Abstract
Background
Photobiomodulation has been gaining traction as a plausible therapy to control orthodontically induced root resorption.
Aim
The aim of the present review was to systematically appraise randomized controlled trials conducted to study the influence of photobiomodulation on external root resorption during orthodontic movement in humans.
Method
ology - A systematic search was carried out employing keywords in various electronic databases namely MEDLINE (Pubmed), Cochrane Library, Google Scholar, Semantic Scholar, ScienceDirect and Opengrey.eu for studies up to March 2020. Pre-defined inclusion and exclusion criteria were used to select the studies. Data extraction was carried out and the risk of bias was assessed using Cochrane Risk of Bias tool. Meta-analysis was conducted using random effects model for selected studies. Subgroup analysis was conducted for resorption on each axial surface of the tooth root viz. mesial, buccal, distal and palatal as well as for vertical thirds viz. cervical, middle and apical third. Summary of Findings was formulated according to GRADE Profile.
Results
The search retrieved 1509 results out of which six studies were included for the systematic review. Two studies showed low overall risk of bias and the remaining four showed unclear risk of bias. The meta-analysis was conducted for three studies with an overall sample size of 120 teeth which showed a pooled mean difference of 0.08 (95% CI 0.15 – (−0.02) to 1.96, p=<0.0001) in favour of photobiomodulation group with respect to mean total resorption per tooth. I2 index revealed 88% heterogeneity.
Conclusion
It is concluded that there is moderate grade of evidence to suggest beneficial effect of photobiomodulation on root resorption. Further high-quality randomized controlled trials with standardized intervention parameters are recommended.
Registration
PROSPERO registration number - CRD42020167291.
Keywords: Photobiomodulation, Root resorption, Systematic review, Meta-analysis, Low-level laser therapy
1. Background
One of the commonly associated iatrogenic effects of fixed orthodontic treatment is the occurrence of orthodontically induced inflammatory root resorption (OIIRR).1 It is described as the loss of root structure manifesting as root length reduction or outward defects which decrease root volume.2 A prospective study showed that 94% of the patients undertaking orthodontic treatment displayed root resorption of more than 1 mm.3 Root resorption may jeopardize the functional ability of teeth by introducing mobility, especially when superimposed with periodontal disease.4,5 Consequently, countering iatrogenic root resorption has become one of the prime objectives of researchers around the globe. Various methods such as shortening of the treatment duration, controlled mechanics or awareness of factors of individual susceptibility such as systemic disorders, genetics, previous trauma or age have been known to display reduced occurrence of OIIRR.6 Newer non-invasive techniques such as low-level laser, light-emitting diodes and low intensity pulsed ultrasound (LIPUS) are also being investigated for the same lately.7,8
Photobiomodulation (PBM) therapy entails exposure of biologic cells or tissues to low levels of red and near-infrared light. The devices consist of semiconductors such as arsenic, aluminium, gallium or indium which convert electrical energy to light energy.9 The energy thus generated acts on cellular and molecular levels to influence bone and cementum remodeling mechanisms. The core mechanisms involve stimulation of mitochondrial activity and ATP production, activation of ion channels and subsequent modulation of the inflammatory process.10 It was formerly believed that photobiomodulation required the usage of coherent laser light, however, of late, light-emitting diodes (LEDs) have also been serving as a cheaper alternative. The basic tenet of operation for LEDs and diode lasers is the same and termed as the PIN (positive-intrinsic-negative) semiconductor diode.11 Currently, photobiomodulation is being tested extensively in orthodontics for pain management and accelerating tooth movement during fixed mechanotherapy, wound healing, bone regeneration after rapid maxillary expansion, root resorption control and post-treatment retention.8,12, 13, 14, 15
Although the effect of photobiomodulation on root resorption has been described by various trials, there continues to exist, a discrepancy in the correlation between OIIRR and photobiomodulation. In view of this background, the present systematic review and meta-analysis was conducted to assess the influence of photobiomodulation on root resorption during orthodontic tooth movement in human subjects enrolled in randomized controlled trials.
2. Materials and methods
2.1. Protocol and registration
The systematic review was registered in PROSPERO on 28th April 2020 (CRD42020167291). It was conducted and reported according to the Cochrane Handbook16 of systematic reviews and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.17,18
2.2. Eligibility criteria
The PICOS (Participants, Intervention, Control, Outcome and Study design) scheme was utilized to assess the eligibility.
2.3. Inclusion criteria-
P – Human teeth subjected to orthodontic force application in any direction.
I – Photobiomodulation therapy using either low-level laser or light-emitting diode.
C – Human teeth subjected to orthodontic force application without any intervention (photobiomodulation).
O – Studies reporting quantitative measurements of root resorption.
S - Randomized controlled trials conducted on humans.
2.4. Exclusion criteria-
-
1.
Non-randomized clinical trials
-
2.
In-vitro studies or animal studies
-
3.
Studies without a control/comparison group.
-
4.
Studies conducted on replanted teeth, teeth with periodontal and/or periapical pathologies or primary teeth.
-
5.
Review articles, case reports, case series, letters to editor.
-
6.
Studies available only in languages other than English.
2.5. Sources of information and research strategy
The search was carried out by two review authors in several electronic bibliographic databases namely MEDLINE via Pubmed, Cochrane Library (Cochrane database of systematic reviews, Cochrane central register of controlled trials (CENTRAL), Google Scholar, Semantic Scholar, ScienceDirect and Opengrey.eu for studies up to March 2020. Reference lists of eligible studies and review articles were also explored. All articles and manuscripts published in English or with English translations available were incorporated in the search.
The search strategy devised included the terms relating to or describing the intervention using MeSH (medical subject headings) terms and subsequently was adapted for use according to different databases.
The search strategies employed for various databases are listed in Table 1-.
Table 1.
Search strategies employed for various databases and results retrieved.
| SNo. | Database | Search strategy | Results retrieved | |
|---|---|---|---|---|
| 1 | Cochrane Library | #1- laser | 19071 | |
| #2 - photobiomodulation | 441 | |||
| #3 = #1 OR #2 | 19289 | |||
| #4 - resorption | 4248 | |||
| #5 = #3 AND #4 | 63 | |||
| Cochrane Database of Systematic Reviews | Cochrane CENTRAL Register of Controlled Trials | |||
| 11 | 52 | |||
| 2 | Pubmed | ((((((tooth movement) OR movement) OR (orthodontic[All Fields] OR orthodontically[All Fields])) OR force)) AND (((((((((((lasers) OR low-level light therapy) OR semiconductor lasers) OR laser) OR phototherapy) OR photobiomodulation) OR diode) OR biostimulation) OR LLLT) OR "PBM") OR "PBT")) AND (((((root resorption) OR tooth resorption) OR cementum) OR cementoclast*) OR (odontoclast[All Fields] OR odontoclastic[All Fields] OR odontoclastogenesis[All Fields] OR odontoclasts[All Fields])) (Filters- Human studies) |
33 | |
| 3 | Google Scholar | "low level laser" OR “photobiomodulation” "root resorption" (searched on 20.1.20) Filters applied – Exclude ‘patents and citations’ Year range- 1990–2000. |
988 | |
| 4 | ScienceDirect | ("laser" OR "light" OR "photobiomodulation" OR "biostimulation" OR "phototherapy" OR "diode") ("cementum" OR "resorption" OR "cemental" OR "cementoclast" OR “odontoclast”) ("tooth movement") (Filter applied – Research articles) |
47 | |
| 5 | Semantic Scholar | Root resorption laser Root resorption photobiomodulation Root resorption light (Filters applied – Journal article, Clinical Trial) |
173 69 136 |
|
| Total | 378 | |||
| 6 | Opengrey.eu | ("laser" OR "light" OR "photobiomodulation" OR "biostimulation" OR "phototherapy" OR "diode") ("cementum" OR "resorption" OR "cemental" OR "cementoclast" OR “odont clast”) ("tooth movement") | 0 | |
| Total | 1509 | |||
2.6. Study selection
Two authors screened the titles and/or abstracts of studies obtained from the search results to shortlist articles that potentially met the inclusion criteria. The full text of these studies were then read and independently assessed for eligibility by the same review team members. A third author opined in case of any disagreements.
2.7. Data items and collection
Data extraction was executed and tabulated under the headings: a) author, year, b) general study characteristics, c) patient demographics, d) details on intervention e) outcome details.
2.8. Risk of bias of individual studies
The risk of bias of included studies was evaluated according to Cochrane guidelines for RoB 2.0 tool for randomized trials. The assessment of risk for individual studies was carried out by two authors independently followed by resolution of discrepancies after discussion with the third author. The studies were categorized as low, high or unclear risk of bias referring to Cochrane Handbook where a low risk of bias was assigned where all the categories were judged as low risk, high risk if a majority of the categories were at high risk and unclear risk if the data was insufficient to formulate a decision.
2.9. Summary measures, data synthesis and assessment of heterogeneity
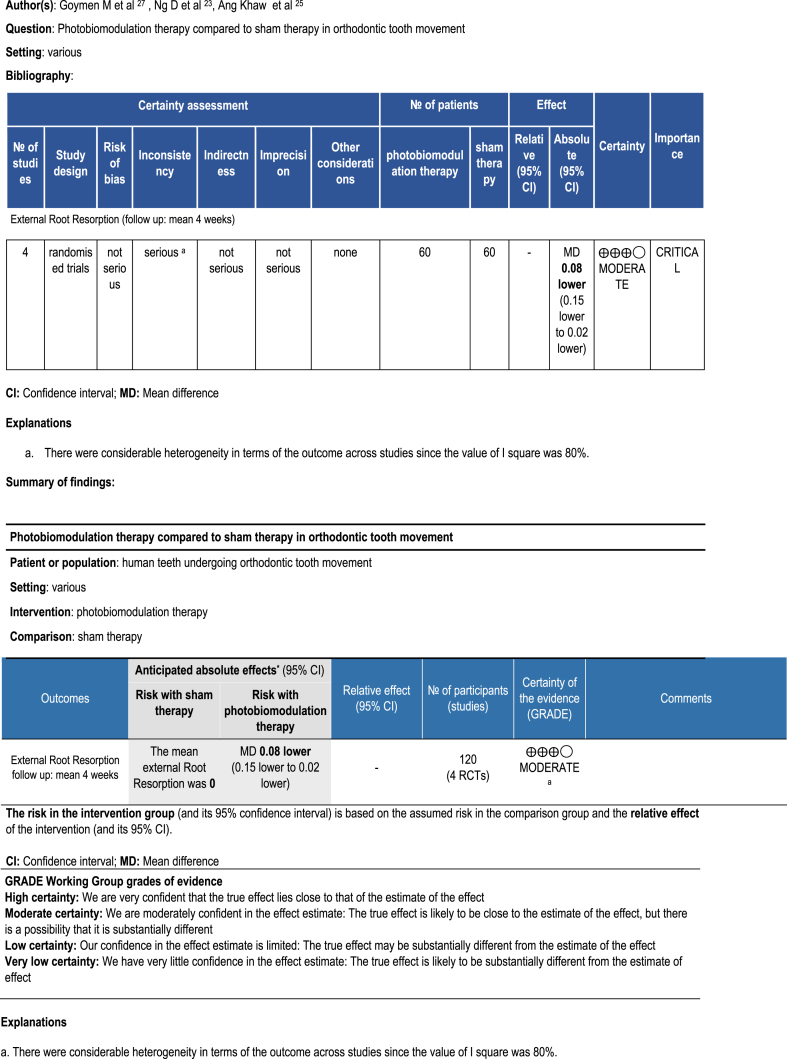
A narrative synthesis of the data extracted from the included studies concerning the type of their intervention, target population characteristics, type of outcome and intervention content was completed. Absolute anticipated effect was calculated and the summary of evidence using GRADE (Grading of Recommendations, Assessment, Development and Evaluation) Evidence Profile was formulated with mean difference as the effect estimate.19
The level of heterogeneity in the outcome measures of the studies was determined using I2 index with significance indicated by p value < 0.05 and the pooled mean difference was calculated. Sub-group analysis was also done to assess root resorption of different axial surfaces and vertical thirds of the root. The heterogeneity for the same was calculated using I2 index. Forest plots were plotted for both mean total root resorption as well as mean resorption volumes on individual axial surfaces and vertical thirds. Funnel plot was plotted for mean total root resorption.
3. Results
3.1. Study selection
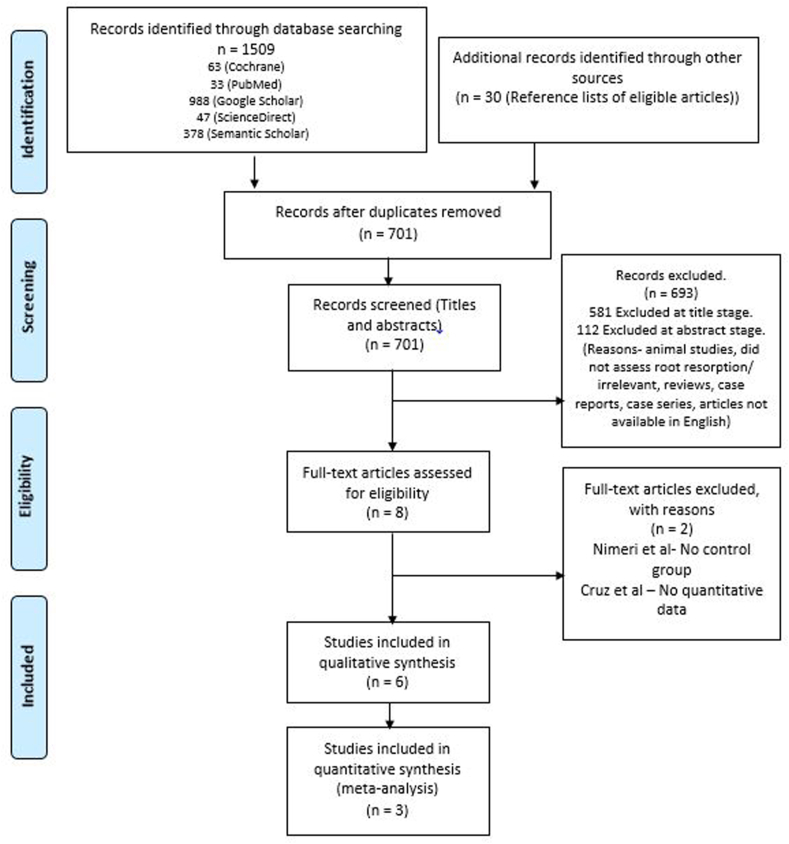
The electronic search retrieved 1509 results from all the databases. Seven hundred and one results remained after removal of duplicates which were then screened by titles and abstracts. Full texts of eight articles were downloaded to be tested for eligibility out of which two were excluded.20, 21, 22, 23, 24, 25, 26, 27 The study by Cruz et al. was excluded due to missing quantitative data and Nimeri et al. was excluded because of missing control group.20,22 The level of agreement between the two authors screening the titles, abstracts and full texts were 0.81, 0.89 and 0.91 as assessed by Kappa's calculation method. Clinical and statistical heterogeneity across the six studies was gauged, on the basis of which three (Ng et al., Ang-Khaw et al. and Goymen et al.) were selected for quantitative analysis.23,25,27 The results retrieved from the search along with reasons behind exclusion have been depicted in the PRISMA Flowchart (Fig. 1) and Table 1.
Fig. 1.
PRISMA flow chart depicting study selection.
3.2. General characteristics of included studies
We included six studies for qualitative analysis. The general characteristics of the studies are reported in Table 2. The studies by Ang-Khaw et al. (2018) and Ng et al. (2017) conducted on 20 patients each were double-blind, randomized controlled trials having split-mouth designs and requiring bilateral maxillary first premolar (MFP) extractions for orthodontic treatment.23,25 Ang-Khaw et al. study comprised 8 males and 12 females and the study of Ng et al. had an equal number patients in both the genders while the mean age of the patients were 16.4 ± 1.3 years and 16.7 ± 1.1 years respectively. Both the studies had a test group and a placebo group. However, the root resorption was assessed after a duration of 70 and 28 days by Ang-Khaw et al. and Ng et al. respectively. Goymen et al. conducted their randomized controlled trial in three different groups of 10 patients each - LLLT group, LED group and control group.27 Fernandes et al. equally divided their total sample of 30 patients into Control group, only ‘Orthodontic Force’ group and ‘Orthodontic Force and PBM’ group.26 The mean age of subjects in Goymen's study was 16.27 ± 0.87 years with 14 males and 16 females; the data was not reported by Fernandes et al. The study by Sousa et al. comprised 10 subjects (6 female and 4 male) involved in a split-mouth design while Okla et al. studied 26 patients who were divided into two groups namely, LLLT and control.21,24 Both the studies were of six months duration. Out of the six studies, four studies (Ng et al., Ang-Khaw et al., Goymen et al. and Fernandes et al.) assessed root resorption three-dimensionally subsequent to photobiomodulation.23,25, 26, 27 Three studies used micro-CT for resorption measurement (Ng et al., Ang-Khaw et al., Goymen et al.) while Fernandes et al. employed conventional computed tomography. The remaining two studies by Okla et al. and Sousa et al. assessed root resorption two-dimensionally by using intra-oral periapical radiographs subsequent to the clinical procedure.21,24
Table 2.
General characteristics of included studies.
| S.No | Author/Year | Study Subjects | Number of Teeth | Mean Age and Gender | Study Groups | Study Design | Study Duration | Method of Evaluation |
|---|---|---|---|---|---|---|---|---|
| 1 | Goymen et al. 201927 | 30 | 30 teeth | 14 males; 16 females Mean age 16.27 ± 0.87 years |
Group 1–10 teeth LLLT and OIRR; Group 2–10 teeth LED and OIRR; Group 3–10 teeth Placebo and OIRR |
Randomized controlled trial | 4 weeks | Micro-computed tomography (micro-CT) 3D Quantitative |
| 2 | Fernandes et al. 201926 | 30 | 30 teeth | Age range- 35–65 years. | G1 Control (n = 10) - Without orthodontic movement and without premature contact; G2 (n = 10) - Orthodontic movement only; G3 (n = 10) - Orthodontic movement plus laser irradiation (LLLT) |
Randomized clinical trial (?) | 90 days | Conventional computed tomography 3D Quantitative |
| 3 | Khaw et al. 201825 | 20 | 40 teeth | 8 males; 12 females Mean age – 15 years 9 months |
Group 1–20 teeth LLLT and OIRR; Group 2 - 20 teeth Sham and OIRR |
Double blind, split mouth randomized controlled trial | 6 weeks | Micro-computed tomography (micro-CT). |
| 4 | Okla et al. 201824 | Initial – 38 Dropouts – 12 Final sample – 26 |
52 teeth | Mean age: Experimental group- 16.7 ± 6.75 years. Control group-13.2 ± 0.99 years. |
Experimental group (n-12) – LLLT (Orthopulse) and OIRR; Control Group (n-11) - Placebo and OIRR |
Randomized controlled trial (?) | 6 months | Digital periapical radiographs, 2D Quantitative |
| 5 | Ng et al. 201723 | 20 | 40 teeth | 10 males - 16.4 ± 1.3years 10 females - 16.7 ± 1.1 years |
Group 1–20 teeth LLLT and OIRR; Group 2 - 20 teeth Placebo and OIRR |
Double blind, split mouth randomized controlled trial | 28 days | Micro-computed tomography, 3D Quantitative |
| 6 | Sousa et al. 200721 | 10 | 26 teeth | 6 female and 4 male patients Mean age of 13.1 years |
Laser Group (LG) - 13 teeth LLLT and OTM with OIRR; Control Group (CG) – 13 teeth Placebo and OTM with OIRR |
Randomized controlled trial (?) | 4 months | Periapical radiographs, 2D Quantitative |
3.3. Characteristics of the interventions
The type of orthodontic movement carried out varied across the studies. Ng et al., Ang-Khaw et al., and Goymen et al., exerted 150g of buccal tipping force on maxillary first premolars. Sousa et al. applied 150g retractive force on canines using NiTi coil spring, Okla et al. studied maxillary central incisors undergoing non-specific decrowding, and Fernandes et al. exerted intrusive force on maxillary molars.21,23,25, 26, 27 Details of the intervention (PBM), namely, the laser type, wavelength, manufacturer, output power, fluence/energy density, total dose per tooth, site of irradiation and duration and frequency were recorded (Table 3). Goymen et al., Ng et al. and Sousa et al. employed Gallium Aluminium Arsenic laser at a wavelength of 810 nm (LLLT group), 808 nm and 780 nm respectively.21,23,27 Ang-Khaw et al. used Aluminium-Gallium–Indium–Phosphorus (AlGaInP) at 660 nm.25 Fernandes et al. used an 808 nm diode but the semiconductor has not been specified.26 The powers used by the authors were 100 mW by Fernandes et al., 75 mW by Ang-Khaw et al., 20 mW by Sousa et al. and 180 mW (continuous delivery group) and 360 mW (pulsed delivery group) by Ng et al.21,25,26 The other two studies did not specify the power used.24,27 Goymen et al. used LED at 850 nm for their second test group.27 Okla et el reported to have used the OrthoPulse® device kit (Biolux Research Ltd.,Vancouver, BC, Canada) for photobiomodulation (850 nm wavelength) and Biolux devices as a placebo (24). In the trials by Ang-Khaw et al. & Ng et al., PBM was applied on 4 buccal and 4 palatal points around the roots of the MFP and Fernandes et al. applied it around 5 buccal and 5 palatal points.23,25,26 Sousa et al. did not specify the details of the points of irradiation while Okla et al. exposed the entire arch. Goymen et al. irradiated 10 points in total. In all the studies except the study by Okla et al., the laser tip was in direct contact with the tissue surface.
Table 3.
Details of intervention (photobiomodulation).
| S.No | Author | Laser type | Wavelength | Model (Manufacturer) | Output power (mW) | Fluence/Energy density (J/cm2) | Total dose per tooth | Site of application | Duration and frequency |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Goymen et al. 201927 | GaAlAs laser device LED application according to the manufacturer's instructions with an 850-nm wavelength |
Laser - 810-nm LED – 850 nm |
Cheese dental laser; Wuhan Gigaa Optronics Technology Co. Ltd., Wuhan, China OrthoPulse, Biolux Research Ltd., Vancouver, BC, Canada |
Not reported | Laser - 8 J/cm2 LED - 20 mW/cm2 |
10 points total | Laser - 0, 3, 7, 14, 21 and 28 days LED -10 min per day |
|
| 2 | Fernandes et al. 201926 | Diode laser | 808 nm | Laser Duo, MMOptics, São Carlos, SP, Brazil | 100 mW | Beam area = 0.04 cm2 Energy density - 25 J/cm2 |
10 points on the gingival tissue (five points per vestibular and five per palatine region): two points on the cervical third (one mesial and one distal gingiva), two points on the apical third (one mesial and one distal), and one point in the middle third (root center) | 10 s per point Three different moments: immediately after force application (T0), after 3 (T1) and 7 days (T2), as well as, whenever a new elastic chain was placed to activate the intrusion, during a total of 3 months |
|
| 3 | Khaw et al. 201825 | Aluminum-gallium-indium-phosphorus laser | 660 nm | Thor Photomedicine, Buckinghamshire, United Kingdom | 75-mW | Power density of 0.245 W/cm2 Fluence of 3.6 J/cm2 1/e2 spot size - 0.260 cm2, 1/e2 power density - 0.245 W/cm2 |
Total energy - 7.6 J | 4 points buccally and 4 palatally 2 points at the cervical portion (mesial and distal), 1 at midroot, and 1 at the apex of the tooth per buccal and lingual sides |
15 s per point LLLT regimen was performed at weekly sessions over a period of 6 weeks |
| 4 | Okla et al. 201824 | 850 nm | OrthoPulse® Biolux Research Ltd., Vancouver, BC, Canada |
Not reported | Continuous wave, 0.065 J/cm2 | Complete arch | 5 min per arch per day | ||
| 5 | Ng et al. 201723 | AlGaAs Aluminum-gallium-Arsenic |
808 nm | Klas, Konftec Corporation, Taiwan | Continuous mode- 180 mW Pulsed mode- 360 mW at 20 Hz |
Beam area of 0.5 cm2 Total irradiated surface area was 4 cm2 |
1.6 J per point | 4 buccal, 4 palatal points Apex, Middle third (centre of the root), Cervical third (mesial) and Cervical third (distal) |
Continuous laser - 9 s per point Pulsed laser - 4.5 s per point Days 0,1,2,3, 7, 14, 21. |
| 6 | Sousa et al. 201121 | Aluminum-gallium-arsenide (AsGaAl) | 780 nm | Twin Laser (MM Optics Ltda, São Carlos, São Paulo, Brazil) | 20 mW | 5 J/cm2 Irradiated area of about - 0.04 cm2 |
0.2 J of energy per point Total – 2J |
10 s per point Day 0, 3, 7, 30 and 60 |
3.4. Characteristics of the study outcomes
Ng et al., Ang-Khaw et al. and Goymen et al. assessed of the total amount of root resorption in a three-dimensional manner by measuring the volume of root surface craters using micro-CT images. Although Fernandes et al. employed CT for resorption measurement, resorption data was presented as root length loss (millimeters).23,25, 26, 27 Out of these, three studies (Ang-Khaw et al., Ng et al. and Goymen et al.) have further described the distribution of the resorption on four axial surfaces and three vertical thirds for each tooth with mean and standard deviations or standard errors.23,25,27 Fernandes et al. provided a graphical representation of root length changes in the mesiobuccal, distobuccal and palatal roots.26 The remaining two studies by Okla et al. and Sousa et al. evaluated the amount of the root resorption two-dimensionally by measuring the differences in the root length directly or by using the Levander and Malmgren Index on periapical radiographs respectively.21,24 The details have been elucidated in Table 4.
Table 4.
Characteristics of the study outcomes.
| S.No | Author/Year | Outcome (Mean ± SD) |
Difference | Results | Conclusion | ||
|---|---|---|---|---|---|---|---|
| LLLT | LED | Placebo/Sham | |||||
| 1 | Goymen et al. 201927 | Mean Crater Volume −0.42 ± 0.07 mm3 |
Mean Crater Volume −0.25 ± 0.03 mm3 | Mean Crater Volume −0.4 ± 0.06 mm3 |
LLLT versus Placebo- 0.016 mm3 less mean resorption in placebo group. LED versus Placebo- 0.154 mm3 less mean resorption in LED group. p value - 0.099 |
There is a tendency for Group 2 (LED group) to have few resorption values especially on the buccal side and in total. | Within the limitations of the study, no significant difference in root resorption with application of LLLT or LED. |
| 2 | Fernandes et al. 201926 | - | - | - | Only graphical representation provided. p value > 0.05 | Between G2 (orthodontic force only) and G3 (orthodontic force with PBM), shortening of MB and DB roots was greater in G2. No difference in the shortening of palatal root between groups G2 and G3 noted. | No comments made on root resorption. |
| 3 | Khaw et al. 201825 | Mean Crater Volume −0.746 ± 0.41 mm3 |
- | Mean Crater Volume −0.779 ± 0.374 mm3 |
0.033 mm3 less in the test group p value - 0.71 | Greater resorption of crater volume in the sham group compared with the laser group that was not statistically significant | No statistically or clinically significant difference was found in root resorption crater volumes be- tween the control group and the LLLT group when laser was applied weekly for 6 weeks. |
| 4 | Okla et al. 201824 | Mean Root Length - 19.63 mm | - | Mean Root Length - 20.85 mm | p value – 0.021 | Mean root length at the 6-month time interval was significantly shorter for the experimental group compared to the control group | Photobimodulation using Orthopluse did not reduce root resorption. |
| 5 | Ng et al. 201723 | Mean Crater Volume 0.381 ± mm3 |
- | Mean Crater Volume 0.495 mm3 |
114 mm3 less and 23% less mean resorption in Test group p value - 0.026 | LLLT treatment produces an average 0.114 mm3 (23%) less root resorption than the placebo. | LLLT seems promising in preventing or reducing orthodontic root resorption during the initial stages of orthodontic force application. |
| 5 | Sousa et al. 200721 | Mean resorption according to Levander and Malmgren Index – 0.08 | - | Mean resorption according to Levander and Malmgren Index – 0.15 | 0.07 (Levander Malmgren Index) p value - 0.592 | No statistically significant difference was found in the resorption of either root between the laser-irradiated and non-irradiated groups | No comments made on root resorption. |
3.5. Risk of bias of included studies
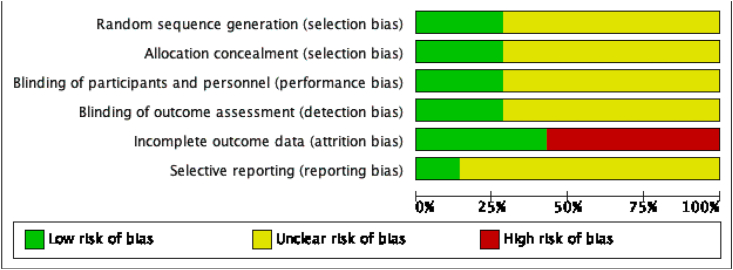
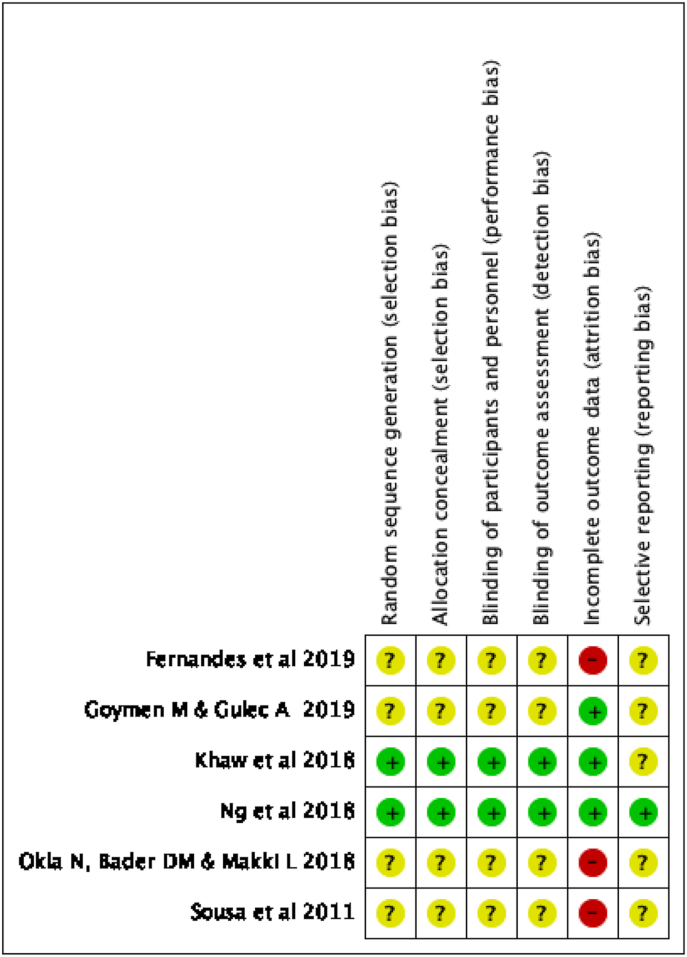
The risk of bias of all the included studies was ascertained within the specified domains of the Cochrane Risk of bias 2.0 tool. Out of the six studies, two clinical studies (Ng et al., Ang-Khaw et al.) had a low risk of bias across the various domains of Selection bias, Performance bias, Detection bias, Attrition Bias and Reporting bias as the studies conformed to the guidelines and reported the data in detail.23,25 The remaining four studies were placed in the category of overall unclear risk of bias as the information provided in the studies was insufficient to allot them to a high risk or a low risk category.21,24,26,27 Three studies namely Fernandes et al., Sousa et al. and Okla et al. failed to provide three-dimensional quantitative resorption data to be included in the meta-analysis, hence have been marked as a high risk of attrition bias.21,24,26 Performance of various trials in specific domains of the Cochrane Risk of bias tool is depicted in Table 5 along with pictorial representations generated in Revman software (version 5.4) in Fig. 2, Fig. 3. The Kappa statistic for inter-observer agreement for overall risk of bias categorization was 0.85.
Table 5.
Risk of Bias Assessment of included studies.
| S.No | Author | Selection Bias |
Performance Bias (Blinding of personnel) | Detection Bias (Blinding of outcome assessment) | Incomplete Outcome Data (Attrition Bias) | Reporting Bias (Selective reporting) | |
|---|---|---|---|---|---|---|---|
| Random Sequence Generation | Allocation Concealment | ||||||
| 1 | Goymen et al. 201927 | Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk Individuals included were randomly divided into three groups. |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’. |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’. |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
Low No missing outcome data |
Unclear Trial number not available |
| 2 | Fernandes et al. 201926 | Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk |
Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
High One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta-analysis; |
Unclear Trial number not available |
| 3 | Khaw et al. 201825 | Low The randomization scheme was generated by using www.randomization.com. Block sizes of 4, 6, 6, and 4 were used to maintain equal numbers of laser and sham treated sites between the left and right sides of the patients. |
Low Participants and investigators enrolling participants could not foresee assignment because a web based sequence was used to conceal allotment |
Low Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken |
Low Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. The outcome assessor was only unblinded after the teeth were scanned, root resorption craters counted, and the data had been collected and verified. |
Low No dropouts, the outcome assessment was completed on all |
Unclear Not available on the site |
| 4 | Okla et al. 201824 | Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk |
Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
High One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta-analysis |
Unclear Trial number not available |
| 5 | Ng et al. 201723 | Low The investigators describe a random component in the sequence generation process using a remote computerized random number generator. |
Low Participants and investigators enrolling participants could not foresee assignment because of the use of random permuted blocks with allocation concealed in sequentially numbered, opaque, sealed envelopes. |
Low Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken. It was a double-blind trial, both the experimental laser and the placebo-laser beams were invisible to the naked eye, and at 808 nm there was negligible glow from the laser; hence, both the participants and operator were blinded during this trial. |
Low Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. The outcome assessor was only unblinded after the teeth were scanned, root resorptions craters counted, and the data had been collected and verified. |
Low No dropouts, the outcome assessment was completed on all |
Low The study protocol is available and all of the study's pre-specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre-specified way |
| 6 | Sousa et al. 201121 | Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk |
Unclear Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk. |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
Unclear Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’ |
High One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta-analysis; |
Unclear Trial number not available |
Fig. 2.
Risk of bias of studies in specific domains of Cochrane Risk of Bias tool.
Fig. 3.
Risk of bias of individual studies in each domain of Cochrane Risk of Bias tool.
3.6. Results of individual studies, synthesis of results and additional analyses
Based on the magnitude of homogeneity in the methodologies and study outcomes, the number of studies included in the meta-analysis was three out of six (Ng et al., Ang-Khaw et al. and Goymen et al.)23,25,27 These studies were split-mouth randomized controlled trials applying 150g buccal tipping on maxillary first premolars and used micro-CT for volumetric analysis. The study by Ng et al. showed an average 0.114 mm3 less root resorption than the placebo which had statistical significance (P = 0.026). In the study by Ang Khaw et al., there was a mean difference of 0.033 mm3 greater resorption crater volume in the sham group compared with the intervention group which statistically insignificant (P = 0.71).25 For the purpose of synthesizing the results, the three study groups of Goymen et al. were arranged into two sets – first, the laser versus placebo group and second, the LED versus placebo group. In their study, there was a non-significant increase of 0.016 mm3 in resorption in laser group vis-à-vis placebo group and a non-significant decrease in resorption of 0.154 mm3 in LED group compared to control group.27
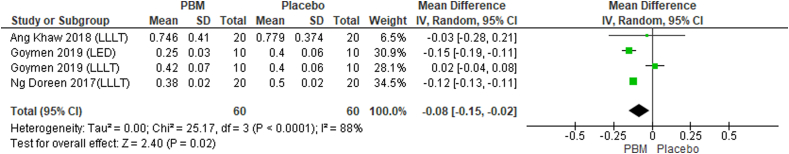
The overall sample size of the meta-analysis of the 4 groups extracted out of 3 studies consisted of 60 teeth in the photobiomodulation (Laser/LED) arm and 60 teeth in the placebo arm. Mean difference was used to determine the association and random effect model was applied for meta-analysis. There was high heterogeneity in the included studies as determined by I2 index (88%) with appreciable variation in the confidence intervals. The pooled mean difference for overall total root resorption was 0.08 (95% CI 0.15 – (−0.02) to 1.96, p=<0.0001) in favour of photobiomodulation group i.e. significantly lesser total root resorption was seen in the photobiomodulation group (Fig. 4).
Fig. 4.
Forest plot of mean total root resorption.
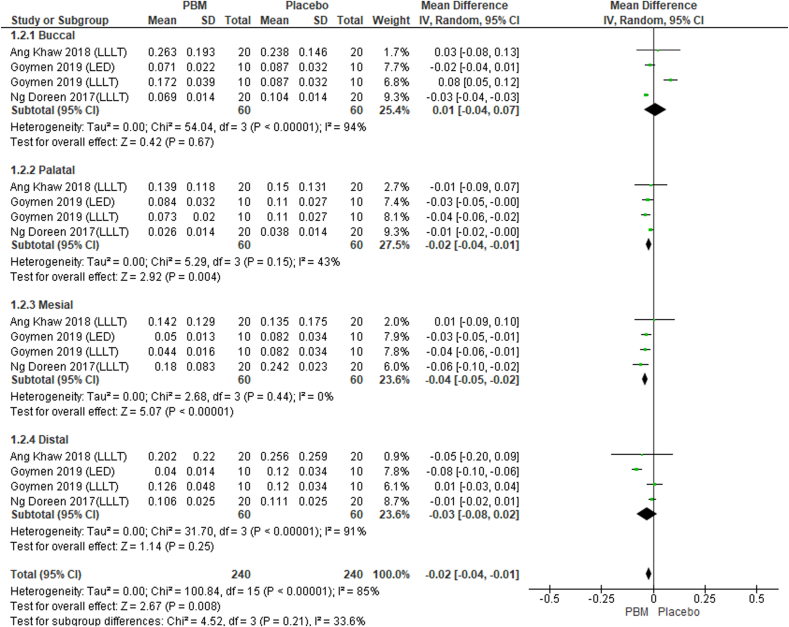
Subgroup analysis (Fig. 5) was done to determine the root resorption on different axial surfaces. I2 test revealed high heterogeneity in the included studies for resorption data for the buccal (94%, p < 0.01) and distal (91%, p < 0.01) surfaces while it was lower for palatal surface (43%, p = 0.15) and the least for mesial surface resorption values (0%, p = 0.44). The pooled mean differences obtained in root resorption between the photobiomodulation groups and control groups were 0.03, −0.02, −0.04, −0.03 for buccal, palatal, mesial and distal surfaces respectively.
Fig. 5.
Forest plot of mean resorption on each axial surface of root i.e. buccal, palatal, mesial and distal surface.
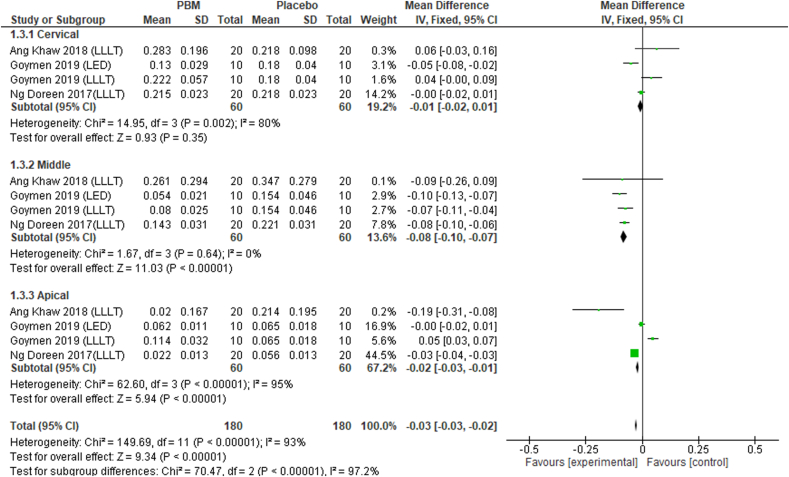
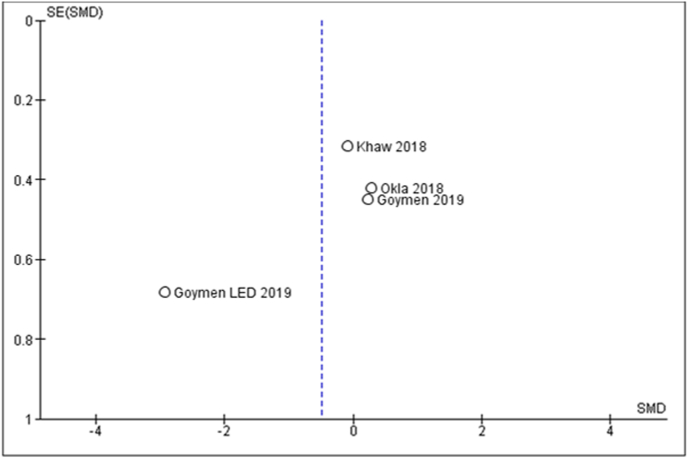
Furthermore, subgroup analysis (Fig. 6) was conducted for resorption volumes on three vertical divisions of a premolar root viz. cervical, middle and apical third. I2 testing showed high heterogeneity and non-significant pooled mean differences between test and control groups with respect to cervical and apical thirds. The pooled mean difference for the middle third was 0.08 in favour of photobiomodulation (p < 0.00001). The funnel plot is depicted in Fig. 7.
Fig. 6.
Forest plot of mean resorption on each vertical third of root surface i.e. coronal, middle and apical third.
Fig. 7.
Funnet plot.
4. Discussion
The present systematic review applied the selection criteria so as to restrict the review to human trials aiming to scrutinize the impact of photobiomodulation on orthodontic root resorption. A systematic review by Michelogiannikis in 2019 included both animal and human studies and concluded that photobiomodulation effects on root resorption were debatable.8 There is skepticism about the extrapolation of conclusions of animal research onto man since there is a considerable difference between the tooth size of rats and humans.12 To avoid incoherence in drawing conclusions, the participants included in the present systematic review were limited to human teeth.
The criterion of intervention in this review was selected as photobiomodulation in the form of low-level diode laser or light-emitting diode. In the present study, the final data which was synthesized for meta-analysis included three groups with LLLT and one with LED as intervention group.
The focus of the method of outcome assessment in the current systematic review was laid on quantification of the root resorption so as to enable decisive interpretation of the magnitude of effect of the intervention. Out of the six studies, two studies employed periapical radiographs (Sousa et al., Okla et al.) while the remaining used three-dimensional computed tomography. The validities of 2D radiographic analyses can be questionable as demonstrated by Chan et al. owing to parallax errors and surface material denudation while preparing specimens for the same.28 Furthermore, owing to the meagre methodological homogeneity amongst the 6 studies, trials with two-dimensional resorption data were excluded from the meta-analysis (Sousa et al., Okla et al.).21,24 Although Fernandes et al. employed conventional computed tomography for resorption measurement, data was presented as root length shortening (millimeters), permitting the study to be excluded from the meta-analysis.26 Consequently, three studies, Ng et al., Ang-Khaw et al. and Goymen et al. qualified and were selected for the meta-analysis.23,25,27 Mean difference was the calculated summary effect as the outcome was a continuous variable and the random effects model was used due to the heterogeneity amongst the selected studies. The risk of bias assessment using Cochrane's RoB tool revealed that two out three studies chosen for meta-analysis carried ‘low’ overall risk of bias (Ng et al. and Ang-Khaw et al.) and one study carried ‘unclear’ risk of bias (Goymen et al.).
The meta-analysis demonstrated a positive effect of photobiomodulation with regards to mean total root resorption per tooth although it depicts considerable statistical heterogeneity and the evidence for the same is strong (p < 0.05). The sub-group analyses of axial surfaces show decrease in root resorption in the irradiated teeth on their mesial, distal and palatal surfaces but there is statistically significant heterogeneity for buccal and distal surfaces (I2 = 94% and 91% respectively). Further, the low and moderate heterogeneities of mesial and palatal surface resorptions are based on weak statistical evidence. Similarly, in terms of vertical thirds, photobiomodulation groups tended to demonstrate lower resorption per vertical third but only the middle third showed overlapping confidence intervals and insignificant heterogeneity (I2 = 0%). The Summary of Findings (SoF) table formulated according to GRADE Pro in order to appraise the quality of evidence showed a moderate overall quality of evidence. Risk of bias was not serious as the potential limitations in study design were unlikely to lower the confidence in the estimate of the effect. Inconsistency was graded as serious owing to the considerable heterogeneity in the outcome. Indirectness and imprecision were not serious and hence the certainty of evidence was moderate (Table 6). The funnel plot generated to evaluate publication bias shows asymmetry but the interpretation derived from it should not be relied upon as the number of studies in considerably low.
Table 6.
Summary of Findings according to GRADE Assessment Profile.
4.1. Limitations and recommendations
A limitation of the present systematic review is the low number of randomized controlled trials conducting quantitative analysis of root resorption using comparable measurement methods. There is also a probability for different biological reactions being elicited by different wavelengths of photobiomodulation lights.29,30 Even though there may not be significant therapeutic differences between LLLT and LED, the evidence for the same has yet to be established. Furthermore, orthodontic force factors have a bearing on the magnitude and distribution of root resorption along with the duration of study and outcome assessment method which were found to be variable.31 In view of this knowledge, the results of the meta-analysis must be interpreted with caution. It is strongly recommended that high-quality trials with more uniformity in intervention methodology be executed.
5. Conclusions
The following conclusions may be drawn from the present review:
-
1.
There is moderate grade of evidence to suggest that photobiomodulation has a beneficial effect on root resorption.
-
2.
More high-quality randomized controlled trials with similarity in intervention methods are required for better strength of evidence regarding the influence of PBM on root resorption related to orthodontic tooth movement.
Ethics approval and participation consent
Not applicable.
Consent for publication
The authors give consent for publication.
Funding
The study is self-funded.
Availability of supporting data
The data can be shared on request.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jobcr.2022.05.014.
Contributor Information
Nida Nayyer, Email: drnidanayyer@outlook.com.
Tulika Tripathi, Email: drtulikatripathi@yahoo.com.
Gayatri Ganesh, Email: gayatri2ganesh@gmail.com.
Priyank Rai, Email: priyankraibraces@hotmail.com.
ABBREVIATIONS
- PBM
Photobiomodulation
- OIIRR
Orthodontically induced inflammatory root resorption
- ATP –
Adenosine Triphosphate
- microCT
micro-computed tomography
- LLLT
Low-level laser therapy
- LED
Light-emitting diode
- μm3 –
cubic micrometer
- mm3
cubic millimeter
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Weltman B., Vig K.W.L., Fields H.W., Shanker S., Kaizar E.E. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137(4):462–476. doi: 10.1016/j.ajodo.2009.06.021. Available from: [DOI] [PubMed] [Google Scholar]
- 2.Brezniak N., Wasserstein A. Orthodontically induced inflammatory root resorption . Part I : the basic science aspects. Angle Orthod. 2002;72(2):175–179. doi: 10.1043/0003-3219(2002)072<0175:OIIRRP>2.0.CO;2. Available from: [DOI] [PubMed] [Google Scholar]
- 3.Lund H., Grondahl K., Hansen K., Grondahl H. Apical root resorption during orthodontic treatment A prospective study using cone beam CT. Angle Orthod. 2012;82:480–487. doi: 10.2319/061311-390.1. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jönsson A., Malmgren O., Levander E. Long-term follow-up of tooth mobility in maxillary incisors with orthodontically induced apical root resorption. Eur J Orthod. 2007;29(5):482–487. doi: 10.1093/ejo/cjm047. Available from: [DOI] [PubMed] [Google Scholar]
- 5.Sondeijker C.F.W., Lamberts A.A., Beckmann S.H., et al. Development of a clinical practice guideline for orthodontically induced external apical root resorption. Eur J Orthod. 2020;42(2):115–124. doi: 10.1093/ejo/cjz034. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brezniak N., Wasserstein A. Orthodontically induced inflammatory root resorption . Part II : the clinical aspects. Angle Orthod. 2002;72(2):180–184. doi: 10.1043/0003-3219(2002)072<0180:OIIRRP>2.0.CO;2. Available from: [DOI] [PubMed] [Google Scholar]
- 7.Raza H., Major P.W., Dederich D., El-Bialy T. Effect of low-intensity pulsed ultrasound on orthodontically induced root resorption caused by torque: a prospective, double-blind, controlled clinical trial. Angle Orthod. 2016;86(4):550–557. doi: 10.2319/081915-554.1. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michelogiannakis D., Al-shammery D., Akram Z., Rossouw P.E., Javed F., Romanos G.E.S.C. Arch Oral Biol. 2019;100:1–13. doi: 10.1016/j.archoralbio.2019.01.017. Available from: [DOI] [PubMed] [Google Scholar]
- 9.Chung H., Dai T., Sharma S.K., Huang Y.-Y., Carroll J.D., Hamblin M.R. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533. doi: 10.1007/s10439-011-0454-7. http://link.springer.com/10.1007/s10439-011-0454-7 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zein R., Selting W., Hamblin M.R. Review of light parameters and photobiomodulation efficacy: dive into complexity. J Biomed Opt. 2018;23(12):1–17. doi: 10.1117/1.JBO.23.12.120901. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heiskanen V., Hamblin M.R., Diseases M., Hospital M.G. Photobiomodulation : lasers vs light emitting diodes. Photochem Photobiol Sci. 2019;17(8):1003–1017. doi: 10.1039/c8pp00176f. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seifi M., Vahid-Dastjerdi E. Tooth movement alterations by different low level laser protocols: a literature review. J Laser Med Sci. 2015;6(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Deana N.F., Zaror C., Sandoval P., Alves N. Effectiveness of low-level laser therapy in reducing orthodontic pain: a systematic review and meta-analysis. Pain Res Manag. 2017;2017 doi: 10.1155/2017/8560652. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cepera F., Torres F.C., Scanavini M.A., et al. Effect of a low-level laser on bone regeneration after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2012 Apr;141(4):444–450. doi: 10.1016/j.ajodo.2011.10.023. Available from: [DOI] [PubMed] [Google Scholar]
- 15.Mcgrath C, Gu M. Effects of Low-Level Laser Therapy as an Adjunct for Orthodontic Retention : A Systematic Review of Human and Animal Studies. Pre-screen. Available from: 10.21203/rs.3.rs-28836/v1. [DOI]
- 16.Atrium T., Gate S., Road T.C., Collaboration T.C., Kingdom U. 2011. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- 17.PRISMA checklist. http://prisma-statement.org/prismastatement/Checklist.aspx Available from:
- 18.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions : explanation and elaboration. J Clin Epidemiol. 2009;62 doi: 10.1371/journal.pmed.1000100. e1–34. Available from: [DOI] [PubMed] [Google Scholar]
- 19.Guyatt G.H., Oxman A.D., Santesso N., et al. GRADE guidelines : 12 . Preparing Summary of Findings tables - binary outcomes. J Clin Epidemiol. 2013;66(2):158–172. doi: 10.1016/j.jclinepi.2012.01.012. Available from: [DOI] [PubMed] [Google Scholar]
- 20.Cruz D.R., Kohara E.K., Ribeiro M.S., Wetter N.U. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Laser Surg Med. 2004;35(2):117–120. doi: 10.1002/lsm.20076. Available from: [DOI] [PubMed] [Google Scholar]
- 21.da Silva Sousa M.V., Scanavini M.A., Sannomiya E.K., Velasco L.G., Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg. 2011;29(3):191–196. doi: 10.1089/pho.2009.2652. https://www.liebertpub.com/doi/10.1089/pho.2009.2652 Available from: [DOI] [PubMed] [Google Scholar]
- 22.Nimeri G., Kau C.H., Corona R., Shelly J. The effect of photobiomodulation on root resorption during orthodontic treatment. Clin Cosmet Invest Dent. 2014;6:1–8. doi: 10.2147/CCIDE.S49489. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ng D., Chan A.K., Papadopoulou A.K., Dalci O., Petocz P., Darendeliler M.A. The effect of low-level laser therapy on orthodontically induced root resorption: a pilot double blind randomized controlled trial. Eur J Orthod [Internet] 2017:1–9. doi: 10.1093/ejo/cjx065. Available from: [DOI] [PubMed] [Google Scholar]
- 24.Okla N., Bader D., Makki L. Effect ofphotobiomodulation on maxillary decrowding and root resorption: a randomized clinical trial. APOS Trends Orthod. 2018;8:86–91. doi: 10.4103/apos. [DOI] [Google Scholar]
- 25.Ang Khaw C.M., Dalci O., Foley M., Petocz P., Darendeliler M.A., Papadopoulou A.K. Physical properties of root cementum: Part 27. Effect of low-level laser therapy on the repair of orthodontically induced inflammatory root resorption: a double-blind, split-mouth, randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 2018;154(3):326–336. doi: 10.1016/j.ajodo.2018.04.022. Available from: [DOI] [PubMed] [Google Scholar]
- 26.Fernandes M.R.U., Suzuki S.S., Suzuki H., Martinez E.F., Garcez A.S. Photobiomodulation increases intrusion tooth movement and modulates IL‐6, IL‐8 and IL‐1β expression during orthodontically bone remodeling. J Biophot. 2019;12(10) doi: 10.1002/jbio.201800311. [DOI] [PubMed] [Google Scholar]
- 27.Goymen M., Gulec A. Effect of photobiomodulation therapies on the root resorption associated with orthodontic forces: a pilot study using micro computed tomography. Clin Oral Invest. 2020;24(4):1431–1438. doi: 10.1007/s00784-019-03155-w. [DOI] [PubMed] [Google Scholar]
- 28.Chan E.K.M., Darendeliler M.A. Exploring the third dimension in root resorption. Orthod Craniofac Res. 2004;7(2):64–70. doi: 10.1111/j.1601-6343.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y., Huang Y., Wang Y., Lyu P., Hamblin M.R. Biochimica et Biophysica Acta Photobiomodulation of human adipose-derived stem cells using 810 nm and 980 nm lasers operates via different mechanisms of action. BBA - Gen Subj. 2017;1861(2):441–449. doi: 10.1016/j.bbagen.2016.10.008. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santana-blank L., Rodrı E., Santana-rodrı K. Theoretic , experimental , clinical bases of the water oscillator hypothesis in near-infrared photobiomodulation. 2010; Photomed Laser Surg. 2010 Aug;28(Suppl 1):S41–S52. doi: 10.1089/pho.2009.2647. [DOI] [PubMed] [Google Scholar]
- 31.Nayyer N., Tripathi T., Gopal R. Effect of photobiomodulation on external root resorption during orthodontic tooth movement—a scoping review. Laser Dent Sci. 2019;3(4):219–226. doi: 10.1007/s41547-019-00072-9. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data can be shared on request.