Abstract
Objectives:
To examine post-traumatic stress disorder (PTSD) among Black adults in younger, middle, and older ages.
Methods:
Using nationally representative data from the National Survey of American Life, we estimated lifetime and 12-month prevalence of PTSD in Black men and women ages 18–34, 35–49, and 50+. We determined PTSD persistence and severity by age group, then associations of PTSD with socio-economic status, chronic stress, and racial discrimination in middle age.
Results:
The lifetime prevalence of PTSD was higher in Black women/men ages 18–34 (prevalence=14.0%/6.3%) and 35–49 (12.8%/4.6%) versus 50 and older (8.7%/5.1%). Those ages 35–49 were more likely than younger/older Black adults to have severe interference in work, relationships, and activities domains. In middle age, PTSD was associated with unemployment, lower education, poverty, and stress in Black men, and unemployment, divorce, poverty, stress, and discrimination in Black women.
Discussion:
Black women experience a disproportionate burden of PTSD in middle age.
Keywords: Post-Traumatic Stress Disorder, Disability, Work, Poverty, Discrimination
Post-traumatic stress disorder (PTSD) is a common and disabling mental health disorder, with about one in fifteen U.S. adults meeting criteria for PTSD during the lifetime (Alegria et al., 2013; Goldstein et al., 2016). In contrast to typical patterns of racial disparities where Black Americans (including African Americans and/or Caribbeans of African descent) have equivalent or lower lifetime prevalence compared to Whites (Thomas Tobin et al., 2020), the prevalence of PTSD is higher among Black Americans, especially Black women, with nearly one in eight African American women experiencing PTSD at some point during their lifetime (Valentine et al., 2019). When present, PTSD among Black Americans is often chronic, severe and goes untreated (Hale et al., 2018; Himle et al., 2009; Jones et al., 2020; Mays et al., 2018; Nobles, Valentine, Gerber, et al., 2016). Among Black Americans especially, PTSD is associated with increased risks for diabetes and hypertension (Nobles, Valentine, Borba, et al., 2016), as well as heart disease and stroke (Vidal et al., 2018). PTSD often co-occurs with other psychiatric disorders, such as Major Depressive Disorder and substance use disorders, and contributes to chronic illness and poor health outcomes (Carter et al., 2020; Nichter et al., 2019; Sommer et al., 2019). Some have even speculated that PTSD may play a role in Black women’s disparities in maternal mortality and birth outcomes (Seng et al., 2011; Villarosa, 2018). Moreover, the risk of developing PTSD extends into middle and older age in Black populations (Himle et al., 2009), potentially contributing to disability and impairment in later life (Jones et al., 2022).
There are a number of factors known to contribute to the excess burden of PTSD among Black adults in the U.S. including elevated exposure to types of potentially traumatic events that confer risk for PTSD, such as childhood maltreatment, physical and sexual assault, and military combat (McLaughlin et al., 2019; Roberts et al., 2011). In addition to specific types of trauma, cumulative trauma exposure and limited psychosocial resources contribute to elevated PTSD risk in Black women (Gaffey et al., 2019; Gluck et al., 2021). Faced with the cumulative stressors associated with race, class, and gender oppression, Black women tend to be especially vulnerable to persistent poverty and interpersonal violence that contribute to increased risk of meeting criteria for PTSD (Lacey et al., 2021; Mekawi et al., 2021). Additionally, there is growing evidence of the association of racial discrimination on the course of PTSD and negative health outcomes (Bird et al., 2021; Brooks Holliday et al., 2020; Mekawi et al., 2020; Sibrava et al., 2019; Vines et al., 2017). Pre-trauma exposure to racial discrimination is associated with increased risk for PTSD in Black adults following a traumatic event (Bird et al., 2021). Experiences of discrimination contribute to neurobiolologic changes in emotion regulation (Fani et al., 2021), adding to the severity of PTSD (Mekawi et al., 2021; Mekawi et al., 2020). There is also evidence that PTSD is a mediating pathway through which racial discrimination contributes to Black-White disparities in cardiovascular-related conditions (Gavin et al., 2021).
While prior research has examined the prevalence and risk factors of PTSD in Black Americans overall, our understanding of PTSD across the life course and its burden remains limited. Studies that have examined PTSD at different stages of adulthood have focused on prevalence, finding that lifetime prevalence is often greatest among Black Americans in young adulthood (Himle et al., 2009). Other studies focused on PTSD persistence and severity have tended to control for age, rather than examining the burden of PTSD among Black adults of varying ages (Jones et al., 2020; Mays et al., 2018; Sibrava et al., 2019). Because discrimination occurs among Blacks Black Americans of all ages, there may be an increased burden of PTSD among Black adults in middle and older ages in terms of severity of PTSD interference and downstream consequences for health and social outcomes. Identifying the characteristics of PTSD at different ages across the lifespan may thus be an important component in identifying interventions to reduce health disparities.
This study uses a life course approach to document the prevalence, persistence, and severity of PTSD among Black adults varying in age. We focus specifically on the lifetime and 12-month prevalence of PTSD among Black men and women; their disorder persistence and severity of interference in work, home, relationship, and social domains; and associations of lifetime PTSD with social disadvantage, chronic stress, and experiences of racial discrimination. Examining these features of PTSD across multiple periods of adulthood may offer a more comprehensive view of PTSD among Black populations and inform the development of age- and race-specific mental health treatments.
Methods
Study Design and Procedures
We conducted a cross-sectional analysis of data from the National Survey of American Life (NSAL), a nationally representative, population-based survey of mental health and mental health services use among Black Americans (Jackson, Neighbors, et al., 2004). Drawing on Diagnostic and Statistical Manual of Mental Disorders 4th Edition (DSM-IV) criteria, the NSAL is the largest survey of psychiatric disorders among Black Americans to date. As described elsewhere, the overall response rate was 72.3% (Jackson, Neighbors, et al., 2004). Respondents included 5,191 Black adults, of whom n=1,856 were younger (ages 18–34), n=1,774 were in the middle-age group (ages 35–49), and n=1,561 were ages 50 or older.
Measures
Lifetime and 12-Month Prevalence.
The NSAL assessed probable lifetime and twelve-month DSM-IV psychiatric disorders using a fully structured interview: the World Health Organization’s Composite International Diagnostic Interview (WHO-CIDI) (Jackson, Torres, et al., 2004; World Health Organization, 2017–2018). The WHO-CIDI section assessed exposure to 22 potentially traumatic events, including accidents, natural disasters, interpersonal violence from a parent, romantic partner or stranger, kidnapping, sexual assault, military combat, refugee, civilian in a war zone, and witnessing violence to others. Respondents who affirmed exposure to a potentially traumatic event were asked about PTSD symptoms specific to the traumatic event, age of trauma and first age of PTSD symptoms, and the most recent time at which they experienced PTSD symptoms. Our analysis focused on respondents who met PTSD criteria at any time during the lifetime, and those who met criteria within the 12 months prior to the interview.
Persistence.
We identified respondents who experienced PTSD in two time periods spanning more than 12 months apart. Specifically, persistence was estimated for the subsample of respondents who met criteria for PTSD during the lifetime and who also reported an age of onset at least two years prior to the interview. We calculated the proportion of this subsample who also met criteria for PTSD in the twelve months prior to the interview (Jones et al., 2020; Mays et al., 2018). This measure captures chronic and/or recurring PTSD.
Severity of Impairment.
We used the Sheehan Disability Scale to characterize PTSD severity in the twelve months prior to the interview (Leon et al., 1997). The Sheehan Disability Scale assesses the extent to which a disorder interferes with roles in four domains: 1) ability to clean, shop and take care of the home; 2) work; 3) ability to form and maintain close relationships; and 4) social life (Leon et al., 1997). Respondents were asked to think about a month in the prior year when their symptoms were most severe, and then rate the extent to which symptoms interfered with each role domain on a 0–10 scale. Severity, calculated separately for each domain, was classified as “mild” if respondents rated their interference as 0–3, “moderate” if they rated interference as 4–6, and “severe” if they rated interference as 7–10 (Levine et al., 2013).
Demographic and Socio-economic Variables.
The NSAL measured demographic and socio-economic characteristics, including gender, ethnicity (African American or Caribbean Black), employment status (employed, unemployed, out of the workforce), education (high school or less vs. more), marital status (married or cohabitating, widowed, separated, or divorced, single), geographic region of the U.S. (northeast, south, Midwest, west), health insurance status (yes or no), and having a usual source of care. Low income was defined as living in a household with an annual income less than 138% of the Federal Poverty Level. We combined responses from two items assessing marital status and number of children in the household to determine if respondents were single parents (yes or no).
Chronic Stress.
The survey asked respondents whether they had experienced any of 10 chronic stressors during the previous month such as problems related to health, money, employment, law enforcement, or family. We counted the number of stressors endorsed, then categorized the total as 0, 1, 2, or 3 or more.
Racial Discrimination.
The NSAL included a 10-item version of the Everyday Discrimination Scale to measure the frequency of routine experiences of unfair treatment (Carden et al., 2021; Williams et al., 1997). Responses ranged from never (1) to nearly every day (6). We summed responses to the 10 items to create a total discrimination score, then created a 2-level measure splitting the index at the median for low (0) versus high (1) racial discrimination.
Statistical Analysis
All statistical analyes were conducted in SAS (SAS Institute Inc., 2005), using design variables to adjust for the complex sampling design of the NSAL and a post-stratification weight We first examined the distribution of sociodemographics, chronic stress and perceived discrimination for respondents in younger, middle, and older age groups. We then used cross-tabulations to estimate lifetime and 12 month prevalence of PTSD for Black men and women in each age group. We report weighted study proportions and their standard errors. Similar procedures were used to determine disorder persistence and severity across the lifespan in the subsamples meeting lifetime and 12-month disorder criteria, respectively.
To better understand PTSD-related morbidity, we used cross-tabulations to examine the distribution of sociodemographic characteristics, chronic stress, and perceived discrimination of those with a lifetime history of PTSD, compared to those with no lifetime PTSD. Analyses, conducted separately for men and women, were limited to those in age groups with elevated PTSD prevalence and severity.
Results
Sociodemographic Characteristics and Prevalence of DSM-IV Post-Traumatic Stress Disorder Socioeconomic Status, Chronic Stress and Discrimination.
There were some notable differences in the sociodemographic characteristics of Black adults across age groups (Table 1). Those age 18–34, compared to those in middle and older age groups, were more likely to be unemployed, never married, and single parents (p-values<0.001). Those age 50 and older, compared to Black adults in younger and middle age groups, were more likely to be out of the work force, widowed, and to have health insurance and a usual source of care (p-values<0.001). Black adults age 35–49, compared to those who were younger or older, had the greatest chronic stress (p<0.001). They were also more likely than the other groups to experience higher levels of racial discrimination (56.8% versus 52.1% and 42.3%; p<0.001).
Table 1.
Demographic Characteristics, Chronic Stress, Discrimination and PTSD Prevalence among Black Adults in Younger, Middle, and Older Age Groups in the National Survey of American Life
| Age 18–34 (n=1856) |
Age 35–49 (n=1774) |
Age 50 and older (n=1561) |
|||||
|---|---|---|---|---|---|---|---|
| %1 | SE | % | SE | % | SE | p-value | |
| Gender | 0.53 | ||||||
| Men | 44.1 | 1.6 | 48.8 | 1.3 | 43.5 | 1.5 | |
| Women | 55.9 | 1.6 | 54.2 | 1.3 | 56.5 | 1.5 | |
| Ethnicity | 0.04 | ||||||
| African American | 91.9 | 0.8 | 93.5 | 0.6 | 93.8 | 0.7 | |
| Caribbean Black | 8.1 | 0.8 | 6.5 | 0.6 | 6.2 | 0.7 | |
| Employment | <0.001 | ||||||
| Employed | 74.8 | 1.4 | 78.4 | 1.7 | 45.9 | 2.1 | |
| Unemployed | 59.1 | 14.5 | 39.5 | 9.6 | 18.7 | 5 | |
| Out of workforce | 10.7 | 1 | 12.0 | 1.2 | 49.1 | 2.2 | |
| Education | <0.001 | ||||||
| Some college or greater | 38.8 | 2.1 | 43.5 | 1.9 | 33.2 | 1.8 | |
| No college | 61.2 | 2.1 | 56.5 | 1.9 | 66.8 | 1.8 | |
| Marital Status | <0.001 | ||||||
| Married/cohabitating | 32.9 | 1.6 | 50.6 | 1.8 | 44.2 | 1.7 | |
| Widowed | 0.3 | 0.1 | 1.3 | 0.3 | 23.9 | 1.2 | |
| Separated/divorced | 6.4 | 1.0 | 26.8 | 1.4 | 24.1 | 1.5 | |
| Never married | 60.4 | 1.9 | 21.4 | 1.6 | 7.8 | 0.9 | |
| Single parent | 25.1 | 1.2 | 13.8 | 1.3 | 6.0 | 0.8 | <0.001 |
| Region | 0.70 | ||||||
| Northeast | 20.4 | 1.4 | 17.2 | 1.4 | 17.6 | 1.9 | |
| Midwest | 17.3 | 2.4 | 17.8 | 1.7 | 18.3 | 2.5 | |
| South | 54.2 | 2.9 | 54.2 | 2.6 | 54.7 | 3.0 | |
| West | 8.1 | 1.1 | 10.7 | 1.4 | 9.4 | 2.1 | |
| Insured | 76.9 | 1.4 | 81.6 | 1.3 | 87.7 | 1.3 | <0.001 |
| Has usual source of care | 79.2 | 1.4 | 86.6 | 1.2 | 93.2 | 0.9 | <0.001 |
| Income below 138% FPL | 36.8 | 2.3 | 28.8 | 1.9 | 33.4 | 1.9 | 0.003 |
| Chronic stress | <0.001 | ||||||
| 0 | 23.6 | 1.7 | 21.6 | 1.7 | 31.9 | 1.7 | |
| 1 | 26.7 | 1.5 | 24.2 | 1.2 | 30.8 | 1.6 | |
| 2 | 22.0 | 1.4 | 24.0 | 1.5 | 30.0 | 23.3 | |
| 3 or more | 27.7 | 1.8 | 30.2 | 1.7 | 14.0 | 1.0 | |
| High racial discrimination | 52.1 | 1.7 | 56.8 | 2.1 | 42.3 | 2.0 | <0.001 |
| Lifetime PTSD | |||||||
| Overall | 10.6 | 1.0 | 9.1 | 0.9 | 7.1 | 0.8 | <0.001 |
| Men | 6.3 | 1.5 | 4.6 | 1.1 | 5.1 | 1.4 | 0.67 |
| Women | 14.0 | 1.3 | 12.8 | 1.4 | 8.7 | 1.1 | 0.007 |
| 12 Month PTSD | |||||||
| Overall | 5.1 | 0.9 | 3.6 | 0.6 | 2.8 | 0.6 | 0.08 |
| Men | 3.4 | 1.0 | 2.2 | 0.8 | 2.6 | 1.1 | 0.70 |
| Women | 6.4 | 1.1 | 4.7 | 0.8 | 2.9 | 0.6 | 0.02 |
Abbreviations: FPL = federal poverty level; PTSD = post-traumatic stress disorder; SE = standard error
Survey-weighted percent
p-values from Rao-Scott test, a version of X2 that accounts for the complex sampling design and survey weights
Lifetime Prevalence.
About one in ten Black adults ages 18–34 met criteria for PTSD during the lifetime, compared to one in eleven Black adults age 35–49 and one in fourteen of those ages 50 and older (p<0.001). The age patterning of PTSD was also observed in women, with about one in seven Black women age 18–34 meeting PTSD criteria during the lifetime compared to one in eight Black women age 35–49 and just one in twelve of Black women ages 50 and older (p<0.001). In Black men, there were no statistical differences in the prevalence of PTSD across the three age groups. Among those in the younger, middle, and older age groups, about one in twenty Black men (5–6%) met PTSD criteria.
12 Month Prevalence.
The age patterning of disorder prevalence was less pronounced when examining PTSD criteria in the 12 months prior to the interview. About one in twenty Black adults met 12-month PTSD criteria, compared to about one in thirty Black adults age 35–49, and one in thirty-five of those ages 50 and older (p=0.08). There were no statistical differences in the 12-month prevalence of PTSD across the age groups of Black men (p=0.70). In Black women, however, the 12-month prevalence of PTSD was greater for those age 18–34 (6.4%) compared to those age 35–49 (4.7%) and those age 50 and older (2.9%; p=0.02).
Persistence of Post-Traumatic Stress Disorder
Nearly half of Black adults age 18–34 who met criteria for PTSD during the lifetime also met criteria in the 12 months prior to the interview (47.4%; results not tabled). Among middle age and older Black adults, just two in five of those PTSD experienced a persistent disorder (39.6% and 40.3% among those ages 35–49 and 50 or older, respectively). There was no statistical difference in the percentage of adults who met persistence criteria across age groups (p=0.56).
Severity of Interference from Post-Traumatic Stress Disorder
Of the three age groups, Black adults in middle-age reported the greatest severity of interference from their disorder, with unique patterns by domain of interference (Figure 1).
Figure 1.
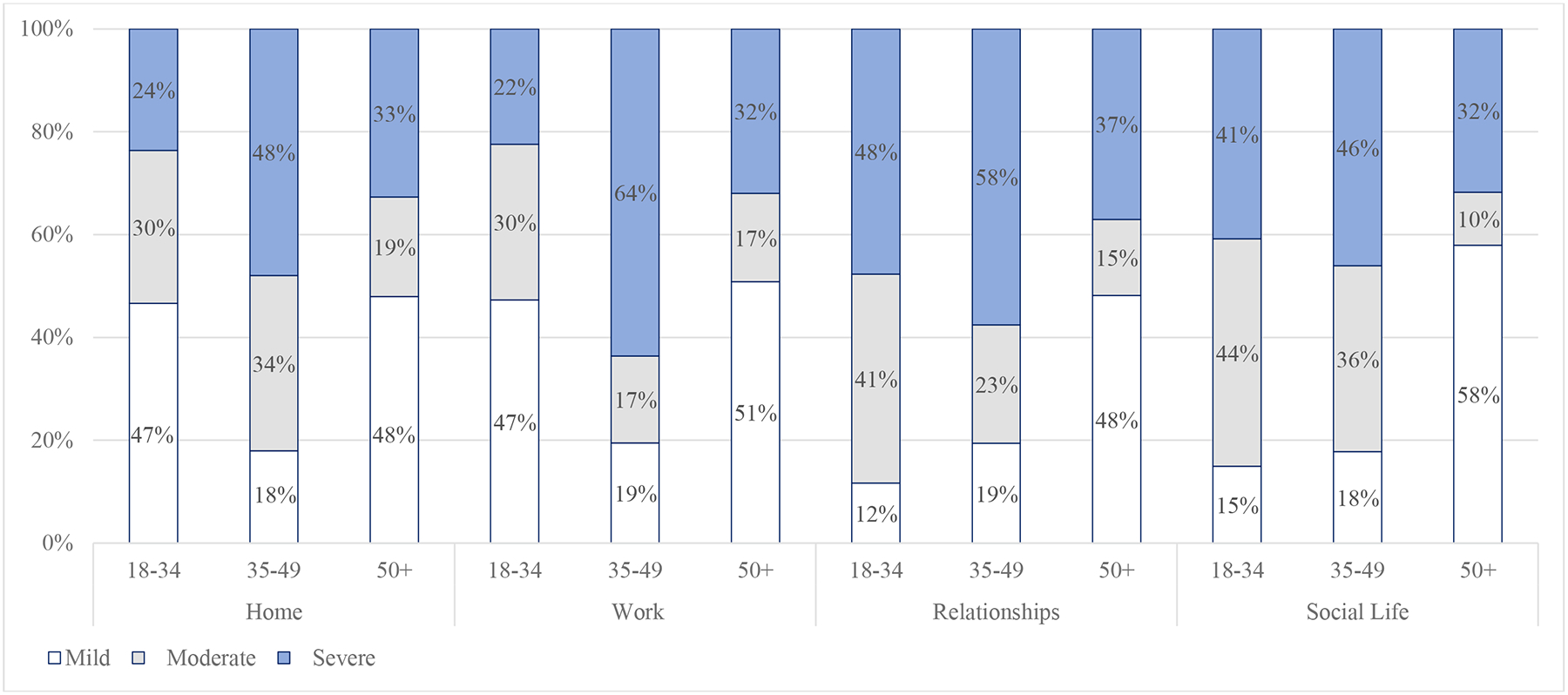
Severity of interference among Black adults who met DSM-IV criteria for PTSD in the prior 12 months, by age and interference domain in the National Survey of American Life
Home.
Black adults age 35–49 experienced the greatest interference from PTSD in their home responsibilities (p=0.07). One half of Black adults in the middle age group reported severe interference in their ability to clean, shop and take care of the home (47.9%). Among those ages 18–34, about one in four reported severe home interference (23.6%); while among those ages 50 and older, just one in three reported moderate or severe home interference (32.7%).
Work.
Black adults age 35–49 also experienced the greatest interference from PTSD in their ability to work (p=0.004). Two in three middle-age Black adults reported severe work interference (63.6%), compared to about one in four of those age 18–34 (22.4%) and one in three of those ages 50 and older (32.0%).
Relationships.
Black adults with PTSD in younger and middle age experienced severe interference in their ability to form and maintain close social relationships (p<0.001). Among those age 18–34, more than four in five reported moderate or severe interference with social relationships (40.7% and 47.7% had moderate and severe interference, respectively). A similar pattern was observed among those age 35–49, with four in five experiencing moderate or severe interference with relationships (23.1% and 57.5%); while about one-half of those age 50 and older experience moderate or severe relationship interference (14.8% and 37.0%).
Social Life.
A similar pattern was observed for social activities, with younger and middle-age Black adults experience greater PTSD interference with social activities when compared to older Black adults (p<0.001). Among those age 18–34, more than four in five reported moderate or severe interference with social activities (46.1% and 40.8% had moderate and severe interference, respectively). Among those age 35–49, four in five also experienced moderate or severe interference with their social life (36.2% and 46.1%), compared to about two in five in those age 50 and older (10.3% and 31.8% had moderate and severe social interference, respectively).
Associations of Socioeconomic Characteristics, Chronic Stress and Discrimination with Post-Traumatic Stress Disorder in Middle Age
Among Black adults age 35–49, having a lifetime history of PTSD was associated with disadvantage in several areas. Those with a history of PTSD were more likely to be unemployed or out of the work force, compared to those who did not meet PTSD criteria during the lifetime (p<0.001). They were more likely to be separated or divorced (p<0.001), to be single parents (p=0.02), and to live in households with very low income (p’s<0.001). In addition, those with a lifetime history of PTSD experienced more chronic stress compared to those without PTSD (p<0.001).
Factors associated with PTSD differed among Black men and women in middle age. For instance, Black men who met criteria for PTSD during the lifetime were much less likely than men without any history of PTSD to be employed and have at least some college education (p-values<0.01). They were more likely to live in households with very low income (p=0.003), and to experience higher levels of chronic stress (p<0.001). Black women who met criteria for PTSD during the lifetime were more likely than women without any history of PTSD to be separated or divorced (p=0.007). They were also more likely to be unemployed or out of the work force (p=0.03), and to experience poverty (p=0.02), chronic stress (p<0.001), and greater race-based discrimination (p=0.05).
Discussion
Results of our study underscore that looking only at prevalence of PTSD in Black Americans as a group misses some of the important distinctive burdens that occur as a function of the challenges faced across the life course. While prior studies have found that Black Americans experience the greatest immediate risk of PTSD in their late teens and early adulthood (Himle et al., 2009), our results suggest an elevated burden of PTSD in middle age through lifetime prevalence, severity of interference with home, work, relationships and social activities, and substantial levels of chronic stress. This has important implications for successfully navigating unique cultural and socioeconomic tasks of middle age such as work, gaining economic security, social relationships, childbearing and caretaking of both children and parents.
We also observed gender patterns in the burden of PTSD, with women having greater lifetime and 12-month PTSD prevalence than men, particularly in younger and middle ages, and unique associations of PTSD with socioeconomic disadvantage in middle age. Of particular concern was our observation of declines in educational attainment in middle-age Black men with PTSD and increases in marriage separation in middle-age Black women with PTSD. These results are consistent with those from earlier studies which found that PTSD onset was associated with elevated rates of divorce (Breslau et al., 2011; Kessler et al., 1998). Because Black women are more likely than Black men to be single parents, and single parenthood was associated with PTSD in the overall sample, these findings have implications for maternal and child health. Without treatment, PTSD has detrimental impacts on maternal-infant bonding, parenting quality, and early child relationships (Erickson et al., 2019).
In contrast to the patterns observed in studies of physical health, older Black adults in our study experienced the lowest lifetime prevalence of PTSD and the least severe interference from PTSD in home, relationships, and social activities. These findings intuitively do not map onto life course perspectives of health, where the prevalence of chronic disease and health disparities are seen increasingly in both middle and older age (Sommer et al., 2021). There are several thoughts about the lower prevalence and severity of PTSD observed in older Black adults in the NSAL data. One is there may be survivor effects as Black Americans tend to die prematurely and those who participate in our 50+ sample have survived and may have developed effective coping strategies. PTSD also increases mortality risk (Giesinger et al., 2020; Trivedi et al., 2020), which would also contribute to potential survivor effects. The second may be cohort effects. There is evidence from another study of PTSD and aging in the general U.S. population (Reynolds et al., 2016) that older adults report lower prevalence of types of traumatic events (e.g., interpersonal violence, sexual assault) that confer PTSD risk in Black women (Lacey et al., 2021). In another paper in this issue, post traumatic events (PTE) in older Black adults were found to be associated with depressive symptoms and psychological distress (Brooks et al., 2022); when screened and found in the 12-months prior to the interview, PTEs were treated with anti-depressants. The most commonly experienced types of PTEs in their study were having someone close die unexpectedly, seeing someone badly injured, being mugged, having a life-threatening illness, and being in a life-threatening car accident (Brooks et al., 2022). The good news is that despite experiencing such PTEs they did not go on in large numbers based on our results to advance to PTSD.
A third possibility, discussed in other papers, involves psychological theories of successful aging (Reynolds et al., 2016) and cognitive theories on stress processing and emotional regulation in older adults (Jones et al., 2022). We do know that PTSD as well as other anxiety disorders are persistent and contribute to increased disability in older age (Jones et al., 2022, even if the disorder is not perceived to offer severe interference. According to the Selective Optimization with Compensation Model (Baltes & Baltes, 1990), successful aging occurs when people selectively attend to activities and thoughts that contribute to well-being and reduced stress, and they have developed compensatory strategies that enable them to continue these pursuits even as their health and other resources decline with age. Building on this premise, Carstensen and colleagues (1999) developed the Socioemotional Selectivity Theory, which contends that as people age emotion regulation goals are more at work by older adults who are invested in enjoying the present. Tull and colleagues (2020) provide examples of several studies using various methodologies indicating that emotional control in adults increases with age and overall self-reported levels of negative emotion decreases with increased ages. (Gross, 2015a, 2015b; Gross & Levenson, 1997; Lawton et al., 1992). Tull et al (2020) also provide studies with evidence that older adults report less distress than younger adults in particular stressful situations that includes daily hassles, property loss, as well as interpersonal conflict. In preliminary results of an interview study underway by the senior author there was a noticeable difference in reporting about the experiences of racism in Black men ages 18–24, 40–60 and 65+ years of age. While older men recounted horrendous examples of racism which for some were life-threatening, it was clear they were looking forward rather than backwards about the incidents. Some of the older men in response to the request to talk about their worst experience of racism indicated that they had not talked about or shared the event since its occurrence. In contrast the fervor and upset in which the youngest group relayed their experiences signaled the ways in which those incidents were still being experienced as stressful and unresolved.
In middle age, in contrast to older age, Black men and women experience chronic stress in multiple domains, including those related to health, money, and employment. These stressors were heightened in Black men and women who have experienced PTSD. We also see, particularly for Black women, chronic stressors associated with PTSD and structural racism interfere with achieving the tasks of middle age. There are likely multiple pathways by which discrimination, which is not only race-based at the individual level but also includes structural racism associated with work, poverty, and disintegration of social relationships, is linked with stress and PTSD. In a prior study, work-related stress due to unfair treatment in the workplace, being overqualified for jobs in which they were hired, working more than 40 hours a week, or worry about job loss, was found to mediate the relationship between major experiences of discrimination and PTSD in Black adults (Archibald, 2021). This prior work suggests that discrimination is a source of stress that confers risk for PTSD. In the present study, we found that middle-age Black adults with PTSD often experience severe interferences in their work, relationships, and social activities. Thus, it is likely also the case that PTSD adds to chronic stress in work and other domains through task and relationship interference.
The findings illustrate a need for research into the mechanisms that link discrimination, chronic stress, PTSD and health in Black men and women in middle age. Identifying the mechanisms through which discrimination contributes to PTSD morbidity will be essential for designing interventions to reduce health disparities. Indeed, the stress burden associated with PTSD likely contributes to weathering and allostatic load effects increasing contributions to physical health disparities and shorten life expectancies (Giesinger et al., 2020; Nobles, Valentine, Borba, et al., 2016). Examination of data from the Nurses’ Health study as well as a meta-analysis review suggests that PTSD may be associated with premature senescence-early or accelerated aging (Lohr et al., 2015; Roberts et al., 2015; Roberts et al., 2017). Another area in need of critical examination is if and how PTSD as a consequence of discrimination may be a contributing factor in maternal and infant morbidity and mortality for Black women.
We note study limitations. First, the sample is limited to non-institutionalized adults living in U.S. households. Given that histories of incarceration, homelessness and active-duty military service confer risk for PTSD, our estimates of PTSD prevalence in Black men and women across the life course are likely conservative. Second, assessment of traumatic events and PTSD symptoms were collected retrospectively and may be subject to recall bias. This could have bearing on our lifetime estimates particularly among older Black adults. We cannot in the present study determine if our finding of lower prevalence and severity of PTSD in Black adults age 50 and older are due to declines in recall with aging, cohort effects, cognitive strategies for dealing with stressful events or survivor effects. Third, the data was cross-sectional in nature, raising concerns of potential reverse causality. The present study was not able to determine if socioeconomic factors like unemployment and poverty were the probable drivers of the development of PTSD risk in Black men and women (McLaughlin et al., 2013; Steenkamp et al., 2017) or, conversely, if severity of PTSD interference contributed to a reduction in Black adults’ educational, employment and economic opportunities – relationships that are sometimes observed in longitudinal studies of psychiatric disorders in the general U.S. population (Burnett-Zeigler et al., 2013; Mojtabai, Stuart, Hwang, Eaton, et al., 2015; Mojtabai, Stuart, Hwang, Susukida, et al., 2015). Longitudinal studies of Black adults’ mental health would help to clarify the temporal nature of discrimination, PTSD, employment, stress, and poverty across the life span. Finally, it is important to acknowledge heterogeneity within the Black population in the U.S. (Tamier, 2021). Prior studies have found elevated risk for late life PTSD onset in Black adults of Caribbean origin (Himle 2009). The present study was underpowered to examine cultural and immigration factors that may contribute to PTSD prevalence and severity in older Caribbean groups. This is an important area of inquiry for future studies.
This is the first large population-based, nationally represented study of Black adults to our awareness that has had a sufficient sample to apply a developmental perspective in the investigation of PTSD. The study despite its limitations adds several contributions to our knowledge of PTSD in Black adults including that burden as measured by prevalence, severity and persistence varies in its impact by developmental stages and gender. The findings underscore the need for mental health care for PTSD in Black Americans, using a developmental lens to increase successful accomplishment of developmental milestones. Successfully meeting these milestones in middle-age benefits not just the individual but they have implications for the parenting of Black children, family and social relations which are sources of support both emotionally and economically and in the caretaking of parents. Innovative solutions will be needed to expand treatment access during early adult years when being uninsured is often highest. Even with increases in insurance coverage for young adults that occurred through the Affordable Care Act, Black adults are more likely than Whites to be uninsured (Kaiser Family Foundation, 2019), and they experience other barriers to mental health treatment (e.g., stigma, mistrust of the health care system, healthcare discrimination, costs) that are not addressed through insurance expansions alone (Alang, 2019; Hudson et al., 2018; Mays et al., 2017). Addressing these barriers is critical and, in designing PTSD interventions for young Black mothers, it may be important to combine evidence-based treatments with therapies that target parenting and attachment relationships to advance maternal-child health (Erickson et al., 2019).
In middle age, treatment access remains important for preventing and managing chronic health conditions, as does aiding coping strategies to combat chronic stress and promote emotional well-being. Given the link between PTSD and employment outcomes (Stevenson et al., 2021), it may be important to develop PTSD treatment that can be delivered within the context of vocational training programs to mitigate poor economic outcomes in middle age and beyond as has been shown with anxiety disorders (Himle et al., 2019). In addition, as discussed in another paper in this issue, for older Black men and women, there is a need to implement age and culturally targeted screening measures within the primary care setting to help identify, diagnose and treat PTSD (Jones et al., 2022). Finally, our results further demonstrate the undercurrent of racial discrimination that persists throughout the life course and its relationship to PTSD prevalence and severity in Black women in particular (Sibrava et al., 2019). Public health and health system strategies that confront structural racism will be needed to reduce the elevated burden of PTSD in Black Americans overall, and to advance the economic, health, and social outcomes for Black men and women with PTSD across the life course.
Table 2.
Demographic and Socioeconomic Characteristics, Chronic Stress, and Discrimination among Black Men and Women in Middle Age, by Lifetime PTSD from the National Survey of American Life
| Overall | Men | Women | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No PTSD (n=1553) |
PTSD (n=152) |
No PTSD (n=592) |
PTSD (n=28) |
No PTSD (n=961) |
PTSD (n=124) |
||||||||||
| %1 | SE | % | SE | p-value2 | % | SE | % | SE | p-value | % | SE | % | SE | p-value | |
| Ethnicity | |||||||||||||||
| African American | 93.4 | 0.6 | 92.6 | 1.8 | 0.70 | 93.7 | 0.8 | 85.4 | 8.1 | 0.20 | 93.1 | 0.6 | 94.8 | 1.2 | 0.19 |
| Caribbean Black | 6.6 | 0.6 | 7.4 | 1.8 | 6.3 | 0.8 | 14.6 | 8.1 | 6.9 | 0.6 | 5.2 | 1.2 | |||
| Employment | <0.001 | <0.001 | 0.03 | ||||||||||||
| Employed | 81.0 | 1.8 | 58.6 | 5.4 | 85.9 | 1.9 | 45.0 | 12.0 | 76.5 | 2.6 | 62.7 | 6.1 | |||
| Unemployed | 8.6 | 1.4 | 22.0 | 3.8 | 7.2 | 1.7 | 33.5 | 11.3 | 9.9 | 1.5 | 18.5 | 4.0 | |||
| Out of workforce | 10.4 | 1.1 | 19.4 | 4.1 | 6.9 | 1.3 | 21.5 | 10.4 | 13.5 | 1.9 | 18.8 | 4.3 | |||
| Education | 0.40 | 0.008 | 0.97 | ||||||||||||
| Some college or greater | 44.3 | 2.2 | 38.3 | 6.2 | 43.3 | 3.1 | 14.4 | 7.6 | 45.1 | 2.4 | 45.4 | 6.8 | |||
| No college | 55.7 | 2.2 | 61.7 | 6.2 | 56.7 | 3.1 | 85.6 | 7.6 | 54.9 | 2.4 | 54.6 | 6.8 | |||
| Marital Status | <0.001 | 0.15 | 0.007 | ||||||||||||
| Married/cohabitating | 52.4 | 1.9 | 38.2 | 4.4 | 59.8 | 3.0 | 36.8 | 12.4 | 45.8 | 2.5 | 38.6 | 5.2 | |||
| Widowed | 1.1 | 0.3 | 3.7 | 1.7 | 0.9 | 0.4 | 3.3 | 3.2 | 1.2 | 0.3 | 3.8 | 2.0 | |||
| Separated/divorced | 25.2 | 1.4 | 40.9 | 4.0 | 21.2 | 2.4 | 39.5 | 11.7 | 28.8 | 1.4 | 41.3 | 4.6 | |||
| Never married | 21.3 | 1.7 | 17.2 | 4.0 | 18.2 | 2.1 | 20.4 | 10.6 | 24.2 | 2.2 | 16.2 | 4.0 | |||
| Single parent | 13.3 | 1.3 | 22.8 | 4.8 | 0.02 | 5.3 | 1.0 | 5.4 | 5.3 | 0.98 | 20.6 | 2.2 | 28.0 | 5.8 | 0.19 |
| Region | 0.008 | 0.11 | 0.08 | ||||||||||||
| Northeast | 17.3 | 1.7 | 22.0 | 3.7 | 18.8 | 2.9 | 14.5 | 7.3 | 15.9 | 1.6 | 24.2 | 4.3 | |||
| Midwest | 15.3 | 1.1 | 26.0 | 5.5 | 12.9 | 1.6 | 32.9 | 12.2 | 17.5 | 1.9 | 23.9 | 6.3 | |||
| South | 55.9 | 2.6 | 44.8 | 5.3 | 56.3 | 3.4 | 38.9 | 10.6 | 55.5 | 2.8 | 46.5 | 6.4 | |||
| West | 11.6 | 1.6 | 7.3 | 1.8 | 12.1 | 1.5 | 13.7 | 8.8 | 11.1 | 2.1 | 5.4 | 2.0 | |||
| Insured | 82.4 | 1.5 | 74.0 | 5.4 | 0.13 | 81.3 | 1.8 | 75.5 | 10.8 | 0.37 | 83.3 | 1.9 | 74.4 | 6.6 | 0.17 |
| Has usual source of care | 86.4 | 1.2 | 87.4 | 4.4 | 0.84 | 80.7 | 2.3 | 90.5 | 6.6 | 0.29 | 91.6 | 1.1 | 86.5 | 5.5 | 0.28 |
| Income below 138% FPL | 27.3 | 1.9 | 48.3 | 5.9 | <0.001 | 20.8 | 2.6 | 48.9 | 11.5 | 0.003 | 33.2 | 2.5 | 48.1 | 7.1 | 0.02 |
| Chronic stress | <0.001 | <0.001 | <0.001 | ||||||||||||
| 0 | 23.1 | 1.8 | 5.0 | 2.3 | 29.3 | 3.0 | 6.1 | 5.1 | 17.6 | 1.6 | 4.7 | 2.6 | |||
| 1 | 25.8 | 1.4 | 8.9 | 3.0 | 29.6 | 2.3 | 0.2 | 0.2 | 22.5 | 2.0 | 11.6 | 3.6 | |||
| 2 | 24.0 | 1.6 | 22.2 | 4.0 | 22.8 | 2.4 | 20.6 | 9.6 | 25.0 | 2.0 | 22.7 | 4.2 | |||
| 3 or more | 27.0 | 1.7 | 63.8 | 4.7 | 18.3 | 2.4 | 73.1 | 10.3 | 34.9 | 2.3 | 61.0 | 5.8 | |||
| High racial discrimination | 56.7 | 2.1 | 64.3 | 4.4 | 0.08 | 59.7 | 3.5 | 66.2 | 11.8 | 0.57 | 54.0 | 2.2 | 63.8 | 5.2 | 0.05 |
Abbreviations: DSM IV = Diagnostic and Statistical Manual of Mental Disorders, 4th edition; PTSD = Post-Traumatic Stress Disorder; SE = Standard Error
Survey-weighted percent
p-values from Rao-Scott test, a version of X2 that accounts for the complex sampling design and survey weights
Funding Acknowledgments
The data collection on which this study is based was supported by the National Institute of Mental Health (NIMH; U01-MH57716), with supplemental support from the Office of Behavioral and Social Science Research at the National Institutes of Health (NIH) and the University of Michigan. Dr. Jones’ effort was supported by a Career Development Award from the Department of Veterans Affairs (VA), VA Health Services Research and Development (CDA 19-233, Award No IK2HX003090). The preparation of this manuscript was supported by grants from National Institute on Minority Health and Health Disparities (MD006923) and the National Institute of Mental Health (MH115344). The contents of this article do not represent the views of the Department of Veterans Affairs, the National Institutes of Health, or the United States Government.
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Alang SM (2019). Mental health care among blacks in america: Confronting racism and constructing solutions. Health services research, 54(2), 346–355. 10.1111/1475-6773.13115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Fortuna LR, Lin JY, Norris FH, Gao S, Takeuchi DT, Jackson JS, Shrout PE, & Valentine A (2013). Prevalence, risk, and correlates of posttraumatic stress disorder across ethnic and racial minority groups in the united states. Medical care, 51(12), 1114–1123. 10.1097/MLR.0000000000000007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archibald PC (2021). Factors influencing the relationship between work-related stress and posttraumatic stress disorder among working black adults in the united states. The Yale journal of biology and medicine, 94(3), 383–394. https://www.ncbi.nlm.nih.gov/pubmed/34602878 [PMC free article] [PubMed] [Google Scholar]
- Baltes PB, & Baltes MM (1990). Psychological perspectives on successful aging: The model of selective optimization with compensation. In Baltes PB & Baltes MM (Eds.), Successful aging: Perspectives from the behavioral sciences. Cambridge University Press. 10.1017/CBO9780511665684.003 [DOI] [Google Scholar]
- Bird CM, Webb EK, Schramm AT, Torres L, Larson C, & deRoon-Cassini TA (2021). Racial discrimination is associated with acute posttraumatic stress symptoms and predicts future posttraumatic stress disorder symptom severity in trauma-exposed black adults in the united states. Journal of traumatic stress, 34(5), 995–1004. 10.1002/jts.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Miller E, Jin R, Sampson NA, Alonso J, Andrade LH, Bromet EJ, de Girolamo G, Demyttenaere K, Fayyad J, Fukao A, Galaon M, Gureje O, He Y, Hinkov HR, Hu C, Kovess-Masfety V, Matschinger H, Medina-Mora ME, Ormel J, Posada-Villa J, Sagar R, Scott KM, & Kessler RC (2011). A multinational study of mental disorders, marriage, and divorce. Acta Psychiatr Scand, 124(6), 474–486. 10.1111/j.1600-0447.2011.01712.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks Holliday S, Dubowitz T, Haas A, Ghosh-Dastidar B, DeSantis A, & Troxel WM (2020). The association between discrimination and ptsd in african americans: Exploring the role of gender. Ethnicity & health, 25(5), 717–731. 10.1080/13557858.2018.1444150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks J, Taylor RJ, & Chatters L (2022). The impact of traumatic events on mental health among older african american and black caribbeans adults. Journal of aging and health, 34(3):390–400. 10.1177/08982643221086336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett-Zeigler I, Ilgen MA, Bohnert K, Miller E, Islam K, & Zivin K (2013). The impact of psychiatric disorders on employment: Results from a national survey (nesarc). Community mental health journal, 49(3), 303–310. 10.1007/s10597-012-9510-5 [DOI] [PubMed] [Google Scholar]
- Carden KD, McDuffie DL, Murry K, Bui C, & Allen RS (2021). Minority stress process among older black americans: The role of age, perceived discrimination, and anxiety. Aging Ment Health, 1–9. 10.1080/13607863.2021.1904380 [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, & Charles ST (1999). Taking time seriously: A theory of socioemotional selectivity. American psychologist, 54(3), 165. [DOI] [PubMed] [Google Scholar]
- Carter S, Powers A, & Bradley B (2020). Ptsd and self-rated health in urban traumatized african american adults: The mediating role of emotion regulation. Psychological trauma: theory, research, practice and policy, 12(1), 84–91. 10.1037/tra0000472 [DOI] [PubMed] [Google Scholar]
- Erickson N, Julian M, & Muzik M (2019). Perinatal depression, ptsd, and trauma: Impact on mother-infant attachment and interventions to mitigate the transmission of risk. International review of psychiatry, 31(3), 245–263. 10.1080/09540261.2018.1563529 [DOI] [PubMed] [Google Scholar]
- Fani N, Carter SE, Harnett NG, Ressler KJ, & Bradley B (2021). Association of racial discrimination with neural response to threat in black women in the us exposed to trauma. JAMA Psychiatry, 78(9), 1005–1012. 10.1001/jamapsychiatry.2021.1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffey AE, Aranda F, Burns JW, Purim-Shem-Tov YA, Burgess HJ, Beckham JC, Bruehl S, & Hobfoll SE (2019). Race, psychosocial vulnerability and social support differences in inner-city women’s symptoms of posttraumatic stress disorder. Anxiety, stress, and coping, 32(1), 18–31. 10.1080/10615806.2018.1532078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin AR, Woo B, Conway A, & Takeuchi D (2021). The association between racial discrimination, posttraumatic stress disorder, and cardiovascular-related conditions among non-hispanic blacks: Results from the national epidemiologic survey on alcohol and related conditions-iii (nesarc-iii). Journal of racial and ethnic health disparities. 10.1007/s40615-020-00943-z [DOI] [PubMed] [Google Scholar]
- Giesinger I, Li J, Takemoto E, Cone JE, Farfel MR, & Brackbill RM (2020). Association between posttraumatic stress disorder and mortality among responders and civilians following the september 11, 2001, disaster. JAMA network open, 3(2), e1920476. 10.1001/jamanetworkopen.2019.20476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluck RL, Hartzell GE, Dixon HD, Michopoulos V, Powers A, Stevens JS, Fani N, Carter S, Schwartz AC, Jovanovic T, Ressler KJ, Bradley B, & Gillespie CF (2021). Trauma exposure and stress-related disorders in a large, urban, predominantly african-american, female sample. Archives of women’s mental health, 24(6), 893–901. 10.1007/s00737-021-01141-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, Pickering RP, Ruan WJ, Huang B, & Grant BF (2016). The epidemiology of dsm-5 posttraumatic stress disorder in the united states: Results from the national epidemiologic survey on alcohol and related conditions-iii. Social psychiatry and psychiatric epidemiology, 51(8), 1137–1148. 10.1007/s00127-016-1208-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (2015a). Emotion regulation: Current status and future prospects. Psycholological inquiry, 26(1), 1–26. 10.1080/1047840X.2014.940781 [DOI] [Google Scholar]
- Gross JJ (2015b). The extended process model of emotion regulation: Elaborations, applications, and future directions. Psychological inquiry, 26(1), 130–137. 10.1080/1047840X.2015.989751 [DOI] [Google Scholar]
- Gross JJ, & Levenson RW (1997). Hiding feelings: The acute effects of inhibiting negative and positive emotion. Journal of abnormal psychology, 106(1), 95–103. 10.1037//0021-843x.106.1.95 [DOI] [PubMed] [Google Scholar]
- Hale AC, Sripada RK, & Bohnert KM (2018). Past-year treatment utilization among individuals meeting dsm-5 ptsd criteria: Results from a nationally representative sample. Psychiatric services, 69(3), 341–344. 10.1176/appi.ps.201700021 [DOI] [PubMed] [Google Scholar]
- Himle JA, Baser RE, Taylor RJ, Campbell RD, & Jackson JS (2009). Anxiety disorders among african americans, blacks of caribbean descent, and non-hispanic whites in the united states. Journal of anxiety disorders, 23(5), 578–590. 10.1016/j.janxdis.2009.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himle JA, LeBeau RT, Weaver A, Brydon DM, Bybee D, Kilbourne AM, Rose RD, Tucker KM, Kim R, Perez M, Smith FN, Sinco BR, Levine S, Hamameh N, Golenberg Z, McKiver M, Wierzbicki PT, Hasratian AM, & Craske MG (2019). Study protocol: A multisite trial of work-related cognitive behavioral therapy for unemployed persons with social anxiety. Contemporary clinical trials communications, 16, 100464. 10.1016/j.conctc.2019.100464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson DL, Eaton J, Banks A, Sewell W, & Neighbors H (2018). “Down in the sewers”: Perceptions of depression and depression care among african american men. American journal of men’s health, 12(1), 126–137. 10.1177/1557988316654864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, & Torres M (2004). Methodological innovations in the national survey of american life. International journal of methods in psychiatric research, 13(4), 289–298. https://www.ncbi.nlm.nih.gov/pubmed/15719533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, Trierweiler SJ, & Williams DR (2004). The national survey of american life: A study of racial, ethnic and cultural influences on mental disorders and mental health. International journal of methods in psychiatric research, 13(4), 196–207. https://www.ncbi.nlm.nih.gov/pubmed/15719528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AL, Cochran SD, Rafferty J, Taylor RJ, & Mays VM (2020). Lifetime and twelve-month prevalence, persistence, and unmet treatment needs of mood, anxiety, and substance use disorders in african american and u.S. Versus foreign-born caribbean women. International journal of environmental research and public health, 17(19). 10.3390/ijerph17197007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AL, Rafferty J, Cochran SD, Abelson JM, & Mays VM (2022). Persistence, impairment, disability and unmet treatment of lifetime and 12-month anxiety disorders in black men and women, 50 years of age and older. Journal of aging and health, 34(3):378–389. 10.1177/08982643221086065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2019). Uninsured rates for the nonelderly by race/ethnicity. Kaiser Family Foundation. [Google Scholar]
- Kessler RC, Walters EE, & Forthofer MS (1998). The social consequences of psychiatric disorders, iii: Probability of marital stability. Am J Psychiatry, 155(8), 1092–1096. 10.1176/ajp.155.8.1092 [DOI] [PubMed] [Google Scholar]
- Lacey KK, Mouzon DM, Parnell RN, & Laws T (2021). Severe intimate partner violence, sources of stress and the mental health of u.S. Black women. Journal of women’s health, 30(1), 17–28. 10.1089/jwh.2019.8215 [DOI] [PubMed] [Google Scholar]
- Lawton MP, Kleban MH, Rajagopal D, & Dean J (1992). Dimensions of affective experience in three age groups. Psychology and aging, 7(2), 171. [DOI] [PubMed] [Google Scholar]
- Leon AC, Olfson M, Portera L, Farber L, & Sheehan DV (1997). Assessing psychiatric impairment in primary care with the sheehan disability scale. Int J Psychiatry Med, 27(2), 93–105. 10.2190/T8EM-C8YH-373N-1UWD [DOI] [PubMed] [Google Scholar]
- Levine DS, Himle JA, Taylor RJ, Abelson JM, Matusko N, Muroff J, & Jackson J (2013). Panic disorder among african americans, caribbean blacks and non-hispanic whites. Soc Psychiatry Psychiatr Epidemiol, 48(5), 711–723. 10.1007/s00127-012-0582-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohr JB, Palmer BW, Eidt CA, Aailaboyina S, Mausbach BT, Wolkowitz OM, Thorp SR, & Jeste DV (2015). Is post-traumatic stress disorder associated with premature senescence? A review of the literature. Am J Geriatr Psychiatry, 23(7), 709–725. 10.1016/j.jagp.2015.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays VM, Jones AL, Cochran SD, Taylor RJ, Rafferty J, & Jackson JS (2018). Chronicity and mental health service utilization for anxiety, mood, and substance use disorders among black men in the united states; ethnicity and nativity differences. Healthcare (Basel), 6(2). 10.3390/healthcare6020053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays VM, Jones AL, Delany-Brumsey A, Coles C, & Cochran SD (2017). Perceived discrimination in health care and mental health/substance abuse treatment among blacks, latinos, and whites. Med Care, 55(2), 173–181. 10.1097/MLR.0000000000000638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Alvarez K, Fillbrunn M, Green JG, Jackson JS, Kessler RC, Sadikova E, Sampson NA, Vilsaint CL, Williams DR, & Alegria M (2019). Racial/ethnic variation in trauma-related psychopathology in the united states: A population-based study. Psychological medicine, 49(13), 2215–2226. 10.1017/S0033291718003082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry, 52(8), 815–830 e814. 10.1016/j.jaac.2013.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekawi Y, Carter S, Brown B, Martinez de Andino A, Fani N, Michopoulos V, & Powers A (2021). Interpersonal trauma and posttraumatic stress disorder among black women: Does racial discrimination matter? Journal of trauma & dissociation : the official journal of the International Society for the Study of Dissociation (ISSD), 22(2), 154–169. 10.1080/15299732.2020.1869098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekawi Y, Watson-Singleton NN, Kuzyk E, Dixon HD, Carter S, Bradley-Davino B, Fani N, Michopoulos V, & Powers A (2020). Racial discrimination and posttraumatic stress: Examining emotion dysregulation as a mediator in an african american community sample. European journal of psychotraumatology, 11(1), 1824398. 10.1080/20008198.2020.1824398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Stuart EA, Hwang I, Eaton WW, Sampson N, & Kessler RC (2015). Long-term effects of mental disorders on educational attainment in the national comorbidity survey ten-year follow-up. Soc Psychiatry Psychiatr Epidemiol, 50(10), 1577–1591. 10.1007/s00127-015-1083-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Stuart EA, Hwang I, Susukida R, Eaton WW, Sampson N, & Kessler RC (2015). Long-term effects of mental disorders on employment in the national comorbidity survey ten-year follow-up. Soc Psychiatry Psychiatr Epidemiol, 50(11), 1657–1668. 10.1007/s00127-015-1097-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichter B, Norman S, Haller M, & Pietrzak RH (2019). Physical health burden of ptsd, depression, and their comorbidity in the u.S. Veteran population: Morbidity, functioning, and disability. Journal of psychosomatic research, 124, 109744. 10.1016/j.jpsychores.2019.109744 [DOI] [PubMed] [Google Scholar]
- Nobles CJ, Valentine SE, Borba CP, Gerber MW, Shtasel DL, & Marques L (2016). Black-white disparities in the association between posttraumatic stress disorder and chronic illness. Journal of psychosomatic research, 85, 19–25. 10.1016/j.jpsychores.2016.03.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobles CJ, Valentine SE, Gerber MW, Shtasel DL, & Marques L (2016). Predictors of treatment utilization and unmet treatment need among individuals with posttraumatic stress disorder from a national sample. General hospital psychiatry, 43, 38–45. 10.1016/j.genhosppsych.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds K, Pietrzak RH, Mackenzie CS, Chou KL, & Sareen J (2016). Post-traumatic stress disorder across the adult lifespan: Findings from a nationally representative survey. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry, 24(1), 81–93. 10.1016/j.jagp.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Roberts AL, Agnew-Blais JC, Spiegelman D, Kubzansky LD, Mason SM, Galea S, Hu FB, Rich-Edwards JW, & Koenen KC (2015). Posttraumatic stress disorder and incidence of type 2 diabetes mellitus in a sample of women: A 22-year longitudinal study. JAMA Psychiatry, 72(3), 203–210. 10.1001/jamapsychiatry.2014.2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the united states. Psychological medicine, 41(1), 71–83. 10.1017/S0033291710000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Koenen KC, Chen Q, Gilsanz P, Mason SM, Prescott J, Ratanatharathorn A, Rimm EB, Sumner JA, Winning A, De Vivo I, & Kubzansky LD (2017). Posttraumatic stress disorder and accelerated aging: Ptsd and leukocyte telomere length in a sample of civilian women. Depress Anxiety, 34(5), 391–400. 10.1002/da.22620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. (2005). Sas/stat user’s guide, version 9.1. In SAS Institute Inc. [Google Scholar]
- Seng JS, Kohn-Wood LP, McPherson MD, & Sperlich M (2011). Disparity in posttraumatic stress disorder diagnosis among african american pregnant women. Archives of women’s mental health, 14(4), 295–306. 10.1007/s00737-011-0218-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibrava NJ, Bjornsson AS, Perez Benitez ACI, Moitra E, Weisberg RB, & Keller MB (2019). Posttraumatic stress disorder in african american and latinx adults: Clinical course and the role of racial and ethnic discrimination. The American psychologist, 74(1), 101–116. 10.1037/amp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommer JL, El-Gabalawy R, & Mota N (2019). Understanding the association between posttraumatic stress disorder characteristics and physical health conditions: A population-based study. Journal of psychosomatic research, 126, 109776. 10.1016/j.jpsychores.2019.109776 [DOI] [PubMed] [Google Scholar]
- Sommer JL, Reynolds K, El-Gabalawy R, Pietrzak RH, Mackenzie CS, Ceccarelli L, Mota N, & Sareen J (2021). Associations between physical health conditions and posttraumatic stress disorder according to age. Aging & mental health, 25(2), 234–242. 10.1080/13607863.2019.1693969 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Schlenger WE, Corry N, Henn-Haase C, Qian M, Li M, Horesh D, Karstoft KI, Williams C, Ho CL, Shalev A, Kulka R, & Marmar C (2017). Predictors of ptsd 40 years after combat: Findings from the national vietnam veterans longitudinal study. Depression and anxiety, 34(8), 711–722. 10.1002/da.22628 [DOI] [PubMed] [Google Scholar]
- Stevenson BJ, Mueller L, Kelly MM, & Rosenheck RA (2021). Correlates of obtaining employment among veterans receiving treatment for severe ptsd in specialized intensive programs. The Psychiatric quarterly, 92(3), 981–994. 10.1007/s11126-020-09864-w [DOI] [PubMed] [Google Scholar]
- Tamier C (2021). Key findings about black america. https://www.pewresearch.org/hispanic/2008/02/11/ii-population-projections/
- Thomas Tobin CS, Erving CL, Hargrove TW, & Satcher LA (2020). Is the black-white mental health paradox consistent across age, gender, and psychiatric disorders? Aging & mental health, 1–9. 10.1080/13607863.2020.1855627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi RB, Post EP, Piegari R, Simonetti J, Boyko EJ, Asch SM, Mori A, Arnow BA, Fihn SD, Nelson KM, & Maynard C (2020). Mortality among veterans with major mental illnesses seen in primary care: Results of a national study of veteran deaths. J Gen Intern Med, 35(1), 112–118. 10.1007/s11606-019-05307-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Vidaña AG, & Betts JE (2020). Emotion regulation difficulties in ptsd. In Tull MT & Kimbrell NA (Eds.), Emotion in posttraumatic stress disorder: Etiology, assessment, neurobiology, and treatment (pp. 295–310). Academic Press. [Google Scholar]
- Valentine SE, Marques L, Wang Y, Ahles EM, Dixon De Silva L, & Alegria M (2019). Gender differences in exposure to potentially traumatic events and diagnosis of posttraumatic stress disorder (ptsd) by racial and ethnic group. General hospital psychiatry, 61, 60–68. 10.1016/j.genhosppsych.2019.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal C, Polo R, Alvarez K, Falgas-Bague I, Wang Y, Le Cook B, & Alegria M (2018). Co-occurrence of posttraumatic stress disorder and cardiovascular disease among ethnic/racial groups in the united states. Psychosomatic medicine, 80(7), 680–688. 10.1097/PSY.0000000000000601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarosa L (2018, April 11). Why black mothers and babies are in a life-or-death crisis. New York Times. https://www.nytimes.com/2018/04/11/magazine/black-mothers-babies-death-maternal-mortality.html [Google Scholar]
- Vines AI, Ward JB, Cordoba E, & Black KZ (2017). Perceived racial/ethnic discrimination and mental health: A review and future directions for social epidemiology. Current epidemiology reports, 4(2), 156–165. 10.1007/s40471-017-0106-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yan Y, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of health psychology, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017–2018). The world health organization world mental health composite international diagnostic interview: Wmh-cidi. Retrieved May 10 from https://www.hcp.med.harvard.edu/wmhcidi/


