Abstract
Sarcoidosis is a chronic multisystemic granulomatous disease of unknown origin, with variable clinical manifestations and various types of cutaneous manifestations (1). Plaque sarcoidosis that presents as an annular pattern is called annular sarcoidosis. Here, we report an unusual case of annular sarcoidosis with a geographic pattern containing Cutibacterium (Propionibacterium) acnes (C. acnes).
CASE REPORT
A 78-year-old woman visited our department because of an expanding erythema on her forehead for 7 years. She had been suffering from diabetes and hypertension. She also had glaucoma secondary to uveitis for 5 years. Physical examination revealed annular erythema with a geographic appearance on her forehead (Fig. 1a). The skin within the confines of the annular erythema was slightly atrophic. The biopsy specimen from the erythematous ridge of the exanthem showed epithelioid granuloma with slight lymphocytic infiltration in the upper dermis, whereas the biopsy specimen from the inner part of the annular erythema showed mild fibrosis without granuloma or lymphocytic infiltration (Fig. 1b, Fig. 2a, b). Bilateral hilar lymphadenopathy was found on chest computed tomography scan. No apparent abnormality was found on electrocardiogram. The serum level of angiotensin converting enzyme was within normal limits, while the serum levels of lysozyme (11.0 μg/ml; normal range, 3.4–8.6 μg/ml) and soluble interleukin-2 receptor (866 U/ml; normal range, 145–519 U/ml) were slightly elevated. We diagnosed her condition as sarcoidosis with involvement of the lung, eyes, and skin. A treatment with topical tacrolimus gradually relieved the patient’s exanthema, and her rash completely disappeared. Eventually, the exanthema and the bilateral hilar lymphadenopathy gradually resolved without systemic treatment.
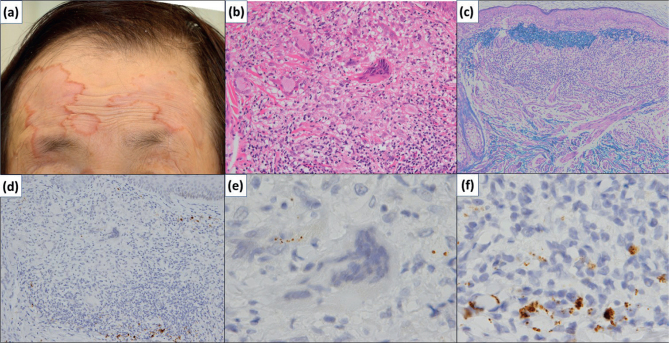
Fig. 1.
Macroscopic and histopathologic findings of the biopsy specimen from the raised border of the exanthem. (a) Macroscopically, the erythema on the face presents as fused annular lesions, resulting in a geographic pattern. (b) The peripheral raised border contains an epithelioid granuloma with giant cells in the upper and middle dermis layers (H&E stain, original magnification ×200). (c) There are fragmented elastic fibres around the granuloma of the peripheral lesion, but there is no apparent elastophagocytosis (VB stain, original magnification ×100). (d) Immunohistochemical staining with PAB antibody reveals small round bodies within the granulomas of the raised border. (e) Small round bodies are seen in the giant cells suggesting phagocytosis of Cutibacterium acnes. (f) Small round bodies in the granuloma are seen [immunohistochemical staining with PAB antibody, original magnification ×200 (d), ×1,000 (e, f)].
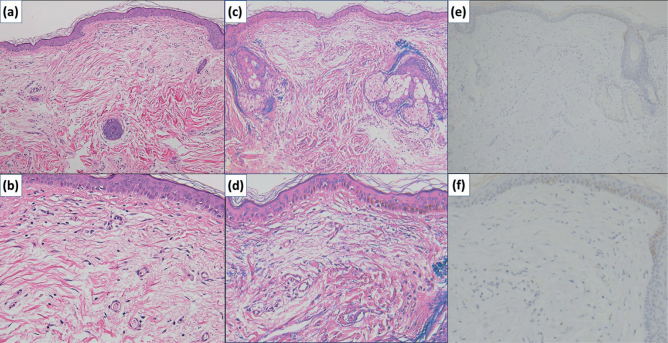
Fig. 2.
Histopathologic findings of the biopsy specimen from the central region of the exanthem. (a, b) Mild fibrosis is seen in the upper dermis [H&E stain, original magnification ×100 (a) and ×200 (b)]. (c, d) In the upper dermis, the elastic fibres are less and fragmented. In the periadnexal areas, aggregation of fragmented elastic fibres is seen [VB stain, original magnification ×100 (c) and ×200 (d)]. (e, f) Small round bodies, which suggest the presence of Cutibacterium acnes, are absent in the central region of the exanthem [immunohistochemical staining with PAB antibody, original magnification ×100 (e, f)].
To clarify the target of the granulomatous reaction in the cutaneous lesion of this case, Victoria blue (VB) staining and immunohistochemical staining with C. acnes-specific monoclonal antibody (PAB antibody), which specifically reacts with the C. acnes cell membrane, were performed on the skin biopsy specimens (2, 3). VB stain of the biopsy specimen of the peripheral lesion revealed fragmented elastic fibres around the granuloma but not in the granuloma itself (Fig. 1c). On the other hand, the biopsy specimen from the inner lesion showed decreased elastic fibres, which were also fragmented, in the upper dermis (Fig 2c, d). Immunohistochemical staining with PAB antibody revealed small round bodies within the granulomas of the peripheral lesion, suggesting phagocytosis of C. acnes (Fig. 1c–e). These small round bodies were not found in the inner lesion (Fig. 2e, f). Therefore, in this case, we presumed that the target of the granulomatous reaction in the exanthem was C. acnes.
DISCUSSION
Annular sarcoidosis is a rare subtype of cutaneous sarcoidosis. Although its exact prevalence rate is unknown, annular sarcoidosis was reported to account for 8% of the cases of cutaneous sarcoidosis in an Indian population (4). However, majority of the previously reported cases did not present with coalescent annular sarcoidosis (5, 6). In the case presented here, the cutaneous lesions showed annular and unusual geographic patterns.
To the best of our knowledge, this is the first case report on annular sarcoidosis with a geographic pattern. Annular elastolytic giant cell granuloma (AEGCG) is one of the differential diagnoses for annular sarcoidosis. The most apparent pathologic difference between AEGCG and annular sarcoidosis is the target of the granulomatous reaction. Phagocytosis of C. acnes has been known to participate in the pathogenesis of sarcoidosis. On the other hand, AEGCG has been known to be a result of a granulomatous reaction to elastic fibres in the dermis and to occasionally accompany systemic sarcoidosis (7, 8). This case suggests that immunohistochemistry with PAB antibody can provide supporting information for the diagnosis of cutaneous sarcoidosis, especially in cutaneous sarcoidosis with an unusual geographic appearance.
REFERENCES
- 1.Bachmeyer C, Eguia B, Callard P, Moguelet P. Purpuric papulonodular sarcoidosis mimicking granulomatous pigmented purpura. Eur J Dermatol 2011; 21: 110–111. [DOI] [PubMed] [Google Scholar]
- 2.Asahina A, Miura K, Saito I, Oshikata C, Ishii N, Eishi Y. Cutaneous sarcoidosis with livedoid lesions: evidence of the involvement of Propionibacterium acnes. J Dermatol 2013; 40: 501–502. [DOI] [PubMed] [Google Scholar]
- 3.Takama H, Yanagishita T, Muto J, Ohshima Y, Takahashi E, Tsuzuki T, et al. Granulomatous pigmented purpuric dermatosis containing Propionibacterium acnes. Eur J Dermatol 2018; 28: 540–542. [DOI] [PubMed] [Google Scholar]
- 4.Mahajan VK, Sharma NL, Sharma RC, Sharma VC. Cutaneous sarcoidosis: Clinical profile of 23 Indian patients. Indian J Dermatol Venereol Leprol 2007; 73: 16–21. [DOI] [PubMed] [Google Scholar]
- 5.Zafer T, Burce C, Ebru Z, Zindanci I, Demir FT, Kavala M. Annular sarcoidosis mimicking granuloma annulare: a case report. North Clin Istanb 2014; 1: 114–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moche MJ, Glassman SJ, Modi D, Grayson W. Cutaneous annular sarcoidosis developing on a background of exogenous ochronosis: a report of two cases and review of the literature. Clin Exp Dermatol 2010; 35: 399–402. [DOI] [PubMed] [Google Scholar]
- 7.Berliner JG1, Haemel A, LeBoit PE, Pincus LB. The sarcoidal variant of annular elastolytic granuloma. J Cutan Pathol 2013; 40: 918–920. [DOI] [PubMed] [Google Scholar]
- 8.Hanke CW, Bailin PL, Roenigk HH Jr., Annular elastolytic giant cell granuloma. A clinicopathologic study of five cases and a review of similar entities. J Am Acad Dermatol 1979; 1: 413. [PubMed] [Google Scholar]