Abstract
While ultrasound (US) is considered an important tool for hepatocellular carcinoma (HCC) surveillance, it has limited sensitivity for detecting early-stage HCC. Abbreviated MRI (AMRI) has recently gained popularity owing to better sensitivity in its detection of early-stage HCC than US, while also minimizing the time and cost in comparison to complete contrast-enhanced MRI, as AMRI includes only a few essential sequences tailored for detecting HCC. Currently, three AMRI protocols exist, namely gadoxetic acid-enhanced hepatobiliary-phase AMRI, dynamic contrast-enhanced AMRI, and non-enhanced AMRI. In this study, we discussed the rationale and technical details of AMRI techniques for achieving optimal surveillance performance. The strengths, weaknesses, and current issues of each AMRI protocol were also elucidated. Moreover, we scrutinized previously performed AMRI studies regarding clinical and technical factors. Reporting and recall strategies were discussed while considering the differences in AMRI protocols. A risk-stratified approach for the target population should be taken to maximize the benefits of AMRI and the cost-effectiveness should be considered. In the era of multiple HCC surveillance tools, patients need to be fully informed about their choices for better adherence to a surveillance program.
Keywords: Hepatocellular carcinoma, Surveillance, Abbreviated magnetic resonance imaging
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most prevalent primary liver cancer and a leading cause of cancer-related death worldwide [1,2]. The incidence rate of HCC has increased in recent decades [2,3]. Early detection of HCC allows patients to be considered for curative therapies that improve survival. Hence, the importance of HCC surveillance in high-risk patients cannot be overemphasized [4]. International guidelines for HCC management recommend imaging-based HCC surveillance for at-risk patients [5,6,7] using a bi-annual ultrasound (US) with or without serum α-fetoprotein (AFP) measurements. Overall, US has shown a wide range of sensitivity (58%–94%) and high specificity (> 90%) for detecting HCC [8,9].
Although the use of US has been universally accepted for HCC surveillance, recent studies have raised concerns about its sensitivity for detecting HCC at early or very early stages [9,10,11,12]. A meta-analysis of 15 studies and 4400 patients reported that US sensitivity was as low as 47% for early-stage HCC [10]. Two recent prospective studies conducted in a surveillance setting also reported poor US sensitivity for very early stage HCC (< 30%) [11,12]. Recently updated international guidelines for HCC allow alternative surveillance tools, including CT or MRI [5,6,7]. Considering the need for continuous periodic surveillance, the use of CT has inherent drawbacks relating to radiation hazards and the risks of using iodine contrast agents, despite its acceptable diagnostic performance [12]. Complete MRI is widely used for characterizing focal hepatic lesions and has superb performance. However, MRI as a surveillance tool has limitations due to the extended time and costs involved in the examination and interpretation of results [11].
To overcome these limitations, abbreviated MRI (AMRI) using a few essential MRI sequences has gained acceptance. AMRI provides the same high performance as conventional MRI but saves time and reduces the cost by eliminating redundant sequences. Several recently published meta-analyses support AMRI as a surveillance tool [5,13,14,15]. However, some studies included in these meta-analyses were conducted in a diagnostic setting with a high incidence of HCC. The sequences selected for AMRI, which can affect the performances of AMRI-based surveillance programs, varied across different studies. Additionally, the successful clinical implementation of AMRI must consider the reporting methods for AMRI results, the quality of the examinations, and a recall strategy for positive results. The limited availability of MRI compared to US necessitates a tailored strategy for using AMRI-based HCC surveillance. For example, prioritizing patients who would gain the most benefits from AMRI than from US (rather than applying AMRI uniformly to all target populations for HCC surveillance).
This review illustrated the current landscape and future perspectives of AMRI by presenting the rationale and results of AMRI-based studies considering the study population and technical details. We also discussed the reporting of patient results and follow-up, and described the use of a risk-stratified approach for better cost-effectiveness.
AMRI Methods and Performances
For effective surveillance using AMRI, scanning methods should be simplified by including only essential image sequences to maximize detection ability while minimizing time and cost. Currently, there are three AMRI protocols: gadoxetic acid-enhanced MRI with hepatobiliary-phase (HBP) imaging (referred to as HBP-AMRI), dynamic contrast-enhanced MRI (referred to as DCE-AMRI), and non-enhanced MRI (referred to as NE-AMRI) (Table 1). The high sensitivity and acceptable specificity of these AMRI protocols have been reported previously [5,13,14,15]. Although recent meta-analyses have summarized the diagnostic accuracy of AMRI with or without contrast-enhancement (Table 2) [5,13,14,15], many of the included studies were conducted in a diagnostic setting in which the complete MRIs were originally indicated in patients with known or suspected liver lesions, which likely caused selection bias and overestimation of the sensitivity of AMRI. The results of such studies should be interpreted with care, considering factors that may affect the results, including clinical factors (e.g., clinical settings, HCC incidences, and underlying liver diseases) and technical details of the MRI sequences. In this review, we focused on the performance of AMRI studies conducted in a surveillance setting.
Table 1. Summary of AMRI Approaches.
| HBP-AMRI | DCE-AMRI | NE-AMRI | |
|---|---|---|---|
| Sequences | HBP, DWI, T2WI | Pre- and post-contrast T1WI (AP, PVP, DP/TP) | DWI, T2WI, optional T1W IP/OP |
| Scan time including set-up time*, min | < 15 | < 17 | < 14 |
| Strength | - Highest sensitivity among AMRI approaches | - No requirement of a recall test after positive results - Evaluation of vascular thrombus |
- Most time- and cost-saving - No contrast agent-related issues |
| Weakness | - Relatively high false-positive by detecting precursor lesions - Additional recall tests needed - Lesion conspicuity on HBP imaging influenced by liver function - Limited evaluation for vascular thrombus - Potential harms related to contrast agent |
- Short time window for AP imaging - Not evaluable ancillary imaging features - Potential harms related to contrast agent |
- Heavily dependent on DWI for lesion detection which is prone to artifacts - Limited evaluation for vascular thrombus - Additional recall tests needed |
*Reported values from the literature including the set-up time (i.e., room turnover, installation, calibration, sequence preparation, and intravenous line placement if required). AMRI = abbreviated MRI, AP = arterial phase, DCE = dynamic contrast enhanced, DP/TP = delayed/transitional phase, DWI = diffusion-weighted imaging, HBP = hepatobiliary-phase, IP/OP = in/opposed phase, NE = non-enhanced, PVP = portal venous phase, T1W = T1-weighted, T2WI = T2-weighted imaging
Table 2. Summary of Meta-Analyses on the Diagnostic Performance of AMRI for Hepatocellular Carcinoma Detection.
| Study | Year | Total Number of AMRI Studies | Number of Studies Performed in a Diagnostic Setting | Number of Studies Performed in a Surveillance Setting | Pooled Sensitivity (%)* | Pooled Specificity (%)* |
|---|---|---|---|---|---|---|
| Gupta et al. [13] | 2021 | 15 | 7 | 8 | 86 (84–88) | 94 (91–96) |
| Chan et al. [14] | 2021 | 22 | 18 | 4 | 86.8 (83.9–89.4) | 90.3 (87.3–92.7) |
| Kim et al. [5] | 2021 | 10 | 3 | 7 | 86 (80–90) | 96 (93–98) |
| Kim et al. [15] | 2021 | 4 | 1 | 3 | 87 (80–94) | 94 (90–98) |
*Numbers in parentheses are 95% confidence intervals. AMRI = abbreviated MRI
HBP-AMRI
Details of Sequences
HBP-AMRI using gadoxetic acid aims to maintain the highly sensitive nature of HBP imaging for lesion detection while reducing the examination time by omitting dynamic contrast-enhanced sequences for lesion characterization. The examination workflow is simplified and quickened by injecting gadoxetic acid while the patient is in the waiting area rather than the MRI unit. The imaging sequences of HBP-AMRI include HBP imaging, diffusion-weighted imaging (DWI), and T2-weighted image (T2WI). The reported image acquisition time of HBP-AMRI is less than 15 minutes including the set-up time (i.e., room turnover, installation, calibration, sequence preparation, and intravenous line placement if required) [16,17,18]. With the evolving imaging techniques and the application of deep learning, the examination time may become even shorter soon.
HBP imaging is typically acquired 15–20 minutes after the gadoxetic acid injection. It uses the most sensitive imaging sequence to detect HCC with high liver-to-lesion contrast [19,20]. However, it is limited in lesion characterization as HBP hypointensity itself is not specific for HCC. For example, HBP hypointensity is also found in other lesions, including benign lesions such as hepatic hemangiomas and premalignant lesions such as dysplastic nodules [21,22,23]. Vessels also show hypointensity on HBP, which can cause a perception error and hinder the detection of true focal hepatic lesions.
DWI is known as a highly sensitive sequence for detecting HCC and other hepatic malignancy based on the high cellularity of the lesion [24,25,26,27,28]. Hence, DWI may be considered in addition to HBP-AMRI to enhance sensitivity, particularly for small hepatic lesions adjacent to vessels. The sensitivity of HBP-AMRI can be maximized by combining HBP imaging and DWI [17]. In previous studies, MRI for HCC surveillance mostly utilized free-breathing DWI with two to three b-values ranging from 0 to 1000 s/mm2 (Table 3). However, the optimal number and range of b-values for surveillance have not yet been fully determined. The acquisition time of DWI in liver MRI is reported to be 3–6 minutes with the free-breathing method and 5–6 minutes with the respiratory triggering method [29]. The simultaneous multi-slice (SMS) technique is a recently introduced option for accelerating the image acquisition of DWI [30]. SMS-DWI has shown acceptable image quality with a shorter acquisition time than conventional DWI [31,32].
Table 3. Summary of AMRI Studies Performed in a Surveillance Setting.
| Study | Year | Study Design | Country | Sample Size | M/C Etiology (%) | LC (%) | HCC (%) | Sens (%) | Spec (%) | Detected HCC Size (cm) | Sequences | Sequence Details | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.5T* | 3T* | |||||||||||||
| HBP-AMRI | ||||||||||||||
| Marks et al. [51] | 2015 | R | USA | 298 | HCV (51.0) | NR | 16.4 | 83.7 | 93.2 | 1.0–1.9: 28.6%, ≥ 2.0: 71.4% | HBP | |||
| DWI (FB) | b = 0, 300–400 | b = 0, 500–600 | ||||||||||||
| T2WI | TE 78–120 | TE 68–97 | ||||||||||||
| Tillman et al. [52] | 2018 | R | USA | 79 | HBV (41.8) | 64.6 | 16.5 | 85.2 | NR | Median, 2.1 (range, 1.1–10) | HBP | |||
| T2WI | TE 90–95 | TE 80–90 | ||||||||||||
| Brunsing et al. [16] | 2019 | R | USA | 141 | HCV (42.6) | 92.9 | 8.5 | 92.0 | 91.0 | Range, 1.1–4.3 | HBP | |||
| DWI (FB) | - | b = 0–50, 500, 1000 | ||||||||||||
| T2WI | - | TE 70–100 | ||||||||||||
| Vietti Violi et al. [17] | 2020 | R | USA | 237 | HCV (25.7) | 87.3 | 5.5 | 80.8 | 94.9 | Mean, 3.4 (range, 1–12) | HBP | |||
| DWI (FB) | b = 50, 400, 800 | b = 50, 400, 800 | ||||||||||||
| T2WI | TE 227–240 | TE 180–228 | ||||||||||||
| Park et al. [53] | 2021 | R | Korea | 382 | HBV (72.3) | 100.0 | 11.3 | 86.0 | 95.6 | Mean, 1.6 | HBP | |||
| DWI (RT) | b = 0, 50, 500 | - | ||||||||||||
| T2WI | TE 154 | - | ||||||||||||
| DCE-AMRI | ||||||||||||||
| Vietti Violi et al. [17] | 2020 | R | USA | 237 | HCV (25.7) | 87.3 | 5.5 | 84.6 | 99.8 | Mean, 3.4 (range, 1–12) | T1w DCE | Gadoxetic acid | Gadoxetic acid | |
| T2WI | TE 227–240 | TE 180–228 | ||||||||||||
| NE-AMRI | ||||||||||||||
| Sutherland et al. [77] | 2017 | P | Australia | 192 | HBV (56.0) | NR | 3.0 | 83.0 | 98.0 | Range, 0.8–3.1 | DWI (RT) | b = 100, 400, 800† | ||
| Vietti Violi et al. [17] | 2020 | R | USA | 237 | HCV (25.7) | 87.3 | 5.5 | 61.5 | 95.5 | Mean, 3.4 (range, 1–12) | DWI (FB) | b = 50, 400, 800 | b = 50, 400, 800 | |
| T2WI | TE 227–240 | TE 180–228 | ||||||||||||
| Park et al. [27] | 2020 | R | Korea | 382 | HBV (72.3) | 100.0 | 11.3 | 79.1 | 97.9 | Mean, 1.6 | DWI (RT) | b = 0, 50, 500 | - | |
| T2WI | TE 154 | - | ||||||||||||
| Ahmed et al. [82] | 2020 | P | Egypt | 41 | HCV (100.0) | 100.0 | 24.3 | 100.0 | 100.0 | NR | DWI (NR) | b = 0, 200, 800 | - | |
| T2WI | NR | - | ||||||||||||
| Choi et al. [81]‡ | 2020 | P | Korea | 161 | HBV (72.3) | 100.0 | 19.3 | 71.0 | NR | NR | DWI (NR) | - | b = 0, 50, 500 | |
| T2WI | - | NR | ||||||||||||
| T1W IP/OP | ||||||||||||||
*TE in msec and b-value in s/mm2, †Field strength was not reported, ‡Diagnostic performance from three repetitive rounds of annual NE-AMRI. AMRI = abbreviated MRI, AP = arterial phase, DCE = dynamic contrast enhanced, DWI = diffusion-weighted imaging, FB = free-breathing, HBP = hepatobiliary-phase, HBV = Hepatitis B virus, HCC = hepatocellular carcinoma, HCV = Hepatitis C virus, IP/OP = in/opposed phases, LC = prevalence of liver cirrhosis, M/C = most common, NE = non-enhanced, NR = not reported, P = prospective, PVP = portal venous phase, R = retrospective, RT = respiratory triggered, Sens = sensitivity, Spec = specificity, TE = echo time, TP = transitional phase, TR = repetition time
T2WI is essential, not only to detect lesions, but also to exclude common benign lesions, such as hemangiomas or cysts that mimic HCC on DWI or HBP imaging. By excluding these typical benign lesions with bright T2 signal intensity, the specificity for HCC detection is improved. HCC, in contrast, shows mild to moderate-high T2 signal in most of the cases. In HCC surveillance, a heavily T2WI sequence is preferred to a moderately T2WI for HBP-AMRI (Table 3). A heavily T2WI sequence is preferable for discriminating cysts and hemangiomas from solid tumors than a moderately T2WI sequence [33,34,35]. As HBP and DWI are both important for lesion detection using HBP-AMRI, a heavily T2WI sequence may be a better triage tool. The T2 signal intensity of hemangioma in AMRI may be affected by intratumoral retention of gadoxetic acid [36,37]. However, since all the images can be acquired within 15–20 minutes following contrast injection, the residual gadolinium content within the hemangioma would be minimal. Thus, the T2 shortening effect of gadolinium may be negligible. According to previous studies, there were no significant changes in the conspicuity and signal-to-noise ratio of hemangioma before and after gadoxetic acid injection (after the transitional phase) in both heavily and moderately T2WI sequences [38,39].
Deep learning techniques can shorten the image acquisition time and enhance the image quality of both T2WI and DWI, which traditionally demanded long acquisition times [40,41,42,43,44]. The advances in image processing through deep learning are expected to further enhance the time efficiency of AMRI programs.
T1-weighted dual-echo imaging enables the assessment of intralesional fat, an ancillary feature favoring HCC, particularly according to the Liver Imaging-Reporting and Data System (LI-RADS) [45]. T1-weighted dual-echo imaging can be acquired in a single breath-hold using most current MRI systems. However, no study regarding the effect of gadolinium in T1-weighted dual-echo imaging in HBP-AMRI has been conducted in a surveillance setting. Two studies conducted in diagnostic settings [46,47] evaluated HBP-AMRI, including T1-weighted dual-echo imaging. However, in both studies, HBP-AMRI scans were retrospectively simulated from the complete gadoxetic acid-enhanced MRI scans and thus did not reflect contrast effects on dual-echo imaging. Theoretically, owing to the paramagnetic effect of gadolinium, its presence may cause a signal loss in chemical shift imaging. According to previous studies that evaluated the influence of gadoxetic acid on fat quantification using liver MRI, fat fraction obtained 15–20 minutes after gadoxetic acid injection was smaller than that calculated on pre-contrast imaging [48,49,50]. The effects of gadoxetic acid on dual-echo imaging and its utility in HBP-AMRI should be further elucidated in future studies.
Performance
To date, five studies [16,17,51,52,53] have assessed the performance of HBP-AMRI in a surveillance setting for at-risk patients with no history of HCC (Table 3). Four of the studies included prospectively recruited patient cohorts [16,51,52,53]. In one study, HBP-AMRI scans were acquired and interpreted prospectively [16], while in the other four studies, HBP-AMRI scans were simulated by extracting only the required sequences from the previously acquired complete contrast-enhanced MRI scans and interpreted retrospectively. In studies conducted in a surveillance setting, the reported per-patient sensitivity ranged from 80.8% to 92.0%, and the specificity ranged from 91.0% to 95.6%. According to a recent meta-analysis by Gupta et al. [13], the pooled sensitivity and specificity of six studies on HBP-AMRI [16,17,46,51,52,54] was 86% and 94%, respectively. Although no prospective study has yet been published, there is an ongoing clinical trial to compare the clinical feasibility of HBP-AMRI versus US in Korea (NCT03731923).
Reporting
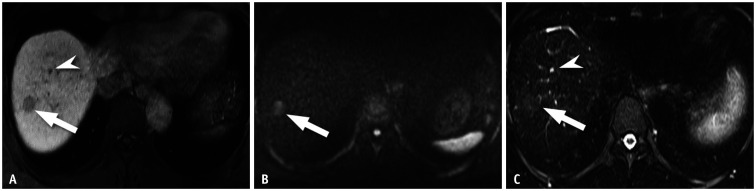
The assessment and recall criteria of HBP-AMRI across reported studies, including the number of categories and scoring systems, varied [16,17,51,52,53]. However, the studies commonly regarded the lesion size ≥ 10 mm, HBP hypointensity, mild to moderate T2 hyperintensity, and/or restricted diffusion as suspicious features requiring further evaluation for HCC (Fig. 1).
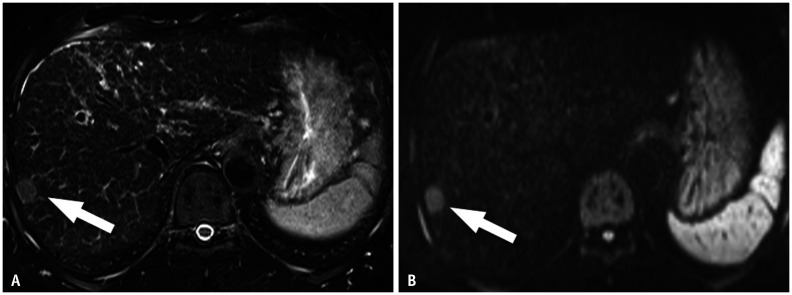
Fig. 1. Positive HBP-abbreviated MRI examination.
A-C. In a 58-year-old male with hepatitis B-associated liver cirrhosis, a HBP image (A) demonstrates a 1.2-cm hypointense observation in liver segment VIII (arrow). This observation shows restricted diffusion on diffusion-weighted imaging (B, b-value = 500 s/mm2, arrow) and mild high signal intensity on heavily T2WI (C, arrow). The patient underwent biopsy, and this observation was pathologically confirmed as a very early stage hepatocellular carcinoma. Note that there is another tiny hypointense observation anteriorly to the 1.2-cm observation on the HBP image (A, arrowhead), which can be easily regarded as a negative observation by its markedly high signal intensity on T2WI (C, arrowhead). HBP = hepatobiliary-phase, T2WI = T2-weighted imaging
Although there have been no guidelines on how to report AMRI, a standardized report for effective and consistent recommendations to referring clinicians is preferable. Structured reporting of HBP-AMRI for HCC surveillance could adapt that of the US LI-RADS, which was also developed for a surveillance setting [18,55]. The assessment of each HBP-AMRI study can be reported as “negative”, “subthreshold”, or “positive” for suspected observations. A study with the following observation(s): lesions ≥ 10 mm, that are not definitely benign or a thrombus in a vein, should be regarded as “positive” and recall tests recommended. Given the repetitive nature of surveillance, the interval between observation(s) prior to the HBP-AMRI should also be considered. Table 4 shows the suggested standardized reporting and recall strategy for liver observations in each AMRI protocol.
Table 4. Suggested Standardized Reporting and Recall Strategies for Liver Observations Found on Each AMRI Protocol.
| Category | HBP-AMRI | DCE-AMRI | NE-AMRI | |||
|---|---|---|---|---|---|---|
| Definition | Recall Strategy | Definition | Recall Strategy | Definition | Recall Strategy | |
| Negative | - No observation - Only definitely benign observation(s)* |
- Return to routine surveillance | - No observation | - Return to routine surveillance | - No observation - Only definitely benign observation(s)* |
- Return to routine surveillance |
| - LR-1 | ||||||
| - LR-2 | ||||||
| Subthreshold | - Observation(s) < 10 mm, not definitely benign† - Previous positive observation(s) confirmed as false positive |
- Short-term follow-up | - LR-3 | - Short-term follow-up | - Observation(s) < 10 mm, not definitely benign† - Previous positive observation(s) confirmed as false positive |
- Short-term follow-up |
| Positive | - Observation(s) ≥ 10 mm, not definitely benign† - Changes in imaging characteristics‡ or threshold growth§ of previous subthreshold observation(s) - Thrombus in a vein |
- Immediate further evaluation with diagnostic test (dynamic CT/MRIǁ) | - LR-5 | - Confirmatory diagnosis of HCC without additional recall tests | - Observation(s) ≥ 10 mm, not definitely benign† - Changes in imaging characteristics‡ or threshold growth§ of previously subthreshold observation(s) - Thrombus in a vein |
- Immediate further evaluation with diagnostic imaging (dynamic CT/ MRI¶) |
| - LR-4 | - Second-look MRI (NE-AMRI or HBP-AMRI) or - Multidisciplinary decision for individualized workup |
|||||
| - LR-TIV | - Multidisciplinary decision for individualized workup | |||||
| - LR-M | ||||||
*Marked T2 hyperintensity suggesting hemangioma or cyst, †Diffusion restriction or mild to moderate T2 hyperintensity or HBP hypointensity, ‡Any new appearance of not-definitely-benign characteristics, §Size increase by ≥ 50% in ≤ 6 months, ∥For MRI, extracellular contrast material is preferred over gadoxetic acid, ¶Diffusion-weighted imaging and T2-weighted imaging can be omitted and only pre- and post-contrast enhanced T1-weighted sequences need to be added. AMRI = abbreviated MRI, DCE = dynamic contrast enhanced, HBP = hepatobiliary-phase, HCC = hepatocellular carcinoma, NE = non-enhanced
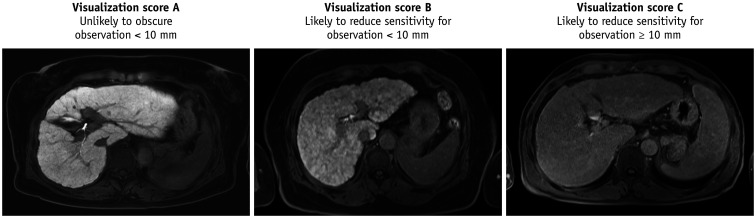
The image quality of HBP images should also be reported, as the image quality affects the lesion conspicuity [56,57]. Similar to that of the US LI-RADS [55], the image quality of the HBP-AMRI could be categorized according to the presence and severity of limitations, and the likeliness of reduced sensitivity to detect liver observations. For HBP images, the relative signal intensity of the liver compared to that of the vessels, the heterogeneity of liver texture, and the presence of image artifact should be considered (Fig. 2) [18]. The suggested image quality classification for each AMRI protocol is summarized in Table 5.
Fig. 2. Image quality categorization of HBP-AMRI.
The image quality of HBP-AMRI could be categorized according to the presence and the severity of limitations and the likeliness of reduced sensitivity to detect liver observations on HBP images. The relative signal intensity of the liver compared to that of the vessels, the heterogeneity of liver texture, and the presence of image artifact should be considered. AMRI = abbreviated MRI, HBP = hepatobiliary-phase
Table 5. Classification of Image Quality of Each Imaging Modality.
| HBP-AMRI | DCE-AMRI | NE-AMRI | ||
|---|---|---|---|---|
| Key sequence | HBP imaging | Arterial phase imaging | Diffusion-weighted imaging | |
| Score | ||||
| A (unlikely to obscure observation < 10 mm) | - Liver signal considerably higher than that of the vessels - Liver texture homogeneous or mildly heterogeneous |
- No or minimal motion artifact, no effect on diagnostic quality - Proper timing of late arterial phase imaging |
- No or minimal motion or susceptibility artifact, no effect on diagnostic quality | |
| B (likely to reduce sensitivity for observation < 10 mm) | - Liver signal only slightly higher than that of the vessels - Liver texture moderately heterogeneous |
- Moderate motion artifact, some but not severe effect on diagnostic quality | - Moderate motion or susceptibility artifact, some but not severe effect on diagnostic quality | |
| C (likely to reduce sensitivity for observation ≥ 10 mm) | - Liver signal same or lower than that of the vessels - Liver texture severely heterogeneous - Severe artifact |
- Severe or extensive motion artifact, barely interpretable or nondiagnostic | - Severe or extensive motion or susceptibility artifact, barely interpretable or nondiagnostic | |
Visualization score B or C will require a brief description of the specific limitations by the radiologist. AMRI = abbreviated MRI, DCE = dynamic contrast enhanced, HBP = hepatobiliary-phase, NE = non-enhanced
Recall Tests
Suggested algorithms for recall and management of the detected liver observations of each AMRI protocol are shown in Figure 3. Recall tests are required if a “positive” observation is detected on HBP-AMRI for further characterization. As vascular profiles of lesions essential for the diagnosis of HCC are not evaluable with HBP-AMRI alone, confirmatory imaging tests should contain dynamic contrast-enhancement phases in which arterial phase hyperenhancement (APHE) and washout can be demonstrated. Both dynamic contrast-enhanced CT and MRI can be used as confirmatory tests. Park et al. [47] suggested that dynamic CT can be used as a sequential examination for liver observations detected on HBP-AMRI. When MRI is used, imaging sequences in the HBP-AMRI that have already been evaluated are not necessarily repeated. Instead, only dynamic contrast-enhanced sequences are included. Regarding the contrast agent of confirmatory MRI, extracellular contrast media (ECCM) is preferred to gadoxetic acid, as arterial phase images of gadoxetic acid-enhanced MRI are often unsatisfactory, owing to the weaker arterial enhancement [58,59] and respiratory motion artifacts, with a reported incidence of 4.8% to 26.7% [60,61,62].
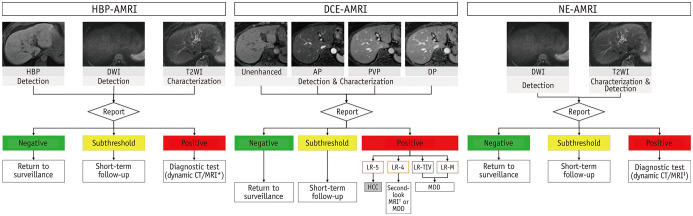
Fig. 3. Summary of AMRI protocols with suggested algorithms for reporting and recall strategies of the detected liver observation.
*For MRI, extracellular contrast material may be preferred to gadoxetic acid, †NE-AMRI or HBP-AMRI, ‡DWI and T2WI can be omitted. AMRI = abbreviated MRI, AP = arterial phase, DCE = dynamic contrast-enhanced, DP = delayed phase, DWI = diffusion-weighted imaging, HBP = hepatobiliary-phase, HCC = hepatocellular carcinoma, MDD = multidisciplinary discussion, NE = non-enhanced, PVP = portal venous phase, T2WI = T2-weighted imaging
Issues
There are several issues with HBP-AMRI-based HCC surveillance. First, false-positive findings on HBP imaging can be relatively high. HBP hypointensity can be seen in “any” focal hepatic lesion with reduced expression of OATP transporter (including HCC and non-HCC lesions) [21]. Discriminating benignity and malignancy in HBP hypointense lesions is not always possible with only DWI and T2WI in the absence of dynamic information. For a surveillance test, high sensitivity is important. On the contrary, low specificity may lead to unnecessary referrals, resulting in potential psychologic and physiologic harm to the patient [63]. Thus, the impact of false positives due to a relatively low specificity should be considered when implementing HBP-AMRI as an HCC surveillance tool. Second, recall tests providing hemodynamic information should be mandatory in a positive case. However, this increases cost and time. Third, patients with poor liver function and consequently poor hepatic enhancement during HBP may hinder the detection of HCC on HBP images [56,57]. Fourth, tumor thrombus, found in up to 44% of patients with HCC, is an important factor determining the proper therapeutic option [64], and can be missed with HBP-AMRI due to the lack of dynamic contrast-enhancement sequences. Although the occluded vein may show restricted diffusion [65], sensitivity is limited and DWI alone cannot reliably discriminate a tumor thrombus from a bland thrombus [66,67]. Fifth, increasing concerns regarding the potential risks related to gadolinium-based MRI contrast agents, including nephrogenic systemic fibrosis and the retention of gadolinium in human tissues must be considered [68,69]. Given the repetitive nature of surveillance tests, potential risks should not be easily dismissed.
DCE-AMRI
Details of Sequences
DCE-AMRI is composed of fat-saturated T1-weighted pre-contrast images and successive post-contrast phase images (arterial phase, portal venous phase, and delayed phase/transitional phase) following the administration of either ECCM or liver-specific contrast agent. DCE-AMRI is timesaving as it omits sequences other than the dynamic contrast-enhancement phases, such as DWI or T2WI. The reported approximate image acquisition time for DCE-AMRI is less than 17 minutes, including set-up time [17,70].
The major advantage of this strategy is that it can demonstrate the major features essential for a definite diagnosis of HCC [45]. If the lesion fulfills LR-5 criteria, an HCC diagnosis can be made with DCE-AMRI alone without the need for further confirmatory tests. Another advantage is that a vascular thrombus can be detected and characterized on DCE-MRI, and this is crucial for HCC diagnosis and management.
Performance
Studies on the performance of DCE-AMRI are relatively scarce, and no previous study has evaluated the performance of ECCM-enhanced DCE-AMRI in a surveillance setting. Since 2017, only two retrospective studies [70,71] have explored the value of ECCM-enhanced DCE-AMRI in detecting HCC in a diagnostic setting. Lee et al. [70] evaluated the differences of LI-RADS categorization between DCE-AMRI and complete MRI, and detected only 5% of changes in LI-RADS categorization. This study did not evaluate the diagnostic performance of DCE-AMRI. Khatri et al. [71] reported a per-patient sensitivity of 92.1%, and specificity of 88.6% for DCE-AMRI conducted in a diagnostic setting. In this study, the HCC prevalence was 32.6%. Thus, the performance of DCE-AMRI using ECCM in a surveillance population should be further validated prospectively.
Two retrospective studies have investigated gadoxetic acid-enhanced DCE-AMRI [17,46]. One study was conducted in a surveillance setting [17] using simulated DCE-AMRI, including T1 DCE images (washout was evaluated only on portal venous phase images), DWI, and T2WI, without HBP images (Table 3), and reported a sensitivity of 84.6% and a specificity of 99.8%. However, it is unclear whether the MRI protocol used in this study could be regarded as a “true abbreviated” MRI, as only the HBP sequence was omitted from the complete MRI protocol, and therefore, the scan time would be similar to a complete ECCM-enhanced MRI. The other retrospective study was in a diagnostic setting [46] and reported the performance of gadoxetic acid-enhanced DCE-AMRI, with a sensitivity of 90.3% and a specificity of 100.0%.
Reporting
As all major features and a subset of ancillary features can be evaluated with DCE-AMRI, LI-RADS could be adopted for the standardized reporting of DCE-AMRI (Fig. 4). The two aforementioned ECCM contrast-enhanced DCE-AMRI studies [70,71] also used the LI-RADS. Considering that the imaging features evaluable using DCE-AMRI are the same as those of dynamic CT, the interpretation and reporting of DCE-AMRI could also adopt those for dynamic CT, such as CT LI-RADS [45], without major modification. As such, LR-4, LR-5, LR-TIV, and LR-M lesions detected on DCE-AMRI may be considered positive findings (Table 4). The reporting system of DCE-AMRI warrants further refinement and standardization. The imaging quality of arterial phase imaging, with considerations to artifacts or timing, should also be reported (Table 5).
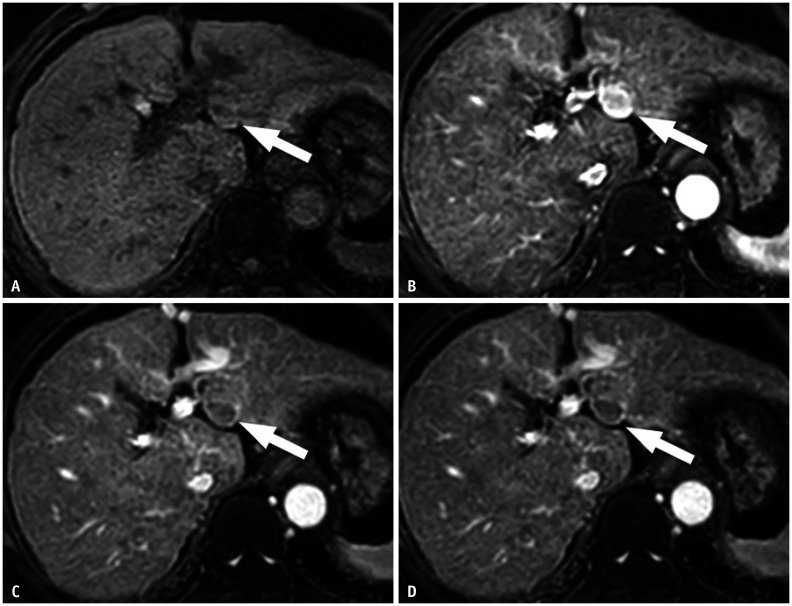
Fig. 4. Positive dynamic contrast-enhanced abbreviated MRI examination.
A-D. In a 77-year-old female with liver cirrhosis who underwent extracellular contrast media-enhanced liver MRI, non-enhanced T1-weighted image (A) and arterial phase image (B) demonstrate a 2-cm observation demonstrating arterial phase hyperenhancement in liver segment III (arrows). Portal venous phase image (C) and delayed phase image (D) show washout appearance of the observation (arrows), meeting the criteria for LR-5. Note the enhancing capsule of the observation.
Recall Tests
The callback strategy or follow-up recommendations for observation(s) detected by DCE-AMRI has not been clearly investigated. DCE-AMRI can demonstrate the major features of HCC as defined by LI-RADS [45]. If the lesion fulfills the LR-5 criteria on DCE-AMRI, no further confirmatory test is required. For LR-TIV and LR-M observations found on DCE-AMRI, additional dynamic CT or complete MRI may be unnecessary because no further change of the LI-RADS category can be made [45]. Further management for these lesions should be tailored through multidisciplinary discussion for individual patients, considering comorbidities or preferences (Table 4) [45,72]. For lesions of LI-RADS category 4, further MRI tests, including sequences other than DCE MRI, will likely be needed. If LR-3 or LR-4 observations are detected on DCE-AMRI, further management may differ according to different treatment practice patterns [7,73]. In countries that prioritize sensitivity over specificity, a second-look HBP-AMRI or NE-AMRI as a component of a sequential examination may be recommended [74]. For observations smaller than 10 mm, HBP MRI is a better choice as a second-look MRI [74]. However, if specificity is preferred to sensitivity, further management can follow the LI-RADS recommendation (Table 4, Fig. 3).
Issues
On DCE-AMRI, the acquisition of optimal arterial phase imaging is essential as lesion characterization primarily relies on the presence of APHE. Consequently, the relatively narrow time window of optimal arterial phase imaging may be a unique challenge to DCE-AMRI. Additionally, owing to the lack of additional sequences, such as DWI and T2WI, ancillary features favoring HCC or malignancy are not evaluable on DCE-AMRI [45]. Furthermore, similar to HBP-AMRI, DCE-AMRI is not without gadolinium-related issues.
We are skeptical about the use of gadoxetic acid for DCE-AMRI. The major strength of gadoxetic acid is to maximize sensitivity in HBP imaging with high liver-to-lesion contrast. Obtaining only dynamic contrast-enhanced sequences while omitting HBP images would decrease the diagnostic performance of MRI using gadoxetic acid [75,76]. Drawbacks in the arterial phase of gadoxetic acid-enhanced MRI would further mitigate its performance in HCC detection [58,59,60,61,62].
NE-AMRI
Details of Sequences
NE-AMRI consists of DWI and T2WI, with optional T1-weighted in/opposed imaging. NE-AMRI is the simplest strategy of the three AMRI options. Recent studies have reported that the simulated scan time of NE-AMRI comprising DWI and T2WI was less than 14 minutes, including set-up time [27]. Moreover, contrary to the contrast-enhanced AMRI protocols, NE-AMRI is free from gadolinium-related costs and concerns.
DWI is excellent in detecting HCC [24,25,26,27,28]. Sutherland et al. [77] prospectively evaluated a DWI-only strategy for HCC surveillance, which showed sensitivity and specificity of 83% and 98%, respectively. Most previous studies that evaluated NE-AMRI for HCC surveillance used a free-breathing or respiratory-triggered DWI sequence with three b-values, ranging from 0 to 800 s/mm2 (Table 3). The optimal number and range of b-values for NE-AMRI have not yet been determined. Unlike HBP-AMRI, in which both HBP imaging and DWI can sensitively detect lesions, in NE-AMRI, only DWI plays a major role in lesion detection. Therefore, care must be taken to achieve good image quality when designing the DWI pulse sequence.
T2WI enables lesion detection as well as characterization. The primary role of T2WI in HBP-AMRI is to increase the specificity by excluding common benign lesions rather than lesion detection per se. In contrast, in NE-AMRI, the role of T2WI for lesion detection is increased given the lack of back-up from HBP images. Therefore, moderately T2WI sequences seem to be more suitable than heavily T2WI sequences for NE-AMRI surveillance, as the lesion conspicuity and signal-to-noise ratio are better in moderately T2WI sequences [78,79], although there is a paucity of published results at present (Table 3). The scan and set-up time of NE-AMRI is shorter than in other AMRI strategies. Together with the evolving image techniques, including deep learning, it may be possible to obtain both heavily and moderately T2WI sequences without a significant increase in scan time. Further investigations are required to design and validate the optimal T2 pulse sequence for NE-AMRI.
T1-weighted dual-echo imaging can be obtained in a single breath-hold using most current MRI systems, and is acceptable to be included in the NE-AMRI protocol considering time. According to the LI-RADS [45], T1-weighted dual-echo imaging enables the assessment of intralesional fat, an ancillary feature favoring HCC in particular. However, not all fat-containing lesions are HCCs. Dysplastic nodules can also contain fat [80].
Performance
NE-AMRI has also shown acceptable performance for HCC surveillance. Recently, one clinical trial (MAGNUS-HCC, NCT02551250) evaluated the diagnostic performance of the annual NE-AMRI (T2WI, DWI, and T1-weighted in/opposed images) for HCC surveillance in patients with liver cirrhosis compared to that of biannual US [81]. In this study, the per-patient sensitivity of NE-AMRI was 71.0%, and the positive predictive value (PPV) was 61.1%, which are both higher than those of US (sensitivity, 45.2%; PPV, 33.3%). Additionally, the false referral rate of NE-AMRI was 2.7%. Another clinical trial evaluating NE-AMRI for HCC surveillance in patients with liver cirrhosis (MIRACLE-HCC, NCT02514434) is ongoing.
Four retrospective studies [17,27,77,82] have evaluated the performance of NE-AMRI in a surveillance setting, and the sensitivity and specificity ranged from 61.5% to 100% and 95.5% to 100%, respectively. One study [27] comparing NE-AMRI (T2WI and DWI) and US in a surveillance setting showed a significantly higher per-exam sensitivity (79.1% vs. 27.9%) and specificity (97.9% vs. 94.5%) for NE-AMRI than US.
Reporting
NE-AMRI for HCC surveillance can be interpreted as “negative”, “subthreshold”, or “positive” for suspected observations. “Positive” is defined by the presence of an observed lesion ≥ 10 mm, showing either diffusion restriction or mild-to-moderate T2 hyperintensity (Table 4, Fig. 5) [17,27,82]. The image quality of DWI should be reported with consideration to artifacts (Table 5).
Fig. 5. Positive non-enhanced abbreviated MRI examination.
A, B. A 65-year-old male with hepatitis B-associated cirrhosis. Diffusion-weighted imaging image (A, b-value = 500 s/mm2) and T2-weighted imaging (B) both demonstrate a 1.5-cm hyperintense nodule in the right hepatic lobe (arrows). This patient underwent partial hepatectomy after 3 months, and this observation was confirmed as a very early stage hepatocellular carcinoma.
Recall Tests
Confirmatory tests are required for all “positive” NE-AMRI studies. Either dynamic CT or complete MRI (using either gadoxetic acid or ECCM) can be used for recall testing. When MRI is used, DWI and T2WI are not necessarily repeated, and only pre- and post-contrast enhanced T1-weighted sequences need to be added (Table 4).
Issues
First, the relatively low sensitivity of NE-AMRI should be noted. Whereas the sensitivity of HBP-AMRI ranges from 80.8% to 92.0%, the sensitivity of NE-AMRI ranges from 61.5% to 100%. In Vietti Violi et al. [17], which reported the diagnostic performance of both simulated HBP-AMRI (HBP imaging, DWI, and T2WI) and NE-AMRI (DWI and T2WI), the sensitivity of HBP-AMRI was 80.8%, while that of NE-AMRI was 61.5%. suggesting the incremental value of HBP imaging on AMRI for increasing sensitivity. However, in the same study, the specificity of NE-AMRI (95.5%) was slightly higher than that of HBP-AMRI (94.9%), which is consistent with the overall trend of the two strategies (specificity of HBP-AMRI ranged from 91.0% to 95.6%, while that of NE-AMRI was higher, ranging from 95.5% to 100.0%). Second, NE-AMRI greatly depends on DWI for lesion detection, which is vulnerable to artifacts such as susceptibility artifacts. Therefore, the presence of artifacts in DWI would reduce its sensitivity to detect liver lesions and this should be clearly reported when reporting image quality so that a second-look exam or changing to another surveillance method may be considered. Third, a recall test is always required when the NE-AMRI is positive. Fourth, like in HBP-AMRI, NE-AMRI has limited sensitivity to detect and characterize tumor thrombus. Regarding the gadolinium-related issues, the relative benefit and harm of each strategy should be explored through a cost-effectiveness study.
Patient Selection for AMRI Surveillance Programs
Given the relatively limited availability of MRI and the higher costs compared to US, AMRI-based HCC surveillance should be tailored toward those who can benefit most from AMRI, rather than applying it uniformly to all target populations for HCC surveillance. Considering the initial rationale, AMRI-based HCC surveillance may be beneficial for populations whose US examinations are likely to generate inadequate quality. The sonic window and quality of US are particularly impaired in patients with liver cirrhosis, a major risk factor for HCC, due to the progressed distortion and heterogeneity of the hepatic parenchyma. Indeed, 20%–30% of US examinations in patients with liver cirrhosis are classified as inadequate for HCC surveillance [83,84]. The sensitivity of US is also lowered in patients with obesity or steatohepatitis, which are increasingly common in surveillance populations [84,85], as they result in limited sonic beam penetration. According to a recent study, the sensitivity of US was only 21% in patients with body mass index (BMI) ≥ 30 kg/m2 compared to 77% in those with BMI < 30 kg/m2 [86]. Accordingly, patients with advanced liver cirrhosis, obesity, or non-alcoholic steatohepatitis (NASH) are likely to benefit more from AMRI than US. Previous US examinations may help to predict the quality of subsequent US examinations. According to a recent study that evaluated three consecutive rounds of HCC surveillance, the image quality of US in the first round remained unchanged in the follow-up rounds in the vast majority of cases (83.3%–92.2%) [53].
Patients at high risk of developing HCC would likely benefit from AMRI-based surveillance. Most previous studies of AMRI-based HCC surveillance included patients at high risk for HCC such as liver cirrhosis, due to the higher incidence of HCC in these patients than the average surveillance populations [87,88]. In three Korean studies that evaluated the diagnostic performance of AMRI in prospective surveillance cohorts [27,53,81] using a prognostic model to assess the risk of developing HCC [89], only patients with liver cirrhosis and with an estimated annual HCC risk exceeding 5% were included. The resultant HCC prevalence of the three studies ranged from 11.3% to 19.3%. There is increasing evidence to support risk-stratified HCC surveillance strategies, i.e., to allocate more sensitive approaches to patients with higher risks [11,12,27,81,90,91].
Patient Preference and Adherence Issues
For the successful application of AMRI-based surveillance, both the diagnostic performance of AMRI and patients’ adherence to surveillance programs are paramount. Despite the proven efficacy of surveillance related to survival, many patients at risk of HCC do not undergo consistent surveillance [92,93,94,95]. According to a meta-analysis, the pooled adherence rate to HCC surveillance was only approximately 52% (95% confidence interval, 38%–66%) [95].
Notably, patient preference and values play an important role in adherence to surveillance programs [96]. According to a recent study by Woolen et al. [97], which surveyed patients at risk of HCC to elicit preferences for characteristics of HCC surveillance methods, participants strongly preferred AMRI (29.0%), complete MRI (23.3%), or novel blood-based biomarker testing (20.9%) to US alone (3.4%) or with AFP (8.8%). In the era of multiple HCC surveillance tools, patients must be provided with relevant and updated information, as well as the opportunity to align their preferences to surveillance tools. This, in turn, would facilitate higher patient adherence to surveillance programs, and ultimately, improve survival.
Cost-Effectiveness and Payment Issue
A cornerstone factor to consider in the successful application of AMRI for HCC surveillance should be the patient’s outcome over costs [98]. The key factors in determining the cost-effectiveness of cancer screening include test costs, diagnostic performances of the tests, the incidence of cancer, and treatment-enhanced survival [99,100,101]. There is increasing evidence to support the cost-effectiveness of risk-stratified HCC surveillance strategies using MRIs. According to Goossens et al. [90], applying AMRI to high- and intermediate-risk patients without screening low-risk patients had the lowest incremental cost-effective ratio of $2100 per quality-adjusted life-years. Kim et al. [91] opined that gadoxetic acid-enhanced MRI is a cost-effective surveillance option in high-risk patients with an annual incidence rate of 1.81% or higher. Contrastingly, in patients at a low or intermediate risk of HCC, US is the preferred strategy for HCC surveillance. Defining indications and target populations of AMRI-based HCC surveillance should be based on the cost-effectiveness analysis, which warrants further studies. With evolving MRI techniques including deep learning techniques, the time required for AMRI examination will decrease in the near future. This will further improve the cost-effectiveness of AMRI surveillance.
The payment for AMRI for HCC surveillance is an unresolved issue. Although the studies mentioned earlier have proposed a potential cost-effectiveness model for AMRI, refinement and standardization of the AMRI protocols across sites and the validation of its cost-effectiveness by multicenter clinical trials would be needed to secure reimbursement by health insurance for AMRI for HCC surveillance.
CONCLUSION
The introduction of AMRI has changed the landscape of HCC surveillance. AMRI reduces redundant MRI sequences by obtaining only a few essential sequences for detecting HCC such as HBP imaging, DWI, and T2WI. The three currently proposed AMRI protocols are HBP-AMRI, DCE-AMRI, and NE-AMRI. Each protocol has its unique benefits and drawbacks. All three AMRI techniques have shown excellent performance for detecting HCC, although evidence from prospective studies conducted in a true surveillance setting remains insufficient. Refining MRI sequences to achieve acceptable performance within a minimal timeframe is a prerequisite of an effective AMRI surveillance program. Updated MRI techniques such as SMS and deep learning techniques, are expected to propel the speed of AMRI examination and improve its time efficiency. AMRI should be reported in a standardized manner to guide recall tests explicitly and consistently. For this purpose, a modification of the US or CT LI-RADS seems to be a reasonable approach. AMRI-based HCC surveillance should be tailored toward those in whom US quality is inadequate, such as patients with severe liver cirrhosis, obesity, and NASH; those who underwent precedent US exams with unsatisfactory quality; and those who carry high rather than low or moderate risk of HCC. Patients generally prefer AMRI over other surveillance options. The patient’s preference may lead to better adherence to AMRI programs.
Footnotes
Conflicts of Interest: So Yeon Kim who is on the editorial board of the Korean Journal of Radiology was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
- Conceptualization: So Yeon Kim.
- Methodology: So Yeon Kim, Hyo Jung Park.
- Project administration: So Yeon Kim.
- Resources: So Yeon Kim, Nieun Seo.
- Supervision: So Yeon Kim.
- Validation: So Yeon Kim, Hyo Jung Park.
- Visualization: So Yeon Kim, Hyo Jung Park.
- Writing—original draft: Hyo Jung Park.
- Writing—review & editing: all authors.
Funding Statement: None
Availability of Data and Material
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
References
- 1.Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7:6. doi: 10.1038/s41572-020-00240-3. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Liver Cancer Collaboration. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the global burden of disease study 2015. JAMA Oncol. 2017;3:1683–1691. doi: 10.1001/jamaoncol.2017.3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petrick JL, Kelly SP, Altekruse SF, McGlynn KA, Rosenberg PS. Future of hepatocellular carcinoma incidence in the United States forecast through 2030. J Clin Oncol. 2016;34:1787–1794. doi: 10.1200/JCO.2015.64.7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417–422. doi: 10.1007/s00432-004-0552-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim DH, Choi SH, Shim JH, Kim SY, Lee SS, Byun JH, et al. Meta-analysis of the accuracy of abbreviated magnetic resonance imaging for hepatocellular carcinoma surveillance: non-contrast versus hepatobiliary phase-abbreviated magnetic resonance imaging. Cancers (Basel) 2021;13:2975. doi: 10.3390/cancers13122975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the study of liver diseases. Hepatology. 2018;68:723–750. doi: 10.1002/hep.29913. [DOI] [PubMed] [Google Scholar]
- 7.National Cancer Center (NCC); Korean Liver Cancer Association (KLCA) 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Korean J Radiol. 2019;20:1042–1113. doi: 10.3348/kjr.2019.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bolondi L. Screening for hepatocellular carcinoma in cirrhosis. J Hepatol. 2003;39:1076–1084. doi: 10.1016/s0168-8278(03)00349-0. [DOI] [PubMed] [Google Scholar]
- 9.Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MA, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30:37–47. doi: 10.1111/j.1365-2036.2009.04014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tzartzeva K, Obi J, Rich NE, Parikh ND, Marrero JA, Yopp A, et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: a meta-analysis. Gastroenterology. 2018;154:1706–1718.e1. doi: 10.1053/j.gastro.2018.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SY, An J, Lim YS, Han S, Lee JY, Byun JH, et al. MRI with liver-specific contrast for surveillance of patients with cirrhosis at high risk of hepatocellular carcinoma. JAMA Oncol. 2017;3:456–463. doi: 10.1001/jamaoncol.2016.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoon JH, Lee JM, Lee DH, Joo I, Jeon JH, Ahn SJ, et al. A comparison of biannual two-phase low-dose liver CT and US for HCC surveillance in a group at high risk of HCC development. Liver Cancer. 2020;9:503–517. doi: 10.1159/000506834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta P, Soundararajan R, Patel A, Kumar-M P, Sharma V, Kalra N. Abbreviated MRI for hepatocellular carcinoma screening: a systematic review and meta-analysis. J Hepatol. 2021;75:108–119. doi: 10.1016/j.jhep.2021.01.041. [DOI] [PubMed] [Google Scholar]
- 14.Chan MV, Huo YR, Trieu N, Mitchelle A, George J, He E, et al. Noncontrast MRI for hepatocellular carcinoma detection: a systematic review and meta-analysis–a potential surveillance tool? Clin Gastroenterol Hepatol. 2022;20:44–56.e2. doi: 10.1016/j.cgh.2021.02.036. [DOI] [PubMed] [Google Scholar]
- 15.Kim DH, Choi SH, Shim JH, Kim SY, Lee SS, Byun JH, et al. Magnetic resonance imaging for surveillance of hepatocellular carcinoma: a systematic review and meta-analysis. Diagnostics (Basel) 2021;11:1665. doi: 10.3390/diagnostics11091665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brunsing RL, Chen DH, Schlein A, Wolfson T, Gamst A, Mamidipalli A, et al. Gadoxetate-enhanced abbreviated MRI for hepatocellular carcinoma surveillance: preliminary experience. Radiol Imaging Cancer. 2019;1:e190010. doi: 10.1148/rycan.2019190010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vietti Violi N, Lewis S, Liao J, Hulkower M, Hernandez-Meza G, Smith K, et al. Gadoxetate-enhanced abbreviated MRI is highly accurate for hepatocellular carcinoma screening. Eur Radiol. 2020;30:6003–6013. doi: 10.1007/s00330-020-07014-1. [DOI] [PubMed] [Google Scholar]
- 18.An JY, Peña MA, Cunha GM, Booker MT, Taouli B, Yokoo T, et al. Abbreviated MRI for hepatocellular carcinoma screening and surveillance. Radiographics. 2020;40:1916–1931. doi: 10.1148/rg.2020200104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahn SS, Kim MJ, Lim JS, Hong HS, Chung YE, Choi JY. Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology. 2010;255:459–466. doi: 10.1148/radiol.10091388. [DOI] [PubMed] [Google Scholar]
- 20.Ueno A, Masugi Y, Yamazaki K, Komuta M, Effendi K, Tanami Y, et al. OATP1B3 expression is strongly associated with Wnt/β-catenin signalling and represents the transporter of gadoxetic acid in hepatocellular carcinoma. J Hepatol. 2014;61:1080–1087. doi: 10.1016/j.jhep.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Joo I, Kim SY, Kang TW, Kim YK, Park BJ, Lee YJ, et al. Radiologic-pathologic correlation of hepatobiliary phase hypointense nodules without arterial phase hyperenhancement at gadoxetic acid–enhanced MRI: a multicenter study. Radiology. 2020;296:335–345. doi: 10.1148/radiol.2020192275. [DOI] [PubMed] [Google Scholar]
- 22.Joo I, Lee JM, Lee DH, Jeon JH, Han JK, Choi BI. Noninvasive diagnosis of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: can hypointensity on the hepatobiliary phase be used as an alternative to washout? Eur Radiol. 2015;25:2859–2868. doi: 10.1007/s00330-015-3686-3. [DOI] [PubMed] [Google Scholar]
- 23.Kim TK, Lee E, Jang HJ. Imaging findings of mimickers of hepatocellular carcinoma. Clin Mol Hepatol. 2015;21:326–343. doi: 10.3350/cmh.2015.21.4.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim YK, Lee WJ, Park MJ, Kim SH, Rhim H, Choi D. Hypovascular hypointense nodules on hepatobiliary phase gadoxetic acid-enhanced MR images in patients with cirrhosis: potential of DW imaging in predicting progression to hypervascular HCC. Radiology. 2012;265:104–114. doi: 10.1148/radiol.12112649. [DOI] [PubMed] [Google Scholar]
- 25.Piana G, Trinquart L, Meskine N, Barrau V, Beers BV, Vilgrain V. New MR imaging criteria with a diffusion-weighted sequence for the diagnosis of hepatocellular carcinoma in chronic liver diseases. J Hepatol. 2011;55:126–132. doi: 10.1016/j.jhep.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 26.Vandecaveye V, De Keyzer F, Verslype C, Op de Beeck K, Komuta M, Topal B, et al. Diffusion-weighted MRI provides additional value to conventional dynamic contrast-enhanced MRI for detection of hepatocellular carcinoma. Eur Radiol. 2009;19:2456–2466. doi: 10.1007/s00330-009-1431-5. [DOI] [PubMed] [Google Scholar]
- 27.Park HJ, Jang HY, Kim SY, Lee SJ, Won HJ, Byun JH, et al. Non-enhanced magnetic resonance imaging as a surveillance tool for hepatocellular carcinoma: comparison with ultrasound. J Hepatol. 2020;72:718–724. doi: 10.1016/j.jhep.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 28.Kim HJ, Lee SS, Byun JH, Kim JC, Yu CS, Park SH, et al. Incremental value of liver MR imaging in patients with potentially curable colorectal hepatic metastasis detected at CT: a prospective comparison of diffusion-weighted imaging, gadoxetic acid-enhanced MR imaging, and a combination of both MR techniques. Radiology. 2015;274:712–722. doi: 10.1148/radiol.14140390. [DOI] [PubMed] [Google Scholar]
- 29.Taouli B, Koh DM. Diffusion-weighted MR imaging of the liver. Radiology. 2010;254:47–66. doi: 10.1148/radiol.09090021. [DOI] [PubMed] [Google Scholar]
- 30.Barth M, Breuer F, Koopmans PJ, Norris DG, Poser BA. Simultaneous multislice (SMS) imaging techniques. Magn Reson Med. 2016;75:63–81. doi: 10.1002/mrm.25897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taron J, Martirosian P, Erb M, Kuestner T, Schwenzer NF, Schmidt H, et al. Simultaneous multislice diffusion-weighted MRI of the liver: analysis of different breathing schemes in comparison to standard sequences. J Magn Reson Imaging. 2016;44:865–879. doi: 10.1002/jmri.25204. [DOI] [PubMed] [Google Scholar]
- 32.Obele CC, Glielmi C, Ream J, Doshi A, Campbell N, Zhang HC, et al. Simultaneous multislice accelerated free-breathing diffusion-weighted imaging of the liver at 3T. Abdom Imaging. 2015;40:2323–2330. doi: 10.1007/s00261-015-0447-3. [DOI] [PubMed] [Google Scholar]
- 33.Choi JY, Kim MJ, Chung YE, Kim JY, Jones AC, de Becker J, et al. Abdominal applications of 3.0-T MR imaging: comparative review versus a 1.5-T system. Radiographics. 2008;28:e30. doi: 10.1148/rg.e30. [DOI] [PubMed] [Google Scholar]
- 34.Semelka RC, Kelekis NL, Thomasson D, Brown MA, Laub GA. HASTE MR imaging: description of technique and preliminary results in the abdomen. J Magn Reson Imaging. 1996;6:698–699. doi: 10.1002/jmri.1880060420. [DOI] [PubMed] [Google Scholar]
- 35.Yu JS, Kim KW, Kim YH, Jeong EK, Chien D. Comparison of multishot turbo spin echo and HASTE sequences for T2-weighted MRI of liver lesions. J Magn Reson Imaging. 1998;8:1079–1084. doi: 10.1002/jmri.1880080512. [DOI] [PubMed] [Google Scholar]
- 36.Lee MJ, Kim MJ, Yoon CS, Song SY, Park K, Kim WS. The T2-shortening effect of gadolinium and the optimal conditions for maximizing the CNR for evaluating the biliary system: a phantom study. Korean J Radiol. 2011;12:358–364. doi: 10.3348/kjr.2011.12.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nakamura Y, Ohmoto T, Saito T, Kajima T, Nishimaru E, Ito K. Effects of gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid on T2-weighted MRCP. Magn Reson Med Sci. 2009;8:143–148. doi: 10.2463/mrms.8.143. [DOI] [PubMed] [Google Scholar]
- 38.Chung TK, Lee CH, Lee J, Choi JW, Kim KA, Park CM. Usefulness of postcontrast T2-weighted images in shortening the total scan time of a gadoxectic acid enhanced MRI of the liver: a comparison between precontrast and postcontrast T2-weighted images. J Korean Soc Radiol. 2010;62:249–256. [Google Scholar]
- 39.Ahn SJ, Kim MJ, Hong HS, Kim KA, Song HT. Distinguishing hemangiomas from malignant solid hepatic lesions: a comparison of heavily T2-weighted images obtained before and after administration of gadoxetic acid. J Magn Reson Imaging. 2011;34:310–317. doi: 10.1002/jmri.22658. [DOI] [PubMed] [Google Scholar]
- 40.Lee D, Lee J, Ko J, Yoon J, Ryu K, Nam Y. Deep learning in MR image processing. Investig Magn Reson Imaging. 2019;23:81–99. [Google Scholar]
- 41.Shanbhogue K, Tong A, Smereka P, Nickel D, Arberet S, Anthopolos R, et al. Accelerated single-shot T2-weighted fat-suppressed (FS) MRI of the liver with deep learning-based image reconstruction: qualitative and quantitative comparison of image quality with conventional T2-weighted FS sequence. Eur Radiol. 2021;31:8447–8457. doi: 10.1007/s00330-021-08008-3. [DOI] [PubMed] [Google Scholar]
- 42.Herrmann J, Gassenmaier S, Nickel D, Arberet S, Afat S, Lingg A, et al. Diagnostic confidence and feasibility of a deep learning accelerated HASTE sequence of the abdomen in a single breath-hold. Invest Radiol. 2021;56:313–319. doi: 10.1097/RLI.0000000000000743. [DOI] [PubMed] [Google Scholar]
- 43.Herrmann J, Nickel D, Mugler JP, 3rd, Arberet S, Gassenmaier S, Afat S, et al. Development and evaluation of deep learning-accelerated single-breath-hold abdominal HASTE at 3 T using variable refocusing flip angles. Invest Radiol. 2021;56:645–652. doi: 10.1097/RLI.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 44.Hu Z, Wang Y, Zhang Z, Zhang J, Zhang H, Guo C, et al. Distortion correction of single-shot EPI enabled by deep-learning. Neuroimage. 2020;221:117170. doi: 10.1016/j.neuroimage.2020.117170. [DOI] [PubMed] [Google Scholar]
- 45.American College of Radiology. CT/MRI LI-RADS® v2018 CORE. Web site. [Published 2018]. [Accessed November 7, 2021]. https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-2018-Core.pdf?la=en .
- 46.Besa C, Lewis S, Pandharipande PV, Chhatwal J, Kamath A, Cooper N, et al. Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdom Radiol (NY) 2017;42:179–190. doi: 10.1007/s00261-016-0841-5. [DOI] [PubMed] [Google Scholar]
- 47.Park SH, Kim B, Kim SY, Shim YS, Kim JH, Huh J, et al. Abbreviated MRI with optional multiphasic CT as an alternative to full-sequence MRI: LI-RADS validation in a HCC-screening cohort. Eur Radiol. 2020;30:2302–2311. doi: 10.1007/s00330-019-06546-5. [DOI] [PubMed] [Google Scholar]
- 48.Hernando D, Wells SA, Vigen KK, Reeder SB. Effect of hepatocyte-specific gadolinium-based contrast agents on hepatic fat-fraction and R2*. Magn Reson Imaging. 2015;33:43–50. doi: 10.1016/j.mri.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Koo NH, Choi KW, Yoo BG. Effect of Gd-EOB-DTPA on hepatic fat quantification using two-point Dixon technique. Journal of Korea Contents Association. 2017;17:215–221. [Google Scholar]
- 50.Park CC, Hamilton G, Desai A, Zand KA, Wolfson T, Hooker JC, et al. Effect of intravenous gadoxetate disodium and flip angle on hepatic proton density fat fraction estimation with six-echo, gradient-recalled-echo, magnitude-based MR imaging at 3T. Abdom Radiol (NY) 2017;42:1189–1198. doi: 10.1007/s00261-016-0992-4. [DOI] [PubMed] [Google Scholar]
- 51.Marks RM, Ryan A, Heba ER, Tang A, Wolfson TJ, Gamst AC, et al. Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid-enhanced MRI for hepatocellular carcinoma surveillance. AJR Am J Roentgenol. 2015;204:527–535. doi: 10.2214/AJR.14.12986. [DOI] [PubMed] [Google Scholar]
- 52.Tillman BG, Gorman JD, Hru JM, Lee MH, King MC, Sirlin CB, et al. Diagnostic per-lesion performance of a simulated gadoxetate disodium-enhanced abbreviated MRI protocol for hepatocellular carcinoma screening. Clin Radiol. 2018;73:485–493. doi: 10.1016/j.crad.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 53.Park HJ, Kim SY, Singal AG, Lee SJ, Won HJ, Byun JH, et al. Abbreviated magnetic resonance imaging vs ultrasound for surveillance of hepatocellular carcinoma in high-risk patients. Liver Int. 2021 Nov; doi: 10.1111/liv.15110. [Epub] [DOI] [PubMed] [Google Scholar]
- 54.Whang S, Choi MH, Choi JI, Youn SY, Kim DH, Rha SE. Comparison of diagnostic performance of non-contrast MRI and abbreviated MRI using gadoxetic acid in initially diagnosed hepatocellular carcinoma patients: a simulation study of surveillance for hepatocellular carcinomas. Eur Radiol. 2020;30:4150–4163. doi: 10.1007/s00330-020-06754-4. [DOI] [PubMed] [Google Scholar]
- 55.American College of Radiology. Ultrasound LI-RADS® v2017. Web site. [Accessed November 11, 2021]. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/Ultrasound-LI-RADS-v2017 .
- 56.Kim JY, Lee SS, Byun JH, Kim SY, Park SH, Shin YM, et al. Biologic factors affecting HCC conspicuity in hepatobiliary phase imaging with liver-specific contrast agents. AJR Am J Roentgenol. 2013;201:322–331. doi: 10.2214/AJR.12.9478. [DOI] [PubMed] [Google Scholar]
- 57.Kim SY, Wu EH, Park SH, Wang ZJ, Hope TA, Yee J, et al. Comparison of hepatocellular carcinoma conspicuity on hepatobiliary phase images with gadoxetate disodium vs. delayed phase images with extracellular cellular contrast agent. Abdom Radiol (NY) 2016;41:1522–1531. doi: 10.1007/s00261-016-0703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brismar TB, Dahlstrom N, Edsborg N, Persson A, Smedby O, Albiin N. Liver vessel enhancement by Gd-BOPTA and Gd-EOB-DTPA: a comparison in healthy volunteers. Acta Radiol. 2009;50:709–715. doi: 10.1080/02841850903055603. [DOI] [PubMed] [Google Scholar]
- 59.Tamada T, Ito K, Sone T, Yamamoto A, Yoshida K, Kakuba K, et al. Dynamic contrast-enhanced magnetic resonance imaging of abdominal solid organ and major vessel: comparison of enhancement effect between Gd-EOB-DTPA and Gd-DTPA. J Magn Reson Imaging. 2009;29:636–640. doi: 10.1002/jmri.21689. [DOI] [PubMed] [Google Scholar]
- 60.Davenport MS, Viglianti BL, Al-Hawary MM, Caoili EM, Kaza RK, Liu PS, et al. Comparison of acute transient dyspnea after intravenous administration of gadoxetate disodium and gadobenate dimeglumine: effect on arterial phase image quality. Radiology. 2013;266:452–461. doi: 10.1148/radiol.12120826. [DOI] [PubMed] [Google Scholar]
- 61.Kim DW, Choi SH, Park T, Kim SY, Lee SS, Byun JH. Transient severe motion artifact on arterial phase in gadoxetic acid-enhanced liver magnetic resonance imaging: a systematic review and meta-analysis. Invest Radiol. 2022;57:62–70. doi: 10.1097/RLI.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 62.Huh J, Kim SY, Yeh BM, Lee SS, Kim KW, Wu EH, et al. Troubleshooting arterial-phase MR images of gadoxetate disodium-enhanced liver. Korean J Radiol. 2015;16:1207–1215. doi: 10.3348/kjr.2015.16.6.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Petrasek J, Singal AG, Rich NE. Harms of hepatocellular carcinoma surveillance. Curr Hepatol Rep. 2019;18:383–389. doi: 10.1007/s11901-019-00488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Takizawa D, Kakizaki S, Sohara N, Sato K, Takagi H, Arai H, et al. Hepatocellular carcinoma with portal vein tumor thrombosis: clinical characteristics, prognosis, and patient survival analysis. Dig Dis Sci. 2007;52:3290–3295. doi: 10.1007/s10620-007-9808-2. [DOI] [PubMed] [Google Scholar]
- 65.Bae JS, Lee JM, Yoon JH, Jang S, Chung JW, Lee KB, et al. How to best detect portal vein tumor thrombosis in patients with hepatocellular carcinoma meeting the Milan criteria: gadoxetic acid-enhanced MRI versus contrast-enhanced CT. Liver Cancer. 2020;9:293–307. doi: 10.1159/000505191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ahn JH, Yu JS, Cho ES, Chung JJ, Kim JH, Kim KW. Diffusion-weighted MRI of malignant versus benign portal vein thrombosis. Korean J Radiol. 2016;17:533–540. doi: 10.3348/kjr.2016.17.4.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sandrasegaran K, Tahir B, Nutakki K, Akisik FM, Bodanapally U, Tann M, et al. Usefulness of conventional MRI sequences and diffusion-weighted imaging in differentiating malignant from benign portal vein thrombus in cirrhotic patients. AJR Am J Roentgenol. 2013;201:1211–1219. doi: 10.2214/AJR.12.10171. [DOI] [PubMed] [Google Scholar]
- 68.Rogosnitzky M, Branch S. Gadolinium-based contrast agent toxicity: a review of known and proposed mechanisms. Biometals. 2016;29:365–376. doi: 10.1007/s10534-016-9931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Levine D, McDonald RJ, Kressel HY. Gadolinium retention after contrast-enhanced MRI. JAMA. 2018;320:1853–1854. doi: 10.1001/jama.2018.13362. [DOI] [PubMed] [Google Scholar]
- 70.Lee JY, Huo EJ, Weinstein S, Santos C, Monto A, Corvera CU, et al. Evaluation of an abbreviated screening MRI protocol for patients at risk for hepatocellular carcinoma. Abdom Radiol (NY) 2018;43:1627–1633. doi: 10.1007/s00261-017-1339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Khatri G, Pedrosa I, Ananthakrishnan L, de Leon AD, Fetzer DT, Leyendecker J, et al. Abbreviated-protocol screening MRI vs. complete-protocol diagnostic MRI for detection of hepatocellular carcinoma in patients with cirrhosis: an equivalence study using LI-RADS v2018. J Magn Reson Imaging. 2020;51:415–425. doi: 10.1002/jmri.26835. [DOI] [PubMed] [Google Scholar]
- 72.Chernyak V, Fowler KJ, Kamaya A, Kielar AZ, Elsayes KM, Bashir MR, et al. Liver imaging reporting and data system (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology. 2018;289:816–830. doi: 10.1148/radiol.2018181494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang JD. Detect or not to detect very early stage hepatocellular carcinoma? The western perspective. Clin Mol Hepatol. 2019;25:335–343. doi: 10.3350/cmh.2019.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Park SH, Kim B, Kim SY, Choi SJ, Huh J, Kim HJ, et al. Characterizing computed tomography-detected arterial hyperenhancing-only lesions in patients at risk of hepatocellular carcinoma: can non-contrast magnetic resonance imaging be used for sequential imaging? Korean J Radiol. 2020;21:280–289. doi: 10.3348/kjr.2019.0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paisant A, Vilgrain V, Riou J, Oberti F, Sutter O, Laurent V, et al. Comparison of extracellular and hepatobiliary MR contrast agents for the diagnosis of small HCCs. J Hepatol. 2020;72:937–945. doi: 10.1016/j.jhep.2019.12.011. [DOI] [PubMed] [Google Scholar]
- 76.Min JH, Kim JM, Kim YK, Kang TW, Lee SJ, Choi GS, et al. Prospective intraindividual comparison of magnetic resonance imaging with gadoxetic acid and extracellular contrast for diagnosis of hepatocellular carcinomas using the liver imaging reporting and data system. Hepatology. 2018;68:2254–2266. doi: 10.1002/hep.30122. [DOI] [PubMed] [Google Scholar]
- 77.Sutherland T, Watts J, Ryan M, Galvin A, Temple F, Vuong J, et al. Diffusion-weighted MRI for hepatocellular carcinoma screening in chronic liver disease: direct comparison with ultrasound screening. J Med Imaging Radiat Oncol. 2017;61:34–39. doi: 10.1111/1754-9485.12513. [DOI] [PubMed] [Google Scholar]
- 78.Coates GG, Borrello JA, McFarland EG, Mirowitz SA, Brown JJ. Hepatic T2-weighted MRI: a prospective comparison of sequences, including breath-hold, half-Fourier turbo spin echo (HASTE) J Magn Reson Imaging. 1998;8:642–649. doi: 10.1002/jmri.1880080319. [DOI] [PubMed] [Google Scholar]
- 79.Schwartz LH, Seltzer SE, Tempany CM, Silverman SG, Piwnica-Worms DR, Adams DF, et al. Prospective comparison of T2-weighted fast spin-echo, with and without fat suppression, and conventional spin-echo pulse sequences in the upper abdomen. Radiology. 1993;189:411–416. doi: 10.1148/radiology.189.2.8210368. [DOI] [PubMed] [Google Scholar]
- 80.Hanna RF, Aguirre DA, Kased N, Emery SC, Peterson MR, Sirlin CB. Cirrhosis-associated hepatocellular nodules: correlation of histopathologic and MR imaging features. Radiographics. 2008;28:747–769. doi: 10.1148/rg.283055108. [DOI] [PubMed] [Google Scholar]
- 81.Choi MH, Choi JI, Yoon JH, Lee CH, Kang TW, Kim HA, et al. Annual non-contrast liver MRI versus biannual liver ultrasonography for surveillance of HCC in patients with liver cirrhosis (MAGNUS-HCC): results of a prospective, multicenter trial; Proceedings of the 76th Annual Meeting of the Korean Congress of Radiology; 2020 Sep 19; Seoul, Korea. Korean Society of Radiology; p. 204. [Google Scholar]
- 82.Ahmed NNA, El Gaafary SM, Elia RZ, Abdulhafiz EM. Role of abbreviated MRI protocol for screening of HCC in HCV related cirrhotic patients prior to direct-acting antiviral treatmen. Egypt J Radiol Nucl Med. 2020;51:102 [Google Scholar]
- 83.Son JH, Choi SH, Kim SY, Jang HY, Byun JH, Won HJ, et al. Validation of US liver imaging reporting and data system version 2017 in patients at high risk for hepatocellular carcinoma. Radiology. 2019;292:390–397. doi: 10.1148/radiol.2019190035. [DOI] [PubMed] [Google Scholar]
- 84.Simmons O, Fetzer DT, Yokoo T, Marrero JA, Yopp A, Kono Y, et al. Predictors of adequate ultrasound quality for hepatocellular carcinoma surveillance in patients with cirrhosis. Aliment Pharmacol Ther. 2017;45:169–177. doi: 10.1111/apt.13841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wong LL, Reyes RJ, Kwee SA, Hernandez BY, Kalathil SC, Tsai NC. Pitfalls in surveillance for hepatocellular carcinoma: how successful is it in the real world? Clin Mol Hepatol. 2017;23:239–248. doi: 10.3350/cmh.2017.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Esfeh JM, Hajifathalian K, Ansari-Gilani K. Sensitivity of ultrasound in detecting hepatocellular carcinoma in obese patients compared to explant pathology as the gold standard. Clin Mol Hepatol. 2020;26:54–59. doi: 10.3350/cmh.2019.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fattovich G. Natural history and prognosis of hepatitis B. Semin Liver Dis. 2003;23:47–58. doi: 10.1055/s-2003-37590. [DOI] [PubMed] [Google Scholar]
- 88.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 89.Velázquez RF, Rodríguez M, Navascués CA, Linares A, Pérez R, Sotorríos NG, et al. Prospective analysis of risk factors for hepatocellular carcinoma in patients with liver cirrhosis. Hepatology. 2003;37:520–527. doi: 10.1053/jhep.2003.50093. [DOI] [PubMed] [Google Scholar]
- 90.Goossens N, Singal AG, King LY, Andersson KL, Fuchs BC, Besa C, et al. Cost-effectiveness of risk score–stratified hepatocellular carcinoma screening in patients with cirrhosis. Clin Transl Gastroenterol. 2017;8:e101. doi: 10.1038/ctg.2017.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim HL, An J, Park JA, Park SH, Lim YS, Lee EK. Magnetic resonance imaging is cost-effective for hepatocellular carcinoma surveillance in high-risk patients with cirrhosis. Hepatology. 2019;69:1599–1613. doi: 10.1002/hep.30330. [DOI] [PubMed] [Google Scholar]
- 92.Singal AG, Yopp AC, Gupta S, Skinner CS, Halm EA, Okolo E, et al. Failure rates in the hepatocellular carcinoma surveillance process. Cancer Prev Res (Phila) 2012;5:1124–1130. doi: 10.1158/1940-6207.CAPR-12-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Davila JA, Morgan RO, Richardson PA, Du XL, McGlynn KA, El-Serag HB. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology. 2010;52:132–141. doi: 10.1002/hep.23615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Edenvik P, Davidsdottir L, Oksanen A, Isaksson B, Hultcrantz R, Stål P. Application of hepatocellular carcinoma surveillance in a European setting. What can we learn from clinical practice? Liver Int. 2015;35:1862–1871. doi: 10.1111/liv.12764. [DOI] [PubMed] [Google Scholar]
- 95.Zhao C, Jin M, Le RH, Le MH, Chen VL, Jin M, et al. Poor adherence to hepatocellular carcinoma surveillance: a systematic review and meta-analysis of a complex issue. Liver Int. 2018;38:503–514. doi: 10.1111/liv.13555. [DOI] [PubMed] [Google Scholar]
- 96.Singal AG, Volk ML, Rakoski MO, Fu S, Su GL, McCurdy H, et al. Patient involvement in healthcare is associated with higher rates of surveillance for hepatocellular carcinoma. J Clin Gastroenterol. 2011;45:727–732. doi: 10.1097/MCG.0b013e31820989d3. [DOI] [PubMed] [Google Scholar]
- 97.Woolen SA, Singal AG, Davenport MS, Troost JP, Khalatbari S, Mittal S, et al. Patient preferences for hepatocellular carcinoma surveillance parameters. Clin Gastroenterol Hepatol. 2022;20:204–215.e6. doi: 10.1016/j.cgh.2021.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.European Society of Radiology (ESR) ESR concept paper on value-based radiology. Insights Imaging. 2017;8:447–454. doi: 10.1007/s13244-017-0566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Arguedas MR, Chen VK, Eloubeidi MA, Fallon MB. Screening for hepatocellular carcinoma in patients with hepatitis C cirrhosis: a cost-utility analysis. Am J Gastroenterol. 2003;98:679–690. doi: 10.1111/j.1572-0241.2003.07327.x. [DOI] [PubMed] [Google Scholar]
- 100.Cucchetti A, Trevisani F, Cescon M, Ercolani G, Farinati F, Poggio PD, et al. Cost-effectiveness of semi-annual surveillance for hepatocellular carcinoma in cirrhotic patients of the Italian liver cancer population. J Hepatol. 2012;56:1089–1096. doi: 10.1016/j.jhep.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 101.Ruggeri M. Hepatocellular carcinoma: cost-effectiveness of screening. A systematic review. Risk Manag Healthc Policy. 2012;5:49–54. doi: 10.2147/RMHP.S18677. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.