Abstract
Introduction
This study aims to evaluate the clinical efficacy of a hydroxyapatite toothpaste containing a Polyol Germanium Complex with threonine in treating dentine hypersensitivity. The study also seeks to monitor the quality of life of the treated dentine hypersensitivity sufferers.
Materials and methods
This study is a randomized clinical trial with a total of 120 patients with dentine hypersensitivity. All participants were divided into three groups: patients assigned to the GARDA SILK toothpaste; patients receiving the conventional fluoride toothpaste for comparison purposes, and patients asked to brush their teeth without toothpaste. The modified Quigley-Heine Plaque Index was assessed at the baseline and after treatment. Sensitivity was assessed at baseline, 3, 7 and 14 days using the air stimulus (Schiff Index). The impact of dentine hypersensitivity on the quality of life was assessed before and after the treatment with the Russian version of the Dentine Hypersensitivity Experience Questionnaire (DHEQ).
Results
After 14 days of treatment, the mean Plaque Index scores in Groups 1 and 2 did not exceed 1 and averaged 0.72 ± 0.249 and 0.86 ± 0.213, respectively. In Group 3, the mean Plaque Index was significantly higher (1.04 ± 0.070, p < 0.05). The mean Schiff sensitivity scores in Group 1 decreased to 2.45 ± 0.42 at 3 days, 1.84 ± 0.26 at 7 days, and 1.02 ± 0.34 at 14 days. Group 2 exhibited smaller reductions in the Schiff index at all time points. In this group, Schiff scores dropped to 2.67 ± 0.28 after 3 days, 2.34 ± 0.44 after 7 days, and 1.93 ± 0.36 after 14 days.
Conclusion
The GARDA SILK hydroxyapatite toothpaste with a threonine-containing Polyol Germanium Complex (PGC) is effective in maintaining good oral hygiene, reducing dentine hypersensitivity, and improving the quality of life of dentine hypersensitivity sufferers.
Keywords: Dentine hypersensitivity, Professional oral hygiene, Desensitizing toothpaste, Hydroxyapatite, Polyol Germanium Complex (PGC), The quality of life
1. Introduction
Today, hyperesthesia is among the leading non-carious defects of hard tooth tissues (Gillam, 2017, Olley and Sehmi, 2017). Dentine hypersensitivity (DH) is defined as an acute, short term pain arising from dentin exposure to an external stimulus, which cannot be explained by other reasons (Longridge and Youngson, 2019).
Currently, the most widely accepted theory behind the mechanism of DH is the hydrodynamic theory attributed to Brannstrom (West et al., 2013). According to this theory, DH occurs when there is access to dentinal tubules that open as a result of the gingival recession or loss of enamel.
Albeit that DH is a chronic condition that can worsen over time and requires qualified treatment (Zeola et al., 2019), patients often adapt to the inconveniences and do not seek medical help from dentists (Mason et al., 2019).
Currently, there is a wide range of desensitizing agents (DA) that can be used to treat DH (AlKahtani, 2017, Samburova et al., 2021). Even though the benefits of various DAs are not fully understood, multiple studies report a positive effect of desensitizing toothpaste (Elovikova et al., 2019, Hu et al., 2018, Seong et al., 2020).
Despite significant progress in the treatment of DH, many issues remain controversial. Therefore, searching for new means and methods of DH treatment remains an urgent problem of modern dentistry.
The Russian company Venteil Group released a hydroxyapatite toothpaste for sensitive teeth − GARDA SILK − enriched with threonine-containing Polyol Germanium Complex (PGC). The toothpaste is intended for everyday care. The PGC complex used within the formulation is a mix of organic ligands (such as calcium, phosphorus, germanium, magnesium, zinc, and threonine amino acid), which stimulate calcium metabolism when released in the oral cavity. It makes the plaque more soluble and easy to remove during brushing and helps thicken and re-mineralize the enamel. The binding of organogermanium complexes with the enamel promotes the formation of a hybrid layer similar to the original enamel, which seals open dentinal tubules and protects underlying dentin (Shurova, 2017).
The PGC-enriched hydroxyapatite toothpaste requires assessment in a clinical trial and the development of usage guidelines before its widespread introduction in dental practice. As such, this study aims to assess the clinical efficacy of a hydroxyapatite toothpaste containing a polyol-germanium (PGC) complex with threonine using the example of GARDA SILK paste in treating DH. The study also aims to monitor the quality of life of treated DH patients.
2. Materials and methods
2.1. Study design
This study is a randomized clinical trial conducted in the [BLINDED]. The sample comprised a total of 120 patients aged 18–35 years with dentine hypersensitivity who agreed to participate in the study.
Individuals with somatic disorders and a history of allergy to any ingredient present in the toothpaste were not included in the clinical trial. Those who refused to undergo repeated examinations and did not comply with the study protocol were also excluded.
Eligible patients were divided into three groups of 40 each via simple randomization. Group 1 (observation group) was instructed to use the provided GARDA SILK toothpaste twice a day. Group 2 (comparison group) was asked to brush their teeth twice a day with conventional fluoride toothpaste. Group 3 (control group) was instructed to brush their teeth twice a day with a toothbrush that did not contain toothpaste.
The GARDA SILK toothpaste used in the observation group has the following composition: Water, Hydrated Silica, Glycerin, Hydrogenated Starch Hydrolysate, Hydroxyapatite, Sodium Methyl Cocoyl Taurate, Xanthan Gum, Aroma, Echinacea Purpurea Extract, Polyol Germanium Complex (PGC) with the Amino Acid Threonine, Menthol, Sodium Saccharin, O-Cymen-5-Ol, Hydroxyacetophenone.
Before the beginning of treatment, all patients underwent professional oral hygiene using a combined Air Flow cleaning technique (mechanical + ultrasonic cleaning of teeth) to remove plaque and tartar. All patients were taught the Bass brushing method and instructed to use soft toothbrushes, oral rinses, and dental floss.
2.2. Results evaluation
The oral hygiene level was evaluated through the Turesky modification of the Quigley-Hein Plaque Index (TQHPI) (Mason et al., 2019). All vestibular and oral surfaces of the teeth were stained with a plaque staining solution (CURAPROX PCA 260). Plaque accumulation was scored as follows: ‘0′ − no plaque; ‘1′ − separate flecks of plaque in the cervical area of the tooth; ‘2′ − a thin continuous band of plaque (up to 1 mm) in the cervical area of the tooth; ‘3′ − a band of plaque wider than 1 mm coercing less than one-third of the crown of the tooth; ‘4′ − plaque covering more than one-third but less than two-thirds of the crown of the tooth; ‘5′ − plaque covering two-thirds or more of the crown of the tooth. The modified Plaque Index (mPI) was measured for all teeth at the baseline and after two weeks.
DH was assessed by an application of a 1-second blast of air from the dental-unit air syringe. Air was delivered perpendicularly to the cervical surface of the tooth from a distance of 1 cm. The subject’s response was rated on a Schiff Index Sensitivity Scale as: ‘0′ − no response to stimuli; ‘1′ − subject feels discomfort, but does not insist on discontinuation of the stimulus; ‘2′ − subject feels discomfort and requests discontinuation of the stimulus; ‘3′ − subject feels severe pain and moves away from the stimulus to discontinue it immediately. Dentin hypersensitivity was assessed at the baseline and after 3, 7, and 14 days.
The impact of DH on daily life was determined with the Russian version of the Dentine Hypersensitivity Experience Questionnaire (DHEQ). It has 15 items assessing the everyday impacts related to DH. Each item is scored from 1 to 7. The higher the score, the greater the impact. The survey was conducted at the baseline and after 14 days.
2.3. Statistical analysis
Statistical analysis was conducted with the aid of the Rstudio software (version 1.2.1335 2009–2019). The Schiff index scores generally had normal distribution (Shapiro-Wilk test). The only exception is Group 1 after 2 weeks. Levene’s test confirmed the homogeneity of variance in all groups, except for measurements taken after 14 days of treatment (in this case, the Greenhouse-Gesser correction was applied). A hybrid factor analysis was conducted to assess the influence of different factors on the overall Schiff sensitivity score. The post hoc analysis was carried out with Tukey’s and Student’s multiple comparison tests for intergroup and intragroup comparison, respectively.
2.4. Ethics approval
The authors declare that the work is written with due consideration of ethical standards. The study was conducted in accordance with the ethical principles approved by the Ethics Committee of [BLINDED] University and the World Medical Association Declaration of Helsinki. All participants gave their written informed consent.
3. Results
At baseline, all three groups had satisfactory levels of oral hygiene and showed similar mPI scores (Table 1). After 14 days, the mPI scores for Groups 1 and 2 were 0.72 ± 0.249 and 0.86 ± 0.213, respectively, indicating good oral hygiene (the index value does not exceed 1). The change between these two groups is statistically insignificant (p > 0.05). The Plaque Index in Group 3 reduced to 1.04 ± 0.070 after two weeks, indicating that complying with the provided instructions for oral hygiene was enough to ensure good hygiene. Nonetheless, it was significantly higher than in the other two groups (p < 0.05).
Table 1.
Values (M ± m) of Modified Plaque Index at Baseline and after 14 Days of PGC-enriched Hydroxyapatite Treatment.
| Baseline | After 14 days | |
|---|---|---|
| Group 1 | 2.38 ± 0.181 | 0.72 ± 0.249 |
| Group 2 | 2.43 ± 0.194 | 0.86 ± 0.213 |
| Group 3 | 2.49 ± 0.260 | 1.04 ± 0.170 |
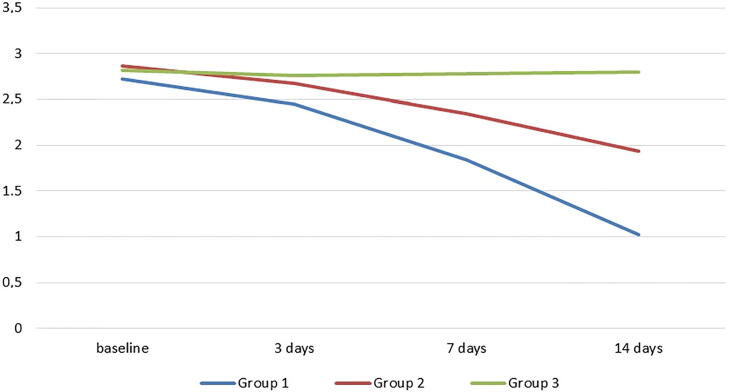
Mean baseline Schiff sensitivity scores were 2.72 ± 0.32 in Group 1, 2.86 ± 0.28 in Group 2, and 2.82 ± 0.26 in Group 3. Groups 1 and 2 both achieved reductions in air sensitivity, but improvements in Group 1 were more substantial (Fig. 1). The mean Schiff sensitivity score of Group 1 decreased to 2.45 ± 0.42 at 3 days, 1.84 ± 0.26 at 7 days, and 1.02 ± 0.34 at 14 days. The mean Schiff sensitivity score of Group 2 decreased to 2.67 ± 0.28 at 3 days, 2.34 ± 0.44 at 7 days, and 1.93 ± 0.36 at 14 days. Meantime, Group 3 demonstrated no significant changes in air sensitivity.
Fig. 1.
Change from baseline to days 3, 7 and 14 for Schiff sensitivity score across the studied groups.
The multivariate analysis of variance (MANOVA) confirmed the substantial impact of the studied toothpaste. It also shows significant changes in the Schiff sensitivity with time. Combining these two factors (toothpaste choice and time) appeared to have substantial effects on subjects' responses. The Tukey post hoc test revealed no statistically significant differences in baseline Schiff sensitivity scores between groups (p = 0.822). However, at 3, 7 and 14 days, Group 1 had significantly lower Schiff sensitivity scores than Groups 2 and 3 (p < 0.01 and p < 0.001, respectively). The Student's test with Bonferroni correction for multiple comparisons showed significant reductions from baseline in Schiff sensitivity scores in Groups 1 and 2 at all follow-ups (p < 0.001 and p < 0.01, respectively). The control group’s reductions were insignificant at all time points (p > 0.05).
DHEQ results revealed that DH has significantly impacted patients’ daily lives. At the same time, no statistical differences were found between the groups. Mean baseline DHEQ scores were 72.4 ± 8.2 in Group 1, 69.8 ± 10.2 in Group 2; and 71.6 ± 7.8 in Group 4. After 14 days, Group 1 exhibited a tendency towards significant QoL improvement (p < 0.05) with a mean DHEQ score of 48.7 ± 5.8. Patients using fluoride toothpaste reported slight reductions in DHEQ scores (63.7 ± 8.5), but these changes were not statistically significant (p > 0.05). Patients in the control group indicated ‘no change’ in DHEQ scores at 14 days. Overall, patients using GARDA SILK toothpaste had statistically significantly better QoL after 14 days of treatment compared to Groups 2 and 3 (p < 0.05).
4. Discussion
The present study evaluated the clinical efficacy of GARDA SILK toothpaste − the hydroxyapatite toothpaste for sensitive teeth enriched with threonine-containing Polyol Germanium Complex (PGC). The Plaque Index score assessed after two weeks of treatment showed a good level of oral hygiene. There were no statistically significant differences between patients assigned to PGC-enriched hydroxyapatite toothpaste and fluoride toothpaste. Yet, there was a statistically significant difference between these two groups and patients brushing without toothpaste. This finding suggests that the GARDA SILK toothpaste is as effective as the conventional fluoride toothpaste in maintaining oral hygiene.
Based on the hydrodynamic theory, the DH treatment should either block neural transmission within the dentinal tubules or reduce fluid flow inside them (Liu et al., 2020, West et al., 2013). The first treatment strategy involves using potassium-containing compounds, such as potassium nitrate. By increasing the extracellular concentration of potassium ions in deep dentin cavities, it is possible to depolarize the membranes of the nerve fibres and make them unable to repolarize, thereby blocking neural transmission (Hall et al., 2019, Seong et al., 2021). As regards the second strategy, various agents have been used as desensitizers in toothpaste formulations to reduce fluid flow within the dentinal tubules (Hu et al., 2018, Martins et al., 2020).
Desensitizing toothpastes operate by an occlusion mechanism and cause varying degrees of dentin tubule occlusion and dentin mineralization, often after just a few days of usage. However, the occlusion may be partially reduced after acid exposure, leading to re-opening of the dentinal tubules (van der Weijden et al., 2017a, van der Weijden et al., 2017b). To avoid this happening, patients need to regularly use desensitizing toothpastes and other agents (rinses, gels, etc.).
Not all desensitizing kinds of toothpaste are equally effective, though (Balevi, 2020). Currently, there is no single standard for desensitizing kinds of toothpaste, and the search for the most effective components for DH treatment continues.
Martins and et al. (2020) indicate that potassium + stannous fluoride (SnF2), calcium-sodium phosphosilicate (CSP), potassium + hydroxyapatite, strontium and potassium show larger positive effects on tactile response than fluorides. The CSP toothpaste was the best choice for cold stimuli. For air stimulus, arginine, potassium + hydroxyapatite, potassium + SnF2, and CSP were more effective than fluoride for air stimulus.
Another meta-analysis (Hu et al., 2018) revealed that toothpastes containing potassium, stannous fluoride, potassium + strontium, potassium + strontium fluoride, calcium, sodium phosphosilicate, arginine, and nano-hydroxyapatite (n-HA) are effective in relieving DH symptoms. The authors, however, advised against the use of toothpastes with strontium and amorphous calcium phosphate.
5. Conclusions
The study revealed that the GARDA SILK hydroxyapatite toothpaste with a threonine-containing Polyol Germanium Complex (PGC) was as good as the conventional fluoride toothpaste in maintaining good oral hygiene. After 14 days of treatment, the threonine-containing PGC significantly reduced tooth sensitivity and thus improved the QoL of patients. The present findings suggest that GARDA SILK toothpaste can be a recommended therapeutic and prophylactic option for patients with DH.
6. Author statement
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by NV, VS, IN, DN and NN. The first draft of the manuscript was written by IG and AD. All authors read and approved the final manuscript.
7. Ethics approval
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The research was approved by the local ethics committess of The First Sechenov Moscow State Medical University.
8. Data statement
Data will be available on request.
Funding
This study was supported by the “Russian Academic Excellence Project 5-100″.
CRediT Author Statement
Natalia Vlasova: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Vadim Samusenkov: Conceptualization, Investigation, Validation, Visualization, Writing – review & editing. Irina Novikova: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Denis Nikolenko: Data curation, Methodology, Validation, Visualization, Writing – review & editing. Nikita Nikolashvili: Formal analysis, Resources, Software, Supervision, Writing – review & editing. Ilana Gor: Data curation, Project administration, Writing – review & editing. Anna Danilina: Formal analysis, Project administration, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was supported by the “Russian Academic Excellence Project 5-100”.
Footnotes
Peer review under responsibility of King Saud University.
References
- AlKahtani R. Dentin desensitizing agents: too many options. Gen. Dent. 2017;65(5):17–20. [PubMed] [Google Scholar]
- Balevi B. Not all desensitizing toothpastes perform equally well. J. Evid. Based Dent. Pract. 2020;20(3) doi: 10.1016/j.jebdp.2020.101460. [DOI] [PubMed] [Google Scholar]
- Elovikova T.M., Ermishina E.Y., Koshcheev A.S. Analysis of the impact of therapeutic and prophylactic toothpaste containing bicarbonate and sodium fluoride on the state of the oral cavity in inflammatory periodontal diseases in young patients (clinical and laboratory research) Periodontology. 2019;1:45–51. [Google Scholar]
- Gillam D.G. A new perspective on dentine hypersensitivity–guidelines for general dental practice. Dent. Update. 2017;44(1):33–42. doi: 10.12968/denu.2017.44.1.33. [DOI] [PubMed] [Google Scholar]
- Hall C., Sufi F., Milleman J.L., Milleman K.R. Efficacy of a 3% potassium nitrate mouthrinse for the relief of dentinal hypersensitivity: An 8-week randomized controlled study. J. Am. Dent. Assoc. 2019;150(3):204–212. doi: 10.1016/j.adaj.2018.10.023. [DOI] [PubMed] [Google Scholar]
- Hu M.L., Zheng G., Zhang Y.D., Yan X., Li X.C., Lin H. Effect of desensitizing toothpastes on dentine hypersensitivity: A systematic review and meta-analysis. J. Dent. 2018;75:12–21. doi: 10.1016/j.jdent.2018.05.012. [DOI] [PubMed] [Google Scholar]
- Liu X.X., Tenenbaum H.C., Wilder R.S., Quock R., Hewlett E.R., Ren Y.F. Pathogenesis, diagnosis and management of dentin hypersensitivity: an evidence-based overview for dental practitioners. BMC Oral Health. 2020;20(1):220. doi: 10.1186/s12903-020-01199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longridge N.N., Youngson C.C. Dental pain: dentine sensitivity, hypersensitivity and cracked tooth syndrome. Prim. Dent. J. 2019;8(1):44–51. doi: 10.1177/205016841900800101. [DOI] [PubMed] [Google Scholar]
- Martins C.C., Firmino R.T., Riva J.J., Ge L., Carrasco-Labra A., Brignardello-Petersen R., Colunga-Lozano L.E., Granville-Garcia A.F., Costa F.O., Yepes-Nuñez J.J., Zhang Y., Schünemann H.J. Desensitizing toothpastes for dentin hypersensitivity: a network meta-analysis. J. Dent. Res. 2020;99(5):514–522. doi: 10.1177/0022034520903036. [DOI] [PubMed] [Google Scholar]
- Mason S., Burnett G.R., Patel N., Patil A., Maclure R. Impact of toothpaste on oral health-related quality of life in people with dentine hypersensitivity. BMC Oral Health. 2019;19(1):226. doi: 10.1186/s12903-019-0919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olley R.C., Sehmi H. The rise of dentine hypersensitivity and tooth wear in an ageing population. Br. Dent. J. 2017;223(4):293–297. doi: 10.1038/sj.bdj.2017.715. [DOI] [PubMed] [Google Scholar]
- Samburova, M., Safonov, V., Avdushko, S., 2021. Ecological and biological features of the primrose distribution in Transbaikalia as the model territory of Eastern Siberia. Bot. Rev., in press. 10.1007/s12229-021-09264-0. [DOI]
- Seong J., Newcombe R.G., Foskett H.L., Davies M., West N.X. A randomised controlled trial to compare the efficacy of an aluminium lactate/potassium nitrate/hydroxylapatite toothpaste with a control toothpaste for the prevention of dentine hypersensitivity. J. Dent. 2021;108 doi: 10.1016/j.jdent.2021.103619. [DOI] [PubMed] [Google Scholar]
- Seong J., Newcombe R.G., Matheson J.R., Weddell L., Edwards M., West N.X. A randomised controlled trial investigating efficacy of a novel toothpaste containing calcium silicate and sodium phosphate in dentine hypersensitivity pain reduction compared to a fluoride control toothpaste. J. Dent. 2020;98 doi: 10.1016/j.jdent.2020.103320. [DOI] [PubMed] [Google Scholar]
- Shurova, N., 2017. Comparative estimation of efficiency desensitizers for treatment of hyperesthesia. Diss. Cand. Med. Sci. Nizhny Novgorod: Federal State Budget Educational Institution of Higher Education “Nizhegorodskaya State Medical Academy ”of the Ministry of Health of Russia.
- van der Weijden F.N., van Loveren C., Slot D.E., van der Weijden G.A. Preventive dentistry 4. Prevention and treatment of dentine hypersensitivity. Nederlands Tijdschrift Voor Tandheelkunde. 2017;124(3):133–139. doi: 10.5177/ntvt.2017.03.17107. [DOI] [PubMed] [Google Scholar]
- van der Weijden F.N., van Loveren C., Slot D.E., van der Weijden G.A. Preventive dentistry 3. Prevalence, aetiology and diagnosis of dentine (hyper) sensitivity. Nederlands Tijdschrift Voor Tndheelkunde. 2017;124(2):85–90. doi: 10.5177/ntvt.2017.02.16235. [DOI] [PubMed] [Google Scholar]
- West N.X., Lussi A., Seong J., Hellwig E. Dentin hypersensitivity: pain mechanisms and aetiology of exposed cervical dentin. Clin. Oral Investig. 2013;17(1):9–19. doi: 10.1007/s00784-012-0887-x. [DOI] [PubMed] [Google Scholar]
- Zeola L.F., Soares P.V., Cunha-Cruz J. Prevalence of dentin hypersensitivity: Systematic review and meta-analysis. J. Dent. 2019;81:1–6. doi: 10.1016/j.jdent.2018.12.015. [DOI] [PubMed] [Google Scholar]