Abstract
Background:
Coronary artery calcium (CAC) is a measure of atherosclerotic burden and well-validated for risk stratification in middle- to older-aged adults. Few studies have investigated CAC in younger adults, and there is no calculator for determining age, sex, and race-based percentiles among individuals <45 years old.
Objectives:
To determine the probability of CAC >0 and develop age-sex-race percentiles for U.S. adults aged 30–45 years.
Methods:
We harmonized three datasets – Coronary Artery Risk Development in Young Adults (CARDIA), the CAC Consortium, and the Walter Reed Cohort – to study CAC in 19,725 asymptomatic Black and White individuals aged 30–45 without known atherosclerotic cardiovascular disease (ASCVD). After weighting each cohort equally, the probability of CAC >0 and age-sex-race percentiles of CAC distributions were estimated using nonparametric techniques.
Results:
The prevalence of CAC >0 was 26% among White males, 16% among Black males, 10% among White females, and 7% among Black females. CAC >0 automatically placed all females at >90th percentile. CAC >0 placed White males at the 90th percentile at age 34 compared to Black males at age 37. An interactive webpage allows one to enter an age, sex, race, and CAC score to obtain the corresponding estimated percentile.
Conclusions:
In a large cohort of U.S. adults aged 30–45 without symptomatic ASCVD, the probability of CAC >0 varied by age, sex and race. Estimated percentiles may help interpretation of CAC scores among young adults relative to their age-sex-race matched peers and can henceforth be included in CAC score reporting.
Keywords: cardiovascular diseases, cardiovascular risk, coronary artery calcium, coronary artery disease, multidetector computed tomography, percentiles, premature atherosclerosis, primary prevention, young adults
Tweet:
The first calculator for determining age, sex, and race-based percentiles of coronary artery calcium (CAC) for individuals aged 30–45 years, from a dataset of 19,725 asymptomatic Black and White individuals.
CONDENSED ABSTRACT
We studied CAC in 19,725 Black and White individuals aged 30–45 without symptomatic cardiovascular disease to determine the probability of CAC >0 and develop age-sex-race percentiles. CAC >0 automatically placed females at >90th percentile. CAC >0 placed White males at the 90th percentile at age 34 compared to Black males at age 37. An interactive webpage allows one to enter an age, sex, race, and CAC score to obtain the corresponding estimated percentile. This may help interpretation of CAC scores among young adults relative to their age-sex-race matched peers and can henceforth be included in CAC score reporting.
INTRODUCTION
Atherosclerotic cardiovascular diseases (ASCVD) cause nearly one-third of all deaths in the United States and are the leading cause of global mortality.(1) Multiple cardiovascular guidelines recommend use of 10-year absolute ASCVD risk estimates to guide preventive treatments;(2) however, because these scores rely heavily on subject age, nearly all young adults are estimated to have low 10-year ASCVD risk, and even those with non-optimal risk factors are often not offered preventive therapies despite the possibility of subclinical atherosclerosis.(3) Better methods of ASCVD risk stratification are needed to identify young patients who are most likely to benefit from preventive interventions at an earlier age.(2,4)
The need for early detection of subclinical coronary artery disease has led to investigation of coronary artery calcification (CAC) as a direct marker of atherosclerosis. Numerous studies have demonstrated the prognostic utility of CAC to stratify risk for individuals without known ASCVD.(2) Although most efforts have focused on the yield of measurement in middle to older-aged adults, there is increasing interest in CAC as a clinical decision-making tool to identify young adults at elevated risk so preventive measures can be employed to alter their atherosclerotic trajectories and long-term risks.(2,5) Due to a lower overall prevalence of CAC in the young, specific tools for prediction and interpretation of CAC scores are needed to help direct primary preventive efforts among young adult subpopulations with higher prevalence of CAC.(5,6) For example, the Multi-Ethnic Study of Atherosclerosis (MESA) CAC Reference tool allows calculation of age, sex, and race-based CAC percentiles, has become standard for clinical CAC reporting, and is referenced in current prevention guidelines; however, this tool is limited to ages 45–84.(6)
To fill this gap, we aimed to perform the largest study of CAC in US young adults to date by harmonizing three cohorts comprising 19,725 combined individuals to estimate the probability of CAC>0 and develop age-sex-race CAC percentile scores for individuals aged 30–45 years.
METHODS
Study Cohort
We investigated CAC in 19,725 predominantly Black and White individuals aged 30–45 at the time of their CAC exam without symptomatic CVD from three studies: (1) the Walter Reed Cohort (n=8,840), a study of eligible low-risk adult patients who underwent CAC testing at Walter Reed Army Medical Center between January 1997 and August 2009,(1) (2) the CAC Consortium (n=7,507), a multi-center cohort study of eligible patients who were referred for CAC scoring for clinical risk stratification between 1992 through 2011,(7) and (3) the Coronary Artery Risk Development in Young Adults (CARDIA; n=3,378) study, a community-based NHLBI-funded cohort of patients with socioeconomic diversity and nearly equal numbers of Black and White participants with CAC exams starting between 1995–2001 and intermittent retesting at 5-year intervals (8). For subjects with multiple CAC exams, we used the earliest exam available. We excluded individuals with missing race and very young adults aged 18–29 due to small numbers and lack of generalizability from a selected, potentially high-risk subset of the general population where CAC testing is not routinely performed. Informed consent was waived due to the retrospective nature of the study (University of Virginia Institutional Review Board-Health Sciences Research Study Tracking #22517).
Calcium Scoring
CAC scoring was performed in all individuals based on the Agatston method.(9) Electron beam computed tomography (EBT) and multidetector CT scanners (MDCT) were used in the three cohorts.(10–12) Prior studies have demonstrated no clinically meaningful differences between CAC scores derived from EBT versus MDCT scanners.(13) CARDIA performed two CT scans 1–2 minutes apart for each participant and had both scans reviewed independently of the other. The mean score was used. CARDIA also utilized a standard calcium phantom scanned underneath the participants; studies have demonstrated no significant differences between phantom-adjusted and unadjusted Agatston CAC scores.(11)
Statistical Analysis
Individuals were classified based on the presence or absence of calcium and further subdivided into CAC score groups of 0 (none), 1–10 (low), 11–100 (moderate), and >100 (high). Demographics, baseline characteristics, and prevalence of cardiovascular risk factors at the time of CAC exam for the total dataset and each of the sex-race groups for which percentiles were created (White males, White females, Black males, Black females) are shown in Table 1. There were insufficient individuals to create percentiles for other races. Comparisons between individual cohorts are shown in Table 2. A p < 0.05 was considered significant for all comparisons. Definitions for risk factors in each dataset can be found in prior publications.(1,10,14) Of note, smoking was recorded as current smoker in CARDIA and the CAC Consortium and ever smoker in the Walter Reed Cohort.
Table 1:
Characteristics of the Study Sample
| All (N=19,725) |
Females (N=5,403) |
Males (N=14,322) |
White Females (N=3,691) |
White Males (N=11,352) |
Black Females (n=1,363) |
Black Males (N=1,9653 |
|
|---|---|---|---|---|---|---|---|
| Age, mean (SD) | 41 (3.3) | 41 (3.2) | 41 (2.9) | 41 (3.2) | 41 (3.1) | 40 (3.7) | 41 (3.4) |
| Race, n (%) | |||||||
| • White | 15,043 (76) | 3,691 (68) | 11,352 (79) | - | - | - | - |
| • Black | 3,316 (17) | 1,363 (25) | 1,953 (14) | - | - | - | - |
| CAC Score, mean (SD) | 14 (91) | 5 (70) | 18 (98) | 6 (81) | 17 (93) | 3 (20) | 12 (91) |
| CAC Group, n (%) | |||||||
| • CAC=0 | 15,655 (79) | 4,921 (91) | 10,734 (73) | 3,424 (93) | 8,668 (74) | 1,272 (93) | 1,650 (84) |
| • CAC >0 | 4,070 (21) | 482 (9) | 3,588 (25) | 362 (10) | 3,026 (26) | 95 (7) | 311 (16) |
| • CAC 1–10 | 1,671 (8) | 222 (4) | 1,449 (10) | 169 (5) | 1,218 (10) | 46 (3) | 136 (7) |
| • CAC 11–100 | 1775 (9) | 203 (4) | 1,572 (11) | 152 (4) | 1,334 (11) | 38 (3) | 128 (6) |
| • CAC >100 | 624 (3) | 57 (1) | 567 (4) | 41 (1) | 474 (4) | 11 (1) | 47 (2) |
| Hypertension, n (%) | 3123 (16) | 703 (13) | 2420 (17) | 406 (11) | 1,762 (15) | 240 (18) | 492 (26) |
| Hyperlipidemia, n (%) | 8155 (41) | 1,926 (36) | 6,229 (44) | 1,333 (36) | 5,101 (44) | 511 (38) | 810 (41) |
| Smoking*, n (%) | 1,988 (10) | 683 (13) | 1,304 (9.1) | 402 (11) | 946 (8) | 265 (19) | 290 (15) |
| Diabetes, n (%) | 572 (3) | 190 (3.5) | 382 (3) | 125 (3) | 246 (2) | 55 (4) | 97 (5) |
Recorded as current smoking in CARDIA and CAC Consortium, ever smoking in Walter Reed Cohort
Table 2.
Characteristics of the Unweighted Cohorts by Sex
| Females N=5,403 |
Males N=14,322 |
|||||||
|---|---|---|---|---|---|---|---|---|
| CARDIA N=1,856 |
WRC N=1,684 |
CACC N=1,863 |
CARDIA N=1,522 |
WRC N=7,156 |
CACC N=5,644 |
|||
| Mean Age (years) +/− SD | 40.0 +/− 3.7 | 41.7 +/− 2.7 | 41.4 +/− 2.9 | <0.001 | 39.8 +/− 3.8 | 41.8 +/− 2.6 | 41.1 +/− 3.0 | <0.001 |
| Race, n (%) | <0.001 | <0.001 | ||||||
| • White | 925 (50) | 1,187 (70) | 1,579 (85) | 847 (55) | 5,497 (77) | 5,000 (89) | ||
| • Black | 931 (50) | 369 (22) | 63 (3) | 675 (44) | 1,170 (16) | 108 (2) | ||
| Mean CAC Score +/− SD | 3.2 +/− 31.9 | 2.9 +/− 24.5 | 9.8 +/− 111.9 | <0.001 | 14.0 +/− 126.5 | 12.8 +/− 70.6 | 24.9 +/− 117.0 | <0.001 |
| CAC Group, n (%) | <0.001 | <0.001 | ||||||
| • CAC=0 | 1,737 (94) | 1,562 (93) | 1,622 (87) | 1,257 (83) | 5,694 (80) | 3,783 (67) | ||
| • CAC >0 | 119 (6) | 122 (7) | 241 (13) | 265 (17) | 1,462 (20) | 1,861 (33) | ||
| • CAC 1–10 | 61 (3) | 53 (3) | 100 (5) | 109 (7) | 541 (8) | 799 (14) | ||
| • CAC 11–100 | 43 (2) | 57 (3) | 103 (5) | 118 (8) | 700 (9) | 754 (13) | ||
| • CAC 101+ | 15 (1) | 12 (1) | 30 (3) | 38 (2) | 221 (3) | 300 (5) | ||
| Hypertension, n (%) | 139 (7) | 296 (18) | 268 (14) | <0.001 | 106 (7) | 1,330 (19) | 984 (17) | <0.001 |
| Hyperlipidemia, n (%) | 764 (41) | 372 (22) | 790 (42) | <0.001 | 723 (48) | 2,339 (34) | 3,167 (56) | <0.001 |
| Smoking*, n (%) | 382 (21) | 83 (5) | 219 (12) | <0.001 | 352 (23) | 348 (5) | 604 (11) | <0.001 |
| Diabetes, n (%) | 72 (4) | 59 (4) | 59 (3) | 0.43 | 35 (2) | 173 (2) | 174 (3) | 0.052 |
Smoking recorded as current in CARDIA and CACC, ever in Walter Reed. CARDIA = Coronary Artery Risk Development in Young Adults, CACC = CAC Consortium, CAC = Coronary Artery Calcium.
Given the diverse settings of each of the studies and their different sizes, the three cohorts were weighted so that each contributed 1/3 of the final analytic dataset. We also applied standardized weighting methods to the CAC Consortium so each study site was equally represented. The pooled and weighted analysis thus leveraged study heterogeneity, with equal contribution from the community-based CARDIA sample as from each of the clinical populations, in an effort to provide a truer reflection of the variation within the US population with access to medical care. The weighted dataset was then used to calculate the estimated probability of CAC >0 and calculate the CAC percentiles.
We modeled the probability of CAC >0 as a function of age, stratified by sex and race for White and Black participants. Since the distribution of CAC in this young cohort was skewed, with the majority of young subjects having no calcium, we used a nonparametric local weighted estimated scatterplot smoothing (LOWESS) regression applied to the raw data. This nonparametric approach allowed us to consider age as a continuous variable and provided greater precision in estimation of percentiles by using the pooled residual distribution, after accounting for age, sex, and race.
Next, we followed the protocol used in the creation of MESA-derived CAC population percentiles to create our percentile scores.(6) Following the methods described by McClelland et al., we modeled the mean of the log CAC distribution nonparametrically as a function of age for males and females using LOWESS regression.(15) We subtracted the corresponding estimated value from each observation in the positive log-transformed CAC distribution. The pooled residuals from the model were ranked and each kth percentile (k=1…100) was calculated. Adding these to the fitted value for a particular age, sex, and race yielded an estimated percentile for the log-transformed positive CAC variable. Taking the exponential of this percentile yielded the kth percentile of the positive portion of the CAC distribution. If a certain proportion (p) had zero calcium, the kth percentile calculated above is the 100×{p+((1−p)k)/100} percentile of the overall distribution. We modeled p as a nonparametric function of age by fitting a LOWESS regression within each sex and race. Thus, the percentiles of the whole distribution are estimated as a function of the percentiles of the positive calcium scores, and the process does not involve any parametric assumptions.(6) The 75th, 90th, and 95th, 97.5th percentiles were compared between Black males, Black females, White males, and White females. Calculations were performed with STATA, version 15.1.
Lastly, an interactive percentile calculator was created on a public webpage with the same design as the MESA percentile calculator that allows one to enter an age, sex, and race to obtain an estimated probability of CAC > 0 and corresponding estimated 75th, 90th, 95th, and 97.5th CAC percentiles (Central Illustration).(16) One can optionally add an observed CAC score to obtain the estimated age-sex-race percentile for that score.(16)
Central Illustration. Online CAC Percentile Calculator with example 36-year-old White male patient.
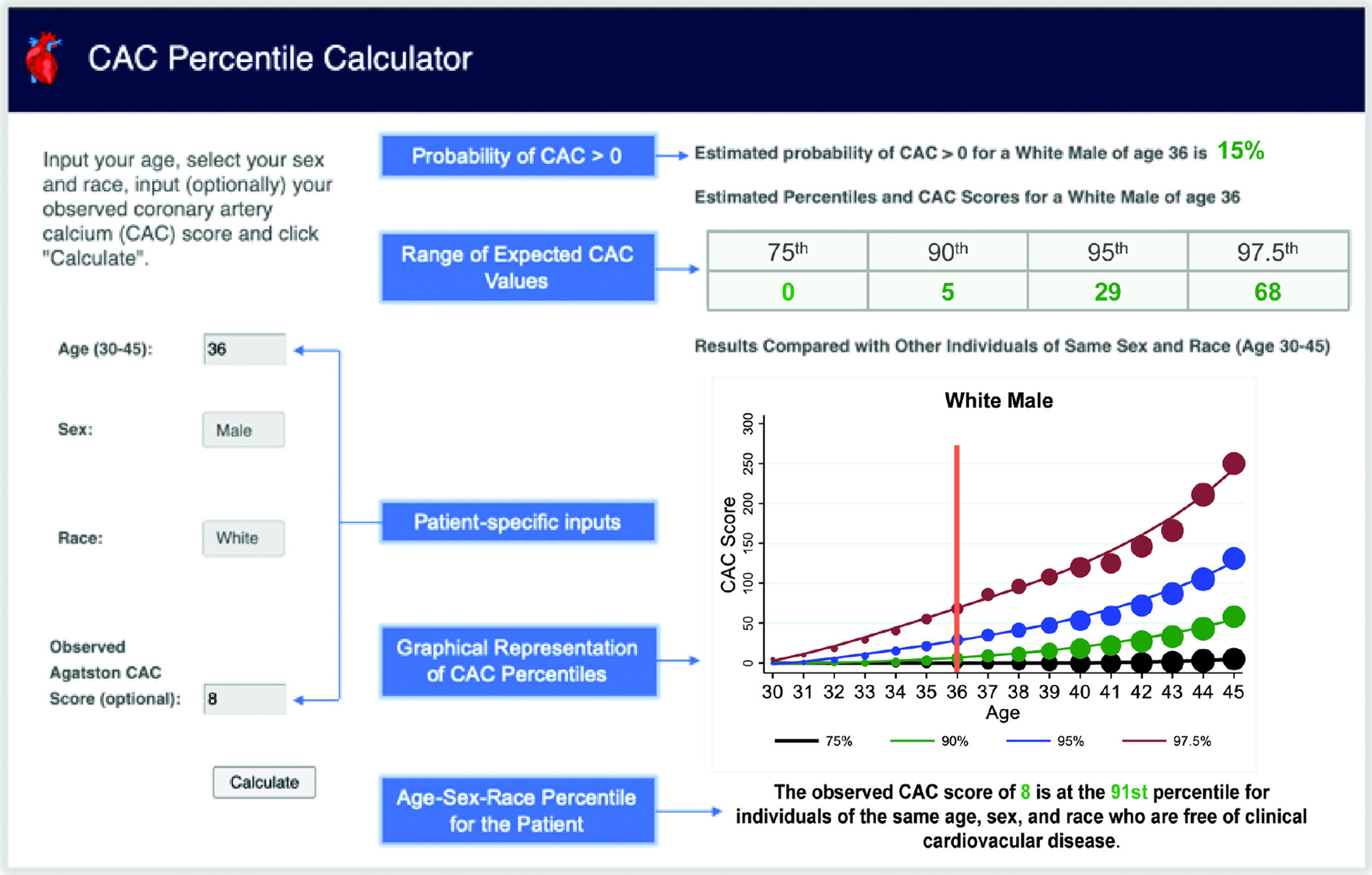
Despite having a low absolute CAC score of 8, he is at the 91st percentile compared to his age-sex-race matched peers. CAC = coronary artery calcium. (16)
RESULTS
Table 1 presents the baseline characteristics at time of CAC exam. The cohort (n=19,725) was 73% male with mean ± SD age 41 ± 3 years. 76.5% of subjects self-identified as being White, while approximately 16.5% identified as Black and 7% as other racial/ethnic groups (including Hispanic, Asian, Native American, etc.). There were only sufficient numbers of White and Black individuals to calculate subsequent CAC probabilities and percentiles. Black individuals comprised a greater proportion of all females (25%) compared to males (13%). Overall, the prevalence of hypertension was 17%, hyperlipidemia was 41%, smoking was 10%, and diabetes was 3%. Hypertension and hyperlipidemia were more common in males, while smoking and diabetes were more common in females. The prevalence of CAC and risk factors for each individual cohort by sex are shown in Table 2.
The overall prevalence of any CAC was 21% with 8%, 9%, and 3% having scores of 1–10, 11–100, and >100 AU, respectively. Males had a higher prevalence of non-zero CAC (25%) and higher mean CAC scores (18 ± 98) than did females (9% and 5 ± 70, respectively). White individuals had higher CAC scores than Black individuals; the prevalence of CAC >0 was 26% among White males, 16% among Black males, 10% among White females, and 7% among Black females. Figure 1 displays the probability of a non-zero CAC score for each sex and race group (Black and White) as a function of age, which was modeled using a nonparametric fit. The solid line represents a local regression smoother applied to the raw data. The individual circles represent the observed age-specific probability, with circle size reflecting the available sample size at that age (larger circles indicate more participants). Overall, the prevalence and amount of calcification was greater at older ages, which was more pronounced in males than in females. Sex-specific plots for the individual cohorts are shown in Supplemental Figure 1.
Figure 1. Estimated and observed weighted probability of detectable CAC by sex/race.
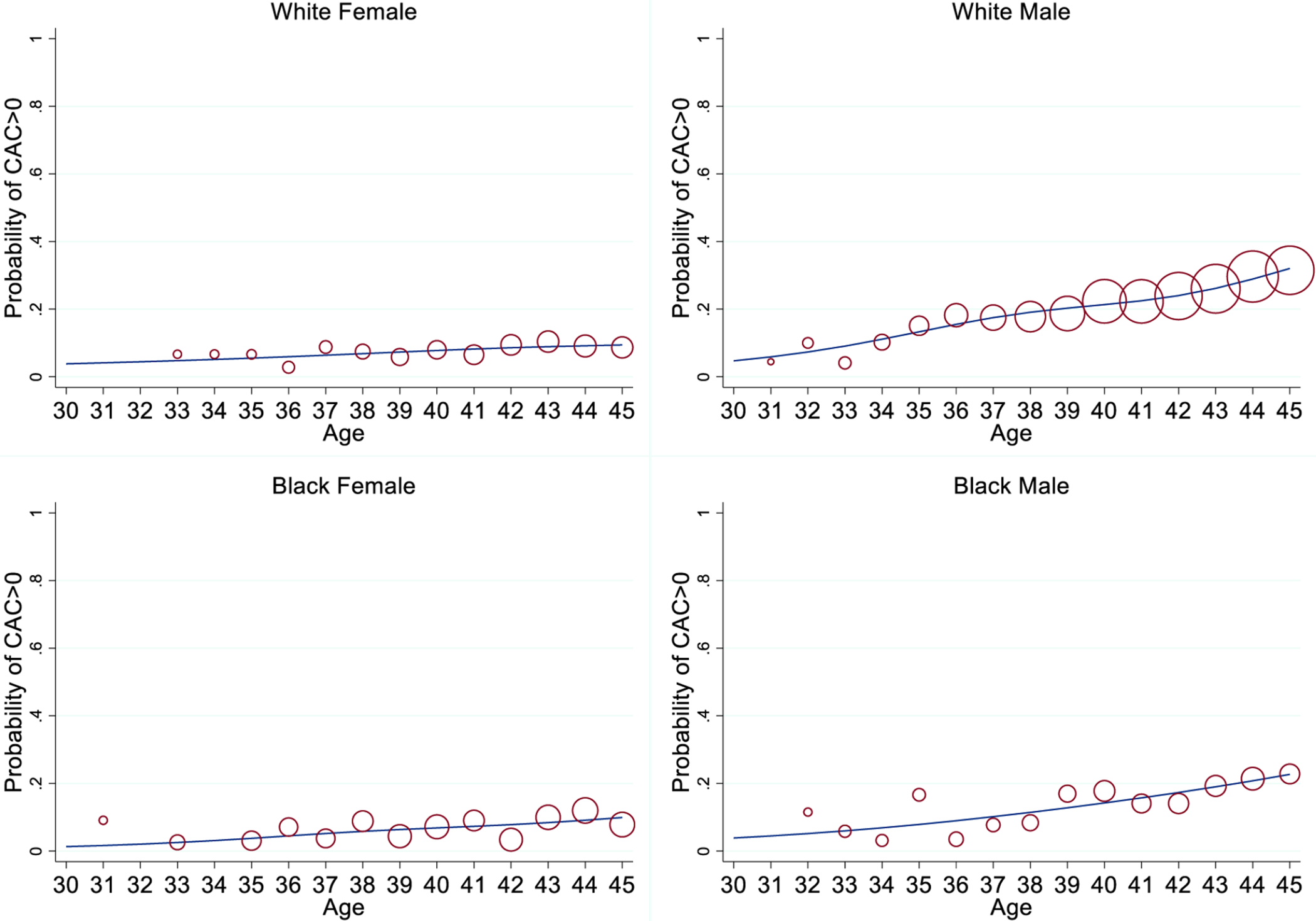
White females (top left), White males (top right), Black females (bottom left), and Black males (bottom right). Solid line represents a local regression smoother applied to the raw data. Individual points reflect the observed age-specific probability with larger point size indicating more subjects at that age.
Table 3 displays estimated CAC percentiles by age, sex, and race over one-year age increments. This table reflects the importance of considering self-identified race in addition to age and sex when interpreting CAC scores, as has been demonstrated in MESA.(6) Among individuals of the same age, men had higher percentile scores than women and White participants had higher percentiles than Black participants. Further distribution details may be obtained from the public webpage (Central Illustration), where an interactive form allows one to enter age (in years), sex, and race (for White and Black participants) to obtain a corresponding set of estimated percentiles for adults aged 30–45. The link is included in this reference.(16)
Table 3:
CAC Values Corresponding to Estimated Weighted Percentiles across Age, by Sex and Race Groups
| Age | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | 40 | 41 | 42 | 43 | 44 | 45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White Female | ||||||||||||||||
| 75th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 90th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 95th | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 2 | 2 | 3 | 4 | 5 | 8 | 10 | 12 | 12 |
| 97.5th | 4 | 5 | 7 | 7 | 8 | 10 | 10 | 11 | 12 | 15 | 21 | 27 | 37 | 47 | 64 | 76 |
| White Male | ||||||||||||||||
| 75th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | 5 |
| 90th | 0 | 0 | 0 | 0 | 1 | 3 | 5 | 8 | 11 | 15 | 18 | 21 | 26 | 32 | 43 | 55 |
| 95th | 0 | 1 | 4 | 9 | 15 | 21 | 29 | 35 | 41 | 47 | 53 | 59 | 72 | 83 | 105 | 131 |
| 97.5th | 2 | 9 | 18 | 29 | 40 | 55 | 68 | 80 | 96 | 100 | 111 | 125 | 146 | 166 | 190 | 249 |
| Black Female | ||||||||||||||||
| 75th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 90th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 95th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 5 | 8 | 9 | 11 | 13 | 12 |
| 97.5th | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 7 | 10 | 16 | 23 | 30 | 36 | 41 | 40 | 37 |
| Black Male | ||||||||||||||||
| 75th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 90th | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 5 | 7 | 9 | 12 | 22 | 36 |
| 95th | 0 | 0 | 1 | 2 | 3 | 4 | 6 | 10 | 14 | 17 | 26 | 33 | 42 | 54 | 85 | 138 |
| 97.5th | 5 | 9 | 5 | 8 | 12 | 16 | 24 | 35 | 42 | 47 | 64 | 82 | 96 | 119 | 175 | 277 |
Figure 2 shows the percentile curves for each combination of sex and race as a function of age. Each plot shows the estimated curves for the 75th, 90th, 95th, and 97.5th percentiles of CAC across age. As before, the individual circles represent the observed age-specific percentile, with circle size reflecting the available sample size at that age (larger circles indicate more subjects). Figure 3 compares the 90th and 95th percentiles by sex/race groups on the same plots.
Figure 2. Estimated weighted CAC percentiles by age for each sex/race group.
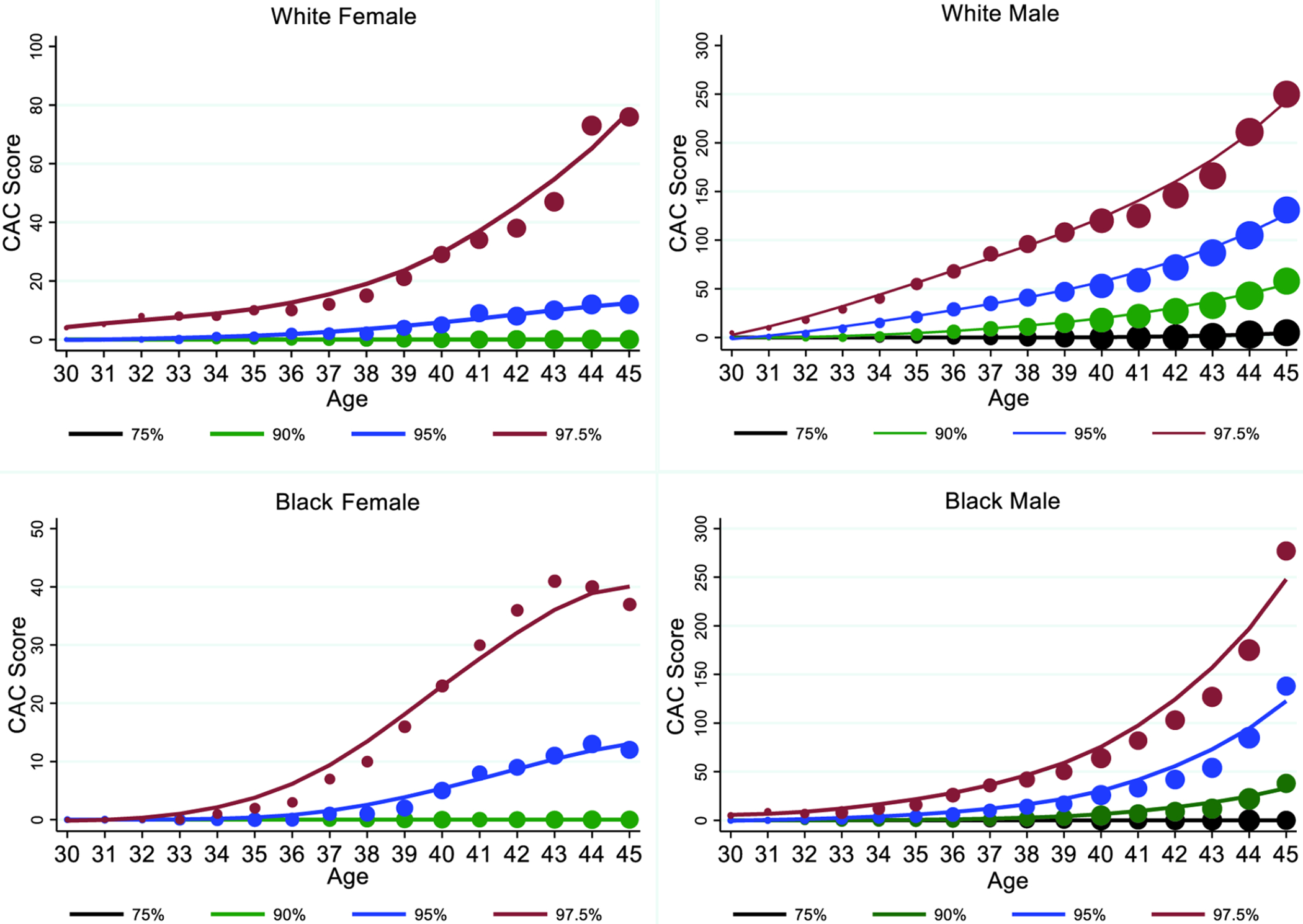
White females (top left), White males (top right), Black females (bottom left), and Black males (bottom right). Each plot shows the estimated curves for the 75th (black line), 90th (green line), 95th (blue line), and 97.5th (red line) percentiles of CAC across age. Individual points reflect the observed empirical percentiles for each age with larger point size indicating more subjects at that age within each graph.
Figure 3. Estimated weighted 90th and 95th CAC percentiles by age, sex, race.
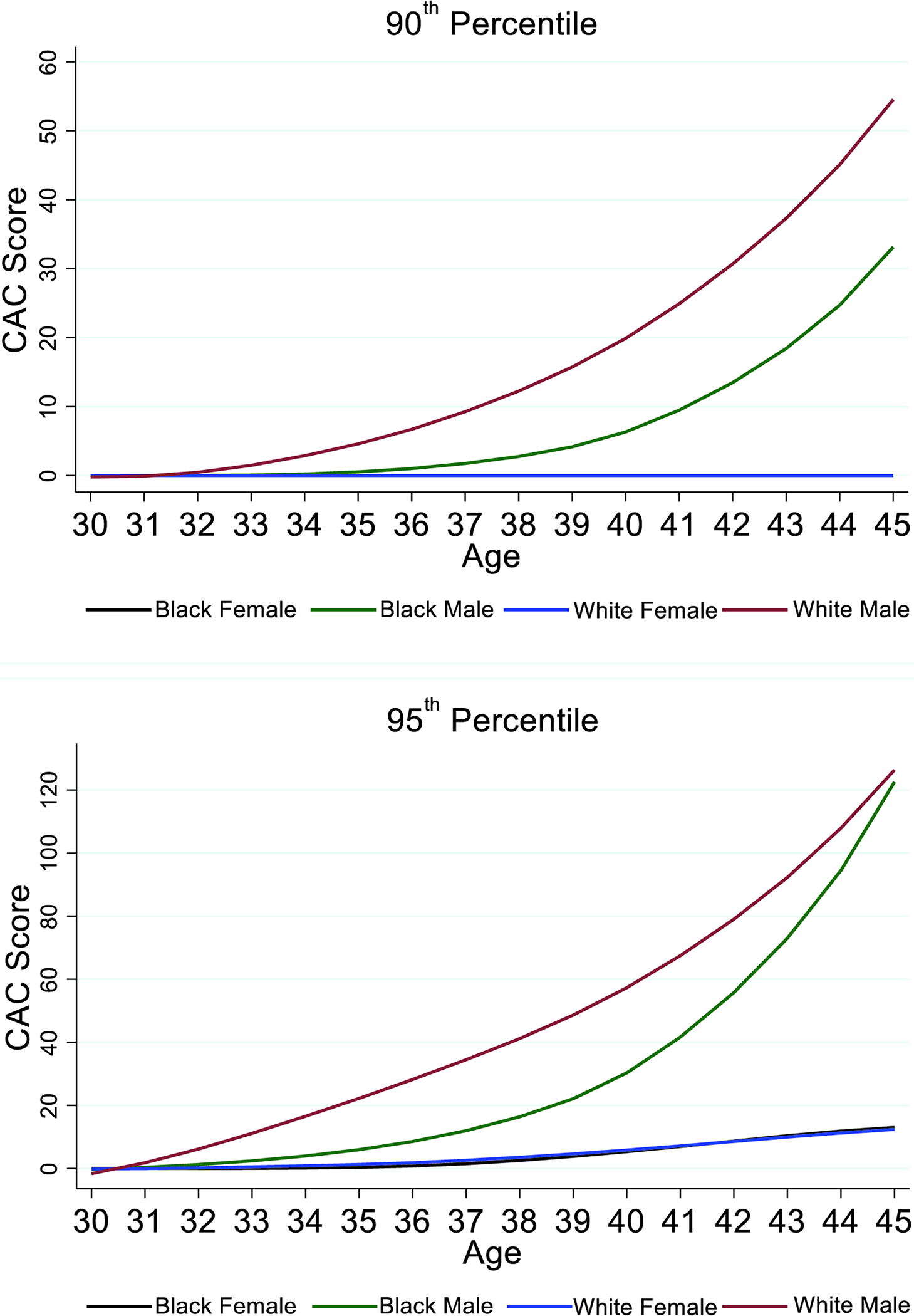
Please note the differing y-axis in each figure. Black females (black line), Black males (green line), White females (blue line), White males (red line).
DISCUSSION
Generalizability of Percentiles
We harmonized three datasets to perform the largest study on CAC in U.S. young adults to date (n=19,725). Our findings are supported by our pooled and weighted analysis, which comprised three large heterogeneous populations, including the only community-based population in this age range, CARDIA, which was 55% female and 47% Black.(14) The few other datasets containing CAC scans in adults <45 years of age that were not used were limited by much smaller samples sizes (17) or were highly selected referral-based cohorts with higher CAC prevalence than studies in similar populations.(18) Hence, to our knowledge, our study represents the majority of data on CAC in U.S. young adults,(19) with the potential downsides of using referral-based cohorts justified by the benefits of a much larger population and diversity in sampling sites creating the necessary statistical power for such an analysis.
The percentiles in this study were close but not identical to the percentiles derived from 6,110 patients aged 45–84 in MESA.(6) Like in MESA, we found that Black and female participants tended to have the lowest burden of CAC. We used a similar smoothing approach to prevent overfitting of the data, which may increase the generalizability and comparability of our findings. At age 45, where the present percentile estimates end and MESA estimates begin, our prevalence estimates of CAC >0 (9% for Black females, 9% for White females, 23% for Black males, 32% for White males) were similar to MESA (8% for Black females, 7% for White females, 19% for Black males, 25% for White males). The 90th percentile value for CAC at age 45 in MESA vs. the present study was 16 vs. 38 AU for Black males and 36 vs. 55 AU for White males, respectively. MESA also found the 75th percentile at age 45 was CAC = 0 for all groups, whereas we found it was CAC = 5 in White males. Compared to MESA, our study had far more total individuals (2,503 vs. 15,480 White and 1,613 vs. 3,328 Black), and more individuals aged 44–46 (129 vs. 4,249 White and 86 vs. 800 Black in MESA vs. the present study, respectively). (6)
The MESA eligibility criteria of being free of cardiovascular disease and diabetes, a major cardiovascular risk factor, may have had unintended consequences on their percentile estimates. For example, take the hypothetical case of a 35-year old White male with an elevated CAC score who went on to suffer a major cardiovascular event within 10 years, as has been reported in outcomes studies.(10,14,19) Because of the existence of overt cardiovascular disease, this individual and other higher-risk young adults like him would have been excluded from MESA and therefore not represented in the MESA percentiles. With only around 100 individuals represented at age 44–46 in MESA, exclusion of only a few such participants may have influenced the percentile estimates. This could partly explain why the same percentile at age 45 corresponds to somewhat lower CAC values in MESA than the present study. However, these minor differences likely have negligible clinical implications. For a 45-year old White male with a CAC score of 40, our percentile calculator places him at the 87th percentile while MESA places him at the 90th percentile. Even if a future guideline uses a percentile cutoff of 90 to recommend intensive preventive therapy, clinicians are still likely to interpret the 87th percentile as an alarm sign to engage in a risk-benefit patient-provider discussion. The similarity between the studies also suggests that the indications for scanning did not make a meaningful difference in the percentile estimates. Further work is needed to harmonize of our study with the MESA percentiles.
It is unclear how well percentile estimates represent the general population. The overall risk factor profile of our cohort was comparable to adults at mean age 44 from the National Health and Nutrition Examination Survey (NHANES) 1999–2016, with the exception of a higher prevalence of hyperlipidemia in our cohort and a lower prevalence of diabetes.(20,21) Our prevalence of smoking is similar to recent estimates of smoking in young adults.(22) The MESA-derived percentiles cohort, in contrast, had a higher prevalence of hypertension and importantly excluded participants with diabetes.(6) The CAC Consortium and Walter Reed populations also included individuals referred or self-referred for CAC scanning for clinical indications, whereas CARDIA and MESA did not. While referral cohorts may introduce a potential bias towards a higher burden of CAC than in the general population, NHLBI cohorts like CARDIA and MESA may have a reverse bias of being healthier than the general population.(23) Hence, our findings may have most applicability for the clinical population of Black and White individuals living in the United States rather than the general U.S. or international populations.(24)
Utility of Percentiles
Our study demonstrates that the yield of a CAC exam in young adults is generally higher in men than in women and in White than in Black individuals. Knowing the probability of detecting any CAC in this age group may aid the identification of cutoffs for targeted scanning of select young adult populations. While age and genetics are the dominant factors associated with development of atherosclerosis at a young age, multiple studies have also shown a higher prevalence of CAC with more ASCVD risk factors.(1,10,25) CARDIA, for example, found strong independent associations of CAC with age, male sex, White race (vs. Black), systolic blood pressure, low-density lipoprotein, cigarette smoking, blood glucose, and body-mass index.(11) There is rising interest to predict the conversion to CAC >0 in order to determine when an individual should have their first CAC exam. A recent analysis in the CAC Consortium found that, compared to those without risk factors, individuals with diabetes developed CAC 6.4 years earlier on average, while smoking, hypertension, dyslipidemia, and family history of coronary disease were independently associated with developing CAC 3.3–4.3 years earlier.(26) Additionally, polygenic risk scores have potential to identify high risk young adults for early CAC screening in the future.(27,28)
While the probability of detecting any CAC may help with determining who to scan and when, CAC percentile curves may guide how intensive to be with treatment. Percentile scores cannot necessarily be used to conclude a patient’s absolute risk, but they do provide context as to what constitutes a high CAC score in an individual relative to others of the same age, sex, and race (i.e. relative risk). In this sense, they assist with estimating lifetime risk trajectory, since most individuals’ CAC scores grow along their percentile curve in the absence of interventions that disrupt natural history.(29)
The 2019 ACC/AHA Primary Prevention Guidelines recommend CAC exams for individuals considering initiating statin therapy at borderline to intermediate risk, in whom risk is reclassified upwards with CAC ≥100 or age/sex/race percentile ≥ 75th for those <55 years old.(2) Although detection of any CAC in young patients will place them at higher percentiles by default (in fact, the 75th percentile for all subjects in our study was 0 except for White males approaching their mid 40s), percentile quantification may still offer useful opportunities for targeted preventive therapy and may assist in post-testing patient discussions related to relative burden of atherosclerosis and risk. The 2021 National Lipid Association recently recommended expanding the population of individuals eligible for CAC scanning to select adults <40 years with a family history of premature ASCVD or multiple ASCVD risk factors, in whom CAC>0 was used as a threshold for intensifying lifestyle therapy and possibly initiating statin therapy.(30) For females in this study, the presence of any CAC at ages 30–45 years automatically placed them at the ≥ 90th age-sex-race percentile and hence may suggest initiation of preventive therapies or lifestyle modifications to alter their ASCVD risk. In contrast, future guidelines for young adult males may emphasize more intensive treatment if, for example, one’s score places them at the ≥ 90th percentile. Raggi et al. initially showed that age-sex percentiles were more specific for predicting incident acute myocardial infarction than absolute CAC scores.(31) A later analysis of the MESA-derived age-sex-race percentiles concluded that, while absolute CAC score was a better predictor of short-term coronary heart disease events, age-sex-race percentiles may be especially helpful for interpretation of lifetime risk.(32) While it is unknown in this young age group how percentile scores correlate to short-term risk, they may prove to be strong indicators of lifetime atherogenic trajectory that help encourage adoption of heart-healthy lifestyle behaviors earlier in life, particularly among those with low absolute CAC that corresponds to a very high percentile score.
Limitations
As the aim of this study was to create CAC percentiles for young adults and place these into context of the existing literature, we did not explore the long-term clinical outcomes. Future investigations will explore the relationships of these percentiles with outcomes to help determine how they may guide preventive therapy or aid in determining the timing of a CAC exam for individuals <45 years old. We did not have enough data to calculate percentiles for Hispanic, East Asian, South Asian, Native American, or other racial/ethnic groups, although differences in the prevalence of CAC among these groups have been previously described.(6,33,34). In the context of important recent discussions on race in medical research, we demonstrate clear differences in the probability of CAC and estimated age-sex-race adjusted percentiles among self-reported White and Black individuals, suggesting that race offers useful, incremental knowledge compared to age and sex alone for interpretation of CAC scores relative to similar peers. Future calculators may be able to stratify individuals based on more objective genomic and transcriptomic markers, which will need to be integrated and reconciled with ethnic, socioeconomic and educational factors, currently thought as dominant in the epidemiology of cardiovascular diseases.(35) At present, the alternative of ignoring race and using tools derived from datasets with unequal representation may have predictable and undesirable consequences of over- or underestimating ASCVD risk in certain populations. Acknowledging these limitations, we advocate for additional research to increase diversity, representation, and equality in subclinical atherosclerosis research both within the United States and abroad.
Future Directions
Our study marks an important step towards understanding the prevalence and natural progression of CAC across the entire adult lifespan. Creation of a CAC percentile calculator for all ages using a synthetic cohort (for example, our study + MESA + Atherosclerosis Risk in Communities (ARIC) to reflect those age >75), with appropriate representation of racial and ethnic subgroups, and a single webpage housing all CAC tools would help unify efforts for utilization of CAC as one of the most powerful risk assessment tools for ASCVD primary prevention.(36) Existing and future age-sex-race percentiles may be considered for incorporation into future prevention guidelines, Society of Cardiovascular Computed Tomography reporting guidelines,(37) and inclusion in all CAC score reports.
CONCLUSIONS
We provide the first calculator of age, sex, and race-based CAC percentiles for ages 30–45, derived from the largest study population of CAC among US young adults to date, to fill an important knowledge gap for clinical practice. While any CAC in this age group is abnormal, CAC percentiles provide a method to interpret how high a CAC score is in an individual relative to his or her age-sex-race matched peers. Our results lay the groundwork for the development of future guidelines for targeted measurement, re-classification of long-term risk, and potential recommendations for intensive preventive therapy among select young adults.
Supplementary Material
PERSPECTIVES.
Competency in Patient Care and Procedural Skills:
Any degree of coronary artery calcification (CAC) detected by CT imaging places women between the ages of 30 and 45 years above the 90th percentile of cardiovascular risk. Men reach the 90th percentile when CAC is detected at age 34 years for White and 37 years for Black individuals.
Translational Outlook:
A CAC percentile calculator based on cohorts representing racial and ethnic subgroups at all ages could enhance utilization of this powerful risk assessment tool.
Acknowledgments:
This manuscript has been reviewed by CARDIA for scientific content. The online calculator (www.cac-tools.com) was created by Rehan Javaid, University of Virginia School of Engineering Class of 2023.
Funding:
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I & HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). The Coronary Artery Calcium Consortium was supported by grant L30 HL110027.
Abbreviations:
- ASCVD
atherosclerotic cardiovascular diseases
- CVD
cardiovascular disease
- CAC
coronary artery calcification
- MESA
Multi-Ethnic Study of Atherosclerosis
- CARDIA
Coronary Artery Risk Development in Young Adults
- NHLBI
National Heart Lung and Blood Institute
- LOWESS
local weighted estimated scatterplot smoothing
- ARIC
Atherosclerosis Risk in Communities
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None
REFERENCES
- 1.Mitchell JD, Paisley R, Moon P, Novak E, Villines TC. Coronary Artery Calcium and Long-Term Risk of Death, Myocardial Infarction, and Stroke: The Walter Reed Cohort Study. JACC Cardiovasc Imaging 2018;11:1799–1806. [DOI] [PubMed] [Google Scholar]
- 2.Arnett DK, Blumenthal RS, Albert MA et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh A, Collins BL, Gupta A et al. Cardiovascular Risk and Statin Eligibility of Young Adults After an MI: Partners YOUNG-MI Registry. J Am Coll Cardiol 2018;71:292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dzaye O, Dudum R, Reiter-Brennan C et al. Coronary artery calcium scoring for individualized cardiovascular risk estimation in important patient subpopulations after the 2019 AHA/ACC primary prevention guidelines. Prog Cardiovasc Dis 2019;62:423–430. [DOI] [PubMed] [Google Scholar]
- 5.Saad M, Pothineni NV, Thomas J et al. Coronary Artery Calcium Scoring in Young Adults: Evidence and Challenges. Curr Cardiol Rep 2018;20:10. [DOI] [PubMed] [Google Scholar]
- 6.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2006;113:30–7. [DOI] [PubMed] [Google Scholar]
- 7.Blaha MJ, Whelton SP, Al Rifai M et al. Rationale and design of the coronary artery calcium consortium: A multicenter cohort study. J Cardiovasc Comput Tomogra 2017;11:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedman GD, Cutter GR, Donahue RP et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–16. [DOI] [PubMed] [Google Scholar]
- 9.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. [DOI] [PubMed] [Google Scholar]
- 10.Miedema MD, Dardari ZA, Nasir K et al. Association of Coronary Artery Calcium With Long-term, Cause-Specific Mortality Among Young Adults. JAMA Netw Open 2019;2:e197440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loria CM, Liu K, Lewis CE et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol 2007;49:2013–20. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell JD, Fergestrom N, Gage BF et al. Impact of Statins on Cardiovascular Outcomes Following Coronary Artery Calcium Scoring. J Am Coll Cardiol 2018;72:3233–3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mao SS, Pal RS, McKay CR et al. Comparison of coronary artery calcium scores between electron beam computed tomography and 64-multidetector computed tomographic scanner. J Comput Assist Tomogr 2009;33:175–8. [DOI] [PubMed] [Google Scholar]
- 14.Carr JJ, Jacobs DR Jr., Terry JG et al. Association of Coronary Artery Calcium in Adults Aged 32 to 46 Years With Incident Coronary Heart Disease and Death. JAMA Cardiol 2017;2:391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cleveland WS. Robust Locally Weighted Regression and Smoothing Scatterplots. J Am Stat Assoc 1979;74:829–836. [Google Scholar]
- 16.CAC Percentile Calculator. Available at: www.cac-tools.com. 2022.
- 17.Paixao Andre RM, Ayers Colby R, Rohatgi A et al. Cardiovascular Lifetime Risk Predicts Incidence of Coronary Calcification in Individuals With Low Short‐Term Risk: The Dallas Heart Study. J Am Heart Assoc 2014;3:e001280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tota-Maharaj R, Blaha MJ, McEvoy JW et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J 2012;33:2955–2962. [DOI] [PubMed] [Google Scholar]
- 19.Javaid A, Mitchell JD, Villines TC. Predictors of Coronary Artery Calcium and Long-Term Risks of Death, Myocardial Infarction, and Stroke in Young Adults. J Am Heart Assoc 2021;10:e022513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krittanawong C, Kumar A, Wang Z et al. Coronary artery disease in the young in the US population-based cohort. Am J Cardiovasc Dis 2020;10:189–194. [PMC free article] [PubMed] [Google Scholar]
- 21.Egan BM, Li J, Sutherland SE et al. Sociodemographic Determinants of Life’s Simple 7: Implications for Achieving Cardiovascular Health and Health Equity Goals. Ethn Dis 2020;30:637–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults—United States, 2019. MMWR Recomm Rep 2020;69:1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark AL, Lammiman MJ, Goode K, Cleland JGF. Is taking part in clinical trials good for your health? A cohort study. Eur J Heart Fail 2009;11:1078–1083. [DOI] [PubMed] [Google Scholar]
- 24.Pereira AC, Gomez LM, Bittencourt MS et al. Age, Gender, and Race-Based Coronary Artery Calcium Score Percentiles in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Clin Cardiol 2016;39:352–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bild DE, Folsom AR, Lowe LP et al. Prevalence and correlates of coronary calcification in black and white young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arterioscler Thromb Vasc Biol 2001;21:852–7. [DOI] [PubMed] [Google Scholar]
- 26.Dzaye O, Razavi AC, Dardari ZA et al. Modeling the Recommended Age for Initiating Coronary Artery Calcium Testing Among At-Risk Young Adults. J Am Coll Cardiol 2021;78:1573–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Severance LM, Carter H, Contijoch FJ, McVeigh ER. Targeted Coronary Artery Calcium Screening in High-Risk Younger Individuals Using Consumer Genetic Screening Results. JACC Cardiovasc Imaging 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blaha MJ. Predicting Age of Conversion to CAC >0: A Role for Polygenic Risk Scores? JACC Cardiovasc Imaging 2021. [DOI] [PubMed] [Google Scholar]
- 29.Erbel R, Lehmann N, Churzidse S et al. Progression of coronary artery calcification seems to be inevitable, but predictable - results of the Heinz Nixdorf Recall (HNR) study. Eur Heart J 2014;35:2960–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orringer CE, Blaha MJ, Blankstein R et al. The National Lipid Association scientific statement on coronary artery calcium scoring to guide preventive strategies for ASCVD risk reduction. J Clin Lipidol 2021;15:33–60. [DOI] [PubMed] [Google Scholar]
- 31.Raggi P, Callister TQ, Cooil B et al. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation 2000;101:850–5. [DOI] [PubMed] [Google Scholar]
- 32.Budoff MJ, Nasir K, McClelland RL et al. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2009;53:345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mehta A, Patel J, Al Rifai M et al. Inflammation and coronary artery calcification in South Asians: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis 2018;270:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gooding HC, Gidding SS, Moran AE et al. Challenges and Opportunities for the Prevention and Treatment of Cardiovascular Disease Among Young Adults: Report From a National Heart, Lung, and Blood Institute Working Group. J Am Heart Assoc 2020;9:e016115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schultz WM, Kelli HM, Lisko JC et al. Socioeconomic Status and Cardiovascular Outcomes. Circulation 2018;137:2166–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol 2018;72:434–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hecht HS, Blaha MJ, Kazerooni EA et al. CAC-DRS: Coronary Artery Calcium Data and Reporting System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT). J Cardiovasc Comput Tomogra 2018;12:185–191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


