Abstract
Background
Our study aimed to assess the burden of obesity on the health system and outcomes in patients with non-valvular cardiomyopathy.
Methods
A retrospective analytical cohort, single-center study was conducted at King Abdullah Medical City (KAMC), Makkah, from June 2019 to June 2020, and includes all non-valvular cardiomyopathy (NVCM) patients. The patients were divided into two groups, obese (BMI≥30) and non-obese (BMI<30). The two groups were compared using a t-test and a chi-squared test for continuous and categorical data and regression analysis.
Results
A single-center, retrospective study was conducted at KAMC, Makkah, and included all NVCM patients (ejection fraction or EF≤45%) who were admitted during this study period. A total of 626 NVCM patients were included in this cohort study; they had a mean BMI of 29±8.1 and a mean EF of 28.4±9.7. Patients were divided into two groups, obese (BMI≥30) and non-obese (BMI<30). Obese patients represented 37% (n=231) of our study population. The non-ischemic category of cardiomyopathy had a higher prevalence among the obese (35% vs 27%). A higher percentage of obese patients presented with heart failure (HF) symptoms rather than ischemia or arrhythmia (46%, 40%, and 7% for HF symptoms, ischemia, and arrhythmia, respectively). There was no significant difference in NVCM complications, including cardiogenic shock, pulmonary edema, and cardiac arrest, between the two groups. Obese patients had a significantly higher post-myocardial infarction (MI) ejection fraction (29.7±9.7 vs 27.5±9.7, p=0.01). We found a statistically significant positive correlation between BMI and length of in-hospital stay (P=0.04). In-hospital mortality was non-significantly different between our two groups, although numerically, it was higher among the non-obese group (obesity paradox) (10% vs 12%, p=0.2). Type of cardiomyopathy, cerebrovascular stroke, smoking, and sacubitril/valsartan intake were detected as independent predictors of in-hospital mortality among our patients.
Conclusions
Obesity among NVCM patients sets more burden on health facilities by the prolongation of the in-hospital stay of patients although BMI is not an independent predictor of death in those patients.
Keywords: body mass index: bmi, non-valvular cardiomyopathy, in-hospital outcome, health system, obesity
Introduction
In the last several decades, cardiomyopathies have become a more prevalent cause of heart failure in young individuals [1]. When heart failure gets worse, the length of time patients stay in the hospital, the cost of care, and the healthcare system's burden all go up [2]. Several clinical and laboratory indicators may be used to determine the prognosis of heart failure patients, one of which is obesity, which is defined as a body mass index (BMI) of more than or equal to 30 [3].
Obesity is a risk factor for heart failure and an important prognostic factor [4]. Obesity has become more common in recent decades, with 68% of US people being classified as overweight or obese [1]. Despite the fact that obesity is associated with increased all-cause mortality, after adjusting for established cardiovascular risk factors, such as body mass index (BMI) and waist circumference (WC), obesity is only marginally associated with coronary heart disease and stroke [4-6]. There is conflicting data on whether greater BMI is associated with an increased risk of heart failure or not [7-8]. Obesity, especially severe obesity, can cause hemodynamic changes that dispose of cardiac morphology and ventricular function changes [9]. These changes comprise cardiac left ventricular hypertrophy, output increase, diastolic and systolic dysfunction, including both ventricles, and may predispose to left and right heart failure, which may be exacerbated by obesity-related comorbidities, such as hypertension, sleep apnea/obesity hypoventilation syndrome, and neurohormonal and metabolic modifications, a condition known as obesity cardiomyopathy [10].
The majority of studies have documented an inverse relationship between obesity and heart failure; this concept is that overweight and mild-to-moderately obese patients have a better prognosis and lower risk of complications than normal-weight patients, a concept termed the obesity paradox [11]. Weight loss seems to be the only way to get rid of obesity-related comorbidities [12]. Healthcare investigators and workers should pay attention to the prevention of obesity and the treatment of affected individuals [13].
The obesity pandemic has left non-negligible bills to be paid by those affected, health services, and communities [13]. The correlation between obesity and NVCM was not well-assessed. In Saudi Arabia, limited studies have assessed the association between body weight/body mass index (BMI) and the in-hospital outcomes among patients with Non-Valvular Cardiomyopathy. so, we aimed in this study to estimate the burden of obesity on the health system and in-hospital outcomes of patients with non-valvular cardiomyopathy.
This article was previously presented as a poster at the American College of Cardiology’s 70th Annual Scientific Session & Expo (ACC.21) in Atlanta, GA, on May 17, 2021.
Materials and methods
Study design
This is a retrospective analytical cohort study that included 626 non-valvular cardiomyopathies (NVCM) patients admitted at King Abdullah Medical City (KAMC) during the period from June 2019 to June 2020.
Participants
We included all patients admitted to the cardiac center at KAMC with an established diagnosis of NVCM from June 2019 to June 2020. Those patients who fit the inclusion eligibility criteria in KAMC records were included. we exclude any patients with insufficient data and any patients outside the scope of the service of KAMC.
Ethical approval
Our study was designed to be part of the standards of patient care to investigate and improve the quality of NVCM prognoses and outcomes among a diverse population. Consent was taken, and the study received approval from the ethics committee/institutional review board (IRB) of our institution, King Abdullah Medical City, Mecca, Saudi Arabia (No. H-02- K-001).
Data collection
All demographic data were collected (including age, gender, nationality, height, weight, and residency status (Pilgrim, Resident, or Saudi). Risk factors, including diabetes mellitus (DM), hypertension (HTN), smoking, dyslipidemia, presence of chronic kidney disease (CKD), old cerebrovascular accidents (CVA), chronic obstructive lung disease (COPD), peripheral vascular disease (PVD), and atrial fibrillation (AF), were identified from the history and case note. Clinical presentation (heart failure symptoms, ischemia, or arrhythmias), Laboratory results (including hemoglobin (HB), blood urea nitrogen (BUN), creatinine, serum sodium (Na), serum potassium (K), troponin, glycosylated hemoglobin (HBA1c), brain natriuretic peptide (BNP), and vitamin D level) were obtained from the electronic and medical records. Echocardiography data (ventricular function, left ventricular (LV) thickness, LV, right ventricle (RV), and left atrium (LA) sizes, valvular assessment, left ventricular thrombus, and pericardial effusion) and coronary angiography findings (vessel involvement and procedure done) were also recorded. History of device insertion, including implantable cardioverter-defibrillator and cardiac resynchronization therapy (ICD/CRTD) and in-hospital outcome measures (including in-hospital death, cardiogenic shock, cardiac arrest, arrhythmias, pulmonary edema, ventilation, and length of hospital stay) were reviewed and recorded. Management strategies used for our patients, including medical treatment and revascularization therapy (percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)) were also identified. Discharge medications, including sacubitril/valsartan (Entresto), angiotensin-converting enzyme inhibitors (ACEi), antiplatelet (aspirin and clopidogrel), beta-blockers, statins, diuretics (including loop diuretics, spironolactone, and metolazone), digoxin, nitrates, and digoxin were also recorded.
Definitions and group division
Concerning the etiology of NVCM, the diagnosis was as follows:
I - Dilated cardiomyopathy (DCM): Left ventricular ejection fraction (LVEF) <0.45 (>2SD) as well as a left ventricular end-diastolic diameter >117% of the estimated value adjusted for age and body surface according to the Henry equation: (45·3(BSA) 1/3"0·03(age)"7·2), which corresponds to two SD of the predicted normal limit +5%).
II - Ischemic cardiomyopathy (ICM): Diagnostic criteria were similar to DCM in addition to coronary artery disease obstruction (≥50% narrowing of the diameter of the lumen of the left main coronary artery or ≥70% narrowing of the diameter of the lumen of the left anterior descending coronary artery, left circumflex artery, or right coronary artery).
III - Hypertrophic cardiomyopathy (HCM): In the absence of secondary causes of hypertrophy (HTN, aortic stenosis), it is diagnosed based on ≥15 mm wall thickness in one or more myocardial segments measured by echocardiography. The BMI is calculated by dividing a person's weight in kilograms by the square of their height in meters. The World Health Organization (WHO) states that for adults, obesity is defined as a body mass index of 30 or greater. Our study’s patients were divided into two groups according to BMI: group 1 obese (BMI≥30) and group 2 non-obese (BMI<30), and we compared both groups concerning all mentioned data.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software package (SPSS Inc.; Chicago, IL), version 21.0. Data are presented as mean ± SD for continuous data and percentage for categorical variables. Univariate analysis was done using the t-test or chi-squared test for continuous and categorical data, respectively. P-value ≤0.05 was considered significant and not significant if it is >0.05. Correlations and regression analysis were also calculated.
Results
A total of 626 consecutive NVCM patients were admitted to our cardiac center during the period from 2019 to 2020. They were divided into two groups: non-obese NVCM (395 patients (63%)) and obese NVCM (231 patients (37%)). We categorized our data into main five categories.
Baseline characteristics and clinical data
As shown in Table 1, the Saudis were more obese compared to non-Saudi patients (P=0.08). Age, cardiovascular risk factors, residency status, and associated morbidities were found to be statistically non-significant in both the non-obese and obese groups of patients. The obese patients had less prevalence of ischemic cardiomyopathy (ICM) as an etiology of heart failure (63% vs 71%% for obese and non-obese, respectively) but a higher prevalence of DCM (35% vs 27% for obese and non-obese, respectively). Concerning the prevention of sudden cardiac death and improving both quality of life as well as mortality, the utilization of device therapy (ICDs/CRTDs) was significantly higher among obese NVCM patients (P=0.029).
Table 1. Baseline demographic and clinical data of non-obese and obese NVCM patients.
NVCM: non-valvular cardiomyopathy; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; PVD: peripheral vascular disease; ICD: implantable cardiac defibrillator; CRTD: cardiac resynchronization therapy defibrillator
| Variable | Non-obese 395 (63%) | Obese 231 (37%) | P-value |
| Age, Years (Mean ± SD) | 56.76±13.49 | 55.21± 12.47 | 0.345 |
| Male gender, N (%) | 327 (83%) | 178 (77%) | 0.091 |
| Saudi nationality, N (%) | 284 (72%) | 192 (83%) | 0.081 |
| Pilgrims, N (%) | 45 (11.4%) | 14 (6%) | 0.132 |
| DM, N (%) | 249 (63%) | 145 (62.7%) | 0.242 |
| HTN, N (%) | 257 (65%) | 157 (68%) | 0.760 |
| Dyslipidemia, N (%) | 103 (26%) | 51 (22%) | 0.636 |
| Smoking, N (%) | 134 (34%) | 90 (39%) | 0.512 |
| Chronic kidney disease, N (%) | 55 (14%) | 39 (17%) | 0.396 |
| Cerebrovascular accident, N (%) | 67 (17%) | 51 (22%) | 0.266 |
| COPD, N (%) | 20 (5%) | 16 (7%) | 0.705 |
| PVD, N (%) | 16 (4%) | 17 (7%) | 0.400 |
| Atrial fibrillation, N (%) | 60 (15%) | 25 (11%) | 0.455 |
| Ischemic cardiomyopathy, N (%) | 281 (71%) | 145 (63%) | 0.140 |
| Dilated cardiomyopathy, N (%) | 106 (27%) | 81 (35%) | 0.140 |
| Hypertrophic cardiomyopathy, N (%) | 8 (2%) | 5 (2%) | 0.140 |
| Device insertion (ICD/CRTD) | 43 (11%) | 40 (17%) | 0.029 |
Clinical presentation, laboratory findings, and in-hospital outcome measures
As shown in Table 2, the obese patients showed higher presentation with heart failure symptoms rather than ischemia and arrhythmias (46%, 40%, and 7% vs 37%, 54%, and 5%; P=0.014 for obese and non-obese, respectively). There was potentially lower in-hospital mortality among obese patients (10% vs 12%; P=0.25). Other in-hospital outcome measures, including cardiogenic shock, cardiac arrest, and pulmonary edema, were also slightly lower among obese compared to non-obese patients.
Table 2. Clinical presentation and in-hospital outcomes of non-obese and obese NVCM patients.
NVCM: non-valvular cardiomyopathy
| Variable | Non-obese 395 (63%) | Obese 231 (37%) | P value |
| Congestive heart failure, N (%) | 146 (37%) | 106 (46%) | 0.014 |
| Ischemic symptoms (chest pain), N (%) | 213 (54%) | 92 (40%) | |
| Arrhythmias on presentation, N (%) | 20 (5%) | 16 (7%) | |
| Others, N (%) | 16 (4%) | 17 (7%) | |
| In hospital death, N (%) | 48 (12%) | 23 (10%) | 0.254 |
| Cardiogenic shock N (%) | 23 (6%) | 7 (3%) | 0.133 |
| Cardiac arrest, N (%) | 24 (6%) | 9 (4%) | 0.585 |
| Arrhythmias during hospitalization, N (%) | 83 (21%) | 51 (22%) | 0.457 |
| Pulmonary edema, N (%) | 31 (8%) | 14 (6%) | 0.694 |
| Intubated/Ventilated, N (%) | 24 (6%) | 13 (5.6%) | 0.612 |
| Length of hospital stay (Mean± SD) | 13.12±39.757 | 15.61±48.204 | 0.015 |
Table 3 represents the values of laboratory markers that were identified among obese NVCM patients (P=0.09, 0.06, 0.01, 0.07, and 0.07 for hemoglobin on discharge, serum creatinine, peak troponin, glycated hemoglobin (HBA1C), and brain natriuretic peptide (BNP), respectively).
Table 3. Laboratory findings of non-obese and obese NVCM patients.
NVCM: non-valvular cardiomyopathy; BUN: blood urea nitrogen; HbA1C: glycated hemoglobin; BNP: brain natriuretic peptide
| Test name | Non-obese 395 (63%) | Obese 231 (37%) | P-value |
| HB on admission (mg/dl), Mean ± SD | 13.32 ± 2.08 | 13.99 ± 10.73 | 0.125 |
| HB on discharge (mg/dl), Mean ± SD | 12.79 ± 2.09 | 12.77 ± 2.32 | 0.096 |
| Creatinine (mg/dl), Mean ± SD | 2.09 ± 1.077 | 1.50 ± 1.45 | 0.069 |
| BUN (mg/dl) ), Mean ± SD | 21.14 ± 12.645 | 20.73 ±14.457 | 0.393 |
| Serum sodium (mg/dl), Mean ± SD | 135.97 ± 10.718 | 138.11 ± 8.57 | 0.654 |
| Serum potassium (mg/dl), Mean ± SD | 4.22 ± .567 | 4.26 ± 0.632 | 0.185 |
| Troponin (mg/dl), Mean ± SD | 47.96 ± 271.962 | 15.19 ± 60.308 | 0.017 |
| HbA1C (mg/dl), Mean ± SD | 7.78 ± 2.386 | 7.69 ± 2.010 | 0.076 |
| BNP (pg/ml), Mean ± SD | 1159.09 ± 2529.3 | 919.76 ± 1202.5 | 0.07 |
| Vitamin D (ng/ml), Mean ± SD | 20.31 ± 13.311 | 15.54 ± 15.030 | 0.729 |
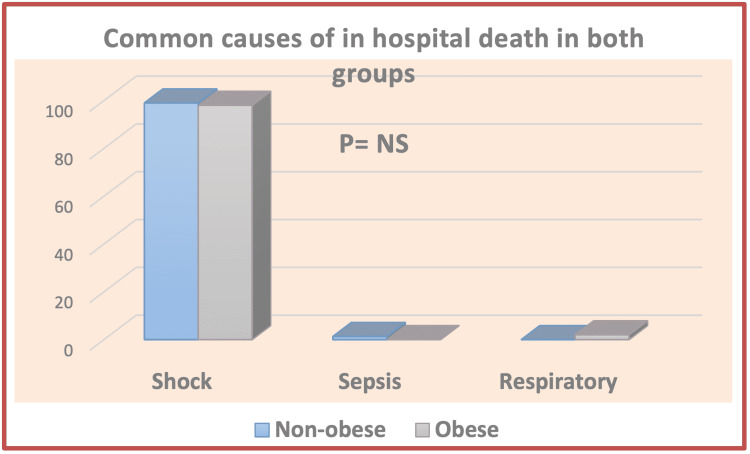
It can be seen from the data in Figure 1 that cardiogenic shock is the most common recorded cause of mortality among our patients.
Figure 1. Common causes of in-hospital death in both groups .
Cardiac imaging data
Obese NVCM patients showed a significantly higher mean LV ejection fraction such as 29.72±9.78 vs 27.52±9.73; P=0.012 but worse RV dysfunction (P=0.018) compared to the non-obese group of patients. Other echocardiography parameters, including LV and LA sizes, valvular dysfunction, LV thrombus, and pericardial effusion, were all found to be statistically non-significant in both groups (Table 4).
Table 4. Echocardiography of non-obese and obese NVCM patients.
NVCM: non-valvular cardiomyopathy; LVEF: left ventricular ejection fraction; RV: right ventricle; LV: left ventricle; LA: left atrium; MR: mitral regurgitation
| Variable | Non-obese 395 (63%) | Obese 231 (37%) | P-value |
| LVEF (Mean ± SD) | 27.52±9.73 | 29.72±9.78 | 0.012 |
| Diastolic dysfunction grade II/III, N (%) | 138 (35%) | 90 (39%) | 0.390 |
| Thickened LV | 28 (7%) | 21 (9%) | 0.488 |
| LV dilation, N (%); Moderate; Severe | 48 (12%) 75 (19%) | 32 (14%) 39 (17%) | 0.902 |
| Moderate/Severe RV dilation, N (%) | 32 (8%) | 30 (13%) | 0.186 |
| Moderate/Severe RV dysfunction, N (%) | 44 (11%) | 42 (18%) | 0.018 |
| Moderate/Severe LA dilation, N (%) | 94 (24%) | 49 (21%) | 0.684 |
| MR grade III/IV, N (%) | 103 (26%) | 69 (30%) | 0.272 |
| TR grade III/IV, N (%) | 79 (20%) | 32 (14%) | 0.222 |
| Left ventricular thrombus, N (%) | 36 (9%) | 23 (10%) | 0.902 |
| Pericardial effusion, N (%) | 20 (5%) | 9 (4%) | 0.430 |
Nevertheless, obese patients had a significantly lower incidence of both single and multi-vessel disease (P<0.05) (Table 5).
Table 5. Angiographic data and management strategies of ischemic cardiomyopathy subgroup of non-obese and obese NVCM patients.
NVCM: non-valvular cardiomyopathy; LM: left main; LAD: left anterior descending; LCX: left circumflex; RCA: right coronary artery; MVD: coronary microvascular disease; PCI: percutaneous coronary intervention; PCTA: percutaneous transluminal coronary angioplasty; CABG: coronary artery bypass graft
| Variable | Non-obese ICM 281 (45%) | Obese ICM 145 (23%) | P-value |
| LM disease, N (%) | 19 (6.8%) | 9 (6.2%) | 0.840 |
| LAD disease, N (%) | 169 (60%) | 68 (47%) | 0.008 |
| LCX disease, N (%) | 109 (39%) | 32 (22%) | 0.000 |
| RCA disease, N (%) | 110 (39%) | 39 (27%) | 0.006 |
| MVD, N (%) | 135 (48%) | 48 (33%) | 0.001 |
| Medical treatment, N (%) | 56 (20%) | 74 (51%) | 0.008 |
| PCI/PTCA, N (%) | 138 (49%) | 41 (28%) | |
| CABG, N (%) | 87 (31%) | 31 (21%) |
Management
Obese patients showed significantly higher medical therapy utilization and lower revascularization management compared to non-obese NVCM patients (P=0.008) (Table 5).
Regarding medical treatment, obese patients were more candidates for sacubitril/valsartan (Entresto) (P=0.062) and potentially were in higher need of different types of diuretics as compared to the non-obese group of patients (Table 6).
Table 6. Discharge medications of non-obese and obese NVCM patients.
NVCM: non-valvular cardiomyopathy; ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker
| Variable | Non-obese 395 (63%) | Obese 231 (37%) | P-value |
| Sacubtril/valsartan (Entresto), N (%) | 103 (26%) | 79 (34%) | 0.062 |
| ACEi/ARBs, N (%) | 241 (61%) | 120 (52%) | 0.052 |
| Aspirin, N (%) | 336 (85%) | 192 (83%) | 0.460 |
| Clopidogrel, N (%) | 245 (62%) | 125 (54%) | 0.070 |
| Beta-blockers, N (%) | 363 (92%) | 206 (89%) | 0.352 |
| Statin, N (%) | 312 (79%) | 188 (81%) | 0.662 |
| Loop diuretics, N (%) | 304 (77%) | 180 (78%) | 0.726 |
| Spironolactone, N (%) | 268 (68%) | 162 (70%) | 0.613 |
| Metolazone, N (%) | 20 (5%) | 14 (6%) | 0.570 |
| Nitrates, N (%) | 107 (27%) | 56 (24%) | 0.494 |
| Digoxin, N (%) | 12 (3%) | 14 (6%) | 0.086 |
Regression and correlations
Ischemic cardiomyopathy as an etiology of NVCM, history of cerebrovascular stroke, smoking, and intake of sacubitril/valsartan were the independent predictors of mortality among our patients. BMI was not found to be an independent predictor of in-hospital death in the current study (Table 7).
Table 7. Binary regression analysis of independent predictors of in-hospital mortality.
ICM: ischemic cardiomyopathy
| Variable | B | S.E | Exp (B) | P-value |
| Age | -0.269 | 0.323 | 0.764 | 0.405 |
| BMI | 0.002 | 0.025 | 1.002 | 0.951 |
| Smoking | 0.046 | 0.019 | 1.047 | 0.013 |
| Type of cardiomyopathy (ICM) | 0.033 | 0.011 | 1.034 | 0.003 |
| Cerebrovascular stroke | 0.899 | 0.455 | 0.407 | 0.048 |
| Sacubitril/Valsartan | 0.530 | 0.313 | 1.698 | 0.050 |
Most importantly, there was a significant positive correlation between BMI and in-hospital length of stay (p=0.04).
Discussion
King Abdullah Medical City is the only cardiac center in the region providing tertiary care services, such as revascularization and advanced heart failure therapy, and hence receives most of the NVCM patients for proper evaluation, workup, and further advanced management. Moreover, its location in the holy city of Makkah is unique, as it receives a considerable number of Hajj patients and residents of different nationalities. This allowed us to study that diverse population; it also reflects a significant burden for the provided service and hospital costs. All these factors contributed to the creation of the current study. To our knowledge, no study has been done in Saudi Arabia to see how BMI affects NVCM patients and the healthcare system when they are being treated in a hospital.
We included around 626 patients diagnosed with NVCM who were referred and admitted to our cardiac center from June 2019 to June 2020, with 37% obese patients and 63% non-obese.
Saudi patients with heart failure were more obese compared to non-Saudis. The different genetic, racial, environmental, and cultural backgrounds of non-Saudis who came from various places might explain this finding. There was no statistical difference between the two groups in terms of their age or gender, as well as their risk factors like diabetes, hypertension, and smoking.
Obese patients with NVCM exhibited lower in-hospital mortality rates than non-obese NVCM patients (obesity paradox). This was prescribed in previous studies conducted to assess the relationship between BMI and mortality in HF patients [14-18]. Our findings cope with the obesity paradox that was discussed before in cardiac patients, generally including ischemic heart and HF patients. However, it demonstrates an inverse relationship between BMI and in-hospital mortality rates; we do not know if this relationship can be applied to morbidly obese patients (BMI>35 kg/m2). Multiple mechanisms can explain the obesity paradox in HF patients. The catabolic state that occurs in HF patients with obesity represents the metabolic reserve, and high levels of serum lipoproteins associated with increased body fat in obese patients may also play an anti-inflammatory role, neutralizing circulating bacterial endotoxins or cytokines [19]. Some theories have been used to explain the obesity paradox as the early presentation of obese patients with less complex disease, and multiple comorbidities cause early recognition and treatment of the patients [17,20]. The higher value of hemoglobin on discharge, lower values of serum creatinine, HBA1C, BNP, and peak troponin, and significantly lower incidence of multi-vessel disease in NVCM obese patients might help explain potentially favorable outcomes among them.
A nationwide cohort study to evaluate the short-term effect of obesity in hospitalized patients with HF was published in 2020, included more than 1.5 million HF patients, and concluded that obesity was not associated with a higher incidence of inpatient mortality; however, it prolonged in-hospital stay in hospitalized patients with HF [21]. Our study’s finding was per this, as there was a significant positive correlation between BMI and in-hospital length of stay. This might be explained by the complexity of their disease and the higher need for HF management.
Although LVEF tended to be higher in obese patients, similar results to Harrison et al. [22], RV systolic function was more affected among them. This can be due to obesity-related pulmonary diseases, which may cause more burden on right ventricular performance, including obstructive sleep apnea, episodes of subclinical hypoxemia, high risk of recurrent DVT, and pulmonary embolization. Moreover, our findings suggest that the obese have a paradoxically lower coronary artery disease burden and severity. This again implies the presence of the "obesity paradox" and might be explained by the possible referral of obese patients to coronary angiography earlier than their non-obese counterparts.
In the current study, BMI was not recognized as an independent predictor for in-hospital death. This agreed with multiple studies that acknowledged that obese patients had significantly lower in-hospital and overall mortalities [22-23]. Obesity was not an independent predictor of overall mortality after multivariate analysis. In-hospital mortality in the current study was independently predicted by the type of cardiomyopathy (ischemic cardiomyopathy), smoking, and history of CVA, and this highlights different risk predictors that might affect prognosis in patients with different characteristics. The use of sacubitril/valsartan was also identified as a predictor of mortality among our patients, and this reflects the appropriate utilization of this drug in those patients with advanced disease, taking into consideration that its long-term efficacy is not tested in the current study due to a lack of follow up.
Interestingly, regarding the etiology and management of NVCM, obese patients had less prevalence of ICM and higher prevalence of DCM; this explains why obese patients presented to the hospital with congestive heart failure manifestations more often than other manifestations, with a higher need for device therapy in the form of ICD or CRTD and requiring more sacubitril/valsartan use. These results were synonymous with one large, longitudinal, population-based study whose main findings were that increased BMI was linked with an increased risk of heart failure in both genders, and this risk increased with BMI rise [7,24].
There was no significant difference in other outcomes of HF, including pulmonary edema, cardiac arrest, arrhythmias, dyspnea, and cardiogenic shock, between the two BMI categories. Our data are consistent with other published data [16]. Finally, the results of our study should give the heart failure research community a focused view of obesity’s impact on in-hospital outcomes in different types of NVCM and how an advanced HF treatment, including sacubitril/valsartan and device therapy, is effectively approached and used in candidate patients. Our research also highlights the burden of obesity on the health system, including a tertiary center with a considerable volume of variable population and a high flow rate.
Limitations
Part of the study was conducted during the coronavirus disease 2019 (COVID-19) pandemic. In addition, the number of enrolled patients is limited due to the nature of the single-center study and the selection of NVCM patients only, so the results can’t be generalizable. Moreover, there was no follow-up data or long-term outcomes since some patients were pilgrims or non-Saudis, and others lost their follow-up in the hospital. As our study includes patients with EF less than or equal to 45, we had patients with heart failure with preserved ejection fraction (HFpEF). The influence of obesity on both groups should be studied separately in the coming studies. We hope to reduce the effect of this limitation by motivating more hospitals to conduct similar research to create multicenter, larger sample studies in the future.
Conclusions
Although BMI was not an independent predictor of in-hospital mortality in patients with NVCM, obesity prolongs the in-hospital stay of NVCM patients, which causes less bed availability and more burden on the health care system. Most of the obese patients presented with heart failure symptoms rather than ischemic symptoms or arrhythmia and had a lower prevalence of MVD. In-hospital mortality was lower in obese patients but not statistically significant. The type of cardiomyopathy, cerebrovascular stroke, smoking, and sacubitril/valsartan intake were the independent predictors of in-hospital mortality. There is a need for prospective studies to elucidate the mechanisms of this relationship.
Identification and awareness of the mortality and morbidity predictors in NVCM patients might lessen the burden and save time and money for society. This study highlights the necessity of obesity management since it’s a heavy burden on both the health system and financial resources. Another reason is that it was found that obesity prolongs in-hospital stay. This study also suggests that other research addressing obesity with a larger sample size should be conducted to further explore the mortality and morbidity predictors in patients with NVCM. It is worth mentioning that health care systems should pay attention not only to obesity prevention but also to the treatment of patients with full medical and financial support, which in turn will prevent a significant burden on health system resources.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. King Abdullah Medical City IRB, Mecca, Saudi Arabia issued approval NO. H-02-K-001. This is to inform you that the above-mentioned proposal has been the subject of review by KAMC IRB registered at the National BioMedical Ethics Committee, King Abdulaziz City for Science and Technology on 14-07-1433 (Registration no. H-02-K-001) and is following the GCP-ICH regulations (OHRP Registration no. IORG0011096). The opinion of the IRB is to approve the extension and proposed changes
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Body mass index in young women and risk of cardiomyopathy: a long-term follow-up study in Sweden. Robertson J, Lindgren M, Schaufelberger M, et al. Circulation. 2020;141:520–529. doi: 10.1161/CIRCULATIONAHA.119.044056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Factors influencing the length of hospital stay of patients with heart failure. Wright SP, Verouhis D, Gamble G, Swedberg K, Sharpe N, Doughty RN. Eur J Heart Fail. 2003;5:201–209. doi: 10.1016/s1388-9842(02)00201-5. [DOI] [PubMed] [Google Scholar]
- 3.Body mass index: an effective predictor of ejection fraction improvement in heart failure. Ye LF, Li XL, Wang SM, Wang YF, Zheng YR, Wang LH. Front Cardiovasc Med. 2021;8:586240. doi: 10.3389/fcvm.2021.586240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Wormser D, Kaptoge S, Di Angelantonio E, et al. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dietary and policy priorities for cardiovascular disease, diabetes, and obesity. A comprehensive review. Mozaffarian D. Circulation. 2016;133:187–225. doi: 10.1161/CIRCULATIONAHA.115.018585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Lancet. 2014;383:970–983. doi: 10.1016/S0140-6736(13)61836-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Obesity and the risk of heart failure. Kenchaiah S, Evans JC, Levy D, et al. N Engl J Med. 2002;347:305–313. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 8.Increased heart failure risk in normal-weight people with metabolic syndrome compared with metabolically healthy obese individuals. Voulgari C, Tentolouris N, Dilaveris P, Tousoulis D, Katsilambros N, Stefanadis C. J Am Coll Cardiol. 2011;58:1343–1350. doi: 10.1016/j.jacc.2011.04.047. [DOI] [PubMed] [Google Scholar]
- 9.Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Alpert MA, Omran J, Bostick BP. Curr Obes Rep. 2016;5:424–434. doi: 10.1007/s13679-016-0235-6. [DOI] [PubMed] [Google Scholar]
- 10.Impact of obesity and weight loss on cardiac performance and morphology in adults. Alpert MA, Omran J, Mehra A, Ardhanari S. Prog Cardiovasc Dis. 2014;56:391–400. doi: 10.1016/j.pcad.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Impact of obesity in hospitalized patients with heart failure: a nationwide cohort study. Gajulapalli RD, Kadri A, Gad M, Chahine J, Nusairat L, Rader F. South Med J. 2020;113:568–577. doi: 10.14423/SMJ.0000000000001174. [DOI] [PubMed] [Google Scholar]
- 12.Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Haase CL, Lopes S, Olsen AH, Satylganova A, Schnecke V, McEwan P. Int J Obes (Lond) 2021;45:1249–1258. doi: 10.1038/s41366-021-00788-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Influence of obesity and malnutrition on acute heart failure. Zapatero A, Barba R, Gonzalez N, et al. Rev Esp Cardiol (Engl Ed) 2012;65:426–410. doi: 10.1016/j.recesp.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 14.A study on prevalence of dyslipidemia in obese patients in a teaching hospital in Kerala. Jacob BS, Balachandran J, Paul VB. http://saspublisher.com/wp-content/uploads/2014/03/SJAMS-22B642-646.pdf J Appl Med Sci. 2014;2:2014–2013. [Google Scholar]
- 15.Obesity and age of first non-ST-segment elevation myocardial infarction. Madala MC, Franklin BA, Chen AY, et al. J Am Coll Cardiol. 2008;52:979–985. doi: 10.1016/j.jacc.2008.04.067. [DOI] [PubMed] [Google Scholar]
- 16.The obesity paradox in non-ST-segment elevation acute coronary syndromes: results from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative. Diercks DB, Roe MT, Mulgund J, et al. Am Heart J. 2006;152:140–148. doi: 10.1016/j.ahj.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Prevalence of 'hypertriglyceridemic waist' in men who participated in the Quebec Health Survey: association with atherogenic and diabetogenic metabolic risk factors. Lemieux I, Alméras N, Mauriège P, Blanchet C, Dewailly E, Bergeron J, Després JP. https://pubmed.ncbi.nlm.nih.gov/12167959/ Can J Cardiol. 2002;18:725–732. [PubMed] [Google Scholar]
- 18.Obesity in patients with non-ST-segment elevation acute coronary syndromes: results from the SYNERGY trial. Mahaffey KW, Tonev ST, Spinler SA, et al. Int J Cardiol. 2010;139:123–133. doi: 10.1016/j.ijcard.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Jung UJ, Choi MS. Int J Mol Sci. 2014;15:6184–6223. doi: 10.3390/ijms15046184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Relation between body mass index, waist circumference, and death after acute myocardial infarction. Zeller M, Steg PG, Ravisy J, et al. Circulation. 2008;118:482–490. doi: 10.1161/CIRCULATIONAHA.107.753483. [DOI] [PubMed] [Google Scholar]
- 21.Influence of obesity on morbidity and mortality after acute myocardial infarction. Hoit BD, Gilpin EA, Maisel AA, Henning H, Carlisle J, Ross J Jr. Am Heart J. 1987;114:90534–90539. doi: 10.1016/0002-8703(87)90534-5. [DOI] [PubMed] [Google Scholar]
- 22.Study on correlation of obesity with short-term prognosis in acute myocardial infarction. Haridasan V, Rajesh KF, Sajeev CG, et al. Indian Heart J. 2016;68:306–310. doi: 10.1016/j.ihj.2015.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Impact of body mass index on in-hospital outcomes after percutaneous coronary intervention for ST segment elevation acute myocardial infarction. Kosuge M, Kimura K, Kojima S, et al. Circ J. 2008;72:521–525. doi: 10.1253/circj.72.521. [DOI] [PubMed] [Google Scholar]
- 24.The effect of obesity on health outcomes. Dixon JB. Mol Cell Endocrinol. 2010;316:104–108. doi: 10.1016/j.mce.2009.07.008. [DOI] [PubMed] [Google Scholar]