Abstract
Background
Missense mutations in the mitochondrial alanyl-tRNA synthetase 2 (AARS2) gene are clinically associated with infantile mitochondrial cardiomyopathy or adult-onset leukoencephalopathy with early ovarian failure. To date, approximately 40 cases have been reported related to AARS2 mutations, while its genetic and phenotypic spectrum remains to be defined.
Case presentation
We identified a 24-year-old Chinese female patient with adult-onset leukoencephalopathy carrying novel compound heterozygous pathogenic mutations in the AARS2 gene (c.718C > T and c.1040 + 1G > A) using a whole-exome sequencing approach.
Conclusions
Our findings further extend the mutational spectrum of AARS2-related leukoencephalopathy and highlight the importance of the whole-exome sequencing in precisely diagnosing adult-onset leukoencephalopathies.
Keywords: AARS2, Leukoencephalopathy, Gene mutation, White matter, Ovarian failure
Background
Since mitochondrial DNA (mtDNA) spans only about 16.5 kilobase pairs (kbp), it primarily relies on the nuclear-encoded proteins for transcriptional and translational regulation of its own housekeeping genes. Mutations in these mitochondrial genes are increasingly viewed as a cause of neurological disorders in humans. The alanyl-tRNA synthetase 2 (AARS2, OMIM612035) gene, located on chromosome 6p21.1, is a nuclear gene that encodes mitochondria-specific alanyl-tRNA synthetase enzyme, which plays a crucial role in mitochondrial translation [1]. AARS2 gene mutations cause two separate and extremely rare clinical phenotypes, namely infantile mitochondrial cardiomyopathy [2] and adult-onset leukoencephalopathy with early ovarian failure [3, 4]. Due to the broader application of next-generation sequencing in clinical practice, we have been able to recognize the expanding phenotypic spectrum of AARS2 mutations, including a benign phenotype without leukoencephalopathy and lethal primary pulmonary hypoplasia [5, 6]. Notably, some reported cases of familial pulmonary hypoplasia with AARS2 mutations had been linked to the European founder (c.1774C > T variant) [5]. Phenotypic heterogeneity is also evident in individuals with identical AARS2 variants [5]. Therefore, a better understanding of this devastating disease is urgently warranted. Here, we reported novel AARS2 mutations [c.718C > T (p. Leu240Phe) and c.1040 + 1G > A] associated with adult-onset leukoencephalopathy and early ovarian failure in a 24-year-old female patient. Clinical features, brain magnetic resonance imaging (MRI) characteristics and genetic testing performed during the diagnosis are presented in this case study.
Case presentation
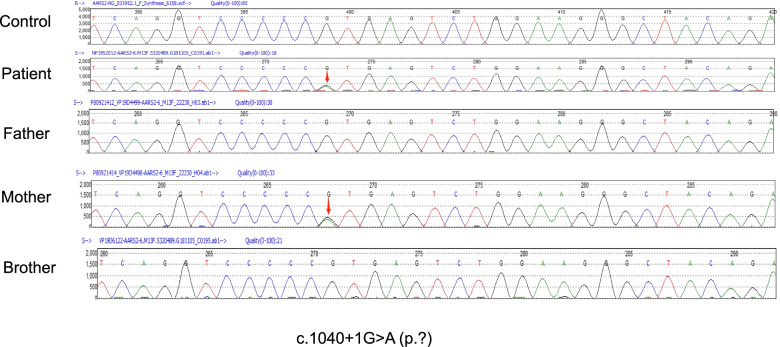
A 24-year-old female patient was admitted to the Department of Neurology at Liaocheng People's Hospital due to persistent amenorrhea for 2 years and weakness of both lower limbs for the past 10 months. She had no remarkable medical history, except for raising the head and walking later than other children of the same age. There was no problem with the pregnancy or delivery and also no history of drug abuse or hallucinations. No consanguineous marriage in her family was reported. She had irregular menstruation with prolonged menstrual cycles. The first symptom of amenorrhea or absence of menstruation was recorded when the patient was 22 years old. The patient felt like stepping on cotton when walking, and it was a little bit difficult for her to stand up after sitting. At the initial phase, these clinical symptoms were slightly improved after a short period of symptomatic manifestations. However, she started to seclude herself from social activities, while her bilateral lower extremity weakness progressively deteriorated without a remitting period. She also exhibited signs of cognitive decline and abnormal mental behaviors. For example, she had a slow reaction time and always presented delayed responses to doctor’s questions. Reduced communicative participation was noted in this patient during the initial screening. Her calculating and reading abilities were also decreased progressively. She had been suffering from motor function deficits (lower limb tremor, bradykinesia and rigid muscles), requiring active physical assistance for daily activities. Upon neurological evaluation, her muscle strengths of all four limbs were graded as 4-/5. A decreased sense of vibration and numbness of lower limbs were recorded in lower extremities. Moderate station ataxia (Romberg test) and tandem walking tests were not feasible in this patient. The tendon reflexes of lower limbs were sightly active and other remarkable signs, including bilateral Babinski sign and Kernig sign, were not evident. Routine laboratory investigations indicated normal renal and hepatic functions. The endocrinological hormone profiling in the serum showed that the levels of estradiol were 33.473 pg/ml (Reference ranges, follicular phase: 26.6–161 pg/ml; luteal phase: 187–382 pg/ml; ovulation: 187–382 pg/ml; menopause: 5.37–38.4 pg/ml), luteinizing hormone was 55.7mIU/ml (Reference ranges, follicular phase: 2.58–12.1 mIU/ml; luteal phase: 0.83–15.5 mIU/ml; menopause: 13.1–86.5 mIU/ml), and follicle-stimulating hormone was 87.9 mIU/ml (Reference ranges, follicular phase: 1.98–11.6 mIU/ml; luteal phase: 1.38–9.58 mIU/ml; menopause: 21.5–131 mIU/ml). Blood tests for the levels of very-long-chain fatty acids and lysosomal enzyme activities were unremarkable. T2-weighted sagittal and fluid-attenuated inversion recovery (FLAIR) images revealed white matter hyperintensities and abnormal signals on bilateral periventricular regions, corona radiata, and corpus callosum (Fig. 1A-C). White matter rarefaction was visible on FLAIR. Restricted diffusion in selective white matter was noted (Fig. 1D). Magnetic resonance spectroscopy (MRS) showed an increased ratio of Cho and Cr in frontal lesions (Fig. 1E). Whole-exome sequencing results indicated that the exon4 of the AARS2 gene contained a missense mutation at c.718C > T (p.Leu240Phe) in this proband (Fig. 2), when matched with the HG19 reference genome sequence and the transcript variant NM_020745.3. In silico analyses using multiple bioinformatics methods suggested this mutation as ‘probably damaging’. Furthermore, an alternative splicing mutation (c.1040 + 1G > A) was also noted (Fig. 3), as confirmed by in silico analysis (a pathological variant). Both transcript variants were not previously reported in the general population database and might have deleterious effects. The father of this patient carried a heterozygous AARS2 gene mutation (c.1040 + 1G > A), and the mother also had a heterozygous mutation c.718C > T in the same gene. The patient’s brother did not show either of these variants. Coenzyme complex treatment and glucocorticoid therapy had no therapeutic impact on this patient. During the recent follow-up visit, her health condition was found to be worsened further, and the patient’s movement was mostly restricted to bed.
Fig. 1.
Brain magnetic resonance imaging of this patient (A-D) Axial T1W1, T2WI, fluid-attenuated inversion recovery (FLAIR) and diffuse weighted imaging (DWI), respectively. T1-hypointense and hyperintense signal abnormalities on T2W1 and FLAIR can be noted around the corpus callosum and bilateral ventricles. Diffusion restriction in selective white matter was noted. E Magnetic resonance spectroscopy (MRS) showed an increased Cho/Cr ratio in frontal lesions
Fig. 2.
AARS2 gene mutations (missense mutation) in the patient and her father. The patient had a missense mutation in the AARS2 gene c.718C > T (p.Leu240Phe). The variant was transmitted paternally (red arrows)
Fig. 3.
AARS2 gene mutation (splicing mutation) in the patient and her mother. The patient had a splicing mutation in the AARS2 gene c.1040 + 1G > A (p.?). The variant was transmitted maternally (red arrows)
Discussion and conclusions
In this study, we reported the case of a Chinese female patient diagnosed with adult-onset leukoencephalopathy who mainly suffered from prematurely terminated menstruation and progressive motor decline following the disease onset. Brain MRI symmetrical features suggested genetic leukoencephalopathies. Genetic analysis revealed that the patient carried novel compound heterozygous pathogenic mutations in the AARS2 gene (c.718C > T and c.1040 + 1G > A). These compound heterozygous mutations were co-segregated with the disease phenotype in her family. Both variants were predicted to be pathogenic by in silico analysis. The c.1040 + 1G > A in the AARS2 gene was reported to be associated with frontotemporal dementia in a Korean patient [7], while the c.718C > T has not been reported in the literature. We have carefully ruled out other possibilities based on the patient’s medical background and the presence of pathogenic mutations in the AARS2 gene in her parents, and a definitive diagnosis of AARS2-related leukoencephalopathy was made.
AARS2 is a nuclear-encoded mitochondrial enzyme that is essential for the mitochondrial translation machinery. AARS2 protein contains several functional domains, such as the aminoacylation domain, editing domain, and C-terminal domain [8]. Diseases associated with the AARS2 gene mutations include missense, nonsense and/or frameshift alterations in both alleles, consistent with an autosomal recessive inheritance, which can lead to mitochondrial respiratory chain complex deficiency and metabolic dysfunctions [9]. Pathogenic AARS2 variants were first identified in infants suffering from cardiomyopathy since the heart has a higher content of mitochondria to meet energy demand. Patients with infantile mitochondrial cardiomyopathy caused by AARS2 mutations usually have combined complex I and III deficiencies, while individuals with AARS2-related leukoencephalopathy exhibit an isolated complex IV deficiency [10–12]. Studies have suggested that infantile mitochondrial cardiomyopathy with AARS2 gene mutations are most frequently noted in the editing domain of the enzyme that severely compromises its aminoacylation capacity [13]. By contrast, milder variants may cause a partial decrease in the AARS2’s synthetase function associated with leukoencephalopathy and premature ovarian insufficiency [5, 13].
It is important to note that patients with AARS2-related leukoencephalopathy may be erroneously named as hereditary diffuse leukoencephalopathy with spheroids (HDLS) due to the clinical as well as histopathological similarities between these two diseases [14, 15]. HDLS was first named by a Swedish research group in 1984 [16]. Later, the AARS gene mutation (p.Cys152Phe) was identified as a possible cause in the original Swedish HDLS family, who were negative for CSF1R gene mutation [17]. Screening for pathogenic AARS2 gene mutations is thus needed to be recommended in selective CSF1R-negative leukoencephalopathy individuals [3]. Furthermore, the average age of onset of these two rare diseases is distinct, with AARS2-related leukoencephalopathy being 27.3 years [18] and CSF1R-related leukoencephalopathy being 41.4 years [19]. Our reported AARS2-related leukoencephalopathy patient suffered from typical clinical symptoms including ceased menstruation, cognitive decline, and decreased strength of limbs in her 20’s, which were consistent with previous case reports. However, it is important to note that the onset age has a wide range and may not be sufficient to distinguish them clinically.
AARS2-related leukoencephalopathy is reportedly less common than CSF1R-related leukoencephalopathy. With approximately 40 cases caused by AARS2 gene mutations have been reported in the literature [20], we have just begun to recognize the wide genetic and phenotypic spectrum related to AARS2 gene mutations. The whole-exome sequencing has emerged as a powerful approach in the diagnosis of adult-onset leukoencephalopathies, and more collaborative efforts are needed in order to improve better therapeutic management.
Acknowledgements
Not applicable
Abbreviations
- MtDNA
Mitochondrial DNA
- AARS2
Alanyl-tRNA synthetase 2
- MRI
Magnetic resonance imaging
- FLAIR
Fluid-attenuated inversion recovery
- MRS
Magnetic resonance spectroscopy
- HDLS
Hereditary diffuse leukoencephalopathy with spheroids
- CSF1R
Colony stimulating factor 1 receptor
Authors’ contributions
FY, CT and YY: study design. FY, HJ and CT: data collected. HJ: manuscript writing. All authors contributed to the article and approved the submitted version.
Funding
Not applicable.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
As this case was not involved in any experimental interventions, no formal research ethics approval was required.
Consent for publication
The relatives of this patient provided written informed consent to the publication of the information and images related to this manuscript. This report does not contain any personal information that could lead to the identification of the patient.
Competing interests
The authors declare that they have no conflict of interests and that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yan Fan and Jinming Han contributed equally to this work.
Contributor Information
Jinming Han, Email: hanjinming1202@126.com.
Yanyan Yang, Email: 442667324@qq.com.
References
- 1.Fine AS, Nemeth CL, Kaufman ML, Fatemi A. Mitochondrial aminoacyl-tRNA synthetase disorders: an emerging group of developmental disorders of myelination. J Neurodev Disord. 2019;11:29. doi: 10.1186/s11689-019-9292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gotz A, Tyynismaa H, Euro L, Ellonen P, Hyotylainen T, Ojala T, Hamalainen RH, Tommiska J, Raivio T, Oresic M, et al. Exome sequencing identifies mitochondrial alanyl-tRNA synthetase mutations in infantile mitochondrial cardiomyopathy. Am J Hum Genet. 2011;88:635–642. doi: 10.1016/j.ajhg.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch DS, Zhang WJ, Lakshmanan R, Kinsella JA, Uzun GA, Karbay M, Tufekcioglu Z, Hanagasi H, Burke G, Foulds N, et al. Analysis of Mutations in AARS2 in a Series of CSF1R-Negative Patients With Adult-Onset Leukoencephalopathy With Axonal Spheroids and Pigmented Glia. JAMA Neurol. 2016;73:1433–1439. doi: 10.1001/jamaneurol.2016.2229. [DOI] [PubMed] [Google Scholar]
- 4.Wang D, Yu M, Zhang W, Wang Z, Yuan Y. AARS2 Compound Heterozygous Variants in a Case of Adult-Onset Leukoencephalopathy With Axonal Spheroids and Pigmented Glia. J Neuropathol Exp Neurol. 2018;77:997–1000. doi: 10.1093/jnen/nly087. [DOI] [PubMed] [Google Scholar]
- 5.Kiraly-Borri C, Jevon G, Ji W, Jeffries L, Ricciardi JL, Konstantino M, Ackerman KG, Lakhani SA: Siblings with lethal primary pulmonary hypoplasia and compound heterozygous variants in the AARS2 gene: further delineation of the phenotypic spectrum. Cold Spring Harb Mol Case Stud. 2019;5(3):a003699. 10.1101/mcs.a003699. [DOI] [PMC free article] [PubMed]
- 6.De Michele G, Galatolo D, Lieto M, Maione L, Cocozza S, Santorelli FM, Filla A. New AARS2 Mutations in Two Siblings With Tremor, Downbeat Nystagmus, and Primary Amenorrhea: A Benign Phenotype Without Leukoencephalopathy. Mov Disord Clin Pract. 2020;7:684–687. doi: 10.1002/mdc3.12991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim EJ, Kim YE, Jang JH, Cho EH, Na DL, Seo SW, Jung NY, Jeong JH, Kwon JC, Park KH, et al. Analysis of frontotemporal dementia, amyotrophic lateral sclerosis, and other dementia-related genes in 107 Korean patients with frontotemporal dementia. Neurobiol Aging. 2018;72:186 e181–186 e187. doi: 10.1016/j.neurobiolaging.2018.06.031. [DOI] [PubMed] [Google Scholar]
- 8.Song C, Peng L, Wang S, Liu Y. A novel compound heterozygous mutation in AARS2 gene (c.965 G > A, p.R322H; c.334 G > C, p.G112R) identified in a Chinese patient with leukodystrophy involved in brain and spinal cord. J Hum Genet. 2019;64:979–983. doi: 10.1038/s10038-019-0648-7. [DOI] [PubMed] [Google Scholar]
- 9.Srivastava S, Butala A, Mahida S, Richter J, Mu W, Poretti A, Vernon H, VanGerpen J, Atwal PS, Middlebrooks EH, et al. Expansion of the clinical spectrum associated with AARS2-related disorders. Am J Med Genet A. 2019;179:1556–1564. doi: 10.1002/ajmg.a.61188. [DOI] [PubMed] [Google Scholar]
- 10.Seo GH, Oh A, Kim EN, Lee Y, Park J, Kim T, Lim YM, Kim GH, Kim CJ, Yoo HW, et al. Identification of extremely rare mitochondrial disorders by whole exome sequencing. J Hum Genet. 2019;64:1117–1125. doi: 10.1038/s10038-019-0660-y. [DOI] [PubMed] [Google Scholar]
- 11.Dallabona C, Diodato D, Kevelam SH, Haack TB, Wong LJ, Salomons GS, Baruffini E, Melchionda L, Mariotti C, Strom TM, et al. Novel (ovario) leukodystrophy related to AARS2 mutations. Neurology. 2014;82:2063–2071. doi: 10.1212/WNL.0000000000000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang X, Wang Q, Tang H, Chen B, Dong X, Niu S, Li S, Shi Y, Shan W, Zhang Z. Novel Alanyl-tRNA Synthetase 2 Pathogenic Variants in Leukodystrophies. Front Neurol. 2019;10:1321. doi: 10.3389/fneur.2019.01321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Euro L, Konovalova S, Asin-Cayuela J, Tulinius M, Griffin H, Horvath R, Taylor RW, Chinnery PF, Schara U, Thorburn DR, et al. Structural modeling of tissue-specific mitochondrial alanyl-tRNA synthetase (AARS2) defects predicts differential effects on aminoacylation. Front Genet. 2015;6:21. doi: 10.3389/fgene.2015.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konno T, Kasanuki K, Ikeuchi T, Dickson DW, Wszolek ZK. CSF1R-related leukoencephalopathy: A major player in primary microgliopathies. Neurology. 2018;91:1092–1104. doi: 10.1212/WNL.0000000000006642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han J, Sarlus H, Wszolek ZK, Karrenbauer VD, Harris RA. Microglial replacement therapy: a potential therapeutic strategy for incurable CSF1R-related leukoencephalopathy. Acta Neuropathol Commun. 2020;8:217. doi: 10.1186/s40478-020-01093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Axelsson R, Roytta M, Sourander P, Akesson HO, Andersen O. Hereditary diffuse leucoencephalopathy with spheroids. Acta Psychiatr Scand Suppl. 1984;314:1–65. [PubMed] [Google Scholar]
- 17.Sundal C, Carmona S, Yhr M, Almstrom O, Ljungberg M, Hardy J, Hedberg-Oldfors C, Fred A, Bras J, Oldfors A, et al. An AARS variant as the likely cause of Swedish type hereditary diffuse leukoencephalopathy with spheroids. Acta Neuropathol Commun. 2019;7:188. doi: 10.1186/s40478-019-0843-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tang Y, Qin Q, Xing Y, Guo D, Di L, Jia J. AARS2 leukoencephalopathy: A new variant of mitochondrial encephalomyopathy. Mol Genet Genomic Med. 2019;7:e00582. doi: 10.1002/mgg3.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen J, Luo S, Li N, Li H, Han J, Ling L. A Novel Missense Mutation of the CSF1R Gene Causes Incurable CSF1R-Related Leukoencephalopathy: Case Report and Review of Literature. Int J Gen Med. 2020;13:1613–1620. doi: 10.2147/IJGM.S286421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Axelsen TM, Vammen TL, Bak M, Pourhadi N, Stenor CM, Gronborg S. Case report: 'AARS2 leukodystrophy'. Mol Genet Metab Rep. 2021;28:100782. doi: 10.1016/j.ymgmr.2021.100782. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.