Abstract
Objectives
This study is to evaluate the efficacy of participatory ergonomic (PE) intervention on musculoskeletal disorders (MSDs) and work ability among young dental professionals in China.
Methods
A cluster randomized controlled trail was conducted during 2015–2016. Twenty‐nine departments from five hospitals in the South of China were randomized into intervention (14 departments) and control (15 departments), with individuals of 125 and 138 dental professionals, respectively. Main participatory ergonomic interventions involved work posture, repetitive motions, tool usage, work break relaxation and work time re‐arrangement with total 235 ergonomic changes in the trail. Individual ergonomic risk exposure was assessed by investigator's observation using quick exposure check (QEC). Work ability index (WAI) and MSDs were collected by questionnaires at baseline, and every 3 months during the 1‐year follow‐up.
Results
Follow‐up rate was 91% and 96% for the intervention and control group, respectively. Significant reductions in ergonomic risk exposure and MSD prevalence on six anatomic sites were found in the PE group during the different follow‐up stages. WAI scores improved by 1.1 (95% CI 0.43, 1.89) after the 9‐month intervention. Compared to the control, the PE participants significantly reduced MSDs on neck (OR = 2.93, 95% CI: 1.25, 4.03) and wrists/hands (OR = 2.33, 95% CI: 1.08, 4.21), marginally increased WAI scores by 0.53 (95% CI: −0.02, 1.56) due to the interventions.
Conclusion
PE intervention is effective in reducing ergonomic risk exposure and MSDs on neck and wrists/hands among young dental professionals. PE ought to be offered in the early dental career for preventing MSDs.
Keywords: dental professionals, musculoskeletal disorders, participatory ergonomics, randomized control trial, work ability
1. INTRODUCTION
Dentistry is a profession that needs both high technical skills and physical ability. Occupational health in dentistry has been drawing more and more attention in China. A number of previous studies worldwide including in China have reported a high prevalence of musculoskeletal disorders (MSDs) among dental professionals because of heavy ergonomic loading, such as awkward position, over flexed neck, rotated wrists, and extended static posture. 1 , 2 , 3 , 4 It is estimated that the prevalence of general musculoskeletal pain ranges between 64% and 93%. 5 Even worse, MSD symptoms often started as early as the student or internship phases. 6 Musculoskeletal pain has been identified as early as during their entry‐level dental education. Dental professionals are prone to suffer from MSDs, and result in either an early retirement, losing workdays, or disability. 7 A cross‐sectional study in China showed high ergonomic risk exposure was significantly related to reduced work ability among young dental professionals. 8
Ergonomic interventions particularly participatory ergonomics (PE) have been proved to be a promising approach to reduce ergonomic risk factors or MSDs. A systematic review provided partial to moderate evidence that PE interventions have a positive impact on musculoskeletal symptoms, reducing injuries and workers’ compensation claims, and a reduction in lost days from work or sickness absence. 9 However, inconsistent results had been reported and more high‐quality studies need to confirm. A RCT study showed that the participatory intervention did not reduce perceived physical workload and no evidence was found for the efficacy of the intervention in preventing musculoskeletal disorders among kitchen workers. 10 Our recent study revealed that ergonomic risk exposure was significantly associated with work ability among dental professionals. 8 It is not difficult to understand that the presence of MSDs may affect not only the physical function but also mental capacities, even future work ability prediction. We supposed that MSDs were the primary outcome due to ergonomic risk exposure and then result in decreasing work ability. However, whether PE could improve work ability is still controversy. Some previous researches demonstrated the presence of MSD affected work ability, 11 , 12 while other reported there was no significant relationship between MSDs and work ability. 13 Meanwhile, previous studies were cross‐sectional designs which limited the causal inference due to time sequence. For now, there have been very few reports about the efficacy of PE intervention on ergonomic risk exposure, MSDs, and work ability among young dental professionals in their early career.
Therefore, in this study we carried out a cluster‐randomized controlled trail among Chinese young dental professionals, to examine the efficacy of PE intervention on their ergonomic risk exposure, MSDs, and work ability during 1‐year follow‐up.
2. METHODS
2.1. Study design
We designed a single‐blind, randomized controlled trial among young dental professionals in the South of China. The participants were allocated to a 12‐month intervention period, and paralleled as signed to receive the participatory intervention or normal ergonomic education as control group. The study duration was from November 2015 to October 2016.
2.2. Ethics
The study was approved by the committee of the Chinese University of Hong Kong and Putian University on biomedical research ethics. The trial was registered as “Ergonomic intervention for prevention MSDs—dental professional” at Putian University. All participants were informed about the purpose and content of the study and gave their written informed consent to participate in the study. All intervention measurements conformed to the Declaration of Helsinki.
2.3. Participant recruitment and following up
Figure 1 shows the complete flow of participants in this trial. We contacted 33 departments in five stomatological hospitals and 29 departments approved to participate the trail. Then, 14 departments were randomized in intervention group with 125 dental professionals and 15 were in control group with 138 professionals. To reduce the contamination bias, we use the cluster sample method to recruit participants. All professionals within the participating departments were allowed to participate in either the intervention or control group. The baseline questionnaire was sent to the subjects, of 105 (84%) subjects responded in the intervention group, and 113 (82%) responded in the control group. Exclusion of age more than 35 years and/or being pregnancy, finally 200 participants met the inclusion criteria, with 97 included in the intervention group and 103 in the control group. After 12 months, 88 participants (90.7%) in the intervention and 99 (96.1%) in the control were successfully followed up.
FIGURE 1.
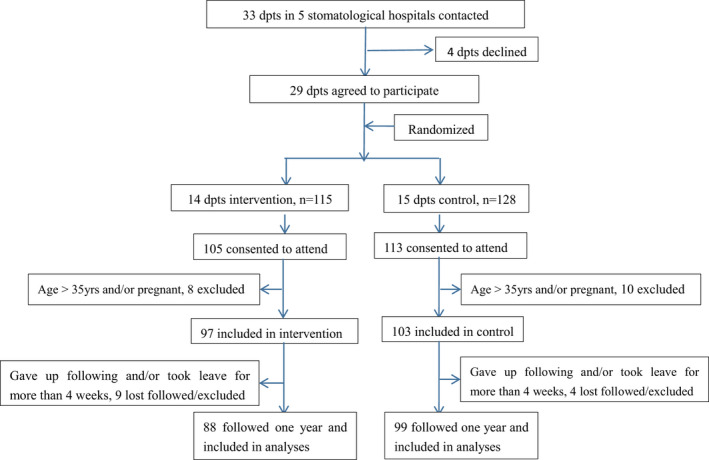
Overview of participants recruitment in the different phases of the trial
2.4. Control group
Before the project started, both intervention and control departments were requested to take a 45‐min ergonomic lesson about basic knowledge on MSD prevention and control. The lesson was used as a sham intervention and can be considered as an ethic strategy to prevent MSDs among the control departments.
2.5. Participatory ergonomic intervention
Each intervention department formed an intervention working group, in which one department manager, one employee representative, and a trained ergonomist were group members. Under the guidance of a trained ergonomist, the working group followed the steps of the PE program during a 2‐h meeting. All decisions during the meeting were made by the working group members and were based on consensus. All working group meetings were focused on the prevention of MSDs on neck, shoulders/arms, back, and hands/wrists in the department. By following the steps of the PE program, the working group observed their work field, evaluated, and prioritized the main risk factors for MSDs. Then the working group identified, evaluated, and proposed the ergonomic measures. Those measures focused on work posture adjustment, repetitive motions reduction, proper tool usage, work break relaxation, and work time re‐arrangement. All information about the prioritized risk factors and ergonomic measures were written down in an implementation plan. To enhance the implementation, the trained ergonomist in the working group visited working sites three times every week, and evaluated the intervention measures or modify the intervention process according to the participants’ responses for the intervention measures. Each time visit lasted from half an hour to 2 h, depending on the PE subjects’ understanding and acceptance for the ergonomic changes. The visiting frequency and duration time were reduced until the PE subjects implemented those ergonomic changes correctly and fixed their behaviors habitually based on the working group agreement. The rationale for this intervention was to ensure that participants were sufficiently informed about the ergonomic hazards to which they may be exposed to and thus were able to participate actively in their own protection. During the 1‐year intervention, total 235 ergonomic changes in their daily dental practices were made, including work posture, repetitive motions, tool usage, work break relaxation, and work time re‐arrangement in the intervention group.
2.6. Outcome measures
We assessed ergonomic risk exposure, MSD symptoms, and WAI by means of observations and questionnaires at baseline, 3‐month, 6‐month, and 12‐month during the 1‐year follow‐up. We set MSD symptom as the primary outcome and WAI as the secondary outcome.
We applied Quick Exposure Check (QEC) to assess participants’ ergonomic exposure. 14 The QEC has been validated in the Chinese population and the intra‐ and inter‐raters reliability were also examined to be reliable. 15 , 16 Three interviewers who had been trained with QEC completed the field observations and interviews during participants’ daily practices. Four body parts of participants with six anatomic sites were observed and assessed for the calculation of ergonomic exposure scores and exposure level based on the algorithm, including neck, shoulders/arms, back, and wrists/hands. 14 We calculated the total ergonomic exposure scores by adding four body part score and stress, vibrations, and work pace score as well. Total exposure scores were divided into four levels based on quartile. Above 50% exposure level was considered as high exposure level.
WAI was assessed by face to face using the WAI questionnaire. WAI has been confirmed to be a simple and reliable tool to apply in work ability assessment. 17 It also was validated in occupational health context and applications in China. 18 Briefly, the WAI questionnaire contains seven aspects in assessing work ability, including current work ability compared to the lifetime best, work ability in relation to the demands of the job, number of current diseases diagnosed by physician, estimated work impairment due to diseases, sick leave during the past year, own prognosis of work ability 2 years from now and mental resources. WAI score ranges from 7 to 49 and further classified into four levels, for example, poor (7–27), moderate (28–37), good (38–43), and excellent (44–49).
We used a modified version of Chinese Nordic Musculoskeletal Questionnaire (CNMQ) to investigate MSD symptoms. CNMQ has been proved to be a reliable and valid tool in screening MSDs in Chinese background. 19 The participants were asked about the presence and intensity of any pain, ache, burning, stiffness, numbness, or tingling in the four body regions (neck, shoulders/arms, low back, and wrists/hands) in daily dental practices. Positive MSDs were defined as having musculoskeletal complaints/pains on the four body parts during the last 3 months.
Other than QEC and WAI information collection, demographics, daily physical exercises time, height/weight, smoking, drinking habits, and past medical history were also collected in the baseline assessment. The intervention group received the PE intervention and follow‐up assessments were performed on the 3‐month, 6‐month, and 12‐month, respectively. The control group did not participate in the PE program throughout the study time.
2.7. Sample size
A priori power calculation based on MSD’s pain symptom revealed that 64 participants in each group were needed to achieve 95% statistical power and a standard deviation of 1.5, while a minimal relevant pre‐to‐post difference of pain intensity of 1 was sufficient to test the null‐hypothesis of equality (α = 0.05). 20 We estimated around 10% drop‐out during 1‐year follow‐up period and an inflation factor 1.2 for the clustered RCT, 21 the sample size for each group needs 85. Total 97 participants in the intervention and 103 in the control in this study met the requirement.
2.8. Statistical analysis
All analyses were performed according to the intention‐to‐treat principle (ITT), in which all randomized participants are included in the statistical analyses. 22 Data analyses first focused on the comparisons of the changes in ergonomic risk exposure, MSDs, and WAI between the intervention and control group. All analyses were based on parametric statistical methods due that the data distribution for the two groups was almost normal. To assess the randomization, descriptive statistics including t‐test, chi‐square test, and ANOVA were used to compare the baseline characteristics between the two groups. To adjust the potential confounders, then multivariable analysis was performed using SPSS 21.0 (SPSS Inc). MSD change from the symptom to relieved or no symptom was defined positive dependable variable in the logistic model. WAI improvement calculated from each stage (3‐, 6‐, 9‐, 12‐month) WAI scores minus baseline WAI scores was defined as a dependable variable in the linear regression model. Logistic mixed models were applied to study the intervention effects on MSD prevalence (Odds Ratio, OR). Linear mixed models were used to study the intervention effects on WAI. For all analyses, a two‐tailed significance level of P < .05 was considered statistically significant.
3. RESULTS
Table 1 presents the baseline characteristics of the participants. At baseline, there is no significant difference between the intervention and control group either in potential confounders (including job title, gender, age, educational level, BMI, smoking and drinking habits, physical exercise times) or in the outcome (WAI).
TABLE 1.
Baseline characteristics between intervention and control group
| Intervention group (n = 88) | Control group (n = 99) | P value | |||||
|---|---|---|---|---|---|---|---|
| N | % | Mean (SD) | N | % | Mean (SD) | ||
| Job title | 0.331 | ||||||
| Dentists | 40 | 45.5 | 49 | 49.5 | |||
| Dental nurse | 29 | 32.9 | 31 | 31.3 | |||
| Assistants | 19 | 21.6 | 19 | 19.2 | |||
| Gender | 0.322 | ||||||
| Male | 31 | 35.2 | 31 | 31.3 | |||
| Female | 57 | 64.8 | 68 | 68.7 | |||
| Age (yrs) | 27.12 (5.33) | 28.25 (6.04) | 0.420 | ||||
| Education | 0.663 | ||||||
| High school | 4 | 4.5 | 6 | 6.1 | |||
| College | 51 | 58.0 | 61 | 61.6 | |||
| Graduate | 33 | 37.5 | 32 | 32.3 | |||
| BMI | 21.45 (3.71) | 20.89 (3.58) | 0.531 | ||||
| Smoking | 4 | 4.5 | 4 | 4.0 | 0.865 | ||
| Drinking | 10 | 11.4 | 15 | 15.2 | 0.577 | ||
| Physical exercise time per day (min), n (%) | 0.395 | ||||||
| <30 | 50 | 56.8 | 60 | 60.6 | |||
| 30–60 | 30 | 34.1 | 32 | 32.3 | |||
| >60 | 8 | 9.1 | 7 | 7.1 | |||
| WAI | 39. 1 (3.5) | 39.2 (3.6) | 0.376 | ||||
| Poor | 2 | 2.3 | 2 | 2.0 | 0.285 | ||
| Moderate | 25 | 28.4 | 29 | 29.3 | |||
| Good | 35 | 39.8 | 36 | 36.4 | |||
| Excellent | 26 | 29.5 | 32 | 32.3 | |||
Abbreviations: BMI, body mass index; SD, standard deviation; WAI, work ability index.
Table 2 summarizes the total ergonomic changes during the 1‐year PE intervention. The most changes occurred in the neck and wrists/hands part, accounting for 20% and 15%, respectively, in the total changes. Following was the work pace and stress with more than 11%, due to the intervention of work time re‐arrangement and relaxation. Due to the work task content for dental professionals, 82% of participants’ back had a static posture during most of working time, the PE intervention was limited to change this risk factor, which only accounted for 4% among the total changes.
TABLE 2.
Summary of ergonomic changes in the intervention group
| Body part | Ergonomic risk factor | Before intervention, n (%) a | After intervention, n (%) a | Ergonomic changes, n (%) b |
|---|---|---|---|---|
| Neck | Head/neck bent or twisted excessively | 68 (77.3) | 20 (22.3) | 48 (20.4) |
| Shoulders/arms | Arm move frequently | 23 (26.1) | 10 (11.4) | 13 (5.5) |
| Above shoulder height | 31 (35.2) | 9 (10.2) | 22 (9.4) | |
| Back | Flexed, twisted or side bent | 46 (52.3) | 23 (26.1) | 23 (9.8) |
| Move frequently | 20 (22.7) | 10 (11.4) | 10 (4.3) | |
| Static posture most of time | 72 (81.8) | 63 (71.6) | 9 (3.8) | |
| Hands/wrists | Deviated or bent wrist position | 66 (75.0) | 31 (35.2) | 35 (14.9) |
| Similar repeated motion | 33 (37.5) | 16 (18.2) | 17 (7.2) | |
| Others | Have difficulty in keeping up with work | 41 (46.6) | 15 (17.0) | 26 (11.1) |
| Feel stressful at work | 37 (42.0) | 10 (11.4) | 27 (11.5) | |
| Experience vibration at work | 49 (55.7) | 44 (50.0) | 5 (2.1) | |
| Total changes | 235 |
Percentage accounted in the 88 intervention participants.
Percentage accounted in the total ergonomic changes.
Table 3 shows the changes in ergonomic exposure scores and high exposure level in the intervention and control group. Compared to the baseline, ergonomic exposure scores and/or the percentage of high ergonomic exposure level on four body sites in the intervention group was significantly reduced after different follow‐up times. For control group, there was no significant change in exposure scores and percentage of high exposure level on the four body sites.
TABLE 3.
Changes in ergonomic risk exposure in the two groups during follow‐up
| Intervention group | Control group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Neck | Shoulders/arms | Back | Hands/wrists | Neck | Shoulders/arms | Back | Hands/wrists | ||
| Baseline | Total scores, mean (SD) | 11.56 (3.88) | 21.02 (5.47) | 15.89 (5.95) | 24.20 (7.42) | 12.02 (4.01) | 19.55 (5.97) | 16.75 (5.36) | 25.06 (8.03) |
| High exposure level, n (%) | 41 (46.6) | 5 (5.7) | 8 (9.1) | 19 (21.6) | 43 (43.4) | 6 (6.1) | 8 (8.1) | 20 (20.0) | |
| 3 months | Total Scores, mean (SD) | 9.50 (3.65) | 19.51 (5.68) | 13.80 (5.46) | 22.17 (7.12) | 11.52 (3.67) | 18.71 (6.56) | 16.55 (6.33) | 23.11 (7.52) |
| High exposure level, n (%) | 23 (26.1)* | 3 (3.4) | 5 (4.5) | 12 (13.6) | 36 (36.4) | 4 (4.0) | 6 (6.1) | 14 (14.1) | |
| 6 months | Total Scores, mean (SD) | 8.32 (3.72)* | 18.50 (4.96) | 13.11 (5.50) | 21.03 (6.85) | 10.77 (3.82) | 18.93 (6.31) | 15.32 (6.05) | 23.65 (7.13) |
| High exposure level, n (%) | 20 (22.7)* | 2 (2.3) | 3 (3.4) | 9 (10.2)* | 37 (37.4) | 5 (5.1) | 5 (5.1) | 15 (15.2) | |
| 9 months | Total Scores, mean (SD) | 8.86 (4.01)* | 17.56 (5.03)* | 13.65 (6.10) | 19.06 (6.91)* | 12.16 (4.15) | 19.12 (5.71) | 16.54 (7.11) | 24.76 (6.55) |
| High exposure level, n (%) | 27 (30.7)* | 1 (1.1) | 4 (4.5) | 8 (9.1)* | 40 (40.4) | 5 (5.1) | 7 (7.1) | 16 (16.2) | |
| 12 months | Total Scores, mean (SD) | 9.22 (3.96) | 17.97 (5.33)* | 12.85 (5.23)* | 20.66 (7.55) | 11.24 (3.93) | 17.89 (5.82) | 17.33 (6.36) | 23.98 (6.89) |
| High exposure level, n (%) | 25 (28.4)* | 2 (2.3) | 2 (2.3) | 10 (11.4) | 39 (39.4) | 4 (4.0) | 8 (8.1) | 15 (15.2) | |
Abbreviation: SD, standard deviation.
Compared to the baseline, P < .05.
Table 4 shows the changes in MSD prevalence and WAI during the 1‐year follow‐up. Compared to the prevalence of baseline, MSDs on neck, low back and wrists/hands were significantly reduced after 9‐month or 12‐month in the intervention group, while no significant changes were found in the control group during the follow‐up. For WAI, significant improvement by 1.1 scores was seen in the intervention group after 9‐month follow‐up. No statistical change was detected for WAI in the control group.
TABLE 4.
Changes in MSD prevalence and WAI during the follow‐up
| Intervention group | Control group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Neck, n (%) | Shoulders/arms,n (%) | Low back, n (%) | Wrists/hands, n (%) | WAI, Mean (SD) | Neck, n (%) | Shoulders/arms, n (%) | Low back, n (%) | Wrists/hands, n (%) | WAI, Mean (SD) | |
| Baseline | 43 (48.9) | 24 (27.3) | 29 (32.9) | 26 (29.5) | 39.1 (3.5) | 48 (48.5) | 28 (28.3) | 32 (32.3) | 29 (29.3) | 39.2 (3.6) |
| 3 months | 36 (40.9) | 19 (21.6) | 22 (25.0) | 21 (23.9) | 39.3 (3.7) | 42 (42.4) | 23 (23.2) | 30 (30.3) | 25 (25.3) | 39.0 (3.7) |
| 6 months | 30 (34.1) | 20 (22.7) | 20 (22.7) | 18 (20.5) | 38.9 (4.0) | 42 (42.4) | 25 (25.3) | 26 (26.3) | 22 (22.2) | 39.1 (4.1) |
| 9 months | 32 (36.4) | 13 (14.8)* | 21 (23.9) | 21 (23.9) | 40.2 (3.6)* | 45 (45.5) | 22 (22.2) | 27 (27.3) | 24 (24.2) | 38.9 (3.6) |
| 12months | 28 (31.8)* | 16 (18.2) | 17 (19.3)* | 14 (15.9)* | 40.1 (3.9) | 43 (43.4) | 23 (23.2) | 28 (28.3) | 22 (22.2) | 39.3 (3.7) |
Abbreviations: MSD, musculoskeletal disorder; SD, standard deviation; WAI, work ability index.
Compared to the baseline, P < .05.
Table 5 shows the intervention effects on MSD reduction and WAI improvement through 1‐year participatory intervention. Derived from the logistic models, participatory intervention statistically increased the possibility of change from MSD symptom to relieved or no symptom on neck (OR = 2.93, 95% CI: 1.25, 4.03) and wrists/hands (OR = 2.33, 95% CI: 1.08, 4.21). In the linear regression model, WAI marginally increased after 9‐month intervention (B = 0.53, 95% CI −0.02, 1.56).
TABLE 5.
Intervention effects on MSD reduction and WAI improvement
| OR | 95% CI | P value | |
|---|---|---|---|
| Neck | |||
| 3 months | 1.16 | 0.51, 2.78 | 0.591 |
| 6 months | 2.14 | 0.95, 3.68 | 0.068 |
| 9 months | 1.77 | 0.83, 3.26 | 0.131 |
| 12 months | 2.93 | 1.25, 4.03 | 0.015 |
| Shoulders/arms | |||
| 3 months | 1.16 | 0.51, 2.78 | 0.591 |
| 6 months | 1.77 | 0.83, 3.26 | 0.131 |
| 9 months | 2.23 | 0.97, 4.69 | 0.062 |
| 12 months | 2.11 | 0.92, 4.26 | 0.070 |
| Wrists/hands | |||
| 3 months | 1.05 | 0.62, 3.10 | 0.501 |
| 6 months | 0.96 | 0.58, 2.91 | 0.189 |
| 9 months | 1.72 | 0.98, 3.57 | 0.052 |
| 12 months | 2.33 | 1.08, 4.21 | 0.008 |
| Low back | |||
| 3 months | 1.33 | 0.79, 3.18 | 0.233 |
| 6 months | 1.78 | 0.85, 3.62 | 0.103 |
| 9 months | 1.65 | 0.78, 3.32 | 0.151 |
| 12 months | 2.04 | 0.95, 4.29 | 0.061 |
| B | 95% CI | P | |
|---|---|---|---|
| WAI improvement | |||
| 3 months | 0.16 | −0.09, 1.15 | 0.277 |
| 6 months | −0.09 | −0.12, 1.09 | 0.389 |
| 9 months | 0.53 | −0.02, 1.56 | 0.055 |
| 12 months | 0.35 | −0.05, 1.31 | 0.089 |
Abbreviations: CI, confidence interval; MSD, musculoskeletal disorder; OR, odds ratio; WAI, work ability index.
4. DISCUSSION
4.1. Main findings
In this cluster randomized controlled trial, we assessed the efficacy of a PE intervention on ergonomic risk exposure, musculoskeletal disorders, and work ability among young dental professionals. The PE intervention delivered to the young dental professionals showed more effective on reducing ergonomic exposure and MSD symptoms on neck and wrists/hands than the control after 12‐month interventions. Work ability marginally increased after 9‐month follow‐up in the intervention group.
4.2. Results explanation and compared to other studies
Participants allocated to PE experienced a significant reduction of ergonomic risk exposure, particularly on neck and wrists/hands during different follow‐up times. The exposure score of neck was reduced by 3.24 scores with the PE intervention, which indicated that the ergonomic risk exposure significantly decreased when compared to the baseline after 6‐month intervention, the percentage of high exposure level decreased significantly by 23.8% as well. The prevalence of MSD symptoms on the four body sites reduced significantly after 9‐month or 12‐month intervention as well. In contrast, those in the control had no significant change either on ergonomic risk exposure or MSDs. To further identify the intervention effect on MSDs, we used multivariate analyses to exclude out the possible confounding. The results showed that the PE intervention after 12‐month had a significant benefit on reducing MSD symptoms on neck and wrists/hands. Previous studies have reported inconsistent results regarding to the PE effects on health outcomes including MSDs. A RCT study in Hong Kong reported a positive effect on reducing musculoskeletal disorders with PE interventions among healthcare workers. 23 Droeze et al. reported a clear relation between ergonomic implementation of recommendations and a reduction in MSD, which there were 72% of the dentists reported a reduction or disappearance of the main complaint in dentists. 24 A systematic review summarized that there was partial to moderate evidence that PE interventions have a positive impact on musculoskeletal symptoms, reducing injuries and workers’ compensation claims, and a reduction in lost days from work or sickness absence. 25 Our present study supported that PE was effective in both reducing ergonomic risk exposure and MSDs. However, some literature reported a negative effect on either reducing exposure to ergonomic risk including psychosocial and physical risks or MSD reduction with a PE intervention. 10 , 26 Although PE neither reduced low‐back and neck pain prevalence nor pain intensity and duration, nor was it effective in the prevention of low‐back and neck pain, PE was more effective in the recovery from low‐back pain. 27 Another study in Japan pointed out that PE was effective in workplace improvement, but need to maintain the effective by keeping regular interventions. 28 The inconsistent results might be explained by the different study subjects, cultural context, and the PE implementation. 24 Young dental professionals in our study might not be comparable to blue‐collar workers in those previous studies, and even the job tasks varied during the follow‐up which was also a partial explanation of inconsistency.
Regarding WAI, PE participants had an improvement with 1.1 scores increasing after 9‐month compared to the baseline, which indicated that the intervention was effective in improving WAI. The controls did not have similar results. Multivariate analyses showed the PE effect on WAI reached marginally significant after 9‐month with an average of 0.53 score improvement. WAI is an instrument used as a predictor for long‐term sickness absence and early retirement. 17 , 29 Our recent investigation found that WAI reduction was significantly associated with the high level of ergonomic risk exposure. 8 Despite PE in this current study did not reach a positive effect on WAI, we still detected an improvement of WAI and this is important for young dental professionals to prevent WAI from deteriorating in their early career. The presence of a high initial work ability level among the young participants and relatively short‐term follow‐up might be the explanations. 30 Thus, more studies with longer follow‐up times and full age coverage are warrant to clarify whether PE could improve WAI.
4.3. Strengths and weakness
This study had both strengths and weakness. We applied a cluster‐randomized controlled trial design which protests against systematic bias. Furthermore, all data analysis is performed in accordance with the intention‐to‐treat principle and using a mixed‐model, which both increases the amount of data used and allows for sophisticated handling of missing observations. 22 Meanwhile, high follow‐up rate (intervention group 90.7%, control 96.1%) and the linear repeated‐measures mixed‐model which is a robust and often uses to handling missing values in intervention studies, reduce the potential bias due to the miss data as much as possible. On the other hand, there are also limitations in this study. Participants in our study are young and the average age is 27–28 years, which might not represent all ages and causes the generalizability of the study to the entire population of dental professionals. In addition, the inability to blind the participants introduces multiple risks of non‐specific effects, including possible placebo effects in respect of changes in the selected outcomes, particularly among those participants in the same hospitals. However, we used clustered method to randomize the participants and the contamination might be minor. Furthermore, the outcomes are measured either by self‐report questionnaire or examiners’ observation, and the data might have the risk of recall bias. However, this risk would be expected to be identical for both intervention and control group, thus decreasing the possibility of detecting significant differences between the two groups.
5. CONCLUSION
In conclusion, the PE intervention among young dental professionals is more effective than the controls in reducing ergonomic risk exposure and MSDs on neck and wrists/hands. A tendency of improving WAI in the intervention group was seen but needs more studies to confirm. The findings from this current study suggest that PE should be offered as early as the dental career starts, to reduce the possibility of MSDs among dental professionals.
DISCLOSURE
Approval of the research protocol: The study was approved by the committee of the Chinese University of Hong Kong and Putian University on biomedical research ethics. Informed consent: All participants were informed about the purpose and content of the study and gave their written informed consent to participate in the study. All intervention measurements conformed to the Declaration of Helsinki. Registry and the Registration No. of the study/Trial: The trial was registered as “Ergonomic intervention for prevention MSDs—dental professional,” No. Epi019. Animal Studies: N/A. Conflict of Interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work published in this paper.
ACKNOWLEDGMENTS
The authors acknowledge all dental professionals who participated in this project and the staffs who helped to complete this work in the hospitals.
This study was funded by the Fujian Provincial Bureau of Science and Technology (2020J01915) and the Putian University Talent Fund (2019019).
AUTHOR CONTRIBUTION
Dr. Sihao conceived of the presented idea. Sihao and Cheng chung designed the trial. Dr. Xudong and Mrs. Zhenyi completed the field work and helped to collected all data. Sihao and Cheng chung performed the data analyses. Mr. Xianzhe help to supervise the field work and check the procedures. All authors discussed the results and contributed to compose the manuscript.
Lin S, Tsai CC, Liu X, Wu Z, Zeng X. Effectiveness of participatory ergonomic interventions on musculoskeletal disorders and work ability among young dental professionals: A cluster‐randomized controlled trail. J Occup Health. 2022;64:e12330. doi: 10.1002/1348-9585.12330
Funding information
This study was funded by the Fujian Provincial Bureau of Science and Technology (2020J01915) and the Putian University Talent Fund (2019019).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Feng B, Liang QI, Wang Y, et al. Prevalence of work‐related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open. 2014;4:e006451. doi: 10.1136/bmjopen-2014-006451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu P, Shen B, Kang S, et al. Correlation between ergonomic load and work‐related musculoskeletal disorders among dentists. Chin J Ind Med. 2021;34(4):294‐297. [Google Scholar]
- 3. Taib MFM, Bahn S, Yun MH, et al. The effects of physical and psychosocial factors and ergonomic conditions on the prevalence of musculoskeletal disorders among dentists in Malaysia. Work. 2017;57(2):297‐308. [DOI] [PubMed] [Google Scholar]
- 4. Aminian O, Alemohammad ZB, Hosseini MH. Neck and upper extremity symptoms among male dentists and pharmacists. Work. 2015;51(4):863‐868. doi: 10.3233/WOR-141969 [DOI] [PubMed] [Google Scholar]
- 5. Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009;7:159‐165. [DOI] [PubMed] [Google Scholar]
- 6. Morse T, Bruneau H, Michalak‐Turcotte C, et al. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. J Dent Hyg. 2007;81(1):1‐16. [PubMed] [Google Scholar]
- 7. Hoevenaars JG. Dentist and disability: a matter of occupational disease? Ned TijdschrTandheelkd. 2002;109:207‐211. [PubMed] [Google Scholar]
- 8. Lin S, Wu Z, Tang W, et al. Ergonomic risk exposure and work ability among young dental professionals in China: a cross‐sectional study. J Occup Health. 2020;62(1): doi: 10.1002/1348-9585.12154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rivilis I, Van Eerd D, Cullen K, et al. Effectiveness of participatory ergonomic interventions on health outcomes: a systematic review. Appl Ergon. 2008;39:342‐358. [DOI] [PubMed] [Google Scholar]
- 10. Haukka E, Leino‐Arjas P, Viikari‐Juntura E, et al. A randomised controlled trial on whether a participatory ergonomics intervention could prevent musculoskeletal disorders. Occup Environ Med. 2008;65:849‐856. doi: 10.1136/oem.2007.034579 [DOI] [PubMed] [Google Scholar]
- 11. Monteiro M, Alexandre MCN, et al. Work ability and musculoskeletal disorders among workers from a public health institution. Int J Occup Saf Ergon. 2009;15(3):319‐324. [DOI] [PubMed] [Google Scholar]
- 12. Souza A, Alexandre MCN. Musculoskeletal symptoms, work ability, and disability among nursing personnel. Workplace Health Saf. 2012;60(8):353‐360. [DOI] [PubMed] [Google Scholar]
- 13. Akodu AK, Ashalejo ZO. Work‐related musculoskeletal disorders and work ability among hospital nurses. J Taibah Univ Med Sci. 2019;14(3):252‐261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. David G, Woods V, Buckle P. Further Development of the Usability and Validity of the Quick Exposure Check (QEC). HSE: Robens Centre for Health Ergonomics; 2005. https://www.hse.gov.uk/research/rrhtm/rr211.htm [Google Scholar]
- 15. Lin S. Development of a Tool for the Comprehensive Evaluation of Ergonomic Exposure at the Workplace and its Application Study in China (Dissertation). Sichuan University; 2006. [Google Scholar]
- 16. Lin S, Tang W, Wang Z, et al. CQEC development and Reliability examination for ergonomic exposure assessment at workplace. Strait J Prev Med. 2007;13(5):3‐6. doi: 10.3969/j.issn.1007-2705.2007.05.002 [DOI] [Google Scholar]
- 17. Ilmarinen J. The work ability index (WAI). Occup Med. 2006;57(2):160. doi: 10.1093/occmed/kqm008 [DOI] [Google Scholar]
- 18. Lin S, Wang Z, Wang M. Work ability of workers in western China: reference data. Occup Med. 2006;56:89‐93. [DOI] [PubMed] [Google Scholar]
- 19. Dong Y, Mamat N, Wang F, et al. Establishment and verification of the Chinese Musculoskeletal Questionnaire. Chin Occup Med. 2020;47(1):8‐14. doi: 10.11763/j.issn.2095-2619.2020.01.002 [DOI] [Google Scholar]
- 20. Dworkin RH, Turk DC, McDermott MP, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146(3):236‐244. [DOI] [PubMed] [Google Scholar]
- 21. Zebis MK, Andersen LL, Pedersen MT, et al. Implementation of neck/shoulder exercises for pain relief among industrial workers: a randomized controlled trial. BMC Musculoskelet Disord. 2011;12:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lachin JM. Statistical considerations in the intent‐to‐treat principle. Control Clin Trials. 2000;21:167‐189. [DOI] [PubMed] [Google Scholar]
- 23. Lee EWC, Fok JPC, Lam AT, Law RKY, Szeto GPY, Li PPK. The application of participatory ergonomics in a healthcare setting in Hong Kong. Work. 2014;48:511‐519. [DOI] [PubMed] [Google Scholar]
- 24. Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work. 2005;25(3):211‐220. [PubMed] [Google Scholar]
- 25. Rivilis I, Van Eerd D, Cullen K, et al. Effectiveness of participatory ergonomic interventions on health outcomes: a systematic review. Appl Ergon. 2008;39:342‐358. [DOI] [PubMed] [Google Scholar]
- 26. Driessen MT, Proper KI, Anema JR, et al. Participatory ergonomics to reduce exposure to psychosocial and physical risk factors for low back pain and neck pain: results of a cluster randomised controlled trial. Occup Environ Med. 2011;68:674‐681. doi: 10.1136/oem.2010.056739 [DOI] [PubMed] [Google Scholar]
- 27. Driessen MT, Proper KI, Anema JR, et al. The effectiveness of participatory ergonomics to prevent low‐back and neck pain – results of a cluster randomized controlled trial. Scand J Work Environ Health. 2011;37(5):383‐393. doi: 10.5271/sjweh.3163 [DOI] [PubMed] [Google Scholar]
- 28. Kajiki S, Izumi H, Hayashida K, Kusumoto A, Nagata T, Mori K. A randomized controlled trial of the effect of participatory ergonomic low back pain training on workplace improvement. J Occup Health. 2017;59:256‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sell L, Bültmann U, Rugulies R, et al. Predicting long‐term sickness absence and early retirement pension from self‐reported work ability. Int Arch Occup Environ Health. 2009;82:1133‐1138. [DOI] [PubMed] [Google Scholar]
- 30. Lidegaard M, Sogaard K, Krustrup P, et al. Efects of 12 months aerobic exercise intervention on work ability, need for recovery, productivity and rating of exertion among cleaners: a worksite RCT. Int Arch Occup Environ Health. 2018;91:225‐235. doi: 10.1007/s00420-017-1274-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


