Abstract
A 58-year-old man was admitted for stable angina. The coronary angiogram revealed a coronary-pulmonary fistula with a nonsignificant atheroma. We decided to perform percutaneous embolization of the fistula in view of the symptoms and the hemodynamic assessment findings. Embolization was performed using a liquid embolic agent with no residual flow. (Level of Difficulty: Intermediate.)
Key Words: coronary artery fistula, fractional flow reserve, liquid embolic agent
Abbreviations and Acronyms: CAF, coronary artery fistula; CPAF, coronary-pulmonary artery fistula; FFR, fractional flow reserve; LAD, left anterior descending (coronary artery); LEA, liquid embolic agent
Central Illustration

History of Presentation
A 57-year-old man was admitted to our department (European Hospital of Paris, La Roseraie, Aubervilliers, France) for typical angina with symptoms present for 2 months. Cardiac auscultation revealed normal first and second heart sounds without murmurs.
Learning Objectives:
-
•
To assess the hemodynamic impact of a coronary fistula by using FFR.
-
•
To show the feasibility of embolization with a liquid agent in a coronary fistula.
Past Medical History
The patient had current smoking as a risk factor of atherosclerosis and a history of coronary artery disease with chronic obstructive pulmonary disease.
Differential Diagnosis
The differential diagnosis included myocardial ischemia, microvascular angina, or noncardiac chest pain (esophageal).
Investigations
The electrocardiogram did not show any significant repolarization disorder, and the chest radiograph revealed a normally shaped heart without dilation and normal pulmonary vascularity. The transthoracic echocardiogram indicated that the cardiac structure and function were normal, without an abnormal shunt. Considering the cardiovascular risk factors and the typical characteristics of the symptoms, the decision was made to perform diagnostic coronary angiography, which revealed a nonsignificant atheroma and 1 coronary-pulmonary fistula (CPAF) originating from the middle left anterior descending (LAD) coronary artery and draining into the pulmonary artery (Figure 1, Videos 1 and 2).
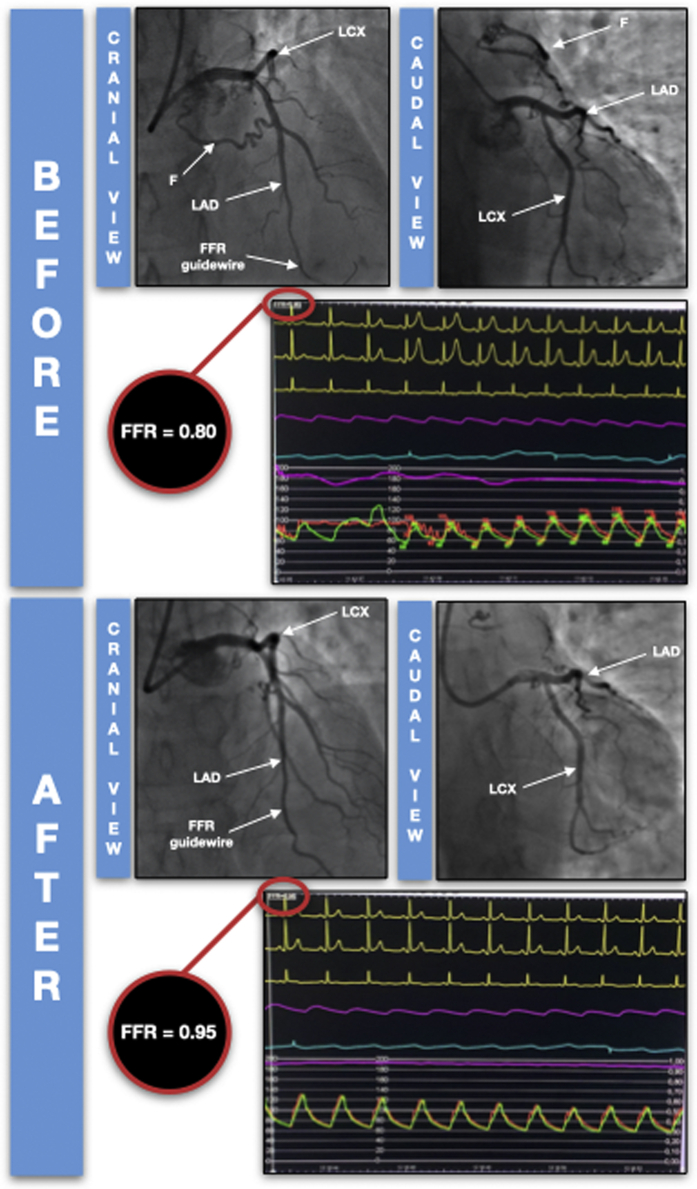
Figure 1.
Coronary Angiograms and FFR Assessment Before and After Embolization of the Fistula
F = fistula; FFR = fractional flow reserve; LAD = left anterior descending (artery); LCx = left circumflex (artery).
Management
Given these findings, treatment options were discussed by the heart team. Surgical treatment was discarded, and the indication for embolization of the fistula was retained after proof of myocardial ischemia by fractional flow reserve (FFR). A right radial 7-F approach was selected, and a 7-F guiding catheter was used to catheterize the left main coronary artery. A pressure guidewire was positioned at the distal LAD artery. The FFR in this site was 0.80 under maximal hyperemia. Selective catheterization of the fistula was performed using a microcatheter and a microguide. After checking the position and stability of the microcatheter with hand iodinated contrast injection, the microcatheter was flushed with physiologic saline to clear the contrast material; the microcatheter dead space and hub were then filled with 0.34 mL of dimethyl sulfoxide. Slow injection of 0.4 mL of a liquid embolic agent (LEA), was performed under subtracted fluoroscopy. After a period of 5 minutes, necessary for the copolymerization and solidification of the LEA, a control angiogram was performed through the guiding catheter and showed an excellent final result with no residual flow in the fistula (Figure 1, Videos 3 and 4). Finally, we performed a new pressure measurement under maximal hyperemia that revealed a clear improvement with an FFR at 0.95. After the procedure, the subsequent clinical course was uneventful, and the patient was discharged the next day with aspirin, 100 mg/d. The patient felt that his symptoms were relieved and reported the absence of any discomfort during the 1-year follow-up period.
Discussion
A coronary artery fistula (CAF) is a congenital or acquired abnormal vascular communication of coronary arteries with cardiac chambers or any segment of the systemic or pulmonary circulation. CAFs are uncommon, accounting for 0.3% of congenital heart diseases.1 Although most patients with CAF are asymptomatic or have an incidental diagnosis, angina is the most frequent symptom in patients presenting with symptoms. In patients presenting with ischemic symptoms caused by fistula in the absence of coronary artery disease, the proposed explanation for this discrepancy between the clinical symptoms and anatomical findings is the theory of the “coronary steal phenomenon,” with coronary blood preferentially passing through the fistula instead of more distal myocardial capillaries.2 The diagnosis and functional assessment of CAFs are challenging. Myocardial perfusion single photon-emission computed tomography was performed in many previous studies to demonstrate fistula-related myocardial ischemia in patients with CAF.3,4 Myocardial perfusion positron emission tomography with better spatial resolution and sensitivity may be a promising tool to evaluate myocardial ischemia in patients with CPAF.3,5 The use of FFR to interrogate the functional significance of CAF is not new. Some cases of FFR use to assess the functional severity of the CAF alone or in combination with coexisting de novo mild to moderate coronary lesions have been reported.6,7 A low FFR indicates the presence of myocardial ischemia associated with anatomically normal vessels. At maximum hyperemia, a coronary steal phenomenon can be manifested, especially if the donor vessel supplies the territory of a dominant vessel. Härle et al6 demonstrated that the FFR under maximal hyperemia improved in the donor vessel when the fistula was temporarily occluded with a balloon; thus, it was assumed that FFR measurement is a feasible means of diagnosing functional severity in patients with possible coronary steal. In our case, we performed an FFR measurement under maximal hyperemia without temporary balloon occlusion of the fistula, and it was positive at 0.80. A clear improvement in the FFR value (at 0.95) was observed after closure of the fistula, and this allowed us to conclude that the coronary steal resulting from the fistula was hemodynamically significant. The American College of Cardiology and American Heart Association 2008 guidelines recommend intervening in all large fistulas, irrespective of whether symptoms are present, and in small to medium fistulas in patients with symptoms.8 Several percutaneous options are available using coils or occluders. Currently, an LEA is usually used in combination with coils for embolization of brain vascular malformations,9 and the first successful percutaneous treatment of a CAF with an LEA embolization system worldwide was performed by Tchantchaleishvili et al.10 In the case reported here, we planned the use of coils as a secondary bailout embolization technique in case we had unsatisfactory results with an LEA. Of note, the cost of a detachable coil system is higher than that of an LEA ampule, especially if multiple coils were to be used.
Follow-Up
After the procedure, the subsequent clinical evolution was uneventful, and the patient was discharged the next day with aspirin, 100 mg/d. The patient felt that his symptoms were relieved and reported the absence of any discomfort during the 1-year follow-up period.
Conclusions
Even though it is a rare anomaly, CAF can cause a coronary steal phenomenon that can be objectively evaluated by FFR. Percutaneous closure of a CAF has become the preferred method of treatment, and the LEA system is a promising embolic agent that could be safely used.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Coronary-Pulmonary Fistula Originating From the Middle LAD Coronary Artery: Caudal View
Coronary-Pulmonary Fistula Originating From the Middle LAD Coronary Artery: Cranial View
Final Result of Embolization: Cranial View
Final Result of Embolization: Caudal View
References
- 1.Vavuranakis M., Bush C.A., Boudoulas H. Coronary artery fistulas in adults: incidence, angiographic characteristics, natural history. Cathet Cardiovasc Diagn. 1995;35:116–120. doi: 10.1002/ccd.1810350207. [DOI] [PubMed] [Google Scholar]
- 2.Latson L.A. Coronary artery fistulas: how to manage them. Catheter Cardiovasc Interv. 2007;70:110–116. doi: 10.1002/ccd.21125. [DOI] [PubMed] [Google Scholar]
- 3.Said S.A., Nijhuis R.L., Akker J.W., et al. Unilateral and multilateral congenital coronary-pulmonary fistulas in adults: clinical presentation, diagnostic modalities, and management with a brief review of the literature. Clin Cardiol. 2014;37:536–545. doi: 10.1002/clc.22297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Said S.A., van der Werf T. Dutch survey of coronary artery fistulas in adults: congenital solitary fistulas. Int J Cardiol. 2006;106:323–332. doi: 10.1016/j.ijcard.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 5.Said S.A., Nijhuis R.L., Op den Akker J.W., et al. Diagnostic and therapeutic approach of congenital solitary coronary artery fistulas in adults: Dutch case series and review of literature. Neth Heart J. 2011;19:183–191. doi: 10.1007/s12471-011-0088-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Härle T., Kronberg K., Elsasser A. Coronary artery fistula with myocardial infarction due to steal syndrome. Clin Res Cardiol. 2012;101:313–315. doi: 10.1007/s00392-011-0405-1. [DOI] [PubMed] [Google Scholar]
- 7.Hollenbeck R.D., Salloum J.G. Sequential moderate coronary artery fistula and moderate coronary artery stenosis causing ischemia demonstrated by fractional flow reserve and relieved following percutaneous coronary intervention. Catheter Cardiovasc Interv. 2014;83:443–447. doi: 10.1002/ccd.25170. [DOI] [PubMed] [Google Scholar]
- 8.Warnes C.A., Williams R.G., Bashore T.M., et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e143–e263. doi: 10.1016/j.jacc.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Dabus G., Pizzolato R., Lin E., Kreusch A., Linfante I. Endovascular treatment for traumatic scalp arteriovenous fistulas: results with Onyx embolization. J Neurointerv Surg. 2014;6:405–408. doi: 10.1136/neurintsurg-2013-010724. [DOI] [PubMed] [Google Scholar]
- 10.Tchantchaleishvili V., Becerra-Gonzales V., Fernandez G., Mieszczanska H.Z., Jahromi B.S., Cove C.J. Embolization of cardiac arteriovenous malformation with onyx. J Am Coll Cardiol Intv. 2015;8:e39–e40. doi: 10.1016/j.jcin.2014.10.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronary-Pulmonary Fistula Originating From the Middle LAD Coronary Artery: Caudal View
Coronary-Pulmonary Fistula Originating From the Middle LAD Coronary Artery: Cranial View
Final Result of Embolization: Cranial View
Final Result of Embolization: Caudal View