ABSTRACT
Background:
In China, bereaved parents who have lost their only child are known as Shidu parents, and they tend to present high levels of prolonged grief reactions. To date, a widespread focus has been placed on positive social support, while potential negative experiences have been relatively neglected. Additionally, the role of social support from different sources (i.e. close family members [partner, siblings, grandchildren], peers, and others [relatives, friends, colleagues]) has not been examined thoroughly.
Objective:
The present study investigated whether social support from different sources has a differential impact on postloss adaptation (i.e. prolonged grief and growth). The loss-orientated and restoration-orientated coping strategies of the dual process model were also tested for their mediating roles.
Methods:
A total of 277 Chinese Shidu parents were recruited to complete a series of questionnaires including social support from different sources, prolonged grief symptoms, posttraumatic growth, and dual process coping strategies. Correlation analyses, paired sample t tests and structural equation modelling were conducted.
Results:
More positive support were related to less prolonged grief symptoms and more posttraumatic growth, while more negative support was only related to more prolonged grief. Positive support from close family members and others was significantly related to prolonged grief/growth, and negative support from these sources was significantly positively associated with prolonged grief. Positive or negative support from people who shared a similar experience was unrelated to prolonged grief/growth. Positive and negative support were related to prolonged grief and growth through loss-oriented coping strategies.
Conclusion:
Overall, the present study indicated that positive and negative support experiences from different sources functioned differently in the recovery of Chinese Shidu parents and that loss-oriented coping played a mediating role. These findings highlight the importance of differentiating social support by traits in coping with grief and the crucial mediating role of loss-oriented coping.
HIGHLIGHTS
More positive support correlated with less prolonged grief and more growth, while more negative support correlated with more prolonged grief.
Support from family members and friends was more potent than that from peers.
Social Support correlated with prolonged grief/growth through loss-oriented coping.
KEYWORDS: Social support, Chinese Shidu parents, dual process coping, grief, growth
Abstract
Antecedentes: En China, los padres en duelo que han perdido a su único hijo se conocen como padres Shidu y tienden a presentar altos niveles de reacciones de duelo prolongado. Hasta la fecha, se ha puesto general atención en el apoyo social positivo, mientras que las posibles experiencias negativas se han descuidado relativamente. Además, el papel del apoyo social de diferentes tipos (es decir, familiares cercanos [pareja, hermanos, nietos], compañeros y otros [parientes, amigos, colegas]) no se ha examinado a fondo.
Objetivo: El presente estudio investigó si el apoyo social de diferentes tipos tiene un impacto diferencial en la adaptación posterior a la pérdida (es decir, duelo prolongado y crecimiento). Las estrategias de afrontamiento orientadas a la pérdida y orientadas a la restauración del modelo de proceso dual también fueron probadas por sus roles de mediación.
Métodos: Un total de 277 padres chinos Shidu fueron reclutados para completar una serie de cuestionarios que incluían apoyo social de diferentes tipos, síntomas de duelo prolongado, crecimiento postraumático y estrategias de afrontamiento de procesos duales. Se realizaron análisis de correlación, pruebas t de muestras pareadas y modelos de ecuaciones estructurales.
Resultados: Más apoyo positivo se relacionó con síntomas de duelo menos prolongados y mayor crecimiento postraumático, mientras que un apoyo mas negativo solo se relacionó con duelo más prolongado. El apoyo positivo de familiares cercanos y otras personas se relacionó significativamente con el duelo/crecimiento prolongado, y el apoyo negativo de estos tipos se asoció significativamente de manera positiva con el duelo prolongado. El apoyo positivo o negativo de personas que compartieron una experiencia similar no estuvo relacionado con el duelo/crecimiento prolongado. El apoyo positivo y negativo se relacionó con el duelo prolongado y el crecimiento a través de estrategias de afrontamiento orientadas a la pérdida.
Conclusión: En general, el presente estudio indicó que las experiencias de apoyo positivas y negativas de diferentes tipos funcionaron de manera diferente en la recuperación de los padres chinos Shidu y que el afrontamiento orientado a la pérdida desempeñó un papel mediador. Estos hallazgos resaltan la importancia de diferenciar el apoyo social por rasgos para afrontar el duelo y el papel mediador crucial del afrontamiento orientado a la pérdida.
PALABRAS CLAVE: Apoyo social, padres chinos Shidu, afrontamiento de procesos duales, duelo, crecimiento
Abstract
背景:在中国,失去独生子女的父母被称为失独父母,他们往往会表现出较严重的哀伤反应。迄今为止,社会支持的积极体验被广泛关注,而社会支持的潜在消极体验却相对被忽视。此外,不同来源(如,亲近家人[伴侣、兄弟姐妹、孙辈]、相同经历的人、和其他[亲戚、朋友、同事])社会支持的作用尚未得到充分研究。本研究探索了不同来源的积极和消极支持对丧失后适应(即哀伤和成长)的影响,检验了双程过程模型中丧失导向和恢复导向应对策略的中介作用。
方法:本研究共招募 277 名中国失独父母完成一系列问卷调查,以评估不同来源的积极和消极支持、延长哀伤症状、创伤后成长和双程过程应对策略。使用相关分析和结构方程建模进行数据分析。
结果:较多的积极支持与更少的哀伤症状和更多的创伤后成长有关,而较多的消极支持仅与更多的哀伤症状有关。来自亲近家人和其他人的积极支持与哀伤和成长显著相关,而两种来源的消极支持与哀伤症状显著正相关。来自相似经历人的积极或消极支持与哀伤和成长无关。积极和消极的支持与哀伤和成长之间通过丧失导向应对起中介作用。
结论:总体而言,本研究表明,不同来源的积极和消极支持体验在中国失独父母的丧失后适应中发挥着不同的作用,丧失导向应对在其中起到了中介作用。这些发现强调了区分社会支持的不同特性在应对丧亲之痛中的重要性,以及丧失导向应对的关键中介作用。
关键词 : 社会支持, 中国失独父母, 双程过程应对, 哀伤, 成长
1. Introduction
Losing a child is one of the most distressing events for human beings (Djelantik, Smid, Mroz, Kleber, & Boelen, 2020; Lundorff, Holmgren, Zachariae, Farver-Vestergaard, & O’Connor, 2017). Because of the previous one-child policy, many parents in China have only one child in their lifetimes. Families who lose their only child, have not adopted a child, and are above 49 years old are officially viewed as Shidu families. In Chinese culture, children are the centre of the family and it is hoped they will perpetuate the family and take care of their elderly relatives (Hildebrandt, 2019). Influenced by these cultural factors, Shidu parents may experience a series of psychological and social stressors and exhibit severe mental health problems. For example, previous research has shown that Chinese Shidu families become dysfunctional, with a strong tendency for social withdrawal (He, Tang, Zhu, & Wang, 2014; Su, 2015). Furthermore, a large-sample survey indicated that over one-third of Chinese Shidu parents suffered from potential posttraumatic stress disorder, major depressive disorder, or prolonged grief disorder (Zhou et al., 2018, 2020). Despite this, researchers have that some Shidu parents could recover from the loss and even experience positive changes (Xu et al., 2020, 2021). They may show a tendency of posttraumatic growth, including changes in self-cognition, a more profound understanding of the philosophy of life, and increased compassion towards others (Xu et al., 2021). Therefore, Shidu parents may develop prolonged grief and/or posttraumatic growth. However, it remains unclear how these conditions are correlated and whether they have unique or shared underlying mechanisms (Eisma, Lenferink, Stroebe, Boelen, & Schut, 2019; Xu et al., 2020). Exploring their underlying mechanisms would offer guidance for targeted psychosocial interventions that focus on decreasing prolonged grief or facilitating posttraumatic growth.
Social support seems to be a protective factor against the negative impacts of bereavement. According to the microsociological theory (Maciejewski, Falzarano, She, Lichtenthal, & Prigerson, 2022), bereavement leads to a partial void in one’s social state, and part of the postloss adjustment is to fill this void and construct a new state of social equilibrium. Thus, bereaved people need social support to satisfy their social needs and desires. Existing research found that social support was a stable predictor of a lower risk of bereavement-related complications (Lobb et al., 2010). Receiving more social support was related to less adverse psychological consequences, including depression, prolonged grief, and posttraumatic stress symptoms, among bereaved people (Scott, Pitman, Kozhuharova, & Lloyd-Evans, 2020). Social support was found to present certain protective effects among Chinese Shidu parents. For example, more social support was associated with less suicidal ideation, fewer mental health problems, greater resilience, and a better quality of life (Cao, Yang, & Wang, 2018; Wang, Ren, Wang, Xu, & Wang, 2019; Wang & Xu, 2017). Social support is a critical factor in facilitating positive changes. Research has demonstrated a positive association between social support and grief-related growth among parentally bereaved children (Howard Sharp et al., 2018; Wolchik, Coxe, Tein, Sandler, & Ayers, 2009).
Although supportive social relationships can be satisfying and helpful, negative social relationship experiences can be detrimental and stressful, adversely impacting both physical and mental health. Negative social experiences refer to unsupportive, insensitive, or even harmful responses in relationships (Lincoln, 2000). Researchers have used a multitude of terms to represent negative experiences of social relationships, including social constraints, problematic social relationships, negative interactions, negative exchanges, and negative experiences of social support (Harada, Sugisawa, Sugihara, Yanagisawa, & Shimmei, 2018; Hirsch & Barton, 2011; Juth, Smyth, Carey, & Lepore, 2015). In the present study, we adopted the negative experiences of social support or negative social support. Researchers have proposed the domain-specific model to explain the relationship between the two types of social support experiences (Lincoln, 2000). That is, positive and negative experiences of social support are two different variables rather than two components of a single variable (Newsom, Rook, Nishishiba, Sorkin, & Mahan, 2005). These two variables have a weak correlation or even no correlation (Harada et al., 2018; Khondoker, Rafnsson, Morris, Orrell, & Steptoe, 2017; Rook, 1984) and are related to different dimensions of psychological consequences (Lincoln, 2000). However, compared to the widespread focus on the positive experiences of social support during bereavement, the negative experiences are relatively neglected. Therefore, it is crucial to examine the effect of negative social support as a separate domain.
Bereaved people may receive unsupportive or even negative support from those who are close to them. For example, they may receive unhelpful advice about postloss coping, not be allowed to talk about the loss, or even be criticized for not having done something (Aoun, Breen, White, Rumbold, & Kellehear, 2018; Dyregrov, Kristensen, & Dyregrov, 2018; Dyregrov, 2004). These unsatisfying interpersonal experiences may lead to feelings of being unsupported, misunderstood, or isolated and adversely influence the mental health of bereaved people (Juth et al., 2015). Research on African American people bereaved by homicide found a positive relationship between the number of people who might make the bereaved person upset or angry and prolonged grief symptoms, indicating the possible detrimental role of negative support during bereavement (Burke, Neimeyer, & McDevitt-Murphy, 2010). Unsupportive social interactions such as a limited chances to disclose feelings and thoughts are positively correlated with perceived stress, depressive symptoms, and somatic symptoms among bereaved people (Juth et al., 2015). Like other bereaved people, Chinese Shidu parents may also experience negative feelings when receiving support from others. Some parents reported that their friends and family members did not understand their feelings and even said hurtful words to them, leading them to become socially isolated (Jia, 2015). What is worse is that some of them felt discriminated against and stigmatized by members of their social network (Shi et al., 2019). Nevertheless, to our knowledge, no previous research has investigated the impact of negative social support experiences on Chinese Shidu parents. Additionally, existing research in bereaved people only focused on the relationship between negative social support and negative consequences and thus could not reveal the impact of negative social support on psychological consequences with different valences.
According to the domain-specific model (Lincoln, 2000), positive experiences of social support are related to positive outcomes, while negative experiences of social support are more related to adverse mental health outcomes. However, this theory was not fully verified by empirical studies. Some findings supported the domain-specific framework (Cheng, Li, Leung, & Chan, 2011; Fiori & Consedine, 2013), but some did not (Lewis, Brazeau, & Hill, 2020; Newsom, Nishishiba, Morgan, & Rook, 2003; Newsom et al., 2005). We also searched the literature regarding the relationship between positive and negative social support and prolonged grief/growth. We found that positive social support showed a negative correlation with prolonged grief and a positive relationship wtih posttraumatic growth (Howard Sharp et al., 2018; Lobb et al., 2010; Scott et al., 2020; Wolchik et al., 2009). Negative social support was positively linked with prolonged grief (Burke et al., 2010; Juth et al., 2015). In terms of the relationship between negative social support and growth, most studies revealed no significant findings (Cordova et al., 2007; Danhauer et al., 2013; Koutrouli et al., 2016; Nenova, DuHamel, Zemon, Rini, & Redd, 2013; Wilson, Morris, & Chambers, 2014), and to our knowledge, only one study reported a significant relationship (Champion et al., 2014). Therefore, by referring to the domain-specific model and the above findings, we assume that positive social support will be negatively linked with prolonged grief and positively associated with posttraumatic growth, while negative social support will be positively associated with prolonged grief (Hypothesis 1).
Social support from different sources may influence psychological adaptation differently (Birch, 1998). Specifically, research with bereaved siblings found that support from their parents and peers was negatively correlated with grief symptoms, whereas support from their parents, friends, and teachers was positively correlated with grief-related growth, demonstrating the various effects of support from different sources (Howard Sharp et al., 2018). Research among older Chinese widows reported that support from their adult children played a more important role than that from their friends (Li, Liang, Toler, & Gu, 2005). There are some differences in the informal social network system between Shidu parents and other bereaved people. After losing their only child, Chinese Shidu parents usually choose to maintain a distance from their original social network system (e.g. family members, friends, colleagues). They believe that they are essentially different from people who have children, and that other people do not understand them (Zhang & Jia, 2018). Individuals with similar experiences or peers seem to become one of primary support sources, and Shidu parents usually call these people their ‘new family members’ (Zhang & Jia, 2018). However, limited research has investigated the influence of informal social relationships with different people among Shidu parents. According to the findings of previous studies (Howard Sharp et al., 2018; Li & Chen, 2016; Zhang & Jia, 2018), we assume that the informal support sources of Shidu parents mainly include their close family members (i.e. partner, grandchildren, siblings), peers with similar experiences, and others (i.e. relatives, friends, colleagues). According to the classification of social relationships proposed by Dennis (2003), family members, relatives, friends, and colleagues can be categorized into embedded social networks, and peers can be categorized into created social networks. China is characterized by the familism culture (Yang, 2000). In China, the word ‘family’ refers not only to close family members, including parents, spouses, and children but also to a social group consisting of other relatives, formed by blood ties or marriages (Chinese Academy of Social Sciences, 2012). Under the influence of the familism culture, family members or other relatives may be the first to support and help each other, and Shidu parents may receive support from these individuals after encountering a tragic event. Additionally, Chinese people usually reside closely with their family members and individuals from other social networks (e.g. friends or colleagues) (Li, Mao, Chi, & Lou, 2019). Geographic proximity also enables Shidu parents to rely on these individuals when going through a difficult time (Li et al., 2019; Zhao, Yang, & Zhang, 2022). Therefore, we speculate that embedded social relationships (e.g. close family members [partner, grandchildren, siblings] or others [relatives, friends, colleagues]) may play a more critical role in the postloss adaptation than created social relationships (i.e. peers) (Hypothesis 2).
According to the Dual Process Model (DPM) by Stroebe and Schut (1999, 2010), postloss stressors can be categorized into two types, namely, loss-oriented stressors and restoration-oriented stressors, and postloss coping can be divided into two processes, i.e. loss-oriented and restoration-oriented coping. The loss-oriented coping process (LO) focuses more on the loss itself, such as ruminating about the loss, longing for the deceased, or blaming others or self for the loss. In contrast, the restoration-oriented coping process (RO) addresses the consequences that accompany bereavement, such as taking on future obligations, dealing with postloss debt, or adjusting to a new identity. A balance between the LO and RO coping promotes better postloss adaptation (Caserta, Lund, Utz, & de Vries, 2009; Caserta & Lund, 2007). Previous studies have explored the relationship between dual process coping strategies and postloss adaptation. The results showed that LO coping correlated with prolonged grief and depression positively (Dunn, 2015; Tang & Zhou, 2017) and negatively associated with growth (Caserta et al., 2009), and RO coping was negatively associated with prolonged grief and positively linked with growth (Caserta et al., 2009; Knowles & O’Connor, 2015).
Positive and negative experiences of social support may influence postloss adaptation through LO and RO coping. In an integrative risk factor model (Stroebe, Folkman, Hansson, & Schut, 2006), risk and protective factors related to intrapersonal and interpersonal aspects influence postloss adaptation through appraisal and coping processes. In this model, positive and negative experiences of social support are interpersonal factors. Thus, they may influence postloss adaptation through the coping process. Previous research has shown that social support was positively related to active-emotional and problem-focused coping and negatively associated with avoidant-emotional coping in bereaved people (Lipp & O’Brien, 2020; Somhlaba & Wait, 2008). Additionally, negative social support was found to be positively associated with the use of avoidant coping in individuals who had AIDS-related multiple loss (Ingram, Jones, & Smith, 2001). Until now, the mediating role of LO and RO coping strategies between positive and negative experiences of social support and postloss adaptation has remained unknown. The current study assumes that LO and RO coping strategies mediate the relationship between positive and negative social support and prolonged grief/growth (Hypothesis 3).
From the above, although the role of positive social support in bereaved people’s adjustment has been well investigated, the potential detrimental impact of negative social support is substantially neglected. The respective influence of the two types of social support experiences on positive and negative consequences remains unknown. Additionly, the relative importance of positive and social support from different sources on prolonged grief and growth is unclear, especially among Chinese Shidu parents. Moreover, whether social support experiences play a role in postloss adaptation by influencing the dual process coping strategies needs to be studied. Therefore, the present study’s purpose is to explore the effect of positive and negative experiences of social support from close family members (partner, grandchildren, siblings), peers, and others (relatives, friends, colleagues) on prolonged grief and growth, as well as the mediating roles of LO and RO coping strategies. The current study will not only test the domain-specific model of positive and negative social support by examining their separate effect on adjustment outcomes with different valences but also foster a better understanding of the role of various support sources. The current study is also promising to reveal the crucial roles of dual process coping strategies in the process of bereavement adaptation by elaborating on their mediate mechanisms.
2. Methods
2.1. Participants
Participants were recruited through online social media and offline mutual aid organizations. Individuals were invited to participate if they met the following criteria: (1) they had lost their only child and had no subsequent biological or adopted children; (2) they were aged between 49 and 85 years; (3) they had experienced bereavement for more than six months; (4) they had no communication deficiencies and were able to fill out the questionnaire; and (5) they had no diagnosis of severe mental illnesses (such as psychosis or dementia). A total of 295 participants were recruited. Individuals were excluded if they gave the same or regular responses (e.g. always as a pattern of 1, 2, 3, 4, 5) for consecutive items. The final valid dataset included 277 participants. Participants’ ages ranged from 49 to 83 years old, and their mean age was 62.31 years old. A total of 62.1% of the participants were female. On average, bereavement had occurred approximately 10 years ago, and 41.2% were traumatic death. Please refer to Table 1 for detailed information.
Table 1.
Sociodemographic and bereavement-related characteristics of the participants (N = 277).
| M ± SD or N (%) | |
|---|---|
| Gender | |
| Male | 103 (37.2%) |
| Female | 174 (62.8%) |
| Age (years) | 62.31 ± 6.33 |
| Home location | |
| Rural/county town | 65 (23.4%) |
| City | 212 (76.6%) |
| Education levela | |
| Illiteracy and primary school | 23 (8.3%) |
| High school | 167 (60.3%) |
| Junior college and above | 60 (21.7%) |
| Missing | 27 (9.7%) |
| Duration of bereavementa | 10.06 ± 6.96 |
| Cause of child’s deatha | |
| Non-traumatic (i.e. chronic and acute diseases) | 114 (41.2%) |
| Traumatic (i.e. accident, natural disaster, human-made disaster, suicide, homicide and other) | 146 (52.7%) |
| Missing | 17 (6.1%) |
| Employmenta | |
| Unemployed | 39 (14.1%) |
| Employed | 16 (5.8%) |
| Retired | 194 (70.0%) |
| Missing | 28 (10.1%) |
| Marital status | |
| Divorced or separated | 29 (10.5%) |
| Married | 197 (71.1%) |
| Widowed | 15 (18.4%) |
| Monthly income per person (yuan) | 3516.04 ± 1472.46 |
| Age of child (years) | 25.84 ± 7.87 |
| Grandchildren | |
| Yes | 83 (30.0%) |
| No | 194 (70.0%) |
| Positive social support from close family members | 6.84 (2.61) |
| Negative social support from close family members | 5.38 (1.96) |
| Positive social support from peers | 5.50 (2.34) |
| Negative social support from peers | 4.10 (1.63) |
| Positive social support from others | 5.33 (2.00) |
| Negative social support from others | 4.53 (1.66) |
| Prolonged grief symptom | 40.67 (14.86) |
| Posttraumatic growth | 29.12 (10.90) |
| Loss-orientated coping | 11.57 (3.30) |
| Restoration-orientated coping | 13.94 (3.75) |
Note: M = mean, SD = standard deviation, N = number of participants.
Variables with missing values.
Ethical approval was obtained from Beijing Normal University. Written informed consent was obtained before the survey.
2.2. Measurement tools
2.2.1. Positive and negative experiences of social support
Measures of positive and negative experiences of social support for each relationship (close family members [partner, grandchildren, siblings], peers, and others [relatives, friends, colleagues]) were assessed by a six-item questionnaire. We used the term ‘Tongmingren’ to represent ‘peer’ in the questionnaire, which is a unique expression of ‘peer’ in Chinese Shidu parents. It. All the participants are clear about the meaning of ‘Tongmingren’. These items were created by referring to a few existing measurement tools (Isherwood, King, & Luszcz, 2017; Khondoker et al., 2017). Three items were employed to assess positive social support: (1) They can take care of my daily needs, (2) Their listening to me makes me feel cared for and loved, and (3) They can talk with me and give advice. The other three items were used to assess negative social support: (4) They give unnecessary comforts, (5) They give unhelpful suggestions, and (6) They do not understand my feelings and even criticize my thoughts or behaviours. All items were measured on a 4-point scale (1 = rarely, 2 = a little, 3 = sometimes, 4 = often). For each relationship, positive or negative support scores were calculated by summing the scores of the three items. The scores range from 3 to 12. The higher the score is, the more positive or negative social support a person receive. The model fit of the 6-dimension structure was acceptable: χ2(120) = 321.541, χ2/df < 3; CFI = 0.915; TLI = 0.892; RMSEA = 0.078 (0.068, 0.088); and SRMR = 0.055. The Cronbach’s alpha values of the six subscales ranged from 0.79 to 0.88, indicating good internal reliability.
2.2.2. Prolonged grief symptoms (PGS)
The International Prolonged Grief Disorder Scale (IPGDS), including a standard subscale and a culturally relevant subscale, was used to measure an individual’s prolonged grief symptoms (Killikelly et al., 2020). 5-point Likert scale was adopted with 1 representing ‘never’ and 5 representing ‘several times a day’. This study summed the scores of 13 standardized questions to determine an individual’s level of prolonged grief symptoms, with higher scores indicating higher prolonged grief levels. The scores range from 13 to 65. The Chinese version of the IPGDS has good reliability and validity (Killikelly et al., 2020). Cronbach’s alpha value of the questionnaire for this sample was 0.96.
2.2.3. Posttraumatic growth (PTG)
A short version of the Posttraumatic Growth Inventory (PTGI) with 10 questions was used to evaluate the positive changes among people who had suffered a terrible trauma (Cann, Calhoun, Tedeschi, Taku, & Danhauer, 2009; Tedeschi & Calhoun, 1996). As more than 90% of the Chinese people have no religious belief, the item ‘I have strengthened my faith’ was deleted (Wang, Chen, Wang, & Liu, 2011), leaving 9 items for the final measurement. The inventory uses a 6-point Likert scale with scores ranging from 1 (not at all) to 6 (very large). The total score for all nine items represents the degree of positive change after trauma, with a score ranging from 9 to 54. Cronbach’s alpha was 0.93 for this sample.
2.2.4. Dual process coping
Dual process coping was measured using the Dual Coping Inventory (DCI), which includes two subscales: Loss-orientated coping (DCI-LO) and restoration-orientated coping (DCI-RO) (Tang & Zhou, 2017; Wijngaards-de Meij et al., 2008). There are seven items in the inventory, of which three items are for LO coping (e.g. I dwell on my sorrow), and four are for RO coping (e.g. I try to look ahead). A five-point scale is used to measure responses, with 1 representing ‘not at all’ and 5 representing ‘very much’. In this study, the total value of each subscale was used to represent LO or RO coping tendencies. The higher the score on the relevant scale, the more LO or RO coping is used. The scores of the LO subscale range from 3 to 15, and scores of the RO subscale range from 4 to 20. Cronbach’s alphas of the DCI-LO and the DCI-RO subscales were 0.88 and 0.87, respectively, for this sample.
2.3. Statistical analysis
The proportion of missing values in data for statistical modelling was less than 0.1%. In terms of continuous variables, missing values were imputed with variable means. Listwise deletion was adopted to handle the missing values of the categorical variables. Descriptive analyses were conducted.
To investigate the relationships between social support and postloss adaptation, partial correlation analyses were applied to assess the associations between positive or negative social support and grief/growth. The control variables include sex, age, family monthly income, bereavement length, and whether the individual had a grandchild, as these variables were found to correlate with prolonged grief symptoms and posttraumatic growth.
To examine the relative importance of positive and negative social support from different sources, partial correlation analyses between social support and prolonged grief/posttraumatic growth were performed as stated above. Then, paired sample t tests were conducted to compare the total scores of positive and negative social support with different social relationships.
To examine the mediating effect of dual process coping strategies between positive or negative support and prolonged grief/growth, structural equation modelling (SEM) was conducted as a powerful multivariate analytical tool (Loehlin, 1998; Weston & Gore, 2006). Positive social support, negative social support, LO coping, and RO coping were measured as latent variables. Specifically, we used the positive support from three sources (i.e. families, peers and others) to construct the latent variable of positive social support, and the negative support from the three sources to construct the latent variable of negative social support. The three DCI items of LO coping were regressed onto the latent variable of the LO coping strategy, and the remaining four items were regressed onto the latent variable of the RO coping strategy. In the structural model, we included all the independent, mediate, and dependent variables, including all the above latent variables and the total scores of IPGDS and PTGI. In this model, positive and negative support were independent variables, the dual process coping strategies were mediating variables, and prolonged grief and posttraumatic growth were dependent variables. The model fit was evaluated by the following indexes: the χ2/df value; the root mean square error of approximation (RMSEA); the comparative fit index (CFI); the Tucker-Lewis index (TLI); and the standardized root mean square residual (SRMR). To confirm a good model fit, the χ2/df should be less than 3.0, the CFI and TLI values should be larger than 0.90, and the SRMR and RMSEA values should be smaller than 0.08 (Hu & Bentler, 1999).
To test the significance of the indirect effects in the mediation model, we conducted bias-corrected bootstrap tests with a 95% confidence interval (CI). The mediation analysis was evaluated using 5000 bootstrap samples to calculate the 95% bias-corrected and accelerated bootstrap CIs, a method that is considered more statistically robust than traditional approaches (Mallinckrodt, Abraham, Wei, & Russell, 2006). A significant indirect effect is identified if the 95% CI does not include 0.
We used SPSS 25.0 to perform descriptive statistical analyses, correlation analyses, and pair-sample t tests. The mediation analysis was performed in Mplus software Version 7.0.
3. Results
3.1. Descriptive statistics, correlation analyses, and pair-sample t tests
Table 1 shows the descriptive information of the used variables.
Table 2 presents the correlation analysis results. Positive social support was negatively correlated with LO coping and prolonged grief and positively correlated with RO coping and posttraumatic growth but was not correlated with negative social support. Negative social support was positively associated with LO coping and prolonged grief but was not significantly correlated with RO coping and posttraumatic growth. LO coping was positively correlated with prolonged grief and negatively linked with posttraumatic growth but was not related to RO coping. RO coping was significantly positively associated with posttraumatic growth but was not associated with prolonged grief. A negative association was found between prolonged grief and posttraumatic growth.
Table 2.
Correlation analyses between study variables.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Pos_sup | 1 | ||||||||||
| 2. Neg_sup | .03 | 1 | |||||||||
| 3. Pos_fam | .80*** | −.07 | 1 | ||||||||
| 4. Neg_fam | .05 | .81*** | .05 | 1 | |||||||
| 5. Pos_peer | .62*** | .12 | .20** | .04 | 1 | ||||||
| 6. Neg_peer | −.03 | .71*** | −.16* | .35*** | .21** | 1 | |||||
| 7. Pos_other | .69*** | .03 | .42*** | .01 | .11 | −.09 | 1 | ||||
| 8. Neg_other | .04 | .75*** | −.07 | .41*** | .03 | .31*** | .14* | 1 | |||
| 9. DCI_LO | −.24*** | .15* | −.24*** | .19** | −.05 | .05 | −.20** | .10 | 1 | ||
| 10. DCI_RO | .14* | −.06 | .10 | −.04 | .08 | −.02 | .11 | −.08 | −.09 | 1 | |
| 11. PGS | −.28*** | .20** | −.33*** | .21** | −.06 | .05 | −.17** | .18** | .65*** | −.11 | 1 |
| 12. PTG | .25*** | −.09 | .18** | −.09 | .10 | −.06 | .26*** | −.05 | −.25*** | .45*** | −.27*** |
Note: *** p < .001, ** p < .01, * p < .05. M = mean, SD = standard deviation, Pos_sup = positive social support, Neg_sup = negative social support, Pos_fam = positive social support from family members, Neg_fam = negative social support from family members, Pos_peer = positive social support from peers, Neg_peer = negative social support from peers, Pos_other = positive social support from others, Neg_other = negative social support from others, DCI-LO = Dual Coping Inventory (loss oriented), DCI-RO = Dual Coping Inventory (restoration oriented), PGS = prolonged grief symptoms, PTG = posttraumatic growth.
Specifically, positive social support from family members was significantly linked with LO coping, prolonged grief, and growth, and negative social support from family members was positively correlated with LO coping and prolonged grief. Positive and negative support from peers was unrelated to the two dual process coping strategies, prolonged grief, and growth. Positive social support from others was significantly linked with LO coping, prolonged grief, and growth, and negative social support from others was positively associated with prolonged grief symptoms.
Pair-sample t tests showed that the average scores of positive and negative social support from close family members were the highest relative to the other two sources of relationship sources (close family members vs. peers: t(276) = 6.99, p < .001; close family members vs. others: t(276) = 9.90, p < .001). The average scores of positive support from peers and others showed no significant differences (peers vs. others: t(276) = 0.97, p = .334). The average scores of negative support from peers were the lowest (close family members vs. peers: t(276) = 10.21, p < .001; peers vs. others: t(276) = −3.73, p < .001).
3.2. The mediating role of dual process coping strategies between social support and prolonged grief/growth
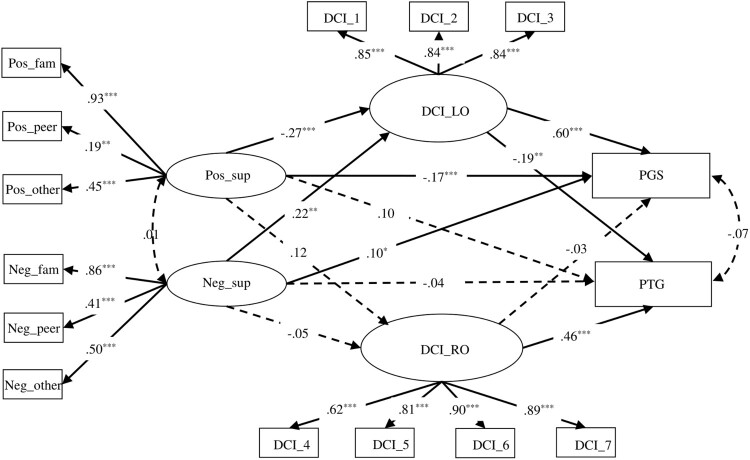
First, we tested the fitness of the measurement models for four latent variables together, including positive and negative social support, LO coping, and RO coping. The model fit well: χ2(61) = 124.346, χ2/df < 3; CFI = 0.952; TLI = 0.939; RMSEA = 0.061 (0.046, 0.077); and SRMR = 0.051. Then, we tested the fitness of the whole proposed structural equation model. The model fit was satisfactory: χ2(135) = 238.473, χ2/df < 3; CFI = 0.939; TLI = 0.919; RMSEA = 0.053 (0.042, 0.064); and SRMR = 0.051. Please see Figure 1 for the model.
Figure 1.
Structural equation model indicating the effects of positive and negative social support on grief and posttraumatic growth through dual-process coping. *** p < .001, ** p < .01, * p < .05. Pos_sup = positive social support, Neg_sup = negative social support, Pos_fam = positive social support from family members, Neg_fam = negative social support from family members, Pos_peer = positive social support from peers, Neg_peer = negative social support from peers, Pos_other = positive social support from others, Neg_other = negative social support from others, DCI-LO = Dual Coping Inventory (loss oriented), DCI-RO = Dual Coping Inventory (restoration oriented), PGS = prolonged grief symptoms, PTG = posttraumatic growth.
The bias-corrected bootstrap test results regarding the mediation effects are shown in Table 3. There was a significant direct effect between positive social support and prolonged grief and a significant indirect impact through LO coping. There was a significant direct effect between negative social support and prolonged grief symptoms and an indirect impact through LO coping. Significant indirect effects were also found between positive and negative social support and growth through LO coping.
Table 3.
Bootstrap test results of mediation paths.
| Paths | β | 95% CI |
|---|---|---|
| Direct effect between Pos_sup and PGS | −0.165 | −0.258, −0.062 |
| Indirect effect between Pos_sup and PGS through DCI-LO | −0.165 | −0.261, −0.084 |
| Indirect effect between Pos_sup and PGS through DCI-RO | −0.004 | −0.017, 0.007 |
| Direct effect between Neg_sup and PGS | 0.100 | 0.010, 0.189 |
| Indirect effect between Neg_sup and PGS through DCI-LO | 0.132 | 0.049, 0.213 |
| Indirect effect between Neg_sup and PGS through DCI-RO | −0.002 | −0.008, 0.012 |
| Direct effect between Pos_sup and PTG | 0.101 | −0.008, 0.211 |
| Indirect effect between Pos_sup and PTG through DCI-LO | 0.051 | 0.013, 0.102 |
| Indirect effect between Pos_sup and PTG through DCI-RO | 0.053 | −0.006, 0.114 |
| Direct effect between Neg_sup and PTG | −0.044 | −0.165, 0.082 |
| Indirect effect between Neg_sup and PTG through DCI-LO | −0.041 | −0.086, −0.008 |
| Indirect effect between Neg_sup and PTG through DCI-RO | −0.022 | −0.097, 0.045 |
Note: Pos_sup = positive social support, Neg_sup = negative social support, DCI-LO = Dual Coping Inventory (loss oriented), DCI-RO = Dual Coping Inventory (restoration oriented), PGS = prolonged grief symptoms, PTG = posttraumatic growth.
4. Discussion
The present study examined the relationship between positive and negative social support from different sources and prolonged grief/growth as well as the mediating role of dual process coping. We found that positive social support was negatively linked with prolonged grief and positively associated with posttraumatic growth, whereas negative social support was only positively related to prolonged grief, supporting Hypothesis 1. Specifically, positive social support from close family members and others was correlated with prolonged grief/growth, and negative social support from these two sources was linked with prolonged grief. The relationship between positive or negative social support from peers and prolonged grief/growth was not significant. These results supported Hypothesis 2. Finally, positive and negative social support were related to prolonged grief/growth via the LO coping process, partially supporting Hypothesis 3.
In support of Hypothesis 1, positive social support was linked with lower grief severity and higher posttraumatic growth, while negative social support was related to more prolonged grief symptoms. The results are consistent with those of previous studies conducted among other populations and demonstrate the protective effect of positive social support and the detrimental impact of negative social support on wellbeing (Hirsch & Barton, 2011; Iob, Kirschbaum, & Steptoe, 2018; Wang et al., 2019). Positive social support offers Shidu parents who encounter difficulties necessary resources, reducing their negative emotions and relieving bereavement-related distress. Furthermore, positive social support helps Shidu parents experience enhanced positive emotions, improves their relationships with themselves and others, and encourages them to rethink the loss and reconstruct life meanings, enabling psychological growth. In contrast, negative social support makes Shidu parents feel unsupported and misunderstood and aggravates their sense of isolation and loneliness (Liu & Rook, 2013), preventing them from recovering from grief. Moreover, excessive negative social support may become an additional interpersonal stressor during the process of adapting to loss, exacerbating bereavement distress.
Negative support was not related to posttraumatic growth, showing that more positive support rather than less negative support motivates positive changes. This is in accordance with previous research that reporting that negative support was associated more with adverse mental health consequences (e.g. depression, posttraumatic stress symptoms) than positive wellbeing (e.g. posttraumatic growth) (Cordova et al., 2007; Danhauer et al., 2013; Koutrouli et al., 2016; Nenova et al., 2013; Newsom et al., 2005; Okabayashi, Liang, Krause, Akiyama, & Sugisawa, 2004; Wilson et al., 2014). Additionally, no association was found between positive and negative support, further supporting the independent roles of these two social experiences. Overall, the findings provide evidence for the domain-specific model of positive and negative social support by demonstrating that these two social experiences are independent and play different roles in coping with stressful events (Croezen et al., 2010; Newsom et al., 2005).
Support from close family members and others was associated with prolonged grief or growth, while support from peers was not. The results supported Hypothesis 2 by demonstrating that social support from Shidu parents’ embedded social relationships (i.e. close family members [partner, grandchildren, siblings] and others [relatives, friends, and colleagues]) plays a more important role than that from created social relationships (i.e. peers). Furthermore, Shidu parents received the most positive support from close family members, suggesting that they may have more positive social interactions with their close family members than with other people. The results may reflect the effect of familism culture in China (Chen, 2019). For Chinese people, kin relationships seem to be the source that is most likely to provide unconditional support when a person is in a health crisis (Dong, Chang, Wong, & Simon, 2012). Chinese Shidu parents seem to largely rely on their kin-centred networks when going through the psychological crisis of losing an only child. Although Chinese Shidu parents stated that they had no home or family after losing their only child and some regarded their peers as new family members (Zhang & Jia, 2018), support from their embedded social relationships still played a crucial role, especially that from their close family members. The results may also reflect the complicated role of peer support in the bereavement adjustment of Shidu parents. Shidu parents, by congregating with people who have had similar experiences, feel like they are part of a group with a shared destiny and social identity, relieving the isolation of feeling like an outlier in society and promoting postloss adaptation. From another perspective, a closer connection with peers may reflect a stronger fear of being in a minority group in society, and receiving more peer support may imply poor mental status. Therefore, a direct relationship between peer support and prolonged grief/growth was not identified. Furthermore, the results may be explained by the original size of Shidu parents’ social networks. It is possible that parents who have larger social networks before their loss can turn to their family members or friends for help and do not need as much support from their peers. In contrast, receiving more helpful support from peers may mean that they have limited support sources in their social networks. Thus, the absence of original social relationships could dilute the beneficial effect of positive peer support. Future research should thoroughly investigate the impact of peer support among Chinese Shidu parents by testing the moderating role of their original social network sizes.
It should be noted that Shidu parents also receive the most negative support from their close family members, which seems to have an adverse impact on their bereavement adaptation. Previous research has demonstrated that social support from family members can be unhelpful and even stressful for bereaved people (Aoun et al., 2018; Zhang & Jia, 2018). It seems that social interactions with close family members are a mixed blessing. When Shidu parents experience the benefits of satisfying support from their close family members, they also must bear the stress of unsupportive responses from those individuals. The findings remind us that when providing psychosocial support to Shidu parents, health care workers should identify the mode of support relationships and make a distinction between limited positive support and excessive negative support; in this way, they can coach family members to provide high-quality support or avoid unsupportive behaviours according to the specific needs of each individual (Nam, 2016).
Positive and negative social support was directly linked with prolonged grief and indirectly associated with prolonged grief/growth via the LO coping strategy. The present research demonstrated that Shidu parents who receive less positive social support or more negative social support tend to adopt the LO coping strategy, which enhances prolonged grief symptoms and impedes bereavement growth. If an individual receives less positive support or more negative support, they may feel they are not understood, cared for, or loved by the people around him or her. Consequently, it may be easy for these individuals to miss and yearn for the goodness and merit of the deceased and turn to the past relationship for comfort (Stelzer & O’Connor, 2021). As is shown in a previous study, feeling pressure from society and being misunderstood by family members were positively related to more engagement in continuing bonds with the deceased (Jones, Crawley, Brierley-Jones, & Kenny, 2021). Additionally, receiving more negative support may also aggrevate their social isolation. As a result, the bereaved may exhibit the LO coping tendency by ruminating about the loss, blaming themselves or others, or questioning their god’s decision. Therefore, they get stuck in their grief and require a longer time and more effort to deal with the pain caused by the loss, presenting prolonged and complicated grief reactions. In contrast, when an individual receives more positive social support or less negative social support from others, they may be distracted from their loss and think less often of their deceased loved one. Thus, their sorrow and grief reactions are relieved and they may even experience some positive changes (Fiore, 2021). As a positive coping resource, positive social support can empower the bereaved people to better cope with the pain caused by death and loss. If bereaved people believe they can rely on their living relatives or friends when they encounter difficulties, they may not mourn their loss alone and helplessly. Positive social support may also remedy the value and benefits of the lost relationship and encourage them to recover and even grow from the loss (Stelzer & O’Connor, 2021). As discussed in previous research, if the father allowed the mother to talk about the child’s death rather than making it a taboo topic, she can better internalize the mental representation of the deceased child, moving towards the grief recovery (Testoni, Bregoli, Pompele, & Maccarini, 2020).
However, RO coping did not mediate the relationship between social support and prolonged grief/growth. One possible reason may be related to the measurement tool used. DCI measures RO coping by using four items regarding thinking about future life, going on with life, or looking ahead, and these questions seem broad and difficult to answer. Shidu parents may feel that they no longer love their deceased child if they answer yes to these questions, and many Shidu parents state that they have no life or future after losing their only child (Zheng, Lawson, & Anderson Head, 2017). Distracting their attention from the loss seems more accessible for Shidu parents than moving on and looking ahead. Therefore, social interactions with other people may not have much effect on influencing RO coping relative to LO coping. As shown in the results, although the relationship between positive social support and RO coping was significant, the correlation coefficient was very low (r = 0.14, p < .05). Future research could use a tool with specific questions, such as the Inventory of Daily Widowed Life (Caserta & Lund, 2007), to measure the RO coping strategy in detail rather than broadly. The results demonstrate that LO and RO coping strategies are independent dimensions and may have different working mechanisms. Actually, the correlation between LO and RO coping was not significant, which was in line with previous studies (Caserta & Lund, 2007; Tang & Zhou, 2017). The findings support the independent characteristics of these coping strategies.
Although a significant mediating role of RO coping was not found, a positive correlation between RO coping and posttraumatic growth was identified. The current findings are consistent with those of previous studies (Caserta et al., 2009; Dunn, 2015; Tang & Zhou, 2017; Wijngaards-de Meij et al., 2008), which reported a positive correlation between less use of the LO strategy or more use of the RO coping strategy and a better bereavement adjustment. As the current study only assessed the extent of LO and RO coping, the conclusion should be that using too much LO coping or too little RO coping is detrimental. However, theoretically, both the LO and RO coping strategies are necessary and helpful parts of the grieving process (Stroebe & Schut, 2010). As the present research was not a process study, we could not illustrate the accurate role of LO or RO coping in the normal mourning process. Additionally, neither too much LO nor RO coping is beneficial, but the flexible oscillation between them facilitates the recovery from loss (Stroebe & Schut, 2010). Similarly, the current study can not reveal the role of the flexible oscillation between LO and RO coping due to the study design. Future research could consider testing the mechanism of the oscillation process between LO and RO coping or the combined effect of the two coping tendencies. Despite this, our study implies that the extent of LO and RO coping could indicate the outcomes of grief recovery.
5. Limitations and future research
The limitations of the current study must be considered. First, the present study was cross-sectional, and the results cannot reveal the causal relationship between social support and postloss adaptation. Future studies can employ a prospective or intervention design to reveal the causal effect. Second, the DCI may not accurately capture the DPM construct. It did not involve specific LO and RO coping strategies but used general items to measure a broad coping tendency. Recently, Eisma, de Lang, and Stroebe (2021) developed a novel measure to assess the specific elements of RO stressors. Future research can develop and employ such tools to assess LO and RO coping. Third, the present study recruited a sample from cities and therefore lacked information from participants in rural areas. People who live in the countryside may differ from urban populations in their social support networks. Fourth, the criterion validity of positive and negative social support measurements was not strictly tested. Future research could use other social support tools to assess the criterion validity of the current measurements. Fifth, the sample was a particular group of bereaved people, and some of the findings may not reflect the experiences of other bereaved people. For example, the results relevant to the relative importance of social support from different sources may not be generalized to other bereaved people, as the sources are various for different bereaved groups. For instance, support from children seems to be crucial for those who experienced a spousal loss, while the current study does not involve this. Moreover, although other findings are hopeful to be generalized to other bereaved individuals (e.g. the roles of positive and negative support on postloss adaptation as well as the mediating role of dual process coping between them), they need to be verified in a more diverse sample of bereaved people.
6. Conclusions
Despite its limitations, there are some critical theoretical and practical values in the present study. First, these findings stress the potential detrimental role of negative social support and provide empirical evidence for the domain-specific model of positive and negative social support. In practical work, increasing positive social support experiences can largely motivate the relief of bereaved parents from the grief and even encourage growth from the loss. Significantly, interventions to help bereaved people alleviate prolonged grief should also focus on recognizing and reducing negative social support experiences. Second, these findings emphasize the significance of enhancing awareness of support from different sources on bereaved people’s postloss adaptation. Specifically, embedded social relationships are crucial for Chinese Shidu parents. Although previous studies have demonstrated the protective role of positive social support for bereaved people, the present study further illustrates that not all sources play equally important roles in postloss adjustment. From a practical perspective, we should recognize the critical value of Shidu parents’ embedded social networks and develop interventions by promoting positive support and decreasing negative support. Third, the current study extended existing research by demonstrating that social support experiences have the potential to adjust the coping process, such as decreasning LO coping tendency, to reduce prolonged grief and facilitate growth.
In conclusion, the current study found that positive and negative social support played an essential part in adverse postloss outcomes (i.e. prolonged grief reactions), but only positive support was linked to positive changes (i.e. posttraumatic growth). Positive and negative social support from close family members (partner, grandchildren, siblings) and others (family, friends, colleagues) played a more important role relative to that from peers. LO coping mediated the relationship between positive and negative social support and prolonged grief/growth, while RO coping did not.
Acknowledgements
We also thank all the participants, without whom this research would not have been possible.
Funding Statement
This work is supported by The Research Project of Shanghai Science and Technology Commission [grant number 20dz2260300], the Fundamental Research Funds for the Central Universities [grant number 2021ECNU-HLYT008], the Fundamental Research Funds for the Central Universities grant number 43800-20101-222104], and the China Postdoctoral Science Foundation grant number 2021M691039].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Conflict of interest declaration
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
Description of authors’ roles
N. Zhou formulated the idea and designed this study, collected the data, and had full access to the data. N. Zhou and Y. Sun analysed the data and drafted the manuscript. X. Liu supervised the data analysis and assisted with writing and improving the manuscript. Z. She, Y. Peng, and J. Xi also contributed to improving the manuscript.
Data availability statement
The data of this study are available from the corresponding author. The data are not publicly available for privacy reasons.
References
- Aoun, S. M., Breen, L. J., White, I., Rumbold, B., & Kellehear, A. (2018). What sources of bereavement support are perceived helpful by bereaved people and why? Empirical evidence for the compassionate communities approach. Palliative Medicine, 32(8), 1378–1388. 10.1177/0269216318774995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch, D. A. (1998). Identifying sources of social support. Journal of School Health, 68(4), 159–161. 10.1111/j.1746-1561.1998.tb06335.x [DOI] [PubMed] [Google Scholar]
- Burke, L. A., Neimeyer, R. A., & McDevitt-Murphy, M. E. (2010). African American homicide bereavement: Aspects of social support that predict complicated grief, PTSD, and depression. OMEGA - Journal of Death and Dying, 61(1), 1–24. 10.2190/OM.61.1.a [DOI] [PubMed] [Google Scholar]
- Cann, A., Calhoun, L. G., Tedeschi, R. G., Taku, K., & Danhauer, S. C. (2009). A short form of the posttraumatic growth inventory. Anxiety, Stress, and Coping, 23(2), 127–137. 10.1080/10615800903094273 [DOI] [PubMed] [Google Scholar]
- Cao, X., Yang, C., & Wang, D. (2018). The impact on mental health of losing an only child and the influence of social support and resilience. OMEGA - Journal of Death and Dying, 80(4), 666–684. 10.1177/0030222818755284 [DOI] [PubMed] [Google Scholar]
- Caserta, M., & Lund, D. (2007). Toward the development of an Inventory of Daily Widowed Life (IDWL): guided by the dual process model of coping with bereavement. Death Studies, 31(6), 505–535. 10.1080/07481180701356761 [DOI] [PubMed] [Google Scholar]
- Caserta, M., Lund, D., Utz, R., & de Vries, B. (2009). Stress-related growth among the recently bereaved. Aging & Mental Health, 13(3), 463–476. 10.1080/13607860802534641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champion, V. L., Wagner, L. I., Monahan, P. O., Daggy, J., Smith, L., Cohee, A., … Unverzagt, F. W. (2014). Comparison of younger and older breast cancer survivors and age-matched controls on specific and overall quality of life domains. Cancer, 120(15), 2237–2246. 10.1002/cncr.28737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, X. (2019). ‘Family-culture’ and Chinese politeness. Acta Linguistica Academica, 66(2), 251–270. 10.1556/2062.2019.66.2.6 [DOI] [Google Scholar]
- Cheng, S. T., Li, K. K., Leung, E. M., & Chan, A. C. (2011). Social exchanges and subjective well-being: Do sources of positive and negative exchanges matter? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66B(6), 708–718. 10.1093/geronb/gbr061 [DOI] [PubMed] [Google Scholar]
- Chinese Academy of Social Sciences . (2012). Contemporary Chinese Dictionary. Beijing: Commercial Press. [Google Scholar]
- Cordova, M. J., Giese-Davis, J., Golant, M., Kronenwetter, C., Chang, V., & Spiegel, D. (2007). Breast cancer as trauma: Posttraumatic stress and posttraumatic growth. Journal of Clinical Psychology in Medical Settings, 14(4), 308–319. 10.1007/s10880-007-9083-6 [DOI] [Google Scholar]
- Croezen, S., Haveman-Nies, A., Picavet, H. S. J., Smid, E. A., De Groot, C., Van’t Veer, P., & Verschuren, W. M. M. (2010). Positive and negative experiences of social support and long-term mortality among middle-aged Dutch people. American Journal of Epidemiology, 172(2), 173–179. 10.1093/aje/kwq095 [DOI] [PubMed] [Google Scholar]
- Danhauer, S. C., Russell, G. B., Tedeschi, R. G., Jesse, M. T., Vishnevsky, T., Daley, K., … Powell, B. L. (2013). A longitudinal investigation of posttraumatic growth in adult patients undergoing treatment for acute leukemia. Journal of Clinical Psychology in Medical Settings, 20(1), 13–24. 10.1007/s10880-012-9304-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis, C. L. (2003). Peer support within a health care context: A concept analysis. International Journal of Nursing Studies, 40(3), 321–332. 10.1016/S0020-7489(02)00092-5 [DOI] [PubMed] [Google Scholar]
- Djelantik, A. A. A. M. J., Smid, G. E., Mroz, A., Kleber, R. J., & Boelen, P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: Systematic review and meta regression analysis. Journal of Affective Disorders, 265, 146–156. 10.1016/j.jad.2020.01.034 [DOI] [PubMed] [Google Scholar]
- Dong, X., Chang, E. S., Wong, E., & Simon, M. (2012). A qualitative study of filial piety among community dwelling, Chinese, older adults: Changing meaning and impact on health and well-being. Journal of Intergenerational Relationships, 10(2), 131–146. 10.1080/15350770.2012.673393 [DOI] [Google Scholar]
- Dunn, C. R. (2015). Young Widows’ Grief: A Descriptive Study of Personal and Contextual Factors Associated with Conjugal Loss. Logan: Utah State University. [Google Scholar]
- Dyregrov, K. (2004). Micro-Sociological analysis of social support following traumatic bereavement: Unhelpful and avoidant responses from the community. OMEGA - Journal of Death and Dying, 48(1), 23–44. 10.2190/T3NM-VFBK-68R0-UJ60 [DOI] [Google Scholar]
- Dyregrov, K., Kristensen, P., & Dyregrov, A. (2018). A relational perspective on social support between bereaved and their networks after terror: A qualitative study. Global Qualitative Nursing Research, 5, 233339361879207. 10.1177/2333393618792076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisma, M. C., de Lang, T. A., & Stroebe, M. S. (2021). Restoration-oriented stressors of bereavement. Anxiety, Stress, & Coping, 35(3), 339–353. 10.1080/10615806.2021.1957849 [DOI] [PubMed] [Google Scholar]
- Eisma, M. C., Lenferink, L. I., Stroebe, M. S., Boelen, P. A., & Schut, H. A. (2019). No pain, no gain: Cross-lagged analyses of posttraumatic growth and anxiety, depression, posttraumatic stress and prolonged grief symptoms after loss. Anxiety, Stress, & Coping, 32(3), 231–243. 10.1080/10615806.2019.1584293 [DOI] [PubMed] [Google Scholar]
- Fiore, J. (2021). A systematic review of the dual process model of coping with bereavement (1999–2016). OMEGA - Journal of Death and Dying, 84(2), 414–458. 10.1177/0030222819893139 [DOI] [PubMed] [Google Scholar]
- Fiori, K. L., & Consedine, N. S. (2013). Positive and negative social exchanges and mental health across the transition to college. Journal of Social and Personal Relationships, 30(7), 920–941. 10.1177/0265407512473863 [DOI] [Google Scholar]
- Harada, K., Sugisawa, H., Sugihara, Y., Yanagisawa, S., & Shimmei, M. (2018). Social support, negative interactions, and mental health: Evidence of cross-domain buffering effects among older adults in Japan. Research on Aging, 40(4), 388–405. 10.1177/0164027517701446 [DOI] [PubMed] [Google Scholar]
- He, L., Tang, X., Zhu, Z., & Wang, J. (2014). Great pain: Qualitative research on grief reactions of the parents who lost their single child. Chinese Journal of Clinical Psychology, 22(5), 792–798. [Google Scholar]
- Hildebrandt, T. (2019). The one-child policy, elder care, and LGB Chinese: A social policy explanation for family pressure. Journal of Homosexuality, 66(5), 590–608. 10.1080/00918369.2017.1422946 [DOI] [PubMed] [Google Scholar]
- Hirsch, J. K., & Barton, A. L. (2011). Positive social support, negative social exchanges, and suicidal behavior in college students. Journal of American College Health, 59(5), 393–398. 10.1080/07448481.2010.515635 [DOI] [PubMed] [Google Scholar]
- Howard Sharp, K. M., Russell, C., Keim, M., Barrera, M., Gilmer, M. J., Foster Akard, T., … Hogan, N. (2018). Grief and growth in bereaved siblings: Interactions between different sources of social support. School Psychology Quarterly, 33(3), 363. 10.1037/spq0000253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Ingram, K. M., Jones, D. A., & Smith, N. G. (2001). Adjustment among people who have experienced AIDS-related multiple loss: The role of unsupportive social interactions, social support, and coping. OMEGA - Journal of Death and Dying, 43(4), 287–309. 10.2190/TV1J-543L-M020-B93V [DOI] [Google Scholar]
- Iob, E., Kirschbaum, C., & Steptoe, A. (2018). Positive and negative social support and HPA-axis hyperactivity: Evidence from glucocorticoids in human hair. Psychoneuroendocrinology, 96, 100–108. 10.1016/j.psyneuen.2018.06.008 [DOI] [PubMed] [Google Scholar]
- Isherwood, L. M., King, D. S., & Luszcz, M. A. (2017). Widowhood in the fourth age: Support exchange, relationships and social participation. Ageing and Society, 37(1), 188–212. 10.1017/S0144686X15001166 [DOI] [Google Scholar]
- Jia, J. (2015). Research on the social work’s intervention in community participation of Shidu elderly—H community in Wuxi as example. Nanjing: Nanjing Agricultural University. [Google Scholar]
- Jones, E. E., Crawley, R., Brierley-Jones, L., & Kenny, C. (2021). Continuing bonds following stillbirth: Protective and risk factors associated with parental bereavement adaptation. Journal of Reproductive and Infant Psychology, 1–17. 10.1080/02646838.2021.1972951 [DOI] [PubMed] [Google Scholar]
- Juth, V., Smyth, J. M., Carey, M. P., & Lepore, S. J. (2015). Social constraints are associated with negative psychological and physical adjustment in bereavement. Applied Psychology: Health and Well-Being, 7(2), 129–148. 10.1111/aphw.12041 [DOI] [PubMed] [Google Scholar]
- Khondoker, M., Rafnsson, S. B., Morris, S., Orrell, M., & Steptoe, A. (2017). Positive and negative experiences of social support and risk of Dementia in later life: An investigation using the English longitudinal study of ageing. Journal of Alzheimer’s Disease, 58(1), 99–108. 10.3233/JAD-161160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killikelly, C., Zhou, N., Merzhvynska, M., Stelzer, E. M., Dotschung, T., Rohner, S., … Maercker, A. (2020). Development of the international prolonged grief disorder scale for the ICD-11: Measurement of core symptoms and culture items adapted for Chinese and German-speaking samples. Journal of Affective Disorders, 277, 568–576. 10.1016/j.jad.2020.08.057 [DOI] [PubMed] [Google Scholar]
- Knowles, L. M., & O’Connor, M. F. (2015). Coping flexibility, forward focus and trauma focus in older widows and widowers. Bereavement Care, 34(1), 17–23. 10.1080/02682621.2015.1028200 [DOI] [Google Scholar]
- Koutrouli, N., Anagnostopoulos, F., Griva, F., Gourounti, K., Kolokotroni, F., Efstathiou, V., … Potamianos, G. (2016). Exploring the relationship between posttraumatic growth, cognitive processing, psychological distress, and social constraints in a sample of breast cancer patients. Women & Health, 56(6), 650–667. 10.1080/03630242.2015.1118725 [DOI] [PubMed] [Google Scholar]
- Lewis, N. A., Brazeau, H., & Hill, P. L. (2020). Adjusting after stroke: Changes in sense of purpose in life and the role of social support, relationship strain, and time. Journal of Health Psychology, 25(12), 1831–1841. 10.1177/1359105318772656 [DOI] [PubMed] [Google Scholar]
- Li, J., & Chen, S. (2016). A new model of Social Support in Bereavement (SSB): An empirical investigation with a Chinese sample. Death Studies, 40(4), 223–228. 10.1080/07481187.2015.1127296 [DOI] [PubMed] [Google Scholar]
- Li, L., Liang, J., Toler, A., & Gu, S. (2005). Widowhood and depressive symptoms among older Chinese: Do gender and source of support make a difference? Social Science & Medicine, 60(3), 637–647. 10.1016/j.socscimed.2004.06.014 [DOI] [PubMed] [Google Scholar]
- Li, M., Mao, W., Chi, I., & Lou, V. W. (2019). Geographical proximity and depressive symptoms among adult child caregivers: Social support as a moderator. Aging & Mental Health, 23(2), 205–213. 10.1080/13607863.2017.1399349 [DOI] [PubMed] [Google Scholar]
- Lincoln, K. D. (2000). Social support, negative social interactions, and psychological well-being. Social Service Review, 74(2), 231–252. 10.1086/514478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipp, N. S., & O’Brien, K. M. (2020). Bereaved college students: Social support, coping style, continuing bonds, and social media use as predictors of complicated grief and posttraumatic growth. OMEGA-Journal of Death and Dying. 10.1177/0030222820941952 [DOI] [PubMed] [Google Scholar]
- Liu, B. S., & Rook, K. S. (2013). Emotional and social loneliness in later life: Associations with positive versus negative social exchanges. Journal of Social and Personal Relationships, 30(6), 813–832. 10.1177/0265407512471809 [DOI] [Google Scholar]
- Lobb, E. A., Kristjanson, L. J., Aoun, S. M., Monterosso, L., Halkett, G. K. B., & Davies, A. (2010). Predictors of complicated grief: A systematic review of empirical studies. Death Studies, 34(8), 673–698. 10.1080/07481187.2010.496686 [DOI] [PubMed] [Google Scholar]
- Loehlin, J. (1998). Latent variable models: An introduction to factor, path, and structural analysis. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Lundorff, M., Holmgren, H., Zachariae, R., Farver-Vestergaard, I., & O’Connor, M. (2017). Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. Journal of Affective Disorders, 212, 138–149. 10.1016/j.jad.2017.01.030 [DOI] [PubMed] [Google Scholar]
- Maciejewski, P. K., Falzarano, F. B., She, W. J., Lichtenthal, W. G., & Prigerson, H. G. (2022). A micro-sociological theory of adjustment to loss. Current Opinion in Psychology, 43, 96–101. 10.1016/j.copsyc.2021.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallinckrodt, B., Abraham, W. T., Wei, M., & Russell, D. W. (2006). Advances in testing the statistical significance of mediation effects. Journal of Counseling Psychology, 53(3), 372–378. 10.1037/0022-0167.53.3.372 [DOI] [Google Scholar]
- Nam, I. (2016). Complicated grief treatment for older adults: The critical role of a supportive person. Psychiatry Research, 244, 97–102. 10.1016/j.psychres.2016.07.044 [DOI] [PubMed] [Google Scholar]
- Nenova, M., DuHamel, K., Zemon, V., Rini, C., & Redd, W. H. (2013). Posttraumatic growth, social support, and social constraint in hematopoietic stem cell transplant survivors. Psycho-oncology, 22(1), 195–202. 10.1002/pon.2073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsom, J. T., Nishishiba, M., Morgan, D. L., & Rook, K. S. (2003). The relative importance of three domains of positive and negative social exchanges: A longitudinal model with comparable measures. Psychology and Aging, 18(4), 746–754. 10.1037/0882-7974.18.4.746 [DOI] [PubMed] [Google Scholar]
- Newsom, J. T., Rook, K. S., Nishishiba, M., Sorkin, D. H., & Mahan, T. L. (2005). Understanding the relative importance of positive and negative social exchanges: Examining specific domains and appraisals. The Journals of Gerontology: Series B, 60(6), P304–P312. 10.1093/geronb/60.6.P304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okabayashi, H., Liang, J., Krause, N., Akiyama, H., & Sugisawa, H. (2004). Mental health among older adults in Japan: Do sources of social support and negative interaction make a difference? Social Science & Medicine, 59(11), 2259–2270. 10.1016/j.socscimed.2004.02.024 [DOI] [PubMed] [Google Scholar]
- Rook, K. S. (1984). The negative side of social interaction: Impact on psychological well-being. Journal of Personality and Social Psychology, 46(5), 1097–1108. 10.1037/0022-3514.46.5.1097 [DOI] [PubMed] [Google Scholar]
- Scott, H. R., Pitman, A., Kozhuharova, P., & Lloyd-Evans, B. (2020). A systematic review of studies describing the influence of informal social support on psychological wellbeing in people bereaved by sudden or violent causes of death. BMC Psychiatry, 20, 1–20. 10.1186/s12888-020-02639-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, G., Wen, J., Xu, X., Zhou, N., Wang, J., Shi, Y., … Stelzer, E.-M. (2019). Culture-related grief beliefs of Chinese Shidu parents: Development and psychometric properties of a new scale. European Journal of Psychotraumatology, 10(1), 1626075. 10.1080/20008198.2019.1626075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somhlaba, N. Z., & Wait, J. W. (2008). Psychological adjustment to conjugal bereavement: Do social networks aid coping following spousal death? OMEGA - Journal of Death and Dying, 57(4), 341–366. 10.2190/OM.57.4.b [DOI] [PubMed] [Google Scholar]
- Stelzer, E. M., & O’Connor, M. F. (2021). Can less ever be more? A model of Emotion Regulation Repertoire of Social Support (ERROSS). Emotion Review, 13(2), 125–138. 10.1177/1754073921992848 [DOI] [Google Scholar]
- Stroebe, M., Folkman, S., Hansson, R., & Schut, H. (2006). The prediction of bereavement outcome: Development of an integrative risk factor framework. Social Science & Medicine, 63(9), 2440–2451. 10.1016/j.socscimed.2006.06.012 [DOI] [PubMed] [Google Scholar]
- Stroebe, M., & Schut, H. (1999). The dual process model of coping with bereavement: Rationale and description. Death Studies, 23(3), 197–224. 10.1080/074811899201046 [DOI] [PubMed] [Google Scholar]
- Stroebe, M., & Schut, H. (2010). The dual process model of coping with bereavement: A decade on. OMEGA - Journal of Death and Dying, 61(4), 273–289. 10.2190/OM.61.4.b [DOI] [PubMed] [Google Scholar]
- Su, J. (2015). An analysis of the effects of social relations on Shidu group. Acta Universitatis Medicinalis Nanjing (Social Science), 000(001), 59–62. [Google Scholar]
- Tang, S., & Zhou, A. (2017). How do risk factors affect bereavement outcomes in later life? An exploration of the mediating role of dual process coping. Psychiatry Research, 255, 297–303. 10.1016/j.psychres.2017.06.001 [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. 10.1002/jts.2490090305 [DOI] [PubMed] [Google Scholar]
- Testoni, I., Bregoli, J., Pompele, S., & Maccarini, A. (2020). Social support in perinatal grief and mothers’ continuing bonds: A qualitative study with Italian Mourners. Affilia, 35(4), 485–502. 10.1177/0886109920906784 [DOI] [Google Scholar]
- Wang, J., Chen, Y., Wang, Y., & Liu, X. (2011). Revision of the Posttraumatic Growth Inventory and testing its reliability and validity. Journal of Nursing Science, 26(14), 26–28. [Google Scholar]
- Wang, Q., Ren, L., Wang, W., Xu, W., & Wang, Y. (2019). Long-term psychological distress of Bosnian war survivors: An 11-year follow-up of former displaced persons, returnees, and stayers. BMC Psychiatry, 19(1), 1–9. 10.1186/s12888-018-1996-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Z., & Xu, J. (2017). Association between resilience and quality of life in Wenchuan Earthquake Shidu parents: The mediating role of social support. Community Mental Health Journal, 53(7), 859–863. 10.1007/s10597-017-0099-6 [DOI] [PubMed] [Google Scholar]
- Weston, R., & Gore Jr, P. A. (2006). A brief guide to structural equation modeling. The Counseling Psychologist, 34(5), 719–751. 10.1177/0011000006286345 [DOI] [Google Scholar]
- Wijngaards-de Meij, L., Stroebe, M., Schut, H., Stroebe, W., van den Bout, J., van der Heijden, P., & Dijkstra, I. (2008). Parents grieving the loss of their child: Interdependence in coping. British Journal of Clinical Psychology, 47(1), 31–42. 10.1348/014466507X216152 [DOI] [PubMed] [Google Scholar]
- Wilson, B., Morris, B. A., & Chambers, S. (2014). A structural equation model of posttraumatic growth after prostate cancer. Psycho-Oncology, 23(11), 1212–1219. 10.1002/pon.3546 [DOI] [PubMed] [Google Scholar]
- Wolchik, S. A., Coxe, S., Tein, J. Y., Sandler, I. N., & Ayers, T. S. (2009). Six-year longitudinal predictors of posttraumatic growth in parentally bereaved adolescents and young adults. OMEGA - Journal of Death and Dying, 58(2), 107–128. 10.2190/OM.58.2.b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, X., Wen, J., Zhou, N., Shi, G., Tang, R., Wang, J., & Skritskaya, N. A. (2020). Grief and posttraumatic growth among Chinese bereaved parents who lost their only child: The moderating role of interpersonal loss. Frontiers in Psychology, 11, 558313. 10.3389/fpsyg.2020.558313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, X., Wen, J., Zhou, N., Shi, G., Wang, J., & Skritskaya, N. A. (2021). Psychometric properties of a revised posttraumatic growth inventory and its short form in Chinese Shidu parents. Current Psychology, 1–11. 10.1007/s12144-021-01717-4 [DOI] [Google Scholar]
- Yang, Z. Y. (2000). Familism Culture and Chinese Culture. Kunming: Yunnan University Press. [Google Scholar]
- Zhang, Y., & Jia, X. (2018). A qualitative study on the grief of people who lose their only child: From the perspective of familism culture. Frontiers in Psychology, 9, 869. 10.3389/fpsyg.2018.00869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, M., Yang, F., & Zhang, Y. (2022). The power of culture: The gendered impact of family structures and living arrangements on social networks of Chinese older adults. Ageing and Society, 42(3), 657–680. 10.1017/S0144686X20001087 [DOI] [Google Scholar]
- Zheng, Y., Lawson, T. R., & Anderson Head, B. (2017). “Our only child Has died”—a study of bereaved older Chinese parents. OMEGA - Journal of Death and Dying, 74(4), 410–425. 10.1177/0030222815612285 [DOI] [PubMed] [Google Scholar]
- Zhou, N., Wen, J., Stelzer, E. M., Killikelly, C., Yu, W., Xu, X., … Maercker, A. (2020). Prevalence and associated factors of prolonged grief disorder in Chinese parents bereaved by losing their only child. Psychiatry Research, 284, 112766. 10.1016/j.psychres.2020.112766 [DOI] [PubMed] [Google Scholar]
- Zhou, N., Yu, W., Huang, H., Shi, G., Luo, H., Song, C., … Killikelly, C. (2018). Latent profiles of physical and psychological outcomes of bereaved parents in China who lost their only child. European Journal of Psychotraumatology, 9(1), 1544026. 10.1080/20008198.2018.1544026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data of this study are available from the corresponding author. The data are not publicly available for privacy reasons.