Abstract
Globally, significant progress has been made in the realm of adolescent sexual and reproductive health. We conceptualised “last mile” adolescents as having two or more of the following factors of identity: refugee, Indigenous, 2SLGBTQIA+, out of school, rurally or remotely located, slum dwelling, incarcerated or previously incarcerated, HIV/AIDS infected, and living with a disability. We conducted a scoping review with an aim to synthesise evidence and identify research gaps in the literature pertaining to the sexual and reproductive health and rights (SRHR) of last mile adolescents. We conducted searches in three databases (Embase, Global Health, and Medline). Fifty-four publications met our inclusion criteria. Our results revealed that the state of evidence on the SRHR of last mile adolescents is poor. Very few studies used qualitative and mixed-method inquiry. The number of studies carried out in North America, Europe, and Oceania were limited. We found insufficient disaggregated data with respect to SRHR-related knowledge, behaviour, and access to services. Adopting an intersectional lens is critical to uncover the multiplicative effects of last mile adolescents’ factors of identity on their SRHR. National data systems should be strengthened to enable the collection of quality disaggregated data which can play a vital role in identifying SRHR inequities affecting last mile adolescents. Research priorities should be realigned to generate data globally on the SRHR of last mile adolescents whose lives are marked by intersecting vulnerabilities.
Keywords: sexual and reproductive health, last mile adolescents, intersectionality, low-resourced settings, gender minority, sexual minority, refugee, Indigenous, disaggregated data
Résumé
Dans le monde, des progrès importants ont été accomplis dans le domaine de la santé sexuelle et reproductive des adolescents. Nous avons conceptualisé les adolescents du « dernier kilomètre » comme ceux qui ont au moins deux des facteurs suivants d’identité: réfugié, autochtone, 2SLGBTQIA+, déscolarisé, rural ou vivant dans un lieu écarté, habitant de bidonville, incarcéré ou précédemment incarcéré, infecté par le VIH/sida, et handicapé. Nous avons réalisé une étude de la portée dans le but de synthétiser les données et d’identifier les lacunes de la recherche dans les publications relatives à la santé et aux droits sexuels et reproductifs des adolescents du dernier kilomètre. Nous avons mené des recherches dans trois bases de données (Embase, Global Health et Medline). Cinquante-quatre publications réunissaient nos critères d’inclusion. Nos résultats ont montré la médiocrité de l’état actuel des données sur la santé et les droits sexuels et reproductifs des adolescents du dernier kilomètre. Rares étaient les données qui utilisaient une méthode d’enquête qualitative et mixte. Le nombre d’études réalisées en Amérique du Nord, en Europe et en Océanie était limité. Nous avons constaté une insuffisance des données ventilées en ce qui concerne les connaissances, les comportements et l’accès aux services de santé sexuelle et reproductive. Il est essentiel d’adopter une perspective intersectionnelle pour dévoiler les conséquences multiplicatives des facteurs d’identité des adolescents du dernier kilomètre sur leur santé et leurs droits sexuels et reproductifs. Les systèmes nationaux de données devraient être consolidés pour permettre le recueil de données ventilées de qualité susceptibles de jouer un rôle capital pour identifier les inégalités dans la santé et les droits sexuels et reproductifs qui touchent les adolescents du dernier kilomètre. Les priorités de la recherche devraient être réalignées pour produire des données à l’échelle mondiale sur la santé et les droits sexuels et reproductifs des adolescents du dernier kilomètre dont les vies sont marquées par des vulnérabilités croisées.
Resumen
Mundialmente, se ha logrado progreso significativo en el campo de salud sexual y reproductiva de adolescentes. Conceptualizamos adolescentes de “última milla” como aquellos que tienen dos o más de los siguientes factores de identidad: refugiado, indígena, 2SLGBTQIA+, fuera de la escuela, ubicado en una zona rural o remotamente, vivienda de tugurios, encarcelado actual o anteriormente, infectado por VIH/SIDA, y vive con una discapacidad. Realizamos una revisión de alcance con la finalidad de sintetizar la evidencia e identificar brechas de investigación en la literatura perteneciente a la salud y los derechos sexuales y reproductivos (SDSR) de adolescentes de última milla. Realizamos búsquedas en tres bases de datos (Embase, Global Health y Medline). Cincuenta y cuatro publicaciones reunieron nuestros criterios de inclusión. Nuestros resultados revelaron que el estado de evidencia sobre SDSR de adolescentes es deficiente. Muy pocos estudios utilizaron investigaciones cualitativas o de métodos combinados. Un número limitado de estudios fueron realizados en Norteamérica, Europa y Oceanía. Encontramos insuficientes datos desagregados con respecto al conocimiento, comportamiento y acceso a los servicios relacionados con SDSR. Para descubrir los efectos multiplicativos que tienen los factores de identidad de adolescentes de última milla en su SDSR, es imperativo adoptar una perspectiva interseccional. Se debe fortalecer los sistemas de datos nacionales para permitir la recolección de datos desagregados de calidad, que pueden desempeñar un papel vital en identificar las inequidades de SDSR que afectan a adolescentes de última milla. Se debe realinear las prioridades de investigación para generar datos mundiales sobre SDSR de adolescentes de última milla cuya vida es marcada por vulnerabilidades interrelacionadas.
Introduction
Sexual and reproductive health (SRH) is integral to adolescent well-being and is intimately associated with the protection of human rights.1 The 2030 Agenda for Sustainable Development has given renewed momentum to global efforts toward the improvement of the sexual and reproductive health and rights (SRHR) of young people. Specifically, Sustainable Development Goal (SDG) 3 (target 3.7) and SDG 5 (target 5.6) address universal access to SRH services and realisation of sexual and reproductive rights. The 2030 Agenda has led governments to strengthen their commitment to SRHR as evidenced by multi-stakeholder projects being implemented globally. However, although the 2030 Agenda provided a solid framework for progress in SRHR, it lacks the full scope required to address the unmet SRHR needs of all.2 Underserved populations have distinct needs and continue to face significant obstacles in accessing SRH care. These vulnerable groups include adolescents, gender and sexual minorities, Indigenous peoples, displaced people and refugees, and persons with disabilities.2
Political, social, and economic factors continue to hinder SRHR information and service delivery to adolescents.3 Of the greatest concern with respect to adolescents’ SRHR are “last mile” populations, i.e. those who are difficult to reach with programmes and services, or those farthest away from attaining positive health outcomes. Globally, last mile adolescents or young people have been characterised as populations that are Indigenous, rurally located, live in extreme poverty, and belong to religious, sexual, gender and ethnic minorities, among others.1 Last mile adolescents often face multiple vulnerabilities that make the attainment of optimal health and rights difficult. They are usually met with numerous barriers in accessing SRH services, such as discriminatory attitudes of health professionals, lack of confidentiality at health facilities, and limited availability of these services.4–10 The complexity of interrelated factors such as the effects of poverty, personal agency, social vulnerability, gender, and familial and cultural values and practices must also be considered.5,10–12
Despite the extent of vulnerability characterising last mile adolescents, studies focusing on their SRHR seem to be limited and the state of evidence is poor. Some previous studies have identified gaps in information on health policy, utilisation of services, and SRHR needs and capacities of persons with disabilities in humanitarian settings; barriers and facilitators for SRH care among young Black males in rural areas; the role of conflicting individual and family sociocultural beliefs in young refugees’ transition from puberty to adolescence; and migrant sex workers’ work environments and access to health services.12–15
The term “last mile” remains under-theorised in social science literature. For the purposes of this review, we developed a conceptualisation of “last mile” rooted in the theory of intersectionality, which recognises the compounding disadvantages of overlapping social identities informed by structural elements of race, gender, sexuality, location, social class, disability status, among others.16,17 We refined our definition of “last mile” using an intersectional lens to identify adolescent populations at the lower tiers of the social hierarchy who enjoy limited power and access to valuable resources. To our knowledge, no scoping review has been conducted specifically focusing on the SRHR of last mile adolescents. This article seeks to map the evidence on last mile adolescents’ SRHR from a global perspective and identify research gaps in the existing literature.
Methods
We conducted a scoping review to collate evidence on the SRHR of last mile adolescents. Scoping reviews are useful in synthesising evidence on a particular topic of interest, exploring the types of evidence, and identifying knowledge gaps.18–19 We adopted the five-stage framework put forward wby Arksey and O’Malley20: identifying the research questions, identifying the relevant studies, selecting studies, charting the data, and finally collating the findings. We cross-checked our findings with the themes addressed in Panel 2 of the Guttmacher-Lancet Commission Report.2
Eligibility criteria
As per our conceptualisation, last mile adolescents:
live in low- and middle-income country (LMIC) settings as well as low resourced high-income country (HIC) settings
are characterised by two or more of the following factors of identity that could contribute to health vulnerability: refugee; Indigenous; 2SLGBTQIA+; out of school; rurally or remotely located; slum-dwelling; incarcerated or previously incarcerated; HIV/AIDS infected; and/or living with a disability
Based on our research questions and feasibility constraints, the following criteria were used to identify studies of interest:
Peer-reviewed journal articles
Published in the English language
Published between 2010 and 2020
Includes adolescents aged 10–24
All genders
Populations in the last mile (as described above)
Includes one or more of the following aspects of SRHR: initiation of sexual activity, unwanted pregnancy, unsafe abortion, sexually transmitted infections, early marriage and childbearing, maternal mortality and morbidity, postpartum haemorrhage, social consequences of leaving school, and SRH services
Exclusively school-based studies, non-peer reviewed studies, opinion and editorial pieces, and grey literature were excluded. School-based studies were excluded because education has been identified as a protective factor for sexual health.21–23 Grey literature was excluded because of the challenges associated with identifying the breadth of potential sources and gathering the data. Articles that focused on broader age ranges were only included if age-disaggregated data for adolescents (aged 10–24) were provided in the analysis. Articles that emerged in our search focusing on other markers of vulnerability (apart from the ones mentioned above), such as racial/ethnic minorities and orphans, were also included if they fulfilled the “two or more vulnerabilities” (last mile) inclusion criteria. In some studies, participants, at the time of data collection, were no longer adolescents; however, the aim of these studies was to explore the adolescent SRHR experiences of these participants. Such studies were also included, if the study population fitted the “two or more vulnerabilities” (last mile) criteria.
Article selection
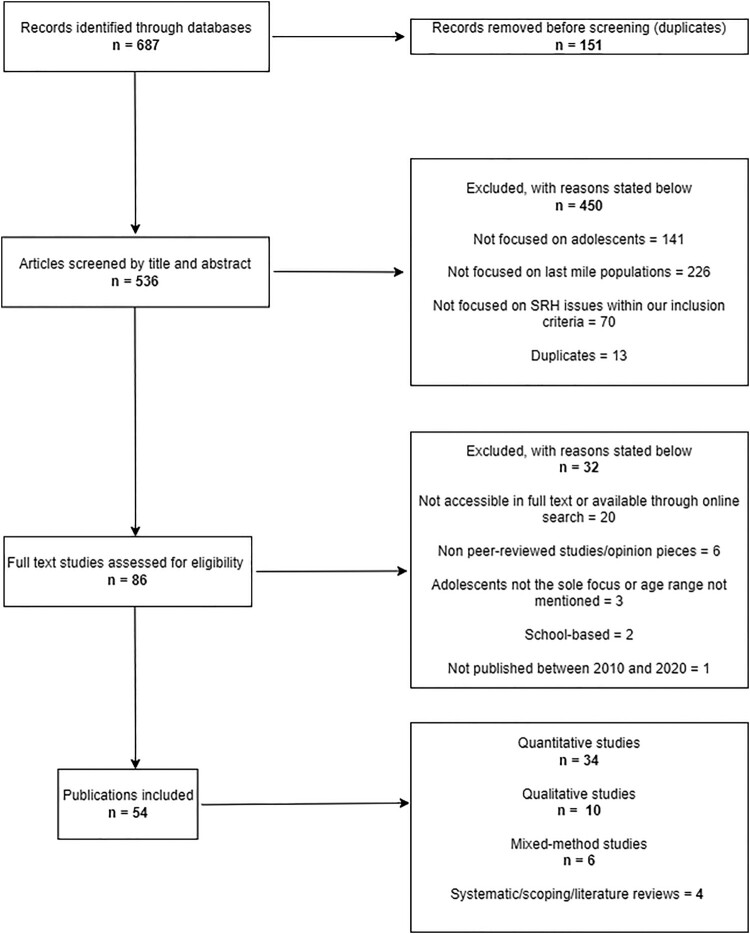
Computerised searches were carried out on three electronic databases: Medline, Embase, and Global Health. Medline and Embase are two of the most authoritative databases used in health research, while Global Health is the only specialised database on public health. The search strategy was customised for each database. Articles published between 2010 and 2020 were filtered. Our search yielded 687 articles in all the three databases combined. These articles were imported into Covidence, an online screening management software, where 151 duplicates were automatically removed, leading to a total of 536 articles.
Two researchers independently carried out the title and abstract screening manually on Covidence for the 536 articles to assess whether they fitted the eligibility criteria. A second title and abstract screening were carried out to ensure the inclusion and exclusion criteria were applied in a consistent manner. Of the 536 articles, 450 were excluded, leading to a remaining total of 86 articles for full-text screening. Articles that could not be located through online search or accessed in full text (20 articles in total) at the time of this review were excluded (see Figure 1 and Appendix). A final tally of 54 peer-reviewed publications met our inclusion criteria and were accessible in full text.4–12,23–67
Figure 1.
Flow diagram of the scoping review process
Data charting
We applied a comprehensive standardised multi-item data charting tool to the 54 articles that underwent full-text review. We adopted a largely deductive approach to data charting. Information was extracted according to key issues and predetermined themes, including basic information such as study aims, publication year, age range of study participants and recruitment method, as well as data on SRH knowledge and behaviour and access to SRH care. We applied a descriptive-analytical method, as recommended by Arksey and O’Malley,20 which is more useful and meaningful than a non-critical manner of data charting that simply reproduces short summaries of articles reviewed. The 54 articles were charted in a uniform manner. However, it was not possible to extract all the required information because not all the articles contained relevant information corresponding to our data charting categories. The researchers were required to take a critical look at the articles and record their own reflections which enabled an ongoing reflective process throughout the data charting exercise.
Results
Characteristics of reviewed publications
Regional distribution of the studies
Thirty-two of the 54 studies focused on last mile populations in sub-Saharan African countries, 13 in Asian countries, and 6 in North American countries (Table 1). Only one study explored the SRH of last mile adolescents in a South American country. None of the studies reviewed had an exclusive focus on European countries or on the Oceania region.
Table 1.
Characteristics of reviewed publications
| Author(s), year | Study design | Study population | ||||
|---|---|---|---|---|---|---|
| Age | Gender | Country of origin/region | Rural/urban | Sampling strategy | ||
| Beguy et al., 201324 | Quantitative, Cross-sectional | 15–19 | Females | Kenya | Urban | Random |
| Beguy et al., 201425 | Quantitative, Longitudinal | 15–22 | Females | Kenya | Urban | Random |
| Blystad et al., 20204 | Qualitative, Cross-sectional | 13–16 | Females | Zambia | Rural | Purposive |
| Bobhate & Shrivastava, 201126 | Quantitative, Cross-sectional | 10–19 | Females | India | Urban | Purposive |
| Bukenya et al., 202027 | Quantitative, Cross-sectional | 10–19 | Males and females | Uganda | Mixed | Random |
| Cadena-Camargo et al., 202028 | Qualitative, Cross-sectional | 18–35a | Females | Colombia | Urban | Snowball |
| Carney et al., 201929 | Mixed-method, Cross-sectional | 16–21 | Females | South Africa | Urban | Purposive |
| Chhabra et al., 201830 | Mixed-method, Cross-sectional | 13–18 | Males and females | Kenya | Urban | Purposive |
| Chimbindi et al., 201831 | Quantitative, Cross-sectional and Longitudinal | 15–24 | Females | South Africa | Rural | Purposive |
| Culbreth et al., 202032 | Quantitative, Cross-sectional | 12–18 | Males and females | Uganda | Urban | Convenience |
| Embleton et al., 20157 | Qualitative, Cross-sectional | 11–24 | Males and females | Kenya | Urban | Purposive |
| Francis et al., 201833 | Quantitative, Cross-sectional | 15–24 | Males and females | South Africa | Rural | Random |
| Gabster et al., 202034 | Qualitative, Cross-sectional | 14–19 | Males and females | Panama | Rural | Purposive |
| Gebreyesus et al., 201935 | Quantitative, Cross-sectional | 10–24 | Males and females | Ethiopia | Rural | Random |
| Gupta et al., 201536 | Quantitative, Cross-sectional | 10–19 | Males and females | India | Mixed | Random |
| Hokororo et al., 201537 | Quantitative, Cross-sectional | 14–20 | Females | Tanzania | Mixed | Purposive |
| Ivanova et al., 20188 | Systematic review | 10–24 | Females | Uganda, Ethiopia, DR Congo, Somalia, Kenya, Nigeria, Djibouti, Rwanda and Sierra Leone | n/a | n/a |
| Ivanova et al., 20199 | Mixed-method, Cross-sectional | 13–19 | Females | Uganda | Rural | Convenience and purposive |
| Kaur, 201838 | Quantitative, Cross-sectional | 15–19 | Females | India | Urban | Not discussed |
| Kayode et al., 20206 | Quantitative, Longitudinal | 16 and above b | Males, transgender women and other/unknown | Nigeria | Urban | Respondent driven |
| Kenny et al., 201939 | Qualitative, Cross-sectional | 15–19 | Females | Cambodia | Rural | Purposive |
| Khawcharoenporn et al., 201940 | Quantitative, Longitudinal | 18–24 | Males | Thailand | Urban | Purposive |
| Latham et al., 201241 | Qualitative, Cross-sectional | Not explicitly stated | Females | USA | Not explicitly stated | Purposive |
| Mark et al., 201711 | Mixed-method, Cross-sectional | Not explicitly stated | Males and females | 23 sub-Saharan African countries | Mixed | Purposive and snowball |
| Mathur et al., 202042 | Quantitative, Cross-sectional | 15–24 | Females | Kenya, Malawi and Zambia | Mixed | Random |
| Mbalinda et al., 201543 | Quantitative, Cross-sectional | 10–19 | Males and females | Uganda | Not explicitly stated | Consecutive |
| McClair et al., 201744 | Quantitative, Cross-sectional | 15–24 | Males | Bangladesh | Urban | Random |
| Melesse et al., 202045 | Literature Review | 15–24 | Males and females | Sub-Saharan Africa | Mixed | n/a |
| Misunas et al., 201946 | Quantitative, Cross-sectional | 20-49b | Males | Bolivia, Central African Republic, Nepal, Lao People’s Democratic Republic, Honduras, Guyana, Guatemala, Cuba, Comoros, Madagascar, Mozambique, Thailand and Nicaragua | Mixed | Two-stage cluster |
| Mtasingwa, 20205 | Qualitative, Cross-sectional | 17–24 | Males and females | Tanzania | Peri-urban | Purposive and random |
| Mu et al., 201547 | Quantitative, Cross-sectional | 12–20 | Males and females | China | Rural | Purposive |
| Ngilangwa et al., 201648 | Mixed-method, Cross-sectional | 10–24 | Males and females | Tanzania | Not explicitly stated | Random, snowball and purposive |
| Nobelius et al., 201149 | Qualitative, Cross-sectional | 13–19 | Males and females | Uganda | Rural | Purposive |
| Nobelius et al., 201250 | Qualitative, Cross-sectional | 13–19 | Males and females | Uganda | Rural | Purposive |
| Parida, 201251 | Quantitative, Cross-sectional | 12–19 | Males and females | India | Rural | Random |
| Ramadhani et al., 202052 | Quantitative, Cross-sectional and longitudinal | 16 and aboveb | Males, transgender women and others | Nigeria | Urban | Respondent driven |
| Ramya et al., 201653 | Quantitative, Cross-sectional | 15–19 | Females | India | Urban | Random |
| Rees et al., 201254 | Quantitative, Cross-sectional | 14–16 | Females | India | Rural | Random |
| Reif et al., 201655 | Quantitative, Cross-sectional | 10–24 | Males and females | Haiti | Urban | Purposive |
| Reisner et al., 201910 | Mixed-method, Cross-sectional | 16–24 | Transgender women, transgender men and others | USA | Not explicitly stated | Purposive |
| Renzaho et al., 201723 | Quantitative, Cross-sectional | 13–24 | Males and females | Uganda | Urban | Random |
| Ricks et al., 201556 | Quantitative, Cross-sectional | 15–23 | Males | USA | Urban | Purposive |
| Robertson et al., 201157 | Quantitative, Longitudinal | 12–18 | Females | USA | Not explicitly stated | Random |
| Rose-clark et al., 201958 | Quantitative, Cross-sectional | 10–19 | Females | India | Rural | Purposive |
| Rosenberg et al., 201559 | Quantitative, Longitudinal | 12–18 | Females | South Africa | Rural | Purposive |
| Sambisa et al., 201060 | Quantitative, Cross-sectional | 15–24 | Males and females | Zimbabwe | Mixed | Two-stage cluster |
| Sharanya, 201461 | Quantitative, Cross-sectional | 13–19 | Females | India | Urban | Multi-stage cluster |
| Swahn et al., 201662 | Quantitative, Cross-sectional | 12–18 | Males and females | Uganda | Urban | Purposive |
| Tirado et al., 202012 | Scoping review | 10–24 | Males and females | Study settings included Australia, Kenya, Uganda, Ethiopia and Tanzania. Sample populations included refugees from Sudan, the Democratic Republic of Congo, Somalia, Burundi, Iraq and Bhutan. | n/a | n/a |
| Toska et al., 202063 | Quantitative, Cross-sectional | 10–24 | Females | South Africa | Mixed | Random and purposive |
| Tumwesigye et al., 201364 | Quantitative, Cross-sectional | 15–24 | Males and females | Uganda | Mixed | Multi-stage cluster |
| Wado et al., 202065 | Scoping review | 10–19 | Males and females | Sub-Saharan Africa | n/a | n/a |
| Wong et al., 201766 | Qualitative, Cross-sectional | 11–19 | Males and females | China | Rural | Purposive |
| Ziraba et al., 201867 | Quantitative, Cross-sectional | 12–23 | Females | Kenya | Urban | Random |
At the time of this study, participants’ age varied from 18 to 35 years; however, their adolescent experiences were explored.
Age-disaggregated data for adolescents available.
Of the 54 studies, 46 indicated whether the study was in an urban setting, rural setting, or both. Of the 46 studies, 20 were conducted in urban areas, 15 in rural areas, 10 in both urban and rural settings, and 1 in a peri-urban setting.
Gender of the study populations
Twenty-five of the 54 publications targeted both male and female last mile adolescents, while 22 exclusively focused on female adolescents, and 4 studies focused on male adolescents. Two studies targeted last mile males, transgender women, and other gender-diverse people and one study focused on last mile transgender men, transgender women, and other gender minorities. Last mile transgender men, gender-fluid, and genderqueer persons were least represented in the reviewed literature.
Study methodologies
Of the retrieved papers, 34 were quantitative, 10 qualitative, 6 mixed-method and 4 were reviews. Of the 34 quantitative studies, 27 were cross-sectional, 5 were longitudinal, and 2 were a mixture of cross-sectional and longitudinal study designs. Two quantitative studies were randomised control trials. All 10 qualitative studies and 6 mixed-method studies were cross-sectional. One mixed-method study included a cluster randomised trial. Of the four review studies, one was a systematic review, one was a general literature overview, and two were scoping reviews.
The identified factors of identity that could lead to vulnerabilities
We explored the various factors of identity that could lead to health vulnerabilities of last mile adolescents studied in 50 publications excluding the four review studies (Table 2). The most common factor of identity was being out of school (31 studies), followed by rural residence (23 studies), infected with HIV/AIDs (16 studies), slum dwelling (12 studies), non-heterosexual (6 studies), belonging to racial and/or ethnic minority groups (4 studies), and incarcerated or having a history of incarceration (3 studies). Refugee, Indigenous adolescents, adolescents living with a disability, and orphaned adolescents were identified in less than four studies while only one study assessed the SRHR of homeless adolescents.
Table 2.
Intersecting factors of identity that could lead to SRHR vulnerabilities among adolescents in 50 reviewed publications
| Indigenous | 2SLGBTQIA+ | Out of school | Rurally located | Slum dwelling | Homeless | Incarcerated/previously incarcerated | HIV/AIDS infected | Physically disabled | Racial/ethnic minorities | Orphaned | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Refugee | 9, 35 | ||||||||||
| Indigenous | 34, 39 | ||||||||||
| 2SLGBTQIA+ | 7 | 5 | 6, 10, 40, 52 | ||||||||
| Out of school | 4, 27–28, 36-37, 42, 46, 49–51, 54, 58-60, 64 | 23–26, 38, 53, 61, 67 | 44 | 29, 43, 47–48 | 48 | 60 | |||||
| Rurally located | 11, 31, 33, 63, 66 | 60 | |||||||||
| Slum dwelling | 32, 55, 62 | 23 | 30 | ||||||||
| Homeless | |||||||||||
| Incarcerated/ previously incarcerated | 41, 56–57 | ||||||||||
| HIV/AIDS infected | 47 | ||||||||||
| Physically disabled | |||||||||||
| Racial/ethnic minorities |
Substantive content of the reviewed studies
Analysis of the data from the 54 selected publications led to the identification of three broad themes: (a) knowledge and awareness, (b) behaviour and practices, and (c) access to services. Table 3 presents an analysis of the regions, methodologies and themes in the reviewed publications and Table 4 describes the linkages between our findings and Panel 2 of the Guttmacher–Lancet Commission Report.
Table 3.
Region, methodology and thematic analysis of 54 reviewed publications
| Category | Sub-category | Number of studies | References |
|---|---|---|---|
| Region | Sub-Saharan Africa | 32 | 4–9, 11, 23-25, 27, 29-33, 35, 37, 42–43, 45, 48–50, 52, 59–60, 62–65, 67 |
| Asia | 13 | 26, 36, 38–40, 44, 47, 51, 53–54, 58, 61, 66 | |
| North America | 6 | 10, 34, 41, 55–57 | |
| South America | 1 | 28 | |
| Methodology | Quantitative | 34 | 6, 23–27, 31–33, 35–38, 40, 42–44, 46–47, 51–64, 67 |
| Qualitative | 10 | 4–5, 7, 28, 34, 39, 41, 49–50, 66 | |
| Mixed method | 6 | 9–11, 29–30, 48 | |
| Review | 4 | 8, 12, 45, 65 | |
| Knowledge | Assessment of quality SRH knowledge | 21 | 8–9, 12, 26, 30, 37–40, 42–43, 46–49, 51, 54, 58, 60–61, 65 |
| Source(s) of information | 6 | 5, 8, 26, 35, 39, 58 | |
| Behaviour and practice | 42 | 4–10, 12, 23–27, 30–35, 37–38, 40, 42–47, 49–50, 52–53, 55–57, 60–65, 67 | |
| Services | Access and/or utilisation | 23 | 4–12, 23, 31, 34, 36, 43–44, 52–54, 58, 61, 63, 65–66 |
| Awareness about available services | 3 | 23, 26, 36 |
Table 4.
Linkages between findings of our scoping review and components of SRHR described in Panel 2 of the Guttmacher–Lancet Commission Report
| Findings of our scoping review | Linkages with Panel 2 of the Guttmacher–Lancet Commission Report |
|---|---|
Knowledge and awareness about:
|
|
Behaviour and practices related to:
|
|
Barriers in access to services:
|
|
Knowledge and awareness
Twenty-three studies reported on knowledge and awareness related to SRHR among last mile adolescents (Table 3). Twenty-one studies focused on the assessment of quality SRHR knowledge among last mile adolescents. Knowledge about basic information relating to STIs and HIV, modes of STI/HIV transmission, condom use negotiation skills, preventive sexual practices, and the female reproductive body, to name a few, were assessed. Sixteen publications explored last mile adolescents’ knowledge about the types, symptoms, and curability of STIs and modes of transmission. Eleven articles described the state of knowledge about preventive sexual practices (e.g. methods of contraception, effectiveness of condoms). Knowledge about menstruation was assessed in six studies: knowledge regarding abortion, fertility, anatomy of the reproductive body, and condom use negotiation skills was highlighted in two studies each; and knowledge pertaining to national health policies was discussed in one study only. Six studies reported the sources of SRHR information for last mile adolescents.
Overall, few studies presented disaggregated data on SRHR knowledge by socioeconomic status, age, gender identity, sexual orientation, and geographical location, or discussed the impact of sociocultural norms on the SRHR knowledge of last mile adolescents. Studies exploring knowledge regarding the physiological functions of reproductive organs and sexual negotiation skills were limited. Assessment of last mile adolescents’ knowledge pertaining to their sexual and reproductive rights (e.g. sexual pleasure, consensual sex, voluntary decision-making based on reproduction and sexuality) and related national laws and policies was found to be especially scant.
Behaviour and practices
Risky sexual behaviour and practices were reported in 42 publications (Table 3). These publications reported high-risk sexual behaviours such as unprotected sex, non-use or low contraceptive use, vaginal/anal sexual intercourse, drug/alcohol abuse, sex in exchange for gifts and/or money, and multiple sexual partnerships. These themes fall under the wide spectrum of high-risk sexual behaviours as defined by various authors.68 Contraceptive use was explored in 33 studies. Contraception was discussed in various contexts, including humanitarian settings, incarceration, slums and rural areas, and multi-country analyses. Transactional sex was discussed in 11 articles. Seven publications reported the association between alcohol/drug use and risky sexual behaviour. Early pregnancy, multiple sexual partnerships, and sexual debut were explored in six studies each. Forced sexual intercourse was discussed in five publications, and menstrual hygiene management in three articles. Disaggregated data on SRHR behaviour and practices by socioeconomic status, sexual orientation, gender identity, ethnicity, and geographical area was found to be limited. Discussions on SRHR behavioural decisions based on sexual pleasure were absent.
Access to services
Access to and/or utilisation of SRH services was discussed in 23 publications (Table 3). Barriers to access to SRH services lead to low utilisation of these services.44 Lack of adolescent-friendly health services was identified as a significant barrier to access to SRH services in 12 publications. These studies cited factors such as judgemental and discriminatory attitudes of health service providers, lack of confidentiality, and feelings of shame, embarrassment, and fear among last mile adolescents as reasons behind their reluctance to seek SRH care. Unaffordability of SRH services was highlighted as a barrier in five articles. Unavailability of some SRH services and commodities (e.g. condoms, abortion services, counselling) at health facilities and refugee camps was identified as a barrier in four publications; distance to health facilities in three studies; and an insufficient number of health care centres in two publications. Only one article highlighted the role of legal restrictions in curtailing access to SRH services. Last mile adolescents residing in urban slums, rural areas, and refugee settlements faced significant challenges in accessing critical SRH care. Awareness about available health services is associated with utilisation of services.36 Knowledge about the availability of SRH services among last mile adolescents was explored in three publications. Four articles presented disaggregated data on utilisation of SRH services by age, school-going status, and gender. Overall, discussions on the effects of restrictive laws and policies and socioeconomic status on access to services were limited. Disaggregated data in relation to access to services and knowledge about the availability of SRH services by socioeconomic status, sexual orientation, gender identity, ethnicity, and geographical area was also found to be scant.
Adopting a “rights” perspective
The Guttmacher–Lancet Commission Report elucidates the principles of human rights related to SRHR (Panel 1), specific elements of sexual and reproductive rights (Panel 2), and the integrated definition of SRHR (Panel 3). The right to SRH includes the freedom to reproductive decision-making “free of discrimination, coercion, and violence”, access SRHR information and services, engage in consensual sex, and “make free, informed, and voluntary decisions” based on one’s “sexuality, sexual orientation, and gender identity”.2 The right to good SRH is, therefore, inextricably linked to universal principles of human rights.
The right to SRH was framed as a human right in eight publications.7,12,23,26,34,38,39,51 Three publications described child marriage as a clear violation of human rights.5,45,46 Four articles invoked the Universal Declaration of Human Rights, Convention on the Rights of the Child, International Covenant on Economic, Social and Cultural Rights, Convention on the Elimination of All Forms of Discrimination against Women, 2030 Agenda, or African Charter on Human and Peoples’ Rights on the Rights of Women in the introductory and/or concluding sections of the articles to briefly frame discussions on early and forced marriage and adolescents’ right to control aspects of their health.4,7,39,46 While three publications presented minimal statistics on knowledge regarding legal age of marriage, SRHR-related national laws and policies, and legality of abortion,26,48,58 only one study systematically assessed last mile adolescents’ knowledge and perceptions on sexual health rights priorities.23
Research gaps identified in the reviewed publications
A review of the 54 publications reveals a diverse set of research gaps related to last mile adolescents’ SRHR. The gaps can be grouped into the following categories: the influence of social conditions and norms on SRH behaviour and practices; data availability; accessibility and utilisation of SRH services; and schooling as a protective factor for sexual health. Six studies highlighted the need to explore the role of sociocultural beliefs and norms on risky SRH practices. Five studies discussed the lack of data and data disaggregation. Four publications called for increased research on the accessibility and utilisation of SRH services along with the barriers to linkage to care. Three studies observed the need to further explore the relationship between school enrolment, risky sexual behaviour, and reproductive outcomes. Last mile adolescent populations characterised by at least one of the following factors of identity require increased research attention: Indigenous, refugees and internally displaced, male youth engaged in sex work, non-binary youth, and mothers living with HIV. Other research gaps mentioned include the need to identify the sources of SRHR information and explore the efficacy of interventions.
Discussion
This scoping review is the first to redefine last mile adolescents through an intersectional lens. We highlighted the health risks to which this segment of the population is susceptible compared to other marginalised groups, making them the “last of the last mile”. Our review suggests that the SRHR of adolescents characterised by at least one of the following factors of identity are under-researched: non-heterosexual, refugees, Indigenous persons, living with a disability, incarcerated or having a history of incarceration, orphaned, homeless, and belonging to racial and/or ethnic minority groups. The SRHR of gender minorities such as transgender men, transgender women, gender-fluid, genderqueer, and non-binary persons also received very little attention in the literature despite the social stigma associated with non-normative expressions of gender69 and the potential that these factors of identity could lead to inequities associated with SRHR. Moreover, there is a limited exclusive focus on the SRHR of heterosexual male adolescents. In the existing literature, the engagement of intersectionality theory along with the study of adolescent SRHR is in its nascence.
The number of studies carried out in the context of countries in North America, Europe, and Oceania was very limited. Last mile adolescents in resource-poor settings in HICs require increased research attention. Very few studies used qualitative and mixed-method inquiry. Qualitative and mixed-method research helps capture health experiences and behaviours, complex phenomena, and the intricacies of the social world, and respond to the multifaceted needs of the stakeholders of policy issues.70,71 Thus, there is a need for increased research in this area, but also – given the strengths of qualitative and mixed-method research – an increase in the number of studies with these types of methodologies is warranted.
The topic of unsafe abortion received limited attention. Early marriage was mostly explored in relation to adolescent girls, not boys. We found a lack of exclusive focus on STIs such as chlamydia, gonorrhoea, and syphilis. Among the sociodemographic factors, race, ethnicity, and religion received less attention than age, gender, education, and geographical location. The influence of sociocultural beliefs, norms, and traditions on SRHR knowledge and behaviour requires increased emphasis. Additionally, there is a need to go beyond cursory descriptions of the linkages between fundamental human rights and SRHR. There exist significant gaps in systematic analyses of SRH-related knowledge, behaviour, perceptions, and access to services through a “rights” lens.
Our review points to insufficient disaggregated data with respect to SRHR knowledge, behaviour, and access to services across different adolescent sub-populations. Moreover, due to the limited focus on gender and sexual minorities, disability and refugee status, and Indigeneity in the publications reviewed, the distinct service barriers faced by adolescents in these populations were not comprehensively identified. Disaggregated data plays a vital role in the achievement of health equity by shedding light on the health needs and experiences of underrepresented populations.12,72 Health researchers have consistently highlighted the need for increased sex-, gender-, age- and racially and ethnically disaggregated data.73–75 Data on other factors of social identity including religion, disability status, available income, HIV or parental status are not routinely collected.76–77 This could be because studies – whether because of sampling limitations or lack of specific interest – do not aim to study sub-group differences at the outset. If researchers do include sociodemographic sub-groups, it is most commonly only one or two (sex/gender or age, for instance) and not multiple identities simultaneously. From the participant perspective, some of these social identities are stigmatised, there may be privacy concerns or people may not wish to report this information regardless of whether it is asked. These concerns and issues are still being considered from ethical and methodological perspectives. Disaggregated data would enable researchers to delve more deeply into the state of SRHR knowledge and behaviour of last mile adolescents and identify intra- and inter-group health disparities. This specific knowledge could more effectively inform health interventions that target last mile populations.
The purpose of this scoping review was to synthesise the literature on the SRHR of last mile adolescents. Our review suggests that the state of evidence on the SRHR of last mile adolescents is poor. In addition to reversing the data bias towards heterosexual and cisgender adolescents, there is an urgent need to extend the scope of research to capture the varied SRH-related behaviours and experiences of adolescents through an intersectional lens. Adopting an intersectional lens can help shed light on the multiplicative effects of last mile adolescents’ factors of identity on their SRHR. Research priorities ought to be realigned with a view to generating data globally on the SRHR of last mile adolescents whose lives are marked by intersecting vulnerabilities. An empirical process of research gap validation and prioritisation should be conducted at the national level with the respective stakeholders in multiple country contexts.
This scoping review has some limitations. We excluded non-English articles which may have resulted in the under-representation of some regions such as South America and Europe in our findings. Additionally, the exclusion of grey literature may have led us to miss references to key publications that our database search possibly omitted. We were also unable to locate a few articles through online search or access them in full text at the time of this review which potentially could have contributed to some important insights on last mile adolescents’ SRHR. Despite these limitations, this review makes important contributions to the literature on last mile adolescents’ SRHR, using an intersectional lens.
Summary and implications
We would like to highlight the urgency of generating evidence on last mile adolescents’ SRHR to capture the deprivation being experienced by the most vulnerable adolescents globally. An intersectional lens is critical for the identification of last mile adolescents and tackling the SRHR inequities among this population. Data systems should be strengthened to enable the collection of quality disaggregated data by gender, location, education, parental and disability status, sexual orientation, Indigeneity, religion, ethnicity, income, etc. Generating robust data would be a foundational step for future programming and policy action. However, privacy laws and criminalisation of 2SLGBTQIA+ identity may present significant challenges in collecting disaggregated data in some countries. Finally, we highlighted the factors of identity of last mile adolescents and dimensions of SRHR that are understudied in the literature. These research gaps ought to be prioritised at the individual country level through a consultative multi-stakeholder process involving government officials, development practitioners, researchers, and youth representatives.
Appendix.
Articles that could not be located through online search or accessed in full text at the time of the scoping review
| Authors | Title |
|---|---|
| Alemu T, Fantahun M | Sexual and reproductive health status and related problems of young people with disabilities in selected associations of people with disability, Addis Ababa, Ethiopia. Ethiop Med J. 2011;49(2):97-108. |
| Bamigboye F, Faponle D | Sexual violence against women and girls fuelling the spread of HIV in urban communities than rural communities in Ondo State, Nigeria. Journal of the International AIDS Society. 2020;23(SUPPL 4): DOI: 10.1002/jia2.25547 |
| Bliss KE | Overcoming barriers to reducing adolescent pregnancy and improving maternal health in Nicaragua In: Schwartz, D. (eds) Maternal Death and Pregnancy-Related Morbidity Among Indigenous Women of Mexico and Central America. Global Maternal and Child Health. Springer, Cham; 2018. DOI: 10.1007/978-3-319-71538-4_38 |
| Destil MNE, Steben M, Clermont M, et al | Factors influencing the sexual and reproductive health of the teenagers in rural areas in Haiti. Tropical Medicine and International Health. 2013;18(1):180. |
| Elimam BGM | Providing post abortion care in a humanitarian setting-an experience from Darfur, Sudan. International Journal of Gynecology and Obstetrics. 2018;143(SUPPL 3):114. DOI: 10.1002/ijgo.12583. |
| Fang LC, Ping NJ, Ping YY | Analysis of the sexual behavior and the influential factors of AIDS infection among out-of-school adolescent MSM in Chongqing. Acta Medicinae Universitatis Scientiae et Technologiae Huazhong. 2015;44(5):603-615. |
| Goyal RS | Whether educational poverty (Deprivation of schooling) affects the adolescent girls’ vulnerability to reproductive and sexual health concerns? Journal of Sexual Medicine. 2013;10(SUPPL. 2):172. DOI: 10.1111/jsm.12150 |
| Hamzah L, Hamlyn E | Sexual and reproductive health in HIV-positive adolescents. Current opinion in HIV and AIDS. 2018;13(3):230-235. DOI: 10.1097/COH.0000000000000456 |
| Imakit R, Ajok S, Talima D, et al | Sexual and reproductive health needs and experiences of youth living with HIV. Journal of the International AIDS Society. 2016;19(5):55. |
| Ivanova O, Nyakato VN, Mlahagwa W, et al | Sexual and reproductive health of refugee adolescent girls in Nakivale refugee settlement in Uganda. International Journal of Gynecology and Obstetrics. 2018;143(3):536. |
| Joshi A, Basu A, Marhefka S | If it is kept secret, it is acceptable: cultural norms and sexual risk behavior among tribal adolescents in Vadodara, India. J Adolesc Heal. 2010;46(2, Supplement 1):S5. DOI:10.1016/j.jadohealth.2009.11.012. |
| Kayalvizhi M, Jagathambal P | Awareness among selected rural adolescent girls on HIV/AIDS. Advance Research Journal of Social Science. 2016;7(2):275-278. |
| Kennedy A, Stathis S | The health and well-being of incarcerated adolescents. Journal of Paediatrics and Child Health. 2011;47(2):14. |
| Liamputtong P | Children, young people and HIV/AIDS: a cross-cultural perspective. In P. Liamputtong (Ed.), Children and Young People Living with HIV/AIDS: A Cross-Cultural Perspective. Springer, Cham; 2016. DOI:10.1007/978-3-319-29936-5_1. |
| Matson PA, Towe VL, Chung SE, et al | Examining the role sexual validation plays on STI risk among adolescent and young adult men involved in the criminal justice system. Journal of Adolescent Health. 2015;56(2 SUPPL. 1):S77-S78. DOI: 10.1016/j.jadohealth.2014.10.154. |
| Pizzol D, Gennaro F, Boscardin C, et al | Teenage pregnancies in Mozambique: the experience of “Servicios Amigos dos Adolescentes” clinics in Beira. African Journal of AIDS Research. 2018;17(1):32-36. |
| Salau ES, Yahaya H, Bello M, et al | Assessment of HIV/AIDS perception and preventive practices among rural youths in Nasarawa State, Nigeria. Journal of Biology, Agriculture and Healthcare. 2012;2(10):17-23. |
| Templeton DJ, Tyson BA, Meharg JP, et al | Aboriginal health worker screening for sexually transmissible infections and blood-borne viruses in a rural Australian juvenile correctional facility. Sex Health. 2010;7(1):44-48. DOI:10.1071/SH09035. |
| Tondare D, Chandra Sekhar K, Kembhavi RS | Knowledge about sexually transmitted diseases and HIV among adolescent boys in urban slums of Mumbai. Indian Journal of Public Health Research and Development. 2013;4(1):75-79. |
| Zaw PPT | Unmet reproductive health needs among poor youths in the slums of Mandalay city, Myanmar. European Journal of Contraception and Reproductive Health Care. 2013;18(1):S99. |
Funding Statement
This work was supported by the Canadian Institutes of Health Research (CIHR) [grant number 168238/2020].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.World Health Organization . Sexual health, human rights and the law. Share-Net Int; 2017. https://share-netinternational.org/sexual-health-human-rights-law/.
- 2.Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress-sexual and reproductive health and rights for all: report of the Guttmacher-Lancet commission. Lancet. 2018;391(10140):2642–2692. DOI: 10.1016/S0140-6736(18)30293-9. [DOI] [PubMed] [Google Scholar]
- 3.Morris JL, Rushwan H.. Adolescent sexual and reproductive health: the global challenges. Int J Gynecol Obstet. 2015;131:S40–S42. DOI: 10.1016/j.ijgo.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Blystad A, Moland KM, Munsaka E, et al. Vanilla bisquits and lobola bridewealth: parallel discourses on early pregnancy and schooling in rural Zambia. BMC Public Health. 2020;20(1):1–11. DOI: 10.1186/s12889-020-09555-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mtasingwa LV. Challenges facing Tanzanian youth in the fight against HIV/AIDS: lessons learnt from Mbeya region, southern highlands. Forum Dev Stud. 2020;47(2):283–306. DOI: 10.1080/08039410.2020.1784264. [DOI] [Google Scholar]
- 6.Kayode BO, Mitchell A, Ndembi N, et al. Retention of a cohort of men who have sex with men and transgender women at risk for and living with HIV in Abuja and Lagos, Nigeria: a longitudinal analysis. J Int AIDS Soc. 2020;23(S6):40–50. DOI: 10.1002/jia2.25592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Embleton L, Wachira J, Kamanda A, et al. “Once you join the streets you will have to do it”: sexual practices of street children and youth in Uasin Gishu County, Kenya Adolescent Health. Reprod Health. 2015;12(1):1–11. doi: 10.1186/s12978-015-0090-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ivanova O, Rai M, Kemigisha E.. A systematic review of sexual and reproductive health knowledge, experiences and access to services among refugee, migrant and displaced girls and young women in Africa. Int J Environ Res Public Health. 2018;15(8):1–12. DOI: 10.3390/ijerph15081583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ivanova O, Rai M, Mlahagwa W, et al. A cross-sectional mixed-methods study of sexual and reproductive health knowledge, experiences and access to services among refugee adolescent girls in the Nakivale refugee settlement, Uganda. Reprod Health. 2019;16(1):1–11. DOI: 10.1186/s12978-019-0698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reisner SL, Jadwin-Cakmak L, Sava L, et al. Situated vulnerabilities, sexual risk, and sexually transmitted infections’ diagnoses in a sample of transgender youth in the United States. AIDS Patient Care STDS. 2019;33(3):120–130. DOI: 10.1089/apc.2018.0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mark D, Armstrong A, Andrade C, et al. HIV treatment and care services for adolescents: a situational analysis of 218 facilities in 23 sub-Saharan African countries. J Int AIDS Soc. 2017;20(Suppl 3):25–33. DOI: 10.7448/IAS.20.4.21591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tirado V, Chu J, Hanson C, et al. Barriers and facilitators for the sexual and reproductive health and rights of young people in refugee contexts globally: a scoping review. PLoS One. 2020;15(7):1–25. DOI: 10.1371/journal.pone.0236316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanabe M, Nagujja Y. “We have a right to love"—The Intersection of Sexual and Reproductive Health and Disability for Urban Refugees in Kampala, Uganda [Internet]. Women’s Refugee Commission; 2014. [cited 2022 Feb 17]. https://www.refworld.org/docid/57ff6fa54.html.
- 14.Burns JC, Reeves J, Calvert WJ, et al. Engaging young Black males in sexual and reproductive health care: a review of the literature. Am J Mens Health. 2021;15(6). DOI: 10.1177/15579883211062024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McBride B, Janushev T.. Criminalisation, health, and labour rights among im/migrant sex workers globally. In: Goldenberg SM, Morgan TR, Forbes A, Baral S, editors. Sex work, health, and human rights. Cham: Springer; 2021. p. 153–171. [PubMed] [Google Scholar]
- 16.Kapilashrami A. What is intersectionality and what promise does it hold for advancing a rights-based sexual and reproductive health agenda? BMJ Sexual Reprod Health. 2020;46:4–7. [DOI] [PubMed] [Google Scholar]
- 17.Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Droit Soc. 2021;108(2):465–487. DOI: 10.3917/drs1.108.0465. [DOI] [Google Scholar]
- 18.Daudt HM, van MC, Scott SJ.. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48. DOI: 10.1186/1471-2288-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143, DOI: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arksey H, O’Malley L.. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32. DOI: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 21.Mmari K, Sabherwal S.. A review of risk and protective factors for adolescent sexual and reproductive health in developing countries: an update. J Adolesc Heal. 2013;53(5):562–572. DOI: 10.1016/j.jadohealth.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 22.Griese ER, Kenyon DB, McMahon TR.. Identifying sexual health protective factors among Northern Plains American Indian youth: an ecological approach utilizing multiple perspectives. Am Indian Alsk Native Ment Health Res. 2016;23(4):16–43. DOI: 10.5820/aian.2304.2016.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Renzaho AMN, Kamara JK, Georgeou N, et al. Sexual, reproductive health needs, and rights of young people in slum areas of Kampala, Uganda: A cross sectional study. PLoS ONE. 2017;12(1):1–21. DOI: 10.1371/journal.pone.0169721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beguy D, Mumah J, Gottschalk L.. Unintended pregnancies among young women living in urban slums: evidence from a prospective study in Nairobi city, Kenya. PLoS ONE. 2014;9(7):1–10. DOI: 10.1371/journal.pone.0101034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beguy D, Ndugwa R, Kabiru CW.. Entry into motherhood among adolescent girls in two informal settlements in Nairobi, Kenya. J Biosoc Sci. 2013;45(6):721–742. DOI: 10.1017/S0021932013000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bobhate PS, Saurabh SR.. Cross sectional study of knowledge and practices about reproductive health among female adolescents in an urban slum in Mumbai. J Fam Reprod Health. 2011;5(4):119–126. [Google Scholar]
- 27.Bukenya JN, Nakafeero M, Ssekamatte T, et al. Sexual behaviours among adolescents in a rural setting in eastern Uganda: a cross-sectional study. Trop Med Int Health. 2020;25(1):81–88. DOI: 10.1111/tmi.13329. [DOI] [PubMed] [Google Scholar]
- 28.Cadena-Camargo Y, Krumeich A, Duque-Páramo MC, et al. Experiences of pregnancy in adolescence of internally displaced women in Bogotá: an ethnographic approach. Reprod Health. 2020;17(1):1–12. DOI: 10.1186/s12978-020-0889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carney T, Browne FA, Myers B, et al. Adolescent female school dropouts who use drugs and engage in risky sex: effects of a brief pilot intervention in Cape Town, South Africa. AIDS Care Psychol Socio-Medical Asp AIDS/HIV. 2019;31(1):77–84. DOI: 10.1080/09540121.2018.1500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chhabra R, Teitelman N, Silver EJ, et al. Vulnerability multiplied: health needs assessment of 13–18-year-old female orphan and vulnerable children in Kenya. World Med Heal Policy. 2018;10(2):129–145. DOI: 10.1002/wmh3.267. [DOI] [Google Scholar]
- 31.Chimbindi N, Mthiyane N, Birdthistle I, et al. Persistently high incidence of HIV and poor service uptake in adolescent girls and young women in rural KwaZulu-Natal, South Africa prior to DREAMS. PLoS One. 2018;13(10):1–17. DOI: 10.1371/journal.pone.0203193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Culbreth R, Swahn MH, Salazar LF, et al. Risk factors associated with HIV, sexually transmitted infections (STI), and HIV/STI Co-infection among youth living in the slums of Kampala, Uganda. AIDS Behav. 2020;24(4):1023–1031. DOI: 10.1007/s10461-019-02444-5. [DOI] [PubMed] [Google Scholar]
- 33.Francis SC, Mthiyane TN, Baisley K, et al. Prevalence of sexually transmitted infections among young people in South Africa: a nested survey in a health and demographic surveillance site. PLoS Med. 2018;15(2):1–25. DOI: 10.1371/journal.pmed.1002512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gabster A, Mayaud P, Pascale JM, et al. Gender norms and sexual behaviours among indigenous youth of the Comarca Ngäbe-Buglé, Panama. Cult Heal Sex. 2020;22(9):1032–1046. DOI: 10.1080/13691058.2019.1648873. [DOI] [PubMed] [Google Scholar]
- 35.Gebreyesus H, Berhe T, Welegebriel Z, et al. Premarital sexual practice and associated factors among adolescents in the refugee camps in Tigray, Northern Ethiopia. BMC Res Notes. 2019;12(1):1–7. DOI: 10.1186/s13104-019-4459-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gupta M, Bhatnagar N, Bahugana P.. Inequity in awareness and utilization of adolescent reproductive and sexual health services in union territory, Chandigarh, North India. Indian J Public Health. 2015;59(1):9–17. DOI: 10.4103/0019-557X.152846. [DOI] [PubMed] [Google Scholar]
- 37.Hokororo A, Kihunrwa A, Hoekstra P, et al. High prevalence of sexually transmitted infections in pregnant adolescent girls in Tanzania: a multi-community cross-sectional study. Sex Transm Infect. 2015;91(7):473–478. DOI: 10.1136/sextrans-2014-051952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaur G. Factors influencing HIV awareness amongst adolescent women: a study of slums in Delhi. Demogr. India. 2018;47:100–111. [Google Scholar]
- 39.Kenny B, Hoban E, Pors P, et al. A qualitative exploration of the sexual and reproductive health knowledge of adolescent mothers from indigenous populations in Ratanak Kiri Province, Cambodia. Rural Remote Health. 2019;19(4):5240. DOI: 10.22605/RRH5240.46. [DOI] [PubMed] [Google Scholar]
- 40.Khawcharoenporn T, Mongkolkaewsub S, Naijitra C, et al. HIV risk, risk perception and uptake of HIV testing and counseling among youth men who have sex with men attending a gay sauna. AIDS Res Ther. 2019;16(1):1–11. DOI: 10.1186/s12981-019-0229-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Latham TP, Sales JM, Renfro TL, et al. Employing a teen advisory board to adapt an evidence-based HIV/STD intervention for incarcerated African-American adolescent women. Health Educ Res. 2012;27(5):895–903. DOI: 10.1093/her/cyr003. [DOI] [PubMed] [Google Scholar]
- 42.Mathur S, Pilgrim N, Patel SK, et al. HIV vulnerability among adolescent girls and young women: a multi-country latent class analysis approach. Int J Public Health. 2020;65(4):399–411. DOI: 10.1007/s00038-020-01350-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mbalinda SN, Kiwanuka N, Eriksson LE, et al. Correlates of ever had sex among perinatally HIV-infected adolescents in Uganda. Reprod Health. 2015;12(1):1–10. DOI: 10.1186/s12978-015-0082-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McClair TL, Hossain T, Sultana N, et al. Paying for sex by young Men Who live on the streets in Dhaka city: compounded sexual risk in a vulnerable migrant community. J Adolesc Heal. 2017;60(2):S29–S34. DOI: 10.1016/j.jadohealth.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 45.Melesse DY, Mutua MK, Choudhury A, et al. Adolescent sexual and reproductive health in sub-Saharan Africa: who is left behind? BMJ Glob Heal. 2020;5(1):1–8. DOI: 10.1136/bmjgh-2019-002231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Misunas C, Gastón CM, Cappa C.. Child marriage among boys in high-prevalence countries: an analysis of sexual and reproductive health outcomes. BMC Int Health Hum Rights. 2019;19(1):1–16. DOI: 10.1186/s12914-019-0212-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mu W, Zhao Y, Khoshnood K, et al. Knowledge and perceptions of sexual and reproductive health and HIV among perinatally HIV-infected adolescents in rural China. AIDS Care Psychol Socio-Medical Asp AIDS/HIV. 2015;27(9):1137–1142. DOI: 10.1080/09540121.2015.1032206. [DOI] [PubMed] [Google Scholar]
- 48.Ngilangwa DP, Rajesh S, Kawala M, et al. Accessibility to sexual and reproductive health and rights education among marginalized youth in selected districts of Tanzania. Pan Afr Med J. 2016;25(Supp 2):1–7. DOI: 10.11604/pamj.supp.2016.25.2.10922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nobelius AM, Kalina B, Pool R, et al. Sexual partner types and related sexual health risk among out-of-school adolescents in rural south-west Uganda. AIDS Care Psychol Socio-Medical Asp AIDS/HIV. 2011;23(2):252–259. DOI: 10.1080/09540121.2010.507736. [DOI] [PubMed] [Google Scholar]
- 50.Nobelius AM, Kalina B, Pool R, et al. “The young ones are the condom generation”: condom use amongst out-of-school adolescents in rural southwest Uganda. J Sex Res. 2012;49(1):88–102. DOI: 10.1080/00224499.2011.568126. [DOI] [PubMed] [Google Scholar]
- 51.Parida P. Understanding on life skill education and adolescent reproductive sexual health in tribal districts of Odisha. Glob Adv Res J Educ Res Rev. 2012;1(6):100–105. http://garj.org/garjerr/pdf/2012/july/Parida.pdf. [Google Scholar]
- 52.Ramadhani HO, Crowell TA, Nowak RG, et al. Association of age with healthcare needs and engagement among Nigerian men who have sex with men and transgender women: cross-sectional and longitudinal analyses from an observational cohort. J Int AIDS Soc. 2020;23(S6):70–79. DOI: 10.1002/jia2.25599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ramya V, Reddy MR, Sridevi BK.. A study on reproductive morbidity and menstrual hygiene among adolescent girls of urban slum area of Chitradurga. Natl J Community Med. 2016;7(3):180–183. www.njcmindia.org. [Google Scholar]
- 54.Rees CA, Long KN, Gray B, et al. Educating for the future: adolescent girls’ health and education in West Bengal, India. Int J Adolesc Med Health. 2012;24(4):321–327. DOI: 10.1515/ijamh-2012-0046. [DOI] [PubMed] [Google Scholar]
- 55.Reif LK, Rivera V, Louis B, et al. Community-based HIV and health testing for high-risk adolescents and youth. AIDS Patient Care STDS. 2016;30(8):371–378. DOI: 10.1089/apc.2016.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ricks JM, Crosby RA, Terrell I.. Elevated sexual risk behaviors among postincarcerated young African American males in the south. Am J Mens Health. 2015;9(2):132–138. DOI: 10.1177/1557988314532680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robertson AA, St Lawrence J, Morse DT, et al. The healthy teen girls project: comparison of health education and STD risk reduction intervention for incarcerated adolescent females. Health Educ Behav. 2011;38(4):423. Robertson, Angela R [corrected to Robertson, Angela A]]. Health Educ Behav. 2011;38(3):241–250. DOI: 10.1177/1090198110372332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rose-Clarke K, Pradhan H, Rath S, et al. Adolescent girls’ health, nutrition and wellbeing in rural eastern India: a based study. BMC Public Health. 2019;19(673):1–11. DOI: 10.1186/s12889-019-7053-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosenberg M, Pettifor A, Miller WC, et al. Relationship between school dropout and teen pregnancy among rural South African young women. Int J Epidemiol. 2015;44(3):928–936. DOI: 10.1093/ije/dyv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sambisa W, Curtis SL, Stokes CS.. Ethnic differences in sexual behaviour among unmarried adolescents and young adults in Zimbabwe. J Biosoc Sci. 2010;42(1):1–26. DOI: 10.1017/S0021932009990277. [DOI] [PubMed] [Google Scholar]
- 61.Sharanya T. Reproductive health status and life skills of adolescent girls dwelling in slums in Chennai, India. Natl Med J India. 2014;27(6):305–310. [PubMed] [Google Scholar]
- 62.Swahn MH, Culbreth R, Salazar LF, et al. Prevalence of HIV and associated risks of sex work among youth in the slums of Kampala. AIDS Res Treat. 2016. DOI: 10.1155/2016/5360180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Toska E, Cluver L, Laurenzi CA, et al. Reproductive aspirations, contraception use and dual protection among adolescent girls and young women: the effect of motherhood and HIV status. J Int AIDS Soc. 2020;23(S5):47–53. DOI: 10.1002/jia2.25558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tumwesigye NM, Ingham R, Holmes D.. Condom use at first and latest sexual events among young people: evidence from a rural and peri-urban setting in Uganda. Afr Health Sci. 2013;13(2):407–414. DOI: 10.4314/ahs.v13i2.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wado YD, Bangha M, Kabiru CW, et al. Nature of, and responses to key sexual and reproductive health challenges for adolescents in urban slums in sub-Saharan Africa: A scoping review. Reprod Health. 2020;17(1):1–14. DOI: 10.1186/s12978-020-00998-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wong WCW, Holroyd E, Miu HYH, et al. Secrets, shame and guilt: HIV disclosure in rural Chinese families from the perspective of caregivers. Vulnerable Child Youth Stud. 2017;12(4):292–303. DOI: 10.1080/17450128.2017.1344343.21. [DOI] [Google Scholar]
- 67.Ziraba A, Orindi B, Muuo S, et al. Understanding HIV risks among adolescent girls and young women in informal settlements of Nairobi, Kenya: lessons for DREAMS. PLoS One. 2018;13(5):1–20. DOI: 10.1371/journal.pone.0197479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chawla N, Sarkar S.. Defining “high-risk sexual behavior” in the context of substance use. J Psychosexual Health. 2019;1(1):26–31. DOI: 10.1177/2631831818822015. [DOI] [Google Scholar]
- 69.Herek G. A nuanced view of stigma for understanding and addressing sexual and gender minority health disparities. LGBT Heal. 2016;3(6):397–399. [DOI] [PubMed] [Google Scholar]
- 70.Creswell JW. Mixed-method research: Introduction and application. Handb Educ Policy. 1999: 455–472. DOI: 10.1016/B978-012174698-8/50045-X. [DOI] [Google Scholar]
- 71.O’Day B, Killeen M.. Research on the lives of persons with disabilities: the emerging importance of qualitative research methodologies. J Disabil Policy Stud. 2002;13(1):9–15. DOI: 10.1177/10442073020130010201. [DOI] [Google Scholar]
- 72.Nguyen AB, Chawla N, Noone AM, et al. Disaggregated data and beyond: future queries in cancer control research. Cancer Epidemiol Biomarkers Prev. 2014;23(11):2266–2272. DOI: 10.1158/1055-9965.EPI-14-0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nowatzki N, Grant KR.. Sex Is Not enough: the need for gender-based analysis in health research. Health Care Women Int. 2011;32(4):263–277. [DOI] [PubMed] [Google Scholar]
- 74.UNICEF . Collecting and reporting of sex- and age-disaggregated data on adolescents at the sub-national level; 2016. https://data.unicef.org/wp-content/uploads/2016/11/Data-Abstraction-Guide-November-2016.pdf.
- 75.Kauh TJ, Read JG, Scheitler AJ.. The critical role of racial/ethnic data disaggregation for health equity. Popul Res Policy Rev. 2021;40(1). DOI: 10.1007/s11113-020-09631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kingori C, Esquivel CL, Hassan Q, et al. Recommendations for developing contextually relevant HIV/AIDS prevention strategies targeting African-born immigrants and refugees in the United States. AIDS Patient Care STDS. 2016;30(10):476–483. DOI: 10.1089/apc.2016.0171. [DOI] [PubMed] [Google Scholar]
- 77.OHCHR . A human rights-based approach to data: leaving no one behind in the 2030 agenda for sustainable development; 2018. https://www.ohchr.org/Documents/Issues/HRIndicators/GuidanceNoteonApproachtoData.pdf.