Abstract
Background:
According to the latest medical evidence, Methadone and buprenorphine-naloxone (Suboxone®) are effective treatments for opioid use disorder (OUD). While the evidence basis for the use of these medications is favorable, less is known about the perceptions of the general public about them.
Objective:
This study aimed to use Twitter to assess the public perceptions about methadone and buprenorphine-naloxone, and to compare their discussion contents based on themes/topics, subthemes, and sentiment.
Methods:
We conducted a descriptive analysis of a small and automatic analysis of a large volume of microposts (“tweets”) that mentioned “methadone” or “suboxone”. In the manual analysis, we categorized the tweets into themes and subthemes, as well as by sentiment and personal experience, and compared the information posted about these two medications. We performed automatic topic modeling and sentiment analysis over large volumes of posts and compared the outputs to those from the manual analyses.
Results:
We manually analyzed 900 tweets, most of which related to access (15.3% for methadone; 14.3% for buprenorphine-naloxone), stigma (17.0%; 15.5%), and OUD treatment (12.8%; 15.6%). Only a small proportion of tweets (16.4% for Suboxone® and 9.3% for methadone) expressed positive sentiments about the medications, with few tweets describing personal experiences. Tweets mentioning both medications primarily discussed MOUD broadly, rather than comparing the two medications directly. Automatic topic modeling revealed topics from the larger dataset that corresponded closely to the manually identified themes, but sentiment analysis did not reveal any notable differences in chatter regarding the two medications.
Conclusions:
Twitter content about methadone and Suboxone® is similar, with the same major themes and similar sub-themes. Despite the proven effectiveness of these medications, there was little dialogue related to their benefits or efficacy in the treatment of OUD. Perceptions of these medications may contribute to their underutilization in combatting OUDs.
Keywords: Twitter, buprenorphine, methadone, social media, medication assisted treatment, opioid use disorder
Introduction
Medications for opioid use disorder (MOUD), methadone, buprenorphine, and naltrexone, are all FDA-approved for the treatment of opioid use disorder (OUD) and have been shown to reduce all-cause mortality, overdose-related mortality and transmission of infectious diseases, while increasing treatment retention and improving long-term outcomes [1]. Methadone and buprenorphine are agonist therapies, while naltrexone is an opioid antagonist; and due to these parallel modes of action, comparative effectiveness studies tend to focus on methadone and buprenorphine [2–4]. Methadone is a long-acting full agonist at the mu-receptor. In contrast, buprenorphine is a partial mu agonist which has a ceiling effect, thus, limiting euphoria and overdose. Despite their proven efficacy, these medications are underutilized for reasons such as treatment access barriers, stigma and misperceptions about their role in recovery [1]. Little is known about the public perceptions about these medications and whether the experiences related with these medications differ, although these factors may also be associated with their underutilization.
Past research to understand the perceptions about MOUDs have focused on interviewing individuals with OUD, but such studies have narrow scopes, lack diverse cohorts and are expensive to conduct or coordinate [5]. Social media, due to its widespread use, offers the opportunity to obtain and study discussions and perceptions associated with specific topics, including health-related topics. One popular social media platform that has been used extensively in past research related to substance use is Twitter. Twitter is a microblogging website and has become a popular platform for individuals to engage in discussions via publicly visible posts. Twitter has 326 million monthly active users, 100 million daily active users, and 500 million tweets per day [6]. Since Twitter microblogs are mostly publicly available, it has increasingly been used to investigate attitudes and perceptions, real-time content, and posts on specific topics through keywords and hashtags. Researchers have used Twitter to study various health and public health-related topics in the past, including topics associated with OUD and substance use disorder [7–10]. In this paper, we use data collected from Twitter to investigate the public perceptions of both buprenorphine-naloxone and methadone, and to compare the discussions of both medications by theme, sub-theme, and sentiment. Our analyses include automatic characterization of big data, and manual, more refined characterization of smaller subsets of data.
Methods
Data collection and preparation
We conducted a manual mixed-methods descriptive study and an automatic data analysis with the aid of natural language processing (NLP) methods to characterize public tweets mentioning methadone and buprenorphine-naloxone. We used the Twitter application programming interface (API) to collect the data using the generic (buprenorphine and methadone) and brand names (Dolophine® and Suboxone®) as keywords. Since medication names are often misspelled on Twitter, we used a spelling variant generator [11] to include misspellings of the medication names in the collection process. We found that in the case of methadone, the generic name was very commonly used in discussions, while trade names were rarely used. In the case of buprenorphine-naloxone, the trade name, Suboxone®, was most commonly used. We found Google Trends search results to verify this finding (Supplementary Material Figure 1). Therefore, throughout the rest of this paper, we use the terms methadone and Suboxone® to refer to these medications. We collected data from March 2018 to March 2020. Data collection was continuous, except for brief arbitrary periods of unexpected minor technical disruptions. During the manual analyses, the researchers used integer IDs for the tweets to hide the user handles of the original posters from the annotators. We preprocessed the data by removing duplicates, non-English tweets, very short tweets (e.g., those shorter than 10 characters and those consisting of emojis only), and tweets that had no content, other than emojies/symbols, in addition to the target word. We only used publicly available posts for this study, and the Institutional Review Board of Emory University reviewed and approved the study.
Manual data annotation and analysis
We drew a random sample from all the collected posts (random selection without replacement from each dataset) for manual analysis and used an adapted thematic analysis [12] to categorize the tweets. We first reviewed a sample of 150 tweets mentioning each medication to find common topics, and then coalesced these topics first into broad themes that represented the high-level information contents of the tweets. Following this, we manually categorized the tweets within each theme into fine-grained topics or sub-themes. Each tweet could have one or more themes (including the uncategorized or unrelated themes) and zero or more sub-themes. We chose example tweets of each theme and sub-theme and complied them in Table 1. We chose example tweets based on those that best represented the theme or sub-theme in a concise manner without overlapping with other themes. Three annotators (MC, AS, and WH) performed the annotations, with a small number (n = 100) of overlapping tweets, which were used to compute inter-annotator agreements (IAA). We computed mean pair-wise IAA using Cohen’s kappa [13]. AS resolved the disagreements between the annotators. We also coded the tweets based on the sentiment expressed in the context of the medication (negative, positive and neutral) and whether they represented personal experiences.
Table 1.
Description of themes associated with tweets mentioning suboxone® and methadone.
| Theme | Description | Example Methadone Tweet | Example Suboxone® Tweet |
|---|---|---|---|
| Access | patients’ ability to obtain medication legally | “Why do junkies get to queue at the chemist everyday for methadone?” | “@username how are you getting suboxone to those who can. ot afford it?” |
| Stigma | the negative view of the medication, its users, its clinics, or objects related to medication | “just seen an addict swig her methadone down in the chemist, what an awful life she is living. so thin and gaunt.” | “@username worry about your suboxone popping daughter and not drama” |
| Pain management | medication being used for to treat pain rather than opioid dependence | “@username It was methadone BID, Norco q6-8h. Just seemed like a lot of opiates for something chronic” | “@username I confess I don’t understand. Suboxone doesn’t strike me as 1st, 2nd or 3rd choice for post-op pain.” |
| OUD Treatment | treatment for OUD, including MOUD or other ways of treating OUD | “@username the accurate statement is: bupe and methadone are more effective than Vivitrol – show me otherwise.” | “instead of free needles, how about free suboxone & vivitrol? #needle exchange” |
| Tapering/ withdrawal | tapering oneself off, or the withdrawal associated with, the medication | “@username Just got off methadone could use all the help and prayers I can get  ” ” |
“#suboxone withdrawal sucks. Don’t be a junkie, kids.” |
| Safety/ side effects | the safety of medication or the side effects of medication | “drugs like vicodin, oxycontin and methadone must be carefully monitored as there is a risk of fatal overdose. however, experts say it is …” | “@username highest death rates from overdose in the u.s include traces of suboxone, fentenal or methadone in their toxicology reports!”
|
| Greed/ corruption | an entity acting as drug dealers or promoting medication out of hope for profits or kickbacks | “opioid dependants were created by greedy pharmaceutical co’s & obamacare .check out the number of methadone clinics and who owns them” | “@username 2 to 1 its pharmaceutical lobbyists pushing this. Suboxone makes gazillions” |
| Continued drug use | continuing to use or abuse opiates or opioids while being prescribed or using medication | “@username My friend has been on methadone for 8 months and is still shooting heroin. I just don’t understand why long-term residential tx isn’t an option. Surely if the drug use hasn’t stopped she needs something more?” | “@username I’ve only encountered 2–3 people who have been sober through suboxone/methadone treatments successfully. Most of the time people just use them as a way to keep doing drugs” |
| Misuse/ diversion | using medication in ways other than prescribed, using illegally obtained medication, or selling prescribed medication | “made a sell to a dude that stays fucked up and he gave me weed and a methadone pill lol” | “#Busted a visitor at Southern New Mexico Correctional Facility was caught trying to introduce suboxone into the facility! #NMCD #SNMCF #notonourwatch” |
| Uncategorized | medication and/or its use but does not fall into one of the above categories | “@username Obama was giving out smokes at the methadone clinic again.” | “In PA everyone was on suboxone  ” ” |
| Unrelated | not related to medication or its use | “Methadone Mary n black eye Bill” | “tales of symphonia and suboxone” |
Following the manual categorization, we compared the themes, topics, and sentiments between the methadone and Suboxone® tweets. We computed the proportions of these themes across the annotated tweets and compared the differences in the proportions using a two-tailed test for proportions. We then performed descriptive analyses of the tweets belonging to each theme, particularly for the more frequently occurring ones, to better describe their contents in terms of sub-themes and expressed sentiments.
Finally, we qualitatively analyzed a sample of tweets that mentioned both Suboxone® and methadone to gain an understanding of if and how they are compared in those tweets. We categorized tweets as pro-Suboxone®, pro-methadone, anti-Suboxone®, anti-methadone, or equal. We categorized tweets as pro-Suboxone® or pro-methadone if they mentioned the benefits of one medication compared to the other, as anti-Suboxone® or anti-methadone if the tweet mentioned downsides of one medication compared to the other. We further categorized these tweets in terms of whether the tweets expressed MOUDs in a positive way (pro-MOUD) or a negative way (anti-MOUD). Tweets that were not obviously positive or negative were categorized as neutral.
Automatic analysis
We performed two automated NLP-driven analyses of all collected unlabeled data. For both sets of tweets, we first performed topic modeling using latent Dirichlet allocation (LDA) [14], which is a statistical method that attempts to identify latent structures and topics within sets of documents. Each document is assumed to be a distribution of topics, which in turn are distributions of words. Thus, the output of the topic model is terms grouped into automatically discovered latent topics. We ran LDA on both sets of tweets with the number of topics (nt) ranging from 5 to 25, with steps of 5. We performed basic preprocessing of the text by lowercasing them, stemming using the Porter stemmer [15], and removing stop-words. For each value of nt we optimized the model based on the perplexity measure and we chose the model with the best perplexity (i.e., lowest). We analyzed the generated topics and compared them with the manually identified themes.
We also conducted a supervised sentiment analysis of both datasets by automatically characterizing the tweets into positive, negative and neutral, and comparing the distributions to those found in the manual analyses. We used the TextBlob NLP tool [16], which has been shown to have an accuracy of 76% for Twitter data [17], to conduct the analysis. The sentiment analysis method implemented in the software generates two values: polarity of sentiment (range: [–1]) and subjectivity (range: [0–1]). We used two methods to obtain aggregated sentiment scores for the datasets: for the first (default), we computed the raw sentiment distributions for both datasets; for the second (subjectivity-scaled), we scaled the sentiment scores using the subjectivity scores. The second model puts more emphasis on opinions that are more likely to be personal accounts (i.e., high subjectivity scores).
Results
Manual categorization
We manually analyzed a total of 900 tweets, 450 for each medication. MC analyzed/annotated 400 tweets, derived the initial themes and sub-themes, and outlined the annotation guidelines. AS annotated 200 tweets (100 for each medication) and WHB annotated 500 tweets (250 for each medication). Average pair-wise IAA between the three annotators was κ = 0.767 (Cohen’s kappa [13]; pair-wise IAAs: 0.765, 0.754, 0.790), which can be considered to be substantial agreement [18].
The methadone and Suboxone ® tweet samples contained similar overall themes, though the sub-themes differed. In total, we included 11 themes. Table 1 provides definitions of the themes and samples of these tweets, and Table 2 provides the percentage of methadone and Suboxone® tweets belonging to these. The top three most frequently occurring themes, other than uncategorized or unrelated, were access (15.3% for methadone; 14.3% for Suboxone®), stigma (17.0%; 14.3%), and OUD treatment (12.8%; 15.6%). Other themes included pain management, tapering/withdrawal, safety/side effects, greed/corruption, continued drug use, and misuse/diversion (Table 2). Most tweets were not from the perspective of personal experience, with only 15.7% (20.4% Suboxone®; 10.9% methadone) describing firsthand experiences and 6.3% (5.8%/6.9%) referring to the experiences of someone close to the poster (e.g., family member).
Table 2.
Analysis of themes associated with tweets mentioning suboxone® and methadone.
| Theme | Methadone Tweets (N = 450) n (%) | Suboxone® Tweets (N = 450) n (%) | p Value |
|---|---|---|---|
| Access | 69 (15.3) | 64 (14.3) | .64 |
| Stigma | 77 (17.0) | 70 (15.5) | .53 |
| Pain management | 25 (5.5) | 32 (7.0) | .33 |
| OUD Treatment | 57 (12.8) | 70 (15.6) | .21 |
| Tapering/ withdrawal | 14 (3.0) | 25 (5.6) | .07 |
| Safety/ side effects | 26 (5.8) | 18 (4.0) | .21 |
| Greed/ corruption | 24 (5.3) | 61 (13.5) | <.001a |
| Continued drug use | 8 (1.8) | 8 (1.8) | 1 |
| Misuse/ diversion | 9 (2.0) | 38 (8.5) | <.001a |
| Uncategorized | 63 (14.0) | 80 (17.3) | .14 |
| Unrelated | 129 (28.8) | 16 (3.5) | <.001a |
statistically significant difference.
Qualitative analysis
Tweets belonging to the access theme revealed factors that act as barriers to treatment for patients with OUD. These tweets typically presented the users’ views about obtaining MOUDs legally and difficulties faced when trying to access them, and often mentioned medication expense and cost coverage. Many tweets about Suboxone® within this theme focused on the high cost and the need for insurance. Methadone tweets in this theme discussed whether the government covered treatment costs or the need for OUD patients to wait in line at designated clinics to receive methadone doses, including firsthand experiences posted by patients (Table 3). The need for queuing at clinics while doses are verified and distributed is often described in medical literature as a barrier to treatment for patients, as well as a reason why zoning is difficult to obtain for methadone clinics [1]. Suboxone® tweets included those posted by physicians, who described the barriers faced by them, particularly the requirement to have a special license (the “x waiver’ – an extra training prescribers must undergo) to be able to prescribe the medication (Table 4). The x-waiver is known to ultimately limit patient access to this medication, as only about 5% of providers are x-waivered [19].
Table 3.
Subthemes of tweets mentioning methadone.
| Theme | Subtheme | Description | Tweets n (% of theme) | Example |
|---|---|---|---|---|
| Access | ||||
| Cost/coveragea | how methadone is covered or paid for, how much it costs patients | 18 (25.7) | “@username methadone is not covered for the working poor either. only those on some type of social assistance.” | |
| Queuing/distribution | the process of receiving methadone, including the need to stand in line at clinics | 13 (18.8) | “i figure that’s either a bus stop right there or a methadone clinic.” | |
| Stigma | ||||
| Opioid “substituting”a | using methadone as “trading” one opioid for another, less desirable opioid | 13 (17.1) | “Mad they got commercials for methadone and suboxone… like get off the street dope! Try ours instead! FOH” | |
| Stigma from healthcare providers | prejudice or negative sentiment towards people on methadone or with OUD from healthcare providers | 9 (11.4) | “Hours spent in EDs watching derision & annoyance they had with him, the ‘#addict’. Help Us! Why no methadone there & then? #overdose #heroin” | |
| OUD treatment | ||||
| Methadone vs suboxonea | directly compares methadone to suboxone | 11 (19.3) | “@username I know at least a dozen people who’ve tried to switch from methadone to buprenorphine, only one was successful long term!” | |
| MOUD successa | successes of any of the MOUD options, including methadone specifically | 9 (15.8) | “methadone + suboxone are effective heroin addiction treatments for many people + should remain the first line response. #phcsalome” | |
| Medical educationa | designed to educate readers, typically contain to facts and data about the opioid crisis or MOUD options | 19 (33.3) | “amitiza nnt = 13 for constipation. does not reverse methadone related constipation!!! #hpm17” | |
| Unrelated | ||||
| Analogies to methadone | compares unrelated things to methadone, often inferring that the thing compared to methadone is less desirable | 24 (18.5) | “@username I’m a full blown crumpet junkie. I’ll have to go on crumpet methadone (English muffins in the states) when I get back just to survive.” | |
| “Try methadone” | have consistent pattern comprised of “question? You probably have []. This causes []. Try methadone.” | 44 (34.1) | “Have freckles? Yes? You suffer from Skitzo. This causes numbness. Try Methadone” | |
subtheme was also seen in suboxone®-containing tweets.
Table 4.
Subthemes of tweets mentioning suboxone®.
| Theme | Subtheme | Description | Tweets n (% of theme) | Example |
|---|---|---|---|---|
| Access | ||||
| Cost/ Coveragea | how suboxone is covered or paid for, how much it costs patients | 25 (39.1) | “@username suboxone is very expensive, came to the u.s. from europe, initial training was data 2000 for an outpatient detox.” | |
| MD awareness/ licensing | difficulties in obtaining suboxone due to physician awareness, prescribing, or licensing issues | 18 (28.1) | “@username but there are only a few docs who can give suboxone to people and they are restricted to 30” | |
| Stigma | ||||
| Opioid “substituting”a | using suboxone as “trading” one opioid for another, less desirable opioid | 19 (27.1) | “Mad they got commercials for methadone and suboxone … like get off the street dope! Try ours instead! FOH” | |
| Myths | fallacies related to suboxone and the opioid epidemic | 18 (25.7) | “It would kill me too! I already have breathing problems. They think #opioids are a big, bad problem (they’re not) but making suboxone will prove to be deadlier. Sorry to say that but I believe it’s already started.” | |
| Suboxone “addiction” | suboxone treatment as “suboxone addiction” or refers to the addictive properties of suboxone | 10 (14.3) | “@username suboxone is one of the to drugs we detox patients from nowadays. #suboxoneaddiction” | |
| OUD treatment | ||||
| Methadone vs suboxonea | directly compares methadone to suboxone | 9 (13.2) | “@username Yes suboxone is a miracle drug to treat the crisis / methadone clinics should be shut down : have big lobby group” | |
| MOUD successa | successes using any of the MOUD options, including specific successes from suboxone | 20 (28.9) | “@username i have 4 years 5 months and 13 days sober… suboxone saved my life for the better. amen to that! #beingthankful” | |
| Medical educationa | designed to educate readers, typically contain to facts and data about the opioid crisis or MOUD options | 17 (23.7) | “@username its already available some places. nalaxone blocks opiate receptors in brain. just like suboxone” | |
| Tapering/ Withdrawal | ||||
| Alternatives | alternatives to treat the opioid withdrawal (including kratom and cannabis) | 8 (32.0) | “will #kratom help ween of suboxone???” | |
subtheme was also seen in methadone-containing tweets.
The stigma theme encompassed tweets that alluded to the public’s negative view about MOUDs. Tweets in this theme directly referenced instances of feeling stigmatized or judged based on the use of MOUD as well as tweets that indirectly referenced the stigma by referring to the medication, its users, or objects related to the use of the medication (such as Suboxone® wrappers) in a negative light. Some tweets asserted the idea that using methadone or Suboxone® is simply “substituting one drug or addiction for another” and that abstinence from all opioids is the only acceptable goal for people with OUD. We categorized such tweets as “opioid substituting” (Tables 3 and 4). Methadone tweets also described situations where individuals experienced stigma from healthcare providers, while Suboxone® tweets mentioned stigma associated with myths (e.g., Suboxone® makes a person more violent), referenced the idea of a “suboxone addiction”, or mentioned addictive properties of Suboxone®.
The OUD treatment theme encompassed tweets that discussed treatment-related chatter for OUD, including MOUD and other ways of treating OUD. Tweets compared methadone and Suboxone® directly, offered opinions on which is better, shared stories of success related to these medications, denounced these options altogether (Tables 3 and 4), and provided information regarding medical education or awareness.
Sentiment and comparative analysis
Most methadone tweets were categorized as neutral (49.1%; n = 450), while the majority of Suboxone® tweets were negative (55.8%; n = 450) (Figure 1). Albeit being small in number, the Suboxone® sample had more tweets categorized as positive than the methadone sample (16.4% vs. 9.3%). Positive tweets discussed the medications’ benefits, success stories, or expressed the idea that the MOUD is good for society, while negative tweets often mentioned side effects, toxicity, stories of failure or continued abuse, or experience of stigma.
Figure 1.
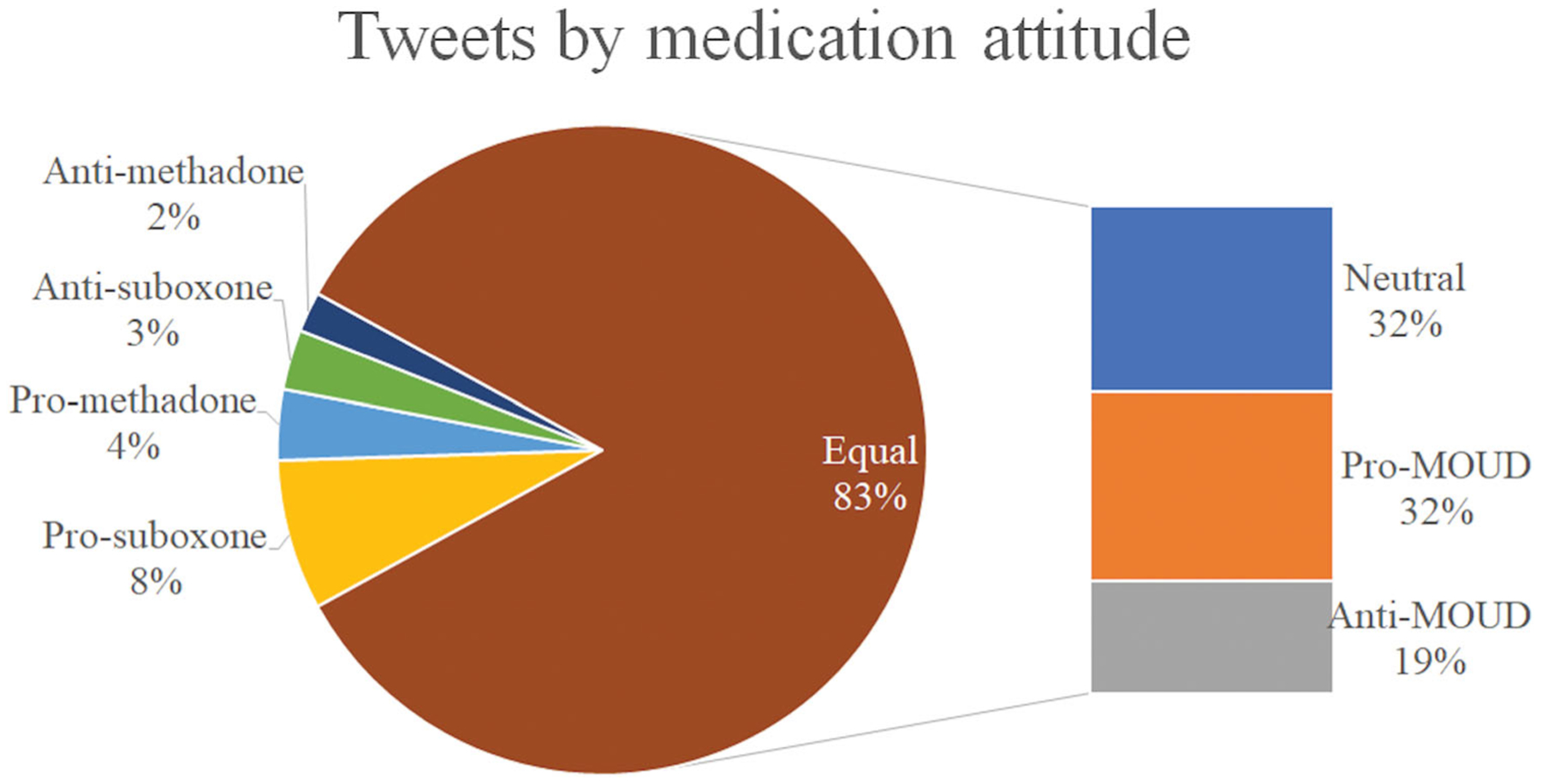
Distribution of user attitude among Tweets mentioning both “methadone” and “suboxone”.
In tweets that mentioned both Suboxone® and methadone, 84.0% (168/200) mentioned the medications in the same light and were thus categorized as equal (Figure 1). Of these 168 tweets, 39 tweets were anti-MOUD (23.0%), 64 were neutral (38.0%), and 65 were pro-MOUD (39.0%). The remainder of the tweets were more likely to mention the benefits of one medication over the other, with 15 tweets being pro-Suboxone® (8%) and 7 tweets being pro-methadone (4%). There were only a small number of tweets that were pointedly against one medication (6 anti-Suboxone® tweets [3%]; 4 anti-methadone tweets [2%]).
Automated analyses
The full dataset included a total of 424,396 tweets, with approximately 50/50 split for the two categories of medications (196,757 (46.4%) for Suboxone®; 227,639 (53.6%) for methadone). Manual inspection of the automatically generated topics revealed that nt=10 provided satisfactory set of topics. We found the automatically derived topics to be easily mappable to the manually identified themes. For the major themes (e.g., access and stigma) we found at least one set of topic words that reflected potential contents belonging to that theme. For methadone, we found topic mappings for 5 themes, while for Suboxone®, we found 7. Figure 2 presents the topic keywords, scaled by their strengths of associations with the topics. Note that specifically for the Access, OUD Treatment and Pain Management themes, we found multiple topics that could be mapped to them. We also observed more terms than presented in the figure that could potentially be mapped to Stigma but were spread across other topics.
Figure 2.
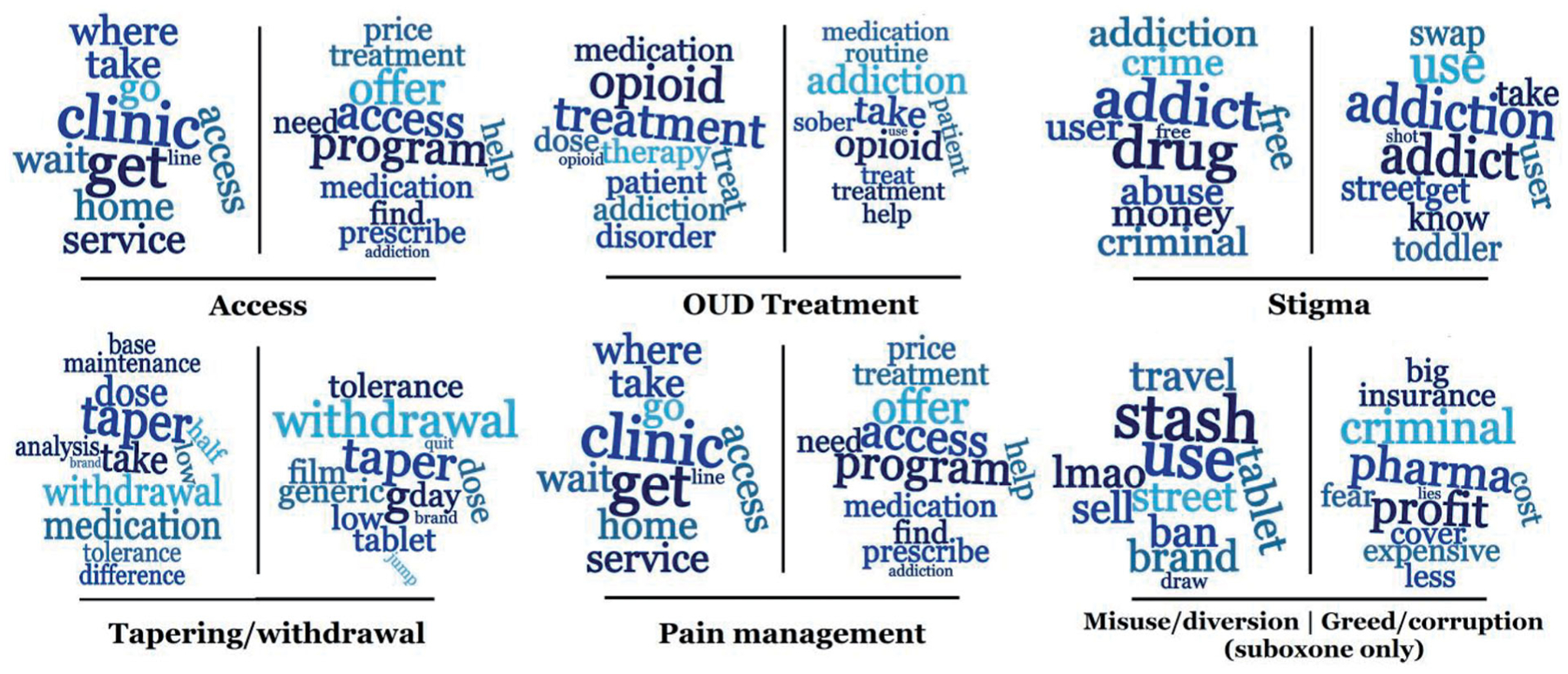
Topic terms discovered via latent Dirichlet allocation from unlabeled data and their possible mappings to manually discovered themes (left: methadone; right: suboxone). Misuse/diversion and Greed/corruption only had possible mappings for suboxone, and they are shown in the bottom left of the figure. Text size indicates strength of association with topic.
Unlike the manual sentiment analyses, our automated approach did not reveal any significant differences between the two medications. Figure 3 presents the sentiment distributions for our default and subjectivity-scaled models. As can be seen in the figure, the distributions are almost identical for the two medications, with most tweets being of neutral sentiment. Longer negative tails are visible for both medications, suggesting that there might be more negative sentiment at the extreme, compared to positive sentiment.
Figure 3.
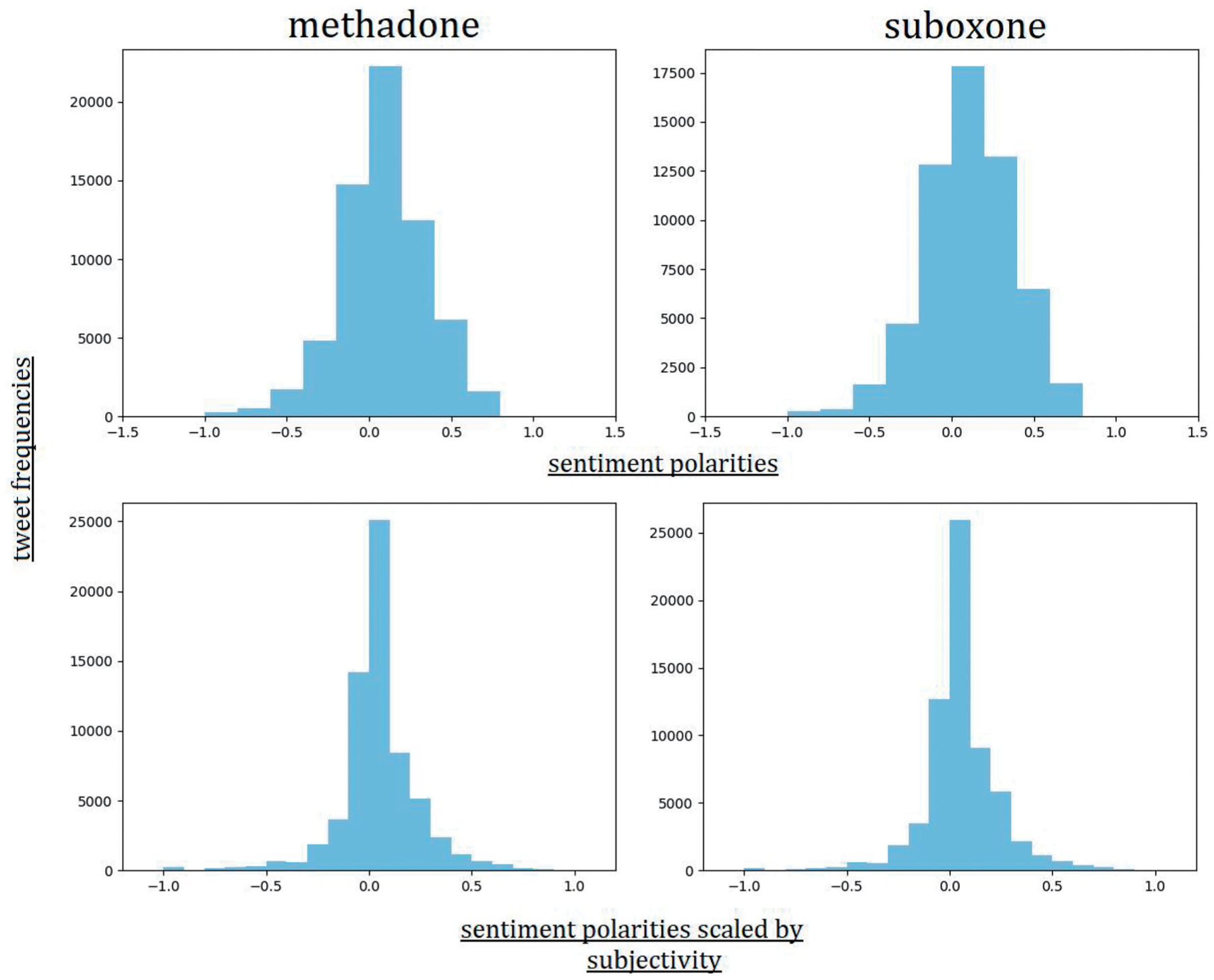
Distributions of automatically detected sentiment polarities for tweets mentioning methadone and Suboxone® (top), and sentiment polarities scaled by subjectivity scores (bottom).
Discussion
Benefits of and barriers to MOUD treatment
Much of the medical literature has focused on the perception of benefits and barriers as they relate to MOUD-based treatment from the viewpoints of doctors and the healthcare systems rather than from the perspectives of the public. The report from the Committee on Medication Assisted Treatment for OUD in 2019 identified the major barriers to MOUD as being misunderstanding and stigma related to OUD and its treatment, inadequate education of professionals meant to treat these patients, current regulations surrounding methadone and buprenorphine, and the fragmented system of care for OUD patients [1]. While many of the methadone- and Suboxone®-related themes we discovered were similar to those discussed in the medical literature, the discussions on Twitter did not include as many of the benefits that these medications have in treating OUD. The sub-theme “MOUD success” only comprised 2% and 5.5% of the methadone and Suboxone® tweets, respectively, suggesting a relative lack of public awareness to the benefits of both medications. As an increasing number of individuals search for relevant health-related information on social media, this relative lack of discussion of the benefits of MOUDs on this platform may skew public opinion of these medications, and hinder efforts to engage patients in evidence-based treatments to address the opioid crisis. This also highlights one area of potential intervention by the healthcare community: there is a role for providers to engage with the public and participate in discussions surrounding MOUD on social media to share success stories and data regarding the benefits of these medications in treating OUD. There is some evidence of this in our samples, with 2% (8) of the 400 tweets analyzed mentioning a doctor–patient or provider–client relationship with individuals with OUD. Interestingly, tweets that mentioned both medications were significantly more likely to be positive than tweets that only mentioned one medication (p < 0.0001), suggesting that users aware of the benefits of these medications discuss these medications together.
Additionally, a small proportion of tweets reflected firsthand experience with these medications, comprising about 20% of tweets that mentioned Suboxone and 10% of tweets that mentioned methadone. Interestingly, this does not parallel the proportion of these prescriptions, as SAMHSA data demonstrated that methadone prescriptions outnumbered suboxone prescriptions almost 5 fold (4.67 times) in 2015. This could relate to suboxone being a newer treatment modality, with more public questions about its uses, side effects, and effectiveness, leading to more online discussion surrounding it. This could be a topic of further research going forward, looking at why patients who use suboxone may be more likely to discuss their use online compared to patients who use methadone.
One important observation of the discussion surrounding barriers to treatment with these medications was the stigma theme. The idea of opioid substitution – the exchange of one opioid addiction for another – is a common subtheme and it is a barrier that makes addressing the opioid crisis more difficult. We found information seeking posts in both tweet samples, indicating that some people use these public discussions to obtain information on MOUDs. There were also tweets that mentioned stigma from healthcare providers, including accounts of patients being told to leave the emergency department (ED) to go to the methadone clinic, as the ED does not prescribe methadone. This unfortunately is a known barrier in OUD treatment, as some healthcare providers have demonstrated negative attitudes towards patients with OUD or feel unprepared to prescribe buprenorphine in the ED [20,21]. Reading about stigma-inducing tweets online could prevent patients with OUD from seeking treatment with MOUD for fear of poor treatment from the healthcare encounter. The automated analysis via topic modeling also revealed the common use of many stigma-invoking terms when posting about these two medications. Recently, studies have shown some success in utilizing programs to increase provider awareness and effectiveness in treating OUD int eh ED as well as starting treatment with suboxone in the ED [22–24]. Similar ED programs along with awareness campaigns through social media may help reduce the use of such terms.
Using social media to assess public perceptions
Recent research related to our work has attempted to analyze publicly available social media chatter about MOUDs to study public perceptions [25]. However, prior to such recent efforts, research on analyzing public perceptions and discussions surrounding methadone and Suboxone® focused primarily on conducting interviews with patients at inpatient treatment facilities. For example, Yarborough (2016) and colleagues grouped the discussions they had with adults with opioid dependence (n = 283) into themes they called “areas of consideration” for MOUD decision making. These included many of the same themes we found in our Twitter discussion including awareness of treatment options, stigma associated with methadone clinics, fear of continued addiction and perceived difficulty of withdrawal, and pain control [26]. Past studies based on face-to-face interviews were also limited in scope by only interviewing people currently in OUD treatment; thus, excluding the perceptions of the general population, and the families and friends of patients treated for OUD. A study conducted by Brown and Altice (2014), investigated the possibility of garnering information regarding buprenorphine/naloxone from online discussion boards, which were public and included discussions posted by people with OUD and the general public. Although the study excluded methadone, the themes discovered by the authors were similar to those found in our current study, including the need for a ready supply of the medication from a variety of sources, distrust of buprenorphine prescribers and the pharmaceutical companies, and a desire to become completely “substance free” [27].
While the work presented in this paper includes considerable manual effort, to effectively and continuously leverage the knowledge encapsulated within social media big data, automatic analysis is necessary as it is not possible to manually analyze all the large volume of data. At the same time, automatic methods often fail to identify the nuances between individual tweets, which are detectable by manual inspection. Thus, the two sets of analyses described in the paper are complementary and present us with a thorough understanding of the topics associated with these two medications that dominate Twitter. Our automated sentiment analysis approach leveraged a much larger dataset to study the distribution of chatter sentiments associated with these two medications. The approach revealed similar sentiment distributions for both treatments, with most posts deemed to be neutral. Comparing the classifications made by the automatic system and our manual sentiment categorization, we discovered that a human expert labeled reports of toxicity or adverse events as negative, but the automatic method often failed to pick up these medical domain-specific concepts. In the future, supervised classification methods, which learn from manually labeled data, may be trained using expert-curated datasets so that their decisions better reflect human judgments.
Limitations and future directions
Due to the use of social media data only, our analyses were limited to individuals who were on Twitter and actively self-reported information, limiting the generalizability of our findings. Twitter users tend to be younger and more racially diverse than the general population. Despite this limitation, Twitter has previously been used to examine attitudes and perceptions, which have been shown to be consistent with attitudes found using survey measures, and such a limitation also affects any survey-based studies [28]. For example, Farhadloo and colleagues (2018) examined the Twitter discussion on Zika and found associations between the two knowledge and behavior, concluding the importance of Twitter as a complementary source of information to gauge patterns of attitudes, knowledge, and behaviors in a population [29]. Similarly, the generalizability of our data is limited by the use of “suboxone” as the only trade name of buprenorphine formulations. While we used the API to search for both “suboxone” and “buprenorphine” as well as the common misspellings of both, we did not specifically search for other brand name formulations of buprenorphine. While in this study we focused on keywords that are more popular on the internet, future studies should incorporate a larger set of medication names, such as other formulations of buprenorphine.
Other limitations of the study include its retrospective nature and the non-inclusion of demographic information. Discussion on social media is constantly shifting and changing, and analysis of a sample of tweets can only offer a snapshot in time of the discussion. However, our samples were from tweets posted over a 2-year period and randomized for the manual analysis, allowing our sample to represent chatter from diverse time periods. It is possible that our samples of tweets came from geographic areas of the country with higher amounts of discussion on these topics, or that participants in the discussion had similar backgrounds. Only a small portion of the tweets we collected do have geolocation information available and so we did not filter based on this criterion for the manual analysis. Our automatic methods, which agree well with the manual analyses, can be used for geolocation-centric analysis in the future. Finally, another limitation of this study was its mixed-methods nature. While there was inter-rater agreement between the manual categorizations of tweets, these categorizations could be easily biased by personal beliefs and feelings toward MOUD.
One future direction of this work would be to use social media like Twitter to engage with the public to discuss MOUDs. This can enable practitioners to highlight aspects of the discussion that are underrepresented in social media, such as the numerous benefits of MOUD, as well as address some of the myths and stigma surrounding these medications. It will be interesting to evaluate whether interventions by physicians can change the public discussion and perception about these medications, and if localized interventions can change prescription practices. While the research on automated chatbots is still very much in its infancy, their rising popularity also warrants the future investigation of their utility for responding to MOUD-related stigma and misinformation on social media. Compared to all the methadone and Suboxone® related information available on Twitter, we only studied a small sample. In the future, we will focus on the development of more sophisticated NLP models and pipelines that can better interpret medical contents in social media chatter.
Conclusions
Our analyses of a sample of Twitter posts mentioning methadone and Suboxone® demonstrates that the discussions regarding the two medications are comparable, with the same major themes and many of the same sub-themes. Our analyses showed that some of the discussions on Twitter parallel that of the medical community, such as the barriers to implementing and using MOUDs for treatment, but they contained little discourse related to the benefits of these medications. Although these discussions are happening spontaneously on social media, it may be possible for the medical community to actively contribute to these discussions and raise awareness of the scientific evidence of the benefit of these medications and disseminate stories of success. Given the recent advances in NLP and the use of automated chatbots for similar purposes, we will consider it an additional future research direction.
Supplementary Material
Funding
This work was supported by National Institute on Drug Abuse [R01DA046619].
Abbreviations:
- API
application programming interface
- ED
mergency department
- IAA
inter-annotator agreements
- MOUD
medications for opioid use disorder
- OUD
opioid use disorder
- LDA
latent Dirichlet allocation
- NLP
Natural language processing
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data for this article can be accessed here.
References
- [1].Mancher M, Leshner AI. National Academies of Sciences, Engineering, and Medicine. Medications for opioid use disorder save lives. Washington (DC): National Academies Press; 2019. [PubMed] [Google Scholar]
- [2].Hser YI, Evans E, Huang D, et al. Long-term outcomes after randomization to buprenorphine/naloxone versus methadone in a multi-site trial. Addiction. 2016;111:695–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lemon LS, Caritis SN, Venkataramanan R, et al. Methadone versus buprenorphine for opioid use dependence and risk of neonatal abstinence syndrome. Epidemiology. 2018;29:261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Strayer RJ, Hawk K, Hayes BD, et al. Management of opioid use disorder in the emergency department: a white paper prepared for the American Academy of Emergency Medicine. J Emerg Med. 2020;58:522–546. [DOI] [PubMed] [Google Scholar]
- [5].Randall-Kosich O, Andraka-Christou B, Totaram R, et al. Comparing reasons for starting and stopping methadone, buprenorphine, and naltrexone treatment among a sample of white individuals with opioid use disorder. J Addict Med. 2019;14: e44–e52. [DOI] [PubMed] [Google Scholar]
- [6].Aslam S Twitter by the Numbers 2020. Stats, Demographics & Fun Facts. 2020. Available from: https://www.omnicoreagency.com/twitter-statistics/
- [7].Chary M, Genes N, Giraud-Carrier C, et al. Epidemiology from Tweets: estimating misuse of prescription opioids in the USA from social media. J Med Toxicol. 2017;13:278–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tufts C, Polsky D, Volpp KG, et al. Characterizing Tweet volume and content about common health conditions across Pennsylvania: retrospective analysis. JMIR Public Health Surveill. 2018;4:e10834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Graves RL, Tufts C, Meisel ZF, et al. Opioid discussion in the Twittersphere. Subst Use Misuse. 2018;53:2132–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sarker A, Gonzalez-Hernandez G, Ruan Y, et al. Machine learning and natural language processing for geolocation-centric monitoring and characterization of opioid-related social media chatter. JAMA Netw Open. 2019;2:e1914672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sarker A, Gonzalez-Hernandez G. An unsupervised and customizable misspelling generator for mining noisy health-related text sources. J Biomed Inform. 2018;88:98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- [13].Cohen J A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- [14].Blei DM, Ng AY, Edu JB. Latent Dirichlet Allocation Michael I. Jordan. 2003;3. [Google Scholar]
- [15].Porter MF. An algorithm for suffix stripping. Program. 1980;14: 130–137. [Google Scholar]
- [16].TextBlob: simplified text processing – TextBlob 0.16.0 documentation. [accessed 2020 Oct 26]. Was 23. Available from: https://textblob.readthedocs.io/en/dev/
- [17].Hasan A, Moin S, Karim A, et al. Machine learning-based sentiment analysis for twitter accounts. MCA. 2018;23:11. [Google Scholar]
- [18].Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–363. [PubMed] [Google Scholar]
- [19].Berk J To help providers fight the opioid epidemic, “X The X Waiver”. Health Affairs Blog. 2019. [Google Scholar]
- [20].Kennedy-Hendricks A, Busch SH, McGinty EE, et al. Primary care physicians’ perspectives on the prescription opioid epidemic. Drug Alcohol Depend. 2016;165:61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Im DD, Chary A, Condella AL, et al. Emergency department clinicians’ attitudes toward opioid use disorder and emergency department-initiated buprenorphine treatment: a mixed-methods study. West J Emerg Med. 2020;21:261–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Martin A, Baugh J, Chavez T, et al. Clinician experience of nudges to increase ED OUD treatment. Am J Emerg Med. 2020;38: 2241–2242. [DOI] [PubMed] [Google Scholar]
- [23].Martin A, Kunzler N, Nakagawa J, et al. Get waivered: a resident-driven campaign to address the opioid overdose crisis. Ann Emerg Med. 2019;74:691–696. [DOI] [PubMed] [Google Scholar]
- [24].Martin A, Mitchell A, Wakeman S, et al. Emergency department treatment of opioid addiction: an opportunity to lead. Acad Emerg Med. 2018;25:601–604. [DOI] [PubMed] [Google Scholar]
- [25].Tofighi B, El Shahawy O, Segoshi A, et al. Assessing perceptions about medications for opioid use disorder and Naloxone on Twitter. J Addict Dis. 2020;39:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Yarborough BJH, Stumbo SP, McCarty D, et al. Methadone, buprenorphine and preferences for opioid agonist treatment: a qualitative analysis. Drug Alcohol Depend. 2016;160:112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Brown SE, Altice FL. Self-management of buprenorphine/naloxone among online discussion board users. Subst Use Misuse. 2014;49:1017–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Perrin A, Anderson M. Social media usage in the U.S. in 2019. Pew Res Cent. 2019. Available from: https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/. Archived at: https://www.webcitation.org/78C8HLwUK [Google Scholar]
- [29].Farhadloo M, Winneg K, Chan MPS, et al. Associations of topics of discussion on Twitter with survey measures of attitudes, knowledge, and behaviors related to zika: probabilistic study in the United States. JMIR Public Health Surveill. 2018;4:e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


