A, Ippolito E, Mariani P, Puddu G. Jumper’s Knee. Am J Sports Med. SAGE Publications Inc STM; 1983;11:58–62. [DOI] [PubMed]
- 39.Santander J, Zarba E, Iraporda H, Puleo S. Can arthroscopically assisted treatment of chronic patellar tendinopathy reduce pain and restore function? Clin Orthop Relat Res. 2012;470:993–997. doi: 10.1007/s11999-011-1886-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shelbourne KD, Henne TD, Gray T. Recalcitrant patellar tendinosis in elite athletes: surgical treatment in conjunction with aggressive postoperative rehabilitation. Am J Sports Med. 2006;34:1141–1146. doi: 10.1177/0363546505284239. [DOI] [PubMed] [Google Scholar]
- 41.van Ark M, van den Akker-Scheek I, Meijer LTB, Zwerver J. An exercise-based physical therapy program for patients with patellar tendinopathy after platelet-rich plasma injection. Phys Ther Sport. 2013;14:124–130. doi: 10.1016/j.ptsp.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 42.Willberg L, Sunding K, Öhberg L, Forssblad M, Alfredson H. Treatment of Jumper’s knee: promising short-term results in a pilot study using a new arthroscopic approach based on imaging findings. Knee Surg Sports Traumatol Arthrosc. 2007;15:676–681. doi: 10.1007/s00167-006-0223-6. [DOI] [PubMed] [Google Scholar]
- 43.Dar G, Mei-Dan E. Immediate effect of infrapatellar strap on pain and jump height in patellar tendinopathy among young athletes. Prosthet Orthot Int. 2019;43:21–27. doi: 10.1177/0309364618791619. [DOI] [PubMed] [Google Scholar]
- 44.Lee W-C, Ng GY-F, Zhang Z-J, Malliaras P, Masci L, Fu S-N. Changes on tendon stiffness and clinical outcomes in athletes are associated with patellar tendinopathy after eccentric exercise. Clin J Sport Med. 2020;30:25–32. [DOI] [PubMed]
- 45.Rio E, Purdam C, Girdwood M, Cook J. Isometric exercise to reduce pain in patellar tendinopathy in-season: is it effective “on the road”? Clin J Sport Med. 2019;29:188–192. doi: 10.1097/JSM.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 46.Rosen AB. Patellar tendon straps decrease pre-landing quadriceps activation in males with patellar tendinopathy. :26. [DOI] [PubMed]
- 47.Scott A, LaPrade RF, Harmon KG, Filardo G, Kon E, Della Villa S, et al. Platelet-rich plasma for patellar tendinopathy: a randomized controlled trial of leukocyte-rich PRP or leukocyte-poor PRP versus saline. Am J Sports Med. 2019;47:1654–1661. doi: 10.1177/0363546519837954. [DOI] [PubMed] [Google Scholar]
- 48.Willberg L, Sunding K, Forssblad M, Fahlstrom M, Alfredson H. Sclerosing polidocanol injections or arthroscopic shaving to treat patellar tendinopathy/jumper’s knee? A randomised controlled study. Br J Sports Med. 2011;45:411–415. doi: 10.1136/bjsm.2010.082446. [DOI] [PubMed] [Google Scholar]
- 49.Andriolo L, Altamura SA, Reale D, Candrian C, Zaffagnini S, Filardo G. Nonsurgical treatments of patellar tendinopathy: multiple injections of platelet-rich plasma are a suitable option: a systematic review and meta-analysis. Am J Sports Med. 2019;47:1001–1018. doi: 10.1177/0363546518759674. [DOI] [PubMed] [Google Scholar]
- 50.Women in Sports Statistics - Female Athletes Participation. International Olympic Committee. 2021. Available from: https://www.olympic.org/women-in-sport/background/statistics
- 51.Zelisko JA, Noble HB, Porter M. A comparison of men’s and women’s professional basketball injuries. Am J Sports Med. 1982;10:297–299. doi: 10.1177/036354658201000507. [DOI] [PubMed] [Google Scholar]
- 52.Gray J, Taunton J, McKenzie D, Clement D, McConkey J, Davidson R. A survey of injuries to the anterior cruciate ligament of the knee in female basketball players. Int J Sports Med. 1985;06:314–316. doi: 10.1055/s-2008-1025861. [DOI] [PubMed] [Google Scholar]
- 53.Bijur PE. Comparison of injury during cadet basic training by gender. Arch Pediatr Adolesc Med. 1997;151:456. doi: 10.1001/archpedi.1997.02170420026004. [DOI] [PubMed] [Google Scholar]
- 54.Jones BH, Bovee MW, Harris JMcA, Cowan DN. Intrinsic risk factors for exercise-related injuries among male and female army trainees. Am J Sports Med. 1993;21:705–10. [DOI] [PubMed]
- 55.Liu SH, Al-Shaikh R, Panossian V, Yang R-S, Soleiman N, Finerman GAM, et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament. J Orthop Res. 1996;14:526–533. doi: 10.1002/jor.1100140405. [DOI] [PubMed] [Google Scholar]
- 56.Hart DA, Archambault JM, Kydd A, Reno C, Frank CB, Herzog W. Gender and neurogenic variables in tendon biology and repetitive motion disorders. Clin Orthop Relat Res. 1998;44–56. [PubMed]
- 57.Liu SH, Al-Shaikh RA, Panossian V, Finerman GAM, Lane JM. Estrogen affects the cellular metabolism of the anterior cruciate ligament: a potential explanation for female athletic injury. Am J Sports Med. 1997;25:704–709. doi: 10.1177/036354659702500521. [DOI] [PubMed] [Google Scholar]
- 58.Yu WD, Panossian V, Hatch JD, Liu SH, Finerman GAM. Combined effects of estrogen and progesterone on the anterior cruciate ligament. Clin Orthopaedics Related Res. 2001;383:268–81. [DOI] [PubMed]
- 59.Miller BF, Hansen M, Olesen JL, Schwarz P, Babraj JA, Smith K, et al. Tendon collagen synthesis at rest and after exercise in women. J Appl Physiol. 2007;102:541–546. doi: 10.1152/japplphysiol.00797.2006. [DOI] [PubMed] [Google Scholar]
- 60.Sullivan BE, Carroll CC, Jemiolo B, Trappe SW, Magnusson SP, Døssing S, et al. Effect of acute resistance exercise and sex on human patellar tendon structural and regulatory mRNA expression. J Appl Physiol. 1985;2009(106):468–475. doi: 10.1152/japplphysiol.91341.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Westh E, Kongsgaard M, Bojsen-Moller J, Aagaard P, Hansen M, Kjaer M, et al. Effect of habitual exercise on the structural and mechanical properties of human tendon, in vivo, in men and women: effect of habitual exercise on the structural and mechanical properties of human tendon. Scand J Med Sci Sports. 2007;18:23–30. doi: 10.1111/j.1600-0838.2007.00638.x. [DOI] [PubMed] [Google Scholar]
- 62.Onambélé GNL, Burgess K, Pearson SJ. Gender-specific in vivo measurement of the structural and mechanical properties of the human patellar tendon. J Orthop Res. 2007;25:1635–1642. doi: 10.1002/jor.20404. [DOI] [PubMed] [Google Scholar]
- 63.Magnusson SP, Hansen M, Langberg H, Miller B, Haraldsson B, Kjoeller Westh E, et al. The adaptability of tendon to loading differs in men and women: Gender differences in tendon adaptation. Int J Exp Pathol. 2007;88:237–240. doi: 10.1111/j.1365-2613.2007.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hansen M, Miller BF, Holm L, Doessing S, Petersen SG, Skovgaard D, et al. Effect of administration of oral contraceptives in vivo on collagen synthesis in tendon and muscle connective tissue in young women. J Appl Physiol. 2009;106:1435–1443. doi: 10.1152/japplphysiol.90933.2008. [DOI] [PubMed] [Google Scholar]
- 65.Burgess KE, Pearson SJ, Breen L, Onambélé GNL. Tendon structural and mechanical properties do not differ between genders in a healthy community-dwelling elderly population. J Orthop Res. 2009;27:820–825. doi: 10.1002/jor.20811. [DOI] [PubMed] [Google Scholar]
- 66.Aubrun F, Salvi N, Coriat P, Riou B. Sex- and age-related differences in morphine requirements for postoperative pain relief. Anesthesiology. 2005;103:156–160. doi: 10.1097/00000542-200507000-00023. [DOI] [PubMed] [Google Scholar]
- 67.Cepeda MS, Carr DB. Women experience more pain and require more morphine than men to achieve a similar degree of analgesia. Anesth Analg. 2003;97:1464–1468. doi: 10.1213/01.ANE.0000080153.36643.83. [DOI] [PubMed] [Google Scholar]
- 68.Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Taenzer AH, Clark C, Curry CS. Gender affects report of pain and function after arthroscopic anterior cruciate ligament reconstruction. Anesthesiology. 2000;93:670–675. doi: 10.1097/00000542-200009000-00015. [DOI] [PubMed] [Google Scholar]
- 70.Raz L, Miller VM. Considerations of sex and gender differences in preclinical and clinical trials. In: Regitz-Zagrosek V, editor. Sex and gender differences in pharmacology. Berlin, Heidelberg: Springer; 2012 [cited 2021 Jan 27]. p. 127–47. Available from: 10.1007/978-3-642-30726-3_7 [DOI] [PubMed]
- 71.Norman JL, Fixen DR, Saseen JJ, Saba LM, Linnebur SA. Zolpidem prescribing practices before and after Food and Drug Administration required product labeling changes. SAGE Open Med. 2017;5:2050312117707687. doi: 10.1177/2050312117707687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Farkas RH. Zolpidem and Driving Impairment — Identifying Persons at Risk. N Engl J Med. 2013;22:689–691. doi: 10.1056/NEJMp1307972. [DOI] [PubMed] [Google Scholar]
- 73.Liu KA, DiPietro Mager NA. Women’s involvement in clinical trials: historical perspective and future implications. Pharm Pract (Granada) 2016;14:708–708. doi: 10.18549/PharmPract.2016.01.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Haughom BD, Erickson BJ, Hellman MD, Jacobs JJ. Do complication rates differ by gender after metal-on-metal hip resurfacing arthroplasty? A systematic review. Clin Orthop Relat Res. 2015;473:2521–2529. doi: 10.1007/s11999-015-4227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Daniels SD, Stewart CM, Garvey KD, Brook EM, Higgins LD, Matzkin EG. Sex-based differences in patient-reported outcomes after arthroscopic rotator cuff repair. Orthop J Sports Med. 2019;7:232596711988195. doi: 10.1177/2325967119881959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kalliainen LK, Wisecarver I, Cummings A, Stone J. Sex bias in hand surgery research. J Hand Surg. 2018;43:1026–1029. doi: 10.1016/j.jhsa.2018.03.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current systematic review are available from the corresponding author on reasonable request.