Abstract
Maternal posttraumatic stress symptoms (PTSS) are associated with adverse consequences for older children, but very few studies have examined links between perinatal maternal PTSS and infant outcomes. Trauma exposure and psychopathology, including PTSS, is often heightened for women during pregnancy through one year postpartum. Therefore, the perinatal period may be a critical time for understanding the risk maternal PTSS and other mental health factors pose to the socioemotional and physical health of infants. The present study explored the relation between maternal PTSS and infant socioemotional and physical health problems in a sample of racially and ethnically diverse mother-infant dyads (N = 295) assessed prenatally and at 12 months postpartum. This study also examined whether there are: (1) moderating effects of maternal depressive symptoms and parenting stress on these associations and (2) indirect effects of PTSS on infant outcomes through observed maternal sensitivity. Results indicated that postpartum depressive symptoms and parenting stress, rather than PTSS, were associated with greater infant socioemotional health problems. However, prenatal PTSS were associated with greater infant physical health problems when mothers also reported clinically significant levels of postpartum depressive symptoms. Maternal sensitivity was not associated with maternal PTSS, depressive symptoms, or parenting stress, nor was it related to infant socioemotional and physical health; thus, maternal sensitivity was not tested as an intermediary mechanism linking maternal mental health with infant outcomes. Implications for promoting maternal mental health in the perinatal period to bolster socioemotional and physical health of infants are discussed.
Keywords: perinatal posttraumatic stress symptoms, perinatal depressive symptoms, perinatal parenting stress, maternal sensitivity, infant socioemotional problems, infant physical health problems
Exposure to a traumatic event or multiple traumatic events can lead to the development of posttraumatic stress symptoms (PTSS), including intrusion (e.g., flashbacks, nightmares), avoidance of trauma-related stimuli or emotions, negative alterations in cognition and mood, and heightened arousal and reactivity (e.g., irritability, angry outbursts, hypervigilance; American Psychiatric Association [APA], 2013). Estimates suggest that approximately 10-12% of women who are exposed to a traumatic event experience PTSS (Olff, 2017). Women may be especially at risk for PTSS during the perinatal period (i.e., pregnancy through one year postpartum; Garcia & Yim, 2017), as epidemiological data suggest that trauma exposure is heightened during this time, and PTSS are more likely to emerge, reemerge, or worsen when women are pregnant or have recently given birth (Cook et al., 2004; Seng et al., 2009). The onslaught of reproductive hormones during and after pregnancy are thought to make women more susceptible to stress, thereby increasing risk for psychopathology (Tung et al., 2019). This is particularly striking for mothers living in poverty, given that 14% of women facing socioeconomic adversity meet criteria for posttraumatic stress disorder (PTSD) during the perinatal period (perhaps due to greater likelihood of trauma exposure), and many more likely experience PTSS (Jain et al., 2018; Cook et al., 2004; Seng et al., 2009).
Pathways by which Maternal Psychological Distress Affects Child Outcomes
Maternal psychological distress in pregnancy, which includes general stress, depressive symptoms, or trauma exposure and subsequent PTSS, has been shown to alter the course of fetal development and adversely impact infant and child health through many interconnected biological systems (see Lewis et al., 2014, Van den Bergh et al., 2017, and Vehmeijer et al., 2019 for reviews). The most studied of these is the hypothalamic-pituitary-adrenal (HPA) axis (Lewis et al., 2014). Specifically, heightened maternal cortisol levels due to psychological distress are associated with excess fetal cortisol, which is thought to induce changes to the fetal HPA axis, programming the fetus’s stress response in a way that is maladaptive outside of the womb (Lewis et al., 2014). Furthermore, the HPA axis plays a role in regulating other physiological processes, like circadian rhythms, physical growth, digestion, and inflammatory responses. Thus, alterations to the HPA axis in utero are linked to numerous detrimental outcomes at the fetal/birth stage, such as intrauterine growth restriction, preterm birth, and low birthweight, as well as in infancy, such as cardiometabolic, respiratory, atopic, and digestive problems, reactive temperament, and impaired socioemotional functioning (Vehmeijer et al., 2019).
Unfortunately, many women who experience psychological distress in pregnancy continue to experience symptoms postnatally, which may affect the quality of the early caregiving environment (Lewis et al., 2014). According to the developmental origins of health and disease (DOHaD) model and other fetal programming hypotheses, exposure to an unhealthy caregiving environment characterized by high levels of maternal psychological distress in the first year of life (another sensitive developmental period) may set off a cascade of risk for psychopathology and disease that has been building since the initial prenatal exposure (Bale, 2014; Barker, 2004; DeSocio, 2019; Van den Bergh et al., 2017). Infants whose stress response systems were altered prenatally may have more difficulty responding to challenges in the postpartum environment, such as displays of maternal distress or inattention, or separation from their caregivers, which may take a toll on both their socioemotional and physical health (Graham et al., 2018; Groh & Narayan, 2019). Although associations between maternal psychological distress and infant outcomes in the perinatal period have been extensively studied, most of these studies have employed a broad definition of psychological distress and have not investigated the effects of PTSS specifically, despite their prevalence and potential influence on infant socioemotional and physical health. Additionally, limited research has explicitly tested an important tenant of the DOHaD hypothesis by measuring maternal mental health factors both prenatally and in the postpartum period.
Maternal PTSS and Child Socioemotional Health Problems
Maternal PTSS are consistently associated with a host of negative psychosocial outcomes in toddlers, preschool-age children, and older children, including emotion regulation difficulties, internalizing and externalizing problems, and PTSD (see Lambert et al., 2014 and van Ee et al., 2016 for reviews). For instance, in a large, population-based study, maternal PTSS at 8-weeks postpartum were associated with poor child socioemotional development two years later (Garthus-Niegel et al., 2016). In another study, concurrent maternal PTSS mediated the association between mothers’ experiences of intimate partner violence and preschool-age children’s internalizing and externalizing symptoms (Greene et al., 2018). A few other studies examined concurrent maternal PTSS and child outcomes in samples where toddlers and preschoolers were assessed together without specifically examining the effects of age: among mothers who were exposed to war-related trauma, heightened PTSS were associated with greater socioemotional difficulties in their young children (e.g., ages 1 to 6 years of age; Pat-Horenczyk et al., 2015; van Ee et al., 2012). Less is known about maternal PTSS and child outcomes in the first year of life. Research by Bosquet Enlow and colleagues (2009, 2011) comprises the very small body of work that has examined socioemotional functioning in infants as it relates to maternal PTSS. In the first study, lifetime maternal PTSS were associated with disrupted infant cardiorespiratory regulation and behavioral distress during a stressor protocol at 6 months postpartum (Bosquet Enlow et al., 2009). In the second study, elevated maternal PTSS at 6 months postpartum predicted higher levels of infant internalizing and externalizing problems, and emotion regulation difficulties, at 13 months postpartum (Bosquet Enlow et al., 2011). Taken together, these studies provide evidence that maternal PTSS may affect child socioemotional functioning during infancy and beyond. However, as maternal PTSS were not measured specifically during pregnancy, these results do not provide clear evidence in support of the DOHaD hypothesis, though researchers speculate that maternal PTSS in pregnancy contribute to the prenatal programming of the child’s stress response system, while postpartum PTSS shape further HPA axis activity and may exacerbate children’s already heightened stress responses, contributing to socioemotional problems (van Ee et al., 2016).
Maternal PTSS and Child Physical Health Problems
In addition to their detrimental influence on socioemotional functioning, maternal PTSS in the perinatal period may increase risk of physical health problems among infants through their enduring effect on multiple biological systems, namely the HPA axis (DeSocio, 2019; Van den Bergh et al., 2017).
Most research in this area has focused on birth or neonatal outcomes. For example, a meta-analysis of 21 studies found that perinatal PTSS were associated with pre-term birth, low birth weight, impaired fetal growth, and a composite of sleeping and eating difficulties (Cook et al., 2018). Similarly, a recent retrospective chart review that followed premature infants over one year showed that maternal PTSS were associated with growth delay (Zhang et al., 2020). However, few studies have examined chronic physical health problems spanning multiple domains such as respiratory, digestive, and skin-related illnesses, all of which may be triggered or exacerbated by infant stress instigated by exposure to maternal PTSS prenatally and/or postpartum. There is support for these associations in the general maternal psychological distress literature, wherein psychological distress in pregnancy—but not necessarily PTSS—has been associated with a variety of physical health problems in infants across the first few years of life, including wheezing, asthma, and other respiratory illnesses, skin illnesses, gastrointestinal problems, and general illnesses (Bush et al., 2021; Kozyrskyj et al., 2008; Phelan et al., 2015; Wright et al., 2002; Zijlmans et al., 2017).
The Role of Depressive Symptoms
PTSS are not the only maternal mental health factor that may contribute to infant socioemotional and physical health problems, and thus should not be examined in isolation. Mothers with PTSS frequently display comorbid depressive symptoms or go on to have depressive symptoms at a later point in time, suggesting that depressive symptoms should be tested in concert with PTSS in the perinatal period to fully understand the effects of mothers’ psychological experiences on infant outcomes. Findings from large representative studies provide compelling evidence that PTSS are often accompanied by depressive symptoms, with 35-80% of adults with PTSD also meeting criteria for major depressive disorder (MDD; Brown et al., 2001; Cougle et al., 2009; Price et al., 2019). Research also suggests comorbidity between PTSS and depressive symptoms specifically during the perinatal period (Agius et al., 2016). Prior work has demonstrated that experiencing both PTSS and depressive symptoms is associated with greater functional impairment compared to experiencing a single type of psychopathology (Cook et al., 2004). Therefore, it is possible that when mothers simultaneously experience PTSS and depressive symptoms, or experience PTSS and depressive symptoms across the perinatal period and thereby are faced with a longer duration of mental illness, they may have greater difficulty responding sensitively to their infants (Erickson et al., 2019). Research to date has primarily focused on how the interplay of maternal PTSS and depressive symptoms affects mother-infant attachment and parenting rather than infant socioemotional and physical health. Understanding how maternal PTSS and depressive symptoms interact to predict infant outcomes in addition to parenting has important implications for the treatment and prevention of health problems in the first year of life.
The Role of Parenting Stress
Parenting stress may also exacerbate links between maternal PTSS on infant socioemotional and physical health problems. Parents with PTSS report more parenting difficulties (e.g., poor parenting behaviors, less satisfaction, higher stress) than other parents (Christie et al., 2019; Wilson et al., 2017), but limited research has examined associations between PTSS and parenting stress during the perinatal period. This gap is notable given that parenting stress has been shown to amplify parental psychopathology (e.g., depressive symptoms) following the birth of a child (Epifanio et al., 2015; Vismara et al., 2016). Some research has shown that higher parenting stress in the perinatal period predicts child adjustment problems in early childhood (Anhalt, Telzra & Brown, 2007). In middle childhood, higher levels of maternal PTSS have been associated with greater parenting stress, which in turn predicts internalizing and externalizing symptoms (Hartzell et al., 2020; Samuelson et al., 2016). Most prior research has examined parenting stress as the mechanism by which PTSS are associated with child outcomes; however, limited work suggests that parenting stress may be a vulnerability factor, amplifying risk for poor infant outcomes in the context of mothers’ PTSS. In other words, infants of mothers with higher levels of PTSS and parenting stress across the perinatal period may be most at risk for socioemotional and physical health problems. To our knowledge, no studies have examined the interaction of PTSS and parenting stress in association with infant outcomes. However, prior work has demonstrated that parenting stress is linked to negative child outcomes in the presence of other risk factors, including temperamental negative affectivity (Wu et al., 2019) and trauma exposure (Cho et al., 2020).
Maternal Sensitivity as a Mechanism
Identifying maternal risk factors in the perinatal period, such as higher levels of PTSS, depressive symptoms, and parenting stress, informs the field as to which infants are most susceptible to negative outcomes, while identifying mechanisms sheds light on how those associations happen. Understanding both risk factors and mechanisms is crucial, as this knowledge may inform interventions aimed at preventing intergenerational effects of trauma early in life. There are multiple pathways in the prenatal and postpartum environments through which maternal mental health may impact the developing child. Prenatal programming of the fetus (e.g., enduring alterations to the HPA axis) is hypothesized as the primary underlying mechanism during pregnancy while sensitive parenting is thought to be a major mechanism following the birth of the infant (van Ee et al., 2016). Prior research suggests that PTSS may adversely impact mothers’ ability to sensitively (e.g., timely, contingently, appropriately) respond to and engage with their infants (e.g., Feeley et al., 2011; Lyons-Ruth & Block, 1996; Bosquet Enlow et al., 2014). For example, Bosquet Enlow and colleagues (2014) demonstrated that maternal PTSS at 6 months postpartum were associated with increased risk for an insecure mother-infant attachment relationship at 13 months postpartum. Maternal depressive symptoms and parenting stress, which may occur during the perinatal period, have also been linked to attachment problems and less sensitive parenting in infancy (see Bernard et al., 2018 and Booth et al., 2018 for reviews).
In addition to the literature suggesting links between maternal mental health and parenting sensitivity, there is some empirical evidence that maternal sensitivity also impacts infant development. First, several studies have demonstrated that greater maternal sensitivity in infancy is predictive of healthy socioemotional development (e.g., greater emotion regulation, higher attachment security, fewer behavior problems; Leerkes et al., 2009; Perry et al., 2016). Although some studies have demonstrated links between parenting behavior and physical health outcomes in childhood (e.g., Belsky et al., 2007; Mitchell et al., 2020) and adulthood (e.g., Buchmann et al., 2010; Farrell et al., 2018), scant research has examined whether parenting behavior may impact physical health during infancy. As one notable exception, Stern and colleagues (2020) found that maternal sensitivity at infant age 5 weeks predicted lower rates of infant respiratory symptoms and skin conditions over the course of the first year of life. Conversely, maternal behavior was not predictive of infant digestive or general illnesses. This finding mirrors results of an earlier study demonstrating that unhealthy mother-infant interaction when infants were 2 months old was associated with more chronic health problems when children were 2 years old (Mäntymaa et al., 2003). Therefore, there is some limited evidence to suggest that maternal sensitivity may be predictive of certain infant physical health outcomes, perhaps due to its effects on infant stress. In summary, while there is preliminary, piecemeal support for maternal sensitivity as an intermediary mechanism in the postpartum period linking maternal PTSS to infant socioemotional and physical health outcomes, limited research has tested these indirect effects. Evaluating these effects in comprehensive analytic models is critical in identifying potential clinical targets for mothers and infants living in high-risk circumstances.
Purpose of the Study
The purpose of the present study was to (a) test the direct effects of maternal PTSS (measured in pregnancy and postpartum) on infant socioemotional and physical health in a sample of mother-infant dyads with significant socioeconomic adversity; (b) test the role of depressive symptoms and parenting stress as moderators; and (c) evaluate whether observed maternal sensitivity in both non-distressing and distressing contexts served as an intermediary mechanism linking maternal mental health factors to infant outcomes (see Figure 1 for conceptual model). Although this study focused on a potential mechanism in the postpartum period (i.e., maternal sensitivity), examining biological mechanisms in pregnancy and postpartum is an important next step for future research. We hypothesized that (1) both prenatal and postpartum PTSS would be positively associated with infant socioemotional and physical health problems, and that (2) these main effects would be qualified by interactions between prenatal PTSS and 12-month PTSS, prenatal PTSS and prenatal depressive symptoms, prenatal PTSS and 12-month postpartum depressive symptoms, and prenatal PTSS and 12-month parenting stress. We examined the interaction between prenatal PTSS and prenatal depressive symptoms to better understand the effect of comorbid, prenatal mental health factors on infant outcomes. We then examined interactions between prenatal and postpartum mental health factors as a preliminary effort to test the DOHaD hypothesis (i.e., does the presence of a maternal mental health factor in the postpartum period push an infant toward socioemotional or physical health problems when they also experienced another maternal mental health factor prenatally?). Finally, we hypothesized that (3) PTSS and interactions with other maternal mental health factors would be indirectly associated with infant socioemotional and physical health through maternal sensitivity measured during non-distressing and distressing tasks. To our knowledge, this is the first comprehensive study of maternal PTSS and other mental health factors across the perinatal period and their effects on infant socioemotional and physical health outcomes, as well as their indirect effects on these outcomes via observed maternal sensitivity.
Figure 1.
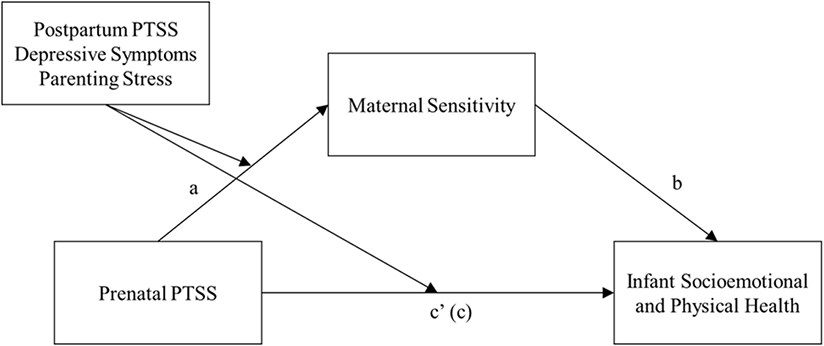
Hypothesized model of the indirect effects of prenatal posttraumatic stress symptoms (PTSS) on infant socioemotional and physical health problems at 12 months postpartum, via observed maternal sensitivity (assessed during distressing and non-distressing tasks at 12 months postpartum), with maternal postpartum PTSS, depressive symptoms (prenatal and postpartum), and parenting stress (postpartum) as moderators. Path c’ is the direct path. Path c is the total effect. Analyses were conducted separately for maternal sensitivity observed during the distressing task and non-distressing task.
Methods
Participants
Participants included 295 mother-infant dyads who were assessed prenatally and at 12 months postpartum (84% retention rate). Mothers and their infants were enrolled in a larger longitudinal project designed to understand if maternal childhood adversity was associated with enrollment and retention in home visiting services, and the extent to which home visiting enhanced parenting and infant outcomes. Women were recruited from Women, Infants, and Children (WIC) clinics during pregnancy. To be eligible for the project, women had to be: (1) referred to home visiting services, (2) pregnant with a singleton, (3) at least 18 years of age, and (4) fluent in English or Spanish. The sample was racially and ethnically diverse; 40% of mothers were Hispanic or Latinx, 42% were White, 19% were Black, 7% were biracial or multiracial, and 32% endorsed other races. Among infants, 49% were Hispanic or Latinx, 35% were White, 17% were Black, 26% were biracial or multiracial, and 22% were other races. Mothers ranged in age from 18 to 44 years (M = 25.61 years; SD = 5.33 years). Thirty-eight percent were first time mothers. At the prenatal assessment, gestational age (GA) ranged from 44 to 283 days (M = 185.60 days; SD = 59.96 days). Ten percent of infants were born premature, and 53% were female. Regarding socioeconomic indicators, 23% of mothers had less than a high school degree, 37% had completed high school, 36% had some postsecondary education, and 4% had a bachelor’s degree. Sixty-five percent of mothers were unemployed in pregnancy, 44% were single parents, and all mothers received public assistance. Over the course of the study, 39% of mothers enrolled in evidence-based home visiting services.
Procedure
Expectant mothers completed baseline assessments at a prenatal enrollment visit, and mothers and their infants completed follow-up assessments at a postpartum visit when infants were 12 months of age. Both prenatal and postpartum visits took place in participants’ homes. Mothers provided written consent for themselves and their infant to participate. They received monetary compensation for their time. All study procedures were approved by the Institutional Review Board at Lifespan.
Measures
Demographics and Potential Covariates
At the prenatal assessment, mothers reported their age, race and ethnicity, educational level, employment status (unemployed vs. employed), marital status (single vs. two-parent household), due date, and whether they were first time mothers. Consistent with prior research (e.g., Tyrka et al., 2015), indicators of socioeconomic risk (education ≤ high school diploma, unemployment, single parenthood) were summed to provide a parsimonious assessment of socioeconomic adversity (possible scores ranged from 0 to 3). At the postpartum assessment, mothers reported their infant’s actual birth date, infant race, ethnicity, and sex. Infant premature birth was determined from the difference between the due date and actual birth date. Mothers also reported whether they had experienced any health problems during pregnancy or after the baby’s birth.
Maternal Posttraumatic Stress Symptoms
At the prenatal and postpartum assessments, mothers completed the Davidson Trauma Scale (DTS; Davidson, 1996; Davidson et al., 1997), a 17-item measure that reflects the symptoms used for PTSD diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; APA, 1994). The DTS assesses three symptom clusters: intrusion (e.g., “have you had painful images, memories, or thoughts of the event”), avoidance/numbing (e.g., “have you been avoiding doing things or going into situations that remind you of the event”, and hyperarousal (e.g., “have you been irritable or had outbursts of anger”; “have you been jumpy or easily startled”). Mothers were asked to think of a past trauma that was most distressing to them and then rate how often in the last week each symptom troubled them, and how severe each symptom was. Mothers rated frequency of each symptom on a 5-point scale ranging from 0 (“not at all”) to 4 (“every day”), and severity of each symptom on a 5-point scale ranging from 0 (“not at all distressing”) to 4 (“extremely distressing”). The current study used the DTS total score, which was computed by adding all item responses together (i.e., total frequency score and total severity score), with a possible range of 0–136. Higher scores indicated greater PTSS. The DTS has been shown to have excellent psychometric properties (Cronbach’s alpha ranges from .97 to .99 for the total score; Chen et al., 2001; McDonald et al., 2009). Further, the DTS has been used extensively in samples of pregnant women (e.g., Becker-Sadzio et al., 2020; Vignato et al., 2018). The DTS demonstrated excellent internal consistency in the current sample (α = .97 at both prenatal and postpartum assessments). Total scores of either 32 or 40 have been used as cut points for a likely PTSD diagnosis for general respondents as well as pregnant women, with some evidence for higher sensitivity and diagnostic efficacy at the cutoff of 32 (McDonald et al., 2009; Vignato et al., 2018).
Maternal Depressive Symptoms
At the prenatal and postpartum assessments, mothers completed the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001), a 9-item screening tool that corresponds with the criteria specified for MDD in the DSM-IV (APA, 1994). The core criteria for MDD have not changed in the DSM-5. Mothers reported on their symptoms of depression (e.g., “little interest or pleasure in doing things”; “feeling down, depressed, or hopeless”) over the last two weeks. Each item was rated on a 4-point scale ranging from 0 (“not at all”) to 3 (“almost every day”). Items were summed to compute a total score, which can range from 0 to 27, with higher scores indicating greater depressive symptoms. The PHQ-9 has excellent psychometric properties and is widely used by researchers and practitioners to assess depressive symptoms (Kocalevent et al., 2013). The PHQ-9 has been validated for use with pregnant women (Wang et al., 2020). Internal consistency for the PHQ-9 in the current sample was α = .81 at the prenatal assessment, and α = .89 at the postpartum assessment. When the PHQ-9 is used for diagnostic purposes, a cutoff score of 10 is the most widely recommended cut point, as previous research has demonstrated that this value provides the best combination of sensitively and specificity (Kroenke et al., 2001).
Parenting Stress
At the (12 months) postpartum assessment, mothers completed the 36-item Parenting Stress Index-Short Form (PSI-SF; Abidin, 2012). Mothers rated items on a 5-point scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). The PSI-SF produces an overall parenting stress score, which can range from the 1st to the 99th percentile. The total percentile score was used for the current study, with higher scores indicating greater parenting stress. The PSI-SF is widely used and has demonstrated strong psychometric properties (Haskett et al., 2006), including in studies of mothers in the perinatal period (e.g., Huizink et al., 2017; Molgora et al., 2020). In the current study, the PSI-SF demonstrated good internal consistency (α = .93).
Maternal Sensitivity
Maternal sensitivity was assessed from videotaped observations of mother-infant interactions during a non-distressing (free play) task and a distressing (frustration) task completed at 12 months postpartum. For the free play task, mothers were asked to play with their infant for seven minutes using developmentally appropriate toys (e.g., toy telephone, car, rings, blocks) provided by our research team. For the frustration task, infants were given a transparent box with an attractive toy inside that they could not obtain (Leerkes & Wong, 2012). The task lasted four minutes. During the first minute mothers were instructed not to interact with the infant. During the last three minutes (the portion of the task that is coded) mothers were instructed to interact with the infant as they normally would, but to not open the box for the infant. Both interactions were video recorded by a research assistant using a handheld camera. Using the Sensitivity scale from the Emotional Availability Scales (Biringen et al., 2000), one trained rater coded all the videos. This rater demonstrated interrater reliability with our laboratory standard (ICC ≥ .80), double coding 20 tapes with our laboratory’s lead coder who is responsible for training staff in this coding procedure. The Sensitivity scale is a 9-point scale that ranges from 1 (“highly insensitive”) to 9 (“highly sensitive”) and assesses the degree to which mothers display a behavioral style that is responsive to infant cues, affectively positive, flexible, interactive, and emotionally connected (e.g., showing genuine interest and positive affect toward infant, reading infant’s signals accurately and responding appropriately, clear emotional connection between infant and mother). The maternal sensitivity score (1-9) for each task was used separately in analyses.
Infant Socioemotional Health
At the postpartum assessment, mothers reported on their infants’ emerging socioemotional problems using the 44-item Brief Infant-Toddler Social and Emotional Assessment (BITSEA; Carter & Briggs-Gowan, 2006). Mothers were asked to estimate how true each statement was for their infant on a 3-point scale (0 = “not true/rarely”, 1 = “somewhat true/sometimes”, 2 = “very true/often”). Responses from all items were averaged together to reflect a total problem behaviors score, with higher scores indicating more socioemotional problems. The BITSEA, which has been used in numerous studies of infants’ behavioral functioning, has demonstrated acceptable reliability and validity (Briggs-Gowan et al., 2004; Briggs-Gowan et al., 2013), and showed adequate internal consistency in the current study (α = .78). To determine clinically significant socioemotional problems, a cutoff score of 13 is used for 12-17-month-old girls, while a cutoff score of 15 is used for 12-17-month-old boys (Briggs-Gowan et al., 2004).
Infant Physical Health
Mothers completed a health interview at the postpartum assessment, administered by a research assistant, providing information on their infant’s physical health problems since birth. Mothers were asked if their baby had been treated for or diagnosed with health conditions that were categorized into five nonoverlapping domains according to the International Classification of Primary Care (i.e., respiratory, digestive, skin, failure to gain weight, and other illnesses and complaints [e.g., jaundice, colic]) and whether the condition was current, as well as acute or chronic (Lamberts & Wood, 1987). The number of chronic physical health problems that mothers endorsed were summed to derive a total score (possible range: 0 to 5). This method has been successfully used in other studies of infant health (Beijers et al., 2010; Stern et al., 2020).
Analytic Plan
Path analysis within structural equation modeling (SEM) was used to examine primary hypotheses. Full-information maximum likelihood (FIML) estimation was used to accommodate missing data (9.1% of values), as this approach minimizes bias when the amount of missing data does not exceed 20% and works for all types of missing data (i.e., MCAR, MAR, NMAR; Schlomer et al., 2010). All path models were fully saturated (i.e., 0 degrees of freedom), thus model fit was not assessed.
Analyses for hypotheses 1 and 2 were carried out in two steps. For the first step, the main effects of prenatal and 12-month PTSS and covariates (model 1), prenatal PTSS, prenatal and 12-month depressive symptoms, and covariates (model 2) and prenatal PTSS and 12-month parenting stress, and covariates (model 3) on both infant socioemotional and physical health problems were tested. Infant socioemotional and physical health problems were simultaneously regressed on predictors and covariates, as this method reduces the possibility of spurious findings. For the second step, interaction terms were added to the main effects models, resulting in model 1a (prenatal PTSS X 12-month PTSS), model 2a (prenatal PTSS X prenatal depressive symptoms), model 2b (prenatal PTSS X 12-month depressive symptoms), and model 3a (prenatal PTSS X 12-month parenting stress).
To test hypothesis 3, that maternal mental health would indirectly affect infant socioemotional and physical health problems through observed maternal sensitivity during non-distressing and distressing tasks, we tested associations between maternal mental health predictors (i.e., prenatal and postpartum PTSS, prenatal and postpartum depressive symptoms, postpartum parenting stress) and maternal sensitivity during each task, and maternal sensitivity during each task and infant socioemotional and physical health problems. Infant outcomes were again regressed simultaneously on maternal sensitivity. If any of these links were significant, we planned to use 10,000 bootstrap replicates to obtain bias-corrected bootstrap confidence intervals to test hypothesized indirect effects (MacKinnon et al., 2004).
Prior to analyses, all variables were inspected for normality using SPSS 25. One value for infant socioemotional problems was greater than 3.29 standard deviations from the mean, and was winsorized. Prenatal and postpartum PTSS were log-transformed instead of winsorized because of high skew and kurtosis.
We examined potential covariates for inclusion in the models (i.e., maternal age, maternal ethnicity, maternal race, status as a first-time mother [primiparous], maternal health problems, enrollment in home visiting intervention, socioeconomic adversity, and infant gestational age and prematurity). Five covariates (i.e., maternal age, maternal ethnicity, status as a first-time mother, socioeconomic adversity, and infant prematurity) were related to PTSS, depressive symptoms, parenting stress, maternal sensitivity, infant socioemotional problems, and/or infant physical health problems. To maximize parsimony, these five were the only covariates included in the models. All models were tested with and without these selected covariates, and there was no change in the direction or significance of paths.
Interaction terms were created from standardized cross-products of the original variables (i.e., PTSS, depressive symptoms, parenting stress) to reduce problems with multicollinearity. Significant interaction terms were probed using standard procedures (Aiken & West, 1991), and simple slopes were calculated at lower (−1 SD) and higher (+1 SD) levels of the moderator variable. We then used the Johnson-Neyman technique for identifying regions of significance (Hayes and Matthes, 2009; Johnson and Neyman, 1936).
Results
Descriptive Analyses
Descriptive statistics, including means, standard deviations, and ranges for study variables are presented in Table 1 and correlations are presented in Table 2. Regarding maternal mental health, during pregnancy 16.7% of mothers had a total DTS score of 40 or above, indicating clinically significant PTSS that may warrant a PTSD diagnosis (McDonald et al., 2009). Alternatively, using a cutoff score of 32 as indicated by some research, 22.3% of mothers had clinically significant PTSS. In addition, 15.9% of mothers had a total PHQ score of 10 or above, indicating clinically significant depressive symptoms (Kroenke et al., 2001). Twenty-six mothers (13.3% of the sample) endorsed both clinically significant PTSS (at cutoff score of 40) and depressive symptoms. At 12 months postpartum, 11.7% of mothers had a total DTS score of 40 or above, while 11.1% of mothers had a total PHQ score of 10 or above. When using a DTS cutoff score of 32, 14.2% of mothers had clinically significant PTSS. Thirteen mothers (6.6% of the sample) endorsed both clinically significant PTSS (at cutoff score of 40) and depressive symptoms at this time point.
Table 1.
Descriptive Statistics of Study Variables
| Raw Mean or n |
SD or % |
Log- Transformed Mean (SD) |
Minimum | Maximum (Log- Transformed) |
|
|---|---|---|---|---|---|
| Prenatal Variables | |||||
| Posttraumatic Stress Symptoms | 19.7 | 25.0 | 2.1 (1.6) | 0 | 110 (4.7) |
| Depressive Symptoms | 5.6 | 4.6 | -- | 0 | 20 |
| Postpartum Variables | |||||
| Posttraumatic Stress Symptoms | 13.8 | 23.1 | 1.5 (1.6) | 0 | 108 (4.7) |
| Depressive Symptoms | 3.5 | 4.7 | -- | 0 | 18 |
| Parenting Stress | 30.6 | 25.5 | -- | 1 | 99 |
| Maternal Sensitivity – Free Play Task | 5.5 | 1.5 | -- | 2 | 8 |
| Maternal Sensitivity – Frustration Task | 4.8 | 1.5 | -- | 0 | 8 |
| Infant Socioemotional Problems | 11.5 | 6.6 | -- | 1 | 41 |
| Infant Physical Health Problems | 0.6 | 0.8 | -- | 0 | 4 |
| Covariates | |||||
| Age | 25.6 | 5.3 | -- | 18 | 44 |
| Ethnicity (% Hispanic or Latinx) | 118 | 40% | -- | -- | -- |
| Socioeconomic Adversity | 1.7 | 0.9 | -- | 0 | 3 |
| Prematurity (% Premature) | 27 | 10% | -- | -- | -- |
| Primiparous (% First Time Mother) | 111 | 38% | -- | -- | -- |
Note. Log-transformed values for prenatal and postpartum posttraumatic stress symptoms were used in analyses.
Table 2.
Correlations among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prenatal | ||||||||||||||
| 1. PTSS | -- | |||||||||||||
| 2. DS | .52*** | -- | ||||||||||||
| Postpartum | ||||||||||||||
| 3. PTSS | .55*** | .34*** | -- | |||||||||||
| 4. DS | .47*** | .50*** | .60*** | -- | ||||||||||
| 5. Parent. Stress | .26*** | .30*** | .32*** | .43*** | -- | |||||||||
| 6. Task 1 Sensitiv. | −.07 | .03 | .01 | .03 | −.08 | -- | ||||||||
| 7. Task 2 Sensitiv. | −.05 | −.01 | .04 | .02 | −.07 | .31** | -- | |||||||
| 8. Socio. Emot. | .16* | .20** | .13 | .23** | .47** | −.16* | −.03 | -- | ||||||
| 9. Physical Health | .12 | .03 | .07 | .09 | .11 | −.11 | −.09 | .04 | -- | |||||
| Covariates | ||||||||||||||
| 10. Age | .07 | .20** | .15* | .10 | .01 | .07 | .07 | −.04 | −.09 | -- | ||||
| 11. Ethnicity | −.13* | −.07 | −.13 | −.17* | −.09 | −.02 | .01 | .01 | .05 | −.16** | -- | |||
| 12. SES | .05 | .06 | −.05 | −.01 | .03 | −.21** | −.22** | .17** | .05 | −.19** | .08 | -- | ||
| 13. Prematurity | −.03 | −.07 | −.06 | −.15* | −.06 | .05 | .05 | −.05 | .12* | .03 | .18** | −.01 | -- | |
| 14. Primiparous | .02 | .01 | −.03 | −.05 | −.09* | −.05 | −.08 | .00 | −.02 | −.25** | −.15* | −.03 | −.09 | -- |
Note. Ethnicity is coded as 0 = non-Hispanic or Latinx, 1 = Hispanic or Latinx; PTSS = posttraumatic stress symptoms; DS = depressive symptoms; Parent. Stress = parenting stress; Task 1 Sensitiv. = observed maternal sensitivity during non-distressing free play task; Task 2 Sensitiv. = observed maternal sensitivity during distressing frustration task; Socio. Emot. = infant socioemotional problems; Physical Health = infant physical health problems; SES = socioeconomic adversity.
p < .001
p < .01
p < .05
For infants, 32.2% scored above the clinical cut point for BITSEA total socioemotional problems at 12 months of age. Regarding physical health, 59.5% of infants had zero chronic health problems, 27.1% had one chronic health problem, 9.5% had two chronic health problems, 3.1% had three chronic health problems, and 0.8% had four chronic health problems.
Primary Analyses
Main and Interactive Effects of PTSS, Depressive Symptoms, and Parenting Stress on Infant Outcomes
Model 1 (see Table 3), which tested whether prenatal and postpartum PTSS would be positively associated with infant socioemotional and physical health problems, revealed no main effects of PTSS on either socioemotional or physical health problems in infants. The interaction between prenatal and postpartum PTSS (Model 1a) was also not associated with either outcome. In Model 2 (see Table 4), there was a main effect of postpartum depressive symptoms on infant socioemotional problems (β = .19, p = .03). Contrary to our hypothesis, that the interaction between prenatal PTSS and prenatal depressive symptoms would be associated with infant outcomes (Model 2a), results showed that this interaction was not associated with either infant outcome, but postpartum depressive symptoms remained positively associated with infant socioemotional problems (β = .20, p = .03). Additionally, the interaction between prenatal PTSS and postpartum depressive symptoms (Model 2b) was not associated with infant socioemotional problems, though the main effects of postpartum depressive symptoms on infant socioemotional problems remained (β = .26, p = .01). Prenatal PTSS were, however, positively associated with infant physical health problems in this model, as hypothesized (β = .21, p = .02). This main effect was qualified by the significant interaction between prenatal PTSS and postpartum depressive symptoms (β = .22, p = .01). As shown in Figure 2, simple slope analyses indicated that prenatal PTSS were associated with infant physical health problems when mothers reported high (b = 2.41, p < .001), but not low (b = .69, p = .42) depressive symptoms at 12 months postpartum. Additionally, examinations of regions of significance revealed that when infants had mothers with clinically significant PTSS (DTS score of 32), and clinically significant depressive symptoms (PHQ-9 score of 12), they displayed more physical health problems than all other infants.
Table 3.
Path Models with Prenatal and Postpartum PTSS Predicting Infant Socioemotional and Physical Health Problems
| Socioemotional Problems at 12 Months β (SE) |
Chronic Physical Health Problems at 12 Months β (SE) |
|
|---|---|---|
| Model 1: Main Effects | ||
| Prenatal PTSS | .01 (.09) | .14 (.09) |
| 12-month PTSS | .01 (.09) | .11 (.09) |
| R2 | .07* | .07* |
| Model 1a: Prenatal PTSS x 12-Month PTSS | ||
| Prenatal PTSS | .01 (.09) | .14 (.09) |
| 12-month PTSS | .01 (.09) | .13 (.09) |
| Prenatal PTSS X 12-month PTSS | .03 (.06) | .03 (.08) |
| R2 | .08* | .07* |
Note. PTSS = posttraumatic stress symptoms. β = beta (standardized), SE = standard error. All models controlled for maternal age, maternal ethnicity, primiparous status, socioeconomic adversity, and infant prematurity. In Model 1, socioeconomic adversity was positively associated with socioemotional problems (β =.18, p < .01) while infant prematurity was positively associated with chronic physical health problems (β =.15, p < .05). These covariates, and no others, remained significant in Model 1a.
p < .05.
Table 4.
Path Models with PTSS and Depressive Symptoms Predicting Infant Socioemotional and Physical Health Problems
| Socioemotional Problems at 12 Months β (SE) |
Chronic Physical Health Problems at 12 Months β (SE) |
|
|---|---|---|
| Model 2: Main Effects | ||
| Prenatal PTSS | .01 (.09) | .14 (.09) |
| 12-month PTSS | .01 (.09) | .11 (.09) |
| Prenatal DS | .09 (.08) | .06 (.08) |
| 12-month DS | .19 (.09) * | .11 (.09) |
| R2 | .09* | .06* |
| Model 2a: Prenatal PTSS x Prenatal Depressive Symptoms | ||
| Prenatal PTSS | .01 (.09) | .14 (.09) |
| 12-month PTSS | .01 (.09) | .01 (.09) |
| Prenatal DS | .11 (.09) | .06 (.09) |
| 12-month DS | .20 (.09) * | .11 (.09) |
| Prenatal PTSS X Prenatal DS | −.05 (.07) | .02 (.08) |
| R2 | .10* | .06* |
| Model 2b: Prenatal PTSS x 12-Month Depressive Symptoms | ||
| Prenatal PTSS | .02 (.09) | .21 (.09) * |
| 12-month PTSS | .02 (.09) | .00 (.09) |
| Prenatal DS | .10 (.08) | .09 (.08) |
| 12-month DS | .26 (.11) * | .05 (.11) |
| Prenatal PTSS X 12-month DS | −.10 (.09) | .22 (.09) ** |
| R2 | .10* | .10* |
Note. PTSS = posttraumatic stress symptoms; DS = depressive symptoms. β = beta (standardized), SE = standard error. All models controlled for maternal age, maternal ethnicity, primiparous status, socioeconomic adversity, and infant prematurity. In Model 2, socioeconomic adversity was positively associated with socioemotional problems (β =.18, p < .01) while infant prematurity was positively associated with chronic physical health problems (β =.15, p < .05). These covariates, and no others, remained significant in Models 2a and 2b.
p < .05
p < .01.
Figure 2.
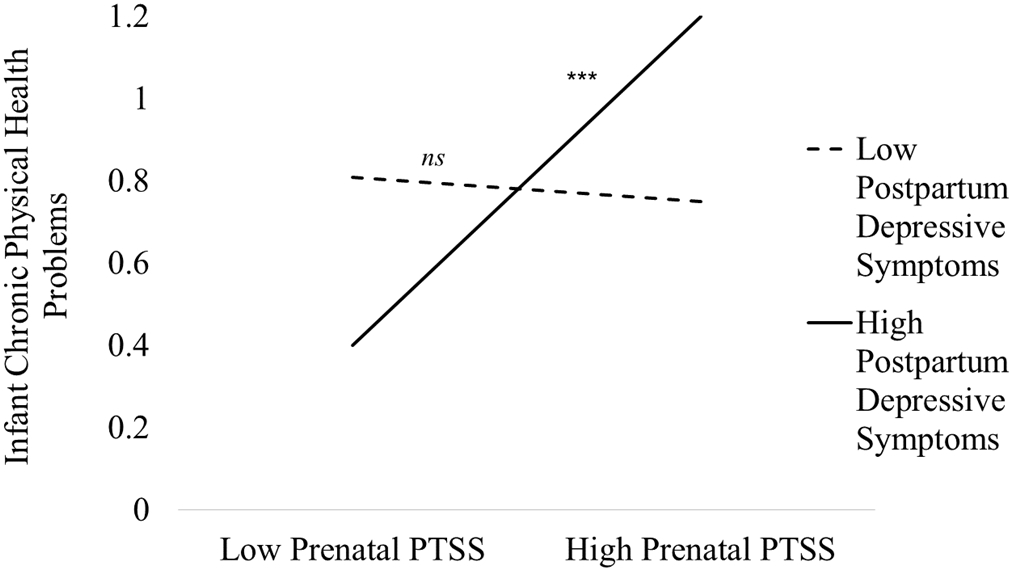
A graphical depiction of the interaction between prenatal posttraumatic stress symptoms (PTSS) and 12-month depressive symptoms in association with infant chronic physical health problems at 12 months postpartum. Note. *** indicates that the simple slope is significant at p < .001, ns indicates that the simple slope is not statistically significant.
Finally, the interaction between prenatal PTSS and postpartum parenting stress (Model 3a; see Table 5) was not associated with infant socioemotional or physical health problems. There was, however, a main effect of postpartum parenting stress on infant socioemotional problems (β = .49, p < .001).
Table 5.
Path Models with PTSS and Parenting Stress Predicting Infant Socioemotional and Physical Health Problems
| Socioemotional Problems at 12 Months β (SE) |
Chronic Physical Health Problems at 12 Months β (SE) |
|
|---|---|---|
| Model 3: Main Effects | ||
| Prenatal PTSS | .04 (.07) | .12 (.08) |
| 12-month PTSS | .04 (.08) | .01 (.08) |
| 12-month Parenting Stress | .48 (.06) *** | .11 (.07) |
| R2 | .26*** | .07* |
| Model 3a: Prenatal PTSS x 12-Month Parenting Stress | ||
| Prenatal PTSS | .04 (.07) | .12 (.08) |
| 12-month PTSS | .03 (.08) | .01 (.08) |
| 12-month Parenting Stress | .49 (.06) *** | .11 (.08) |
| Prenatal PTSS X 12-month Parenting Stress | −.06 (.06) | −.02 (.07) |
| R2 | .26*** | .07* |
Note. PTSS = posttraumatic stress symptoms; DS = depressive symptoms. β = beta (standardized), SE = standard error. All models controlled for maternal age, maternal ethnicity, primiparous status, socioeconomic adversity, and infant prematurity. In Model 3, socioeconomic adversity was positively associated with socioemotional problems (β =.16, p < .01) while infant prematurity was positively associated with physical health problems (β =.14, p < .05). These covariates, and no others, remained significant in Model 3a.
p < .05
p < .01
p < .001.
Indirect Effects of Maternal Sensitivity
We also hypothesized that that there would be indirect effects of maternal PTSS and interactions between maternal PTSS and other mental health factors on infant outcomes through observed maternal sensitivity at 12 months postpartum. Contrary to hypotheses, however, maternal sensitivity assessed during both non-distressing and distressing tasks was not significantly associated with any predictor (i.e., PTSS, depressive symptoms, parenting stress, interaction terms) or outcomes (i.e., socioemotional and physical health problems). Thus, indirect effects via bias-corrected bootstrapping tests were not examined.
Discussion
The present study represents a novel effort to delineate the unique and interactive effects of maternal PTSS, depressive symptoms, and parenting stress in the perinatal period on both socioemotional and physical health problems in infants. Extant research has demonstrated a link between maternal PTSS and a host of negative outcomes in older children, but very few studies have examined these relations in a sample of infants. Furthermore, no studies have tested the interplay of PTSS and depressive symptoms, and PTSS and parenting stress, on infant outcomes, limiting the field’s understanding of the synergistic effects of multiple maternal mental health factors on (1) maternal sensitivity and (2) infant health in two critical domains. Our hypotheses were largely not supported, as maternal PTSS were not robustly associated with infant outcomes, and there was only one significant interaction between PTSS and depressive symptoms. Results indicated that observed maternal sensitivity was not related to maternal mental health factors or infant socioemotional and physical health outcomes, and thus was not assessed as a mediator. Instead, analyses revealed two significant predictors of infant socioemotional problems: postpartum depressive symptoms and parenting stress. Additionally, prenatal PTSS may serve as a risk factor for infant physical health problems, but only when mothers also have clinically significant levels of depressive symptoms in the postpartum period, which may be consistent with the DOHaD hypothesis. These findings add to our knowledge of how multiple maternal mental health factors are associated with infant outcomes and suggest that effects may differ for infant socioemotional versus physical health.
We first hypothesized that prenatal and postpartum PTSS would be positively associated with infant socioemotional and physical health problems, yet our results revealed no main effects of PTSS on either outcome. The lack of association between PTSS and infant socioemotional problems is in contrast to research conducted with older children (Garthus-Niegel et al., 2016; Greene et al., 2018; Pat-Horenczyk et al., 2015; van Ee et al., 2012) and limited work in infancy (Bosquet Enlow et al., 2011), wherein maternal PTSS were associated with higher levels of child socioemotional difficulties or internalizing and externalizing problems. The non-significant association between PTSS and infant physical health problems also departs from previous research demonstrating links between maternal psychological distress and health problems (e.g., Bush et al., 2021; et al., 2015; Zijlmans et al., 2017). Evidence suggests that PTSS in pregnancy alter infant stress responses through prenatal programming of the HPA axis (Lewis et al., 2014). As biological markers were not measured in this study (e.g., cortisol levels), it is unclear whether PTSS in pregnancy may have altered the infant stress response system but not yet influenced socioemotional and physical health outcomes, which may be more observable later in development. In addition to assessing biological markers, future studies should also include earlier indicators of infant dysfunction, such as reactivity in response to a laboratory stressor (Bosquet Enlow et al., 2009). Given that postpartum PTSS also were not related to socioemotional and physical health problems in infants, it is possible that maternal PTSS do not affect infants in the same way that other maternal mental health factors do, such as depressive symptoms. Depressive symptoms may impair mother-infant bonding and affect the developing parent-child relationship to a greater extent than PTSS (Moehler et al., 2006; Ohoka et al., 2014). Perhaps mothers’ PTSS (e.g., hypervigilance, angry outbursts) are more observable and thus more salient to older children, while depressive symptoms have more immediate effects on infants, as they may weaken mother-infant bonding and attachment.
We further hypothesized that there would be interactive effects of prenatal PTSS with postpartum PTSS, prenatal and postpartum depressive symptoms, and postpartum parenting stress on infant outcomes. We found a significant interaction between prenatal PTSS and postpartum depressive symptoms, such that prenatal PTSS predicted more infant physical health problems at 12 months of age, but only when mothers had high, not low, levels of postpartum depressive symptoms. These results address an important knowledge gap as no prior work has focused on maternal PTSS in pregnancy and infant physical health problems. This finding is consistent with the DOHaD hypothesis which posits that suboptimal exposures in the postpartum period set off the cascade of risk for socioemotional and physical health problems that originated with suboptimal exposures in utero. Future research should aim to replicate this effect to determine if this significant interaction is observed in other samples.
In contrast, the interactions between prenatal PTSS and postpartum PTSS, prenatal PTSS and prenatal depressive symptoms, and prenatal PTSS and postpartum parenting stress were not associated with infant socioemotional or physical health problems. Rather, postpartum depressive symptoms and parenting stress were each independently associated with greater infant socioemotional health problems. This finding is consistent with a large body of research showing that mothers’ postpartum depressive symptoms are associated with infant socioemotional health outcomes, (see Barnes & Theule, 2019; Madigan et al., 2018 for review). The current study also builds on prior work showing links between parenting stress and socioemotional outcomes in early and middle childhood (Anhalt et al., 2007; Sher-Censor, Shulman & Cohen, 2018), suggesting that effects of parenting stress on child well-being may be apparent as early as 12 months of life. It is possible that while prenatal depressive symptoms have a greater effect on biological mechanisms and infant stress reactivity, postpartum depressive symptoms and parenting stress have a greater influence on the current caregiving environment and affect infant functioning.
Lastly, we hypothesized that these maternal mental health factors and their interactions would be indirectly associated with infant socioemotional and physical health through observed maternal sensitivity measured during non-distressing and distressing tasks. Instead, maternal PTSS, depressive symptoms, and parenting stress were each unrelated to maternal sensitivity during the free play and frustration tasks, and maternal sensitivity was unrelated with socioemotional or physical health in infants. Although there is some evidence that maternal sensitivity is an important mechanism of the effect of parental functioning on infant socioemotional problems, these associations are not evident in all contexts (Augustine et al., 2019; Leerkes, 2011; Zhou et al., 2017). It may be useful to measure maternal sensitivity in more naturalistic situations (e.g., in response to infant crying in the real world). Moreover, there may be other parenting constructs that are related to both maternal mental health and infant outcomes, such as mother-infant bonding (Bosquet Enlow et al., 2014).
Strengths and Limitations
The present study has several significant strengths. First, we recruited a racially and ethnically diverse sample of women and children, all of whom were receiving public assistance. Due to structurally driven inequities, there are persistent and pronounced racial and ethnic disparities in rates of women living in poverty in the United States (National Academies of Sciences, Engineering, and Medicine, 2017). Given this systemic-level, rather than person-level, risk, examination of our research questions in this sample may contribute to the applicability of these results to multiple groups of people. Second, mothers enrolled in this study had significant socioeconomic adversity, and many had experienced some form of interpersonal violence in childhood or adulthood. Therefore, the current results may hold importance for mothers and their infants living in contexts of risk. Third, we included multiple maternal mental health factors in an effort to comprehensively understand both main and interactive effects of three highly relevant constructs (i.e., PTSS, depressive symptoms, parenting stress) on infant socioemotional and physical health problems. Very limited prior research has examined maternal PTSS and infant physical health problems. Lastly, even though few studies to date have investigated maternal PTSS and infant outcomes in the perinatal period, we moved the literature forward by testing a potentially critical, theoretically driven mechanism with useful clinical implications: maternal sensitivity.
This study also has several limitations that should be considered when interpreting results. First, gestational age at the prenatal time point varied widely; given that biological programming effects of maternal distress may differ based on stage of gestation (Lewis et al., 2014), future research should endeavor to understand how maternal PTSS contribute to alterations in the fetal stress response system at different points in fetal development, and how this specific timing in turn affects infant socioemotional and physical health outcomes. Second, although maternal sensitivity was assessed and coded from observations of two different interactional tasks, the other constructs examined in the study were obtained from maternal report. Thus, reporter bias may have contributed to the nature and strength of some associations. For instance, mothers who self-report high levels of depressive symptoms or parenting stress may be more likely to endorse high rates of behavior problems when completing questionnaires about their children (e.g., Van der Toorn et al., 2010). Future studies should attempt to replicate the current results using a multi-method, multi-informant approach (e.g., diagnostic interviews for maternal PTSS and depressive symptoms, clinician or teacher report of infant socioemotional functioning, health record data for infant physical health problems). Further, naturalistic observations of maternal sensitivity over extended periods of time may provide useful information that we are otherwise unable to capture through laboratory observation. We focused on the role of maternal sensitivity given past research and existing theory, but other aspects of parenting behavior may be more relevant for infants. Third, we chose to test PTSS, depressive symptoms, and parenting stress as the predictors and moderators in our models, but other types of maternal mental health problems may also be important, such as anxiety, substance use, and general emotion dysregulation. Further, other constructs may exacerbate or buffer PTSS (as well as depressive symptoms and parenting stress) including social support, use of clinical services, and even infant temperament. Although we attempted to examine comprehensive models of maternal mental health, additional research is needed to investigate other constructs and complete the picture of how mothers’ functioning and resource utilization affects infant well-being in the perinatal period. Fourth, although the current study includes data from two time points, it will be important for future studies to test associations among maternal mental health factors, parenting constructs, and infant outcomes using repeated measures over a longer period of time. This will be critical for determining both if and when maternal mental health factors contribute to the development of infant health problems.
Conclusions
In summary, we found that postpartum depressive symptoms and parenting stress, but not PTSS, were associated with greater infant socioemotional health problems. This study also provided novel evidence that prenatal PTSS are associated with greater infant physical health problems when mothers report clinically significant levels of depressive symptoms in the postpartum period. Unexpectedly, maternal sensitivity was not tested as an intermediary mechanism linking PTSS or other maternal mental health factors and infant outcomes given non-significant associations. The results of this study also point toward several clinical implications. Given our finding that postpartum depressive symptoms and parenting stress were associated with infant socioemotional health problems when infants are 12 months of age, it may be helpful to screen mothers for these mental health factors during a postpartum obstetrics/gynecology visit, or even during a visit with the infant’s pediatrician, given the frequency of interaction that pediatric providers have with new mothers (Accortt & Wong, 2017; Barkin & Van Cleve, 2020). Mothers with clinically significant depressive symptoms and/or high levels of parenting stress may then be referred to appropriate mental health providers. In addition, screening for both depressive symptoms and PTSS simultaneously may be particularly important, as the interaction between the two was shown to confer risk for infant physical health problems. Screening for a combination of maternal mental health factors at multiple points during the perinatal period may ensure that mothers’ symptoms are treated in a timely fashion, thus preventing the negative downstream effect to infants (Barkin & Van Cleve, 2020; Earls et al., 2019). The current results may also speak to the need for evidence-based treatments that address PTSS, depressive symptoms, and parenting stress together, as well as the dissemination of these treatments to mothers exposed to poverty and other forms of adversity (Beck & Driscoll, 2006; Waters et al., 2020). These efforts may ultimately prevent socioemotional and physical health problems among infants living in high-risk contexts.
Statement on Diversity and Anti-Racism.
The research presented in this manuscript was undertaken with an appreciation for diversity and an anti-racist approach. Understanding links between maternal perinatal posttraumatic stress symptoms and infant health and development is particularly relevant for women living in poverty as 14% of women facing socioeconomic adversity meet criteria for posttraumatic stress disorder during the perinatal period, and many more likely experience posttraumatic stress symptoms. Due to structurally driven inequities, there are persistent and pronounced racial and ethnic disparities in rates of women living in poverty. The current study examined research questions in a racially and ethnically diverse sample, reflective of the demographics of families involved in home visiting in Rhode Island. This manuscript aims to frame risk from a systemic- rather than person-level perspective, and careful choices of language are used throughout the manuscript as not to prescribe blame or bias to mothers based on background, race, ethnicity, or socioeconomic circumstances.
Key Findings for Practitioners.
1. Screening for and treating both postpartum depressive symptoms and parenting stress in new mothers may be important, given their association with greater socioemotional health problems in 12-month-old infants.
2. Infants with mothers who have prenatal posttraumatic stress symptoms and clinically significant depressive symptoms in postpartum are more likely to have physical health problems at 12 months of age.
3. Multiple maternal mental health factors (i.e., posttraumatic stress symptoms, depressive symptoms, and parenting stress) have different associations with infant socioemotional versus physical health outcomes.
Statement of Relevance.
Infant development occurs in the context of early relationships, such that infants’ outcomes are often tied to their parents’ functioning. The current research examines how maternal mental health, specifically posttraumatic stress and depressive symptoms, parenting stress, and their interactions, relates to infant socioemotional and physical health problems at 12 months of age. This study addresses a major gap by investigating how maternal posttraumatic stress in the perinatal period influences infant health in two critical domains.
Acknowledgments
This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number R40MC28318, Maternal and Child Health Field-initiated Innovative Research Studies Program (SHP). Drs. Huffhines and Coe received support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) under grant numbers F32HD100020 (LH) and T32HD101392 (JLC). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, the National Institutes of Health (NIH), HHS, or the U.S. Government. The authors have no conflicts of interest to disclose. The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Abidin RR (1995). Manual for the parenting stress index. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Accortt EE, & Wong MS (2017). It is time for routine screening for perinatal mood and anxiety disorders in obstetrics and gynecology settings. Obstetrical & gynecological survey, 72(9), 553–568. doi: 10.1097/OGX.0000000000000477 [DOI] [PubMed] [Google Scholar]
- Agius A, Xuereb RB, Carrick-Sen D, Sultana R, & Rankin J (2016). The co-existence of depression, anxiety and post-traumatic stress symptoms in the perinatal period: a systematic review. Midwifery, 36, 70–79. 10.1016/j.midw.2016.02.013 [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG, & Reno RR (1991). Multiple regression: Testing and interpreting interactions. sage. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. 10.1177/0306624X13511040 [DOI] [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC. [Google Scholar]
- Anhalt K, Telzrow CF, & Brown CL (2007). Maternal stress and emotional status during the perinatal period and childhood adjustment. School Psychology Quarterly, 22(1), 74. 10.1037/1045-3830.22.1.74 [DOI] [Google Scholar]
- Augustine ME, & Leerkes EM (2019). Associations between maternal physiology and maternal sensitivity vary depending on infant distress and emotion context. Journal of Family Psychology, 33(4), 412–421. 10.1037/fam0000538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes J, & Theule J (2019). Maternal depression and infant attachment security: A meta-analysis. Infant mental health journal, 40(6), 817–834. 10.1002/imhj.21812 [DOI] [PubMed] [Google Scholar]
- Beck CT, & Driscoll J (2006). Postpartum mood and anxiety disorders: A clinician's guide. Jones & Bartlett Learning. [Google Scholar]
- Becker-Sadzio J, Gundel F, Kroczek A, Wekenmann S, Rapp A, Fallgatter AJ, & Deppermann S (2020). Trauma exposure therapy in a pregnant woman suffering from complex posttraumatic stress disorder after childhood sexual abuse: risk or benefit?. European Journal of Psychotraumatology, 11(1), 1697581. 10.1080/20008198.2019.1697581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beijers R, Jansen J, Riksen-Walraven M, & de Weerth C (2010). Maternal prenatal anxiety and stress predict infant illnesses and health complaints. Pediatrics, 126(2), e401–e409. 10.1542/peds.2009-3226 [DOI] [PubMed] [Google Scholar]
- Belsky J, Bell B, Bradley RH, Stallard N, & Stewart-Brown SL (2007). Socioeconomic risk, parenting during the preschool years and child health age 6 years. European Journal of Public Health, 17(5), 508–513. 10.1093/eurpub/ckl261 [DOI] [PubMed] [Google Scholar]
- Bernard K, Nissim G, Vaccaro S, Harris JL, & Lindhiem O (2018). Association between maternal depression and maternal sensitivity from birth to 12 months: a meta-analysis. Attachment & human development, 20(6), 578–599. 10.1080/14616734.2018.1430839 [DOI] [PubMed] [Google Scholar]
- Booth AT, Macdonald JA, & Youssef GJ (2018). Contextual stress and maternal sensitivity: A meta-analytic review of stress associations with the Maternal Behavior Q-Sort in observational studies. Developmental Review, 48, 145–177. 10.1016/j.dr.2018.02.002 [DOI] [Google Scholar]
- Bosquet Enlow M, Egeland B, Carlson E, Blood E, & Wright RJ (2014). Mother–infant attachment and the intergenerational transmission of posttraumatic stress disorder. Development and psychopathology, 26(1), 41–65. 10.1017/S0954579413000515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosquet Enlow M, Kitts RL, Blood E, Bizarro A, Hofmeister M, & Wright RJ (2011). Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behavior and Development, 34(4), 487–503. 10.1016/j.infbeh.2011.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosquet Enlow M, Kullowatz A, Staudenmayer J, Spasojevic J, Ritz T, & Wright RJ (2009). Associations of maternal lifetime trauma and perinatal traumatic stress symptoms with infant cardiorespiratory reactivity to psychological challenge. Psychosomatic Medicine, 71(6), 607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, McCarthy K, Augustyn M, Caronna E, & Clark R (2013). Clinical validity of a brief measure of early childhood social–emotional/behavioral problems. Journal of pediatric psychology, 38(5), 577–587. 10.1093/jpepsy/jst014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, & Cicchetti DV (2004). The Brief Infant-Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. Journal of pediatric psychology, 29(2), 143–155. 10.1093/jpepsy/jsh017 [DOI] [PubMed] [Google Scholar]
- Carter AS, & Briggs-Gowan MJ (2006). Manual for the Infant-Toddler Social & Emotional Assessment (ITSEA)—Version 2. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bale TL (2014). Lifetime stress experience: transgenerational epigenetics and germ cell programming. Dialogues in Clinical Neuroscience, 16(3), 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJ (2004). The developmental origins of chronic adult disease. Acta Paediatrica, 93, 26–33. [DOI] [PubMed] [Google Scholar]
- Barkin JL, & Van Cleve S (2020). Screening for maternal mental health in the pediatric setting: Situational stressors and supports. Journal of Pediatric Health Care, 34(5), 405–406. 10.1016/j.pedhc.2020.04.001 [DOI] [PubMed] [Google Scholar]
- Biringen Z, Robinson JL, & Emde RN (2000). Appendix B: The emotional availability scales (an abridged infancy/early childhood version). Attachment & human development, 2(2), 256–270. 10.1080/14616730050085626 [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, & Mancill RB (2001). Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of abnormal psychology, 110(4), 585–599. 10.1037/0021-843X.110.4.585 [DOI] [PubMed] [Google Scholar]
- Buchmann AF, Kopf D, Westphal S, Lederbogen F, Banaschewski T, Esser G, … & Deuschle M (2010). Impact of early parental child-rearing behavior on young adults’ cardiometabolic risk profile: a prospective study. Psychosomatic medicine, 72(2), 156–162. 10.1097/PSY.0b013e3181c88343 [DOI] [PubMed] [Google Scholar]
- Bush NR, Savitz J, Coccia M, Jones-Mason K, Adler N, Boyce WT, … & Epel E (2021). Maternal stress during pregnancy predicts infant infectious and noninfectious illness. The Journal of Pediatrics, 228, 117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CH, Lin SK, Tang HS, Shen WW, & Lu ML (2001). The Chinese version of the Davidson Trauma Scale: a practice test for validation. Psychiatry and clinical neurosciences, 55(5), 493–499. 10.1046/j.1440-1819.2001.00895.x [DOI] [PubMed] [Google Scholar]
- Cho B, Woods-Jaeger B, & Borelli JL (2020). Parenting Stress Moderates the Relation between Parental Trauma Exposure and Child Anxiety Symptoms. Child Psychiatry & Human Development, 1–10. 10.1007/s10578-020-01087-1 [DOI] [PubMed] [Google Scholar]
- Christie H, Hamilton-Giachritsis C, Alves-Costa F, Tomlinson M, & Halligan SL (2019). The impact of parental posttraumatic stress disorder on parenting: A systematic review. European journal of psychotraumatology, 10(1), 1550345. 10.1080/20008198.2018.1550345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook CAL, Flick LH, Homan SM, Campbell C, McSweeney M, & Gallagher ME (2004). Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstetrics & Gynecology, 103(4), 710–717. 10.1097/01.AOG.0000119222.40241.fb [DOI] [PubMed] [Google Scholar]
- Cook N, Ayers S, & Horsch A (2018). Maternal posttraumatic stress disorder during the perinatal period and child outcomes: A systematic review. Journal of affective disorders, 225, 18–31. 10.1016/j.jad.2017.07.045 [DOI] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, & Kilpatrick DG (2009). PTSD, depression, and their comorbidity in relation to suicidality: cross-sectional and prospective analyses of a national probability sample of women. Depression and Anxiety, 26(12), 1151–1157. 10.1002/da.20621 [DOI] [PubMed] [Google Scholar]
- Davidson J Davidson Trauma Scale (DTS). Tonawanda, New York: Multi-Health Systems Inc.; 1996. [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, … & Feldman ME (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological medicine, 27(1), 153–160. 10.1017/s0033291796004229 [DOI] [PubMed] [Google Scholar]
- DeSocio JE (2018). Epigenetics, maternal prenatal psychosocial stress, and infant mental health. Archives of Psychiatric Nursing, 32(6), 901–906. [DOI] [PubMed] [Google Scholar]
- Earls MF, Yogman MW, Mattson G, Rafferty J, & Committee on Psychosocial Aspects of Child and Family Health. (2019). Incorporating recognition and management of perinatal depression into pediatric practice. Pediatrics, 143(1), e20183259. 10.1542/peds.2018-3259 [DOI] [PubMed] [Google Scholar]
- Epifanio MS, Genna V, De Luca C, Roccella M, & La Grutta S (2015). Paternal and maternal transition to parenthood: the risk of postpartum depression and parenting stress. Pediatric reports, 7(2), 38–44. 10.4081/pr.2015.5872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson N, Julian M, & Muzik M (2019). Perinatal depression, PTSD, and trauma: Impact on mother–infant attachment and interventions to mitigate the transmission of risk. International review of psychiatry, 31(3), 245–263. 10.1080/09540261.2018.1563529 [DOI] [PubMed] [Google Scholar]
- Farrell AK, Waters TE, Young ES, Englund MM, Carlson EE, Roisman GI, & Simpson JA (2019). Early maternal sensitivity, attachment security in young adulthood, and cardiometabolic risk at midlife. Attachment & human development, 21(1), 70–86. 10.1080/14616734.2018.1541517 [DOI] [PubMed] [Google Scholar]
- Feeley N, Zelkowitz P, Cormier C, Charbonneau L, Lacroix A, & Papageorgiou A (2011). Posttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal intensive care unit. Applied Nursing Research, 24, 114–117. [DOI] [PubMed] [Google Scholar]
- Garcia ER, & Yim IS (2017). A systematic review of concepts related to women’s empowerment in the perinatal period and their associations with perinatal depressive symptoms and premature birth. BMC pregnancy and childbirth, 17(2), 1–13. 10.1186/s12884-017-1495-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garthus-Niegel S, Ayers S, Martini J, Von Soest T, & Eberhard-Gran M (2017). The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based, 2-year follow-up study. Psychological medicine, 47(1), 161–170. 10.1017/S003329171600235X [DOI] [PubMed] [Google Scholar]
- Graham KA, Blissett J, Antoniou EE, Zeegers MP, & McCleery JP (2018). Effects of maternal depression in the Still-Face Paradigm: A meta-analysis. Infant Behavior and Development, 50, 154–164. [DOI] [PubMed] [Google Scholar]
- Greene CA, Chan G, McCarthy KJ, Wakschlag LS, & Briggs-Gowan MJ (2018). Psychological and physical intimate partner violence and young children’s mental health: The role of maternal posttraumatic stress symptoms and parenting behaviors. Child abuse & neglect, 77, 168–179. 10.1016/j.chiabu.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groh AM, & Narayan AJ (2019). Infant attachment insecurity and baseline physiological activity and physiological reactivity to interpersonal stress: A meta-analytic review. Child Development, 90(3), 679–693. [DOI] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, & Allaire JC (2006). Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child & Adolescent Psychology, 35(2), 302–312. 10.1207/s15374424jccp3502_14 [DOI] [PubMed] [Google Scholar]
- Hartzell G, Stenson AF, van Rooij SJ, Kim YJ, Vance LA, Hinrichs R, … & Jovanovic T (2020). Intergenerational effects of maternal PTSD: Roles of parenting stress and child sex. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, & Matthes J (2009). Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior research methods, 41(3), 924–936. 10.3758/BRM.41.3.924 [DOI] [PubMed] [Google Scholar]
- Huizink AC, Menting B, De Moor MHM, Verhage ML, Kunseler FC, Schuengel C, & Oosterman M (2017). From prenatal anxiety to parenting stress: a longitudinal study. Archives of women's mental health, 20(5), 663–672. 10.1007/s00737-017-0746-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain KM, Davey-Rothwell M, Crossnohere NL, & Latkin CA (2018). Post-traumatic stress disorder, neighborhood residency and satisfaction, and social network characteristics among underserved women in Baltimore, Maryland. Women's Health Issues, 28(3), 273–280. 10.1016/j.whi.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PO, & Neyman J (1936). Tests of certain linear hypotheses and their application to some educational problems. Statistical research memoirs. [Google Scholar]
- Kocalevent RD, Hinz A, & Brähler E (2013). Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. General hospital psychiatry, 35(5), 551–555. 10.1016/j.genhosppsych.2013.04.006 [DOI] [PubMed] [Google Scholar]
- Kozyrskyj AL, Mai XM, McGrath P, HayGlass KT, Becker AB, & MacNeil B (2008). Continued exposure to maternal distress in early life is associated with an increased risk of childhood asthma. American journal of respiratory and critical care medicine, 177(2), 142–147. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, & Hasbun A (2014). Association between parents’ PTSD severity and children's psychological distress: A meta-analysis. Journal of traumatic stress, 27(1), 9–17. 10.1002/jts.21891 [DOI] [PubMed] [Google Scholar]
- Lamberts H, & Wood M (Eds.). (1987). ICPC, international classification of primary care. Oxford University Press, USA. [Google Scholar]
- Leerkes EM (2011). Maternal sensitivity during distressing tasks: A unique predictor of attachment security. Infant Behavior and Development, 34(3), 443–446. 10.1016/j.infbeh.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leerkes EM, Blankson AN and O’Brien M (2009), Differential Effects of Maternal Sensitivity to Infant Distress and Nondistress on Social-Emotional Functioning. Child Development, 80: 762–775. 10.1111/j.1467-8624.2009.01296.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leerkes EM, & Wong MS (2012). Infant distress and regulatory behaviors vary as a function of attachment security regardless of emotion context and maternal involvement. Infancy, 17(5), 455–478. 10.1111/j.1532-7078.2011.00099.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis AJ, Galbally M, Gannon T, & Symeonides C (2014). Early life programming as a target for prevention of child and adolescent mental disorders. BMC Medicine, 12(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons-Ruth K, & Block D (1996). The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Mental Health Journal: Official Publication of The World Association for Infant Mental Health, 17(3), 257–275. [DOI] [Google Scholar]
- Mackinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan S, Oatley H, Racine N, Fearon RP, Schumacher L, Akbari E, … & Tarabulsy GM (2018). A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. Journal of the American Academy of Child & Adolescent Psychiatry, 57(9), 645–657. 10.1016/j.jaac.2018.06.012 [DOI] [PubMed] [Google Scholar]
- Mäntymaa M, Puura K, Luoma I, Salmelin R, Davis H, Tsiantis J, … & Tamminen T (2003). Infant–mother interaction as a predictor of child's chronic health problems. Child: Care, health and development, 29(3), 181–191. [DOI] [PubMed] [Google Scholar]
- McDonald SD, Beckham JC, Morey RA, & Calhoun PS (2009). The validity and diagnostic efficiency of the Davidson Trauma Scale in military veterans who have served since September 11th, 2001. Journal of anxiety disorders, 23(2), 247–255. 10.1016/j.janxdis.2008.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell AE, Morawska A, & Mihelic M (2020). A systematic review of parenting interventions for child chronic health conditions. Journal of Child Health Care, 24(4), 603–628. 10.1177/1367493519882850 [DOI] [PubMed] [Google Scholar]
- Moehler E, Brunner R, Wiebel A, Reck C, & Resch F (2006). Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother–child bonding. Archives of women's mental health, 9(5), 273–278. 10.1007/s00737-006-0149-5 [DOI] [PubMed] [Google Scholar]
- Molgora S, Fenaroli V, & Saita E (2020). The association between childbirth experience and mother’s parenting stress: The mediating role of anxiety and depressive symptoms. Women & health, 60(3), 341–351. 10.1080/03630242.2019.1635563 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). Communities in action: Pathways to health equity. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Ohoka H, Koide T, Goto S, Murase S, Kanai A, Masuda T, … & Ozaki N (2014). Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant–mother attachment. Psychiatry and clinical neurosciences, 68(8), 631–639. 10.1111/pcn.12171 [DOI] [PubMed] [Google Scholar]
- Olff M (2017). Sex and gender differences in post-traumatic stress disorder: an update. European journal of psychotraumatology, 8, 1351204. 10.1080/20008198.2017.1351204 [DOI] [Google Scholar]
- Pat-Horenczyk R, Cohen S, Ziv Y, Achituv M, Asulin-Peretz L, Blanchard TR, … & Brom D (2015). Emotion regulation in mothers and young children faced with trauma. Infant mental health journal, 36(3), 337–348. 10.1002/imhj.21515 [DOI] [PubMed] [Google Scholar]
- Perry NB, Calkins SD, & Bell MA (2016). Indirect effects of maternal sensitivity on infant emotion regulation behaviors: The role of vagal withdrawal. Infancy, 21(2), 128–153. 10.1111/infa.12101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan AL, DiBenedetto MR, Paul IM, Zhu J, & Kjerulff KH (2015). Psychosocial stress during first pregnancy predicts infant health outcomes in the first postnatal year. Maternal and child health journal, 19(12), 2587–2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Legrand AC, Brier ZM, & Hébert-Dufresne L (2019). The symptoms at the center: examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. Journal of psychiatric research, 109, 52–58. 10.1016/j.jpsychires.2018.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuelson KW, Wilson CK, Padrón E, Lee S, & Gavron L (2017). Maternal PTSD and children's adjustment: Parenting stress and emotional availability as proposed mediators. Journal of Clinical Psychology, 73(6), 693–706. 10.1002/jclp.22369 [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, & Card NA (2010). Best practices for missing data management in counseling psychology. Journal of Counseling psychology, 57(1), 1. 10.1037/a0018082 [DOI] [PubMed] [Google Scholar]
- Seng JS, Low LMK, Sperlich M, Ronis DL, & Liberzon I (2009). Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics and gynecology, 114(4), 839. 10.1097/AOG.0b013e3181b8f8a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher-Censor E, Shulman C, & Cohen E (2018). Associations among mothers’ representations of their relationship with their toddlers, maternal parenting stress, and toddlers’ internalizing and externalizing behaviors. Infant Behavior and Development, 50, 132–139. 10.1016/j.infbeh.2017.12.005 [DOI] [PubMed] [Google Scholar]
- Stern JA, Beijers R, Ehrlich KB, Cassidy J, & de Weerth C (2020). Beyond Early Adversity: The Role of Parenting in Infant Physical Health. Journal of Developmental & Behavioral Pediatrics, 41(6), 452–460. 10.1097/DBP.0000000000000804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung I, Keenan K, Stepp SD, & Hipwell AE (2020). The moderating effects of traumatic stress on vulnerability to emotional distress during pregnancy. Development and psychopathology, 32(2), 673–686. doi: 10.1017/S0954579419000531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrka AR, Ridout KK, Parade SH, Paquette A, Marsit CJ, & Seifer R (2015). Childhood maltreatment and methylation of FKBP5. Development and psychopathology, 27(4 Pt 2), 1637. doi: 10.1017/S0954579415000991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bergh BR, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, … & Schwab M (2017). Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neuroscience & Biobehavioral Reviews. 10.1016/j.neubiorev.2017.07.003 [DOI] [PubMed] [Google Scholar]
- Van der Toorn SL, Huizink AC, Utens EM, Verhulst FC, Ormel J, & Ferdinand RF (2010). Maternal depressive symptoms, and not anxiety symptoms, are associated with positive mother–child reporting discrepancies of internalizing problems in children: a report on the TRAILS Study. European child & adolescent psychiatry, 19(4), 379–388. 10.1007/s00787-009-0062-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ee E, Kleber RJ, & Mooren TT (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant mental health journal, 33(5), 459–468. 10.1002/imhj.21324 [DOI] [PubMed] [Google Scholar]
- Van Ee E, Kleber RJ, & Jongmans MJ (2016). Relational patterns between caregivers with PTSD and their nonexposed children: A review. Trauma, Violence, & Abuse, 17(2), 186–203. 10.1177/1524838015584355 [DOI] [PubMed] [Google Scholar]
- Vehmeijer FO, Guxens M, Duijts L, & El Marroun H (2019). Maternal psychological distress during pregnancy and childhood health outcomes: A narrative review. Journal of Developmental Origins of Health and Disease, 10(3), 274–285. [DOI] [PubMed] [Google Scholar]
- Vignato J, Connelly CD, Bush RA, Georges JM, Semino-Asaro S, Calero P, & Horwitz SM (2018). Correlates of perinatal post-traumatic stress among culturally diverse women with depressive symptomatology. Issues in mental health nursing, 39(10), 840–849. 10.1080/01612840.2018.1488313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara L, Rollè L, Agostini F, Sechi C, Fenaroli V, Molgora S, … & Tambelli R (2016). Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3-to 6-months postpartum follow-up study. Frontiers in psychology, 7, 938. 10.3389/fpsyg.2016.00938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Kroenke K, Stump TE, & Monahan PO (2020). Screening for perinatal depression with the patient health questionnaire depression scale (PHQ-9): A systematic review and meta-analysis. General hospital psychiatry. 10.1016/j.genhosppsych.2020.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters CS, Annear B, Flockhart G, Jones I, Simmonds JR, Smith S, … & Williams JF (2020). Acceptance and Commitment Therapy for perinatal mood and anxiety disorders: A feasibility and proof of concept study. British Journal of Clinical Psychology, 59(4), 461–479. 10.1111/bjc.12261 [DOI] [PubMed] [Google Scholar]
- Wilson CK, Padrón E, & Samuelson KW (2017). Trauma type and posttraumatic stress disorder as predictors of parenting stress in trauma-exposed mothers. Violence and victims, 32(1), 141–158. DOI: 10.1891/0886-6708.VV-D-13-00077 [DOI] [PubMed] [Google Scholar]
- Wright RJ, Cohen S, Carey V, Weiss ST, & Gold DR (2002). Parental stress as a predictor of wheezing in infancy: a prospective birth-cohort study. American journal of respiratory and critical care medicine, 165(3), 358–365. [DOI] [PubMed] [Google Scholar]
- Wu Q, Feng X, Hooper EG, Gerhardt M, Ku S, & Chan MHM (2019). Mother's emotion coaching and preschooler's emotionality: Moderation by maternal parenting stress. Journal of Applied Developmental Psychology, 65, 101066. 10.1016/j.appdev.2019.101066 [DOI] [Google Scholar]
- Zhang T, Zhao L, Ding W, Ma J, & Zhang Y (2020). The influence of perinatal and maternal factors on physical growth at 12 months in prematurely born infants treated in the neonatal intensive care unit: A retrospective chart review and a prospective cohort study. International Journal of Nursing Studies, 109, 103656. 10.1016/j.ijnurstu.2020.103656 [DOI] [PubMed] [Google Scholar]
- Zhou N, Cao H, & Leerkes EM (2017). Interparental conflict and infants’ behavior problems: The mediating role of maternal sensitivity. Journal of Family Psychology, 31(4), 464–474. 10.1037/fam0000288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijlmans MA, Beijers R, Riksen-Walraven MJ, & de Weerth C (2017). Maternal late pregnancy anxiety and stress is associated with children’s health: A longitudinal study. Stress, 20(5), 495–504. [DOI] [PubMed] [Google Scholar]


