Abstract
Background:
Young adults and other working-age adults with cancer are at risk for cancer-related financial toxicity (FT), including material hardships, depletion of coping resources, and psychological burden. We compared these FT domains in young adults (age 18–39 years) (YAs), other working-age adults (age 40–64 years), and older adults (age ≥65 years) receiving cancer care.
Methods:
We surveyed 311 adults using the multi-domain Economic Strain and Resilience in Cancer (ENRICh) instrument measuring FT (0–10 score indicating least to greatest FT; score ≥5 severe FT). Participants were receiving ambulatory care from March-September 2019. Associations of age with overall FT and material hardship, coping resource depletion, and psychological burden FT domains were tested using Kruskal-Wallis and Chi-square tests and multivariable generalized linear models with gamma distribution.
Results:
YAs (median age 31.5) comprised 9.6% of the sample; other working-age adults comprised 56.9%. Overall, material, coping, and psychological FT scores were worse in younger age adults vs. older adults (P<0.001 in all multivariable models). Compared with older adults, younger age adults demonstrated worse material hardship (median scores 3.70 vs. 4.80 vs. 1.30 for YAs, other working-age, and older adults, respectively; P<0.001), coping resource depletion (4.50 vs. 3.40 vs. 0.80; P<0.001), and psychological burden (6.50 vs. 7.00 vs. 1.00; P<0.001). Fifty percent of YAs had severe overall FT vs. 40.7% of other working-age adults and 9.6% of older adults (P<0.001).
Conclusion:
Younger age adults with cancer bore disproportionate FT. Interventions to address unmet needs are critical components for addressing FT in this population.
Keywords: Young Adult, Financial Toxicity, Neoplasms, Cancer Survivors, Healthcare Disparities
Precis:
Young adults (18–39 years old) and other working-age adults (40–64 years old) with cancer experienced disproportionately greater financial toxicity compared with older adult (≥65 years old) counterparts. These younger adults faced not only severe material hardships, but also severe depletion of their coping resources as well as psychological burden from their cancer-related financial stressors.
INTRODUCTION
Working-age adults, including young adults (YAs), with cancer have high out-of-pocket medical costs compared with working-age adults and YAs without cancer.1,2 These excess costs render younger patients at high risk for cancer-related financial hardship and “financial toxicity” (FT).3, 4 Several prior studies of adolescent and YA cancer survivors indicated especially severe and persistent financial concerns long after a cancer diagnosis. For example, in the Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) study, 51%, 70%, and 65% of cancer survivors aged 15 – 20, 21 – 29, and 30 – 39 years old, respectively, reported experiencing a negative financial impact of their disease.5 In another study, YA survivors identified financial concerns as one of their leading unmet survivorship needs.6
FT is a multidimensional problem and incorporates not only material (monetary) hardships, such as accumulating out-of-pocket costs and medical debt during and after receiving cancer care, but also accompanying psychosocial hardships. These include strain/drain on individuals’ coping resources, which leads to economizing responses, such as reduced spending on food and skipping medications, and psychological burden, such as distress and anxiety about cancer-related financial stressors. Moreover, these psychosocial consequences associated with FT can impact individuals’ wellbeing across the cancer care continuum, from active cancer treatment to survivorship.3, 7–10
Evidence suggests that younger individuals with cancer, especially YAs, are particularly vulnerable to psychosocial distress that may exacerbate risk for and consequences of financial hardship.1 Younger individuals with cancer have comparatively lower financial reserves, less financial literacy, and more extreme vocational disruption than older individuals. These problems may be exacerbated by less robust psychosocial coping skills and shifting social support sources in younger individuals.11 Thus, FT assessment and intervention in cancer care delivery settings for individuals in younger, higher-risk age groups may warrant targeting multiple domains of FT, including its psychosocial aspects.11
Informing the design of multidimensional, targeted FT assessment and intervention strategies for future routine implementation in cancer care requires a comprehensive analysis of the spectrum, severity, and comparative impact of the multiple domains of FT among younger age individuals (<65 years), especially in the sub-population of YAs (18–39 years), since they face unique financial and psychosocial challenges. Early in the cancer care/survivorship trajectory—during treatment and early follow-up— is a phase in care when patients have high healthcare utilization (and expenses) and interact closely and frequently with providers. This is also a phase when early FT intervention may minimize downstream adverse effects of FT, such as accumulation of medical debt and non-adherence to curative cancer care.7, 10, 12 Accordingly, in this survey study, we sought to quantify and compare the domains and severity of the material, coping, and psychological FT burdens early in the care and survivorship trajectory for working-age adults (including YA age 18–39 years and other working-age adults age 40–64 years) and older adults with cancer.
MATERIALS AND METHODS
Study Sample
The study sample was derived from Economic Strain and Resilience in Cancer13 study, which included individuals with cancer receiving ambulatory oncology care between March and September 2019. Individuals eligible for this study were age ≥18, had confirmed diagnosis of cancer, and were undergoing ambulatory cancer care (i.e., active cancer treatment or follow-up/surveillance care) at participating oncology clinics within the larger Houston metropolitan area. Participating sites included an academic National Cancer Institute (NCI)-designed comprehensive cancer hospital and one of the center’s regional affiliated community oncology clinics, and a county medical safety-net clinic in the community setting that provides medical financial assistance for individuals with a household income <150% of the Federal Poverty Level. Patients were invited in-person to participate in this survey from participating medical, surgical, or radiation oncology clinics after screening for eligibility.14, 15 Of 491 patients invited, 312 agreed to participate (recruitment response rate 63.5%). Patients who did not answer >50% survey questions (N=1) were omitted, leaving an analytic sample of 311 patients. This study was approved by the Institutional Review Board at the University of Texas M. D. Anderson Cancer Center.
Measuring Financial Toxicity (FT)
The 15-item Economic Strain and Resilience in Cancer (ENRICh) instrument measures patient-reported FT, 14,15, 16 including an overall FT score as well as subscore domains of 1) material hardship such as out-of-pocket costs, spent savings, and lost income; 2) depletion of coping resources such as employment benefits, professional assistance resources from formal organizations, and instrumental help from family and friends; and 3) severity of psychological burdens, such as stress related to finances. These three conceptual domains have been previously identified as comprising FT.3, 9
Each item was scored on a 0 to 10 scale.13 Overall FT score (all items) and the material FT, coping, FT, and psychological FT item subscores were calculated as an arithmetic average of item scores (re-weighted for missing items). The score for overall FT and subscore FT ranged from 0 – 10 (least to most severe FT burden). In analyses, this was tested as a continuous variable as well as a dichotomous variable categorized as “severe” (score ≥5) vs. “not severe” (<5), based on a scoring threshold identified in a prior study associated with adverse care delivery outcomes.12
Age
Participant age at the time of survey completion was calculated based on the date of birth abstracted from the electronic medical record. Patients aged 18–39 years were defined as YA, per current clinical guidelines.17–19 Older adults were defined as ≥65 years based on age-eligibility for Medicare insurance coverage.4, 9, 19, 20 We conducted secondary exploratory analyses on more specific age group categories (18–26, 27–39, 40–54, 55–64, ≥65), to explore for differences in FT by more granular subgroups. The youngest subgroup was defined based on differences developmentally21, 22 and eligibility for parental insurance under the Affordable Care Act.19
Other Covariates
Survey participants reported annual household income, health insurance coverage (including public (Medicaid or Medicare), private (employer-purchased or self-purchased), or uninsured) and highest attained education level. Other clinical and demographic covariates were abstracted from the electronic medical record, including gender, race and Hispanic ethnicity, cancer disease site (e.g., breast, lung, prostate, etc.), cancer stage at diagnosis, and treatment setting (comprehensive care center clinics or county safety net clinic). Categories in univariable and multivariable analyses were collapsed based on distributions.
Statistical Analysis
The univariable associations between age groups and continuous overall FT scores and FT subscores were tested using the Kruskal-Wallis test. Trends in FT scores across ordinal age groups were tested using the Jonckheere’s test. Univariable associations for FT scores and the primary analysis categories for age groups, 18–39 vs. 40–64 vs. ≥65 years, were tested using the Wilcoxon Rank Sum and Kruskal-Wallis test. Other correlations between patient characteristic covariates and overall FT scores were tested using the Kruskal-Wallis test or Wilcoxon Rank Sum test for categorical variables and Spearman’s correlation coefficient for continuous variables.
Multivariable generalized linear regression models with gamma distribution were used to test the associations between age group and overall FT and material, coping, and psychological FT scores, adjusted for clinical and demographic covariates retained in the model that initially demonstrated univariate associations with P<0.25. The Likelihood ratio test was used to examine for the overall effect of age in the multivariable models.
In secondary analyses, we performed exploratory analyses to describe the associations between age and FT outcomes using the specific age group categories (18–26, 27–39, 40–54, 55–64, ≥65). We also tested sensitivity models using the dichotomized FT outcome of severe (≥5) vs. no severe (<5) FT score. Analyses were conducted using SAS Enterprise Guide version 7.11 (Cary, NC). Statistical tests were two-sided with p-value < 0.05 considered statistically significant.
RESULTS
Among 311 survey participants, 30 (9.6%) were aged 18–39, 177 (47%) were 40–64, and 104 (33.4%) were ≥65. A total of 80 (25.7%) received care in the medical safety net community oncology setting. A majority were female (57.2%) and non-Hispanic White (59.8%), and 30.6% had distant metastatic cancer at the time of cancer diagnosis and the most common disease site was breast cancer (35.7%). The median time from diagnosis to survey (FT assessment) for all participants was 7.4 months (IQR 3.4, 13.2). Other key patient characteristics are summarized in Table 1. Univariable associations of clinical and demographic characteristics by age categories are summarized in Supporting Table 1.
Table 1:
Study sample demographic and clinical characteristics (N=311).
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| 18–39 | 30 (9.6%) |
| 40–64 | 177 (57.0%) |
| ≥65 | 104 (33.4%) |
| Median age (years, IQR) | 60 (51 – 68) |
| Gender | |
| Female | 178 (57.2%) |
| Male | 133 (42.8%) |
| Race/Ethnicity | |
| White, Non-Hispanic | 186 (59.8%) |
| Black, Non-Hispanic | 61 (19.6%) |
| Hispanic | 52 (16.7%) |
| Othera | 12 (3.9%) |
| Education Level | |
| Less than High School | 18 (5.8%) |
| High School or GED | 73 (32.5%) |
| Associate Degree or Trade Certification | 122 (39.2%) |
| College Degree | 61 (19.6%) |
| Graduate Degree | 23 (7.4%) |
| Advanced Degree | 13 (4.2%) |
| No Response | 1 (0.3%) |
| Employment | |
| Full-time | 75 (24.1%) |
| Part-time | 15 (4.8%) |
| Unemployed or Disabled | 87 (28%) |
| Retired | 91 (29.3%) |
| Other/No Response | 43 (13.8%) |
| Income | |
| $0 – $19,999 | 69 (22.2%) |
| $20,000 – $49,999 | 66 (21.2%) |
| $50,000 – $99,999 | 77 (24.8%) |
| $100,000 – $199,999 | 54 (17.4%) |
| $200,000 or more | 37 (11.9%) |
| No Response | 8 (2.6%) |
| Insurance Status | |
| Private employer-based | 110 (35.4%) |
| Private marketplace purchased | 20 (6.4%) |
| Medicare | 112 (36%) |
| Medicaid/state or none | 69 (22.2%) |
| Treatment Setting | |
| Medical safety net clinic | 80 (25.7%) |
| Academic center | 311 (74.3%) |
| Cancer Type | |
| Breast | 111 (35.7%) |
| Gastrointestinal | 42 (13.5%) |
| Lung | 31 (10%) |
| Prostate | 31 (10%) |
| Head and neck | 29 (9.3%) |
| Hematologicb | 23 (7.4%) |
| Gynecologic | 7 (2.3%) |
| Central nervous system | 4 (1.3%) |
| Soft tissue | 7 (2.3%) |
| Thyroid | 1 (0.3%) |
| Otherc | 25 (8.0%) |
| Disease Stage at Diagnosis | |
| Local | 111 (38.1%) |
| Regional | 91 (31.3%) |
| Distant | 89 (30.6%) |
Other includes: Asian, Native American, Other, and no response.
Hematologic malignancies include: leukemia, lymphoma, myeloma.
Other includes: Neuroendocrine, non-prostate genitourinary, skin, and thymic cancers.
Abbreviations: interquartile range (IQR), high school equivalency diploma (GED).
FT and age.
Median overall FT score (Table 2) as well as material, coping, and psychological FT scores (Figure 1) were significantly worse for individuals in younger age groups (18–39, 40–64) compared to those ≥65 years (Kruskal-Wallis P<0.001 for all comparisons). In exploratory analysis, the limited sample of patients age 18–26 similarly had trends for worse overall, material, coping, and psychological FT scores (Supporting Table 2).
Table 2:
Overall financial toxicity (FT) score distributions by study participant characteristics (N=311). Higher score indicates worse FT. P-value is reported for the Kruskal-Wallis test comparing scores by group.
|
Characteristic |
Median Overall Financial Toxicity Score | IQR | P-Valuea |
|---|---|---|---|
| Age | <0.001 | ||
| 18–39 | 4.6 | 2.0 – 7.1 | |
| 40–64 | 4.2 | 2.1 – 6.3 | |
| ≥65 | 1.3 | 0.2 – 3.1 | |
| Gender | 0.21 | ||
| Female | 3.5 | 1.6 – 5.7 | |
| Male | 2.8 | 1.0 – 5.4 | |
| Race/Ethnicity | <0.001 | ||
| White, Non-Hispanic | 2 | 0.5 – 4.4 | |
| Black, Non-Hispanic | 5 | 3.6 – 7.3 | |
| Hispanic | 4 | 2.2 – 6.7 | |
| Otherb | 6.3 | 2.8 – 8.1 | |
| Education Level | 0.001 | ||
| Less than High School | 3.5 | 2.5 – 5.3 | |
| High School or GED | 3.9 | 1.5 – 5.9 | |
| Associate Degree or Trade Certification | 3.9 | 1.7 – 6.4 | |
| College Degree | 2.8 | 0.6 – 5.1 | |
| Graduate Degree | 1.8 | 1.0 – 3.1 | |
| Advanced Degree | 1.3 | 0.3 – 2.4 | |
| Employment | <0.001 | ||
| Full-time | 2.5 | 1.0 – 4.7 | |
| Part-time | 5.2 | 2.4 – 7.3 | |
| Unemployed or Disabled | 5.4 | 3.4 – 7.3 | |
| Retired | 1.3 | 0.2 – 3.4 | |
| Other/No Response | 3.3 | 1.6 – 5.7 | |
| Income | <0.001 | ||
| $0 – $19,999 | 5.3 | 2.5 – 7.3 | |
| $20,000 – $49,999 | 4.5 | 2.0 – 6.4 | |
| $50,000 – $99,999 | 2.9 | 0.7 – 5.2 | |
| $100,000 – $199,999 | 1.8 | 0.6 – 3.2 | |
| $200,000 or more | 1.2 | 0.5 – 3.4 | |
| No Response | 4.5 | 2.7 – 8.5 | |
| Insurance Status | <0.001 | ||
| Private employer-based | 3.2 | 1.3 – 5.1 | |
| Private marketplace purchased | 4.5 | 2.1 – 6.3 | |
| Medicare | 1.8 | 0.3 – 3.9 | |
| Medicaid/state or none | 5.4 | 3.4 – 7.1 | |
| Cancer Type | 0.003 | ||
| Breast | 3.1 | 1.4 – 5.4 | |
| Gastrointestinal | 4.2 | 1.7 – 6.2 | |
| Lung | 3.4 | 1.3 – 5.6 | |
| Prostate | 1.7 | 0.3 – 2.6 | |
| Head and neck | 2.4 | 0.6 – 5.3 | |
| Hematologicc | 4.6 | 1.3 – 7.3 | |
| Gynecologic | 1.9 | 1.3 – 4.1 | |
| Central nervous system | 3.5 | 1.8 – 6.0 | |
| Soft tissue | 7.7 | 3.3 – 9.5 | |
| Thyroid | 7.5 | 7.5 – 7.5 | |
| Otherd | 4.0 | 1.7 – 5.4 | |
| Disease Stage | <0.001 | ||
| Local | 2.0 | 0.4 – 4.2 | |
| Regional | 3.5 | 1.3 – 5.3 | |
| Distant | 4.5 | 2.5 – 6.7 |
The p-value represents the results of a Kruskal-Wallis test.
Other includes: Asian, Native American, Other, and no response.
Hematologic malignancies include: leukemia, lymphoma, myeloma.
Other includes: Neuroendocrine, non-prostate genitourinary, skin, and thymic cancers.
Abbreviations: interquartile range (IQR), high school equivalency diploma (GED).
Figure 1:
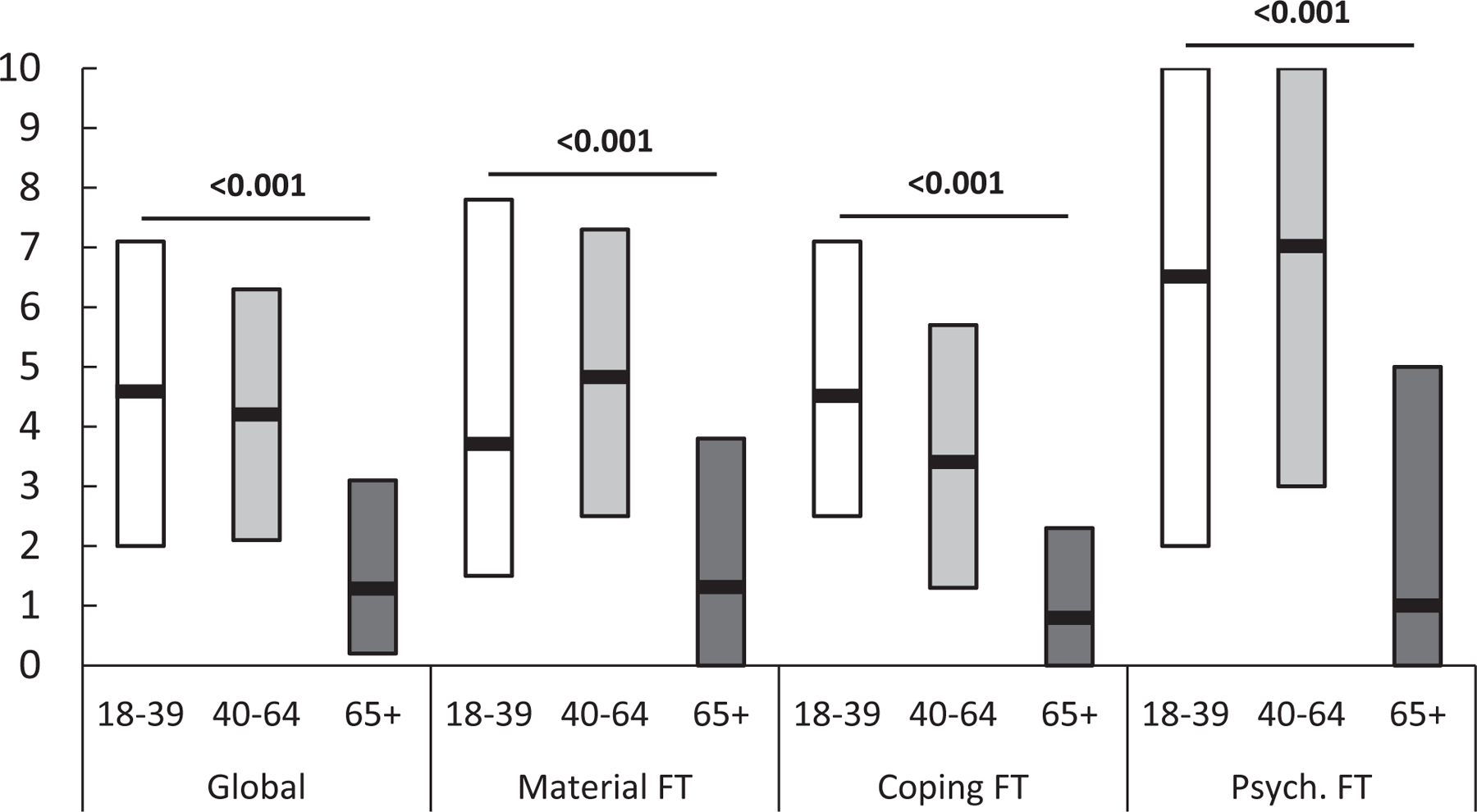
Median financial toxicity (FT) scores and interquartile range, across domains (overall, by age groups (age 18–39, 49–64, and ≥54 years), compared across 3 groups using the Kruskal-Wallis test. Higher scores indicate more severe FT.
After adjusting for demographic and clinical covariates, there remained an increased risk for higher overall FT scores among younger adult age groups: RR=1.95, 95% CI 1.36–2.80, P<0.001 for adults age 18–39; and RR=1.93, 95% CI 1.56–2.38, P<0.001 for age 40–64, compared with age ≥65. Additional RRs for material, coping, and psychological FT are presented in Table 3, demonstrating significantly worse scores for each FT domain (material, coping, and psychological domains) among the younger age groups. There was no difference in risk for overall, material, coping, and psychological FT between the two working-age groups (age 18–39 vs. 40–64); overall FT RR=1.01, 95% CI 0.72–1.41, p=0.94; material FT RR=0.89, 95% CI 0.60–1.32, p=0.56; coping FT RR=1.17, 95% CI 0.81–1.69, p=0.41; psychological FT RR=0.92, 95% CI 0.59–1.45, p=0.73. In these models, other significant covariate predictors of FT varied depending on the FT domain outcome modeled, and included distant metastatic disease at diagnosis, minority race or ethnicity, lower educational attainment, and treatment setting (Supporting Table 3a-d).
Table 3.
Multivariable models: Adjusted risk ratios for financial toxicity (FT) score (across the score range of 0 to 10) by age categories (N=311).
| Age Category (years) |
Overall FT RR (95% CI)a |
Material FT RR (95% CI)a |
Coping FT RR (95% CI)a |
Psychological FT RR (95% CI)a |
|---|---|---|---|---|
| ≥ 65 | Reference | Reference | Reference | Reference |
| 40–64 | 1.93 (1.56–2.38) | 1.92 (1.50–2.47) | 1.89(1.50–2.39) | 2.01(1.50–2.69) |
| 18–39 | 1.95 (1.36–2.81) | 1.71 (1.12–2.63) | 2.21(1.49–3.28) | 1.85(1.13–3.03) |
| P-valuea | <0.001 | <0.001 | <0.001 | <0.001 |
The p-value represents the results of the likelihood ratio test for age. Covariates included: race/ethnicity, gender, education, insurance, treatment facility, and disease stage.
Abbreviations: risk ratio (RR), confident interval (CI), financial toxicity (FT).
Severe FT in younger adults.
Fifty percent of YAs, age 18–39 years, had severe (score ≥5) overall FT vs. 40.7% of adults age 40–64 and 9.6% of adults age ≥65 (P<0.001). In sensitivity analyses using the dichotomous FT outcome (severe vs. not severe FT), there was increased likelihood of severe FT across younger groups: adjusted odds ratio [OR]=5.84, 95% CI 2.07–16.5, P<0.001 for adults age 18–39; and OR=4.58, 95% CI 2.16–9.72, P<0.001 for age 40–64, compared with the referent group of age ≥65. YAs also frequently encountered severe FT across the separate domains: 47% reported severe material, 47% severe coping, and 70% severe psychological FT burden.
On sensitivity analyses, in multivariable models, the increased likelihood of severe FT remained for both younger age groups (YAs and other working-age adults) compared with the referent group of older adults. For severe material FT: in YAs, OR=4.08, 95% CI 1.58–10.53, P=0.004; in other working-age adults, OR=4.57, 95% CI 2.43–8.57, P<0.001. For severe coping FT: in YAs, OR=6.54, 95% CI 1.94–21.99, P=0.002; in other working-age adults, OR=4.38, 95% CI 1.70–11.32, P=0.002. For severe psychological FT: in YAs, OR=3.78, 95% CI 1.41–10.13, P=0.008; in other working-age adults, OR=4.54, 95% CI 2.52–8.17, P<0.001.
DISCUSSION
Among patients receiving cancer care in diverse ambulatory treatment settings, younger cancer patients and survivors demonstrated significantly worse multidimensional aspects of FT. These included worse material hardship, coping resource depletion, and psychological burden compared with older adults age ≥65 years. Confounding effects of minority race/ethnicity, lower educational attainment, lower household income, uninsurance, and medical safety net treatment setting, and diagnosis of cancer at later stage among younger patients partly explained worse FT scores across the younger age spectrum. Yet even after adjustment for these covariates, there was persistently increased risk of FT for participants age 18–39 and 40–64 years compared with older participants age ≥65 years, suggesting other unaccounted factors—socioeconomic, psychosocial, and/or clinical— that further contribute to the complex, multidimensional high-risk FT profile in younger individuals with cancer. A prior study from the National Health Interview Survey3 found that significantly more longer-term cancer survivors aged 18–49 years—approximately 70%— reported any financial hardships compared with approximately 39% of survivors ≥65 years. Our study adds to available evidence by quantifying separate domains of FT experienced by younger individuals in active treatment and early survivorship and accounts for sociodemographic and clinical patient-level covariate characteristics. These specific FT domains are critical to understand and tailor interventions around material hardship, coping burden, and psychological burden for this vulnerable population. Additionally, our study identified that severe FT was highly prevalent among these younger groups during both active treatment and early survivorship.
Effective interventions mitigating FT within care delivery settings remain elusive. An existing model for FT intervention is through “financial navigation”, a strategy to proactively provide treatment cost estimates, budget support, and direct monetary assistance (e.g., copay assistance or insurance maximization, medication assistance, as well as assistance from community resources to help address other social needs (e.g., transportation and housing issues) during treatment or clinical trial participation.23 Early data from ongoing prospective studies suggest that financial navigation alone may only modestly impact the severity of FT scores,24–26 and therefore the efficacy of FT interventions may need further advancement by magnifying targets for coping and psychological FT domains. Data from our present analysis support a strong need to enhance the current model of intervention of financial navigation alone by layering intervention components that specifically address psychosocial distress and provide patients with relevant coping strategies. Kirchoff and Jones recently proposed a model for FT intervention that tailors not only to patients’ socioeconomic and clinical characteristics but also to material and psychological domains of FT as they affect patient health outcomes.27 Our study results support this model of intervention, demonstrating significant impacts of socioeconomic and clinical characteristics, along with patient age, across material, coping, and psychological FT measures.
Nevertheless, a persistent challenge will be adapting and implementing successful intervention models across care settings. Specialty centers, such as a large comprehensive academic center, may have more specialized resources for younger and YA patients, while community-based or underserved settings may have limitations on such resources. This is of concern as the majority of YAs receive their cancer care in the community setting.28
Younger individuals, especially those designated in the YA cancer population (age 18–39) remain a population with a recognized spectrum of persistently unmet needs—including management of symptoms, emotional, and social needs.29 In the present study, YAs demonstrated frequent and severe burden from the coping and psychosocial components/domains of FT, much more than compared to older adults.30, 31 YAs and younger working age adults both can face high out-of-pocket care costs, job loss, disability, and medical debt. The youngest of survivors may be especially vulnerable with lower financial reserves to meet financial demands.32–35 Economizing behaviors in younger age cancer patients and survivors, such as sacrificing material or basic needs, appropriate healthcare, and/or social activities, could have adverse synergistic effects with other unmet psychosocial needs in this group.11 There was a limited number of individuals in the youngest subset, age 18 – 26 years. However, descriptively, in our exploratory description of this group, median scores across all FT domains remained high, emphasizing a need to for future investigation focused on this group. In a recent study of FT specifically within YAs with cancer during the COVID-19 pandemic, economizing behaviors were more prevalent in the context of pandemic-related financial stressors and were associated with worse FT.36 Thus, patient-level interventions to address the coping and psychological domains of FT in YAs with cancer are warranted and timely.
While offering patient-level intervention resources is important to help mitigate FT, other simultaneous advances are needed. In care delivery, implementation of multidimensional FT assessment and screening need to be age-appropriate and cancer phase-appropriate.11 Establishing guidance on quality practice for FT screening needs to be defined, for example, with systematic FT screening and methods for documenting FT at initial clinical encounters and periodic reassessments throughout care to guide and engage the healthcare team’s response to patient FT.37–39 In addition, collection of FT measures should be embedded in the design phase of clinical trials and prospective clinical studies alongside other patient-reported-outcome (PRO) measures to proactively define the comprehensive toxicity profile of new therapeutic options, especially in those at high risk for FT such as younger patients,40 who face distinct stressors such as onco-fertility costs41 and vocational challenges that impact stability of insurance.42 Broad scale collection of these data are critical for informing future targeted policy changes, such as continued uptake of state initiatives to mandate coverage of onco-fertility in YAs41 and incorporating FT screening as a quality measure linked to value-based or performance-based payment. Ultimately, policies to address the root causes of FT are needed, specifically to regulate the growth in the cost of cancer treatments and limit the increase in cost-sharing requirement of private insurance.
This study has limitations. Though the study was multi-site and sought to include a diverse sample, it was carried out in a single large metropolitan area in a non-Medicaid expansion state in cross sectional design. Therefore, future validation of findings in other settings, including other cancer treatment settings, will be needed to increase generalizability. Additionally, longitudinal studies are needed to explicitly characterize changes in FT domains and needs in acute cancer delivery through long-term survivorship to expand the evidence base on changes in the magnitude, severity, and domains of FT over time. Finally, given that the cognitive sequelae of disease and its treatment may impact psychosocial functioning and needs, larger studies inclusive of young patients with additional cancer types such as central nervous system (CNS) cancers will be needed to broaden applicability of these initial findings.
CONCLUSION
In this investigation, working-age adults, including YAs, with cancer bore disproportionate FT, including across coping and psychological domains of FT. Comprehensive mitigation strategies that target multiple FT domains early in the care delivery trajectory are needed to help address unmet needs of younger, high-risk individuals. Current strategies to address unmet psychosocial needs during cancer treatment delivery and survivorship may further serve as a critical component to mitigate FT in vulnerable younger individuals with cancer.
Supplementary Material
Funding:
GLS is supported by the National Cancer Institute (NIH/NCI K07CA211804) and by the Andrew Sabin Family Fellowship. This research was supported in part by the MD Anderson Cancer Center grant P30 CA016672 and used the Decision Science Shared Resource. RMC is supported by grants from the Leukemia and Lymphoma Society and the American Cancer Society.
Footnotes
Conflicts of Interest: K. Robin Yabroff is employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector, for research outside the submitted work. She is not funded by or key personnel for any of these grants, and her salary is solely funded through American Cancer Society funds. The other authors made no disclosures.
REFERENCES
- 1.Lu AD, Zheng Z, Han X, et al. Medical Financial Hardship in Survivors of Adolescent and Young Adult Cancer in the United States. J Natl Cancer Inst 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guy GP Jr, Yabroff KR, Ekwueme DU, et al. Estimating the health and economic burden of cancer among those diagnosed as adolescents and young adults. Health Aff (Millwood) 2014;33: 1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zheng Z, Jemal A, Han X, et al. Medical financial hardship among cancer survivors in the United States. Cancer 2019;125: 1737–1747. [DOI] [PubMed] [Google Scholar]
- 4.Yabroff KR, Zhao J, Han X, Zheng Z. Prevalence and Correlates of Medical Financial Hardship in the USA. J Gen Intern Med 2019;34: 1494–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellizzi KM, Smith A, Schmidt S, et al. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer 2012;118: 5155–5162. [DOI] [PubMed] [Google Scholar]
- 6.Pannier ST, Warner EL, Fowler B, Fair D, Salmon SK, Kirchhoff AC. Age-Specific Patient Navigation Preferences Among Adolescents and Young Adults with Cancer. J Cancer Educ 2019;34: 242–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith GL, Lopez-Olivo MA, Advani PG, et al. Financial Burdens of Cancer Treatment: A Systematic Review of Risk Factors and Outcomes. J Natl Compr Canc Netw 2019;17: 1184–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR. Medical Financial Hardship Intensity and Financial Sacrifice Associated with Cancer in the United States. Cancer Epidemiol Biomarkers Prev 2020;29: 308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yabroff KR, Dowling EC, Guy GP Jr., et al. Financial Hardship Associated With Cancer in the United States: Findings From a Population-Based Sample of Adult Cancer Survivors. J Clin Oncol 2016;34: 259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banegas M, Guy G, de Moor J. For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff (Millwood) 2016;35: 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salsman JM, Bingen K, Barr RD, Freyer DR. Understanding, measuring, and addressing the financial impact of cancer on adolescents and young adults. Pediatr Blood Cancer 2019;66: e27660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maldonado JA, Fu S, Chen YS, et al. Sensitivity of Psychosocial Distress Screening to Identify Cancer Patients at Risk for Financial Hardship During Care Delivery. JCO Oncol Pract 2021: OP2001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith GL, Mendoza TR, Lowenstein LM, Shih YT. Financial Hardship in Survivorship Care Delivery. J Natl Cancer Inst Monogr 2021;2021: 10–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith GL, Lowenstein LM, Peterson SK, et al. Financial toxicity of cancer care: Defining pathways of decline vs resilience. Journal of Clinical Oncology 2018;36: e22150–e22150. [Google Scholar]
- 15.Smith GL, Volk RJ, Lowenstein LM, et al. ENRICH: Validating a multidimensional patient-reported financial toxicity measure. J Clin Oncol 2019;37: 153–153.30457921 [Google Scholar]
- 16.de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the COmprehensive Score for financial Toxicity (COST). Cancer 2017;123: 476–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Closing the Gap: Research and Care Imperatives for Adolescents and Young Adults with Cancer—Report of the Adolescent and Young Adult Oncology Progress Review Group: National Cancer Institute: U.S. Department of Health and Human Services, 2006. [Google Scholar]
- 18.Adolescents and Young Adults with Cancer, V1.2021 NCCN Guidelines: National Comprehensive Cancer Network, 2020. [Google Scholar]
- 19.Young Adults and the Affordable Care Act: Protecting Young Adults and Eliminating Burdens on Businesses and Families FAQs Available from URL: https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/faqs/young-adult-and-aca [accessed September 27, 2020].
- 20.Johnson R. Why the “average age of retirement” is a misleading measure of labor supply. Monthly Labor Review 2001: 38–40. [Google Scholar]
- 21.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 2000;55: 469–480. [PubMed] [Google Scholar]
- 22.Young Adults and the Affordable Care Act: Protecting Young Adults and Eliminating Burdens on Businesses and Families FAQs Available from URL: https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/faqs/young-adult-and-aca.
- 23.Yezefski T, Steelquist J, Watabayashi K, Sherman D, Shankaran V. Impact of trained oncology financial navigators on patient out-of-pocket spending. Am J Manag Care 2018;24: S74–S79. [PubMed] [Google Scholar]
- 24.Nipp RD, Lee H, Gorton E, et al. Addressing the Financial Burden of Cancer Clinical Trial Participation: Longitudinal Effects of an Equity Intervention. Oncologist 2019;24: 1048–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sadigh G, Gallagher K, Obenchain J, et al. Pilot Feasibility Study of an Oncology Financial Navigation Program in Brain Cancer Patients. J Am Coll Radiol 2019;16: 1420–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watabayashi K, Steelquist J, Overstreet KA, et al. A Pilot Study of a Comprehensive Financial Navigation Program in Patients With Cancer and Caregivers. J Natl Compr Canc Netw 2020;18: 1366–1373. [DOI] [PubMed] [Google Scholar]
- 27.Kirchhoff A, Jones S. Financial Toxicity in Adolescent and Young Adult Cancer Survivors: Proposed Directions for Future Research. J Natl Cancer Inst 2021;113: 948–950. [DOI] [PubMed] [Google Scholar]
- 28.Yeager ND, Hoshaw-Woodard S, Ruymann FB, Termuhlen A. Patterns of care among adolescents with malignancy in Ohio. J Pediatr Hematol Oncol 2006;28: 17–22. [PubMed] [Google Scholar]
- 29.Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv 2012;6: 239–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Banegas MP, Schneider JL, Firemark AJ, et al. The social and economic toll of cancer survivorship: a complex web of financial sacrifice. J Cancer Surviv 2019;13: 406–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thom B, Benedict C. The Impact of Financial Toxicity on Psychological Well-Being, Coping Self-Efficacy, and Cost-Coping Behaviors in Young Adults with Cancer. J Adolesc Young Adult Oncol 2019;8: 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaul S, Avila JC, Mehta HB, Rodriguez AM, Kuo YF, Kirchhoff AC. Cost-related medication nonadherence among adolescent and young adult cancer survivors. Cancer 2017;123: 2726–2734. [DOI] [PubMed] [Google Scholar]
- 33.Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol 2012;30: 2393–2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parsons SK, Kumar AJ. Adolescent and young adult cancer care: Financial hardship and continued uncertainty. Pediatr Blood Cancer 2019;66: e27587. [DOI] [PubMed] [Google Scholar]
- 35.Thom B, Benedict C, Friedman DN, Kelvin JF. The intersection of financial toxicity and family building in young adult cancer survivors. Cancer 2018;124: 3284–3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thom B, Benedict C, Friedman DN, Watson SE, Zeitler MS, Chino F. Economic distress, financial toxicity, and medical cost-coping in young adult cancer survivors during the COVID-19 pandemic: Findings from an online sample. Cancer 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jagsi R, Ward KC, Abrahamse PH, et al. Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer 2018;124: 3668–3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bradley CJ, Yabroff KR, Shih YT. A Coordinated Policy Approach to Address Medical Financial Toxicity. JAMA Oncol 2021;7: 1761–1762. [DOI] [PubMed] [Google Scholar]
- 39.Bradley CJ, Yabroff KR, Zafar SY, Shih YT. Time to add screening for financial hardship as a quality measure? CA Cancer J Clin 2021;71: 100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berkman AM, Murphy KM, Siembida EJ, et al. Inclusion of Patient-Reported Outcomes in Adolescent and Young Adult Phase III Therapeutic Trials: An Analysis of Cancer Clinical Trials Registered on ClinicalTrials.gov. Value Health 2021;24: 1820–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Omesi L, Narayan A, Reinecke J, Schear R, Levine J. Financial Assistance for Fertility Preservation Among Adolescent and Young Adult Cancer Patients: A Utilization Review of the Sharing Hope/LIVESTRONG Fertility Financial Assistance Program. J Adolesc Young Adult Oncol 2019;8: 554–559. [DOI] [PubMed] [Google Scholar]
- 42.Siegel RD, Slough RG, Crosswell HE, et al. Drug Recovery and Copay Assistance Program in a Community Cancer Center: Charity and Challenges. J Oncol Pract 2019;15: e628–e635. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


