Abstract
Objective
To determine how sociodemographic factors impact cervical cancer survival in different geographic locations in the USA.
Methods
A retrospective cohort of patients with cervical cancer from January 1, 2004 to December 31, 2015 in the National Cancer Database (NCDB) was identified. Tumor characteristics as well as race, income, insurance type, and treating facility types were compared among nine geographic regions. χ2 tests and Cox regression were used to compare differences between regions; p values <0.05 were considered significant.
Results
A total of 48 787 patients were included. Survival was inferior in seven of nine regions for underinsured patients. In six regions survival was inferior for Medicaid and Medicare patients, respectively: Middle Atlantic: hazard ratio (HR) 1.25 and 1.22; South Atlantic: HR 1.41 and HR 1.22; East North Central: HR 1.36 and HR 1.25; East South Central: HR 1.37 and HR 1.25; West North Central: HR 1.67 and HR 1.42; West South Central: HR 1.44 and HR 1.46. In the Pacific region survival was inferior for Medicare patients (HR 1.35) but not inferior for Medicaid patients. Being uninsured was associated with worse survival in the South Atlantic (HR 1.23), East North Central (HR 1.23), East South Central (HR 1.56), and West South Central (HR 1.31) regions. Annual income level under $38 000 was associated with worse survival in the Middle Atlantic (HR 1.24), South Atlantic (HR 1.35), and East North Central (HR 1.49) regions. Lastly, when compared with academic research institutions, comprehensive community cancer centers had significantly worse survival in four of the nine regions.
Conclusions
Cervical cancer mortality is higher for women with a low income, underinsured (Medicaid or Medicare) or uninsured status, and decreased access to academic institutions in most US regions. An increase in cervical cancer mortality was associated with underinsured or uninsured populations in regions mainly located in the South and Midwest.
INTRODUCTION
The incidence of cervical cancer in the USA has decreased by almost 50% in the last 25 years, which is generally attributed to ongoing preventive measures.1 2 While the decrease in cases has been successful, cervical cancer remains a public health challenge and also a morbid disease. In 2022 there will be an estimated 14 100 new cases and about 4280 deaths, making it the third most common gynecologic cancer.3 Epidemiologic studies have shown significant declines in cervical intra-epithelial neoplasia caused by high-risk human papilloma virus (HPV) 16 and 18, which are responsible for 70% of cervical cancers worldwide.4 Most recently, nationwide data from Sweden showed a significant decrease in the risk of the development of cervical cancer for women who received the quadrivalent HPV vaccine, with the most pronounced reduction in those aged <17 years with an incidence rate ratio of 0.12 (95% CI 0.00 to 0.34).5 Unfortunately, in the USA, gains largely due to preventive measures have not been equally distributed across racial, socioeconomic, and geographic lines.
Health insurance coverage varies regionally across the USA, and while many large databases use insurance coverage as a surrogate for access to care, there are other factors to consider when examining outcomes in cervical cancer. For instance, women in Texas with lower socioeconomic status were more likely to experience an advanced stage diagnosis even when controlling for race and other factors. While Hispanic women in Texas were more likely to present with advanced stage, this does not necessarily translate to worse survival compared with other races. Texas-based studies have also established that there are decreasing levels of disparities, suggesting outreach and other state-based interventions could have a positive effect on outcomes.6
The further a patient with cervical cancer lives from a comprehensive cancer center, the worse their survival appears to be. While these findings cross racial lines, there is a clear exacerbation of this impact in low income African American women, especially in Southern states.7-9 Decreased access to care in this population leads to decreased screening rates and decreased standard of care treatment options. Sharp declines in brachytherapy use have been observed in certain parts of the country despite data showing that brachytherapy improves cause-specific survival and overall survival nationally. However, that survival benefit may not be equally shared across the country as one California-based study showed decreased survival in low socioeconomic status and black populations despite the use of brachytherapy.10 11
Given variable trends in cervical cancer screening, treatment practices, and healthcare insurance coverage across the USA, we set out to determine what factors impact cervical cancer mortality in nine different geographic regions across the USA using data from a national database. These regions are grouped by the National Cancer Database (NCDB) and have natural variation along social, population number and density, demographic, and economic lines. Our hypothesis is that survival differs across cervical cancer populations depending on the region, and the impact of regional differences varies based on sociodemographic factors—namely, insurance status. Different types of insurance include insured (private insurance), Medicaid and Medicare, which are forms of government-sponsored insurance for low income or elderly populations, respectively (underinsured), and uninsured (no insurance).
METHODS
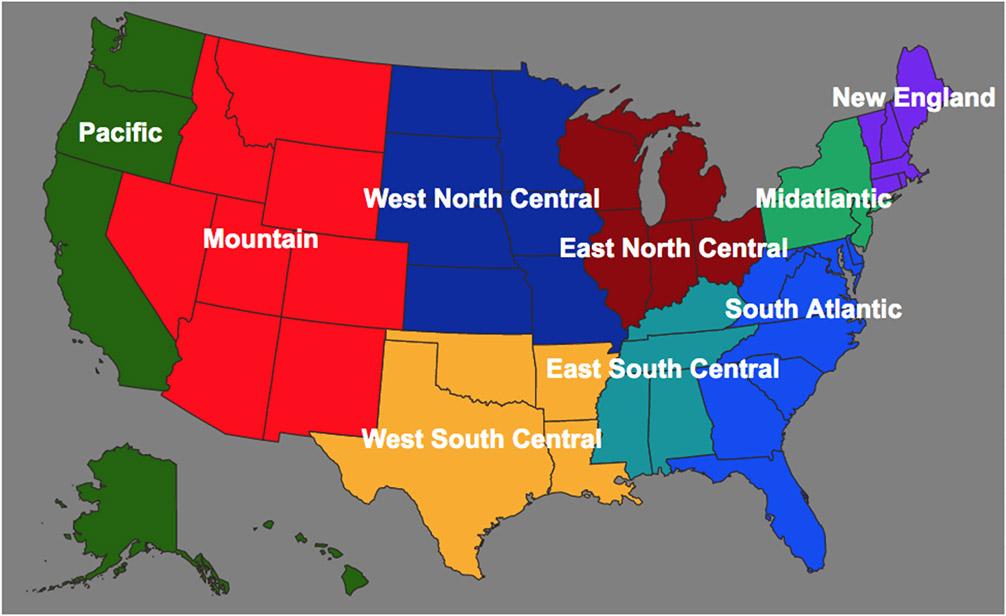
A retrospective population-based cohort study was performed among patients in the NCDB from January 1, 2004 to December 31, 2015 diagnosed with cervical cancer. The NCDB is sourced from tumor registries across the USA and is thought to represent over 70% of cancer cases.12 The NCDB groups cases into nine geographic regions used in the analysis: New England, Middle Atlantic, South Atlantic, East North Central, East South Central, West North Central, West South Central, Mountain, and Pacific (Figure 1). Populations were stratified by these regions.
Figure 1.
Nine National Cancer Database regions.
Extracted patient characteristics included patient race, income, insurance type, and facility type where treatment was administered. Additionally, cancer-specific characteristics including stage, tumor grade, nodal status, and histology were collected. Reference variables are shown in Table 1. Facility types included academic comprehensive cancer programs including National Cancer Institute (NCI) comprehensive cancer centers, integrated network cancer programs, community cancer programs, and comprehensive community cancer programs.13 Patients diagnosed and treated for cervical cancer during this time frame were eligible and patients were included in the regression analysis if they had data available for all of the data elements; those with missing data were excluded. Additional exclusions were rare histologies and age <18 years. Survival was the main outcome, which was measured in months from the date of diagnosis to death from any cause. Outcomes were compared based on the region in which they were treated.
Table 1.
Cervical cancer mortality among all National Cancer Database (NCDB) regions based on clinical and demographic variables
| Variable | HR (95% CI) | P value |
|---|---|---|
| Disease stage | ||
| Microscopic | Reference | |
| Stage IB–IIA2 | 1.60 (1.41 to 1.74) | <0.0001 |
| Stage IIB–IVA | 2.90 (2.60 to 3.23) | <0.0001 |
| Stage IVB | 6.09 (5.42 to 6.83) | <0.0001 |
| Histology | ||
| Squamous | Reference | |
| Adenocarcinoma | 1.17 (1.12 to 1.23) | <0.0001 |
| Adenosquamous | 1.12 (1.02 to 1.23) | 0.0197 |
| Clear cell | 1.56 (1.34 to 1.81) | <0.0001 |
| Grade | ||
| Well differentiated | Reference | |
| Moderately differentiated | 1.22 (1.11 to 1.34) | <0.0001 |
| Poorly/undifferentiated | 1.45 (1.32 to 1.59) | <0.0001 |
| Nodal status | ||
| Negative | Reference | |
| 1 Positive | 1.41 (1.23 to 1.62) | <0.0001 |
| 2–3 Positive | 1.72 (1.48 to 1.99) | <0.0001 |
| ≥4 Positive | 2.52 (1.94 to 2.62) | <0.0001 |
| Race | ||
| White, non-Hispanic | Reference | |
| Black, non-Hispanic | 1.02 (0.97 to 1.07) | 0.46 |
| Hispanic | 0.68 (0.63 to 0.73) | <0.0001 |
| Other, non-Hispanic | 0.79 (0.72 to 0.86) | <0.0001 |
| Insurance status | ||
| Insured | Reference | |
| Not Insured | 1.21 (1.13 to 1.29) | <0.0001 |
| Medicaid | 1.34 (1.27 to 1.41) | <0.0001 |
| Medicare | 1.25 (1.19 to 1.33) | <0.0001 |
| Income by quartile | ||
| ≥$63 000 | Reference | |
| $48 000–$62 999 | 1.11 (1.04 to 1.17) | 0.0013 |
| $38 000–$47 999 | 1.16 (1.08 to 1.24) | <0.0001 |
| <$38 000 | 1.24 (1.15 to 1.33) | <0.0001 |
| Treatment facility | ||
| Academic/research program | Reference | |
| Community cancer program | 1.07 (0.99 to 1.15) | 0.0598 |
| Integrated network cancer program | 1.10 (1.03 to 1.17) | 0.0051 |
| Comprehensive community cancer program | 1.10 (1.05 to 1.15) | <0.0001 |
HR, hazard ratio.
χ2 tests and Cox proportional hazard regression were performed to compare differences among regions adjusting for the aforementeiond variables; p<0.05 was considered statistically significant. Statistical analysis was performed using Statistical Analysis System (SAS) v.9.4 (SAS Institute Inc, Cary, North Carolina, USA). In accordance with the journal’s guidelines, public use data are available at https://www.facs.org/quality-programs/cancer/ncdb/puf and SAS analyzed data can be provided for the reproducibility of this study if such is requested.
This study is Institutional Review Board exempt.
RESULTS
A total of 48 787 patients were identified from the NCDB who met the inclusion criteria and were entered into the analysis. The mean number of patients per region was 5420 (range 1895—10 206). Exclusions for missing data included: 3382 insurance data, 28 905 regional data, and 6319 ethnicity data. The majority of patients were white and had squamous histology. Among all the variables, stage IIB–IVA (HR 2.9; 95% CI 2.60 to 3.23, p<0.001) and stage IVB cervical cancers (HR 6.09; 95% CI 5.42 to 6.83, p<0.0001), poorly differentiated tumors (HR 1.45; 95% CI 1.32 to 1.59, p<0.0001), clear cell histology (HR 1.56; 95% CI 1.34 to 1.81, p<0.0001), and ≥4 positive regional lymph nodes (HR 2.52; 95% CI 1.94 to 2.62, p<0.001) were the tumor characteristics associated with the poorest survival in all regions per multiple variable logistic regression (Table 1). Interestingly, when compared with white non-Hispanic women, Hispanic women (HR 0.68; 95% CI 0.63 to 0.73, p<0.0001) appeared to have a lower risk of cervical cancer mortality in the entire study population; this trend was also realized in those classified as non-Hispanic non-white and non-black termed ‘non-Hispanic other’ (HR 0.79; 95% CI 0.72 to 0.86, p<0.001).
Cervical cancer mortality per region based on insurance status including the receipt of Medicaid or Medicare is shown in Table 2. Survival was inferior in seven of nine regions when comparing insured to Medicaid and/or Medicare patients within each region (Middle Atlantic: HR 1.25, p=0.002 and 1.22, p=0.005); (South Atlantic: HR 1.41, p<0.0001 and HR 1.22 p=0.002); (East North Central: HR 1.36, p<0.0001 and HR 1.25, p=0.001); (East South Central: HR 1.37, p=0.0003 and HR 1.25, p=0.012); (West North Central: HR 1.67, p<0.0001 and HR 1.42, p=0.002); (West South Central: HR 1.44, p<0.0001 and HR 1.46, p=0.0002); (Pacific: HR 1.35, p=0.0009 for Medicare only). Insurance status differences did not affect survival in the New England and Mountain regions, and in the Pacific region decreased survival was only seen in the Medicare population. This is depicted in Figure 2, which shows the NCDB regions with significantly worse survival among cervical cancer patients insured by Medicaid. Uninsured patients had differential survival in the South Atlantic (HR 1.23, p=0.004), East North Central (HR 1.23, p=0.013), East South Central (HR 1.56, p<0.0001), and West South Central (HR 1.31, p=0.0069) regions only. Uninsured patients in the New England, Middle Atlantic, West North Central, Mountain, and Pacific regions did not have differential survival.
Table 2.
Cervical cancer mortality among patients with Medicaid or Medicare (underinsured) and uninsured according to National Cancer Database region (n=48 787)
| Insurance | No of patients | Region | Hazard ratio (95% CI) | P value |
|---|---|---|---|---|
| New England | 2028 | Insurance | Reference | |
| Uninsured | 0.64 (0.37 to 1.11) | 0.11 | ||
| Medicaid | 1.30 (0.96 to 1.77) | 0.09 | ||
| Medicare | 1.02 (0.74 to 1.42) | 0.88 | ||
| Middle Atlantic | 7675 | Insurance | Reference | |
| Uninsured | 1.12 (0.91 to 1.38) | 0.29 | ||
| Medicaid | 1.25 (1.09 to 1.43) | 0.00170 | ||
| Medicare | 1.22 (1.06 to 1.41) | 0.0054 | ||
| South Atlantic | 10 206 | Insurance | Reference | |
| Uninsured | 1.23 (1.07 to 1.41) | 0.004 | ||
| Medicaid | 1.41 (1.26 to 1.57) | <0.0001 | ||
| Medicare | 1.22 (1.08 to 1.38) | 0.0016 | ||
| East North Central | 8275 | Insurance | Reference | |
| Uninsured | 1.23 (1.04 to 1.44) | 0.013 | ||
| Medicaid | 1.36 (1.20 to 1.54) | <0.0001 | ||
| Medicare | 1.25 (1.09 to 1.42) | 0.0012 | ||
| East South Central | 4140 | Insurance | Reference | |
| Uninsured | 1.56 (1.27 to 1.91) | <0.0001 | ||
| Medicaid | 1.37 (1.15 to 1.62) | 0.0003 | ||
| Medicare | 1.25 (1.05 to 1.50) | 0.0120 | ||
| West North Central | 3230 | Insurance | Reference | |
| Uninsured | 1.20 (0.91 to 1.56) | 0.21 | ||
| Medicaid | 1.67 (1.37 to 2.04) | <0.0001 | ||
| Medicare | 1.42 (1.14 to 1.75) | 0.0015 | ||
| West South Central | 5107 | Insurance | Reference | |
| Uninsured | 1.31 (1.08 to 1.58) | 0.0069 | ||
| Medicaid | 1.44 (1.21 to 1.72) | <0.0001 | ||
| Medicare | 1.46 (1.19 to 1.79) | 0.0002 | ||
| Mountain | 1895 | Insurance | Reference | |
| Uninsured | 1.04 (0.73 to 1.48) | 0.85 | ||
| Medicaid | 1.28 (0.97 to 1.70) | 0.084 | ||
| Medicare | 1.36 (0.99 to 1.86) | 0.06 | ||
| Pacific | 6231 | Insurance | Reference | |
| Uninsured | 1.33 (0.99 to 1.78) | 0.55 | ||
| Medicaid | 1.14 (0.97 to 1.33) | 0.12 | ||
| Medicare | 1.35 (1.13 to 1.61) | 0.0009 |
Regions with differential outcomes based on insurance status and the specific status are shown in bold type.
Figure 2.
National Cancer Database regions with significantly worse survival among cervical cancer patients insured by Medicaid in different colors. Labeled states have not adopted, implemented, or only recently implemented the Medicaid expansion. Gray-blue states in the Northeast, Mountain and Pacific regions did not have inferior survival in Medicaid patients. No asterisk, have not adopted or implemented Medicaid expansion. *Adopted but not implemented the Medicaid expansion. **Adopted the Medicaid expansion within the last 6 months.
Annual income level under $38 000 was associated with decreased survival in the Middle Atlantic (HR 1.24, p=0.016), South Atlantic (HR 1.35, p=0.0004), and East North Central (HR 1.49, p<0.0001) regions. Annual income level under $38 000 did not affect survival in the New England, East South Central, West North Central, West South Central, Mountain, and Pacific regions.
Finally, when compared with academic research institutions, survival varied based on the institution where treatment was administered (Table 3). Cervical cancer mortality was similar for community cancer programs in all regions. Mortality was higher for women treated at integrated network cancer programs in the South Atlantic (HR 1.22; 95% CI 1.08 to 1.37, p=0.001) and the Mountain regions (HR 1.43; 95% CI 1.00 to 2.04, p=0.048). However, comprehensive community cancer centers had significantly worse survival in four of nine regions: Middle Atlantic (HR 1.15; 95% CI 1.03 to 1.28, p=0.02), South Atlantic (HR 1.17; 95% CI 1.06 to 1.28, p=0.002), West North Central (HR 1.31; 95% CI 1.11 to 1.53, p=0.001), and West South Central (HR 1.21; 95% CI 1.04 to 1.40, p=0.012) regions. Comprehensive community cancer programs did not have worse survival in the New England, East North Central, East South Central, Mountain, or Pacific regions.
Table 3.
Cervical cancer mortality among patients based on type of facility where care was administered by National Cancer Database region (n=48 787)
| Region | No of patients | Facility type | Hazard ratio (95% CI) | P value |
|---|---|---|---|---|
| New England | 2028 | Academic | Reference | |
| INCP | 1.22 (0.61 to 2.41) | 0.57 | ||
| CoCP | 1.26 (0.79 to 2.01) | 0.33 | ||
| CCCP | 1.17 (0.91 to 1.50) | 0.23 | ||
| Middle Atlantic | 7675 | Academic | Reference | |
| INCP | 1.14 (0.94 to 1.39) | 0.19 | ||
| CoCP | 0.94 (0.74 to 1.21) | 0.64 | ||
| CCCP | 1.15 (1.03 to 1.28) | 0.02 | ||
| South Atlantic | 10 206 | Academic | Reference | |
| INCP | 1.22 (1.08 to 1.37) | 0.001 | ||
| CoCP | 1.00 (0.84 to 1.20) | 0.98 | ||
| CCCP | 1.17 (1.06 to 1.28) | 0.002 | ||
| East North Central | 8275 | Academic | Reference | |
| INCP | 0.90 (0.78 to 1.04) | 0.14 | ||
| CoCP | 1.13 (0.97 to 1.31) | 0.11 | ||
| CCCP | 1.05 (0.95 to 1.17) | 0.33 | ||
| East South Central | 4140 | Academic | Reference | |
| INCP | 0.95 (0.74 to 1.22) | 0.69 | ||
| CoCP | 0.96 (0.76 to 1.21) | 0.75 | ||
| CCCP | 0.90 (0.79 to 1.03) | 0.12 | ||
| West North Central | 3230 | Academic | Reference | |
| INCP | 1.05 (0.58 to 1.93) | 0.87 | ||
| CoCP | 1.18 (0.92 to 1.51) | 0.19 | ||
| CCCP | 1.31 (1.11 to 1.53) | 0.001 | ||
| West South Central | 5107 | Academic | Reference | |
| INCP | 1.07 (0.84 to 1.35) | 0.59 | ||
| CoCP | 0.97 (0.74 to 1.28) | 0.83 | ||
| CCCP | 1.21 (1.04 to 1.40) | 0.012 | ||
| Mountain | 1895 | Academic | Reference | |
| INCP | 1.43 (1.00 to 2.04) | 0.048 | ||
| CoCP | 1.07 (0.64 to 1.78) | 0.79 | ||
| CCCP | 0.91 (0.717 to 1.2) | 0.45 | ||
| Pacific | 6231 | Academic | Reference | |
| INCP | 1.18 (0.93 to 1.50) | 0.18 | ||
| CoCP | 1.19 (0.95 to 1.49) | 0.12 | ||
| CCCP | 1.01 (0.88 to 1.16) | 0.93 |
Regions with differential outcomes based on facility type are shown in bold type.
Academic, academic comprehensive cancer center; CCCP, comprehensive community cancer program; CoCP, community cancer program; INCP, integrated network cancer program.
DISCUSSION
Summary of Main Results
Over a decade’s worth of data from the NCDB showed that the impact of factors traditionally associated with decreased cervical cancer survival—lower socioeconomic status, inadequate insurance coverage, and access to high-volume academic cancer centers—vary regionally. Survival was inferior for Medicaid patients in the majority of regions, but this disparity was not realized in the New England, Pacific, and Mountain regions. Uninsured patients had decreased survival compared with insured patients in the Southern regions and a portion of the Midwest, which was not seen in the Western and Northeastern regions of the USA. Lastly, decreased survival was seen in five of nine regions when not treated at an academic institution.
Results in the Context of Published Literature
It is important to identify these observations in a large nationally representative dataset in order to eliminate barriers to treatment and thus improve outcomes. Moreover, this variability warrants consideration as regional differences in healthcare policy, access, and adherence to standards of care may affect survival. Unfortunately, studies have shown that black and Hispanic populations have much lower rates of insurance coverage compared with white non-Hispanic women. This absence or lapse in insurance coverage accounts for the majority of decreased access to care in these populations.14 15 Some estimates from the early 2000s note that people of color make up over one-third of the US population, but over 50% of the uninsured.16 When evaluating cervical cancer screening among commercially insured women across races, minority women had relatively high rates of Pap screening and decreasing rates of disparities over time. This effect was also seen in high poverty neighborhoods among commercially insured women.17 Similar survival outcomes among black and white women were also seen in a military-based study.18 These studies indicate that insurance coverage and associated increased access appear to mitigate the possible underlying racial disparities seen in cervical cancer.
In 2014, the Patient Protection and Affordable Care Act (ACA) broadly expanded Medicaid.19 The law simplified Medicaid eligibility, basing it solely on income in an attempt to broaden coverage and decrease the state-by-state variability of categorical eligibility requirements. It was initially estimated that the percentage of uninsured women aged 19–64 years would decrease from 20% to 8% if all states adopted this expansion.20 Currently, 12 states have not adopted the ACA’s Medicaid expansion, and two states have adopted but not yet implemented the expansion. There is evidence that Medicaid expansion has improved rates of early stage diagnosis and overall survival in other gynecologic malignancies.21 While most of the current study’s cohort was diagnosed prior to this broad implementation, this is a useful context in which to consider the data and suggest regional solutions. Furthermore, Medicaid expansion has already been associated with more expeditious oncologic care in gynecologic, testicular, bone, and soft tissue malignancies.22-24
It is well established that lower socioeconomic status and lack of private insurance is associated with more advanced disease at the time of diagnosis.25 Moreover, once diagnosed, the same populations are at risk of receiving sub-standard care. A 2018 analysis of 6063 patients with early stage cervical cancer in California found that patients with low socioeconomic status were more likely to receive care that deviated from the National Comprehensive Cancer Network (NCCN) guidelines (OR 0.76, 95% CI 0.64 to 0.92), and Medicaid payer status was associated with inferior survival (HR 1.47, 95% CI 1.15 to 1.87).26 A NCDB study identified 3436 patients with early stage cervical cancer who had undergone hysterectomy and had been diagnosed with regional lymph node metastasis. The authors found that black women were significantly less likely to receive standard of care adjuvant external beam radiation therapy than white women (64.2% vs 70.6%, p=0.037).27
Our data reflect similar findings as patients with Medicaid had statistically worse survival in six regions (Middle Atlantic, South Atlantic, East North Central, East South Central, West North Central, and West South Central). Five of these six regions encompass 11 of the 12 states that elected not to expand Medicaid (Figure 2). Interestingly, we found that inferior survival associated with Medicaid was most profound in these five regions: South Atlantic, East North Central, East South Central, West North Central, and West South Central. Additionally, uninsured women have worse survival in South Atlantic, East North Central, East South Central, and West South Central.
West North Central, which demonstrated the strongest correlation with inferior survivorship in underinsured women, includes seven mainland states (North Dakota, South Dakota, Nebraska, Kansas, Minnesota, Iowa, and Missouri), five of which have not adopted or recently adopted Medicaid expansion within the last year. While the effect of Medicaid expansion on cervical cancer prevention and treatment remains unclear, it is concerning that high-risk states would hesitate to accept all available resources to treat preventable cancer.
Interestingly, a recently published NCDB study found that, despite differences in brachytherapy among race and insurance status, there was no difference in overall survival of uninsured women nationally, which seems paradoxical.28 When analyzing survival outcomes regionally, we see that regions located in Northeast and Western states mirror this finding. However, regions in the Southern and Midwestern USA have survival differences when comparing insured to uninsured populations. The large population of uninsured women in the Northeast and Western USA, who have statistically equivalent survival outcomes in their regions, likely conceal survival differences that exist in the Southern and Midwestern regions when conducting a more broad national analysis (Figure 2, Table 2).
Regional differences in access to care are well-known drivers of disparity in cancer-related outcomes. One 2015 study by Shalowitz et al identified 1125 US counties—home to almost 15 million women—more than 50 miles from the nearest gynecologic oncologist.29 These patients may be more likely to seek care at a community cancer center, and several studies have noted associations between receiving care at non-academic centers and inferior outcomes in other cancers.30 31 In cervical cancer, inferior survival has been associated with lack of guideline-based care in low-volume community facilities.32 33 When suggesting focused approaches to combat these disparities, it may be useful to overlay these data with ours. Shalowitz et al identified the proportion of the female population residing in low access counties in each state. Among the states with the highest proportion of their female populations residing in low access counties, six of the top 13 states were in the West North Central region, and all seven states included in the West North Central region fell in the top 21. West North Central was one of four regions where care at community cancer centers was significantly associated with inferior cervical cancer survival, and among those four regions, West North Central had the strongest association (HR 1.31; 95% CI 1.11 to 1.53, p=0.001).
Strengths and Weaknesses
Ours is the first study to look at cervical cancer survival on a regional basis. An additional strength is a large sample size, which produces generalizable results. Our study is limited by its retrospective approach and limitations inherent to database evaluations including a high number of excluded patients. Moreover, our cohort of patients and their outcomes do not reflect changes in care brought forth by the ACA given the timing of implementation, but speaks to state priorities when it comes to policy. Future investigations are needed to further examine these outcomes once the ACA has been implemented for a number of years. Finally, comparison with the current disparities in the literature remains limited as the use of the nine NCDB geographic regions appears to be rare.
Implications for Practice and Future Research
While disparities in cervical cancer survival are known, our study highlights how the effects of these disparities vary regionally within the USA. Focused policy decisions may impact local access to care and the financial feasibility of such care when insurance coverage is in place. Accordingly, regionally directed changes must be tailored. The question must be posed, ‘Why do uninsured and underinsured cervical cancer patients have equivalent survival in only certain regions of the country?’. It is incumbent on us to recommend policy changes in the South and parts of the Midwest where being uninsured or underinsured is associated with inferior survival. When considering broad solutions to cancer-related disparities, policy makers and medical societies should use regional data to identify truly high-risk regions and promote tactful deployment of resources. Future studies may evaluate policies and interventions to combat disparities affecting cervical cancer survival in this context.
CONCLUSIONS
In most regions of the USA cervical cancer survival is inferior in uninsured or underinsured women. The impact is most profound in the South and Midwest regions and largely equivalent in the Western and Northeastern regions. Steps should be taken to rectify the differences in survival between these regions.
HIGHLIGHTS.
There are regional differences in cervical cancer survival based on insurance status.
Underinsured and uninsured women in the Southeast and Midwest have inferior survival compared with other regions.
These are the same regions that have been resistant to adopting Medicaid expansion through the Affordable Care Act.
Funding
SB was supported in part by P30 CA13148 and P50 CA098252 while CL was supported in part by the UG1 CA23330 and P50 CA098252. These funding sources are from the National Cancer Institute (NCI). CL reports contracted research with Agenus.
Footnotes
Map disclaimer The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests None declared
Data availability statement
Data may be obtained from a third party and are not publicly available. Data was obtained from the National Cancer Database. In accordance with the journal’s guidelines, public use data are available at https://www.facs.org/quality-programs/cancer/ncdb/puf and SAS analyzed data can be provided for the reproducibility of this study if such is requested.
REFERENCES
- 1.Perkins RB, Guido RS, Castle PE, et al. 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 2020;24:102–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howlader NNA, Krapcho M, Miller D, eds. SEER Cancer Statistics Review. Bethesda, MD: National Cancer Institute, 1975–2017. [Google Scholar]
- 3.Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7–33 [DOI] [PubMed] [Google Scholar]
- 4.Petrosky E, Bocchini JA, Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2015;64:300–4. [PMC free article] [PubMed] [Google Scholar]
- 5.Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med 2020;383:1340–8. [DOI] [PubMed] [Google Scholar]
- 6.Zhan FB, Lin Y. Racial/ethnic, socioeconomic, and geographic disparities of cervical cancer advanced-stage diagnosis in Texas. Womens Health Issues 2014;24:519–27. [DOI] [PubMed] [Google Scholar]
- 7.Barrington DA, Dilley SE, Landers EE, et al. Distance from a comprehensive cancer center: a proxy for poor cervical cancer outcomes? Gynecol Oncol 2016;143:617–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoo W, Kim S, Huh WK, et al. Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One 2017;12:e0172548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alimena S, Yang DD, Melamed A, et al. Racial disparities in brachytherapy administration and survival in women with locally advanced cervical cancer. Gynecol Oncol 2019;154:595–601. [DOI] [PubMed] [Google Scholar]
- 10.Mayadev J, Klapheke A, Yashar C, et al. Underutilization of brachytherapy and disparities in survival for patients with cervical cancer in California. Gynecol Oncol 2018;150:73–8. [DOI] [PubMed] [Google Scholar]
- 11.Han K, Milosevic M, Fyles A, et al. Trends in the utilization of brachytherapy in cervical cancer in the United States. Int J Radiat Oncol Biol Phys 2013;87:111–9. [DOI] [PubMed] [Google Scholar]
- 12.Newman LA, Lee CT, Parekh LP, et al. Use of the National Cancer Data Base to develop clinical trials accrual targets that are appropriate for minority ethnicity patients: a report from the American College of Surgeons Oncology Group (ACOSOG) Special Population Committee. Cancer 2006;106:188–95. [DOI] [PubMed] [Google Scholar]
- 13.American College of Surgeons. About cancer program categories. Available: https://www.facs.org/quality-programs/cancer/coc/accreditation/categories#cccp
- 14.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff 2005;24:398–408. [DOI] [PubMed] [Google Scholar]
- 15.Sohn H Racial and ethnic disparities in health insurance coverage: dynamics of gaining and losing coverage over the life-course. Popul Res Policy Rev 2017;36:181–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Kaiser Commission on Medicaid and the Uninsured. Health insurance coverage in America: 2003 data update, 2004. The Henry J Kaiser Family Foundation. Available: https://www.kff.org/uninsured/report/health-insurance-coverage-in-america-2003-data/ [Google Scholar]
- 17.Wharam JF, Zhang F, Xu X, et al. National trends and disparities in cervical cancer screening among commercially insured women, 2001-2010. Cancer Epidemiol Biomarkers Prev 2014;23:2366–73. [DOI] [PubMed] [Google Scholar]
- 18.Farley JH, Hines JF, Taylor RR, et al. Equal care ensures equal survival for African-American women with cervical carcinoma. Cancer 2001;91:869–73. [PubMed] [Google Scholar]
- 19.Kaiser Family Foundation. Status of state Medicaid expansion decisions: interactive MAP Available: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ [Accessed 10 Jul 2020].
- 20.American College of Obstetricians and Gynecologists. ACOG Committee opinion no. 552: benefits to women of Medicaid expansion through the Affordable Care Act. Obstet Gynecol 2013;121:223–5. [DOI] [PubMed] [Google Scholar]
- 21.Barrington DA, Sinnott JA, Calo C, et al. Where you live matters: a National Cancer Database study of Medicaid expansion and endometrial cancer outcomes. Gynecol Oncol 2020;158:407–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weiner AB, Jan S, Jain-Poster K, et al. Insurance coverage, stage at diagnosis, and time to treatment following dependent coverage and Medicaid expansion for men with testicular cancer. PLoS One 2020;15:e0238813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Albright BB, Nasioudis D, Craig S, et al. Impact of Medicaid expansion on women with gynecologic cancer: a difference-in-difference analysis. Am J Obstet Gynecol 2021;224:195.e1–195.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik AT, Alexander J, Khan SN, et al. Has the Affordable Care Act been associated with increased insurance coverage and early-stage diagnoses of bone and soft-tissue sarcomas in adults? Clin Orthop Relat Res 2021;479:493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Halpern MT, Ward EM, Pavluck AL, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol 2008;9:222–31. [DOI] [PubMed] [Google Scholar]
- 26.Pfaendler KS, Chang J, Ziogas A, et al. Disparities in adherence to National Comprehensive Cancer Network treatment guidelines and survival for stage IB-IIA cervical cancer in California. Obstet Gynecol 2018;131:899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nasioudis D, Musselman K, Gordhandas S, et al. Disparities in the use of adjuvant external beam radiation therapy in node-positive cervical cancer patients following hysterectomy. Am J Clin Oncol 2020;43:43–6. [DOI] [PubMed] [Google Scholar]
- 28.Bruce SF, Joshi TV, Chervoneva I, et al. Disparities among cervical cancer patients receiving brachytherapy. Obstet Gynecol 2019;134:559–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shalowitz DI, Vinograd AM, Giuntoli RL. Geographic access to gynecologic cancer care in the United States. Gynecol Oncol 2015;138:115–20. [DOI] [PubMed] [Google Scholar]
- 30.Lee DY, Teng A, Pedersen RC, et al. Racial and socioeconomic treatment disparities in adolescents and young adults with stage II-III rectal cancer. Ann Surg Oncol 2017;24:311–8. [DOI] [PubMed] [Google Scholar]
- 31.Mahal BA, Chen Y-W, Muralidhar V, et al. National sociodemographic disparities in the treatment of high-risk prostate cancer: do academic cancer centers perform better than community cancer centers? Cancer 2016;122:3371–7. [DOI] [PubMed] [Google Scholar]
- 32.Wright JD, Huang Y, Ananth CV, et al. Influence of treatment center and hospital volume on survival for locally advanced cervical cancer. Gynecol Oncol 2015;139:506–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Uppal S, Chapman C, Spencer RJ, et al. Association of hospital volume with racial and ethnic disparities in locally advanced cervical cancer treatment. Obstet Gynecol 2017;129:295–304. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Data was obtained from the National Cancer Database. In accordance with the journal’s guidelines, public use data are available at https://www.facs.org/quality-programs/cancer/ncdb/puf and SAS analyzed data can be provided for the reproducibility of this study if such is requested.