Abstract
Objective
To assess the level of caregiver burden and factors associated with it among family caregivers of persons with dementia (PWD) living in communities of Shanghai, China.
Design
Cross-sectional study.
Setting
Communities in Hongkou District of Shanghai, China.
Participants
A random sample of 109 older adults with dementia and their primary family caregivers.
Main outcome measure
Caregiver burden measured by the Caregiver Burden Inventory (CBI), and the Caregivers’ depressive symptom measured by the simplified Chinese version of Self-rating Depression Scale was the outcome variable of the study. The independent variables, including the cognitive function (measured by Montreal Cognitive Assessment (MoCA), sleep quality assessed by the Pittsburgh Sleep Quality Index, abilities of daily life assessed by the Activities of Daily Living Scale, and behavioural and psychological symptoms assessed by the Neuropsychiatric Inventory of PWDs, the community service utilisation (measured by the Community Service Utilisation Measurement), perceived social support (assessed by three questions), positive aspects of caregiving (PAC) (assessed by the PAC) of dementia caregivers, were analysed. Multivariate linear regression was employed to determine the factors related to caregiver burden.
Results
The average level of CBI was 65.92±16.74. The score of MoCA, PAC and perceived social support of caregivers were negatively associated with caregiver burden (β=−0.84, p<0.001, β=−3.61, p=0.03 and β=−1.22, p=0.001, respectively). Community service utilisation was positively associated (β=3.46, p<0.001) with caregiver burden. Perceived social support by the caregiver moderated the relationship between caregiver burden and caregivers’ depression symptoms.
Conclusion
Dementia caregivers experienced a high level of caregiver burden. The cognitive function of PWD, PAC, social support and community service utilisation were factors associated with caregiver burden. Strengthening social support, providing more high-quality home care services, promoting PAC are imperative to reduce caregiver burden.
Keywords: Dementia, Adult intensive & critical care, Health policy
Strengths and limitations of this study.
The study was conducted in Shanghai, which is the most ageing city in China.
The participants were randomly sampled from a convenient sample of 8800 older adults in seven different communities.
We explored the association between factors of persons with dementia as well as their family caregivers and caregiver burden.
We cannot generalise the conclusion of this study to the whole country since the socioeconomic status, healthcare services and culture vary between different regions of China.
A longitudinal study with larger sample size is needed to explore the linkage between caregiver burden and influencing factors.
Introduction
With the advancement of society, the prevalence of the ageing population has increased. With the increasing age, numerous underlying physiological changes occur, and the risk of the chronic disease rises.1 Dementia is one of the predominant diseases occurring in the ageing population. The age-standardised prevalence of dementia in older adults (age ≥60 years) varies from 5% to 7% in most regions worldwide.2 According to the global population report in 2017, there were nearly 25% of older adults in China and their number is expected to increase to 478.8 million (35.1%) in 2050, according to the Department of Economic and Social Affairs of the United Nations.3 The age-standardised prevalence of dementia in China is 6%. There are approximately 7.4 million persons with dementia (PWDs) in China. The number is expected to reach 18 million by 2030 if effective measures are not undertaken.4
Dementia is characterrised by the deterioration of intellectual functions, executive dysfunction, sleeping disorders, emotional problem, and behavioural and psychological symptoms.5 PWD rely on their family caregivers’ support for daily activities. Family caregivers have to handle deteriorative function and progressive dementia-related symptoms of PWD, thereby increasing the burden. Dementia also has a financial impact on society. The estimated total annual cost of dementia in China is predicted to increase from US$0.9 billion in 1990 to US$114.2 billion in 2030. The costs of informal care accounted for 81.3% of the total estimated cost in 2010.6 Caregiver burden is defined as the extent to which caregivers perceive their emotional or physical health, social life and financial status due to caring for their relatives.7 Due to the negative consequences of dementia, caregiver burden is higher among them compared with the population without dementia.8 To reduce the dementia caregiver burden of PWDs, it is essential to identify factors that influence caregiver burden. Previous studies from Ireland, America, Korea and Spain have reported significant caregiver burden in family caregivers of PWD, and it was associated with age, the severity of dementia, duration of the illness, level of neuropsychiatric symptoms, frontal lobe dysfunction, antidepressant drugs and functional status of PWD.9–12 A cross-section study in Hong Kong revealed that the prevalence of caregiver burnout was 15.5%. Caregiver burnout was associated with PWDs’ activities of daily living (ADLs) dependence and history of falls in the previous 90 days. Factors such as primary caregivers being adult children and the utilisation of allied health services were found to be protective to caregiver burn-out.13 As the social services and healthcare systems are different between Hong Kong and mainland China, factors contributing to caregiver burden may also differ between the two settings. Studies on caregiver burden of dementia caregivers conducted in northern cities of China showed that the average score of caregiver burden measured by the Zarit Burden Interview was 12.2±13.2, which lies in the mild range. Moreover, caregiver burden was associated with the functional status of PWDs, physical status, life satisfaction, depression and anxiety of caregivers.14 The study conducted by Wang et al in central China showed that the mean score of caregiver burden measured by the caregiver burden inventory (CBI) was 44.56±10.18. Caregiver burden was associated with the risk of caregiver’s committed abuse. However, caregiver burden was not found to be associated with social support.15 Liu et al reported that severity of dementia, daily caregiving time, depressive symptom and anxiety of caregivers were associated with caregiver burden in Beijing.16 Abdollahpour et al reported that positive aspects of caregiving (PAC) was negatively associated with caregiver burden among 153 caregivers of people with Alzheimer’s disease (AD) after controlling for caregivers’ age, marriage and dependence of patients.17
Previous studies conducted in northern and central parts of China did not include key factors associated with caregiver burden, such as PAC, social support and community service utilisation. Shanghai, located in Eastern China, is one of the most developed and ageing cities in the country. However, studies about level of caregiver burden of PWD and related factors in Shanghai was limited. Data available for factors such as PAC, perceived social support and utilisation of community services associated with the level of caregiver burden was sparse. To address the knowledge gap, this study aimed to explore the level and factors associated with dementia caregivers’ burden in communities in Shanghai. We hypothesised that the factors associated with caregiver burden were cognitive function, sleep quality, ability of daily life, the behavioural and psychological symptoms of PWDs as well as community service utilisation, social support and PAC.
Psychological health deterioration is one of the consequences of caregiver burden.18 Caregivers experience psychological issues like depression and anxiety after caring for PWDs for a long period of time.14 Social support refers to an individual or a collective resource that can provide emotional and mental assistance.19 The study conducted by Cohen and Thoits proposed and verified the buffering hypothesis and confirmed that social support was a buffer against life stress and protects physical and mental health.20 21 As for dementia caregivers, the antecedents of caregiver burden consist of insufficient financial resources, multiple responsibilities and lack of social activities.18 Adequate social support from family and community can release stress and burden of caregivers and allow them to participate in social activities. A cross-sectional study among people with AD in Taiyuan North China showed that social support was the moderating variable in the relationship between the cognitive function of people with AD and caregiver burden. It can be seen that social support can buffer the negative aspects of caring for people with dementia.22 We proposed that with different levels of social support, the impact of caregiver burden on depressive symptom vary, the social support was the moderating variable in the relationship between caregiver burden and depressive symptoms.
In China, most PWDs live in communities and depend on their family members for caregiving. China’s pilot long-term care (LTC) insurance policy was implemented in 15 cities since 2016. However, the supply and demand of LTC services are unmatched and unbalanced.23 Formal care service is difficult to access at home. Support to family dementia caregivers is limited in most areas of China,24 which is insufficient to reduce the caregiver burden. Furthermore, the Chinese are influenced by Confucianism, which promotes the value of filial piety and family responsibility.25 Especially, in traditional Chinese culture, family secrets should be confined to family members and not be revealed to those outside the family.25 The cultural sense of caregiving obligation may be a barrier for caregivers to seek help outside of the household, which leads to a high level of caregiver burden.26 Therefore, we aimed to conduct this study to examine the level of dementia caregiving burden in Chinese communities and explore the factors related to caregiver burden. Besides, we also explored the relationship between social support, caregiver burden, and depression of caregivers. The results of the study may provide insight into the development of programmes and services to reduce caregiver burden.
Participants and methods
Participants
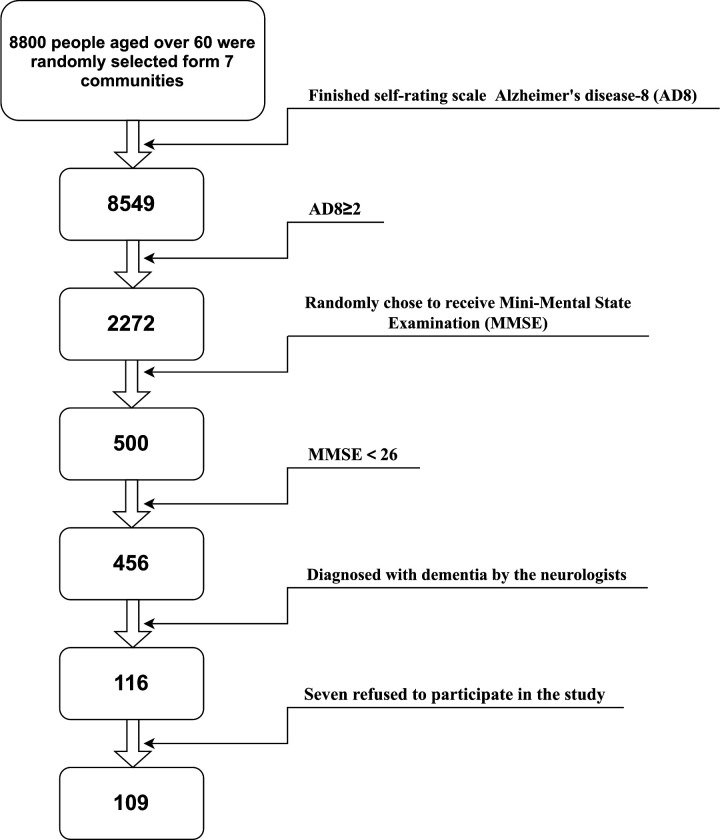
This was a cross-sectional study conducted from March 2017 to March 2018. A total of 8800 older adults were randomly selected from seven community healthcare centres in Hongkou District, Shanghai, China. The healthcare providers in these community centres screened the cognitive function of 8549 older adults using the measure of AD-8 (AD8), A score of 2+ was considered as cognitive impairment. A total of 2272 of the screened persons were designated as cognitively impaired out of which 500 persons were randomly selected using random seed generated by SAS. These selected individuals underwent further cognitive testing using the Mini-Mental State Examination (MMSE). A total of 456 older adults with cognitive impairment (MMSE <26) were identified, and they were invited along with their primary family caregivers to the Neurology Clinic of Changzheng Hospital for further comprehensive neuropsychological assessment by neurologists. The primary family caregivers were defined as unpaid family members who were primarily taking care of the older adults and were well aware of their condition and environment.27 A total of 116 older adults were diagnosed with dementia. All the PWDs met the NIA-AA criteria (2011) for probable AD, the NINDS-AIREN criteria for vascular dementia (VaD), the Gorno-Tempini criteria (2011) for frontotemporal dementia, and dementia with Lewy body (DLB) clinical diagnostic criteria(2005) for DLB, and underwent thorough clinical examinations, medical history taking and assessment of the physical, neurological and psychiatric status, including the Hamilton Anxiety Scale; psychological test; laboratory screening test; ECG; chest radiography; electroencephalography; MRI of the brain; neuropsychological assessment with the use of the MMSE; functional autonomy evaluation using ADL Scale. The exclusion criteria of PWDs included: (1) visual and auditory impairment (2) severe aphasia, (3) the acute stage of chronic disease, (4) unable to sit for more than 40 min, (5) the presence of other nervous system diseases. Seven dyads of PWDs and their family caregivers refused to participate in the study. A total of 109 dyads of PWDs and their primary family caregivers consented to participate in the study. The flow chart of the sampling is shown in figure 1.
Figure 1.
Flow chart of the sampling. Flow chart to identify how the participants were recruited in the study.
The power of the sample size was calculated by the G*power V.3.1; we chose linear multiple regression: fixed model, single regression coefficient. The effect size f2 was set as a large of 0.35,28 the number of predictors was 7, the results showed that the power of the sample was 99.81%, indicating a sound power of the test.
Patients and public involvement
Patients and the public were not involved in this study, including the recruitment, data collection, analysis, interpretation and dissemination of the results.
Variables
Outcome variable
The caregiver burden of the caregivers was measured by the CBI developed by Novak in 1989 to measure the caregiver burden of PWDs. CBI was widely used in disabled stroke patients, spinal cord injuries, chronic-acquired brain injury and neurological Wilson disease in the previous studies.29 CBI included 24 items, which were divided into five domains. Each item was evaluated from ‘never’ (0 points) to ‘always’ (4 points) 5 levels. The five domains were: time-dependence (items 1–5, with 20 points), developmental (items 6–10, with 20 points), physical (items 11–14, with 16 points), social (items 15–18, with 16 points) and emotional (items 19–24, with 24 points).29 The total score of CBI was 96. A higher score correlates with increased caregiver burden. Chou tested the reliability and validity of the Chinese version of CBI, which showed adequate internal consistency reliability, appropriate content validity and concurrent validity.30 The Cronbach’s α coefficients of the five domains ranged from 0.79 to 0.93. The Content of Validity Index of the Chinese version was 95.8%. The exploratory factor analysis showed that there were five common factors for the original scale. The accumulative variance contribution of the five common factors was 62.78%.30 The inventory was used to measure the caregiver burden of dementia caregivers in central China, with a Cronbach’s α coefficient of 0.92.15 The score of CBI>36 indicated the caregivers’ ‘risk of burning out’.31
Independent variables
Caregivers’ variables
The sociodemographic characteristics included age, gender, education, employment and relationship of caregiver with PWDs.
The caregivers’ depressive symptom was measured by the Self-rating Depression Scale developed by Zung to measure the level of depression of adults.32 We used a simplified Chinese version that includes 12 items.
The community service utilisation was measured by the Community Service Utilisation Measurement included 10 items: nursing assistant, housekeeper, doctor, psychologist, daycare centre, food delivered, ambulance, hospitalisation, nursing home and other services. Each item had two options: used or not. These items were developed according to the existing services in the communities of Shanghai.
Caregivers were asked to choose the community service they had used in the past 3 months. The measurement has been used in the previous study.33
Three questions measured social support perceived by caregivers: (1) How many people can be relied on when the situation is urgent; (2) How do people care about the current situations; (3) How easy it is to receive help from neighbours or colleagues when needed—total score ranges from 3 to 14, with higher scores indicating stronger social support. The measurement has been used in the previous study.33
The positive aspects of caregivers were measured by PAC. This scale was developed by Tarlow to evaluate the PAC in 2015 and was translated and tested by Lou., the PAC showed stable reliability and validity.34 The scale is a self-rating scale that includes nine items with two domains, namely self-affirmation and outlook on life. The items used a 5-point Likert-type scale. The higher score indicated more PAC. The content validity and structural validity of the scale were acceptable.34
Participants variables
The sociodemographic characteristics were age, gender and education. The disease characteristics included types of dementia (AD, VaD, frontotemporal dementia, mixed dementia and DLBs), cognitive function, subjective sleep quality, behavioural and psychological symptoms, and ADL.
The cognitive function of the PWDs was assessed by Montreal Cognitive Assessment (MoCA) developed by Nasreddine et al.35 It incorporates eight domains of cognitive function, including attention, executive function, memory, language, visuospatial skills, abstract thinking, calculation and orientation. MoCA score ranges from 0 to 30, with a lower score indicating poorer cognition. MoCA has been widely used in assessing cognitive function among patients with stroke, Parkinson’s disease and other diseases. It has stable sensitivity and specificity. MoCA has been translated into 30 different versions. Wang translated the MoCA-Beijing (BJ) version, and the assessment is available from www.mocatest.org. Chen tested the reliability and validity of the MoCA-BJ in people with obstructive sleep apnoea–hypopnea syndrome. The Cronbach’s α of the MoCA-BJ was 0.73.36
The sleep quality of the PWDs was assessed by the Pittsburgh Sleep Quality Index (PSQI) where the PWDs and their caregivers answered the index. PSQI was developed by Buysse in 1989 and was translated by Liu et al.37 The sensitivity and specificity of the Chinese version of PSQI were 98.3% and 90.3%, respectively.37 The PSQI is a self-report questionnaire that accesses seven dimensions of sleep during the past month. The seven dimensions included subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication and daytime dysfunction. PSQI score ranged from 0 to 21, with higher scores representing poorer subjective sleep quality.37
The abilities of daily life were assessed by the ADL scale. The response was recorded from the dementia caregivers. The scale was modified by Mingyuan Zhang.38 It included 20 items with stable reliability and validity.38 Each item score ranged from 1 (completely independent) to 4 (completely dependent). The total score ranged from 20 to 80, with a lower score indicating a higher level of ADL.
The behavioural and psychological symptoms of PWDs were assessed by the Neuropsychiatric Inventory (NPI) answered by the dementia caregivers. The inventory was used to evaluate the severity and frequency of 10 common abnormal behaviours in PWDs.39 39Wang translated the inventory and tested the reliability and validity of the Chinese version among persons with AD. The Chinese version of NPI is a reliable and valid tool for measuring neuropsychiatric disturbances in people with AD.
Data analysis
To summarise the sociodemographic status and clinical characteristics, descriptive statistics were used. For continuous variables, mean and SD were reported, and for categorical variables, numbers and proportions were reported. The univariate linear regression was used to test the association between demographic, PWDs’ disease-related, and caregivers’ caregiving-related variables and caregiver burden. Then only the statistically significant variables were entered into the multivariate linear regression. The statistically significant value of the univariate linear regression was set as p<0.1.40 Categorical variables were transferred to dummy variables. The coding of the variables is shown in table 1. The SPSS V.26.0 was used to analyse the data. The statistically significant value was p<0.05.
Table 1.
List of the associated variables.
| Associated variables | Variables | Coding | |
| Sociodemographic characteristics | Age | Continuous variable | |
| Gender | Categorical variable | Male=1, female=0 | |
| Education level | Categorical variable | Illiteracy=1 Primary school=2 Middle school=3 High school or above=4 |
|
| Status of work | Categorical variable | ||
| Relationship | Categorical variable | Spouse=1 Children=2 Relatives=3 |
|
| Characteristics of disease | Type of dementia | Categorical variable | AD=1, FTD=2, MD=3, DLB=4, VD=5 |
| MoCA | Continuous variable | ||
| PISQ | Continuous variable | ||
| NPI | Continuous variable | ||
| ADL | Continuous variable | ||
| Characteristics of caregivers | Caregiving years | Categorical variable | No caring=1 <0.5 years=2 0.5–1 year=3 1–4 years=4 5–9 years=5 More than 9 years=6 |
| Education | |||
| Caring hours/week | Categorical variable | 0–8 hours=1 9–20 hours=2 21–40 hours=3 More than 40 hours=4 |
|
| Depressive symptoms | Continuous variable | ||
| Coping Style Questionnaire | Continuous variable | ||
| PAC | Continuous variable | ||
| Social support | Continuous variable | ||
| Community Service Utilisation | Continuous variable | Used=1 Not used=0 |
AD, Alzheimer’s disease; ADL, activities of daily living; DLB, Dementia with Lewy body; FTD, frontotemporal dementia; MD, mixed dementia; MoCA, Montreal Cognitive Assessment; NPI, neuropsychiatric inventory; PAC, positive aspects of caregivers; PSQI, Pittsburgh Sleep Quality Index; VD, vascular dementia.
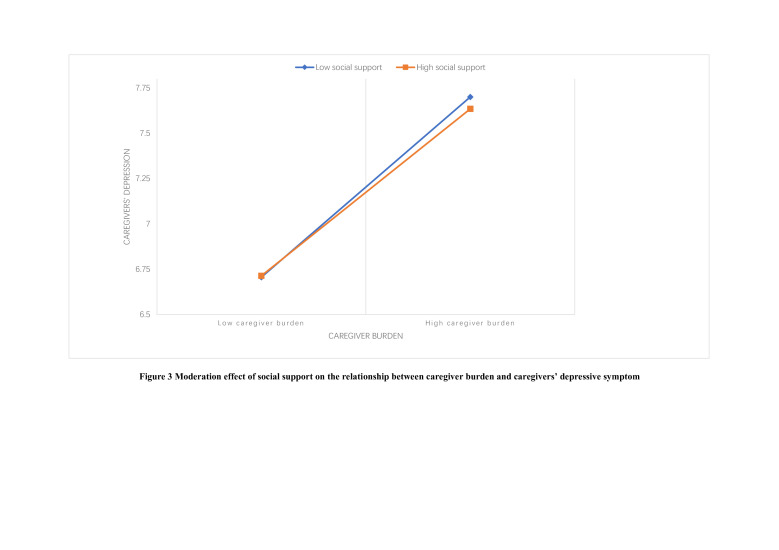
Multiple regression analysis was performed to examine the moderating effect of social support on the relationship between caregiver burden and caregivers’ depressive symptom. Caregiver burden and depressive symptom reduced on receiving social support.
Result
In total, 109 dyads of PWDS and their caregivers were included in the study. Of these PWDs, 37 (33.3%) were diagnosed with AD, 15 (13.5%) with frontotemporal dementia, 22 (19.8%) with mixed dementia, 12 (10.8%) with DLB and 23 (20.7%) with VaD. The average age of the PWDs was 76.02±8.78 years. The percentage of females was 57.8%. Among 109 PWDs, 83 (76.1%) have received education till high school education or above, 12 (11.0%) studied till middle school, 7 (6.4%) till primary school and 7 (6.4%) were illiterate. The average MoCA was 12.50±5.84. The average PSQI was 5.57±5.00. Eighty (72.1%) PWDs reported poor sleep quality. Sociodemographic and disease characteristics of the PWDs are shown in table 2.
Table 2.
Socialdemographic and disease characteristics of the PWDs.
| Characteristics | Mean±SD | N (%) | |
| Sociodemographic characteristics | Age (year) | 76.02±8.78 | |
| Gender | |||
| Female | 63 (57.8) | ||
| Education level | |||
| Below primary school | 14 (12.8) | ||
| Middle school | 12 (11.0) | ||
| High school or above | 83 (76.1) | ||
| Disease characteristics | Type of dementia | ||
| Alzheimer’s | 37 (33.3) | ||
| Frontotemporal | 15 (13.5) | ||
| Mixed | 22 (19.8) | ||
| Dementia with Lewy body | 12 (10.8) | ||
| Vascular dementia | 23 (20.7) | ||
| MoCA total score | 12.50±5.84 | ||
| NPI total symptom scale | 21.50±14.94 | ||
| ADL total score | 42.94±14.17 | ||
| Poor Sleep quality | 80 (72.1) | ||
| Score of PSQI | 5.57±5.00 | ||
| Subjective sleep quality | 0.85±1.02 | ||
| Sleep latency | 1.23±2.01 | ||
| Sleep duration | 0.58±0.83 | ||
| Habitual sleep efficiency | 0.64±1.00 | ||
| Sleep disturbances | 0.64±1.00 | ||
| Use of sleep medications | 1.34±1.49 | ||
| Daytime dysfunction | 1.34±1.49 |
ADL, activities of daily life; MoCA, Montreal Cognitive Assessment; NPI, the Neuropsychiatric Inventory; PSQI, Pittsburgh Sleep Quality Index; PWD, persons with dementia.
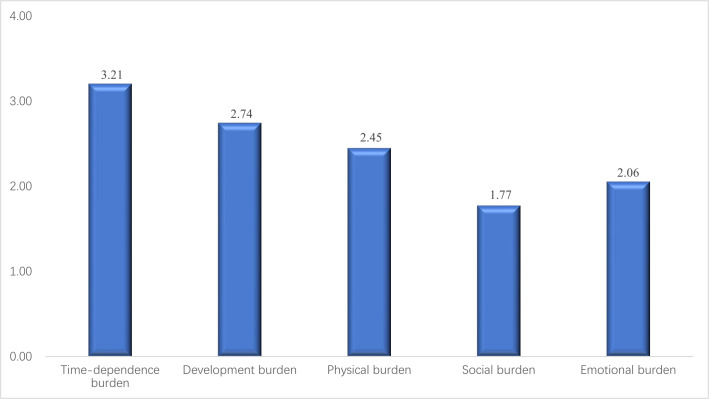
The mean age of the caregivers was 65.18±12.03 years. The percentage of females was 58.7%. Among the 109 caregivers, 66 (50.6%) were spouses and 42 (36.7%) were children of the PWDs. 86 (77.0%) caregivers cared for the PWDs for 1–4 years. 53 (47.7%) caregivers spent 21–40 hours per week on caregiving. The mean score of CBI was 65.92±16.74, which indicated a high level of caregiver burden. The average score of five domains of CBI is shown in figure 2. The sociodemographic characteristics of the caregivers and caregiver burden are shown in table 3.
Figure 2.
Average score of five domains of the Caregiver Burden Index. The average score of the five domains of the Caregiver Burden Index was shown in the figure.
Table 3.
Socialdemographic characteristics and caregiver burden of caregivers.
| Characteristics | Mean±SD | n (%) |
| Age (year) | 65.18±12.03 | |
| Gender | ||
| Female | 64 (58.7) | |
| Education level | ||
| Below primary school or | 12 (11.0) | |
| Middle school | 12 (11.0) | |
| High school or above | 85 (78.0) | |
| Relationship with PWDs | ||
| Spouse | 66 (59.5) | |
| Children | 42 (38.5) | |
| Relatives | 3 (2.7) | |
| Caregiving hours/week (hour) | ||
| <20 | 12 (10.8) | |
| 21–40 | 53 (47.7) | |
| >40 | 44 (39.6) | |
| Caregiving year (years) | ||
| ≤1 | 12 (11) | |
| 1–5 | 86 (77.5) | |
| >5 | 11 (10.1) | |
| Score of SDS | 25.53±3.84 | |
| PAC | 29.49±3.86 | |
| Coping strategy | 92.90±5.78 | |
| Social support | 8.61±1.32 | |
| Community service utilisation | 2.46±1.74 | |
| Score of CBI | 65.92±16.74 | |
| Time-dependence burden | 16.03±5.59 | |
| Development burden | 13.72±3.93 | |
| Physical burden | 9.79±3.48 | |
| Social burden | 7.09±3.07 | |
| Emotional burden | 10.28±3.50 |
CBI, caregiver burden inventory; PAC, Positive aspects of caregiving; PWD, persons with dementia; SDS, Self-rating Depression Scale.
The results of univariate and multivariate linear regression were shown in table 4. PWD age, MoCA, PAC, community service utilisation and the level of social support all had a significant impact on caregiver burden. MoCA, PAC and social support of caregivers were negatively associated with caregiver burden (β=−0.84, p<0.001, β=−3.61, p=0.03 and β=−1.22, p=0.001, respectively), which indicated better PWDs’ cognitive function, more PAC and a higher level of social support were related to less caregiver burden. The community service utilisation were positively associated with caregiver burden (β=3.46, p<0.001), which indicated more community service utilisation were related to more caregiver burden.
Table 4.
Linear regression of CBI
| Variables | Univariate analyses | Multivariate analyses | ||||||||
| B | P value | SE | 95% CI | B | P value | SE | 95% CI | |||
| Lower | Upper | Lower | Upper | |||||||
| Age of PWDs | 0.48 | 0.008 | 0.18 | 0.126 | 0.835 | 0.11 | 0.19 | |||
| Gender of PWDs | 0.41 | 0.90 | 3.26 | −6.06 | 6.87 | |||||
| Education level of PWDs | ||||||||||
| Primary school | −10.43 | 0.25 | 9.00 | −28.28 | 7.42 | |||||
| Middle school | −1.79 | 0.82 | 8.01 | −17.67 | 14.09 | |||||
| High school or above | −4.60 | 0.49 | 6.63 | −17.74 | 8.54 | |||||
| Type of dementia | ||||||||||
| FTD | −3.65 | 0.48 | 5.11 | −13.78 | 6.49 | |||||
| MD | 2.624 | 0.56 | 4.96 | −6.29 | 11.54 | |||||
| DLB | −1.65 | 0.77 | 5.55 | −12.65 | 9.35 | |||||
| VD | 6.74 | 0.13 | 4.43 | −2.05 | 15.54 | |||||
| Score of MoCA | −0.80 | 0.003 | 0.10 | −1.33 | −0.27 | −0.84 | <0.001 | 0.22 | −1.29 | −0.40 |
| Total score of NPI | 0.30 | 0.005 | 0.06 | 0.09 | 0.50 | 0.16 | 0.05 | |||
| Score of ADL | 0.41 | <0.001 | 0.11 | 0.20 | 0.63 | 0.14 | 0.13 | |||
| Score of PSQI | 0.33 | 0.60 | 0.001 | −0.304 | 0.973 | |||||
| Age of caregivers | 0.14 | 0.30 | 0.32 | −0.13 | 0.40 | |||||
| Education level of caregivers | ||||||||||
| Primary school | 14.75 | 0.15 | 10.28 | −5.66 | 35.13 | |||||
| Middle school | 5.75 | 0.55 | 9.69 | −13.46 | 24.96 | |||||
| High school or above | 7.31 | 0.40 | 8.59 | −9.71 | 24.34 | |||||
| Relationship | ||||||||||
| Children | 3.71 | 0.27 | 3.31 | −2.85 | 10.26 | |||||
| Relatives | −17.71 | 0.07 | 9.74 | −37.02 | 1059 | |||||
| Caregiving time for each week | ||||||||||
| 9–20 | −5.00 | 0.65 | 10.94 | −26.67 | 16.70 | |||||
| 21–40 | −0.93 | 0.93 | 9.74 | −20.24 | 18.39 | |||||
| >40 | 6.89 | 0.48 | 9.80 | −12.54 | 26.31 | |||||
| Caregiving years | ||||||||||
| 0.5 | −17.00 | 0.36 | 18.28 | −53.45 | 19.45 | |||||
| 0.5–1 | −15.78 | 0.32 | 15.82 | −47.15 | 15.59 | |||||
| 1–4 | −12.44 | 0.41 | 15.09 | −42.37 | 17.49 | |||||
| 5–9 | 11.86 | 0.46 | 16.04 | −19.95 | 43.67 | |||||
| >9 | 16.00 | 0.34 | 16.78 | −17.27 | 49.27 | |||||
| PAC | −1.33 | 0.001 | 0.40 | −2.12 | −0.54 | −1.22 | 0.001 | 0.34 | −1.90 | −0.55 |
| Coping strategy | −0.25 | 0.38 | 0.28 | −0.80 | 0.31 | |||||
| Social support | −3.32 | 0.006 | 1.18 | −5.667 | −0.972 | −3.61 | <0.001 | 0.99 | −5.58 | −1.64 |
| Community service utilisation | 3.54 | <0.001 | 0.87 | 1.82 | 5.26 | 3.46 | <0.001 | 0.76 | 1.96 | 4.96 |
AD, Alzheimer’s disease; ADL, activities of daily life; CBI, caregiver burden inventory; DLB, Dementia with Lewy bodies; FTD, frontotemporal dementia; MD, mixed dementia; MoCA, Montreal Cognitive Assessment; NPI, neuropsychiatric inventory; PAC, positive aspects of caregivers; PSQI, Pittsburgh Sleep Quality Index; PWD, persons with dementia; VD, vascular dementia.
The moderation effect of social support on the relationship between caregiver burden and caregivers’ depressive symptom was tested. The level of social support independently contributed to caregivers’ depressive symptom. Specifically, a higher level of caregiver burden displayed a high level of depressive symptom (b=0.1235, p<0.001). Moreover, the two-way interaction between social support and caregiver burden significantly contributed to caregivers’ depressive symptom (unstandardised B = −0.027, p=0.011), as reflected in figure 3b.
Figure 3.
Moderation effect of social support on the relationship between caregiver burden and caregivers’ depressive symptom.
Discussion
The level of caregiver burden in this study was relatively higher than that in previous studies.15 16 The study conducted by Wang et al in central China demonstrated that the average CBI score of dementia caregivers was 44.56±10.18.15 Liu et al reported that the average CBI scores for caregivers with mild dementia, moderate dementia, and severe dementia were 19.63±10.75, 36.48±14.20 and 45.29±10.71, respectively, in Beijing.16 The caregiver burden level of our study was higher than that in previous studies conducted in Central and Northern China. It may be due to the different sample source. Our participants were recruited from the general communities in Shanghai. Wang’s study sampled from the Clinical medical Centre of Dementia and Cognitive Impairment in Hubei Province while Liu’s Study sampled from 24 military communities in Beijing. The participants from the clinical centre were able to get professional guidance while the participants from the military community can easily get the service and supplies from the military support compared with the general communities. Our study was a cross-sectional study to explore the level of caregiver burden and factors related to it in PWDs in communities of Shanghai. After controlling for covariates, PWDs’ cognitive function, PAC, social support and community service utilisation were significantly associated with caregiver burden. Social support was a moderator for the relationship between caregiver burden and caregivers’ depressive symptoms.
First, this study has shown that worse cognitive function and older age of PWDs are related to higher caregiver burden, which is consistent with the previous studies in Beijing and Taiyuan of China.16 41 Dementia is always accompanied by neuropsychiatric behaviours and decreased ADL.42 With disease progression, PWD’s dependence on their caregiver increases. The participants suffered from moderate to severe cognitive dysfunction in our study, and the age of the caregivers (65.18±12.03 years) in our research was more than in previous studies (57.5±12.3).16
Second, the level of caregiver burden in our study was relatively high compared with western countries, which can be attributed to the different social environments, cultures, healthcare policies, ethnicity and age of caregivers.23 42 43 Caregiver burden was defined as ‘a multidimensional response to physical, psychological, emotional, social and financial stressors associated with the caregiving experience’.44 Caregiver burden derived from the perceived stressors is influenced by psychosocial factors like social, environmental and cultural.42 A cultural sense of caregiving obligation may augment the distress and burden felt by the caregivers.26 Sharing family affairs with outsiders is not acceptable in Chinese culture.25 A strong sense of family responsibility may prevent caregivers from sharing their caregiving burnout with others. These aspects are not conducive to releasing the burden of caregiving.
Third, although an LTC insurance policy has been introduced since 2016 in 15 cities of China, many PWDs were not included in the policy in the pilot phase.24 The LTC insurance policy was still fragmented. The serious problem included service coverage, service beneficiaries, funding source, payment rates, medical service and senior service, supply option, public–private partnership, and management capacity. Therefore, the actual coverage did not match the actual needs of the disabled elderly.45 The policy did not cover the participants in our study who were from Hongkou District until January 2018, the participants may not be covered by the LTC insurance policy during the interview period. Informal care from family members is the primary source of care for PWDs in China. However, due to the rapid socioeconomic shifts and changing demographic structure, reliance on the care provided by families has become untenable.23 Formal care in most high-income countries has evolved into the home-and community-based care.23 The situation might be responsible for more caregiver burden in our study compared with other countries. Community service was delivered at community healthcare centres. Caregivers needed to take PWDs to community healthcare centres to accept such service. The traffic between home and community healthcare centres may increase caregiver burden. The reimbursement of community service by China’s healthcare insurance was limited. Without the support of insurance, community service utilisation may cause an additional financial burden to dementia caregivers. It has been reported that informal dementia caregivers seldom used respite services.46 The service provided in the communities healthcare centres was limited and it has not met the needs of the PWDs’ caregivers.47 The gap between diverse needs of PWDs’ caregivers and limited supportive community services, especially home visiting services is needed to be closed in the future.
PAC was known to be associated with a lower level of caregiver burden.48 The PAC refers to the satisfaction and reward stemming from the caregiving relationship.49 PAC is associated with a higher level of well-being and better health condition of caregiver.49 Furthermore, PAC can help caregivers cope with challenges related to caregiving.49 Therefore, we found that a higher level of PAC was associated with a lower level of caregiver burden. For further analysis, after controlling for age of PWDs, MoCA, NPI, ADL of PWDs, social support and community service utilisation to caregiver burden the regression analysis showed that the outlook on life (sub-domain of PAC) was associated with caregiver burden (β=−0.45, p<0.001), while the association of self-affirmation (subdomain of PAC) and caregiver burden was not statistically significant (β=0.14, p=0.25). The outlook of life contributed the most to the protective effect on caregiver burden.
We found that caregivers with low-level social support had more depressive symptoms than those with high-level social support. Caregiver burden and depression are complex clinical and social problems.50 Depression of caregivers was associated with providing care, social isolation, limited money and decreased leisure time.51 It has been reported that a higher level of social support is associated with a lower level of caregiver burden.52 In our study, dementia caregivers received social support from family members, relatives, neighbours and colleagues. An earlier study has confirmed that emotional support like reassurance from supporters is critical in reducing depressive symptoms.53 Social support positively influences resilience, and caregivers with strong family support depict elevated resilience.54 Besides, it has been found that sharing in the caregiving role can reduce the caregiver burden effectively.53 Therefore, strengthening social support for caregivers may diminish the adverse effects of depressive symptoms in them.
The results of this study confirmed that the caregiver burden of PWDs was relatively high, and it was dependent on the factors associated with both PWD and the caregiver. Some of these factors could not be altered, such as PWDs’ cognitive function. However, social support and community service are modifiable. Supportive services can be made readily available for dementia caregivers to relieve the caregiver burden. According to the China pilot, LTC insurance policy, the level of disability of older adults is assessed to determine whether the individual met the criterion of LTC insurance. However, the assessment in European and American countries is more in-depth and comprehensive and more detailed regarding specific diseases such as dementia.55 56 The evaluation in China is required to be refined in the future. The Chinese government is now continuously improving the LTC insurance policy, and the coverage is extending to more cities. LTC insurance can provide more specific services to PWDs and caregivers to alleviate depression and reduce their burden. LTC insurance may also effectively reduce the financial burden of PWDs in the future.57
This study had a few limitations also. The participants were recruited from the Hongkou district, part of the centre of Shanghai with high socioeconomic status, advanced community services and improved healthcare resources. Therefore, findings from this study may be restricted as caregiver burden is expected to be higher among family caregivers living in more disadvantaged areas. A large multisite study is needed to confirm the conclusions of this study. Moreover, the study was cross-sectional; thus, the cause-and-effect relationships were not established, and it was not possible to explore the trajectory of caregiver burden of PWD across different stages of the disease. Longitudinal studies are required to overcome these limitations in the future.
Conclusion
This study highlights the emerging issues of dementia and the burden perceived by their family caregivers living in Shanghai communities. Furthermore, the factors associated with caregiver burden were explored. The result verified that caregiver burden is substantial among the family caregivers of PWDs. The cognitive function of PWD, caregivers’ perceived social support and community service utilisation were found to be associated with caregiver burden. Providing adequate social support and home-visit service may alleviate the caregiver burden.
Supplementary Material
Acknowledgments
We thank Dr. Yan Zhang for her contribution to data collection.
Footnotes
ZL, WS and HC contributed equally.
Contributors: ZL designed the concept, analysed data, interpreted data and prepared the manuscript. SW designed the concept, analysed data, interpreted data and prepared the manuscript. HC designed the concept, analysed data, interpreted data and prepared the manuscript. JZ interpreted the outcome and reviewed the manuscript. BW, interpreted the outcome and reviewed the manuscript. HX interpreted the outcome and reviewed the manuscript. PL collected the data. XC collected the data. YY designed the concept, interpreted the outcome and reviewed the manuscript. JL designed the concept, interpreted the outcome and reviewed manuscript. All authors have read and approved the submission and ensure that this is the case. YY was responsible for the overall content as the guarantor.
Funding: This work was supported by Science and Technology Support Projects in Biomedicine Field of Shanghai Science and Technology Commission (#19441907500); Medical Innovation Projects of Second Military Medical University military (#2017JS07); Science and Technology Action Innovation program by the Science and Technology Commission of Shanghai (#17411950104); Characteristic Services of Veteran Cadres Memory Disorders Diagnosis and Treatment in Changzheng hospital (2020CZWJFW12); Natural Science Foundation of Shanghai (#22ZR147750); Shanghai Pujiang Program(#18PJC115); National Natural Science Foundation of China (#72104243).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Ethics Committee: Institutional Review Board (IRB) of Changzheng Hospital, Second Military Medical University. Reference Number: 2019SL026.
References
- 1.World Health Organization . World report on aging and health, 2015. [Google Scholar]
- 2.Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimer's & Dementia 2013;9:63–75. 10.1016/j.jalz.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 3.World population ageing . United nations department of economic and social Affairs population division, 2017. [Google Scholar]
- 4.Ding D, Zhao Q, Guo Q, et al. The Shanghai aging study: study design, baseline characteristics, and prevalence of dementia. Neuroepidemiology 2014;43:114–22. 10.1159/000366163 [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth Edition: DSM-IV-TR®. Washington DC: American Psychiatric Pub, 2000. [Google Scholar]
- 6.Xu J, Wang J, Wimo A, et al. The economic burden of dementia in China, 1990-2030: implications for health policy. Bull World Health Organ 2017;95:18–26. 10.2471/BLT.15.167726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist 1986;26:260–6. 10.1093/geront/26.3.260 [DOI] [PubMed] [Google Scholar]
- 8.Bertrand RM, Fredman L, Saczynski J. Are all caregivers created equal? stress in caregivers to adults with and without dementia. J Aging Health 2006;18:534. 10.1177/0898264306289620 [DOI] [PubMed] [Google Scholar]
- 9.Kim M-D, Hong S-C, Lee C-I, et al. Caregiver burden among caregivers of Koreans with dementia. Gerontology 2009;55:106–13. 10.1159/000176300 [DOI] [PubMed] [Google Scholar]
- 10.Gallagher D, Ni Mhaolain A, Crosby L, et al. Self-efficacy for managing dementia may protect against burden and depression in Alzheimer's caregivers. Aging Ment Health 2011;15:663–70. 10.1080/13607863.2011.562179 [DOI] [PubMed] [Google Scholar]
- 11.Yeager CA, Hyer LA, Hobbs B, et al. Alzheimer's disease and vascular dementia: the complex relationship between diagnosis and caregiver burden. Issues Ment Health Nurs 2010;31:376. 10.3109/01612840903434589 [DOI] [PubMed] [Google Scholar]
- 12.Conde-Sala JL, Garre-Olmo J, Turró-Garriga O, et al. Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer's disease: an exploratory comparative design. Int J Nurs Stud 2010;47:1262–73. 10.1016/j.ijnurstu.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 13.Chan CY, Cheung G, Martinez-Ruiz A, et al. Caregiving burnout of community-dwelling people with dementia in Hong Kong and New Zealand: a cross-sectional study. BMC Geriatr 2021;21:261. 10.1186/s12877-021-02153-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu S, Li C, Shi Z. Caregiver burden and prevalence of depression, anxiety and sleep disturbances in Alzheimer’s disease caregivers in China. Journal of Clinical Nursing 2016. 10.1111/jocn.13601 [DOI] [PubMed] [Google Scholar]
- 15.Min, Wang H, et al. Prevalence and associated factors of elder abuse in family caregivers of older people with dementia in central China: a cross-sectional study. Int J Geriatr Psychiatry 2018. 10.1002/gps.5020 [DOI] [PubMed] [Google Scholar]
- 16.Liu J, Wang L-ning, Tan J-ping, et al. Burden, anxiety and depression in caregivers of veterans with dementia in Beijing. Arch Gerontol Geriatr 2012;55:560–3. 10.1016/j.archger.2012.05.014 [DOI] [PubMed] [Google Scholar]
- 17.Abdollahpour I, Nedjat S, Salimi Y. Positive aspects of caregiving and caregiver burden: a study of caregivers of patients with dementia. J Geriatr Psychiatry Neurol 2018;31:34–8. 10.1177/0891988717743590 [DOI] [PubMed] [Google Scholar]
- 18.Chou KR. Caregiver burden: a concept analysis. J Pediatr Nurs 2000;15:398–407. 10.1053/jpdn.2000.16709 [DOI] [PubMed] [Google Scholar]
- 19.Ross E. Psychosocial approaches to health, illness and disability: A reader for health care professionals [M] 2004.
- 20.Cohen S, Mckay G. Social support, stress, and the buffering hypothesis: a theoretical analysis. Hillsdale 1984. 10.1037/0033-2909.98.2.310 [DOI] [Google Scholar]
- 21.Thoits PA. Conceptual, methodological, and theoretical problems in studying social support as a buffer against life stress. J Health Soc Behav 1982;23:145–59. 10.2307/2136511 [DOI] [PubMed] [Google Scholar]
- 22.Wang Z, Ma C, Han H, et al. Caregiver burden in Alzheimer’s disease: Moderation effects of social support and mediation effects of positive aspects of caregiving. Int J Geriatr Psychiatry 2018;33:1198–206. 10.1002/gps.4910 [DOI] [PubMed] [Google Scholar]
- 23.Du P, Dong T, Ji J. Current status of the long-term care security system for older adults in China. Res Aging 2021;43:016402752094911. 10.1177/0164027520949117 [DOI] [PubMed] [Google Scholar]
- 24.Feng J, Wang Z, Yu Y. Does long-term care insurance reduce hospital utilization and medical expenditures? Evidence from China. Soc Sci Med 2020;258:113081. 10.1016/j.socscimed.2020.113081 [DOI] [PubMed] [Google Scholar]
- 25.Chan SW-C. Family caregiving in dementia: the Asian perspective of a global problem. Dement Geriatr Cogn Disord 2010;30:469–78. 10.1159/000322086 [DOI] [PubMed] [Google Scholar]
- 26.Brandão D, Ribeiro O, Oliveira M, et al. Caring for a centenarian parent: an exploratory study on role strains and psychological distress. Scand J Caring Sci 2017;31:984–94. 10.1111/scs.12423 [DOI] [PubMed] [Google Scholar]
- 27.Joling KJ, van Hout HPJ, Scheltens P, et al. (Cost)-effectiveness of family meetings on indicated prevention of anxiety and depressive symptoms and disorders of primary family caregivers of patients with dementia: design of a randomized controlled trial. BMC Geriatr 2008;8:2. 10.1186/1471-2318-8-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical power analysis for the behavioral sciences. 407. 2nd edn. L. Erlbaum Associates, 1988. [Google Scholar]
- 29.Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist 1989;29:798–803. 10.1093/geront/29.6.798 [DOI] [PubMed] [Google Scholar]
- 30.Chou K-R, Jiann-Chyun L, Chu H. The reliability and validity of the Chinese version of the caregiver burden inventory. Nurs Res 2002;51:324. 10.1097/00006199-200209000-00009 [DOI] [PubMed] [Google Scholar]
- 31.Torrisi M, De Cola MC, Marra A, et al. Neuropsychiatric symptoms in dementia may predict caregiver burden: a Sicilian exploratory study. Psychogeriatrics 2017;17:103–7. 10.1111/psyg.12197 [DOI] [PubMed] [Google Scholar]
- 32.ZUNG WW, ZUNG, William WK. A self-rating depression scale. Arch Gen Psychiatry 1965;12:63. 10.1001/archpsyc.1965.01720310065008 [DOI] [PubMed] [Google Scholar]
- 33.Chen H, Chi I, Liu R. Hospital utilization among Chinese older adults: patterns and predictors. Journal of Aging and Health 2018;31:089826431878054. 10.1177/0898264318780546 [DOI] [PubMed] [Google Scholar]
- 34.Lou VWQ, Lau BH-P, Cheung KS-L. Positive aspects of caregiving (PAC): scale validation among Chinese dementia caregivers (CG). Arch Gerontol Geriatr 2015;60:299–306. 10.1016/j.archger.2014.10.019 [DOI] [PubMed] [Google Scholar]
- 35.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695–9. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 36.Chen X, Zhang R, Xiao Y, et al. Reliability and validity of the Beijing version of the Montreal cognitive assessment in the evaluation of cognitive function of adult patients with OSAHS. PLoS One 2015;10:e0132361. 10.1371/journal.pone.0132361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu XC, Tang MQH, Wang L. Reliability and validity of the Pittsburgh sleep quality index. Chinese Journal of Psychiatry 1996;29:29103–7. [Google Scholar]
- 38.Guo Q, Hong Z. Neuropsychological assessment. 2nd Ed. Shanghai: Shanghai science and technology press, 2016. [Google Scholar]
- 39.Wang T, Xiao S, Li X, Wang H, et al. Reliability and validity of the Chinese version of the neuropsychiatric inventory in mainland China. Int J Geriatr Psychiatry 2012;27:539–44. 10.1002/gps.2757 [DOI] [PubMed] [Google Scholar]
- 40.Bursac Z, Gauss CH, Williams DK, et al. Purposeful selection of variables in logistic regression. Source Code Biol Med 2008;3:17. 10.1186/1751-0473-3-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yu H, Wang X, He R, et al. Measuring the caregiver burden of caring for Community-Residing people with Alzheimer's disease. PLoS One 2015;10:e0132168. 10.1371/journal.pone.0132168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Toni S, Ilona H, Taina H, et al. Neuropsychiatric symptoms and activities of daily living in Alzheimer’s disease: ALSOVA 5-year follow-up study. Int Psychogeriatr, undefined(undefined) 2019:1–11. [DOI] [PubMed] [Google Scholar]
- 43.Allen AP, Buckley MM, Cryan JF, et al. Informal caregiving for dementia patients: the contribution of patient characteristics and behaviours to caregiver burden. Age Ageing 2019;49:52–6. 10.1093/ageing/afz128 [DOI] [PubMed] [Google Scholar]
- 44.Kasuya RT, Polgar-Bailey P, Takeuchi R. Caregiver burden and burnout: a guide for primary care physicians. Postgraduate Medicine 2001;108:119–23. 10.3810/pgm.2000.12.1324 [DOI] [PubMed] [Google Scholar]
- 45.Zhou W, Dai W. Shifting from fragmentation to integration: a systematic analysis of long-term care insurance policies in China. Int J Integr Care 2021;21:11. 10.5334/ijic.5676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Su J-A, Chang C-C. Association between family caregiver burden and affiliate stigma in the families of people with dementia. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17082772. [Epub ahead of print: 17 04 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin W. Community service contracting for older people in urban China: a case study in Guangdong Province. Aust J Prim Health 2016;22:55–62. 10.1071/PY15085 [DOI] [PubMed] [Google Scholar]
- 48.Xue H, Zhai J, He R, et al. Moderating role of positive aspects of caregiving in the relationship between depression in persons with Alzheimer's disease and caregiver burden. Psychiatry Res 2018;261:400. 10.1016/j.psychres.2017.12.088 [DOI] [PubMed] [Google Scholar]
- 49.Tarlow BJ, Wisniewski SR, Belle SH. Positive aspects of caregiving: contributions of the reach project to the development of new measures for alzheimer’s caregiving. Research on Aging 2004;26:429–53. 10.1177/0164027504264493 [DOI] [Google Scholar]
- 50.Springate B, Tremont G. Caregiver burden and depression in mild cognitive impairment. J Appl Gerontol 2013;32:765–75. 10.1177/0733464811433486 [DOI] [PubMed] [Google Scholar]
- 51.Simpson C, Carter P. Dementia behavioural and psychiatric symptoms: effect on caregiver's sleep. J Clin Nurs 2013;22:3042-52. 10.1111/jocn.12127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xian M, Xu L. Social support and self-rated health among caregivers of people with dementia: the mediating role of caregiving burden. Dementia 2020;19:147130121983746. 10.1177/1471301219837464 [DOI] [PubMed] [Google Scholar]
- 53.Huang C-Y, Musil CM, Zauszniewski JA, et al. Effects of social support and coping of family caregivers of older adults with dementia in Taiwan. Int J Aging Hum Dev 2006;63:1–25. 10.2190/72JU-ABQA-6L6F-G98Q [DOI] [PubMed] [Google Scholar]
- 54.Cohen S, Mckay G. Social support, stress, and the buffering hypothesis: a theoretical analysis, 1984. Hillsdale. Available: http://www.psy.cmu.edu/~scohen/buffer84.pdf
- 55.Shanghai Municipal Government . Shanghai’s pilot Measures for long-term care Insurance, 2016. [Google Scholar]
- 56.Zeng Q, Wang Q, Zhang L, et al. Comparison of the measurement of long-term care costs between China and other countries: a systematic review of the last decade. Healthcare 2020;8:117. 10.3390/healthcare8020117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen L, Zhang X, Xu X. Health insurance and long-term care services for the disabled elderly in China: based on CHARLS data. Risk Manag Healthc Policy 2020;13:155–62. 10.2147/RMHP.S233949 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request. Not applicable.