Abstract
Background and aim
Despite the great success of primary total hip arthroplasty (THA), the number of revisions has significantly increased over the past years. The objectives of the study were to investigate the main causes that lead to revision of THA, the time interval between primary THA and revision, and the results of the revision surgery. We also assessed whether there was any correlation between the patients’ age, BMI, diagnosis for primary THA and the cause of failure.
Methods
This paper retrospectively analyzed 189 patients with THA revision surgery performed over a six-year period, between 2015 and 2020. Patients’ charts were reviewed to collect data on patient’s demographics, patient’s primary THA and revision procedures, and the time interval between primary THA and revision surgery. Patients were divided into 3 groups according to the time interval THA-revision: group I (<5 years), group II (5–10 years) and group III (>10 years).
Results
The patients’ mean age (82 men/107 women) was 69.59±7.85 years (range 31–92 years). The most frequent revision cause was aseptic loosening (52%), followed by periprosthetic fractures (18%), infection (17%) and persistent hip instability (12%). Patients’ age (r=0.43) and BMI (r=−0.4) had low correlation with the time interval between THA and revision.
Conclusions
The main causes for revision THA within less than five years are infection and instability, while revision for aseptic loosening is performed especially after five years from the primary THA. Osteonecrosis, post-traumatic osteoarthritis and femoral neck fracture are correlated with a higher incidence of revision at less than five years from the primary THA.
Keywords: total hip replacement, arthroplasty, aseptic loosening, prosthesis failure
Background and aim
Total hip arthroplasty (THA) is the standard treatment for advanced osteoarthritis and displaced femoral neck fractures with high risk of non-union and osteonecrosis [1]. In these cases, THA reported a great success rate in many series with a follow-up longer than 10 years [2]. Despite the great success of primary arthroplasty, the number of revisions had significantly grown over the past years [3] due to the increase of life expectancy, the more frequently use of primary prosthetics, as well as THA in younger patients with increased physical activity [4]. The National Joint Registries of UK reported in 2009 a total of 959.000 arthroplasties per year, of which 12.9% are revisions of arthroplasty [5].
Important factors associated with the prosthetic longevity depend on the prosthesis design, surgical technique, and patients’ characteristics [6]. Regarding the type of prosthesis used, the actual trend shows a decrease in the use of cemented endoprostheses [7]. Concerning the correlation between the age of the primary THA and the results of this procedure, older patients have lower adherence to the recommendations, regarding recovery programs and a bigger risk for unsatisfying results [8]. Obesity, but especially morbid obesity, leads to more complicated and long-lasting intervention, with higher risk of infection and migration of the prosthetic components [9].
The most common causes of revision according to the Swedish Hip Register are aseptic loosening (75%) and osteolysis, and less frequently deep infections (8%), dislocation of the implants (6%), periprosthetic fracture (5%), or fracture of the implant (1%), along with technical errors during surgery [10]. Revisions have lower outcomes compared to primary arthroplasties [11]. Thus, revision of the THA is a much longer intervention, with many risks such as hemorrhage that increases the demand of blood transfusions, the rate of infections, as well as a higher risk for developing deep venous thrombosis with pulmonary embolism, nerve injuries or fractures of the femur [12].
The objectives of the study were to investigate the main causes that lead to revision hip arthroplasty in an orthopedic and traumatology regional center, and the time interval between primary total hip arthroplasty and revision. Furthermore, we evaluated if there is any correlation between the patients’ age, BMI, diagnosis for which primary THA was indicated and the survivorship of the primary THA.
Methods
Study design
We retrospectively analyzed all the cases that required revision of the total hip arthroplasty, performed in the Department of Orthopedics and Traumatology of Emergency Clinical County Hospital of Cluj, Romania, between January 2015 and December 2020, regardless of the cause of failure. Clinical and hospital charts were reviewed retrospectively to collect patients’ age, gender, height, weight, cause of failure, diagnosis for which primary THA was indicated, the time interval between THA and revision, and clinical and operative reports. This study was conducted with the consent of the clinic’s management in order to have access to the patients’ database, respecting their confidential data. Patients who had been treated initially with unipolar or bipolar prosthesis were excluded.
Patients were divided into 3 groups, group I: early complications (<5 years), group II: intermediate complications (5–10 years) and group III: late complications of the THA (>10 years).
The surgical technique for the revision procedure was adapted depending on the cause of failure of the primary THA.
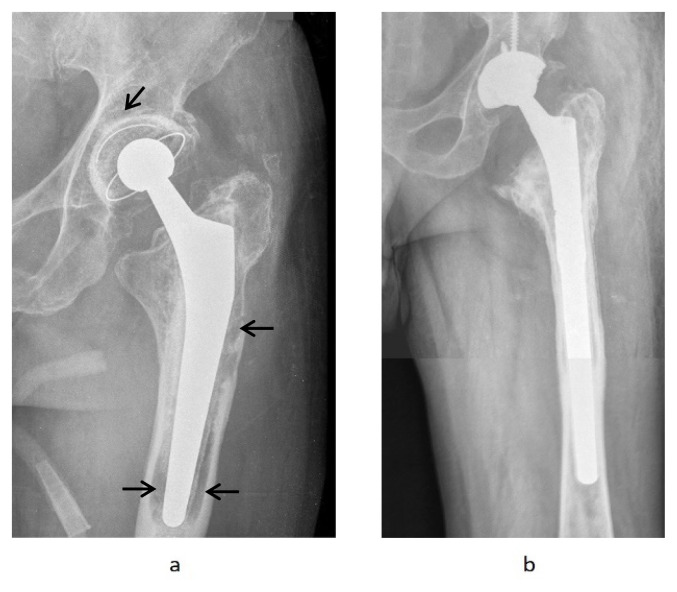
In cases of aseptic loosening or osteolysis, the implant was removed, in order to prepare the acetabular cup and the medullary canal and replaced with a revision endoprosthesis with a longer femoral stem (Figure 1). Tantalum augmentation was used if there was an important bone defect at the acetabular level (3 cases).
Figure 1.
74-year-old patient with aseptic loosening (black arrows) of the cemented THA (a) that was replaced using a cementless long femoral stem and acetabular cup, fixed with 2 screws (b).
Statistical analysis
For statistical analyses we used GraphPad Prism 6.0 for Windows. Descriptive statistics were performed for all parameters evaluated, expressed by mean ± standard deviation. Groups were compared by two-way ANOVA with post-hoc Tukey test. To establish the correlations between the variables the Pearson coefficient was used. The significance limit was established at p <0.05.
Results
One hundred eighty-nine revision arthroplasties were performed (82 men and 107 women), from a total of 1563 total hip arthroplasties (12,1%), with a mean patients’ age of 69.59±7.85 years (31–92). Regarding the type of prostheses that required revision, 115 (61%) were cemented and 74 uncemented (39%), while in the same period of time were performed 1563 primary total hip arthroplasties of which 969 (62%) uncemented and 594 (38%) cemented (Table I).
Table I.
Demographic data of patients and groups division; *statistically significant vs group I (5y).
| I: <5y | II 5–10y | >10y | |||
|---|---|---|---|---|---|
| Age (years) | 66.7±7.3 | 70.35±7.2* | 72.5±9* | ||
| Gender (M/F) | 24/31 | 21/27 | 11/23 | ||
| BMI (kg/m2) | 30.2±4.2 | 28.9±3.8* | 27.33±4* | ||
| Revision cause | Aseptic loosening | 6 | 44 | 49 | 99 |
| Periprosthetic fracture | 18 | 12 | 4 | 34 | |
| Instability | 20 | 3 | - | 23 | |
| Infection | 33 | - | - | 33 | |
| 77 | 59 | 53 | 189 | ||
Out of 189 patients, 99 (52.3%) hips were revised because of aseptic loosening of one or both prosthetic components and 34 (18%) were revised due to periprosthetic fractures. Thirty-three (17.4%) revisions were performed after infection, and twenty-three (12%) because of persistent instability of the hip.
In group I, 6 causes of revision were due to aseptic loosening (8%), 18 due to periprosthetic fractures (23%), 20 due to instability (26%) and 33 due to infection (43%). In group II, the revision was performed in 44 cases due to aseptic loosening (75%), 12 due to periprosthetic fractures (20%) and 3 due to instability (5%). In group III, there were 49 cases of aseptic loosening (92%) and 4 cases of periprosthetic fractures (8%) (Table II, III).
Table II.
Demographic data of patients and groups division; *statistically significant vs group I (5y).
| Femoral neck fracture | Osteo-arthritis | Hip dysplasia | Osteo-necrosis | Inflammatory arthritis | Post-traumatic osteoarthritis | Total | |
|---|---|---|---|---|---|---|---|
| Aseptic loosening (%) | 21 (37%) | 34 (61%) | 17 (65%) | 18 (50%) | 3 (75%) | 6 (60%) | 99 |
| Periprosthetic fracture (%) | 13 (23%) | 9 (16%) | 4 (15%) | 6 (17%) | - | 2 (20%) | 34 |
| Instability (%) | 9 (16%) | 4 (7%) | 2 (8%) | 8 (22%) | - | - | 23 |
| Infection (%) | 14 (24%) | 9 (16%) | 3 (12%) | 4 (11%) | 1 (25%) | 2 (20%) | 33 |
| Total | 57 | 56 | 26 | 36 | 4 | 10 | 189 |
Table III.
Relationship between diagnosis for primary total hip arthroplasty and time interval between THA to revision.
| Femoral neck fracture | Osteo-arthritis | Hip dysplasia | Osteo-necrosis | Inflammatory arthritis | Post-traumatic osteoarthritis | Total | |
|---|---|---|---|---|---|---|---|
| <5 years (%) | 27 (47%) | 17 (30%) | 9 (35%) | 18(50%) | 1 (25%) | 5 (50%) | 77 |
| 5–10 years (%) | 18 (32%) | 21 (38%) | 8 (30%) | 8 (22%) | 2 (50%) | 2 (20%) | 59 |
| >10 years (%) | 12 (21%) | 18 (32%) | 9 (35%) | 10 (28%) | 1 (25%) | 3 (30%) | 53 |
| Total | 57 | 56 | 26 | 36 | 4 | 10 | 189 |
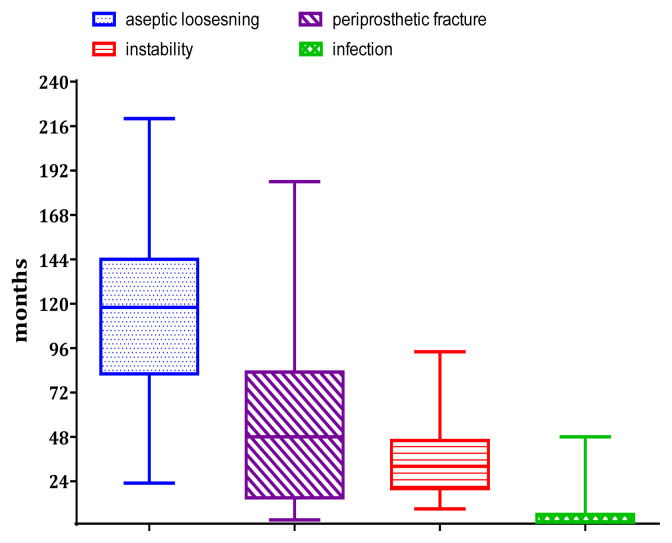
Figure 3.
Time interval between primary total hip arthroplasty and revision according to failure cause.
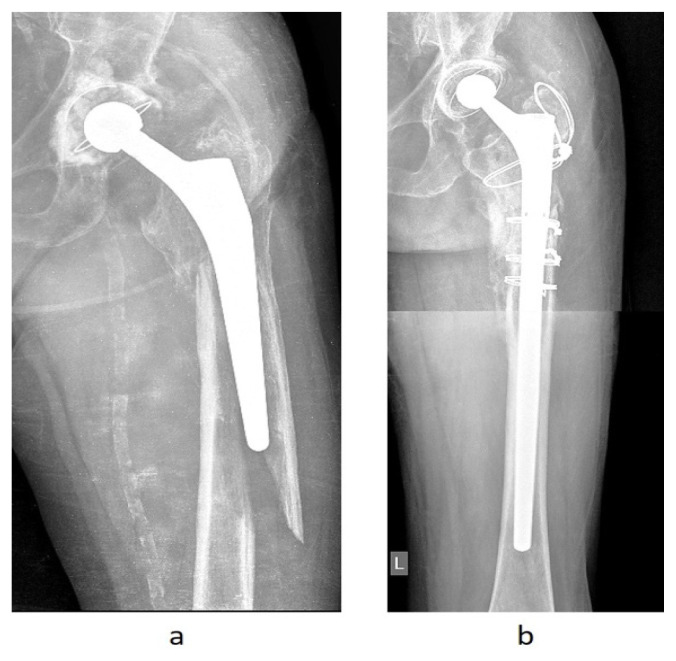
Figure 4.
Periprosthetic fracture Vancouver type B2 and aseptic loosening of the femoral component (a). Treatment of the periprosthetic fracture with cementless long femoral stem and 4 cerclage wires (b).
In group I of 77 patients, 27 had the initial diagnosis of femoral neck fracture (35%), 17 osteoarthritis (22%), 18 osteonecrosis (23%), 9 hip dysplasia (12%), 5 post-traumatic osteoarthritis (7%) and 1 inflammatory arthritis (1%). In group II, out of 59 patients, 21 initially presented with osteoarthritis (36%), 18 with femoral neck fracture (30%), 8 with hip dysplasia (14%), 8 with osteonecrosis (14%), 2 with inflammatory arthritis (3%) and 2 with post-traumatic osteoarthritis (3%). In group III, out of 53 patients, 18 presented with the initial diagnosis of osteoarthritis (34%), 12 with femoral neck fractures (23%), 10 with osteonecrosis (19%), 9 with hip dysplasia (17%), 3 with post-traumatic osteoarthritis (5%) and 1 with inflammatory arthritis (2%).
Concerning the patient’s body mass index (BMI), it was significantly higher in cases of infection (31.65±3.8 [22.9–38.2]), compared to periprosthetic fractures (27.63±4.6 [21.1–37.6]) and aseptic loosening (28.32±4 [20.7–34.8]).
The Pearson coefficient identified a low correlation between the time interval from THA to revision and patient’s age (r=0.43) or BMI (r=−0.4).
The overall time to revision was 78.2 months (0–220 months). Revision of primary total hip arthroplasty was performed because of aseptic loosening after 118 months (23–220 months), periprosthetic fracture after 56 months (3–186 months), persistent hip instability after 36 months (9–94 months) and infection after 2 months (1–48 months) from primary arthroplasty.
Discussion
The most important finding of this study was that aseptic loosening was the most common cause of revision, the average time of its appearance after the primary intervention being 118 months (23–220 months). Aseptic loosening shows an increased incidence as a cause of primary THA failure, as time passes. Six patients (8%) required revision after aseptic loosening in less than five years after primary THA, increasing to 75% between five to ten years, and over 92% of the causes of revision after ten years. The prevalence of revision surgery for aseptic loosening was 55–79% in Swedish Hip Arthroplasty Registry [11]. Aseptic loosening continues to be a major cause for revision for primary cemented arthroplasties [13]. The hip X-rays taken in more than 10% of patients with history of THA, showed an incidence of more than 30% of aseptic loosening of cemented acetabular components [14]. In our study, aseptic loosening occurred most frequently regardless of the initial cause for which primary arthroplasty was performed, with an increased incidence in the case of primary or secondary osteoarthritis.
Periprosthetic fractures are the second most frequent cause (18%) of revision THA, according to the present study. It was the second most common complication in group II (20%) and group III (8%) after aseptic loosening, and third most frequent cause of failure in group I after infections (43%) and persistent hip instability (26%). Periprosthetic fractures occurred as a result of minor traumatism in most of the cases, often as a result of undiagnosed osteolytic lesions [15]. Periprosthetic fractures were treated surgically by open reduction and internal fixation. In these situations, it is preferable that the fixation be done by cerclage wiring/cables (n=3), plates and screws (n=15), a longer femoral stem (n=6) or even by using modular tumor prosthetics (n=2). Patients with type C Vancouver fractures (diaphyseal below the implant), are treated as standard, through open reductions techniques and internal fixation specific to distal femur fractures (n=8).
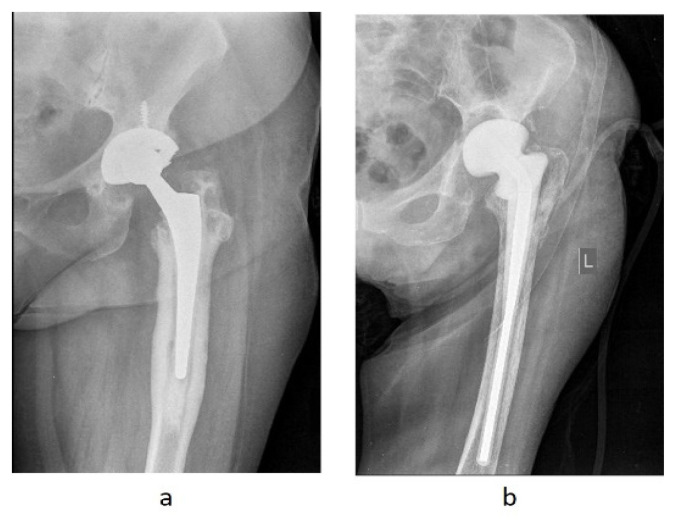
The most frequent complications that occurred in the first 5 years were infections (33 patients) and persistent hip instability (20 patients). In case of septic loosening, if the infection site is no longer active, revision arthroplasty represents a suitable procedure, considering the intervention’s aims to improve the painful symptomatology with a low risk for reinfection. In patients with early signs of infection, less than 3 weeks, the DAIR procedure can be applied (debridement, initially broad-spectrum antibiotics and specific antibiotics after antibiogram and subsequently preserving the implant) [16]. This approach has been proven efficient in some cases of knee arthroplasty and in a few smaller studies on hip arthroplasty [17]. In late presentation patients, more than 3 weeks, it is recommended to remove all the prosthesis components and insert a spacer with antibiotic, vancomycin or gentamicin (Figure 2). Then, at about 8–12 weeks, after the clinical and biological parameters of inflammation and infection (ESR, CRP, procalcitonin) are corrected, the revision procedure is performed.
Figure 2.
63-year-old patient presenting with an uncemented, infected total left hip arthroplasty. First step was the implant removal with debridement of necrotic and infected tissues, parenteral antibiotic therapy according to antibiogram result, and a hip spacer with vancomycin (b).
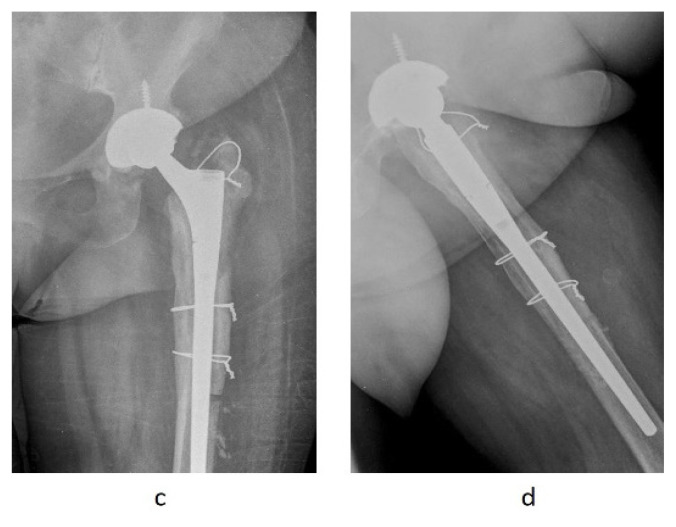
Figure 2.
63-year-old patient presenting with an uncemented, infected total left hip arthroplasty. Second step, after the relief of the inflammatory syndrome, the spacer was removed, and a revision arthroplasty was performed (c = antero-posterior image; d = axial image).
Patients with persistent hip instability (12% of total causes of revision), represented the second most common early complication (26%). The occurrence of this complication is determined by factors linked to patients, being more frequent in females older than 80 years old with neuro-muscular or cognitive deficiency as well as alcoholism or patients who suffered hip surgeries in the past [18]. On the other hand, factors regarding the surgical techniques are also linked to instability [19], such as the size of the femoral head. At this moment it’s recommended to use the 32 mm femoral head, that showed a lower rate of dislocation compared to the 28 mm, while the 36 mm or bigger didn’t show any functional improvement [20]. For the first episode of dislocation, conservative treatment is recommended, by closed reduction and 24 hours rest with progressive resumption of weight-bearing using crutches. Surgical treatment is indicated when conservative treatment fails with persistent instability, continuous pain or if the RX shows from the beginning the mal-alignment of the prothesis components. In these cases, only the modular components can be changed (e.g., femoral head (n=6), acetabular cup (n=3)), or all the components with the reinforcement of the periarticular soft tissue (n=8). For the patients who present repetitive dislocation, arthroplasty with retentive cup is preferred (n=6).
In the present study, we evaluated all the patients who required revision of total hip arthroplasty over a period of six years in an emergency medical center in Cluj-Napoca, Romania. Thus, we identified 189 revision surgery procedures, which represented 12.1% of the total hip arthroplasties performed. Out of these, 43% were performed on men and the rest of 57%, on women. The results were similar to the ones found in the National Journal Register of UK [5], and in the Swedish Hip Arthroplasty Registry [10]. Furthermore, forty-seven patients (24.8%) who required revision were under 65-year-old, 23% of women and 27% of men.
Patients who required revision THA, were divided into three groups according to the time interval between THA and the revision. Of these, 41% of the patients had complications after primary THA in less than five years, while in 31% of the cases the complications occurred between five to ten years. Late complications, at more than ten years after the primary THA, occurred in 28% of the cases. The mean age of the patients who underwent revision of the primary total hip arthroplasty, in the later complications group, was higher than in the other groups, resulting in a slightly positive correlation between age and time interval between THA and revision (r=0.43). In contrast, the body mass index of the patients was higher in the early complications group compared to the other groups, resulting a slightly negative correlation (r=−0.4). These findings were confirmed by Patel et al., who have showed that there is a weak correlation between BMI and the rate of early complications after hip arthroplasty [21]. In the patients initially presented with femoral neck fractures, short- and mid-term complications were more common, especially infections, periprosthetic fractures and instabilities. It was also found that osteonecrosis caused a significant number of instabilities after primary hip arthroplasty. In 50% of cases presented with initial diagnosis of osteonecrosis that required revision, the intervention was performed in the first 5 years. The increased incidence of complications such as instability in these patients is due to major osteo-articular and soft tissue deformities, which influence the postoperative outcome in terms of component positioning and soft-tissue strength.
However, there are some limitations of the study. First, it is a retrospective study in which patients’ charts were analyzed. The number of patients is relatively small but reflects the results of a single center, where both chronic and acute patients are treated. The clinic covers all the emergencies in the geographical area, showing an increased incidence of femoral neck fractures and periprosthetic fractures, as well as dislocations or infections of the total hip arthroplasties. Therefore, the revision interventions include not only the patients initially treated in this clinic, but also the patients treated in other orthopedic centers in the area.
Conclusion
The most common complications after total hip arthroplasty that need revision are aseptic loosening, followed by periprosthetic fractures, infections and persistent hip instability. THA indicated for osteonecrosis, post-traumatic osteoarthritis and femoral neck fracture is correlated with a higher incidence of revision at less than 5 years. While younger patients have a higher risk of needing revision surgery, an increased BMI is associated with a shorter revision surgery time.
References
- 1.Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16:596–607. doi: 10.5435/00124635-200810000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Malviya A, Abdul N, Khanduja V. Outcomes Following Total Hip Arthroplasty: A Review of the Registry Data. Indian J Orthop. 2017;51:405–413. doi: 10.4103/ortho.IJOrtho_177_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weber M, Renkawitz T, Voellner F, Craiovan B, Greimel F, Worlicek M, et al. Revision Surgery in Total Joint Replacement Is Cost-Intensive. Biomed Res Int. 2018;2018:8987104. doi: 10.1155/2018/8987104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meira EP, Zeni J., Jr Sports participation following total hip arthroplasty. Int J Sports Phys Ther. 2014;9:839–850. [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gómez-Barrena E, et al. International survey of primary and revision total knee replacement. Int Orthop. 2011;35:1783–1789. doi: 10.1007/s00264-011-1235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delaunay C, Hamadouche M, Girard J, Duhamel A SoFCOT Group. What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471:3863–3869. doi: 10.1007/s11999-013-2935-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antoniac I, Negrusoiu M, Mardare M, Socoliuc C, Zazgyva A, Niculescu M. Adverse local tissue reaction after 2 revision hip replacements for ceramic liner fracture: A case report. Medicine (Baltimore) 2017;96:e6687. doi: 10.1097/MD.0000000000006687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy BPD, Dowsey MM, Spelman T, Choong PFM. The impact of older age on patient outcomes following primary total knee arthroplasty. Bone Joint J. 2018;100-B(11):1463–1470. doi: 10.1302/0301-620X.100B11.BJJ-2017-0753.R6. [DOI] [PubMed] [Google Scholar]
- 9.Barrett M, Prasad A, Boyce L, Dawson-Bowling S, Achan P, Millington S, et al. Total hip arthroplasty outcomes in morbidly obese patients: A systematic review. EFORT Open Rev. 2018;3:507–512. doi: 10.1302/2058-5241.3.180011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKee GK, Watson-Farrar J. Replacement of arthritic hips by the McKee-Farrar prosthesis. J Bone Joint Surg Br. 1966;48:245–259. [PubMed] [Google Scholar]
- 11.Ulrich SD, Seyler TM, Bennett D, Delanois RE, Saleh KJ, Thongtrangan I, et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008;32:597–604. doi: 10.1007/s00264-007-0364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Postler AE, Beyer F, Wegner T, Lützner J, Hartmann A, Ojodu I, et al. Patient-reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int. 2017;27:180–186. doi: 10.5301/hipint.5000436. [DOI] [PubMed] [Google Scholar]
- 13.Miculescu F, Bojin D, Ciocan LT, Antoniac I, Miculescu M, Miculescu N. Experimental researches on biomaterial-tissue interface interactions. Journal of Optoelectronics and Advanced Materials. 2007;9:3303–3306. [Google Scholar]
- 14.Dattani R. Femoral osteolysis following total hip replacement. Postgrad Med J. 2007;83:312–316. doi: 10.1136/pgmj.2006.053215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JM, Kim TS, Kim TH. Treatment of Periprosthetic Femoral Fractures Following Hip Arthroplasty. Hip Pelvis. 2018;30:78–85. doi: 10.5371/hp.2018.30.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Badarudeen S, Shu AC, Ong KL, Baykal D, Lau E, Malkani AL. Complications After Revision Total Hip Arthroplasty in the Medicare Population. J Arthroplasty. 2017;32:1954–1958. doi: 10.1016/j.arth.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 17.Qasim SN, Swann A, Ashford R. The DAIR (debridement, antibiotics and implant retention) procedure for infected total knee replacement - a literature review. SICOT J. 2017;3:2. doi: 10.1051/sicotj/2016038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bracco P, Bellare A, Bistolfi A, Affatato S. Ultra-High Molecular Weight Polyethylene: Influence of the Chemical, Physical and Mechanical Properties on the Wear Behavior. A Review. Materials (Basel) 2017;10:791. doi: 10.3390/ma10070791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vigdorchik JM, D’Apuzzo MR, Markel DC, Malkani AL, Raterman S, Sharpe KP, et al. Lack of early dislocation following total hip arthroplasty with a new dual mobility acetabular design. Hip Int. 2015;25:34–38. doi: 10.5301/hipint.5000186.. [DOI] [PubMed] [Google Scholar]
- 20.Apostu D, Benea HRC, Beldean D, Oltean-Dan D, Gabri Z, Mester A, et al. The influence of component positioning on total hip replacement biomechanics. HVM Bioflux. 2020;12:22–27. [Google Scholar]
- 21.Patel AD, Albrizio M. Relationship of body mass index to early complications in hip replacement surgery: study performed at Hinchingbrooke Hospital, Orthopaedic Directorate, Huntingdon, Cambridgeshire. Int Orthop. 2007;31:439–443. doi: 10.1007/s00264-006-0222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]