Abstract
The number of shoulder replacements performed each year continues to increase, and the need for revision replacements has grown accordingly. The outcome of a revision replacement may influence which primary implant is selected and the timing of primary surgery, particularly in younger patients. The aim of this study was to establish the expected improvement in shoulder function and implant survival following revision of a hemiarthroplasty and revision of an anatomical total shoulder arthroplasty (TSA). A systematic review and meta-analysis were performed of all studies reporting shoulder scores or implant survival following revision hemiarthroplasty or revision TSA. MEDLINE, EMBASE, CENTRAL, The Cochrane Database of Systematic Reviews and National Joint Registry reports were searched. 15 studies were included, reporting on 593 revision anatomical shoulder replacements. There was large variation in the magnitude of improvement in shoulder scores following revision surgery. Over 80% of revision replacements last 5 years and over 70% last 10 years. There was no significant difference in shoulder scores or implant survival according to the type of primary implant. The belief that revision of a shoulder hemiarthroplasty may lead to improved outcomes compared to revision of a TSA is not supported by the current literature.
Keywords: shoulder, revision, replacement, arthroplasty, survival, shoulder scores, patient reported outcome measures
Introduction
The demand for shoulder replacements continues to rise. Broadening indications, technical innovation, and a growing population have all contributed to an increase in the number of replacements performed each year. The volume of revision surgery has also increased. Since 2012, 52,000 shoulder replacements have been performed in the UK and the rate of revision shoulder replacement is 3.9−9.9% at 8 years, with similar proportions reported in the Australian National Joint Registry.1,2
For anatomical shoulder replacements the most common indications for revision are rotator cuff insufficiency, dislocation and aseptic loosening. 1 A further common indication for revision of hemiarthroplasty is erosion of the native glenoid. 1 Glenoid erosion, rotator cuff integrity, and a well fixed humeral component may all contribute to the challenge of performing a revision replacement. 3 Data on the outcomes of revision shoulder replacement are steadily increasing.
In patients who are considering a shoulder replacement, the risk of revision and the outcomes that can be achieved following revision form part of the decision making process. 4
This is particularly true of young patients where a revision is likely during the patient's lifetime. In young patients, equipoise remains regarding the best implant. 5 Compared to hemiarthroplasty, TSA may lead to an improved range of motion and reduced pain. 6 A hemiarthroplasty removes the risk of glenoid implant complications. However revision may also be necessary due to pain from the native glenoid. 7 In principle, maintaining native glenoid anatomy and bone stock may improve glenoid component implantation, and this can influence the decision about which primary implant to use, particularly in younger patients.8,9 However no previous review could be found which analysed the outcomes of revision hemiarthroplasty and revision TSA. The aim of this review was to investigate the clinical outcomes and survivorship of revision hemiarthroplasty and revision TSA.
Method
The review was completed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 10 The protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO).
The following databases were searched: MEDLINE (OvidSP, 1946 to present), Embase (OvidSP, 1974 to present), CENTRAL and the Cochrane Database of Systematic Reviews. National Joint Registry Reports which included data on shoulder arthroplasty procedures were reviewed. The search was performed in September 2021.
Inclusion Criteria
All randomised and non-randomised studies reporting outcomes of revision anatomical total shoulder arthroplasty and revision hemiarthroplasty were included. Revision to the following implant types were accepted: hemiarthoplasty, TSA and reverse shoulder arthroplasty. All indications for the primary replacement were accepted, however studies were excluded where the majority of primary procedures were performed for trauma, or more than 20% of the revisions were performed for prosthetic joint infection. The specific surgical indications for each revision procedure are detailed in the appendix. A minimum of 12 months follow-up was required for the implant survival outcome.
Outcomes
The primary outcome was the difference in the postoperative shoulder score compared to the preoperative shoulder score. All commonly used and validated shoulder scores were accepted. Secondary outcomes included implant survivorship and complications.
Data Extraction
The search results were managed using Covidence® systematic review software. Duplicates were removed and the remaining abstracts were screened independently by two reviewers. Full text review was performed of relevant articles. A third reviewer was available to discuss any conflicts.
Data was extracted onto pre-specified data collection sheets by two reviewers. Data was collected on the authors, institutions, study design, patient demographics, inclusion and exclusion criteria, number of patients, surgical indication, type of primary and revision implants, loss to follow-up and the outcomes of interest. Risk of bias was assessed by two reviewers. We applied the MINORS instrument which is used to assess both comparative and non-comparative studies. 11
Data Analysis
We performed a quantitative synthesis of the difference in shoulder scores and the survival of the revision implants. Several shoulder scores were used including the American Shoulder and Elbow Score, Constant-Murley Score, Penn Shoulder Score, Oxford Shoulder Score and the University of California, Los Angeles Shoulder Score. To enable meta-analysis of multiple scores the difference in pre-operative and post-operative shoulder scores were pooled using the standardised mean difference and weighted according to standard error. The analyses were performed using Revman® systematic review software using a random effects model. Sensitivity analyses were performed to explore the improvement in shoulder scores following revision of a TSA to TSA, compared to revision of a TSA to RSA.
Meta-analysis of revision implant survivorship was performed using STATA version 16. Study results were weighted according to standard error, calculated from confidence intervals and pooled using a random-effects model. Studies were required to report survival analyses along with confidence intervals for inclusion in the meta-analysis. Where few studies were available the results of individual studies were included in the summary survival graph.
Results
The database searches revealed 5368 studies, 3 further studies were added following manual review of reference lists. Duplicates were removed which left 3917 abstracts for screening. A further 65 studies were excluded on full text review, 15 studies met our inclusion criteria. The PRISMA flow diagram is shown in Figure 1.
Figure 1.
PRISMA study flow diagram.
Of the included studies, 12 were case series and 3 were cohort studies. They reported on a total of 593 revision anatomical shoulder replacements, of which 557 reached the final follow-up period for the shoulder scores. A summary of study characteristics is shown in table 1.
Table 1.
Included Studies. n/r – not Reported. HA – Hemiarthroplasty, m – Months, yr – Years. ASES – American Shoulder and Elbow Score. Constant – Constant-Murley Score. SST – Simple Shoulder Test.
| Study | Primary Implant | Revision implant | Number shoulders | Mean age | Mean follow-up | Shoulder Scores | Included in meta-anal. shoulder scores | Included in survival analysis |
|---|---|---|---|---|---|---|---|---|
| Aibinder 2017 12 | TSA | TSA | 34 | 66 | 8.3 year | None | No | Yes |
| Bartels 2021 13 | TSA | TSA RSA |
145 | 70.2 | 35 m | None | No | Yes |
| Castagna 2013 14 | TSA | RSA | 8 | 73.6 | 31.6 m | Constant | Yes | No |
| Cheung 2008 15 | TSA | TSA | 33 | 65 | 3.8 year | None | No | Yes |
| Deutsch 2007 16 | TSA | TSA | 32 | 62 | 4 yr | ASES | Yes | No |
| Groh 2011 17 | HA | TSA | 15 | 69 | 40 m | UCLA | Yes | No |
| Jaiswal 2019 18 | HA | TSA, RSA & HA | 26 | 69 | 5.2 year | Constant | Yes | No |
| Melis 2012 19 | TSA | RSA | 40 | 71 | 47 m | Constant | Yes | No |
| Otte 2020 20 | TSA | RSA | 75 | 64.6 | 22.3 m | ASES | Yes | No |
| Ravenscroft 2009 21 | HA | TSA | 17 | 66 | 52 m | Constant ASES | No | No |
| Sassoon 2012 22 | HA | TSA | 71 | 55 | 75 m | None | No | Yes |
| Scalise 2008 23 | TSA | RSA | 16 | 69 | 38 m | Penn | Yes | No |
| Shields 2019 24 | TSA | RSA | 42 | 64 | 50 m | ASES | Yes | No |
| Walker 2012 25 | TSA | RSA | 24 | 68.6 | 39.6 m | ASES SST | No | No |
| Weber-Spickschen 2015 26 | TSA | RSA | 15 | 70 | 43 m | ASES OSS WOOS | Yes | No |
UCLA – The University of California at Los Angeles Shoulder Score. OSS – Oxford Shoulder Score. WOOS – Western Ontario Osteoarthritis of the Shoulder Index. Penn – Penn Shoulder Score.
The primary procedure was a total shoulder arthroplasty in 11 studies and a hemiarthroplasty in 4 studies. The type of revision implant varied across the studies; a reverse shoulder arthroplasty was the revision implant in 7 studies, and a TSA in 6 studies. In 2 studies a mixture of revision implants were used.13,18 In the study by Jaiswal and colleagues all the primary procedures were hemiarthroplasties; 18 were revised to a TSA, 7 to a RSA and one to a hemiarthroplasty. 18 The large majority of TSA were revised for aseptic loosening or rotator cuff failure, and the large majority of hemiarthroplasties were revised for painful glenoid erosion or rotator cuff failure. The full list of indications for revision are available in the appendix.
Shoulder Scores
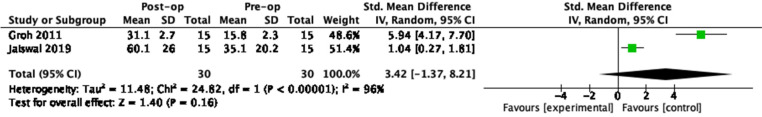
Pre-operative and post-operative shoulder scores were reported in 11 studies. The most commonly used scores were the ASES and Constant-Murley scores. A meta-analysis of 7 studies reporting shoulder scores was possible for TSA as the primary procedure. The mean follow-up duration across all 7 studies was 22–50 months. 2 studies were available for the meta-analysis of scores following revision of a hemiarthroplasty, with a mean follow-up of 40–62 months. The forest plots of the standardised mean difference in pre-operative and post-operative shoulder scores are shown in Figures 2 and 3.
Figure 2.
Revision of a TSA. SMD in perioperative shoulder scores.
Figure 3.
Revision of a hemiarthroplasty. SMD in perioperative shoulder scores.
A sensitivity analysis was performed comparing the improvement in shoulder scores for revision of a TSA to a TSA against revision of a TSA to RSA. The standardised mean difference in shoulder scores was 2.11 (1.42−2.80) for a TSA revised to RSA and 0.75 (0.0−1.49) for TSA revised to a TSA. The forest plots are available in the appendix, the TSA to TSA group was limited to 15 patients across a single study by Deutsch et al. 16
Survivorship
Survival outcomes were reported alongside confidence intervals in 4 studies; 3 following revision of a TSA and 1 following revision of a hemiarthroplasty. The duration of follow-up ranged from 1 to 10 years. There were sufficient studies for meta-analysis of survival outcomes at 5 years following TSA, this is shown in Figure 4.
Figure 4.
5 year survival following revision from a TSA.
Implant survival across all studies is summarised in Figure 5. The majority are of the data points represent single studies. The data for hemiarthroplasty is taken from Sassoon et al. 22 The data for TSA at 1 year is reported by Bartels et al, and 10 year data were extracted from Aibinder et al.12,13
Figure 5.
Implant survival following revision of a TSA and HA.
None of the nine national joint registries which include outcomes for shoulder arthroplasty currently report on patient reported outcomes or survivorship of revision implants. 27
Risk of Bias
The risk of bias assessment was completed using the 8-point MINORS instrument for non-randomised studies without a comparison arm. 11 In the large majority of cases the study aims were clearly stated, and consecutive patients were included. The methodology of all studies was to retrospectively review the outcomes of revision procedures. However in the case of shoulder scores, data was collected prospectively. The follow-up duration was commonly the most recent point of follow-up rather than a pre-specified duration. No studies performed a prospective sample size calculation. The full risk of bias table is available in the appendix.
Discussion
Greater information about outcomes following revision shoulder replacement is valuable both when considering whether to perform a revision replacement and when deciding on the type of primary implant. The burden of revision arthroplasty continues to grow and revision procedures are expensive.28,29 The risks of revision and re-revision are important; recovery of function following a revision replacement may be more modest compared to recovery following a primary replacement,30,31 and revisions can have significant influence on the cost-effectiveness of an implant. 32
Revision of a hemiarthroplasty may lead to improved outcomes due to maintenance of the native glenoid at the time of the primary procedure, but there is limited evidence to support this assumption. Erosion of the native glenoid following hemiarthroplasty can lead to persistent pain and asymmetrical glenoid erosion may occur. 17 Carrol and colleagues demonstrated poor patient satisfaction and unpredictable improvement in symptoms following revision of a hemiarthroplasty to TSA. 33 Our systematic review highlights the broad range of reported improvement in shoulder scores across studies following revision of an anatomical shoulder replacement. Despite a satisfactory mean improvement in shoulder scores there is high variability in outcomes both within and between studies. Large improvements in shoulder scores were demonstrated in some patients, whereas in others it was far more modest. There was no significant difference in shoulder scores or implant survival between revision of a hemiarthroplasty and revision of a total shoulder arthroplasty. Over 80% of revision implants did not require re-revision at 5 years. 73% of revisions where the primary implant was a hemiarthroplasty were free of re-revision at 10 years compared to 79% of revision of a primary total shoulder arthroplasties. These data were based on a small number of studies. Further Kaplan-Meier survival estimates were provided by Sheth et al, but no confidence intervals were included. 34 They showed a significant difference in revision implant survival at 5 years; the survival of a revision of a hemiarthroplasty was 94% compared to 30% of revisions of a TSA. 34 However the TSA group was limited to 10 patients. Our meta-analysis of implant survival at 5 years following revision of a TSA was 83.4% (73.1-93.7). It should be noted that these estimates of implant survival are unadjusted for mortality, rather than crude estimates that are calculated using a competing risks model. 35 The unadjusted estimates report the risk of revision should the patient remain alive during the follow-up period. This is a relevant consideration given the revision population are more likely to be of advancing age.
More recently new bearing surfaces have been introduced. 36 Pyrocarbon humeral heads have been developed with the aim of reducing glenoid wear.37,38 The extent of glenoid wear has not been shown to correlate with shoulder function however it may make revision surgery more challenging. 37 Ceramic humeral heads have shown encouraging wear characteristics and may reduce osteolysis compared to metal heads in total shoulder arthroplasty,39,40 no work could be found investigating the effect of a ceramic head on native glenoid wear following hemiarthroplasty.
The choice of revision implant may further influence outcomes and there is limited work in this area. Our sensitivity analysis suggests revision to a RSA may lead to superior shoulder scores at mid-term follow-up, however uncertainty remains given the small number of included patients and broad confidence intervals. A previous review demonstrated superior shoulder scores following TSA revised to a RSA, compared to TSA revised to a TSA. 41 However it is unclear how the data synthesis was performed and broad inclusion criteria were used. No work could be found comparing implant choices when revising a hemiarthroplasty.
When considering a joint replacement patient's priorities may differ. 42 A high value is placed on symptom relief and improvement in function by patients.4,42 This is an important consideration given that primary TSA may lead to improved pain relief and function compared to hemiarthroplasty. 6 Patients describe an eagerness to return to function and regain control of their life, despite the potential need for a revision in future. 4 The ability to continue employment is particularly important for younger patients. 43
Despite the growing importance of revision shoulder arthroplasty the evidence base centres around relatively small case series. In comparison the revision knee arthroplasty literature is supported by larger and more established joint registries which provide data on re-revision rates. 44 However there remains a relatively small number of articles which report on the clinical outcomes of revision total knee arthroplasty. 45
Broad inclusion criteria were necessary in this systematic review to capture sufficient studies to warrant analysis. The surgical indication of the primary procedure may influence outcomes leading to an overestimation or underestimation of the effect of the primary procedure on the outcome of revision for different indications. Revision for infection was only included if the total proportion of revisions for infection in a study were a maximum of 20%, due to the poor outcomes associated with this revision indication. This threshold was selected as a compromise to capture papers which revised a small proportion of joints for infection but involved sufficiently few patients that it would not substantially bias the results. Three studies included any patients revised for infection, two in the TSA and one in the hemiarthroplasty group.18,20,25 We did not stratify outcomes by indications for revision. It should be noted that indications for revision may overlap, an undiagnosed infection may be present in cases of symptomatic implant loosening, and persistent pain may occur in patients with rotator cuff tears or instability. A sensitivity analysis was performed for the revision implant following a primary TSA, however several revision implants were used across the review leading to additional heterogeneity. The reporting of loss to follow-up was mixed, in 38% of articles the loss to follow-up was over 5%. The use of alternative bearing surfaces including ceramic and pyrocarbon implants may alter the pattern of glenoid wear following hemiarthroplasty, and influence the outcomes of revision replacement. Further data on the outcomes of these implants is necessary.
Conclusion
Revision of a shoulder hemiarthroplasty and revision of a TSA leads to improved shoulder scores, however the magnitude of improvement varies substantially across studies. The improvement in shoulder scores following revision of a hemiarthroplasty was not superior to revision TSA across included studies, and do not support the rationale that revision of a hemiarthroplasty will lead to superior outcomes. Over 80% of revision anatomical replacements last 5 years, 73% of revision hemiarthroplasties and 79% of revision TSA last 10 years.
Supplemental Material
Supplemental material, sj-docx-1-sea-10.1177_24715492221095991 for Revision Shoulder Hemiarthroplasty and Total Shoulder Arthroplasty A Systematic Review and Meta-Analysis by Andrew Davies, Hussain Selmi, Sanjeeve Sabharwal, Martinique Vella-Baldacchino, Alex D. Liddle and Peter Reilly in Journal of Shoulder and Elbow Arthroplasty
Footnotes
Author Contributions: .
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: AD is a Royal College or Surgeons (RCS) / National Joint Registry (NJR) research fellow.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iD: Andrew Davies https://orcid.org/0000-0002-2079-9919
Supplemental material: Supplemental material for this article is available online.
References
- 1.Reed M, Brittain R, Howard P, et al. 18th Annual Report. The National Joint Registry 18th Annual Report 2021. National Joint Registry; 2021. [PubMed] [Google Scholar]
- 2.Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2021 Annual Report, Adelaide; AOA, 2021: 1–434. Accessed from: https://aoanjrr.sahmri.com/annual-reports-2021.
- 3.Dines JS, Uggen C, Kerker J, Dines DM. Revision shoulder arthroplasty. Minerva Ortop e Traumatol. 2006;57(6):509–520. [Google Scholar]
- 4.Conner-spady BL, Marshall DA, Hawker GAet al. et al. You’ll know when you’re ready : a qualitative study exploring how patients decide when the time is right for joint replacement surgery. BMC Health Serv Res. 2014;454 (14):1–10. doi: 10.1186/1472-6963-14-454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Care Excellence (NICE). Joint replacement (primary): hip, knee and shoulder NICE guideline [NG157]. 2020;(June). Available from: https://www.nice.org.uk/guidance/ng157. (Accessed: 15 October 21). [PubMed]
- 6.Craig RS, Goodier H, Singh JA, Hopewell S, Rees JL. Shoulder replacement surgery for osteoarthritis and rotator cuff tear arthropathy. Cochrane Database Syst Rev. 2020;4(4):CD012879. doi: 10.1002/14651858.CD012879.pub2. Accessed 05 September 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elb Surg. 2004;13(6):604–613. doi: 10.1016/j.jse.2004.03.013 [DOI] [PubMed] [Google Scholar]
- 8.Malhas A, Rashid A, Copas D, Bale S, Trail I. Glenoid bone loss in primary and revision shoulder arthroplasty. Shoulder Elb. 2016;8(4):229–240. doi: 10.1177/1758573216648601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson MH, Paxton ES, Green A. Shoulder arthroplasty options in young (< 50 years old) patients : review of current concepts. J Shoulder Elb Surg. 2015;24(2):317–325 [DOI] [PubMed] [Google Scholar]
- 10.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 11.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 12.Aibinder WR, Schoch B, Schleck C, Sperling JW, Cofield RH. Revisions for aseptic glenoid component loosening after anatomic shoulder arthroplasty. J Shoulder Elb Surg. 2017;26(3):443–449. doi: 10.1016/j.jse.2016.08.009 [DOI] [PubMed] [Google Scholar]
- 13.Bartels DW. Revision reverse shoulder arthroplasty for anatomical glenoid component loosening was not universally successful. J Bone Jt Surg – Am. 2021;103(10):879–886. doi: 10.2106/JBJS.20.00555 [DOI] [PubMed] [Google Scholar]
- 14.Castagna A, Delcogliano M, De Caro F, et al. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37(7):1297–1305. doi: 10.1007/s00264-013-1907-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheung E V., Sperling JW, Cofield RH. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elb Surg. 2008;17(3):371–375. doi: 10.1016/j.jse.2007.09.003 [DOI] [PubMed] [Google Scholar]
- 16.Deutsch A, Abboud JA, Kelly J, et al. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elb Surg. 2007;16(6):706–716. doi: 10.1016/j.jse.2007.01.007 [DOI] [PubMed] [Google Scholar]
- 17.Groh GI, Wirth MA. Results of revision from hemiarthroplasty to total shoulder arthroplasty utilizing modular component systems. J Shoulder Elb Surg. 2011;20(5):778–782. doi: 10.1016/j.jse.2010.09.014 [DOI] [PubMed] [Google Scholar]
- 18.Jaiswal A, Malhotra A, Hay S, Kelly CP. Revision shoulder arthroplasty for failed surface replacement hemiarthroplasty. Musculoskelet Surg. 2019;103(1):69–75. doi: 10.1007/s12306-018-0541-0 [DOI] [PubMed] [Google Scholar]
- 19.Melis B, Bonnevialle N, Neyton L, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elb Surg. 2012;21(3):342–349. doi: 10.1016/j.jse.2011.05.021 [DOI] [PubMed] [Google Scholar]
- 20.Otte RS, Naylor AJ, Blanchard KN, et al. Salvage reverse total shoulder arthroplasty for failed anatomic total shoulder arthroplasty: a cohort analysis. J Shoulder Elb Surg. 2020;29(7):S134–S138. doi: 10.1016/j.jse.2020.04.013 [DOI] [PubMed] [Google Scholar]
- 21.Ravenscroft M, Charalambous CP, Haines JF, Trail IA. Outcome of stemmed shoulder hemi-arthroplasty revision. Arch Orthop Trauma Surg. 2009;129(6):797–799. doi: 10.1007/s00402-008-0728-1 [DOI] [PubMed] [Google Scholar]
- 22.Sassoon AA, Rhee PC, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Revision total shoulder arthroplasty for painful glenoid arthrosis after humeral head replacement: the nontraumatic shoulder. J Shoulder Elb Surg. 2012;21(11):1484–1491. doi: 10.1016/j.jse.2011.11.028 [DOI] [PubMed] [Google Scholar]
- 23.Scalise JJ, Iannotti JP. Bone grafting severe glenoid defects in revision shoulder arthroplasty. Clin Orthop Relat Res. 2008;466(1):139–145. doi: 10.1007/s11999-007-0065-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shields E, Wiater JM. Patient outcomes after revision of anatomic total shoulder arthroplasty to reverse shoulder arthroplasty for rotator cuff failure or component loosening: a matched cohort study. J Am Acad Orthop Surg. 2019;27(4):e193–e198. doi: 10.5435/JAAOS-D-17-00350 [DOI] [PubMed] [Google Scholar]
- 25.Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elb Surg. 2012;21(4):514–522. doi: 10.1016/j.jse.2011.03.006 [DOI] [PubMed] [Google Scholar]
- 26.Weber-Spickschen TS, Alfke D, Agneskirchner JD. The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: clinical and radiological results. Bone Jt J. 2015;97B(12):1662–1667. doi: 10.1302/0301-620X.97B12.35176 [DOI] [PubMed] [Google Scholar]
- 27.Aveledo R, Holland P, Thomas M, Ashton F, Rangan A. A comparison of the minimum data sets for primary shoulder arthroplasty between national shoulder arthroplasty registries. Is international harmonization feasible? Shoulder Elb. 2019;11(2):48–55. doi: 10.1177/1758573218755569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhandari M, Smith J, Miller LE, Block JE. Clinical medicine insights : arthritis and musculoskeletal disorders clinical and economic burden of revision knee arthroplasty. 2012;5:89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vanhegan IS, Malik AK, Jayakumar P, Islam SU, Haddad FS. A financial analysis of revision hip arthroplasty - the economic burden in relation to the national tariff. Bone Jt J. 2012;94(5):619–623. doi: 10.1302/0301-620X.94B5.27073 [DOI] [PubMed] [Google Scholar]
- 30.Postler AE, Beyer F, Wegner T, et al. Patient-Reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int. 2017;27(2):180–186. doi: 10.5301/hipint.5000436 [DOI] [PubMed] [Google Scholar]
- 31.Lenguerrand E, Whitehouse MR, Wylde V, Gooberman-hill R, Blom AW. Pain and function recovery trajectories following revision hip arthroplasty : short- term changes and comparison with primary hip arthroplasty in the ADAPT cohort study. PLoS One. 2016;11(10):e0164839. doi: 10.1371/journal.pone.0164839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burn E, Liddle AD, Hamilton TW, et al. Cost-effectiveness of unicompartmental compared with total knee replacement: a population-based study using data from the national joint registry for England and Wales. BMJ Open. 2018;8(4):1–8. doi: 10.1136/bmjopen-2017-020977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elb Surg. 2004;13(6):599–603. doi: 10.1016/j.jse.2004.03.016 [DOI] [PubMed] [Google Scholar]
- 34.Sheth MM, Sholder D, Getz CL, Williams GR, Namdari S. Revision of failed hemiarthroplasty and anatomic total shoulder arthroplasty to reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2019;28(6):1074–1081. doi: 10.1016/j.jse.2018.10.026 [DOI] [PubMed] [Google Scholar]
- 35.Sayers A, Evans JT, Whitehouse MR, Blom AW. Are competing risks models appropriate to describe implant failure? Acta Orthop. 2018;89(3):256–258. doi: 10.1080/17453674.2018.1444876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stone MA, Noorzad AS, Namdari S, Abboud J. Prosthetic bearing surfaces in anatomic and reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2021;29(10):414–422. [DOI] [PubMed] [Google Scholar]
- 37.Cointat C, Raynier JL, Lareyre F, Raffort J, Gauci MO, Boileau P. Short-term outcomes and survival of pyrocarbon hemiarthroplasty in the young arthritic shoulder. J Shoulder Elb Surg. 2022;31(1):113–122. doi: 10.1016/j.jse.2021.06.002 [DOI] [PubMed] [Google Scholar]
- 38.Garret J, Harly E, Le Huec JC, Brunner U, Rotini R, Godenèche A. Pyrolytic carbon humeral head in hemi-shoulder arthroplasty: preliminary results at 2-year follow-up. JSES Open Access. 2019;3(1):37–42. doi: 10.1016/j.jses.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bell SN, Christmas MUSI, Coghlan JA. Proximal humeral osteolysis and glenoid radiolucent lines in an anatomic shoulder arthroplasty: a comparison of a ceramic and a metal humeral head component. J Shoulder Elb Surg. 2020;29(5):913–923. doi: 10.1016/j.jse.2019.09.032 [DOI] [PubMed] [Google Scholar]
- 40.Mueller U, Braun S, Schroeder S, et al. Influence of humeral head material on wear performance in anatomic shoulder joint arthroplasty. J Shoulder Elb Surg. 2017;26(10):1756–1764. doi: 10.1016/j.jse.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 41.Ravi V, Murphy RJ, Moverley R, Derias M, Phadnis J. Outcome and complications following revision shoulder arthroplasty. Bone Jt Open. 2021;2(8):618–630. doi: 10.1302/2633-1462.28.BJO-2021-0092.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goodman SM, Mehta B, Mirza SZet al. Patients’ perspectives of outcomes after total knee and total hip arthroplasty: a nominal group study. BMC Rheumatol. 2020;4(3). doi: 10.1186/s41927-019-0101-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lowe JT, Menendez ME, Dasti U, et al. Patient age affects expectations and outcomes in primary total shoulder arthroplasty for glenohumeral osteoarthritis. Semin Arthroplast JSES. 2020;30(1):50–55. doi: 10.1053/j.sart.2020.04.006 [DOI] [Google Scholar]
- 44.Deere K, Whitehouse MR, Kunutsor SKet al. et al. How long do revised and multiply revised knee replacements last? A retrospective observational study of the national joint registry. Lancet Rheumatol. 2021; 3(6):e438–e446 doi: 10.1016/S2665-9913(21)00079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matthews AH, Marks T, Evans JT, Toms AD, Evans JP. What is the patient experience following revision knee replacement: a systematic review and meta-analysis of the medium term patient reported outcomes. Knee. 2022;35(1):34–44 doi: 10.1016/j.knee.2022.02.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sea-10.1177_24715492221095991 for Revision Shoulder Hemiarthroplasty and Total Shoulder Arthroplasty A Systematic Review and Meta-Analysis by Andrew Davies, Hussain Selmi, Sanjeeve Sabharwal, Martinique Vella-Baldacchino, Alex D. Liddle and Peter Reilly in Journal of Shoulder and Elbow Arthroplasty