Abstract
The COVID-19 pandemic has been experienced as the most significant global disaster after the Spanish flue in 1918. Millions of people lost their life due to a lack of preparedness and ineffective strategies for managing humanitarian supply chains (HSC). Based on the learnings from this pandemic outbreak, different strategies for managing the effective HSC have been explored in the present context of pandemics through a systematic literature review. The findings highlight some of the major challenges faced during the COVID-19 pandemic, such as lack of planning and preparedness, extended shortages of essential lifesaving items, inadequate lab capacity, lack of transparency and visibility, inefficient distribution network, high response time, dependencies on single sourcing for the medical equipment and medicines, lack of the right information on time, and lack of awareness about the protocol for the treatment of the viral disease. Some of the significant learnings observed from this analysis are the use of multiple sourcing of essential items, joint procurement, improving collaboration among all stakeholders, applications of IoT and blockchain technologies for improving tracking and traceability of essential commodities, application of data analytics tools for accurate prediction of next possible COVID wave/disruptions and optimization of distribution network. Limited studies are focused on finding solutions to these problems in managing HSC. Therefore, as a future scope, researchers could find solutions to optimizing the distribution network in context to pandemics, improving tracing and tracking of items during sudden demand, improving trust and collaborations among different agencies involved in HSC.
Keywords: COVID-19, Humanitarian supply chains, Poverty and food security, Swift trust, Prepositioning, Coordination, Collaboration, Systematic literature review
Introduction
The COVID-19 pandemic has caused many disruptions in business and society. It may be considered as the most severe pandemics of this century. Pandemics differ from other disasters in complicacy, information needs and types, the pace of change and impact, and impact for an extended period (Thompson & Anderson, 2021). Pandemics may result in social and economic disruption due to sudden illness and mortality. In general, humanitarian logistics and supply chain management (HLSCM) mainly focus on lifesaving operations after a natural disaster (Kunz & Reiner, 2012). Sokat and Atlay (2021) have highlighted the uniqueness of the vulnerable groups and conducted a literature review to identify the research needs in HLSCM. They observed that no literature is available within the HLSCM that focuses on the uniqueness of the vulnerable groups, risk factors, and the way to mitigate them. The vulnerable people are at high risk of this pandemic, as they do not have proper access to healthcare and social services. Till August 30, 2021, the outbreak of COVID-19 has affected 221 countries of the world and caused the death of millions of the people (Worldometers, 2021). It has a global impact on most countries’ socio-economic conditions due to the lockdown, social distancing, logistics disruption, export–import disruption, and supply and distribution uncertainties. The outbreak of COVID-19 poses a significant challenge for the humanitarian organization to address the various issues related to the relief operations.
The severity of different pandemics depends on their novelty and uniqueness. Various strains of the coronavirus have been found across the world. COVID-19 is the seventh identified coronavirus infecting humans’ respiratory tract and lungs in the last two decades (Burki, 2020). The fungal infection of the sinuses is challenging to treat and is often fatal (BMJ, 2021). Yet, COVID-19 is not fully understood, and some precautions such as social distancing, lockdowns, stay-at-home, use of mask and sanitizer have been prescribed. However, many vaccines are in use, but the effectiveness of the vaccinations is not yet evident. The different companies claim effectiveness as per their experimentation and observation.
Including health and medical issues, COVID-19 has restricted many business and personal activities of the people such as tourism, education, export–import, production, social gathering, movement, etc. The changing demand pattern has affected demand forecasting, manufacturing and supply lead time, inventory management, sourcing strategies, etc. Karuppiah et al. (2021) reviewed the impact of COVID-19 on health, economic, social, and industrial activities. They identified twenty critical challenges in sustainable humanitarian supply chain management. The analysis found the five most significant challenges: problem in facility location, short lead time for emergency supply, the spread of rumours, the rapid emergence of new clusters, and doubt concerned with the available remedies. They recommended public–private partnership as the best strategy to meet these challenges.
Malmir and Zobel (2021) proposed a mathematical model for minimizing the total cost of delivering humanitarian aids for the pandemic relief, focusing on sustainable operations, total transportation and delivery costs, and equity and deprivation costs. They covered the social costs in their model in terms of deprivation and equity cost so that a manager could respond to the pandemic outbreaks in the best possible ways. Farooq et al. (2021) proposed a framework emphasizing the integration of Industry 4.0 technologies, resilience strategies, and sustainability to overcome the impact of the pandemic. Based on the exploration of the possible contribution of HSC in reducing the impact of COVID-19, the following research question is proposed.
RQ1 How does the HSC address the issues related to pandemic outbreak of COVID-19 to reduce the suffering of the people and fulfill their needs.
The ripple effect of COVID-19 has spread across the industry. It has a cascading effect extending through various sectors in a supply chain. The supply of essential items was utterly disrupted due to lockdown and worldwide restrictions on the free flow of goods and services (Ivanov, 2020a). Due to restrictions on export and import, businesses had to put the flow of raw material on hold, which led to a huge shortage of supply of the goods and increased the cost (Dolguiet al., 2020). On the other hand, sales were dramatically reduced due to decreased demand for many perishable items and uneven distribution (Magzter, 2020). Also, it led to the wastage of these items. The occurrence of the COVID-19 pandemic has exposed challenges of the humanitarian supply chain due to shortage and disruption of supplies of essential items such as PPEs (personal protective equipment), testing kits, ventilators, hospital beds, oxygen cylinders, and vaccines. A chaotic situation was observed due to poor communication, contradictory and insufficient information, confusion among first responders and citizens, and lack of resources. These issues led to slow relief, resulting in prolonged suffering and increased deaths. HSCs (Humanitarian Supply Chains) mainly focus on saving lives while responding to disasters and emergencies and are characterized by turbulence, uncertainties, and complex dynamic environments (Day et al., 2012; Van Wassenhove, 2006). Based on the difficulties in managing the HSC during the peak time of COVID-19, the following research question is proposed.
RQ2 What are the main challenges in managing HSC during the COVID-19 pandemic.
Due to restrictions on movement, over control/restriction on travel, shortages in labor and materials, COVID-19 became a serious threat to the life of human beings (Kumar & Singh, 2021a). Unlike SARS or even Ebola, the COVID-19 has disrupted global supply chains as well as humanitarian supply chains. Some of the main challenges influencing the performance of humanitarian supply chains are the poor resource infrastructure, high dependency on donor funding, demand uncertainty, and lack of resources (Kovacs & Spens, 2007; Balcik & Beamon, 2008; Gatignon et al., 2010). Limited research has been done on using insights emerging from COVID 19 for managing HSC. Thus, it is an opportunity to learn new scenarios emerging after the COVID-19 outbreak. Therefore, we are also trying to answer the following research question in our study.
RQ3 What are the learnings from COVID-19 for future research directions in context to HSC.
The recent episode of pandemic outbreak has increased the global burden on humanitarian efforts. The increasing role of HSC may be observed in the outbreaks of epidemics such as SARS (2002–03), Swine Flu-H1N1 virus (2009–10), Ebola (2015–16), MERS (2015–16), and now COVID-19 (2019 to present). In this paper, a systematic literature review (SLR) is used to make the required observations and determine future research directions. It has a long tradition to summarize the results of existing research and propose the hypothesis. The SLR has been recently used successfully in the HSCs context (Dubey et al., 2015; Marić et al., 2021; Queiroz et al., 2020).
The organization of the paper is as follows: Sect. 2 highlights the research methodology, Sect. 3 represents the findings and content analysis of the literature, Sect. 4 deals with learnings from COVID-19, Sect. 5 elaborates the research gaps and directions for future research. Section 5 concludes the research. This study will contribute to identifying new challenges during the pandemic and possible strategies for managing HSC during such uncertain times.
Research methodology
As a first step, the scope of the study considering the interdisciplinary approach is defined. Before exploring the literature on the research articles on the issues related to the pandemic outbreak, we used a grounded theory approach to understand participants’ observation toward COVID-19 and its impact. Grounded theory is based on the approach of naturalistic inquiry and inductive data analysis. Grounded theory discovers new theoretical insights and innovations avoiding the traditional logical deductive reasoning (Connell & Lowe, 1997); and it is considered to be “emergent explicit” (Martin & Woodside, 2008).
According to Nunkoo and Ramkissoon (2016), the sampling process in grounded theory research is based on concepts, properties, dimensions, and characteristics, not on the samples of specific groups and units of time. Due to lockdown and imposition of social distancing, it could not be possible to conduct face-to-face interviews of the participants, logisticians, and sufferers of COVID-19. Online interviews were conducted to know the opinion and observation of the people regarding the humanitarian issues. Interviews were conducted with 12 participants. Out of 12 participants, five experts were working as volunteers in humanitarian supply chains, four experts had suffered from COVID-19. They were cured after treatment, and three experts were working as medical practitioners. Many open-ended questions were asked from the experts, which are not generally found in the research article. Some important component of the research questions are the attitude and motivation of the medical practitioners to help the COVID-19 patients, unavailability of beds in hospitals, unavailability of medicines, lack of oxygen supply, shortage of ventilators, the effectiveness of home quarantine and telemedicine, unavailability of vaccines, food supply, etc. In addition, we also consulted many news articles, news channels, social media, etc.
The concept of the humanitarian supply chain and its application in epidemic/pandemic outbreaks have become more important for the last two decades. Its development is closely integrated with the development of supply chain management. Earlier, it was simply managed as disaster/relief management without using the Humanitarian supply chain or humanitarian logistics management concepts. In recent years, the outbreak of COVID-19 has been considered one of the most dangerous infectious diseases, which has led to the death of more than 4.51 million people worldwide, as shown in Table 1.
Table 1.
Some major epidemics/pandemics across the world
| Years/Duration | Name of the Epidemics/pandemics | Causes | Death (Approx) | Region | References |
|---|---|---|---|---|---|
| 2019- present | COVID-19 | Coronavirus | 4.51 M | Worldwide | Worldometers (2021) |
| 1981-present | HIV/AIDS | Virus/Chimpanzees | 25–35 M | Worldwide | Pandey and Galvani (2019) |
| 1968–1969 | Hong Kong Flu | Influenza A/H3N2 | 1–4 M | Worldwide | Akin and Gözel (2020) |
| 1918–1920 | Spanish flu | Influenza A/H1N1 | 40–50 M | Worldwide | Antonovics et al. (2006) |
| 1519–1520 | Mexico smallpox | Smallpox | 5–8 million | Mexico | Acuña-Soto et al. (2002) |
| 1346–1353 | Black Death | Bubonic plague | 75–200 M | Europ, Asia, North America | DeWitte (2014) |
| 541–549 | Plague of Justinian | Influenza A/H1N1 | 15–100 M | Europe and West Asia | Mordechai et al. (2019) |
| 165–180 | Antonine Plague | Smallpox or measles | 5–10 M | Roman Empire | Yapijakis (2009) |
For the systematic literature review, we have used the concepts of the grounded theory proposed by Wolfswinke et al. (2013). The entire literature review is divided into the following five steps.
Planning Grounded theory and literature review were planned to connect the humanitarian issues with the impact of COVID-19.
Identifying Some keywords such as an epidemic, pandemic, coronavirus, COVID-19, humanitarian supply chains, and humanitarian logistics were searched on the Scopus database.
Evaluating The research articles were sorted based on abstract reading and then final full paper readings.
Collecting/combining From these research articles sorted out from the literature is used to find out the challenges faced in Humanitarian supply chains during the outbreaks of COVID-19, and some significant learnings are outlined.
Explaining and summarizing Some major research gaps are identified, and directions of future research are proposed.
For ensuring the objectivity and reliability of the entire process, a research protocol is developed, as shown in Table 2 (Queiroz et al., 2020). In the second stage, based on the research protocol, many research articles were identified. Only those journals are retained that are indexed by Scopus. The conference papers are not included in this study. Both conceptual and empirical types of papers from the journals are considered in this literature review. Moreover, to extract data and explore the papers, the POP (Publish or Perish) software (De Rond & Miller, 2005) and VOSviewer (Yu et al., 2020) for network analysis are used. At a third stage, the main findings from the analysis of papers are reported. Using the systematic literature review (SLR) methodology, several insights are unveiled into the knowledge literature. Figure 1 highlights the main schematic flow diagram of the review process. Finally, we have shortlisted forty-six research papers for this SLR. Detail of these research papers is also given in Appendix 1. As this SLR is in context to current Covid 19 problem, we have also referred some news articles and reports as given in Appendix 2.
Table 2.
Research protocol for literature review
| S. no | Research protocol | Detailed description |
|---|---|---|
| 1 | Research database: | Scopus database |
| 2 | Publication type: | Peer-reviewed journals (Scopus Indexed) |
| 3 | Language: | English |
| 4 | Date Range: | January 2012- March 12, 2021 |
| 5 | Search filed: | Titles, abstracts, and keywords |
| 6 | Search terms applied in Titles in Scopus database and titles, abstract, and keywords in POP: | “Epidemic” OR “pandemic” OR “COVID 19” or “coronavirus” AND “humanitarian supply chains” |
| 7 | Criteria for inclusion: | Papers that presented some outbreaks in a humanitarian context |
| 8 | Criteria for exclusion: | Papers that presented some outbreak discussion purely without humanitarian concern |
| 9 | Data and network analysis: | Used VOSviewer software |
Fig. 1.
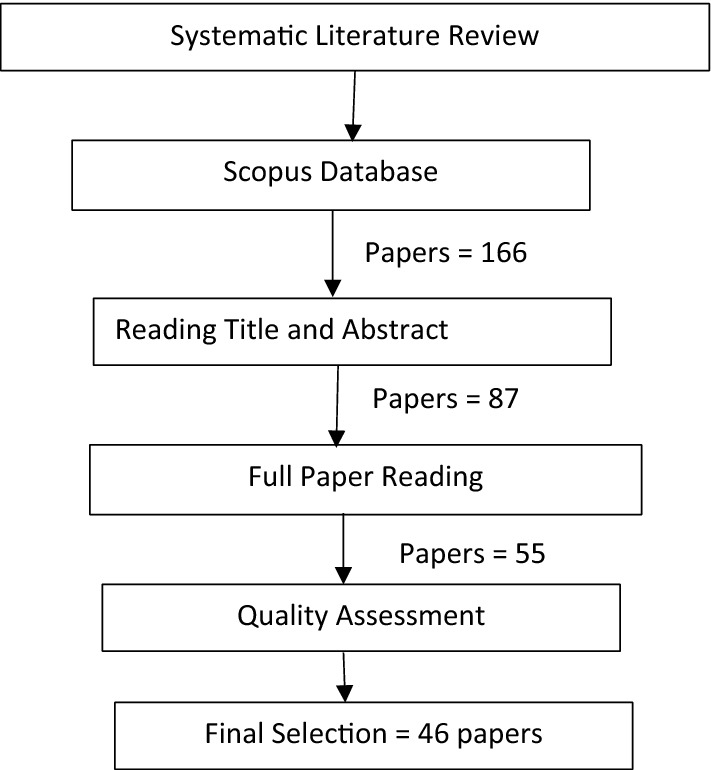
Research protocol for SLR
Research findings and analysis
Research findings have been analyzed in two parts. The first part deals with descriptive analysis, and the second part deals with theoretical analysis.
Descriptive analysis
In this section, we are trying to do a descriptive analysis of papers published in different journals in area of study. Figure 2 shows the number of research articles published in each journal. It is observed that Annals of Operations Research (ANOR) has published the highest number of research papers. Apart from ANOR, the Journal of Humanitarian Logistics and Supply Chain Management (JHLSCM) also represents most publications in this domain. Other journals publishing articles related to the pandemic and humanitarian supply chains are Benchmarking: An International Journal, International Journal of Production Economics, International Journal of Production Research, International Journal of Information Management, Journal of Supply Chain Management, and Transportation Research Part E. Although, many journals have published articles related to pandemics, but their focus is entirely different from humanitarian issues. Some journal focuses on medicines and others on operations and supply chains and some other issues. Therefore, we have mainly considered publications related to pandemics.
Fig. 2.
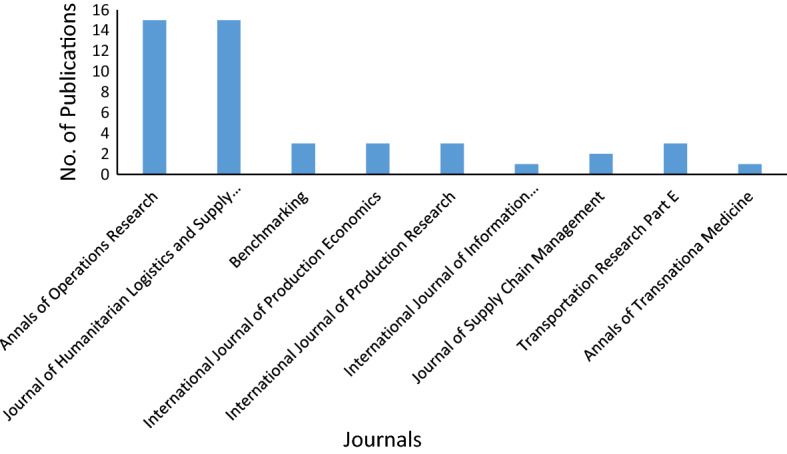
Publications by journals
Figure 3 shows the network visualization of authors and co-authors. Humanitarian Supply Chain Management is a relatively new area of research. Very few authors have contributed to the research in this area. It can be observed that most of the publications related to the humanitarian issues in pandemics have been published within two years (2020–21). Figure 4 shows the year-wise publication of the articles related to Humanitarian supply chains and pandemics.
Fig. 3.
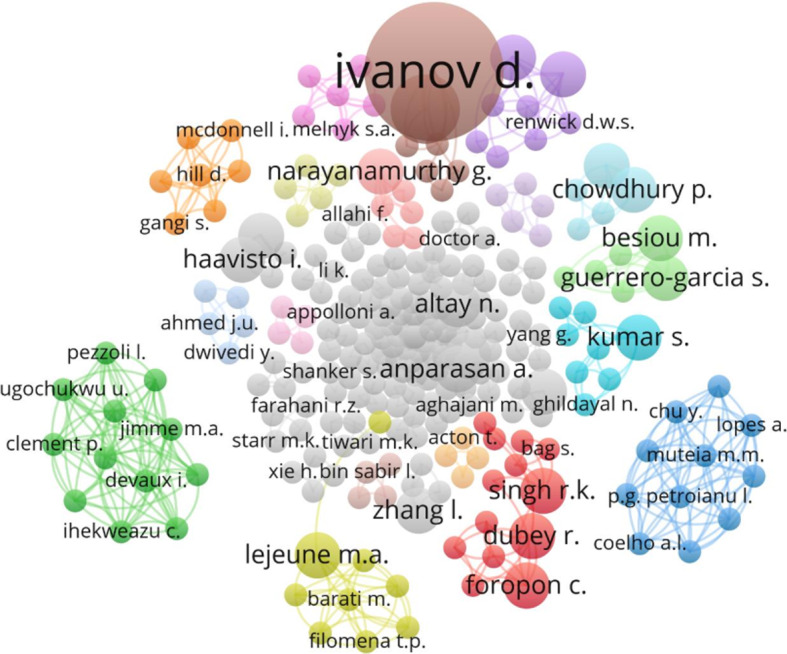
Network visualization of authors and co-authors
Fig. 4.
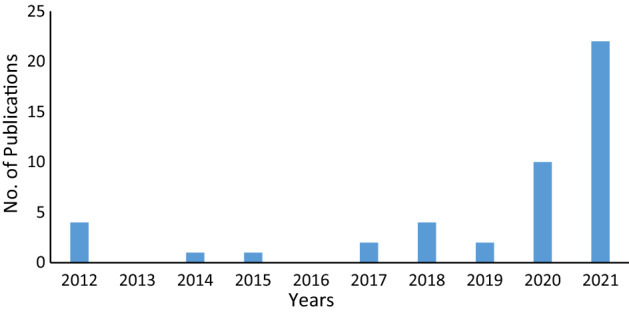
Year-wise publications
Similarly, if the publications are analyzed in terms of countries, the US is first in this dimension, followed by the United Kingdom and India, as shown in Fig. 5. Other leading countries publishing the articles on HLSCM and Pandemics are Germany, France, China, Australia, Brazil, Italy, Iran, and Norway.
Fig. 5.
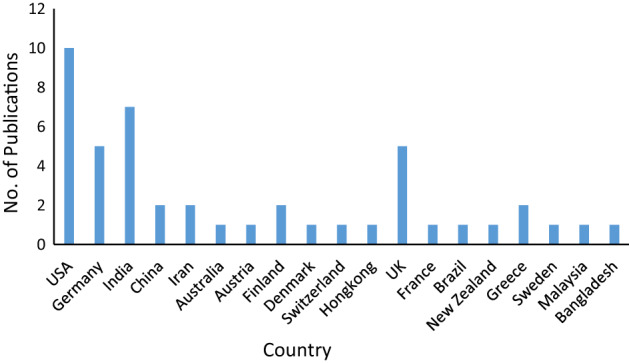
Publications by different countries
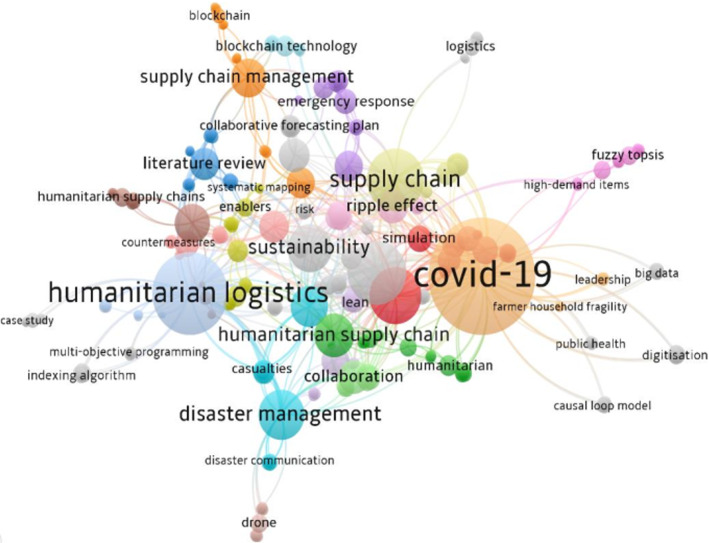
Figure 6 shows keyword dynamics. These are acquired from the titles of references from our dataset of 46 papers considered for review. In this word treemap, the size of circles shows the frequency of keywords, and the color indicates the relationship between them. The role of word segments such as “COVID-19,” “humanitarian logistics,” “supply chain,” “disaster management,” “supply chain management,” and “humanitarian supply chains” is reasonably identifiable. In the other smaller sizes of circles, various other related words such as “ripple effect,” “sustainability,” “collaboration,” and “countermeasure” are shown.
Fig. 6.
Keyword dynamics using VOS viewer
There is a trend to use Coronavirus and COVID-19 interchangeably, but we can also notice the growth of other interesting topics related to “Coronavirus and COVID-19”, such as “emergency response,” “disaster communication,” “causalities,” and “collaborative forecasting.” In the other smaller size circles, we have many related terms. Taking into account the word dynamics, we observe, “COVID 19” and “Humanitarian Logistics” are well-explored topics due to their variations (e.g., disaster management, emergency response, risks, countermeasures, etc.).
Theoretical underpinning
In this study, we have tried to analyze mainly challenges faced by HSC during COVID-19 and possible learnings after these challenges.
Challenges in HSC during COVID-19
From an exhaustive literature review of recent research articles, we have tried to identify and analyze challenges in humanitarian supply chains observed during COVID-19 as follows:
-
(i)
Lack of planning and preparedness 2020 is known as the year of testing pandemic preparedness. Failure to contain the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exposed the unpreparedness of different agencies involved in HSC. SARS-CoV-2 probably leaked over to humans and caused a pneumonia outbreak in Wuhan (Hubei, China) in December 2019 (Villa et al., 2020). In the case of the COVID-19 outbreak, the timely reporting by China was not followed, and the governments across different countries overlooked the menace posed by COVID-19. It was observed that many governments were not adequately prepared to respond and address the issues of the COVID-19 pandemic (Lancet, 2020). They missed a strategic plan for the pandemic response ready to be adapted and implemented against the threat of COVID-19. There is the need to establish a proper national preparedness plan even if the next pandemic may not appear for some years. The lack of a national response strategy led a mass confusion among the responders at the federal, state, and local levels of different governments. The Centres for Disease Control and hospitals did not anticipate the nature of the virus and so could not respond adequately.
-
(ii)
Extended shortages During the first wave of COVID 19, all hospitals and health centers were facing a shortage of various medical equipment such as N95 masks and PPE Kits, among others. Even after one year of the COVID outbreak, i.e., during the second wave of COVID-19 in India, the hospitals were facing a shortage of oxygen supply, beds, ventilators, and vaccines. Many other countries were also facing similar problems but not so acute. Even in the developed countries like the US, the Department of Health and Human Services resonated with the urgent calls from hospitals for more PPEs, as they expected their stocks’ depletion as cases continued to increase (HHS, 2020). Delay of 3–6 months for N95 masks was reported, and supply was insufficient per demand (CBS News, 2020a, b in Appendix 2). Due to high demand and less production of vaccines and stage-wise supply of the vaccines for a different category of the people, the distribution of the vaccines becomes very difficult and results in a shortage of supply.
-
(iii)
Inadequate lab capacity In March 2020, India had only 14 RT-PCR testing labs, and by the end of the month, 106 Virus Research & Diagnostic Laboratories (VRDLs) were added. By July 2020, India had 1600 RT-PCR labs. The number of daily tests shot up from 1500 in April to 200,000 in June and 1 million in October 2020. The first wave of COVID-19 subsided in November; at that time, India had only 2257 COVID-19 testing labs. The average waiting time for getting test results was 12–24 h. However, from December 2020 to May 2021, only 249 new COVID-19 testing labs were added. With the alarming spread of the virus in the second wave, the country's labs could not give results within the same time frame of 12–24 h. Labs across different cities of India such as Delhi, Mumbai, Noida, Lucknow, and Kolkata were taking an average of 3–5 days to give test results (Acharjee, 2021 in Appendix 2). Similar situations were also observed in the US. Many people needing testing had to wait for more than a week to receive the diagnosis and its report. In some cases, testing was too late. In Denver, the state testing lab, including other labs, ran out of testing kits, and a shipment was delayed (Doyle, 2020 in Appendix 2). Many countries were facing a shortage of testing kits and inadequate lab capacity during 2020–21.
-
(iv)Lack of supply of COVID-19 vaccines COVID-19 vaccines have brought a ray of hope to people for returning to normalcy after a long period of lockdown (Warren & Lofstedt, 2021). Many manufacturing companies are trying to develop, manufacture, and fulfill the need for COVID-19 vaccines (Kim et al., 2021). The volume required for the vaccines is very high, considering, on average, two doses for each individual. To cover vaccination for 100% of the world’s population, it is approximated that 16–20 billion doses are required for the current population of approximately 7 billion (Rele, 2021). The development of vaccines requires considerable time because they must be effective and safe (Singh & Mehta, 2016).Availability of vaccines is critical to reducing the potential losses from the pandemic. Governments and academic institutions will have to plan to make the availability of vaccines for the general public (Ocampo & Yamagishi, 2020). The bottlenecks in the development and deployment of the vaccines are to be removed (Rele, 2021). Guttieres et al. (2021) and Abbasi et al. (2020) proposed a framework for COVID-19 vaccination strategies considering the allocation and distribution of the COVD-19 vaccines. The three main phases of vaccines manufacturing are development, dissemination, and distribution (Forman et al., 2021). These three phases are composed of ensuring the continued growth of vaccine candidates, authorization, production, distribution, administering, and monitoring existing vaccines.
-
(v)Lack of awareness and hesitancy in acceptance of the vaccines The success of any vaccination drive depends on its coverage and acceptance rate (Pogue et al., 2020). There might be different concerns of the people regarding the vaccines (Dror et al., 2020). For wide coverage of the population by vaccination and to avoid hesitancy towards the vaccine, it is necessary to understand peoples’ views regarding the vaccine. In the first phase of the COVID-19 vaccination, the healthcare and frontline workers were hesitant to receive the vaccine due to many reasons (The Wire, 2021 in Appendix 2).Experience shows that the uptake of vaccines is more complex. Vaccine uptake and the wider acceptance of vaccines is a social endeavor that requires consideration of human factors. Sponsors need to do critical investigations on human factors related to vaccine acceptance and for public health authorities and other stakeholders to act on this research’s social and behavioral findings (Schoch-Spana et al., 2020).
-
(vi)
Need for Home-based-primary care services Due to mass suffering from COVID-19 and insufficient facilities in hospitals, the governments started to provide home-based primary care (HBPC) services. Also, a large section of the population is either homebound or needs the assistance of another person to leave their homes (Ornstein et al., 2015). In this situation, HBPC provides facilities for such patients to access the required medical care in their homes (Stall et al., 2014; Totten et al., 2016). HBPC reduces the emergency department visits, minimizes the iatrogenic COVID-19 exposure, boosts COVID-19 testing, addresses chronic medical issues, and prevents the escalation of the diseases. Since a large number of hospitals are declared as COVID hospitals (Pisano et al., 2020). The main challenges observed in HBPC are lack of familiarity of the patients with telemedicine, patient anxiety, clinician anxiety, technical difficulties in reaching the patients, and supply shortages, including masks, gowns, and disinfecting materials (Ritchie, 2021).
-
(vii)
Lack of application of advanced technologies Some advanced technologies are available that can be used to mitigate the risk related to the COVID-19. Abd-alrazaq et al. (2020) suggested the use of blockchain technology to fight against the COVID-19. According to them, no comprehensive reviews were conducted to uncover the blockchain solutions to improve the public health efforts against COVID-19. The most prominent use of blockchain technology is contact tracing (a process wherein individuals who have been in close contact with those who have tested positive for COVID-19 are identified) (Choudhury et al., 2021; Xu et al., 2020), immunity passports (an individual is a disease risk-free because he has already been infected with COVID-19 or was given a COVID-19 vaccine) (Eisenstadt et al., 2020), telemedical laboratory services (Celesti et al., 2020), social distancing (Garg et al., 2020), securely sharing patients’ data (Khatoon, 2020), monitoring isolated people (Zheng et al., 2020), tracking and monitoring the COVID-19 status through a trusted source (Marbouh et al., 2020) and, tracking and controlling the delivery of a COVID-19 vaccine (Ramirez and Beltrán, 2020).
According to Kumar, Singh, et al. (2020), Industry 4.0 and the Internet of Things (IoT) (Narwane et al., 2020) offer excellent support for communication in the value chain. It can stop wrong interpretations of information shared among different agencies. The application of IoT can be used for the better care of the patient during the COVID-19 pandemic. Real-time monitoring of the patients suffering from another disease during the COVID-19 period (when most of the hospitals were declared as COVID hospitals) can be possible with the use of IoT. Smart medical devices can be accessed through a smartphone to transfer the required health data to the physician quickly. These devices can also collect oxygen levels, blood pressure, weight, sugar level, etc. (Javaid & Khan, 2021). Tareq et al. (2021) suggested that additive manufacturing technology can be used to rapidly produce medical equipment such as ventilators, nasopharyngeal swabs and PPE, face masks, and face shields on time with customization.
-
(viii)
Lack of supply of medical oxygen The availability of the medical oxygen required for sick patients is not always straightforward. The patients with moderate-severe COVID-19 may require supplemental oxygen using face masks with oxygen flow up to around 5–6 L O2/min. Flow rates can be adjusted by monitoring the oxygen level using pulse oximetry. The level of oxygen (SpO2) must be above 88% in COVID-19. If the patient shows a desaturation level less than 88% for prolonged periods, oxygen supply to the patient can be enhanced by using a non-rebreathing mask. This can provide a fraction of inspired oxygen (FiO2) of 0.6–0.8 and needs an oxygen flow from the oxygen cylinder or piped oxygen of minimal 10–15 L/min (Dondorp et al., 2020).
There are many ways to supply oxygen to patients. The main source of the oxygen supply is oxygen manufacturing plants, transported to the hospitals in the liquid form. It is vaporized and piped to the patient who needs it. Some hospitals also use the oxygen concentrator, but it is limited to supply the oxygen to only moderate patients (The Wire, 2021, in Appendix 2). The wire (2021, in Appendix 2) reported the details of 178 deaths due to the shortage of supply in hospitals in India. Many hospitals in India were facing an acute shortage of oxygen during the second wave in May 2021. India’s daily oxygen production capacity is 7127 metric tonnes, consumption is only 3842 metric tonnes as per the data released by the Indian government at the beginning of April 2021, but suddenly oxygen demand increased in different states, and many hospitals faced problems due to short supply of oxygen (Bhuyan, 2021).
-
(ix)
Medical waste disposal crisis During Covid-19, wide distribution of infectious materials in the form of used facemasks, gloves, and protective equipment, including food and plastic wastes, was found. Sources of these wastes are hospitals, health care centers, and quarantined households. The waste treatment plants were disrupted and forced for emergency treatment and disposals. In Wuhan city, medical waste radically increased from 40 to about 240 tons/day, exceeding the medical waste treatment capacity of 49 tons/day (Hantoko et al., 2021). It is suggested to collect the medical waste separately. However, the separate medical waste collection and treatment is challenging and needs strong coordination between health authorities and waste service management.
In many developing countries, solid wastes, including medical wastes, are discharged in open dumping or in unsanitary landfills where waste scavengers collect recyclable materials without using protective tools (Nzediegwu & Chang, 2020). Also, livestock such as cows, goats, and dogs use the poorly managed landfills as their “food source”, which may lead to the spread of diseases, including COVID-19. The COVID-19 related medical wastes must be packaged with double-layer medical waste bags and labeled as “COVID-19 infection” (Peng et al., 2020). The disinfectants should decontaminate the surface of bags before putting them into a medical container (Wang et al., 2020). The generated waste from the infected homes should also be double-layer packed and sealed before storing them in collection bins.
-
(x)
Issues related to reliability of RT-PCR test RT-PCR (real-time polymerase chain reaction) is used to test the infection of the COVID-19 virus. Although only 45–60% sensitivity of the test is reported (Dong et al., 2021) under the RT-PCR test, the examination of nasal and oropharyngeal swabs, nasopharyngeal washing, or aspirate is primarily recommended as a diagnosis of COVID-19 (Esbin et al., 2020). In the five different studies covering 957 suspected or confirmed patients of COVID-19, the false-negative rate ranged from 2 to 29% (Arevalo-Rodriguez et al., 2020). False-negative results of true infected cases are considered disease-free and lead to transmitting the disease unintentionally. Unfortunately, another single molecular test also cannot guarantee the infection-free status for a suspected case. The false-negative rate of the RT-PCR test can also occur sometimes due to reasons such as viral load (Thompson & Lei, 2020), denaturation or degradation of RNA due to improper manipulation or storage (Karthik et al., 2020), replication of viral loads for a specific period, variation in viral load in different specimens of the same patient (Mallett et al., 2020).
-
(xi)
Requirement of budgeting and rebudgeting by the Government The processes of budgeting and reporting are to be reconsidered to tackle the challenges of COVID-19. Governments are required to put a strong effort into the preventive and supporting roles of budgeting to lessen the public organizations’ exposure to shocks and for supporting resilience. COVID-19 has a significant impact on the budgeting process. The immediate effect has been in the form of rebudgeting (an act to amend the budget during the financial year) (Anessi-Pessina et al., 2012). In the next few years, rebudgeting is likely to be continued to face the uncertainty produced by the pandemic. The changing variants of the coronavirus pose a strong challenge to the budgeting processes. The budgeting and rebudgeting processes must be flexible and strategic to tackle the challenges of COVID-19 (Anessi-Pessina et al., 2020).
-
(xii)
Collaborative approach for managing inventory and demand forecasting COVID-19 Pandemic leads to the creation of unanticipated demand shocks, stockouts, and disruption of healthcare supply chains due to the severe impact on availability, access, and affordability of medical items (Friday et al., 2021). Most of the research articles on managing medical stocks focus on traditional methods such as minimizing the cost and maximizing profit. It leads to stochastic and periodic reviews, vendor-managed inventory, and the use of radio-frequency identification (Jabbarzadeh et al., 2019). However, in the context of pandemics, governments, relief organizations, and individuals deal with clogged inventory processes. Access to the optimal medical stocks during a pandemic supersedes costs and profits. The risks related to stockouts can be avoided if the medicine management follows a collaborative process planning among the key stakeholders for inventory management (Nematollahi et al., 2018).
In both humanitarian and healthcare supply chains, demand to forecast and planning face problems due to lack of data availability, limited quality control, time-wastage, and error-prone supply chains (van der Laan et al., 2016). The overestimation of medical stocks is preferred in humanitarian supply chains, which contradicts the purpose of commercial supply chains to reduce the inventory and improve customer satisfaction. The adverse effect of the overstocking of medical items in the healthcare supply chain deteriorates due to the lack of collaborative planning, forecasting, and replenishment (CPFR) practices (Panahifar et al., 2015). Rustam et al. (2020) advocate the applications of machine learning models in the forecasting of upcoming COVID-19 affected patients. They have used four standard forecasting models: linear regression, least absolute shrinkage, selection operator, support vector machine, and exponential smoothing to forecast the threatening factors of COVID-19. The threatening factors were newly confirmed cases, the number of deaths, and the number of recoveries.
-
(xiii)
Poverty and Food insecurity A large section of the world population is maintaining some forms of social distancing to contain the health crisis. As a result, millions of businesses closed their activities. A large number of workers became unemployed. The government of developed countries like the USA and the UK has promised to compensate for the income losses of businesses and workers and to contain an inevitable economic crisis. But the relief responses of low- and middle-income countries are limited (Laborde et al., 2020).
The lack of food security and increasing poverty is a major issue for underdeveloped and developing countries (Kumar & Singh, 2021a). Low-income countries are facing challenges related to ensuring the availability of nutritious and safe food to poor people (Pingali et al., 2017). The availability of food grains is crucial because a large section of the population cannot get the food (Clapp, 2017). The central and state governments share the responsibility to provide food grains to the targeted population (Reardon et al., 2019).
-
(xiv)
Lack of skilled manpower Increasing community transmission of COVID-19 infections, inadequate testing capacity, and overwhelming health resources lead to the shortages of the skilled health workforce. To fulfill the requirement of a skilled health workforce, it is necessary to bring community health workers (CHW) on board (Ajisegiri et al., 2020). Engagement of the CHW should be done at the earlier stage to hamper outbreak response and primary health services. The shortages of skilled workforce are also observed in other sectors due to social distancing, lockdown, and government instruction to use only one-third of the workers at a time. Kumar and Singh (2021a) have highlighted the issue of shortage and migration of the skilled workforce in agri-food supply chains due to the outbreak of COVID-19.
All the challenges as discussed above in context to humanitarian supply chains because of the pandemic are summarized in Table 3.
Table 3.
Challenges in Humanitarian supply chain during COVID-19
| Challenges | References | Description |
|---|---|---|
| Lack of planning and preparedness | Villa et al. (2020), Lancet (2020) | This is concerned with the failure of the policy to contain the spread of COVID-19 and poor preparedness to face the challenges of the pandemic outbreak |
| Extended shortages | HHS (2020 in Appendix 2), CBS News (2020a, b in Appendix 2) | This is related to the shortages of medical and other relief items such as N95 masks, PPE kits, medicine, ventilators, oxygen cylinders, etc |
| Inadequate lab capacity | Acharjee (May 10, 2021 in Appendix 2), Doyle (2020 in Appendix 2) | It means the available capacity of the lab for COVID-19 testing is not sufficient, and it delays the report of the testing |
| Lack of supply of COVID-19 vaccines | Rele (2021), Singh and Mehta (2016), Ocampo and Yamagishi (2020), Abbasi et al. (2020), Alam et al. (2021) | Due to the lack of supply of COVID-19 vaccines, the distribution is managed in different phases. In the first phase, the vaccines are provided to health workers and people above 60 years. The second phase is considered for people of more than 45 years, and the third phase is for people of more than 18 years |
| Lack of awareness and hesitancy in acceptance of the vaccines | Pogue et al. (2020), Dror et al. (2020), Schoch-Spana et al. (2020) | Lack of awareness and hesitancy in acceptance of the vaccines defeat the purpose of vaccination. It is necessary to address the concerns of the population and bridge the communication gaps |
| Need of Home-based-primary care services (HBPC) | Ornstein et al. (2015), Totten et al. (2016), Stall et al. (2014), Pisano et al. (2020) | Due to shortages of beds, hospitals and healthcare facilities are provided to only critical patients. The moderate patients are suggested to home quarantine and get the services of HBPC |
| Lack of application of advanced technologies | Abd-alrazaq et al. (2020), Kumar, Singh, et al. (2020), Narwane et al. (2020), Tareq et al. (2021), Javaid and Khan (2021) | It is concerned with the application of Blockchain technology, IoT, Big data analytics, Cloud of Things, Additive manufacturing in data monitoring, telemedicine, home care of patients, and rapid production of medical equipment |
| Lack of supply of medical oxygen | Dondorp et al. (2020), The Wire (2021 in Appendix 2) | The lack of supply of oxygen cylinders was observed in the second phase of COVID-19 in India. Due to uneven distribution and an increase in a sudden demand for oxygen cylinders, many hospitals run out of oxygen, resulting in the death of many patients in different hospitals |
| Medical waste disposal crisis | Hantoko et al. (2021), Nzediegwu and Chang (2020), Wang et al. (2020) | COVID-19 medical wastes are highly infectious, and separate treatment of the medical waste and other waste became challenging for developing and low-income countries |
| Issues related to reliability of RT-PCR test | Esbin et al. (2020), Dong et al. (2021), Arevalo-Rodriguez et al. (2020), Thompson and Lei (2020) | The sensitivity of the RT-PCR test is limited to only 45–60%, and the false-negative rate ranged from 2 to 29%. Thus, it also threatens to spread the virus through the infected people as they declared false negatives |
| Requirement of budgeting and rebudgeting by the government | Anessi-Pessina et al. (2012), Anessi-Pessina et al. (2020) | Rebudgeting is an act to amend the budget during the financial year to meet the immediate impact of COVID-19. Due to uncertainty in the spread of the pandemic, special budgeting and rebudgeting are required to meet the challenges |
| A collaborative approach to maintaining optimal inventory and demand forecasting for humanitarian logistics | Friday et al. (2021), Jabbarzadeh et al. (2019), van der Laan et al. (2016), Panahifar et al. (2015), Rustam et al. (2020) | It is concerned with the collaborative decision-making related to inventory management of the medical items and forecasting the pandemics' spread |
| Poverty and Food insecurity | Laborde et al. (2020), Kumar and Singh (2021a), Pingali et al. (2017), Clapp (2017), Reardon et al. (2019), Kumar, Raut, et al. (2020) | The poverty level has increased due to the disruption of all the business and production activities. Unemployment has also increased, which leads to food security problems among poor people |
| Lack of skilled manpower | Ajisegiri et al. (2020), Kumar and Singh (2021a) | Due to the sudden outbreak and rapid spread of the coronavirus, the demand for skilled manpower is increased. On the other hand, due to social distancing, lockdown, and migration of workers, lack of availability of workers has been observed |
Learnings from COVID-19
The severe impact of disasters across the world has attracted the attention of governments, policymakers, non-governmental organizations, and scholars (Dubey et al., 2019a). The pandemic COVID-19 has not only affected the business of several organizations, but it also affected the social and personal life of the people globally across all countries. Many organizations stopped their operations due to a shortage of resources required. Recently, many research articles covering COVID-19 have discussed chaotic situations and their impact on the lives of people. After analyzing challenges, we are discussing some of the learnings for managing HSC in the future.
Preparedness The preparedness of any system gives the ability to face any kind of disruptions like the COVID-19 outbreak. Preparedness is equally important for the humanitarian supply chains and commercial supply chains. This pandemic has taught many lessons to the management of the organizations and supply chains. It is observed that how the preparedness of a supply chain is crucial for a health care industry. Supply chains are to be efficiently managed considering risk and disruption at both supply chain and organizational levels (Whitten et al., 2012). The COVID-19 pandemic has already exposed the vulnerabilities of key industry players, especially those who have a high dependence on international trades in fulfilling their requirements.
Jahre (2017) worked on finding the strategies to improve logistics preparedness in humanitarian supply chains. He observed that better preparedness improves response even if there is a trade-off between cost efficiency and flexibility. Logistics preparedness is mainly concerned with network design and warehouse location for prepositioning of goods (Kunz & Reiner, 2012). Prepositioning can be viewed as only one among many strategies for the strategic stock of medical items, especially in the case of pandemic and disaster management. Tomasini and Wassenhove (2009) differentiated the characteristics of the humanitarian supply chain and commercial supply chain. They used the case study methodology to observe the role of preparedness, response, and collaboration for the private and humanitarian sectors to work together towards social improvements. They implemented these three agendas (preparedness, response, and collaboration) to collaborate with humanitarian organizations and private businesses to develop the case studies. Kovacs and Sigala (2021) discussed the learnings from HSCs that mitigate the risks and overcome supply chain disruptions. These lessons relate to preparedness and mobilization, including standardization, innovation, and collaboration. Logistics preparedness is equally important in commercial as well as humanitarian supply chains for mobilization of the various resources required.
For a pandemic situation, preparedness must lead to the activities to ensure rapid detection of cases and comprehensive response. The preparedness includes the response plans, training of response teams, prepositioning of relief items including medical equipment and medicines, and preparing treatment centers. These activities may be decentralized rapidly to be ahead of the spread of the disease (Mobula et al., 2020).
Prepositioning of relief items In the initial phase of COVID-19, many countries faced a shortage of medical items such as facemasks, PPE kits, ventilators, oxygen cylinders, etc. The humanitarian organizations have been using prepositioning the relief items as a crucial strategy to prepare for disasters including pandemics. Humanitarian organizations carry the prepositioning inventory of the items either alone or jointly (Toyasaki et al., 2017). Prepositioning of relief items is an effective method for disaster preparedness (Bai et al., 2018). Pre-disaster planning and prepositioning the relief items are important in quickly sending the relief items in the disaster zone (Thomas & Kopczak, 2005). Prepositioning of relief items is considered a key component of humanitarian logistics (Opit & Nakade, 2015). It is observed that humanitarian organizations should attempt to hire a strategic warehouse for prepositioning of relief items (Sharifi-Sedeh et al., 2020; Torabi et al., 2018). Recently, many countries have started to pre-position ventilators, PPE, therapeutics, and laboratory equipment for the pandemic response of COVID-19. COVID-19 is not completely eradicated till date i.e. October 2021. The second phase of COVID-19 has already been observed in some countries, and the third wave is expected as predicted by experts. In this situation, forecasting the relief/medical items based on the first and second wave of COVID-19 has become very important.
Joint procurement It is a long history to use joint procurement in the humanitarian supply chain (Herlin & Pazirandeh, 2015). In the COVID-19 response, many organizations are using joint procurement. For example, the International Federation of Red Cross and Red Crescent Societies (IFRC) coordinates the procurement activities in the Red Cross Movement. Similarly, the COVAX coordinates the procurement of COVID-19 vaccines and other necessary items for their administration. Joint purchasing of items leads to low purchase prices, improved product quality, and long-term relationship with suppliers that reduces the risk of supply shortage (Schulz & Blecken, 2010). Joint purchasing between multiple humanitarian organizations is an effective way to manage the purchase of complex products and services.
Multiple sourcing Before the COVID-19 Pandemic, it has been a general trend to use lean manufacturing and to reduce the number of suppliers and contract manufacturers (Cozzolino et al., 2012). However, it does not work when the logistics systems are completely disrupted (Yang et al., 2019). During the first wave of COVID-19, the entire supply chain was disrupted, and most of the humanitarian organizations, hospitals, government agencies, and private organizations were observing the lack of supply of relief items. Now, organizations are not relying on single suppliers rather planning to take multiple sourcing (Haque & Islam, 2018; Kovacs and Sigala, 2021).
Needs assessment There are some general characteristics of the humanitarian supply chains such as operations in a chaotic environment, unpredictability, uncertainty, rapid changes and deployment in demand, ad hoc project supply chains, etc. (Sigala et al., 2020). Need assessment is very important for planning the actions to be taken to fulfill the needs of the beneficiaries. It is the needs of the beneficiaries in terms of the relief items and locations considering the vulnerabilities and capacities of the beneficiaries (Blecken, 2010; Kovacs and Sigala, 2021).
Collaboration among partners Collaboration among private and government agencies has been very important during the first wave of COVID-19. Many manufacturing organizations changed their production plans during COVID-19. In some cases, the production changeover was government initiated to produce respiratory ventilators. For example, Mahindra and Mahindra have indigenously developed a prototype of a bag valve mask, which is commonly known as an Ambu bag within the cost of Rs. 7500 (Mint, 2020 in Appendix 2). Maruti Suzuki India Ltd signed a Memorandum of Understanding (MoU) with the AgVa on March 30 and has produced 1,250 ventilators to date (Mint, April 24, 2020).
Reliance Industry Ltd has set up India’s first dedicated coronavirus hospital for 1,000 beds (The Hindu, March 23, 2020). Similarly, during the second wave of COVID-19 in 2021, many private and public sector companies started to supply oxygen cylinders to different hospitals in India. Many other companies observed new business opportunities related to the production of hand sanitizers and personal protective equipment. Collaboration between different sectors and partnerships between public and private sectors have become more important for supply chain resilience in disaster-affected areas (Tomasini & Van Wassenhove, 2009; Van Wassenhove, 2006).
Coordination A proper coordination among the actors of humanitarian logistics plays an important role in the relief operations. Sabri et al. (2019) treated it as a fundamental challenge in a sustainable humanitarian supply chain. It may result in a lack of communication, lack of clear policies, ineffective distribution of relief items, and stagnation of relief activities (Vega, 2018). Coordination, as a key challenge in humanitarian activities, is a systematic set of involvements that should safeguard and protect vulnerable groups (Begum & Momen, 2019). The coordination in the value chain has numerous complications. Saleh and Karia (2020) interviewed many leaders and highlighted some important directions of the coordination, such as coordination among the international NGOs, coordination between the existed interagency platforms, coordination with the wider international NGOs internal structures, and coordination with the government.
Coordination between the actors engaged in relief operations leads to improvement in the resilience and efficiency of humanitarian supply chains (Singh et al., 2018). It also leads to effective and efficient utilization of the resources and minimizes the cost of the other items to be procured. It also reduces the operational costs and the response time for providing better services (Akhtar et al., 2012). Balcik et al. (2010) proposed some important factors affecting coordination. These are “diversity, donors’ expectations, funding structures, competition for funding, uncertainty, resource scarcity, and oversupply”. Lack of coordination among actors may result in the prolongation of the suffering of the people (Jin et al., 2015). Dubey et al. (2018) studied big data and predictive analytics for improving visibility and coordination in humanitarian supply chains. They found that swift trust is not the condition for improving coordination among the actors in humanitarian supply chains.
Swift trust and commitment Trust is an essential component of both organizational and team phenomena. Trust affects performance in terms of enhancing intra- and inter-organizational cooperation, coordination, and control. Swift trust is a presumptive form of trust, and it was introduced to explain the paradoxical trusting behavior shown by members of new temporary formed teams (Meyerson et al., 1996; Xu et al., 2007). In these temporary teams, an individual who had no past working relationships with other members immediately forms trust and engages himself in trusting behaviors. Swift trust may be defined as the willingness to rely upon team members to perform their roles in a hastily formed temporary team (Zolin, 2002). Dubey et al. (2019b) studied the application of big data analytics in enhancing the swift trust and collaborative performance between civil and military organizations engaged in disaster relief operations.
Hocutt (1998) defined the term commitment as “the intention to continue a course of action or activity”. Trust and commitment have been treated as the two most important factors to make stronger coordination among actors (Conway & Swift, 2000). Wilson (1995) also identified trust as an important factor for improving a relationship. Miettila and Moller (1990) stated that trust is the prerequisite for enhancing commitment. Commitment has been observed as a key driver of coordination (Kabra & Ramesh, 2015).
Risk management Humanitarian supply chains play an important role in effective and efficient disaster relief operations. Several risks have been observed in Humanitarian supply chains. However, there is no common approach, and its applicability has been studied to deal with these risks through recent cases (Baharmand et al., 2017). Kumar and Singh (2021a) studied the impact of COVID-19 on agri-food supply chains and observed that import disruptions, transport restrictions, supply and distribution uncertainties, price volatility, capital shortage, lack of food securities, etc. are some major issues to manage. Procurement risk is also highlighted by some of the authors. Iakovou et al. (2014) advised dual sourcing as a proactive risk mitigation sourcing strategy.
Information sharing Right information at the right time plays a key role in relief operations. Many sources started to work to spread the information during the disaster and led to a chaotic situation (Kumar & Singh, 2021b). Information sharing is consistently underestimated in the HSC (Ergun et al., 2014). Information sharing is an urgent need of humanitarian supply chains. The real-time data collection and its processing must be reliable and consistent. The information-sharing develops trust among the humanitarian organizations and actors. Information sharing is treated as an important driver of success during a crisis (Gunasekaran and Ngai, 2003).
Response time On-time delivery of relief items to the affected people is essential for an efficient and effective humanitarian supply chain (Abidi et al., 2013). Dubey et al. (2020) studied the impact of antecedents such as information sharing, supply chain visibility, swift trust, commitment, and collaboration on the agility of humanitarian supply chains. Dubey and Gunasekaran (2016) used interpretive structural modeling to link the characteristics of sustainable humanitarian supply chains in terms of agility, adaptability, and alignment. Disasters may be divided into two classes: Slow onset disasters and sudden-onset disasters (Jabbour et al., 2019). In slow-onset disasters, a small duration of time interval is available to organize the relief operations. But, when sudden-onset disasters occur, a quick response is required, and no time is available for proper planning and activities. The main requirement during the crisis is to supply the relief items at the right time in the right location to minimize the impact of the disasters. The initial few days just after a disaster are crucial to meet the challenge of providing emergency relief (Tatham & Kovacs, 2007). During COVID-19, response time for the patient needed ventilator support, and oxygen supply were crucial. Thus, response time is influential in pandemic outbreaks.
Supply chain visibility Visibility is one of the critical factors for high performance in commercial as well as humanitarian supply chains (Choi & Sethi, 2010). Visibility is vital when the actor needs access to information regarding materials/relief items across the supply chain (Klueber & O’Keefe, 2013). Lack of visibility can result in overstocking of unwanted items and understocking of urgently needed supplies. Supply chain visibility recently gained the specific attention of researchers and practitioners. Dubey et al. (2020) found the relationship between information sharing, supply chain visibility, and swift trust for managing HSC. Information sharing influences supply chain visibility and develops swift trust among the humanitarian organizations and actors in disaster relief operations. During the second wave of COVID-19 in India, lack of visibility and information sharing among stakeholders created many problems for human beings. All the above learnings identified after the outbreak of COVID-19 are summarised in Table 4.
Table 4.
Learnings from COVID-19 for managing humanitarian supply chains
| Factors | References | Remarks |
|---|---|---|
| Preparedness | Whitten et al. (2012), Jahre (2017), Tomasini and Wassenhove (2009), Kovacs and Sigala (2021), Mobula et al. (2020) | It leads to the ability to face any emergent situation. It is concerned with all the logistics and humanitarian preparation for the probable disasters |
| Prepositioning of relief items | Toyasaki et al. (2017), Bai et al. (2018), Torabi et al. (2018), Sharifi-Sedeh et al. (2020) | Prepositioning is a strategy to maintain the inventory of the relief items at different locations, either alone or jointly, to prepare for disasters, including pandemics |
| Joint procurement | Herlin and Pazirandeh (2015), Schulz and Blecken (2010) | Joint purchasing of items leads to low purchase prices, improved product quality, and long-term relationship with suppliers that reduces the risk of supply shortage |
| Multiple sourcing | Cozzolino et al. (2012), Yang et al. (2019), Haque and Islam (2018), Kovacs and Sigala (2021) | Multiple sourcing is concerned with the procurement of more than one source to ensure the on-time supply of the relief items |
| Needs assessment | Blecken (2010), Kovacs and Sigala (2021) | Need assessment is very important for planning the actions to be taken to fulfill the needs of the beneficiaries |
| Collaboration | Balcik et al. (2010), Tomasini and Van Wassenhove (2009), Van Wassenhove (2006) | Cross-sector collaboration and public–private sector partnerships become very important for supply chain resilience in disaster-affected areas. Many companies observed new business opportunities related to the production of medical items during the pandemics |
| Coordination | Vega (2018), Begum and Momen (2019), Saleh and Karia (2020), Balcik et al. (2010) | Proper coordination among the actors of humanitarian logistics plays a vital role in relief operations. It leads to effective utilization of the resources and minimizes the cost of the other items to be procured |
| Swift trust and commitment | Meyerson et al. (1996), Xu et al. (2007), Hocutt (1998), Miettila and Moller (1990) | Swift trust is a presumptive form of trust, and it was introduced to explain the paradoxical trusting behavior shown by members of new temporary formed teams. Commitment is intended to continue a course of action or activity. Trust is the precondition for enhancing commitment |
| Risk management | Baharmand et al. (2017), Kumar and Singh (2021a), Iakovou et al. (2014) | Many risks have been observed in Humanitarian supply chains, such as import disruption, transport restriction, supply and distribution uncertainties, price volatility, capital shortage, lack of food securities, etc |
| Information sharing | Kumar and Singh (2021b), Ergun et al. (2014), Gunasekaran and Ngai (2003) | Information sharing is an urgent need of humanitarian supply chains. The information-sharing develops trust among the humanitarian organizations and actors |
| Response time | Abidi et al. (2013), Jabbour et al. (2019), Tatham and Kovacs (2007) | Response time is concerned with the minimum time required to send the relief to the sufferers. During COVID-19, response time for the patient needed ventilator support and oxygen supply were very crucial |
| Supply chain visibility | Choi and Sethi (2010), Klueber and O’Keefe (2013), Dubey et al. (2020) | Visibility is vital when the actor needs access to information regarding materials/relief items across the supply chain |
Research gaps and directions for future research
Due to lack of decision-making and medical protocol, the pandemic outbreaks lead to the worst situation and cause lives of the people in mass. It has been a big question that how to manage the relief operations so that substantial disruption of humanitarian supply chains can be avoided without compromising the essential services, including access to health. The availability of the relief items, including the medical items, is to be insured by the proper inventory management. During the pandemic, all the different actors try to maintain a high inventory level without considering the exact demand. This is the second important question, which is concerned with the strategy to be explored to make an effective inventory planning and demand forecasting.
The pandemic outbreaks cause infectious disease due to which people maintain social distancing, home quarantine, and other precautions. In this situation, the coordination of the relief activities among the actors becomes very difficult. This leads to finding a way to improve the coordination among the aid actors. The application of advanced technology may support relief operations. These technologies and the mechanism of their implementation are to be explored. For example, blockchain technology, IoT, Claud computing, robotic application in medical waste handling, additive manufacturing in the rapid production of medical items may be supportive. After analyzing the challenges in Humanitarian supply chains, we have explored different learnings from the COVID-19 pandemic. Based on the literature, some of the research gaps, research questions, and future research directions are summarised in Table 5.
Table 5.
Summary of the research gaps, research questions, and future research directions
| Research Gaps/emerging issues | Open research questions (ORQ) and opportunities |
Future Research Directions |
|---|---|---|
| 1. Strategy to reduce mortality, and ensure that vulnerable people, refugees, and displaced populations have access to testing, referral, and definitive treatment alongside all populations | ORQ1: How to avoid the substantial disruptions to humanitarian operations without compromising access to health and other essential services, and the ability to respond to urgent community needs? |
COVID-19 has failed the existing approach of lean operations, single sourcing, and inventory minimization. Therefore, there is a need for new business models in the prevailing post COVID scenario During COVID-19, lack of strategy and unpreparedness of different agencies were observed. Government and healthcare organizations will have to find the solution that if a similar type of pandemics repeats how quickly HSC can be geared up Some essential items are to be prepositioned in HSC. Future research should suggest optimization models to find the optimum volume of the items and the suitable locations for prepositions |
| 2. Before the COVID-19 pandemic, companies focused on contract manufacturing, lean manufacturing, offshoring, and outsourcing. These strategies did not work at the time of disruptions | ORQ2: What should be the strategy for resource sharing and avoiding single-sourcing during the pandemic situation? |
Joint procurement of essential items from different sources and their feasibility during the time of disaster should be explored as a part of future studies The possibilities of multiple sourcing and local sourcing are to be explored during the pandemics |
| 3. Past epidemic scenarios show that aid coordination systems need to improve across agencies and the UN clusters as a whole | ORQ3: How to improve the coordination among the different aid agencies during the pandemic? |
During and post-disaster, swift trust among the different actors of the humanitarian supply chain and proper coordination are required. Researchers should explore strategies to establish the swift-trust and proper coordination without loss of time The researchers should propose a coordination mechanism between the governments and citizens for a proper flow of the right information from top to bottom to avoid any chaotic situation |
| 4. The availability of time to respond in sudden-onset disaster/ new pandemic is very less which results in a big loss in the form of lives of the population | ORQ4: How to reduce the response time to provide relief in the case of pandemic outbreaks where no medical protocol is available? |
The researchers should suggest a mechanism of collaboration among different government and private partners and international and national NGOs so that decisions could be taken on time Distribution and supply of essential items such as oxygen and some medicines were observed as a major challenge during the COVID-19 outbreak. Therefore, optimization of the distribution network of such critical items can be further studied as a future scope |
| 5. To establish a proper communication channel between the health care service providers and patient, use of telemedicine, maintaining and monitoring of data related to the pandemic | ORQ5: How to implement the emerging technologies in the humanitarian supply chain to address the various challenges during pandemics? |
Lack of use of technology in the health sector and humanitarian operations has also created many challenges, so future studies should be done on the application of emerging technologies in managing HSCs during pandemics Effective tracking of lifesaving items such as oxygen, medicines, and ventilators had been a major challenge. Future research should explore applying technologies such as Blockchain, RFID, and IOT for this purpose |
| 6. In the case of a pandemic outbreak, the quick management of medical resources and effective planning and preparedness has not been observed in most of the regions of the world | ORQ6: How can medical items be categorized according to their use and availability, and do effective planning for the unexpected future? | The methods for classification of the medical items based on availability, utility, and self-life, annual values need to be explored to avoid the unforeseen future |
Conclusion, limitations, and implications
Managing HSC has always been a challenge for all stakeholders due to many uncertainties and the diversity of actors involved across different processes. Operations or processes of HSC are not well defined, as in the case of the commercial supply chain. Although COVID-19 has caused a lot of loss to society and business, it has given different learnings also for managing HSC, specifically during the pandemic. Therefore, in this study, we have tried to capture different learnings after reviewing different research papers published on COVID-19. Although many research articles have been published on different pandemics, very few articles have addressed the issues of the HSC. Mostly the articles published during 2020–21 on COVID-19 are considered for exploring new learnings to manage humanitarian supply chains. COVID-19’s first-time outbreak happened in 2019. Before COVID-19, other pandemics had been observed, but these were limited to a specific zone or region. In this study, VOS viewer is used to demonstrate the networking amongst the authors and co-authors, and keywords. The observation through the literature review is also validated through the feedback of the respondents by interviewing them. Some regional/specific problems are incorporated in this study through interviews of the respondents, which were not addressed properly in the past literature.
Most of the old pandemic outbreaks-related articles are not addressing the issues of HSC. The first time, a global threat of COVID-19 is observed in December 2019 and continues till date. In 1918, a similar type of pandemic named Spanish flue was observed, which caused the death of millions of people. COVID-19 has caused the death of millions of people throughout the world. All the business and daily life activities, including global logistics operations, are disrupted due to this pandemic. All countries faced challenges such as shortage of relief items, medical equipment, and medicines, food items, etc. Based on the analysis, some of the major challenges observed during the pandemic are lack of planning and preparedness due to the sudden spread of a completely new type of disease and unexpected results, extended shortage due to disruption of the global supply chains and production systems, lack of supply of medical items due to increase in the demand throughout the world, unavailability of the technology to contain the spread of the disease, and poverty of the food security. Similarly, we have also learned many things from the spread of the pandemic COVID-19 such as preparedness of HSC professionals on time, strategies to preposition the essential items, coordination and collaboration among stakeholders, accurate information sharing among all stakeholders, and tracking of inventory, etc. The directions for future research have also been recommended to optimize resources and distribution networks of essential items in HSCs. Researchers should also find solutions for overcoming sudden challenges due to disruptions. Prediction of the COVID-19 wave had been a major challenge, and no accurate forecasting models are available for it. Researchers should explore how data analytics can be used for predicting the next wave of COVID-19 or any other possible pandemic. The application of emerging technologies across different functions of HSC is not well explored in available studies. So future studies can be done on the application of emerging Industry 4.0 technologies for better management of HSCs at the time of pandemics. The major contribution of this study is to highlight the challenges during the spread of the new type of pandemic. Major learnings from the spread of COVID-19 have been also researched for effective management of humanitarian supply chains.
Acknowledgements
Authors would like to express sincere thanks to Editor and Anonymous reviewers for giving constructive inputs and suggestions on our paper.
Appendix 1: List of papers considered for the review process
| S. no | Title | References | Journal |
|---|---|---|---|
| 1 | Impacts of epidemic outbreaks on supply chains: Mapping a research agenda amid the COVID-19 pandemic through a structured literature review | Queiroz et al. (2020) | Annals of Operations Research |
| 2 | Social media effectiveness as a humanitarian response to mitigate influenza epidemic and COVID-19 pandemic | Kumar et al. (2021) | |
| 3 | Toward the understanding of national culture in the success of non‐pharmaceutical technological interventions in mitigating the COVID-19 pandemic | Gupta et al. (2021) | |
| 4 | Data laboratory for supply chain response models during epidemic outbreaks | Anparasan, and Lejeune (2018) | |
| 5 | Viable supply chain model: Integrating agility, resilience and sustainability perspectives—lessons from and thinking beyond the COVID-19 pandemic | Ivanov (2020a) | |
| 6 | Exiting the COVID-19 pandemic: after-shock risks and avoidance of disruption tails in supply chains | Ivanov (2021) | |
| 7 | Stopping Covid-19: A pandemic-management service value chain approach | Baveja et al. (2020) | |
| 8 | Agility in the humanitarian supply chain: An organizational information processing perspective and relational view | Dubey et al. (2020) | |
| 9 | Disaster relief operations: Past, present, and future | Dubey et al. (2019a) | |
| 10 | Fighting against COVID-19: What operations research can help and the sense-and-respond framework | Choi (2021) | |
| 11 | A structured literature review on the interplay between emerging technologies and COVID-19–insights and directions to operations fields | Queiroz and Fosso Wamba (2021) | |
| 12 | The human side of humanitarian supply chains: A research agenda and systematization framework | de Camargo Fiorini et al. (2021) | |
| 13 | An analysis of the literature on humanitarian logistics and supply chain management: Paving the way for future studies | Jabbour et al. (2019) | |
| 14 | Application of Industry 4.0 technologies for effective coordination in humanitarian supply chains: A strategic approach | Kumar and Singh (2021b) | |
| 15 | The emergent role of digital technologies in the context of humanitarian supply chains: A systematic literature review | Marić et al. (2021) | |
| 16 | An applied approach to multi-criteria humanitarian supply chain planning for pandemic response | Malmir and Zobel (2021) | Journal of Humanitarian Logistics and Supply chain Management |
| 17 | Serving vulnerable populations under the threat of epidemics and pandemics | Sokat and Altay (2021) | |
| 18 | The COVID-19 epidemic and evaluating the corresponding responses to crisis management in refugees: A system dynamic approach | Allahi et al. (2021) | |
| 19 | A collaborative approach to maintaining optimal inventory and mitigating stockout risks during a pandemic: Capabilities for enabling healthcare supply chain resilience | Friday et al. (2021) | |
| 20 | An analysis of compounding factors of epidemics in complex emergencies: A system dynamics approach | Harpring et al. (2021) | |
| 21 | The COVID-19 response: Considerations for future humanitarian supply chain and logistics management research | Thompson and Anderson (2021) | |
| 22 | Deciding between cash-based and in-kind distributions during humanitarian emergencies | Castillo (2021) | |
| 23 | Humanitarian medical supply chain in disaster response | Dolinskaya, and Guerrero-Garcia (2018) | |
| 24 | Improvement of public distribution system efficiency applying blockchain technology during pandemic outbreak (COVID-19) | Kumar (2020), Kumar, Singh, et al. (2020), Kumar, Raut, et al. (2020)) | |
| 25 | Analyzing the response to epidemics: concept of evidence-based Haddon matrix | Anparasan, and Lejeune (2017) | |
| 26 | Coordination in humanitarian relief chains: chain coordinators | Akhtar et al. (2012) | |
| 27 | Dual sourcing for mitigating humanitarian supply chain disruptions | Iakovou et al. (2014) | |
| 28 | Humanitarian supply chain strategies–a review of how actors mitigate supply chain risks | Jahre (2017) | |
| 29 | A meta‐analysis of humanitarian logistics research | Kunz and Reiner (2012) | |
| 30 | Digitizing the field: designing ERP systems for Triple-A humanitarian supply chains | Sigala et al. (2020) | |
| 31 | Effect of inter-organizational systems appropriation in agility and resilience development: An empirical investigation | Mandal and Dubey (2021) | Benchmarking: An international Journal |
| 32 | Analyzing drivers and barriers of coordination in humanitarian supply chain management under fuzzy environment | Kabra and Ramesh (2015) | |
| 33 | Benchmarks for INGOs’ effective responses during COVID-19 pandemic | Saleh and Karia (2020) | |
| 34 | OR-methods for coping with the ripple effect in supply chains during COVID-19 pandemic: Managerial insights and research implications | Ivanov and Dolgui (2021) | International Journal of Production Economics |
| 35 | Challenges to COVID-19 vaccine supply chain: Implications for sustainable development goals | Alam et al. (2021) | |
| 36 | Epidemics control and logistics operations: A review | Dasaklis, et al. (2012) | |
| 37 | Antecedents and consequences of supply chain risk management capabilities: An investigation in the post-coronavirus crisis | Yang et al. (2021) | International Journal of Production Research |
| 38 | Analysing the interaction of factors for resilient humanitarian supply chain | Singh et al. (2018) | |
| 39 | Impact of COVID-19 on logistics systems and disruptions in food supply chain | Singh et al. (2021) | |
| 40 | Assimilation of business intelligence: The effect of external pressures and top leaders commitment during pandemic crisis | Chaubey and Sahoo. (2021) | International Journal of Information Management |
| 41 | Lessons learned from humanitarian logistics to manage supply chain disruptions | Kovács and Sigala (2021) | Journal of Supply Chain Management |
| 42 | Humanitarian and disaster relief supply chains: A matter of life and death | Day et al. (2012) | |
| 43 | Designing an integrated pharmaceutical relief chain network under demand uncertainty | Akbarpour et al. (2020) | Transportation Research Part E: Logistics and Transportation Review |
| 44 | Predicting the impacts of epidemic outbreaks on global supply chains: A simulation-based analysis on the coronavirus outbreak (COVID-19/SARS-CoV-2) case | Ivanov (2020b) | |
| 45 | Integrated relief pre-positioning and procurement planning in humanitarian supply chains | Torabi et al. (2018) | |
| 46 | A bibliometric analysis using VOSviewer of publications on COVID-19 | Yu et al. (2020) | Annals of Transnational Medicine |
Appendix 2: Newspaper, news releases, and technical reports considered for review
Acharjee, S. (May 10, 2021) India’s covid collapse, part 4: How the delay in test results accelerated spread of the virus. https://www.indiatoday.in/magazine/cover-story/story/20210517-india-s-covid-collapse-part-4-how-the-delay-in-test-results-accelerated-spread-of-the-virus-1800972-2021-05-10.
CBS News (2020a). The Links in the PPE supply chain ‘Have Been Broken’ as hospitals battle coronavirus, CBS News, April 8, available at: https://www.cbsnews.com/news/coronavirus-ppesupply-chain-hospitals/.
CBS News (2020b), “Americans face COVID-19 test delays as virus surges: ‘A Hot Mess’”, CBS News, Jul 9, available at: https://www.cbsnews.com/news/COVID_19-testing-delays-results-surge/.
Doyle, K. (2020), “‘Inexcusable’: Mick Mulvaney pans coronavirus testing delays”, Washington Examiner, July 13, available at: https://www.washingtonexaminer.com/news/inexcusablemulvaney-pans-coronavirus-testing-delays.
HHS (2020). HHS to provide millions of TYVEK protective suits for U.S. healthcare workers. news release, April 8, HHS, available at: https://www.hhs. gov/about/news/2020/04/08/hhs-provide-millions-tyvek-protective-suits-us-healthcareworkers.html
Mint (April 24, 2020). Maruti joins hands with AgVA Healthcare to supply 10,000 ventilators by May-end. https://www.livemint.com/companies/news/maruti-joins-hands-with-agva-healthcare-to-supply-10-000-ventilators-by-may-end-11587747735201.html.
Mint (March 27, 2020). Covid-19: Mahindra's indigenously developed ventilator to cost less than ₹7500. https://www.livemint.com/companies/news/coronavirus-m-m-ready-with-ventilator-prototype-to-cost-less-than-rs-7-500-11585228399566.html
The Hindu (March 23, 2020). Reliance sets up India’s first dedicated coronavirus hospital. https://www.thehindu.com/business/reliance-sets-up-indias-first-dedicated-covid-19-hospital/article31145158.ece
The Wire (April 24, 2021). COVID-19: Oxygen Is Crucial – but It’s Not Easy To Increase Supply on Short Notice. https://science.thewire.in/health/covid-19-oxygen-is-crucial-but-its-not-easy-to-increase-supply-on-short-notice/ Accessed on June 27, 2021.
The Wire (January 21, 2021). COVID-19 Vaccine Hesitancy Worries Centre. https://science.thewire.in/health/covid-19-vaccine-hesitancy-worries-centre/. Accessed on June 27, 2021.
The Wire (May 7, 2021). 178+ COVID Patients Died in India Because of Oxygen Shortage in Recent Weeks. https://science.thewire.in/health/178-covid-patients-died-in-india-because-of-oxygen-shortage-in-recent-weeks/ Accessed on June 27, 2021.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abbasi, B., Fadaki, M., Kokshagina, O., Saeed, N., & Chhetri, P. (2020). Modeling vaccine allocations in the COVID-19 pandemic: A case study in Australia. Available at SSRN 3744520.
- Abd-alrazaq, A. A., Alajlani, M., Alhuwail, D., Erbad, A., Giannicchi, A., Shah, Z., … & Househ, M. (2020). Blockchain technologies to mitigate COVID-19 challenges: A scoping review. Computer Methods and Programs in Biomedicine Update 1, 100001. [DOI] [PMC free article] [PubMed]
- Abidi H, de Leeuw S, Klumpp M. Measuring success in humanitarian supply chains. International Journal of Business and Management Invention. 2013;2(8):31–39. [Google Scholar]
- Acuña-Soto R, Stahle DW, Cleaveland MK, Therrell MD. Megadrought and megadeath in 16th century Mexico. Emerging Infectious Diseases. 2002;8(4):360. doi: 10.3201/eid0804.010175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajisegiri W, Odusanya O, Joshi R. Covid-19 outbreak situation in Nigeria and the need for effective engagement of community health workers for epidemic response. Global Biosecurity. 2020 doi: 10.31646/gbio.69/. [DOI] [Google Scholar]
- Akbarpour M, Torabi SA, Ghavamifar A. Designing an integrated pharmaceutical relief chain network under demand uncertainty. Transportation Research Part e: Logistics and Transportation Review. 2020;136:101867. doi: 10.1016/j.tre.2020.101867. [DOI] [Google Scholar]
- Akhtar P, Marr NE, Garnevska EV. Coordination in humanitarian relief chains: Chain coordinators. Journal of Humanitarian Logistics and Supply Chain Management. 2012;2(1):85–103. doi: 10.1108/20426741211226019. [DOI] [Google Scholar]
- Akin L, Gözel MG. Understanding dynamics of pandemics. Turkish Journal of Medical Sciences. 2020;50(SI-1):515–519. doi: 10.3906/sag-2004-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam ST, Ahmed S, Ali SM, Sarker S, Kabir G. Challenges to COVID-19 vaccine supply chain: Implications for sustainable development goals. International Journal of Production Economics. 2021;239:108193. doi: 10.1016/j.ijpe.2021.108193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allahi F, Fateh A, Revetria R, Cianci R. The COVID-19 epidemic and evaluating the corresponding responses to crisis management in refugees: A system dynamic approach. Journal of Humanitarian Logistics and Supply Chain Management. 2021;11(2):347–366. doi: 10.1108/JHLSCM-09-2020-0077. [DOI] [Google Scholar]
- Anessi-Pessina E, Barbera C, Langella C, Manes-Rossi F, Sancino A, Sicilia M, Steccolini I. Reconsidering public budgeting after the COVID-19 outbreak: Key lessons and future challenges. Journal of Public Budgeting, Accounting & Financial Management. 2020;32(5):957–965. doi: 10.1108/JPBAFM-07-2020-0115. [DOI] [Google Scholar]
- Anessi-Pessina E, Sicilia M, Steccolini I. Budgeting and rebudgeting in local governments: Siamese twins? Public Administration Review. 2012;72(6):875–884. doi: 10.1111/j.1540-6210.2012.02590.x. [DOI] [Google Scholar]
- Anparasan AA, Lejeune MA. Data laboratory for supply chain response models during epidemic outbreaks. Annals of Operations Research. 2018;270(1):53–64. doi: 10.1007/s10479-017-2462-y. [DOI] [Google Scholar]
- Anparasan A, Lejeune M. Analyzing the response to epidemics: Concept of evidence-based Haddon matrix. Journal of Humanitarian Logistics and Supply Chain Management. 2017;7(3):266–283. doi: 10.1108/JHLSCM-06-2017-0023. [DOI] [Google Scholar]
- Antonovics J, Hood ME, Baker CH. Was the 1918 flu avian in origin? Nature. 2006;440(7088):E9–E9. doi: 10.1038/nature04824. [DOI] [PubMed] [Google Scholar]
- Arevalo-Rodriguez, I., Buitrago-Garcia, D., Simancas-Racines, D., Zambrano-Achig, P., Del Campo, R., Ciapponi, A., … & Zamora, J. (2020). False-negative results of initial RT-PCR assays for COVID-19: a systematic review. PloS one, 15(12), e0242958 [DOI] [PMC free article] [PubMed]
- Baharmand H, Comes T, Lauras M. Managing in-country transportation risks in humanitarian supply chains by logistics service providers: Insights from the 2015 Nepal earthquake. International Journal of Disaster Risk Reduction. 2017;24:549–559. doi: 10.1016/j.ijdrr.2017.07.007. [DOI] [Google Scholar]
- Bai X, Gao J, Liu Y. Prepositioning emergency supplies under uncertainty: A parametric optimization method. Engineering Optimization. 2018;50(7):1114–1133. doi: 10.1080/0305215X.2017.1328508. [DOI] [Google Scholar]
- Balcik B, Beamon BM. Facility location in humanitarian relief. International Journal of Logistics. 2008;11(2):101–121. doi: 10.1080/13675560701561789. [DOI] [Google Scholar]
- Balcik B, Beamon BM, Krejci CC, Muramatsu KM, Ramirez M. Coordination in humanitarian relief chains: Practices, challenges and opportunities. International Journal of Production Economics. 2010;126(1):22–34. doi: 10.1016/j.ijpe.2009.09.008. [DOI] [Google Scholar]
- Baveja A, Kapoor A, Melamed B. Stopping Covid-19: A pandemic-management service value chain approach. Annals of Operations Research. 2020 doi: 10.1007/s10479-020-03635-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begum MM, Momen MN. Disaster risk reduction. Singapore: Palgrave Macmillan; 2019. Coordination does matter for disaster management in Bangladesh; pp. 19–35. [Google Scholar]
- Bhuyan A. Experts criticise India's complacency over COVID-19. The Lancet. 2021;397(10285):1611–1612. doi: 10.1016/S0140-6736(21)00993-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blecken A. Supply chain process modelling for humanitarian organizations. International Journal of Physical Distribution & Logistics Management. 2010;40(8–9):675–692. doi: 10.1108/09600031011079328. [DOI] [Google Scholar]
- BMJ. (2021). Covid-19: India sees record deaths as “black fungus” spreads fear. 10.1136/bmj.n1238 [DOI] [PubMed]
- Burki T. Outbreak of coronavirus disease 2019. The Lancet Infectious Diseases. 2020;20(3):292–293. doi: 10.1016/S1473-3099(20)30076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo JG. Deciding between cash-based and in-kind distributions during humanitarian emergencies. Journal of Humanitarian Logistics and Supply Chain Management. 2021;11(2):272–295. doi: 10.1108/JHLSCM-07-2020-0060. [DOI] [Google Scholar]
- Celesti A, Ruggeri A, Fazio M, Galletta A, Villari M, Romano A. Blockchain-based healthcare workflow for tele-medical laboratory in federated hospital IoT clouds. Sensors. 2020;20(9):2590. doi: 10.3390/s20092590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaubey A, Sahoo CK. Assimilation of business intelligence: The effect of external pressures and top leaders commitment during pandemic crisis. International Journal of Information Management. 2021;59:102344. doi: 10.1016/j.ijinfomgt.2021.102344. [DOI] [Google Scholar]
- Choi TM. Fighting against COVID-19: What operations research can help and the sense-and-respond framework. Annals of Operations Research. 2021 doi: 10.1007/s10479-021-03973-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi TM, Sethi S. Innovative quick response programs: A review. International Journal of Production Economics. 2010;127(1):1–12. doi: 10.1016/j.ijpe.2010.05.010. [DOI] [Google Scholar]
- Choudhury H, Goswami B, Gurung SK. CovidChain: An anonymity preserving blockchain based framework for protection against Covid-19. Information Security Journal: A Global Perspective. 2021 doi: 10.1080/19393555.2021.1921315. [DOI] [Google Scholar]
- Clapp J. Food self-sufficiency: Making sense of it, and when it makes sense. Food Policy. 2017;66:88–96. doi: 10.1016/j.foodpol.2016.12.001. [DOI] [Google Scholar]
- Connell J, Lowe A. Generating grounded theory from qualitative data: The application of inductive methods in tourism and hospitality management research. Progress in Tourism and Hospitality Research. 1997;3(2):165–173. doi: 10.1002/(SICI)1099-1603(199706)3:2<165::AID-PTH87>3.0.CO;2-I. [DOI] [Google Scholar]
- Conway T, Swift JS. International relationship marketing: The importance of psychic distance. European Journal of Marketing. 2000;34(11/12):1391–1414. doi: 10.1108/03090560010348641. [DOI] [Google Scholar]
- Cozzolino A, Rossi S, Conforti A. Agile and lean principles in the humanitarian supply chain. Journal of Humanitarian Logistics and Supply Chain Management. 2012;2:16–33. doi: 10.1108/20426741211225984. [DOI] [Google Scholar]
- Dasaklis TK, Pappis CP, Rachaniotis NP. Epidemics control and logistics operations: A review. International Journal of Production Economics. 2012;139(2):393–410. doi: 10.1016/j.ijpe.2012.05.023. [DOI] [Google Scholar]
- Day JM, Melnyk SA, Larson PD, Davis EW, Whybark DC. Humanitarian and disaster relief supply chains: A matter of life and death. Journal of Supply Chain Management. 2012;48(2):21–36. doi: 10.1111/j.1745-493X.2012.03267.x. [DOI] [Google Scholar]
- de Camargo Fiorini P, Jabbour CJC, de Sousa Jabbour ABL, Ramsden G. The human side of humanitarian supply chains: A research agenda and systematization framework. Annals of Operations Research. 2021 doi: 10.1007/s10479-021-03970-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rond M, Miller AN. Publish or perish: Bane or boon of academic life? Journal of Management Inquiry. 2005;14(4):321–329. doi: 10.1177/1056492605276850. [DOI] [Google Scholar]
- DeWitte SN. Mortality risk and survival in the aftermath of the medieval Black Death. PLoS ONE. 2014;9(5):e96513. doi: 10.1371/journal.pone.0096513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolinskaya I, Besiou M, Guerrero-Garcia S. Humanitarian medical supply chain in disaster response. Journal of Humanitarian Logistics and Supply Chain Management. 2018;892:199–226. doi: 10.1108/JHLSCM-01-2018-0002. [DOI] [Google Scholar]
- Dondorp AM, Hayat M, Aryal D, Beane A, Schultz MJ. Respiratory support in COVID-19 patients, with a focus on resource-limited settings. The American Journal of Tropical Medicine and Hygiene. 2020;102(6):1191–1197. doi: 10.4269/ajtmh.20-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, Y. M., Sun, J., Li, Y. X., Chen, Q., Liu, Q. Q., Sun, Z., … & Ye, D. W. (2021). Development and validation of a nomogram for assessing survival in patients with COVID-19 pneumonia. Clinical Infectious Diseases, 72(4), 652–660. [DOI] [PMC free article] [PubMed]
- Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., … & Sela, E. (2020). Vaccine hesitancy: the next challenge in the fight against COVID-19. European Journal of Epidemiology, 35(8), 775–779. [DOI] [PMC free article] [PubMed]
- Dubey R, Gunasekaran A. The sustainable humanitarian supply chain design: Agility, adaptability and alignment. International Journal of Logistics Research and Applications. 2016;19(1):62–82. doi: 10.1080/13675567.2015.1015511. [DOI] [Google Scholar]
- Dubey R, Bryde DJ, Foropon C, Graham G, Giannakis M, Mishra DB. Agility in humanitarian supply chain: An organizational information processing perspective and relational view. Annals of Operations Research. 2020 doi: 10.1007/s10479-020-03824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey R, Gunasekaran A, Papadopoulos T. Disaster relief operations: Past, present and future. Annals of Operations Research. 2019;283(1):1–8. doi: 10.1007/s10479-019-03440-7. [DOI] [Google Scholar]
- Dubey R, Gunasekaran A, Childe SJ, Roubaud D, Wamba SF, Giannakis M, Foropon C. Big data analytics and organizational culture as complements to swift trust and collaborative performance in the humanitarian supply chain. International Journal of Production Economics. 2019;210:120–136. doi: 10.1016/j.ijpe.2019.01.023. [DOI] [Google Scholar]
- Dubey R, Luo Z, Gunasekaran A, Akter S, Hazen BT, Douglas MA. Big data and predictive analytics in humanitarian supply chains: Enabling visibility and coordination in the presence of swift trust. The International Journal of Logistics Management. 2018;29(2):485–512. doi: 10.1108/IJLM-02-2017-0039. [DOI] [Google Scholar]
- Dubey R, Singh T, Gupta OK. Impact of agility, adaptability and alignment on humanitarian logistics performance: Mediating effect of leadership. Global Business Review. 2015;16(5):812–831. doi: 10.1177/0972150915591463. [DOI] [Google Scholar]
- Duran S, Gutierrez MA, Keskinocak P. Pre-positioning of emergency items for CARE international. Interfaces. 2011;41(3):223–237. doi: 10.1287/inte.1100.0526. [DOI] [Google Scholar]
- Eisenstadt M, Ramachandran M, Chowdhury N, Third A, Domingue J. COVID-19 antibody test/vaccination certification: There’s an app for that. IEEE Open Journal of Engineering in Medicine and Biology. 2020;1:148–155. doi: 10.1109/OJEMB.2020.2999214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ergun Ö, Gui L, HeierStamm JL, Keskinocak P, Swann J. Improving humanitarian operations through technology-enabled collaboration. Production and Operations Management. 2014;23(6):1002–1014. doi: 10.1111/poms.12107. [DOI] [Google Scholar]
- Esbin MN, Whitney ON, Chong S, Maurer A, Darzacq X, Tjian R. Overcoming the bottleneck to widespread testing: A rapid review of nucleic acid testing approaches for COVID-19 detection. RNA. 2020;26(7):771–783. doi: 10.1261/rna.076232.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq MU, Hussain A, Masood T, Habib MS. Supply chain operations management in pandemics: A state-of-the-art review inspired by COVID-19. Sustainability. 2021;13(5):2504. doi: 10.3390/su13052504. [DOI] [Google Scholar]
- Forman R, Shah S, Jeurissen P, Jit M, Mossialos E. COVID-19 vaccine challenges: What have we learned so far and what remains to be done? Health Policy. 2021;125:553–567. doi: 10.1016/j.healthpol.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friday D, Savage DA, Melnyk SA, Harrison N, Ryan S, Wechtler H. A collaborative approach to maintaining optimal inventory and mitigating stockout risks during a pandemic: Capabilities for enabling health-care supply chain resilience. Journal of Humanitarian Logistics and Supply Chain Management. 2021;11(2):248–271. doi: 10.1108/JHLSCM-07-2020-0061. [DOI] [Google Scholar]
- Garg C, Bansal A, Padappayil RP. COVID-19: Prolonged social distancing implementation strategy using blockchain-based movement passes. Journal of Medical Systems. 2020;44(9):1–3. doi: 10.1007/s10916-020-01628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatignon A, Van Wassenhove LN, Charles A. The Yogyakarta earthquake: Humanitarian relief through IFRC’s decentralized supply chain. International Journal of Production Economics. 2010;126(1):102–110. doi: 10.1016/j.ijpe.2010.01.003. [DOI] [Google Scholar]
- Gunasekaran A, Ngai EWT. The successful management of a small logistics company. International Journal of Physical Distribution and Logistics Management. 2003;33(9):825–842. doi: 10.1108/09600030310503352. [DOI] [Google Scholar]
- Gupta, M., Shoja, A., & Mikalef, P. (2021). Toward the understanding of national culture in the success of non‐pharmaceutical technological interventions in mitigating COVID-19 pandemic. Annals of Operations Research, 1–18. [DOI] [PMC free article] [PubMed]
- Guttieres D, Sinskey AJ, Springs SL. Modeling framework to evaluate vaccine strategies against the COVID-19 pandemic. Systems. 2021;9(1):4. doi: 10.3390/systems9010004. [DOI] [Google Scholar]
- Hantoko D, Li X, Pariatamby A, Yoshikawa K, Horttanainen M, Yan M. Challenges and practices on waste management and disposal during COVID-19 pandemic. Journal of Environmental Management. 2021;286:112140. doi: 10.1016/j.jenvman.2021.112140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haque M, Islam R. Impact of supply chain collaboration and knowledge sharing on organizational outcomes in pharmaceutical industry of Bangladesh. Journal of Global Operations and Strategic Sourcing. 2018;11:301–320. doi: 10.1108/JGOSS-02-2018-0007. [DOI] [Google Scholar]
- Harpring R, Maghsoudi A, Fikar C, Piotrowicz WD, Heaslip G. An analysis of compounding factors of epidemics in complex emergencies: A system dynamics approach. Journal of Humanitarian Logistics and Supply Chain Management. 2021;11(2):198–226. doi: 10.1108/JHLSCM-07-2020-0063. [DOI] [Google Scholar]
- Herlin H, Pazirandeh A. Avoiding the pitfalls of cooperative purchasing through control and coordination: Insights from a humanitarian context. International Journal of Procurement Management. 2015;8(3):303–325. doi: 10.1504/IJPM.2015.069155. [DOI] [Google Scholar]
- Hippold, S. (2020). Coronavirus: How to secure your supply chain. https://www.gartner.com/smarterwithgartner/coronavirushow-to-secure-your-supply-chain/. Accessed on 24 May 2021.
- Hocutt MA. Relationship dissolution model: Antecedents of relationship commitment and the likelihood of dissolving a relationship. International Journal of Service Industry Management. 1998;9(2):189–200. doi: 10.1108/09564239810210541. [DOI] [Google Scholar]
- Iakovou E, Vlachos D, Keramydas C, Partsch D. Dual sourcing for mitigating humanitarian supply chain disruptions. Journal of Humanitarian Logistics and Supply Chain Management. 2014;4(2):245–264. doi: 10.1108/JHLSCM-03-2013-0008. [DOI] [Google Scholar]
- Ivanov D. Viable supply chain model: Integrating agility, resilience and sustainability perspectives—lessons from and thinking beyond the COVID-19 pandemic. Annals of Operations Research. 2020 doi: 10.1007/s10479-020-03640-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov D. Predicting the impacts of epidemic outbreaks on global supply chains: A simulation-based analysis on the coronavirus outbreak (COVID-19/SARS-CoV-2) case. Transportation Research Part e: Logistics and Transportation Review. 2020;136:101922. doi: 10.1016/j.tre.2020.101922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov D. Exiting the COVID-19 pandemic: After-shock risks and avoidance of disruption tails in supply chains. Annals of Operations Research. 2021 doi: 10.1007/s10479-021-04047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov D, Dolgui A. OR-methods for coping with the ripple effect in supply chains during COVID-19 pandemic: Managerial insights and research implications. International Journal of Production Economics. 2021;232:107921. doi: 10.1016/j.ijpe.2020.107921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabbarzadeh A, Haughton M, Pourmehdi F. A robust optimization model for efficient and green supply chain planning with postponement strategy. International Journal of Production Economics. 2019;214:266–283. doi: 10.1016/j.ijpe.2018.06.013. [DOI] [Google Scholar]
- Jabbour CJC, Sobreiro VA, de Sousa Jabbour ABL, de Souza Campos LM, Mariano EB, Renwick DWS. An analysis of the literature on humanitarian logistics and supply chain management: Paving the way for future studies. Annals of Operations Research. 2019;283:289–307. doi: 10.1007/s10479-017-2536-x. [DOI] [Google Scholar]
- Jahre M. Humanitarian supply chain strategies–a review of how actors mitigate supply chain risks. Journal of Humanitarian Logistics and Supply Chain Management. 2017;7(2):82–101. doi: 10.1108/JHLSCM-12-2016-0043. [DOI] [Google Scholar]
- Javaid M, Khan IH. Internet of Things (IoT) enabled healthcare helps to take the challenges of COVID-19 Pandemic. Journal of Oral Biology and Craniofacial Research. 2021;11(2):209–214. doi: 10.1016/j.jobcr.2021.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin S, Jeong S, Kim J, Kim K. A logistics model for the transport of disaster victims with various injuries and survival probabilities. Annals of Operations Research. 2015;230(1):17–33. doi: 10.1007/s10479-013-1515-0. [DOI] [Google Scholar]
- Kabra G, Ramesh A. Analyzing drivers and barriers of coordination in humanitarian supply chain management under fuzzy environment. Benchmarking: an International Journal. 2015;22(4):559–587. doi: 10.1108/BIJ-05-2014-0041. [DOI] [Google Scholar]
- Karthik K, Babu RPA, Dhama K, Chitra MA, Kalaiselvi G, Senthil Kumar TMA, Raj GD. Biosafety concerns during the collection, transportation, and processing of COVID-19 samples for diagnosis. Archives of Medical Research. 2020;51(7):623–630. doi: 10.1016/j.arcmed.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karuppiah K, Sankaranarayanan B, Ali SM, Paul SK. Key challenges to sustainable humanitarian supply chains: Lessons from the COVID-19 pandemic. Sustainability. 2021;13(11):5850. doi: 10.3390/su13115850. [DOI] [Google Scholar]
- Khatoon, A. (2020). Use of blockchain technology to curb novel coronavirus disease (COVID-19) transmission. Available at SSRN 3584226.
- Kim JH, Marks F, Clemens JD. Looking beyond COVID-19 vaccine phase 3 trials. Nature Medicine. 2021;27(2):205–211. doi: 10.1038/s41591-021-01230-y. [DOI] [PubMed] [Google Scholar]
- Klueber R, O’Keefe RM. Defining and assessing requisite supply chain visibility in regulated industries. Journal of Enterprise Information Management. 2013;26(3):295–313. doi: 10.1108/17410391311325243. [DOI] [Google Scholar]
- Kovács G, Falagara Sigala I. Lessons learned from humanitarian logistics to manage supply chain disruptions. Journal of Supply Chain Management. 2021;57(1):41–49. doi: 10.1111/jscm.12253. [DOI] [Google Scholar]
- Kovács G, Spens KM. Humanitarian logistics in disaster relief operations. International Journal of Physical Distribution & Logistics Management. 2007;37(2):99–114. doi: 10.1108/09600030710734820. [DOI] [Google Scholar]
- Kumar A. Improvement of public distribution system efficiency applying blockchain technology during pandemic outbreak (COVID-19) Journal of Humanitarian Logistics and Supply Chain Management. 2020;11(1):1–28. doi: 10.1108/JHLSCM-06-2020-0050. [DOI] [Google Scholar]
- Kumar A, Singh RK, Modgil S. Exploring the relationship between ICT, SCM practices and organizational performance in agri-food supply chain. Benchmarking: an International Journal. 2020;27(3):1003–1041. doi: 10.1108/BIJ-11-2019-0500. [DOI] [Google Scholar]
- Kumar MS, Raut RD, Narwane VS, Narkhede BE. Applications of industry 4.0 to overcome the COVID-19 operational challenges. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(5):1283–1289. doi: 10.1016/j.dsx.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P, Singh RK. Strategic framework for developing resilience in agri-food supply chains during COVID 19 pandemic. International Journal of Logistics Research and Applications. 2021 doi: 10.1080/13675567.2021.1908524. [DOI] [Google Scholar]
- Kumar P, Singh RK. Application of Industry 4.0 technologies for effective coordination in humanitarian supply chains: a strategic approach. Annals of Operations Research. 2021 doi: 10.1007/2Fs10479-020-03898-w. [DOI] [Google Scholar]
- Kumar S, Xu C, Ghildayal N, Chandra C, Yang M. Social media effectiveness as a humanitarian response to mitigate influenza epidemic and COVID-19 pandemic. Annals of Operations Research. 2021 doi: 10.1007/s10479-021-03955-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunz N, Reiner G. A meta-analysis of humanitarian logistics research. Journal of Humanitarian Logistics and Supply Chain Management. 2012;2(2):116–147. doi: 10.1108/20426741211260723. [DOI] [Google Scholar]
- Laborde, D., Martin, W., & Vos, R. (2020). Poverty and food insecurity could grow dramatically as COVID-19 spreads. International Food Policy Research Institute (IFPRI), Washington, DC. https://www.researchgate.net/profile/Rob_Vos2/publication/343267777_Poverty_and_food_insecurity_could_grow_dramatically_as_COVID-19_spreads/links/5f20772345851515ef509bf7/Poverty-and-food-insecurity-could-grow-dramatically-as-COVID-19-spreads.pdf
- Lancet T. COVID-19: Too little, too late? Lancet (london, England) 2020;395(10226):755. doi: 10.1016/S0140-6736(20)30522-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett, S., Allen, A. J., Graziadio, S., Taylor, S. A., Sakai, N. S., Green, K., … & Halligan, S. (2020). At what times during infection is SARS-CoV-2 detectable and no longer detectable using RT-PCR-based tests? A systematic review of individual participant data. BMC medicine, 18(1), 1–17. [DOI] [PMC free article] [PubMed]
- Malmir B, Zobel CW. An applied approach to multi-criteria humanitarian supply chain planning for pandemic response. Journal of Humanitarian Logistics and Supply Chain Management. 2021;11(2):320–346. doi: 10.1108/JHLSCM-08-2020-0064. [DOI] [Google Scholar]
- Mandal S, Dubey RK. Effect of inter-organizational systems appropriation in agility and resilience development: An empirical investigation. Benchmarking: An International Journal. 2021 doi: 10.1108/BIJ-10-2020-0542. [DOI] [Google Scholar]
- Marbouh, D., Abbasi, T., Maasmi, F., Omar, I. A., Debe, M. S., Salah, K., … & Ellahham, S. (2020). Blockchain for COVID-19: Review, Opportunities, and a Trusted Tracking System. Arabian Journal for Science and Engineering, 45:9895–9911. [DOI] [PMC free article] [PubMed]
- Marić, J., Galera-Zarco, C., & Opazo-Basáez, M. (2021). The emergent role of digital technologies in the context of humanitarian supply chains: a systematic literature review. Annals of Operations Research, 1–42. [DOI] [PMC free article] [PubMed]
- Martin D, Woodside AG. Grounded theory of international tourism behavior. Journal of Travel & Tourism Marketing. 2008;24(4):245–258. doi: 10.1080/10548400802156695. [DOI] [Google Scholar]
- Meyerson D, Weick KE, Kramer RM. Swift trust and temporary groups. In: Kramer RM, Tyler TR, editors. Trust in organizations: Frontiers of theory and research. Sage; 1996. pp. 166–195. [Google Scholar]
- Miettila A, Moller K. Interaction perspective into professional business services: A conceptual analysis. In: Fiocca R, Snehota I, editors. IMP conference: Research developments in international industrial marketing and purchasing. 6. University of Bocconi; 1990. pp. 759–781. [Google Scholar]
- Mobula, L. M., Samaha, H., Yao, M., Gueye, A. S., Diallo, B., Umutoni, C., … & Ahuka-Mundeke, S. (2020). Recommendations for the COVID-19 response at the national level based on lessons learned from the Ebola virus disease outbreak in the Democratic Republic of the Congo. The American journal of tropical medicine and hygiene, 103(1), 12–17. [DOI] [PMC free article] [PubMed]
- Mordechai L, Eisenberg M, Newfield TP, Izdebski A, Kay JE, Poinar H. The justinianic plague: An inconsequential pandemic? Proceedings of the National Academy of Sciences. 2019;116(51):25546–25554. doi: 10.1073/pnas.1903797116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narwane VS, Raut RD, Mangla SK, Gardas BB, Narkhede BE, Awasthi A, Priyadarshinee P. Mediating role of cloud of things in improving performance of small and medium enterprises in the Indian context. Annals of Operations Research. 2020 doi: 10.1007/s10479-019-03502-w. [DOI] [Google Scholar]
- Nematollahi M, Hosseini-Motlagh SM, Ignatius J, Goh M, Nia MS. Coordinating a socially responsible pharmaceutical supply chain under periodic review replenishment policies. Journal of Cleaner Production. 2018;172:2876–2891. doi: 10.1016/j.jclepro.2017.11.126. [DOI] [Google Scholar]
- Nunkoo R, Ramkissoon H. Stakeholders’ views of enclave tourism: A grounded theory approach. Journal of Hospitality & Tourism Research. 2016;40(5):557–558. doi: 10.1177/1096348013503997. [DOI] [Google Scholar]
- Nzediegwu C, Chang SX. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resources, Conservation, and Recycling. 2020;161:104947. doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ocampo L, Yamagishi K. Modeling the lockdown relaxation protocols of the Philippine government in response to the COVID-19 pandemic: An intuitionistic fuzzy DEMATEL analysis. Socio-Economic Planning Sciences. 2020;72:100911. doi: 10.1016/j.seps.2020.100911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opit, P. F., & Nakade, K. (2015). Emergency response model of stock-prepositioning with transportation constraints. In 2015 IEEE international conference on industrial engineering and engineering management (IEEM) (pp. 239–243). IEEE.
- Ornstein, K. A., Leff, B., Covinsky, K. E., Ritchie, C. S., Federman, A. D., Roberts, L., … & Szanton, S. L. (2015). Epidemiology of the homebound population in the United States. JAMA Internal Medicine, 175(7), 1180–1186. [DOI] [PMC free article] [PubMed]
- Panahifar, F., Heavey, C., Byrne, P. J., & Fazlollahtabar, H. (2015). A framework for collaborative planning, forecasting and replenishment (CPFR). Journal of Enterprise Information Management. http://doras.dcu.ie/20876/1/JEIM_2015_-_CPFR-State-of-the-Art.pdf
- Pandey A, Galvani AP. The global burden of HIV and prospects for control. The Lancet HIV. 2019;6(12):e809–e811. doi: 10.1016/S2352-3018(19)30230-9. [DOI] [PubMed] [Google Scholar]
- Peng J, Wu X, Wang R, Li C, Zhang Q, Wei D. Medical waste management practice during the 2019–2020 novel coronavirus pandemic: Experience in a general hospital. American Journal of Infection Control. 2020;48(8):918–921. doi: 10.1016/j.ajic.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pingali P, Mittra B, Rahman A. The bumpy road from food to nutrition security–slow evolution of India's food policy. Global Food Security. 2017;15:77–84. doi: 10.1016/j.gfs.2017.05.002. [DOI] [Google Scholar]
- Pisano, G. P., Sadun, R., & Zanini, M. (2020). Lessons from Italy’s response to coronavirus. Harvard business review, 27. https://fondazionecerm.it/wp-content/uploads/2020/04/HBR-Lessons-from-Italy%E2%80%99s-Response-to-Coronavirus.pdf. Accessed on 27 June 2021.
- Pogue, K., Jensen, J. L., Stancil, C. K., Ferguson, D. G., Hughes, S. J., Mello, E. J., … & Poole, B. D. (2020). Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines, 8(4), 582. [DOI] [PMC free article] [PubMed]
- Queiroz MM, Fosso Wamba S. A structured literature review on the interplay between emerging technologies and COVID-19–insights and directions to operations fields. Annals of Operations Research. 2021 doi: 10.1007/s10479-021-04107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Queiroz MM, Ivanov D, Dolgui A, Wamba SF. Impacts of epidemic outbreaks on supply chains: Mapping a research agenda amid the COVID-19 pandemic through a structured literature review. Annals of Operations Research. 2020 doi: 10.1007/s10479-020-03685-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez Lopez LJ, Beltrán Álvarez N. Blockchain application in the distribution chain of the COVID-19 vaccine: a designing understudy. Advance. 2020;14(2):1–9. doi: 10.31124/advance.12274844.v1. [DOI] [Google Scholar]
- Reardon T, Echeverria R, Berdegué J, Minten B, Liverpool-Tasie S, Tschirley D, Zilberman D. Rapid transformation of food systems in developing regions: Highlighting the role of agricultural research & innovations. Agricultural Systems. 2019;172:47–59. doi: 10.1016/j.agsy.2018.01.022. [DOI] [Google Scholar]
- Rele S. COVID-19 vaccine development during pandemic: Gap analysis, opportunities, and impact on future emerging infectious disease development strategies. Human Vaccines & Immunotherapeutics. 2021;17(4):1122–1127. doi: 10.1080/21645515.2020.1822136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie, C. S., Gallopyn, N., Sheehan, O., Sharieff, S. A., Franzosa, E., Gorbenko, K., … & Leff, B. (2021). COVID Challenges and adaptations among home-based primary care practices: Lessons for an ongoing pandemic from a national survey. Journal of the American Medical Directors Association. 10.1016/j.jamda.2021.05.016 [DOI] [PMC free article] [PubMed]
- Rustam F, Reshi AA, Mehmood A, Ullah S, On BW, Aslam W, Choi GS. COVID-19 future forecasting using supervised machine learning models. IEEE Access. 2020;8:101489–101499. doi: 10.1109/ACCESS.2020.2997311. [DOI] [Google Scholar]
- Sabri Y, Zarei MH, Harland C. Using collaborative research methodologies in humanitarian supply chains. Journal of Humanitarian Logistics and Supply Chain Management. 2019;9:371–409. doi: 10.1108/JHLSCM-06-2018-0041. [DOI] [Google Scholar]
- Saleh FIM, Karia N. Benchmarks for INGOs’ effective responses during COVID-19 pandemic. Benchmarking: an International Journal. 2020;27(10):2863–2886. doi: 10.1108/BIJ-04-2020-0157. [DOI] [Google Scholar]
- Schoch-Spana, M., Brunson, E. K., Long, R., Ruth, A., Ravi, S. J., Trotochaud, M., … & White, A. (2020). The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine. 10.1016/j.vaccine.2020.10.059 [DOI] [PMC free article] [PubMed]
- Schulz SF, Blecken A. Horizontal cooperation in disaster relief logistics: Benefits and impediments. International Journal of Physical Distribution & Logistics Management. 2010;40(8/9):636–656. doi: 10.1108/09600031011079300. [DOI] [Google Scholar]
- Sharifi-Sedeh M, Ardalan A, Torabi SA, Khorasani-Zavareh D. Factors behind the prepositioning of relief items in Iran: A qualitative study. Injury. 2020;51(4):906–912. doi: 10.1016/j.injury.2020.02.083. [DOI] [PubMed] [Google Scholar]
- Sigala IF, Kettinger WJ, Wakolbinger T. Digitizing the field: Designing ERP systems for Triple-A humanitarian supply chains. Journal of Humanitarian Logistics and Supply Chain Management. 2020;10(2):231–260. doi: 10.1108/JHLSCM-08-2019-0049. [DOI] [Google Scholar]
- Singh K, Mehta S. The clinical development process for a novel preventive vaccine: An overview. Journal of Postgraduate Medicine. 2016;62(1):4. doi: 10.4103/0022-3859.173187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh RK, Gupta A, Gunasekaran A. Analysing the interaction of factors for resilient humanitarian supply chain. International Journal of Production Research. 2018;56(21):6809–6827. doi: 10.1080/00207543.2018.1424373. [DOI] [Google Scholar]
- Singh S, Kumar R, Panchal R, Tiwari MK. Impact of COVID-19 on logistics systems and disruptions in food supply chain. International Journal of Production Research. 2021;59(7):1993–2008. doi: 10.1080/00207543.2020.1792000. [DOI] [Google Scholar]
- Sokat KY, Altay N. Serving vulnerable populations under the threat of epidemics and pandemics. Journal of Humanitarian Logistics and Supply Chain Management. 2021 doi: 10.1108/JHLSCM-08-2020-0070. [DOI] [Google Scholar]
- Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. Journal of the American Geriatrics Society. 2014;62(12):2243–2251. doi: 10.1111/jgs.13088. [DOI] [PubMed] [Google Scholar]
- Tareq MS, Rahman T, Hossain M, Dorrington P. Additive manufacturing and the COVID-19 challenges: An in-depth study. Journal of Manufacturing Systems. 2021 doi: 10.1016/j.jmsy.2020.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatham, P., & Kovács, G. (2007). The humanitarian supply network in rapid onset disasters. In Proceedings of the 19th annual conference for Nordic researchers in logistics, NOFOMA (pp. 1059–1074).
- Thomas AS, Kopczak LR. From logistics to supply chain management: The path forward in the humanitarian sector. Fritz Institute. 2005;15(1):1–15. [Google Scholar]
- Thompson DD, Anderson R. The COVID-19 response: Considerations for future humanitarian supply chain and logistics management research. Journal of Humanitarian Logistics and Supply Chain Management. 2021 doi: 10.1108/JHLSCM-01-2021-0006. [DOI] [Google Scholar]
- Thompson D, Lei Y. Mini review: Recent progress in RT-LAMP enabled COVID-19 detection. Sensors and Actuators Reports. 2020;21:100017. doi: 10.1016/j.snr.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasini RM, Van Wassenhove LN. From preparedness to partnerships: Case study research on humanitarian logistics. International Transactions in Operational Research. 2009;16(5):549–559. doi: 10.1111/j.1475-3995.2009.00697.x. [DOI] [Google Scholar]
- Torabi SA, Shokr I, Tofighi S, Heydari J. Integrated relief pre-positioning and procurement planning in humanitarian supply chains. Transportation Research Part e: Logistics and Transportation Review. 2018;113:123–146. doi: 10.1016/j.tre.2018.03.012. [DOI] [Google Scholar]
- Totten, A. M., White-Chu, E. F., Wasson, N., Morgan, E., Kansagara, D., Davis-O'Reilly, C., & Goodlin, S. (2016). Home-based primary care interventions. (Prepared by the Pacific Northwest Evidence-Based Practice Center Under Contract No 290-2012-00014-I) AHRQ Publication No 15 (16)-EHC036-EF. Rockville: Agency for Healthcare Research and Quality; 2016. Rockville, MD: Agency for Healthcare Research and Quality. [PubMed]
- Toyasaki F, Arikan E, Silbermayr L, Falagara Sigala I. Disaster relief inventory management: Horizontal cooperation between humanitarian organizations. Production and Operations Management. 2017;26(6):1221–1237. doi: 10.1111/poms.12661. [DOI] [Google Scholar]
- Van der Laan E, van Dalen J, Rohrmoser M, Simpson R. Demand forecasting and order planning for humanitarian logistics: An empirical assessment. Journal of Operations Management. 2016;45:114–122. doi: 10.1016/j.jom.2016.05.004. [DOI] [Google Scholar]
- Van Wassenhove LN. Humanitarian aid logistics: Supply chain management in high gear. Journal of the Operational Research Society. 2006;57(5):475–489. doi: 10.1057/palgrave.jors.2602125. [DOI] [Google Scholar]
- Vega D. Case studies in humanitarian logistics research. Journal of Humanitarian Logistics and Supply Chain Management. 2018;8:134–152. doi: 10.1108/JHLSCM-01-2018-0005. [DOI] [Google Scholar]
- Villa S, Lombardi A, Mangioni D, Bozzi G, Bandera A, Gori A, Raviglione MC. The COVID-19 pandemic preparedness or lack thereof: From China to Italy. Global Health & Medicine. 2020 doi: 10.35772/ghm.2020.01016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J., Shen, J., Ye, D., Yan, X., Zhang, Y., Yang, W., … & Pan, L. (2020). Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environmental Pollution, 262, 114665. [DOI] [PMC free article] [PubMed]
- Warren GW, Lofstedt R. COVID-19 vaccine rollout risk communication strategies in Europe: A rapid response. Journal of Risk Research. 2021;24(3/4):369–379. doi: 10.1080/13669877.2020.1870533. [DOI] [Google Scholar]
- Whitten GD, Green KW, Zelbst PJ. Triple-A supply chain performance. International Journal of Operations & Production Management. 2012;32(1):28–48. doi: 10.1108/01443571211195727. [DOI] [Google Scholar]
- Wilson DT. An integrated model of buyer-seller relationships. Journal of the Academy of Marketing Science. 1995;23(4):335–345. doi: 10.1177/009207039502300414. [DOI] [Google Scholar]
- Wise, J. (2021). Covid-19: Countries rally to support India through “storm that has shaken the nation”. BMJ: British Medical Journal, 373. [DOI] [PubMed]
- Wolfswinkel JF, Furtmueller E, Wilderom CP. Using grounded theory as a method for rigorously reviewing literature. European Journal of Information Systems. 2013;22(1):45–55. doi: 10.1057/ejis.2011.51. [DOI] [Google Scholar]
- Worldometer. (2021). Countries where COVID-19 has spread. https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread/ Accessed on 30 August 2021.
- Xu G, Feng Z, Wu H, Zhao D. Swift trust in a virtual temporary system: A model based on the Dempster-Shafer theory of belief functions. International Journal of Electronic Commerce. 2007;12(1):93–126. doi: 10.2753/JEC1086-4415120104. [DOI] [Google Scholar]
- Xu H, Zhang L, Onireti O, Fang Y, Buchanan WJ, Imran MA. BeepTrace: Blockchain-enabled privacy-preserving contact tracing for COVID-19 pandemic and beyond. IEEE Internet of Things Journal. 2020 doi: 10.1109/JIOT.2020.3025953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Xie H, Yu G, Liu M. Antecedents and consequences of supply chain risk management capabilities: An investigation in the post-coronavirus crisis. International Journal of Production Research. 2021;59(5):1573–1585. doi: 10.1080/00207543.2020.1856958. [DOI] [Google Scholar]
- Yang Q, Wang Q, Zhao X. A taxonomy of transaction-specific investments and its effects on cooperation in logistics outsourcing relationships. International Journal of Logistics Research and Applications. 2019;22(6):557–575. doi: 10.1080/13675567.2018.1552931. [DOI] [Google Scholar]
- Yapijakis C. Hippocrates of Kos, the father of clinical medicine, and Asclepiades of Bithynia, the father of molecular medicine. In Vivo. 2009;23(4):507–514. [PubMed] [Google Scholar]
- Yu, Y., Li, Y., Zhang, Z., Gu, Z., Zhong, H., Zha, Q., … & Chen, E. (2020). A bibliometric analysis using VOSviewer of publications on COVID-19. Annals of translational medicine, 8(13), 816. 10.21037/atm-20-4235 [DOI] [PMC free article] [PubMed]
- Zheng L, Xiao C, Chen F, Xiao Y. Design and research of a smart monitoring system for 2019-nCoV infection-contact isolated people based on blockchain and Internet of things technology. Research Square. 2020;12(1):1–11. doi: 10.21203/rs.3.rs-18678/v1. [DOI] [Google Scholar]
- Zolin, R. (2002). Swift trust in hastily formed networks. The Hastily Formed Networks Research Group. http://www.nps.edu/Cebrowski/Docs/swifttrust100302.pdf