Abstract
With the ongoing spread of COVID-19, vaccination stands as an effective measure to control and mitigate the impact of the disease. However, due to the unequal distribution of COVID-19 vaccination sites, people can have different levels of spatial accessibility to COVID-19 vaccination. This study adopts an improved gravity-based model to measure the racial/ethnic inequity in transit-based spatial accessibility to COVID-19 vaccination sites in the Chicago Metropolitan Area. The results show that Black-majority and Hispanic-majority neighborhoods have significantly lower transit-based spatial accessibility to COVID-19 vaccination sites compared to White-majority neighborhoods. This research concludes that minority-dominated inner-city neighborhoods, despite better public transit coverage, are still disadvantaged in terms of transit-based spatial accessibility to COVID-19 vaccination sites. This is probably due to their higher population densities, which increase the competition for the limited supply of COVID-19 vaccination sites within each catchment area.
Introduction
Vaccination has been shown to be highly effective in containing the spread of coronavirus disease 2019 (COVID-19). However, due to the spatial distribution inequity of vaccination sites, different population groups can have various levels of spatial accessibility to vaccination sites. A better understanding of the inequity in the spatial accessibility of vaccination sites can help policymakers make adjustments to improve the equity of vaccination site distribution.
Meanwhile, the impact of COVID-19 has also been felt differently by different racial/ethnic groups due to disparities in the socioeconomic determinants of health such as employment, housing, and healthcare [1–4]. Therefore, in light of the proven effectiveness of COVID-19 in reducing the infection and mortality rate [5–7], it is even more important to minimize the inequity faced by the racial/ethnic minority population in accessing vaccination sites in order to protect themselves from COVID-19. Nevertheless, due to the uneven distribution of COVID-19 vaccination resources, there are inequities in vaccination accessibility among different nations and regions as suggested by recent studies [8, 9]. However, little is known to date regarding the inequities in accessing COVID-19 vaccination sites across different races and ethnicities at the local level.
Although the USA is known to be a car-dependent country, a significant portion of its urban population, especially the racial/ethnic minorities, live in carless households and rely on public transit for traveling to different activity sites such as healthcare, employment, and grocery. Therefore, in light of the ongoing COVID-19 vaccination efforts in the USA, we need to better understand transit-based accessibility to COVID-19 vaccination sites and racial/ethnic inequity associated with the COVID-19 vaccination accessibility at the local level in order to improve the accessibility of vaccination to racial/ethnic minorities and protect them from the disproportionate impact from COVID-19.
Since the first COVID-19 case was confirmed in the USA on January 20, 2020, the number of cases in the nation has grown exponentially [10]. As of early November 2021, the USA has accumulated more than 46 million COVID-19 cases and 746,000 deaths [11]. Despite the wide-ranging impact of the COVID-19 pandemic, the extent of impact varies across different population groups, with racial/ethnic minority populations being more fatally affected [1]. Specifically, Luck (2022) discovered that the mortality rate for the White population in the USA was 76 deaths per million, which was much lower than that of the Black population which had a mortality of 211 deaths per million [4]. Kim and Bostwick (2020) revealed that 62.8% of all COVID-19-associated deaths in Chicago were Black people, which were spatially concentrated in Black-majority neighborhoods in the southern and western parts of Chicago [12]. Gross et al. (2020) uncovered that the COVID-19-associated death risk was 18-fold higher among the Black population than the White population in Wisconsin, while the Hispanic population had an 88% higher death risk than White patients [13]. Therefore, the racial/ethnic minority population have been shown to be more vulnerable to the mortal impact of COVID-19. In the meantime, vaccination has been shown to be very effective in reducing the probability of severe illness and death from COVID-19 [6, 7]. Specifically, Polack et al. (2020) found that a two-dose regimen of BNT162b2 mRNA Covid-19 Vaccine developed by Pfizer-BioNTech was 95% effective in preventing COVID-19 for individuals 16 years old or above [6]. Voysey et al. (2021) revealed that ChAdOx1 nCoV-19 vaccine developed by AstraZeneca-University of Oxford was 62.1% effective in preventing COVID-19 when administered in two standard doses, and 90.0% effective in preventing COVID-19 when administered in a low dose followed by a standard dose. Many COVID-19 vaccines such as the abovementioned ones developed by Pfizer-BioNTech and AstraZeneca-University of Oxford require two doses of vaccine in order to achieve a lasting maximal level of protection and for recipients to be considered fully vaccinated [6, 14, 15]. Further, subsequent vaccine booster shots have been recommended and implemented by the health authorities in countries such as Israel and the USA in order to compensate for the waning vaccine effectiveness [16, 17]. Therefore, constant and good access to COVID-19 vaccination is key to combating COVID-19 and protecting people from hospitalization and death.
Nevertheless, just like many other socioeconomic resources such as employment [18], grocery [19], and recreation [20], studies have also found inequity in the distribution of vaccination resources [21]. Past studies have found that better spatial accessibility to vaccination resources/services is associated with higher vaccination rates [22, 23]. Specifically, Fu et al. (2009) found that children in Washington DC with the highest level of spatial access to pediatric vaccination providers have a 36% higher likelihood of being up-to-date in terms of vaccination than children with the lowest level of spatial access to pediatric vaccination providers [22]. Further, Whitehead et al. (2022) revealed a strong and significant positive association between the average spatial accessibility to vaccination services and the vaccination rate of the Māori population in Aotearoa New Zealand, based on District Health Boards data [23]. Given the importance of good spatial access to vaccination providers in improving vaccination rates, many recent studies have tried to reveal the inequity in spatial accessibility to COVID-19 vaccination. However, most of these studies on COVID-19 vaccination distribution inequity only focus on highlighting the inequity among different countries, especially between the higher-income and lower-income countries [8, 9]. In comparison, insufficient attention has been directed towards revealing the inequity faced by the socially vulnerable population (e.g., racial/ethnic minorities) at the local level. This is because the socially vulnerable population such as the racial/ethnic minority population tend to be disadvantaged in accessing various socioeconomic resources such as healthcare and they should be on equal footing, if not prioritized, in accessing COVID-19 vaccination with the White population since racial/ethnic minority populations have been shown to suffer from higher COVID-19 mortality rate.
Besides the barrier of spatial accessibility, the long-standing racism and discrimination along with historic scandals such as the Tuskegee Experiment have led to a distrust of the healthcare system and vaccine hesitancy among the racial/ethnic minorities, especially the Black communities, in the USA, which have resulted in low vaccine willingness and COVID-19 vaccination rate among the racial/ethnic minority population [24, 25]. As a consequence, inequities faced by the racial/ethnic minorities in spatial accessibility to COVID-19 vaccination sites, in combination with the already low vaccination willingness among them, can further reduce the effectiveness of the efforts to increase the COVID-19 vaccination rate. A low COVID-19 vaccination rate can in turn further exacerbate the COVID-19 incidence and mortality rate among the racial/ethnic minorities. Therefore, understanding and reducing the inequity in the spatial access to COVID-19 vaccination sites across racial/ethnic groups at the local level serves as the foundation for bridging the vaccination rate gap, which helps improve the protection against COVID-19 for the racial/ethnic minorities.
Therefore, this study aims at revealing the inequity in the spatial accessibility to COVID-19 vaccination sites for the racial/ethnic minority population. Moreover, as the racial/ethnic minority populations are more likely to reside in carless households and more dependent on public transit for accessing socioeconomic opportunities [26, 27], we particularly concentrate on revealing the racial/ethnic inequity in transit-based spatial accessibility to COVID-19 vaccination sites. Spatial accessibility in our study is defined as the ease of reaching COVID-19 vaccination sites using public transit. The spatial accessibility measure adopted in our study is an improved gravity-based model that accounts for not only the demand for and supply of vaccination sites but also the inflation effect of supply and demand.
Data and Methodology
Data Source
We obtained the data for the study mainly from three different sources. First, the census trace-level sociodemographic data, which include the population, race/ethnicity, and median household income information, were obtained from the 2018 American Community Survey (ACS) [28]. The vaccination site data by GISCorps was acquired from the ArcGIS Hub [29]. A vaccination site for our study refers to any location providing COVID-19 vaccine and the vaccination sites in the study area include pharmacies (e.g., CVS, Walgreens), clinics (including mobile clinics), public health departments, and all other non-medical facilities (e.g., parking lots, gymnasiums, and community centers). The transit-based travel time was obtained through the Google Maps Directions API [30], which provides real-time transit-based travel time that accounts for ingress/egress, transfer, and onboard time.
Study Area
We chose the Chicago Metropolitan Area as the study area, which includes seven counties (i.e., Cook, DuPage, Kane, Kendall, Lake, McHenry, and Will) in northeastern Illinois according to the definition of the Chicago Metropolitan Agency for Planning. The metropolitan area has the second-largest public transit system in the USA that includes both bus and train services.
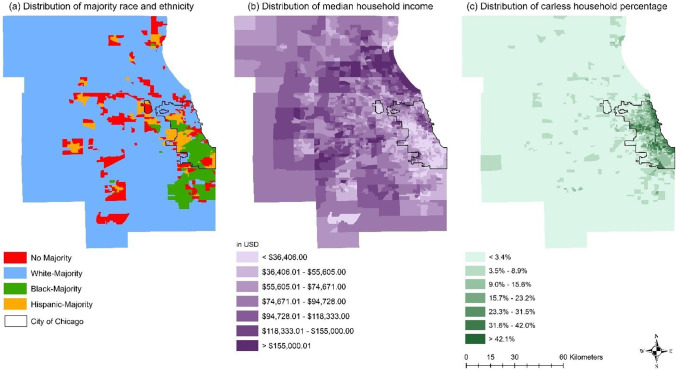
The region has been known to have a high level of economic and residential segregation with most of the racial/ethnic minority population being largely confined within or near the inner city (i.e., the City of Chicago) as shown in Fig. 1.
Fig. 1.
Distribution of (a) majority race and ethnicity; (b) median household income; and (c) carless household percentage
As shown in Fig. 1(a), the study area shows a clear residential segregation pattern with most racial/ethnic minority neighborhoods being concentrated within the inner city or in the proximity of the inner city. In this research, we determined the majority race/ethnicity of each census tract as follows. If over 50% of a census tract’s population is White, we then considered this census tract as a White-majority census tract. The same goes for Black or Hispanic-majority census tracts. For census tracts with no one race/ethnicity exceeding 50% of the census tract’s population, we considered them as no-majority census tracts. To avoid double-counting, the White and Black populations in our study were non-Hispanic White and Black populations.
Figure 1(b) further illustrates that minority-dominated neighborhoods tend to have lower median household income, while Fig. 1(c) indicates that most neighborhoods with high carless household percentages are clustered within the inner city.
To better demonstrate the inequity in car ownership and income in the study area, we produced Table 1 to show the median metrics of carless household percentage and median household income by majority race/ethnicity for all the census tracts in the study area.
Table 1.
Median carless household percentage and household income by majority race and ethnicity
| Majority race and ethnicity | Median carless household percentage | Median household income |
|---|---|---|
| No majority | 4.3% | $57,525 |
| White-majority | 1.3% | $91,010 |
| Black-majority | 14.9% | $34,088 |
| Hispanic-majority | 4.9% | $47,955 |
As shown in Table 1, the median percentage of carless households in Black-majority neighborhoods (i.e., census tracts) far exceeds the White-majority and Hispanic-majority neighborhoods, while the median percentage of carless households in Hispanic-majority neighborhoods is substantially higher than that of the White-majority neighborhoods. Meanwhile, the median household income for White-majority neighborhoods is far higher than those of the Black-majority and Hispanic-majority neighborhoods. Therefore, both Fig. 1 and Table 1 corroborate the residential and economic segregation in the study area.
Besides, the study area is serviced by three major public transit operators overseen by the Regional Transportation Authority, which includes the Chicago Transit Authority (CTA), Metra, and Pace.
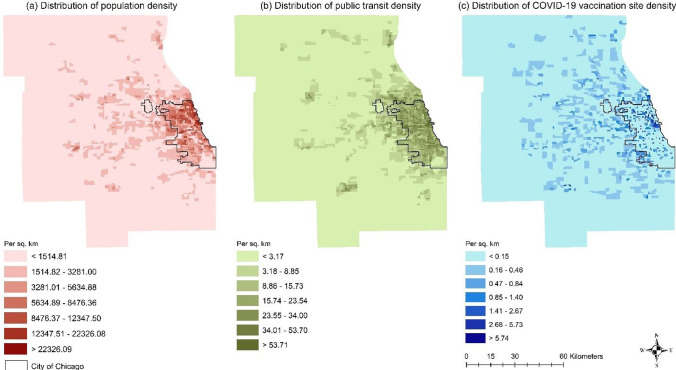
As shown by Fig. 2(a, b), most of the densely populated neighborhoods are within or close to the inner city, which largely overlaps neighborhoods with a high density of public transit. Nevertheless, the distribution of COVID-19 vaccination sites presents a more complex picture. Neighborhoods with high vaccination site density appear to spread around the entire study area except for its periphery.
Fig. 2.
Distribution of the (a) population density; (b) public transit density; and (c) COVID-19 vaccination site density
Methodology
We adopted an improved gravity-based measure accounting for not only the supply of and demand for vaccines but also the inflation effect, which refers to the inflation of supply and demand due to the aggregation of population and level of service [31]. Specifically, we calculated transit-based spatial accessibility to vaccination sites at the census tract level based on Eqs. (1)–(2).
| 1 |
where Ci is the transit-based potential demand for COVID-19 vaccination at census tract i; me is the population of census tract e whose centroid falls within the catchment (i.e., tei ≤ t0); tei is the transit-based travel time between census tract e and census tract i; t0 is the threshold transit-based travel time and its value is set at 50 min; tei is the transit-based travel time between census tract e and census tract i; β is the impedance function parameter and its value is set at 0.15. The values of t0 and β were set based on previous healthcare spatial accessibility studies for the same study area [32, 33].
| 2 |
where TAj is the transit-based spatial accessibility to COVID-19 vaccination site at census tract j; hi is the number of vaccination sites in census tract i whose centroid falls within the catchment (i.e., tij ≤ t0); tij is the transit-based travel time between census tract i and census tract j; t0 is the threshold transit-based travel time and its value is set at 50 min like above; β is the impedance function parameter and its value was set at 0.15 like above. Moreover, to test how different values of t0 and β affect the spatial accessibility results, we also performed a sensitivity analysis. The differences in the spatial accessibility results obtained with different t0 and β values are within 3.5%, which indicates that different t0 and β values have no significant effect on the spatial accessibility results.
Our COVID-19 vaccination transit-based spatial accessibility measure discounted the supply of COVID-19 vaccination sites by the demand of the population and impedance of transit-based travel time within the threshold while accounting for the inflation effect.
Results
Based on the methodology described above, we measured the distribution of transit-based spatial accessibility to vaccination sites at the census tract level and obtain the results as shown in Fig. 3.
Fig. 3.
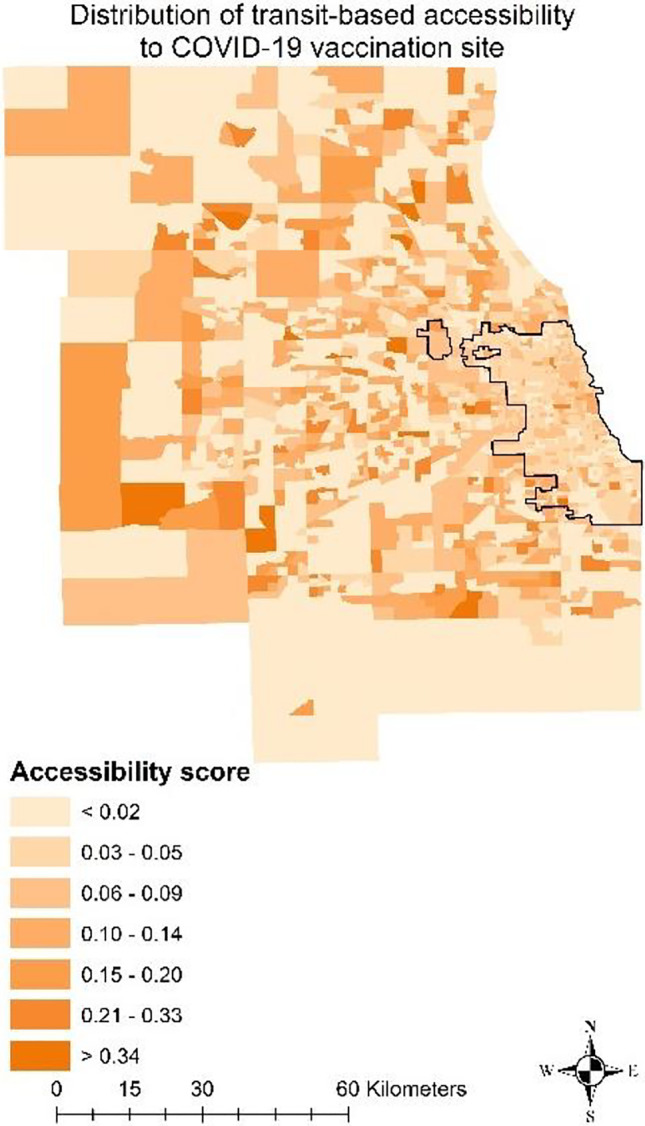
Distribution of transit-based spatial accessibility to COVID-19 vaccination sites
As shown in Fig. 3, neighborhoods within the inner city generally have lower transit-based spatial accessibility compared to those outside the inner city. Despite having relatively low transit density as shown in Fig. 2(b), many suburban neighborhoods actually enjoy good transit-based spatial accessibility to COVID-19 vaccination sites. This could be explained by the relatively low population density in the suburban area, which means less competition for the supply of COVID-19 vaccination sites. To further illustrate the racial/ethnic inequity in transit-based spatial accessibility to COVID-19 vaccination sites, we produced Fig. 4.
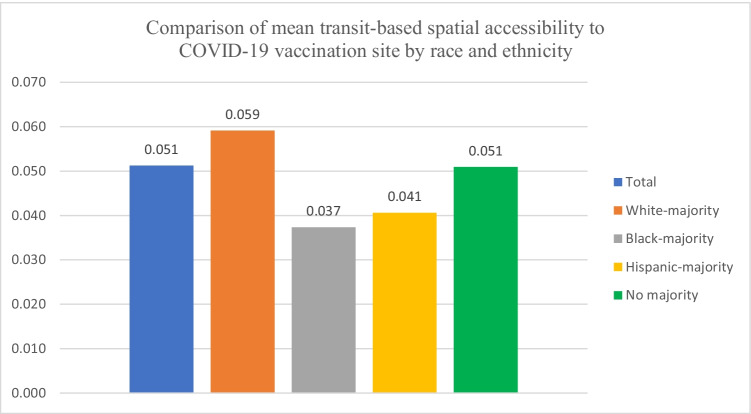
Fig. 4.
Comparison of mean transit-based spatial accessibility to COVID-19 vaccination site by race and ethnicity
As illustrated in Fig. 4, by using the mean transit-based spatial accessibility score (i.e., 0.051) of all census tracts within the study area as the benchmark, it can be seen that the transit-based spatial accessibility scores of Black-majority (0.037) and Hispanic-majority (0.041) census tracts are 27.45% and 19.61% lower than the benchmark. In comparison, the transit-based spatial accessibility score for the White-majority census tracts is 15.69% higher than the benchmark. For census tracts with no majority race/ethnicity, their mean transit-based spatial accessibility score is on par with the benchmark. This shows that the minority-dominated census tracts generally have much lower transit-based spatial accessibility to COVID-19 vaccination sites than the White-majority census tracts.
To better understand the distribution patterns of the transit-based spatial accessibility scores across the four racial/ethnic groups, we calculated and examined the descriptive statistics, which are shown in Table 2.
Table 2.
Descriptive statistics of the transit-based spatial accessibility scores across different racial/ethnic groups
| No majority | White-majority | Black-majority | Hispanic-majority | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Statistic | Std. error | Statistic | Std. error | Statistic | Std. error | Statistic | Std. error | ||
| Mean | 0.051 | 0.003 | 0.059 | 0.002 | 0.037 | 0.002 | 0.041 | 0.002 | |
| 95% confidence interval for mean | Lower bound | 0.045 | 0.055 | 0.033 | 0.036 | ||||
| Upper bound | 0.057 | 0.064 | 0.042 | 0.045 | |||||
| 5% trimmed mean | 0.044 | 0.050 | 0.032 | 0.036 | |||||
| Median | 0.034 | 0.037 | 0.027 | 0.031 | |||||
| Variance | 0.003 | 0.005 | 0.002 | 0.002 | |||||
| Std. deviation | 0.055 | 0.074 | 0.042 | 0.039 | |||||
| Minimum | 0.000 | 0.000 | 0.000 | 0.000 | |||||
| Maximum | 0.279 | 1.000 | 0.413 | 0.304 | |||||
| Range | 0.279 | 1.000 | 0.413 | 0.304 | |||||
| Interquartile range | 0.059 | 0.076 | 0.027 | 0.031 | |||||
| Skewness | 1.929 | 0.143 | 3.620 | 0.076 | 4.478 | 0.128 | 3.099 | 0.144 | |
| Kurtosis | 4.103 | 0.285 | 28.971 | 0.151 | 30.179 | 0.255 | 15.223 | 0.288 | |
As shown in Table 2, the skewness values for all four racial/ethnic groups are much large than 1, which indicates that the distributions of the accessibility scores are highly skewed. Since the skewness values are all positive, they indicate that the accessibility scores for all four racial/ethnic groups are clustered in the lower end.
Afterward, we proceeded to test whether the mean differences across different racial/ethnic groups are statistically significant using the Kruskal–Wallis test. We adopted the Kruskal–Wallis test because the accessibility scores for the four racial/ethnic groups are highly skewed instead of being normally distributed as indicated in Table 2. The P-value obtained through the Kruskal–Wallis test is 0.009, which is much lower than the significance level of 0.05 and indicates that the mean differences across different racial/ethnic groups are statistically significant.
In summary, although the inner city where racial/ethnic minorities concentrate tends to have better coverage of public transit, it also has a higher population density. The higher population density can lead to more intense competition for the supply of COVID-19 vaccination sites among the people within the catchment area and decreases the overall transit-based spatial accessibility to COVID-19 vaccination sites. Moreover, despite the lower population density in the suburb, many suburban census tracts have a high density of COVID-19 vaccination sites. In other words, lower population density means lower demand, while higher COVID-19 vaccination site density represents higher supply, which tips the supply and demand balance in favor of the suburban residents that are overwhelmingly White.
Discussion and Conclusion
This study aims at measuring the racial/ethnic inequity in transit-based spatial accessibility to COVID-19 vaccination sites at the local metropolitan level. The results show that the minority-dominated (i.e., Black-majority and Hispanic-majority) census tracts have significantly lower transit-based spatial accessibility compared to the White-majority census tracts as well as census tracts with no majority race/ethnicity. In addition, our findings also align well with those from other studies regarding transit-based spatial accessibility to healthcare resources/services [34–36]. For instance, Palm et al. (2021) recently found that transit riders from socially disadvantaged groups including the non-White, low-income, physically disabled, and carless had a higher likelihood of deferring medical care during COVID-19 than other transit riders in Toronto and Vancouver [34]. Sharma and Patil (2021) revealed greater spatial inequity for the slum population than the non-slum population in Greater Mumbai in accessing government hospitals by public transit [35]. Du et al. (2020) discovered that subdistricts in Beijing with higher proportions of the population with low educational attainment (high school or below) are concentrated in the urban peripheries with transit-based trips to hospitals lasting over 60 min, which is significantly longer than the urban subdistricts where the population tends to have higher educational attainment [36]. Overall, our study results along with the findings from other studies indicate that the socially marginalized population such as the racial/ethnic minorities, low-income, low-education, and physically disabled are commonly disadvantaged in transit-based spatial accessibility to healthcare resources/services like hospital and vaccination sites.
Despite living in inner-city neighborhoods with better public transit coverage, racial/ethnic minority residents could have lower transit-based spatial accessibility to vaccination sites due to more competition for the supply of COVID-19 vaccination sites from the overall higher population density in the inner city. Therefore, policymakers should make adjustments to the COVID-19 vaccination strategy in order to improve transit-based spatial accessibility to vaccination for racial/ethnic minority residents.
The first recommendation is to set up mobile walk-in vaccination clinics within or close to major transit stations or bus stops. Many existing ad hoc COVID-19 vaccination sites have been reported to be located in car-centric places such as drive-through clinics or parking lots, which cater to the driving population without giving much consideration to the carless population [37, 38]. Therefore, policymakers should make adjustments to the reality that many racial/ethnic minority residents are carless and depend on public transit and mobile vaccination clinics near transit can improve their access to vaccination.
Moreover, given the high population density in the inner city, more vaccination sites should be opened within inner-city neighborhoods, especially the minority-dominated neighborhoods in the south and west of the inner city, in order to reduce the competition for the supply of vaccination sites.
This study specifically focuses on revealing the inequity in the distribution of transit-based spatial accessibility to COVID-19 vaccination sites across different racial/ethnic groups, which is a key factor affecting the vaccination rate. Nevertheless, we recognize that the spatial accessibility to vaccination sites is not the sole factor affecting the vaccination rate. Good spatial accessibility to vaccination alone may not necessarily lead to high vaccination rates, especially among some racial/ethnic minority groups because of various non-spatial reasons including distrust of vaccination due to historic scandals targeting racial/ethnic minority groups such as the Tuskegee Experiment [24, 25, 39]. Therefore, besides improving the spatial access to COVID-19 vaccines, local governments should also put more resources into the promotion, education, and communication about COVID-19 vaccine information among racial/ethnic minority communities, while also tackling disinformation about COVID-19 vaccination. Specifically, the government should not only convey clear, transparent and easily understood information (e.g., benefits and potential allergic reactions or side effects) about COVID-19 vaccines to the local racial/ethnic minority communities through various channels such as community centers and social media, but also acknowledge the rightful and legitimate concerns and mistrust about vaccination due to systemic racism and discrimination.
Finally, we acknowledge that there are some limitations to our research. First of all, by using aggregate data for this research, we assumed that residents living in the same census tract have the same socioeconomic status. The study thus did not account for the differences in socioeconomic status among residents in the same census tract, which can lead to the ecological fallacy. Just like any area-based research using aggregate data, our study is not immune to the modifiable areal unit problem (MAUP). The MAUP affects the results of area-based research since the values of area-based attributes may vary by the selected zoning scheme or geographic scale of the areal units [40]. Further, due to data availability issues, there are some additional limitations to our study. Specifically, we did not integrate the temporal dimension (e.g., opening hours of the vaccination sites) into the spatial accessibility measure. Variations in the opening hours of vaccination sites can increase or reduce a vaccination site’s availability during different times of the day, which may result in concurrent variations in spatial accessibility to vaccination during different times of the day. Further, since we did not have data about the capacity of each vaccination site, our spatial accessibility measure did not differentiate the supply capacity of each vaccination site. In reality, the capacities of vaccination sites vary by factors such as area and available staff. Therefore, because of the lack of vaccination site capacity data, we assumed that all vaccination sites have the same capacity in our spatial accessibility measure.
Author Contribution
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Dong Liu and Zihan Kan. The first draft of the manuscript was written by Dong Liu. Mei-Po Kwan helped revise the first and revised versions of the paper. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Mei-Po Kwan was supported by grants from the Hong Kong Research Grants Council (RGC) (General Research Fund Grant no. 14605920, 14611621; Collaborative Research Fund Grant no. C4023-20GF; Research Matching Grant RMG 8601219) and a grant from the Research Committee on Research Sustainability of Major Research Grants Council Funding Schemes of the Chinese University of Hong Kong. Zihan Kan was supported by an RGC Postdoctoral Fellowship from the Research Grants Council of Hong Kong (PDFS2021-4S08).
Data Availability
All data used in this study are public data available on the web.
Code Availability
Not applicable; this study does not involve coding.
Declarations
Ethics Approval
Not applicable; this study uses public data available on the web.
Consent to Participate
Not applicable; this study uses public data available on the web.
Consent for Publication
Not applicable; this study uses public data available on the web.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dong Liu, Email: dliu457@uwo.ca.
Mei-Po Kwan, Email: mpk654@gmail.com.
Zihan Kan, Email: zihankan@cuhk.edu.hk.
Yimeng Song, Email: yimsong@polyu.edu.hk.
Xuefeng Li, Email: lixuefengseu@foxmail.com.
References
- 1.Wrigley-Field E. US racial inequality may be as deadly as COVID-19. Proc Natl Acad Sci USA. 2020;117(36):21854–21856. doi: 10.1073/pnas.2014750117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abedi V, Olulana O, Avula V, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities. 2020;8(3):732–742. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shannon J, Abraham A, Adams GB, Hauer M. Racial disparities for COVID19 mortality in Georgia: spatial analysis by age based on excess deaths. Soc Sci Med. 2022;292:114549. doi: 10.1016/j.socscimed.2021.114549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luck AN, Preston SH, Elo IT, Stokes AC. The unequal burden of the Covid-19 pandemic: capturing racial/ethnic disparities in US cause-specific mortality. SSM Popul Health. 2022;17:101012. doi: 10.1016/j.ssmph.2021.101012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipsitch M, Dean N. Understanding COVID-19 vaccine efficacy. Science. 2020;370(6518):763–765. doi: 10.1126/science.abe5938. [DOI] [PubMed] [Google Scholar]
- 6.Polack F, Thomas S, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/nejmoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Voysey M, Clemens S, Madhi S, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99–111. doi: 10.1016/s0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathieu E, Ritchie H, Ortiz-Ospina E, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5(7):947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 9.Stok F, Bal M, Yerkes M, de Wit J. Social inequality and solidarity in times of COVID-19. Int J Environ Res Public Health. 2021;18(12):6339. doi: 10.3390/ijerph18126339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mills W, Sender S, Lichtefeld J, et al. Supporting individuals with intellectual and developmental disability during the first 100 days of the COVID-19 outbreak in the USA. J Intellect Disabil Res. 2020;64(7):489–496. doi: 10.1111/jir.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#trends_dailycases. 2021. Accessed November 30, 2021.
- 12.Kim S, Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ Behav. 2020;47(4):509–513. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gross C, Essien U, Pasha S, Gross J, Wang S, Nunez-Smith M. Racial and ethnic disparities in population-level Covid-19 mortality. J Gen Intern Med. 2020;35(10):3097–3099. doi: 10.1007/s11606-020-06081-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chung H, He S, Nasreen S, Sundaram ME, Buchan SA, Wilson SE, Chen B, Calzavara A, Fell DB, Austin PC, Wilson K. (2021) Effectiveness of BNT162b2 and mRNA-1273 covid-19 vaccines against symptomatic SARS-CoV-2 infection and severe covid-19 outcomes in Ontario, Canada: test negative design study. Brit Med J. 374. 10.1136/bmj.n1943 [DOI] [PMC free article] [PubMed]
- 15.Amirthalingam G, Bernal JL, Andrews NJ, Whitaker H, Gower C, Stowe J, Tessier E, Subbarao S, Ireland G, Baawuah F, Linley E. Serological responses and vaccine effectiveness for extended COVID-19 vaccine schedules in England. Nat Commun. 2021;12(1):1–9. doi: 10.1038/s41467-021-27410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. COVID-19 Booster Shot. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/booster-shot.html#print. 2021. Accessed November 30, 2021.
- 17.Mahase E. COVID-19 booster vaccines: what we know and who’s doing what. Brit Med J. 2021:n2082. 10.1136/bmj.n2082 [DOI] [PubMed]
- 18.Liu D, Kwan M. Measuring spatial mismatch and job access inequity based on transit-based job accessibility for poor job seekers. Travel Behav Soc. 2020;19:184–193. doi: 10.1016/j.tbs.2020.01.005. [DOI] [Google Scholar]
- 19.Jiao J, Azimian A. Measuring accessibility to grocery stores using radiation model and survival analysis. J Transp Geogr. 2021;94:103107. doi: 10.1016/j.jtrangeo.2021.103107. [DOI] [Google Scholar]
- 20.Liu D, Kwan M, Kan Z. Analysis of urban green space accessibility and distribution inequity in the City of Chicago. Urban For Urban Green. 2021;59:127029. doi: 10.1016/j.ufug.2021.127029. [DOI] [Google Scholar]
- 21.Tatar M, Shoorekchali J, Faraji M, Wilson F. (2021) International COVID-19 vaccine inequality amid the pandemic: perpetuating a global crisis?. J Glob Health. 11. 10.7189/jogh.11.03086 [DOI] [PMC free article] [PubMed]
- 22.Fu LY, Cowan N, McLaren R, Engstrom R, Teach SJ. Spatial accessibility to providers and vaccination compliance among children with medicaid. Pediatrics. 2009;124(6):1579–1586. doi: 10.1542/peds.2009-0233. [DOI] [PubMed] [Google Scholar]
- 23.Whitehead J, Carr PA, Scott N, Lawrenson R. Structural disadvantage for priority populations: the spatial inequity of COVID-19 vaccination services in Aotearoa. NZMA. 2022;135(1551):1175–8716. [PubMed] [Google Scholar]
- 24.Hildreth JE, Alcendor DJ. Targeting COVID-19 vaccine hesitancy in minority populations in the US: implications for herd immunity. Vaccines. 2021;9(5):489. doi: 10.3390/vaccines9050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen LH, Joshi AD, Drew DA, Merino J, Ma W, Lo CH, Kwon S, Wang K, Graham MS, Polidori L, Menni C. Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nat Commun. 2022;13(1):1–9. doi: 10.1038/s41467-022-28200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ermagun A, Tilahun N. Equity of transit accessibility across Chicago. Transport Res D: Tr E. 2020;86:102461. doi: 10.1016/j.trd.2020.102461. [DOI] [Google Scholar]
- 27.Liu D, Kwan M, Kan Z, Song Y. An integrated analysis of housing and transit affordability in the Chicago metropolitan area. Geogr J. 2021;187(2):110–126. doi: 10.1111/geoj.12377. [DOI] [Google Scholar]
- 28.United States Census Bureau. American Community Survey. https://data.census.gov/cedsci/advanced?y=2018. 2018. Accessed April 8, 2021.
- 29.ArcGIS Hub. COVID-19 Vaccination provider locations in the United States. https://hub.arcgis.com/datasets/c50a1a352e944a66aed98e61952051ef_0/explore. 2021. Accessed November 4, 2021.
- 30.Google Maps Platform. Google Maps Directions API Documentation. https://developers.google.com/maps/documentation/directions/get-directions. 2022. Accessed April 8, 2022.
- 31.Paez A, Higgins C, Vivona S. Demand and level of service inflation in floating catchment area (FCA) methods. PLoS ONE. 2019;14(6):e0218773. doi: 10.1371/journal.pone.0218773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo W, Wang F. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago region. Environ Plann B Plann Des. 2003;30(6):865–884. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu D, Kwan M, Kan Z. Analyzing disparities in transit-based healthcare accessibility in the Chicago Metropolitan Area. Can Geogr. 2021 doi: 10.1111/cag.12708. [DOI] [Google Scholar]
- 34.Palm M, Sturrock SL, Howell NA, Farber S, Widener MJ. The uneven impacts of avoiding public transit on riders’ access to healthcare during COVID-19. J Transp Health. 2021;1(22):101112. doi: 10.1016/j.jth.2021.101112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharma G, Patil GR. Public transit accessibility approach to understand the equity for public healthcare services: a case study of Greater Mumbai. J Transp Geogr. 2021;1(94):103123. doi: 10.1016/j.jtrangeo.2021.103123. [DOI] [Google Scholar]
- 36.Du F, Mao L, Wang J, Jin H. Inferring transit-based health seeking patterns from smart card data–a case study in Beijing, China. Health Place. 2020;1(65):102405. doi: 10.1016/j.healthplace.2020.102405. [DOI] [PubMed] [Google Scholar]
- 37.Brenneis M. No car? Accessing the vaccine will be difficult. Madison, WI: State Smart Transportation Initiative. https://ssti.us/2021/03/01/no-car-accessing-the-vaccine-will-be-difficult/. 2021. Accessed April 8, 2022.
- 38.Glenza J. 34 bus stops away: the hurdles car-less Americans face to reach vaccine sites. The Guardian. 2021. https://www.theguardian.com/us-news/2021/feb/04/rural-americans-barriers-access-vaccination-sites. Accessed April 8, 2022.
- 39.Strully KW, Harrison TM, Pardo TA, Carleo-Evangelist J. Strategies to address COVID-19 vaccine hesitancy and mitigate health disparities in minority populations. Front Public Health. 2021;9:384. doi: 10.3389/fpubh.2021.645268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kwan MP. The uncertain geographic context problem. Ann Assoc Am Geogr. 2012;102(5):958–968. doi: 10.1080/00045608.2012.687349. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this study are public data available on the web.
Not applicable; this study does not involve coding.