Abstract
Background.
The purpose of this study was to examine outcomes, toxicity, and dosimetric characteristics of patients treated with reirradiation for head and neck cancers.
Methods.
Fifty patients underwent ≥2 courses of radiation therapy (RT) postoperatively or definitively with or without chemotherapy. Composite dose volume histograms (DVHs) for selected anatomic structures were correlated with grade ≥3 late toxicity.
Results.
Median initial and retreatment radiation dose was 64 and 60 Gy, respectively. Median overall survival (OS), progression-free survival (PFS), and 1-year PFS rates were 18 months, 11 months, and 45%, respectively, with 13 months median follow-up. Thirty-four percent of patients experienced grade ≥3 late toxicity with 1 death from carotid blowout. The DVH corresponding to the carotid blowout fell above the third quartile compared with other patients.
Conclusion.
Our analysis is the first to systematically evaluate the dose to the carotid artery using composite dosimetry in head and neck reirradiation patients, and demonstrates a promising technique for evaluating the dose to other normal tissue structures.
Keywords: head and neck, reirradiation, carotid arteries, blowout, dosimetry
INTRODUCTION
Patients with recurrent or second primary head and neck squamous cell carcinomas (HNSCCs) have traditionally faced limited treatment options. Surgical resection, when feasible, is considered first line treatment in patients with local-only recurrence. However, operability and resectability is contingent on anatomic as well as patient factors (ie, comorbidities and performance status). Although surgical patients demonstrate improved outcomes compared with those who are deemed unfit/unresectable, 5-year overall survival (OS) rates remain poor.1 As the majority of patients are ineligible for surgery, current standard therapy includes chemoradiotherapy, palliative/salvage chemotherapy, radiation therapy (RT) alone, or best supportive care. Treatment with chemotherapy alone portends a lower survival relative to the surgical group, with the 2-year to 3-year OS rates of 5% to 10%.2–6
Concern for increased acute and chronic treatment-related toxicities has resulted in a provider bias against reirradiation as a potential treatment option. Specific concerns relate to toxicities associated with high composite radiation dose and include carotid blowout, osteoradionecrosis, trismus, and spinal cord injury. Despite these concerns, a decade of studies has demonstrated reirradiation with or without chemotherapy to be a potentially safe and effective treatment option in well-selected patients.
The therapeutic ratio remains narrow for radiation treatment in HNSCC, even in the setting of primary course. Therefore, recent prospective and retrospective studies have aimed to limit toxicity through various techniques, such as utilization of split course hyperfractionated treatment, along with more tightly conformal methods, such as intensity modulated radiotherapy (IMRT).7–12 A recent phase III randomized trial demonstrated a disease-free survival advantage in postoperative patients who underwent reirradiation and chemotherapy versus observation with radiation as salvage therapy. However, the OS was not statistically different, presumably because of the increased acute and late toxicities, as well as crossover with salvage radiation.13
Careful attention to various key structures of the head and neck through analysis of composite dosimetry may allow improvement in therapeutic ratio, leading to improved OS as well as preserved quality of life.
MATERIALS AND METHODS
Patients
A retrospective review of patients with HNSCC treated at our institution who underwent at least 2 courses of radiation treatment, was carried out with institutional review board approval. Inclusion criteria required patients to have undergone reirradiation with nonpalliative intent for recurrent or second primary HNSCC. Recurrences and second primary cancers were typically detected through follow-up imaging study (CT or positron emission tomography [PET]/CT), and confirmed via biopsy in equivocal cases. Lymphoma was allowed if this represented the initial course, although all retreatments were for HNSCCs. The indication for repeat radiation treatment was either local recurrence or second primary HNSCC with treatment intensity ≥30 Gy. Patients who were selected for reirradiation had disease recurrence/second primary cancer arise ≥6 months after the initial treatment course, to help select out patients with radioresistant tumors. Subjective ability to tolerate further treatment was also a major factor in determining eligibility and was assessed utilizing the Eastern Cooperative Oncology Group (ECOG) score. Patients who underwent salvage reirradiation for unresectable recurrent disease and patients who underwent postoperative/adjuvant reirradiation were included in this study. Postoperative reirradiation was typically only selected for patients who demonstrated a high risk of recurrence, which, in accordance with prior literature, was determined as evidence of extracapsular extension of tumor, or positive or close surgical margins.13–15 Patients with unresectable, limited volume recurrence in a previously treated field were treated with salvage concurrent chemoradiotherapy without surgical resection. Second primary cancers were restaged based on new disease presentation. Recurrences were not explicitly restaged using the American Joint Committee on Cancer TNM system, except to note locoregional failure deemed amenable to reirradiation with definitive intent.
Fifty patients met these criteria and were included in the study. In order to provide information about the extent of recurrence and treatment area, the planning target volume (PTV) in cubic centimeters was recorded for both recurrent and second primary cancers. This represented volume of gross disease in all patients as no elective nodal coverage was pursued. Comprehensive dosimetric analysis was limited to 21 patients who had available initial and retreatment radiotherapy plans. ECOG performance status, age at retreatment, smoking history, and tumor characteristics were gathered for all patients.
Treatment
Patients were seen and evaluated by a multidisciplinary team of medical oncologists, radiation oncologists, and otolaryngologists. Chemotherapy and surgery were offered at the discretion of the medical oncologist and evaluating surgeon. Concurrent chemotherapy regimens included cisplatin, carboplatin/paclitaxel, or cetuximab for most patients. Surgery consisted of maximal safe resection with or without reconstruction as appropriate. Patients were not considered for postoperative or adjuvant treatment if excisional biopsy alone was performed or if there was gross residual disease postsurgery.
Patients were simulated and immobilized with long thermoplastic masks. All patients underwent CT-based planning, as well as PET/CT when available for target delineation. PET fusion with the planning CT using rigid reconstruction was applied when PET/CT was used. IV contrast was used in the majority of patients except when contraindicated because of kidney function/allergies. Kilovoltage port films were used for localization. Radiation treatment volume was commonly a 10 mm clinical target volume expansion of the gross tumor volume, with a further expansion of 3 to 5 mm to create the PTV. No elective nodal coverage was done in the reirradiation setting. In the case of postoperative treatment, the operative bed was contoured and similar expansions to the clinical target volume and PTV were created.
Follow-up
Patients were evaluated for acute toxicity at 1 and at 4 weeks after retreatment. Patients were then seen every 3 months unless toxicity prompted more regular follow-up. Surveillance imaging was not carried out systematically. However, a majority of patients received a CT scan of the neck at 4 to 6 weeks and a PET/CT scan at 3 months after treatment, or when clinical findings suggesting recurrence or toxicity were identified. Otolaryngology and medical oncology also followed all patients when involved in their treatment.
At each follow-up with the multidisciplinary team, patients were assessed for treatment-related failure and toxicity. Local failure was defined as progressive disease within the treatment volume in both postoperative and definitive radiation patients. In the event imaging was used to document failure, the investigators individually reviewed the imaging and any available radiology reports. In the event of equivocal imaging findings, a tissue biopsy was used to differentiate between treatment-related changes and tumor recurrence. Regional failure was defined as lymph node recurrence either within the treatment volume or within other regionally defined lymph nodes of the cervical, pharyngeal, or supraclavicular area. Distant failure was defined as the presence of measurable disease at sites outside of the head and neck. Similar to local failures, biopsy was used to clarify equivocal imaging findings within regional or distant sites.
Toxicity
Acute and long-term toxicities were assessed retrospectively by reviewing the electronic medical record and graded according to the Common Terminology Criteria for Adverse Events version 4.0. Toxicities were considered acute if the onset was first noted within 30 days of treatment completion. Toxicities persistent from the initial course of treatment that remained unchanged in severity were not scored as retreatment-related toxicity.
Dosimetry
In order to evaluate radiation dose within standardized contours, head and neck structures of interest were systematically recontoured at the time of study and the composite radiation dose over the multiple treatment courses was analyzed. Notable structures of interest included carotid arteries, brainstem, spinal cord, mandible, esophagus, and pharyngeal constrictors. The carotid arteries were contoured from the skull base to the brachiocephalic artery (right carotid) or level of the manubrium (left carotid).
A composite plan refers to a treatment plan that takes into account total dose from all prior radiation courses. The composite dose was calculated as a direct summed value of the dose. Composite plans were generated at the time of retreatment by the treating radiation oncologist for 15 of the 21 patients who were analyzable for composite dosimetry. For these patients, composite plans were analyzed directly in MIM software version 5.6 planning program (MIM Software, Cleveland, OH). For the remaining 6 patients, individual radiation plans generated in the Pinnacle3 Planning System (Philips Radiation Oncology Systems, Fitchburg, WI) were imported into MIM and composite plans were generated retrospectively. For these 6 patients, the simulation scans for each course were fused without the use of deformable image registration and the individual dose files were then added together to generate the composite plan. Deformable registration was not used in these 6 patients to maintain consistency with the rigidly deformed plans available from the other 15 patients.
From the composite plans, composite dose volume histograms (DVHs) were generated, the maximum dose to 0.1 cc volume, the maximum dose to 1.0 cc volume, and mean dose to all structures were calculated. Additionally, the V70, V100. and V120 (volume of contoured structure receiving 70, 100, and 120 Gy. respectively) were extracted explicitly for the carotid arteries. These parameters were then described in relation to the observed radiotherapy-associated toxicities.
To observe trends in long-term toxicity with composite dose, plots were created representing minimum/maximum, inner quartiles, and median values for volume versus dose received in various key structures. These plots were derived from the individual patient DVHs for each structure of interest. For bilateral structures, such as the carotid arteries, left and right structures were treated as separate data points but were represented within the same plot. From these plots, numeric quantities, such as V70, V100, and V120 values, can be obtained for the other key structures.
Statistics
The Kaplan–Meier method was used to estimate time to event outcomes for OS, as well as local, regional, locoregional, and distant progression-free survival (PFS). The final day of treatment was calculated as time zero for time to event analysis. The impact of clinical/demographic (age, sex, second primary vs recurrence), and treatment (retreatment interval, dose, and use of concurrent chemotherapy) related factors on failure-free survival was investigated by testing the time to event strata using the log-rank statistic.
A univariate Cox proportional hazards analysis was also used to evaluate the influence of primary versus recurrence, and retreatment interval on PFS and OS, after assessing for proportional hazards assumptions. All statistical measures were performed in SAS software version 9.2 (SAS Institute, Cary, NC).
Composite DVHs for each structure were exported from MIM in tabular format with dose grouped in bin sizes of 100 cGy, whereas the volume remained as a continuous variable. The raw data, therefore, consisted of absolute volumes receiving at least 0 cGy, 100 cGy, or 200 cGy, etc, until the maximum dose for the structure was reached. The data was then imported into Wolfram Mathematica version 7.0 (Wolfram Research, Champaign, IL) and minimum, first quartile, median, third quartile, and maximum volumes were computed for each bin and plotted. The modified Wald method was used to determine the point estimate and 95% confidence intervals (CIs) for the probability of carotid blowout at set composite maximum doses within 6-month and 12-month follow-up intervals.
RESULTS
Patients
Patient demographics and tumor characteristics are summarized in Table 1. The median age at retreatment was 64 years (range, 27–92 years) with the majority of patients (68%) undergoing retreatment for local recurrences. Most patients (60%) had stage IVA/B primary cancer and most second primary cancers (63%) were stage IVA. The median treatment volume among all patients was 121 cc (range, 10–493 cc). Laryngeal (28%) and oral cavity (14%) cancers were the most common sites at initial presentation. Regional lymph node recurrence (20%) was the most common indication for retreatment, followed by local recurrences of oropharyngeal (16%) and laryngeal (16%) carcinoma. The majority of patients (68%) were ECOG 1 at the time of retreatment.
TABLE 1.
Patient and tumor characteristics.
| Patient characteristics | |
|---|---|
|
| |
| No. of patients | 50 |
| Age, years (range) | |
| Median age at initial treatment | 57 (26–91) |
| Median age at retreatment | 64 (27–92) |
| ECOG performance status | No. of patients (%) |
| 0 | 2 (4) |
| 1 | 34 (68) |
| 2 | 9 (18) |
| 3 | 5 (10) |
| Tumor characteristics | |
| Tumor location of initial disease | |
| Base of tongue | 3 (6) |
| Oral cavity | 7 (14) |
| Oropharynx | 5 (10) |
| Larynx | 14 (28) |
| Hypopharynx | 4 (8) |
| Nasopharynx | 5 (10) |
| Parotid gland | 3 (6) |
| Lymphoma | 2 (4) |
| Skin | 2 (4) |
| Unknown primary | 3 (6) |
| Tumor location of recurrent or second primary disease | |
| Base of tongue | 6 (12) |
| Oral cavity | 7 (14) |
| Oropharynx | 8 (16) |
| Larynx | 8 (16) |
| Hypopharynx | 3 (6) |
| Nasopharynx | 5 (10) |
| Parotid gland | 2 (4) |
| Local nodes | 10 (20) |
| Second disease type | |
| Local recurrence | 34 (68) |
| Second primary | 16 (32) |
| Stage for initial disease | |
| I | 7 (14) |
| II | 9 (18) |
| III | 4 (8) |
| IVA | 27 (54) |
| IVB | 3 (6) |
| Stage for second primary tumors* | |
| I | 0 |
| II | 5 (31) |
| III | 1 (6) |
| IVA | 10 (63) |
| IVB | 0 |
Abbreviation: ECOG, Eastern Cooperative Oncology Group.
Stage for the 16 second primary tumors. Recurrences were not restaged.
Treatment
Treatment details are summarized in Table 2. The median first course total radiation dose was 64 Gy (range, 37–70.2 Gy) with a median fraction dose of 2 Gy. Median total dose during reirradiation was 60 Gy (range, 30–72.6 Gy) with a median fraction dose of 2 Gy. Four patients were retreated with bid radiotherapy, 1 patient was treated with 3 Gy per fraction with definitive intent using hypofractionation, and the rest were treated with conventional fractionation. Seventy-two percent of patients were retreated with IMRT (Step and Shoot, 8–9 field IMRT), and 28% with traditional opposed lateral fields using mainly 3D-conformal radiotherapy. Median time between primary and retreatment courses of radiation was 28 months (range, 6–356 months). After excluding the 2 patients who died during re-treatment, all but 5 patients completed the entire prescribed course of radiation. For the 5 patients who did not complete the entire course, all completed >75% of their prescribed radiation dose before stopping because of acute toxicities.
TABLE 2.
Treatment details.
| Treatment details | |
|---|---|
|
| |
| Median interval between radiation treatments (range) | 28 mo (6–356 mo) |
| Data for first treatment course | |
| Radiation treatment | Dose (range) |
| Median radiation dose | 64 Gy (37–70.2 Gy) |
| Median dose per fraction | 2 Gy (1.8–2.8 Gy) |
| No. of patients (%) | |
| Surgical treatment | 23 (46) |
| Concurrent chemotherapy treatment | 20 (40) |
| Cisplatin | 9 (45) |
| Carboplatin/paclitaxel | 2 (10) |
| Cetuximab | 0 |
| Other | 9 (45) |
| Data for re-treatment course | |
| Radiation treatment | Dose (range) |
| Median radiation dose | 60 Gy (37–72.6 Gy) |
| Median dose per fraction | 2 Gy (1.1–3.0 Gy) |
| No. of patients (%) | |
| Surgical treatment | 24 (48) |
| Concurrent chemotherapy | 41 (82) |
| Cisplatin | 2 (5) |
| Carboplatin/paclitaxel | 22 (54) |
| Cetuximab | 6 (15) |
| Other | 11 (27) |
Forty percent of patients underwent concurrent chemotherapy at initial treatment, whereas 82% received chemotherapy at re-treatment. The most common concurrent chemotherapy used during initial treatment was cisplatin (45%), either every 3 weeks or weekly. Carboplatin/paclitaxel combination chemotherapy was the most common therapy during re-treatment (54%). Just under half of all patients underwent surgery before initial treatment and a similar number underwent surgery before re-treatment.
Acute and late toxicities
Re-treatment-related toxicities are summarized in Table 3. Acute toxicities documented with reirradiation treatment were not different or more severe than toxicities documented with first round RT. The majority of reirradiation patients experienced grade 2 acute toxicity (40%). Forty-two percent of patients experienced grade 3 or higher acute toxicities. Two patients were gastric tube (G-tube) dependent after therapy (grade 4 toxicity). Two patients died at home of unknown causes midway through their radiation course. One patient died at fraction 20 of a planned 30 fractions, and the second patient died at fraction 7 of a planned 30 fractions, both receiving 2 Gy per fraction.
TABLE 3.
Composite dosimetry and re-treatment toxicity.
| Composite dosimetry and re-treatment toxicity | ||
|---|---|---|
|
| ||
| Composite dosimetry | ||
| No. of patients eligible for dosimetric evaluation | 21 | |
| Median dose or volume (range) | ||
| Retreatment PTV | 121 cc (10–439 cc) | |
| Composite maximum dose | 128 Gy (81–187 Gy) | |
| Brainstem 0.1 cc maximum dose | 46 Gy (0–83 Gy) | |
| Spinal cord 0.1 cc maximum dose | 50 Gy (14–80 Gy) | |
| Larynx mean dose | 44 Gy (5–120 Gy) | |
| Pharyngeal constrictor mean dose | ||
| Superior | 68 Gy (0–120 Gy) | |
| Middle | 73 Gy (1–121 Gy) | |
| Inferior | 61 Gy (6–149 Gy) | |
| Parotid gland mean dose | 37.5 Gy (0.5–73 Gy) | |
| Mandible 0.1 cc maximum dose | 101 Gy (1–136 Gy) | |
| Carotid arteries | ||
| Mean dose | 60 Gy (3–130 Gy) | |
| 0.1 cc maximum dose | 106 Gy (22–160 Gy) | |
| 1.0 cc maximum dose | 99 Gy (12–137 Gy) | |
| V70 | 2 cc (0–14 cc) | |
| V100 | 1 cc (0–7 cc) | |
| V120 | 0 cc (0–4 cc) | |
| Acute toxicity* | All patients (50) | Patients in dosimetric analysis (21) |
| No. of patients (%) | No. of patients (%) | |
| Grade 1 | 9 (18) | 3 (14) |
| Grade 2 | 20 (40) | 7 (33) |
| Grade 3 | 17 (34) | 9 (43) |
| Grade 4 | 2 (4) | 1 (5) |
| Grade 5 | 2 (4) | 1 (5) |
| Late toxicity | ||
| Grade 1 | 10 (18) | 3 (14) |
| Grade 2 | 6 (12) | 5 (24) |
| Grade 3 | 14 (28) | 3 (14) |
| Grade 4 | 2 (4) | 2 (10) |
| Grade 5 (carotid blowout) | 1 (2) | 1 (5) |
Abbreviation: PTV, planning target volume.
Acute toxicity defined as occurring within 30 days after completing radiation treatment. Toxicity graded by Common Terminology Criteria for Adverse Events version 4.0 criteria.
Late toxicities were noted in 33 patients with a median onset of 4 months post re-treatment. Of these patients, grade 3 toxicity was observed in 14 patients (42%). The most common late toxicity was new or worsened trismus in 5 patients (15%) and G-tube dependence in 5 patients (15%), followed by esophageal strictures requiring dilation in 4 patients (12%). One patient experienced grade 4 toxicity with severe dysphagia requiring stenting and a temporary Dobhoff tube placement followed by G-tube placement and dependence.
Carotid blowout and death occurred in 1 patient 6 months after completing radiation treatment. This patient had an initial stage IVA supraglottic laryngeal cancer treated with IMRT to 70 Gy in 2 Gy fractions with concurrent cisplatin chemotherapy. He did not undergo surgical resection or neck dissection at initial treatment. He experienced a supraglottic recurrence 14 months after completing radiation treatment and subsequently underwent total laryngectomy, partial glossectomy, and bilateral selective levels 2 to 4 neck dissection. Concurrent reirradiation and chemotherapy with weekly carboplatin/paclitaxel was administered; however, this patient received only 52 Gy in 2 Gy fractions via IMRT of a total prescribed 60 Gy because of the development of a cutaneous fistula. Of note, this tumor did encase the carotid artery and tumor-related injury cannot be ruled out as a cause of this complication.
Disease control and overall survival
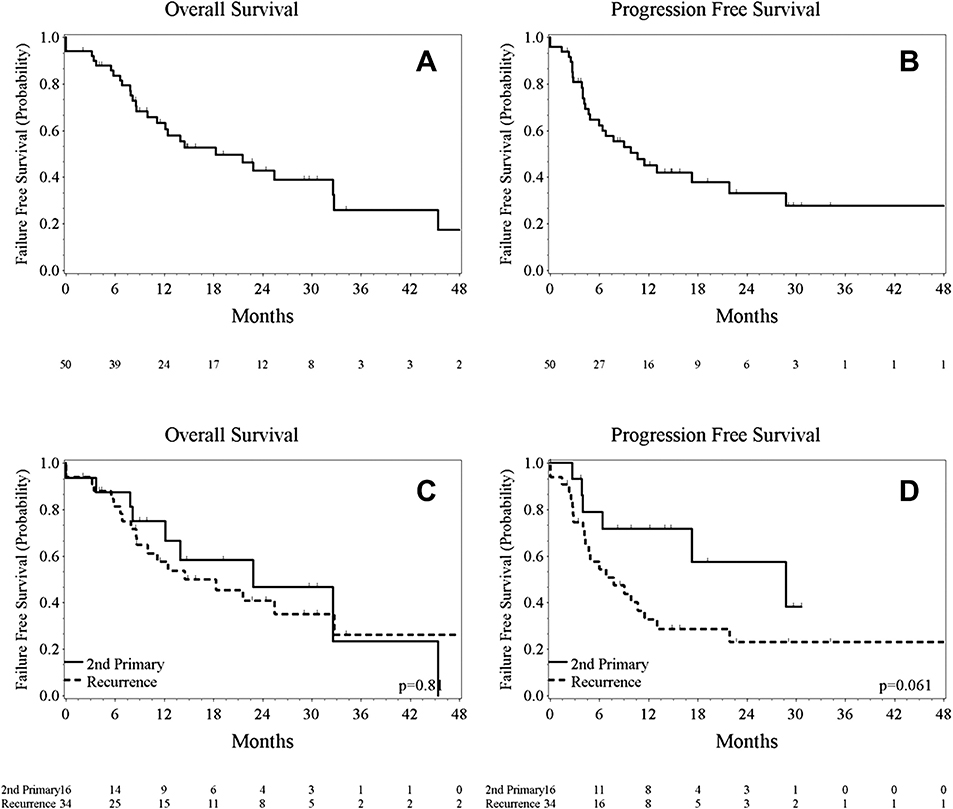
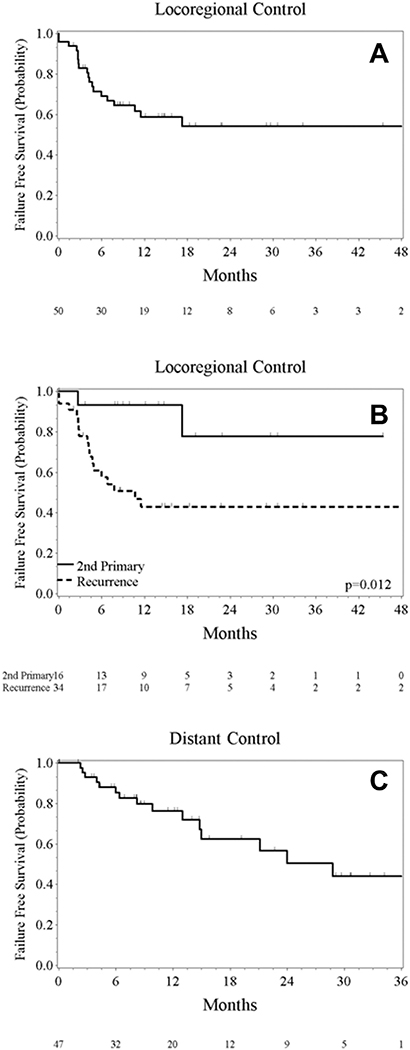
OS and PFS are reported in Kaplan–Meier curves in Figure 1. The median PFS was 11 months (95% CI = 6–29 months) with a 1-year PFS rate of 47%. PFS favored second primary cancers with a median PFS of 28 versus 9 months (p = .10). The re-treatment interval was not found to alter the hazard for diminished PFS (hazard ratio [HR]5 0.99; p = .06). The median OS was 18 months (95% CI = 10–32 months) including 3 patients who died during or within 30 days of re-treatment. Neither second primary cancers (HR5 0.91; p = .81) nor retreatment interval (HR5 1.0; p = .85) was found to be associated with prolonged survival. The 1-year local control, regional control, and locoregional control was 58% (95% CI = 42% to 71%), 81% (95% CI = 65% to 91%), and 52% (95% CI = 36% to 66%), respectively. Among 47 nonmetastatic patients, 14 experienced distant failures, with a 1-year distant control of 75% (95% CI = 42% to 71%). Plots for locoregional control for all patients, stratified by second primary versus recurrences and distant control in nonmetastatic patients are illustrated in Figure 2.
FIGURE 1.
Kaplan–Meier estimates of overall survival for all patients (A), stratified by second primary versus recurrences (C), and progression-free survival for all patients (B), and stratified by second primary cancers versus recurrences (D).
FIGURE 2.
Kaplan–Meier estimates of locoregional control for all patients (A), stratified by second primary versus recurrences (B), and distant failure-free survival (C).
Dosimetric evaluation to organs at risk
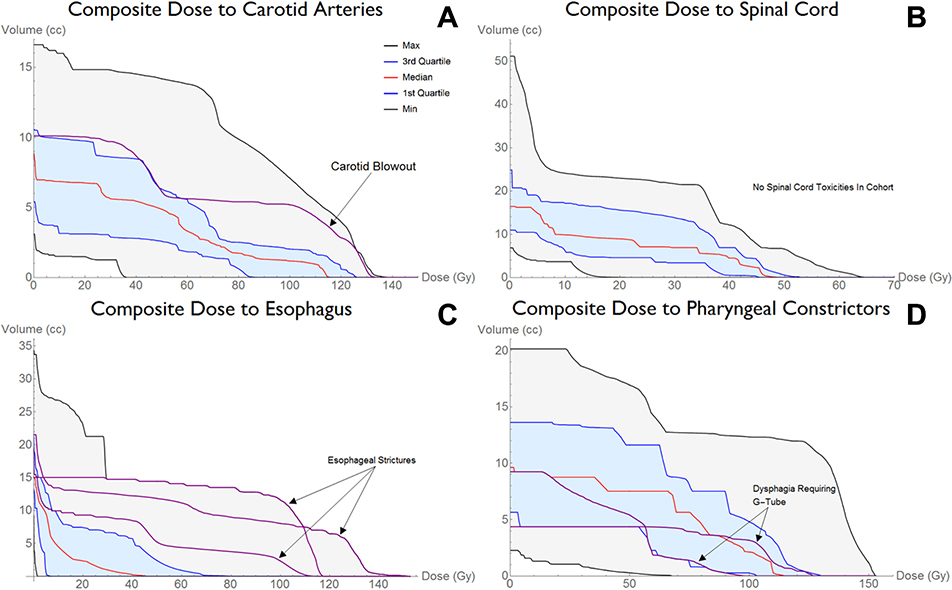
From the composite plans, the median maximum point dose (defined as 0.1 cc volume) received was 128 Gy (range. 81–187 Gy). Dosimetric plots for key structures are displayed in Figure 3. Notably, patients with late toxicities tended to have dose in the third quartile or higher compared with all other patients for the corresponding structures. Dose to the carotid arteries was near to or above the upper border of the third quartile for the patient who experienced a carotid blowout, indicating a higher cumulative dose. Similarly, all 3 patients with esophageal strictures requiring dilation demonstrated doses to the esophagus above the third quartile compared with others in the cohort. No clear trend was observed using dose to the pharyngeal constrictor muscles in predicting dysphagia requiring G-tube dependence.
FIGURE 3.
Dosimetric plots for key structures. The bottom and top black lines represent the minimum and maximum values. The blue lines represent the first and third quartiles. The red line represents the median value. Note that the patient with the carotid blowout event (purple line in panel A) had a composite dose that fell above the third quartile for most of the dose range, and approached the maximum for volume at the highest doses. Any patient with grade 3 or higher toxicity has their dose-volume histogram overlaid on top of the corresponding structure. The anatomic pharyngeal constrictor group (superior, middle, or inferior) receiving the highest total dose for each patient was selected for analysis. G-tube, gastric tube.
Although our goal was to establish dose constraints using composite dosimetry, the small number of events limited our ability to define a specific threshold above which toxicity could be accurately predicted. The major limiting factor in the patients unable to be included in the dosimetric analysis was lack of archived composite radiation plans combined with lack of access to their primary course radiation plans that would be required to construct a composite plan retrospectively. Despite the limitations of a small sample size, we were able to describe a point estimate and 95% CI for the probability of carotid blowout at 6 and 12 months relative to the maximum composite dose to the carotids through the use of the modified Wald chi-square method. The chances of developing a carotid blowout at a maximum dose of <120 Gy and >120 Gy were 4.6% (95% CI = 0% to 8.2%) versus 13.3% (95% CI = 0% to 35.4%) at 6 months and 5.9% (95% CI = 0% to 18%) versus 25% (95% CI = 1.1% to 58.2%) at 12 months, respectively. We view these analyses as a necessity in future studies trying to limit toxicity in the re-treatment setting as these descriptive analyses will contribute to our general understanding of organs at risk tolerance doses.
DISCUSSION
Reirradiation for locally recurrent or second primary HNSCCs is a treatment option that has seen increasing acceptance over the past decade. Prior approaches have been limited to salvage surgical resection or palliative chemotherapy for unresectable patients. Surgical resection has demonstrated improved 5-year OS rates compared to chemotherapy alone, however, resection remains limited to only a minority of patients.16 Major obstacles preventing surgical candidacy include advanced tumor stage, nonfavorable tumor location, and poor patient functional status. For the majority of patients not qualifying for surgery, palliative chemotherapy has remained the traditional treatment modality. However, even with multiagent chemotherapy regimens, the OS at 2 to 3 years remains poor.2–4,6
The first prospective multi-institutional trial examining reirradiation with concurrent chemotherapy in this patient population was conducted in Radiation Therapy Oncology Group 9610. Patients with either locally recurrent HNSCC or second primary HNSCC within the prior radiation field were treated for their second malignancy with definitive 5-fluorouracil/hydroxyurea chemotherapy and reirradiation using 1.5 Gy bid to a total of 60 Gy. Toxicities encountered during the acute period (within 90 days) included 2 deaths from carotid blowouts and 4 deaths from hematologic events (neutropenia). Forty-nine percent of patients experienced grade 3 or greater nonhematologic toxicity. Of all living patients, 22% experienced grade 3 or higher late toxicities. Median OS was 8.5 months.17
More recently, results from a phase III trial were published in which 130 patients with recurrent or second primary HNSCC were randomized to either surgical resection alone (wait and see arm) or surgery followed by accelerated hyperfractionated radiation at 1.5 Gy bid and 5-fluorouracil/hydroxyurea chemotherapy (RT arm).13 Significant differences were seen in local control and PFS between the RT and wait and see arm arms with HRs of 2.73 and 1.68, respectively. Despite the advantages in disease control, this trial did not find a significant difference (p = .5) in OS between the 2 arms, although fewer patients in the RT arm died from local recurrence compared with those in the wait and see arm. The improved disease control was not without cost, as more patients died of treatment-related toxicity, distant metastases, and new primary disease in the RT arm compared to the wait and see arm.
In the current analysis, we examined a cohort of patients undergoing repeat postoperative or definitive reirradiation for HNSCC. Patients in our study experienced favorable local control and PFS compared with rates reported in current literature of patients undergoing surgical resection alone13 or with combination chemotherapy regimens.18–20
One of the major limitations of head and neck irradiation stems from both disabling late toxicities, such as trismus and dysphagia, as well as fatal complications, such as carotid blowout. In our study, we utilized composite dosimetry to describe toxicity as it relates to cumulative dose. Although we did not encounter enough late toxicity events to firmly establish a dose constraint, we did note patients with toxicity events had composite DVHs that fell at or above the third quartile when compared with all other analyzed patients. We did observe 1 carotid blowout event 6 months from their reirradiation in our cohort of 50 patients. This results in a calculated incidence of carotid blowout of 2%, and is consistent with the estimated crude rate of carotid blowout from a meta-analysis by McDonald et al.21 Unfortunately, the cause of death is unknown in the 2 patients who died during their retreatment course. As the onset of carotid blowout has been found to have a range spanning from on-treatment to several years after treatment, carotid blowout as a cause of death cannot be completely ruled out. Extensive review of electronic medical records as well as review of the social security death registry could not further elucidate the cause of death in those 2 patients, however, electronic medical record review did not reveal any vascular complications, such as cutaneous fistulas, as were noted in the patient who did have the carotid blowout event.
CONCLUSION
Further clinical investigation is required to identify a dose threshold for toxicity events in the reirradiation setting. However, the method of composite dosimetric analysis described in this study may serve as a guide for future investigations exploring reirradiation dose to head and neck structures. The prospective Radiation Therapy Oncology Group studies (9610 and 9911) and the majority of the retrospective data discuss only limiting the spinal cord dose to either a composite value of <50 Gy, or minimizing the dose from the retreatment to <10 Gy. With the increasing availability of IMRT and inverse planning, dose constraints to traditionally contoured head and neck structures will likely increase the therapeutic ratio as we better define the risks of these toxicities within the reirradiated population. Furthermore, with the concern for carotid blowout, contouring these structures and constraining them to a reasonable level may help limit the risk of this catastrophic event.
REFERENCES
- 1.Taussky D, Dulguerov P, Allal AS. Salvage surgery after radical accelerated radiotherapy with concomitant boost technique for head and neck carcinomas. Head Neck 2005;27:182–186. [DOI] [PubMed] [Google Scholar]
- 2.Gibson MK, Li Y, Murphy B, et al. Randomized phase III evaluation of cisplatin plus fluorouracil versus cisplatin plus paclitaxel in advanced head and neck cancer (E1395): an intergroup trial of the Eastern Cooperative Oncology Group. J Clin Oncol 2005;23:3562–3567. [DOI] [PubMed] [Google Scholar]
- 3.Forastiere AA, Leong T, Rowinsky E, et al. Phase III comparison of high-dose paclitaxel + cisplatin + granulocyte colony-stimulating factor versus low-dose paclitaxel + cisplatin in advanced head and neck cancer: Eastern Cooperative Oncology Group Study E1393. J Clin Oncol 2001;19:1088–1095. [DOI] [PubMed] [Google Scholar]
- 4.Wong SJ, Machtay M, Li Y. Locally recurrent, previously irradiated head and neck cancer: concurrent re-irradiation and chemotherapy, or chemotherapy alone? J Clin Oncol 2006;24:2653–2658. [DOI] [PubMed] [Google Scholar]
- 5.Vokes EE, Schilsky RL, Weichselbaum RR, et al. Cisplatin, 5-fluorouracil, and high-dose oral leucovorin for advanced head and neck cancer. Cancer 1989;63(6 Suppl):1048–1053. [DOI] [PubMed] [Google Scholar]
- 6.Forastiere AA, Shank D, Neuberg D, Taylor SG IV, DeConti RC, Adams G. Final report of a phase II evaluation of paclitaxel in patients with advanced squamous cell carcinoma of the head and neck: an Eastern Cooperative Oncology Group trial (PA390). Cancer 1998;82:2270–2274. [PubMed] [Google Scholar]
- 7.Spencer SA, Harris J, Wheeler RH, et al. Final report of RTOG 9610, a multi-institutional trial of reirradiation and chemotherapy for unresectable recurrent squamous cell carcinoma of the head and neck. Head Neck 2008; 30:281–288. [DOI] [PubMed] [Google Scholar]
- 8.Langer CJ, Harris J, Horwitz EM, et al. Phase II study of low-dose paclitaxel and cisplatin in combination with split-course concomitant twicedaily reirradiation in recurrent squamous cell carcinoma of the head and neck: results of Radiation Therapy Oncology Group Protocol 9911. J Clin Oncol 2007;25:4800–4805. [DOI] [PubMed] [Google Scholar]
- 9.Biagioli MC, Harvey M, Roman E, et al. Intensity-modulated radiotherapy with concurrent chemotherapy for previously irradiated, recurrent head and neck cancer. Int J Radiat Oncol Biol Phys 2007;69:1067–1073. [DOI] [PubMed] [Google Scholar]
- 10.Sulman EP, Schwartz DL, Le TT, et al. IMRT reirradiation of head and neck cancer-disease control and morbidity outcomes. Int J Radiat Oncol Biol Phys 2009;73:399–409. [DOI] [PubMed] [Google Scholar]
- 11.Sher DJ, Haddad RI, Norris CM Jr, et al. Efficacy and toxicity of reirradiation using intensity-modulated radiotherapy for recurrent or second primary head and neck cancer. Cancer 2010;116:4761–4768. [DOI] [PubMed] [Google Scholar]
- 12.Zwicker F, Roeder F, Hauswald H, et al. Reirradiation with intensity-modulated radiotherapy in recurrent head and neck cancer. Head Neck 2011;33:1695–1702. [DOI] [PubMed] [Google Scholar]
- 13.Janot F, de Raucourt D, Benhamou E, et al. Randomized trial of postoperative reirradiation combined with chemotherapy after salvage surgery compared with salvage surgery alone in head and neck carcinoma. J Clin Oncol 2008;26:5518–5523. [DOI] [PubMed] [Google Scholar]
- 14.Kasperts N, Slotman BJ, Leemans CR, de Bree R, Doornaert P, Langendijk JA. Results of postoperative reirradiation for recurrent or second primary head and neck carcinoma. Cancer 2006;106:1536–1547. [DOI] [PubMed] [Google Scholar]
- 15.Bernier J, Cooper JS, Pajak TF, et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (#9501). Head Neck 2005;27:843–850. [DOI] [PubMed] [Google Scholar]
- 16.Taussky D, Rufibach K, Huguenin P, Allal AS. Risk factors for developing a second upper aerodigestive cancer after radiotherapy with or without chemotherapy in patients with head-and-neck cancers: an exploratory outcomes analysis. Int J Radiat Oncol Biol Phys 2005;62:684–689. [DOI] [PubMed] [Google Scholar]
- 17.Spencer SA, Harris J, Wheeler RH, et al. RTOG 96–10: reirradiation with concurrent hydroxyurea and 5-fluorouracil in patients with squamous cell cancer of the head and neck. Int J Radiat Oncol Biol Phys 2001;51:1299–1304. [DOI] [PubMed] [Google Scholar]
- 18.Salama JK, Vokes EE, Chmura SJ, et al. Long-term outcome of concurrent chemotherapy and reirradiation for recurrent and second primary head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys 2006;64:382–391. [DOI] [PubMed] [Google Scholar]
- 19.Lee N, Chan K, Bekelman JE, et al. Salvage re-irradiation for recurrent head and neck cancer. Int J Radiat Oncol Biol Phys 2007;68:731–740. [DOI] [PubMed] [Google Scholar]
- 20.Kharofa J, Choong N, Wang D, et al. Continuous-course reirradiation with concurrent carboplatin and paclitaxel for locally recurrent, nonmetastatic squamous cell carcinoma of the head-and-neck. Int J Radiat Oncol Biol Phys 2012;83:690–695. [DOI] [PubMed] [Google Scholar]
- 21.McDonald MW, Moore MG, Johnstone PA. Risk of carotid blowout after reirradiation of the head and neck: a systematic review. Int J Radiat Oncol Biol Phys 2012;82:1083–1089. [DOI] [PubMed] [Google Scholar]