Abstract
Objectives
The Arab ethnic minority makes up 21% of Israel’s population and accounted for 40.5% of confirmed cases during the second wave of COVID-19. This study aims to assess the characteristics of compliance with the guidelines of the Ministry of Health and related factors that can explain the outbreak of COVID-19 among the Arab population during the second wave.
Methods
A cross-sectional online survey was conducted among 810 respondents from the Arab community during October 2020. The survey was distributed via social media such as Facebook and WhatsApp. The health belief model items, the theory of reasoned action items, trust in formal institutions, and pandemic fatigue were assessed, and a path analysis was performed.
Results
Positive correlations were demonstrated between both personal and social networks compliance (nuclear family, extended family, friends, etc.) and perceived severity of COVID-19, trust in formal institutions, attitudes toward compliance, and subjective norms (r = .12 to r = .64, p < .001, N = 810). Pandemic fatigue was negatively correlated with personal and social networks compliance, perceived severity of COVID-19, trust in institutions, attitudes toward compliance, and subjective norms (r = − .21 to r = − .48, p < .001). Positive correlations were evident between compliance with quarantine and perceived severity of COVID-19 and attitudes (r = .31 and r = .28, p < .001, respectively). Personal compliance was significantly lower among men (M = 3.93, SD = 0.94) and younger respondents (M = 4.14, SD = 0.71), while social networks compliance was lower among Muslims (M = 3.78, SD = 0.75).
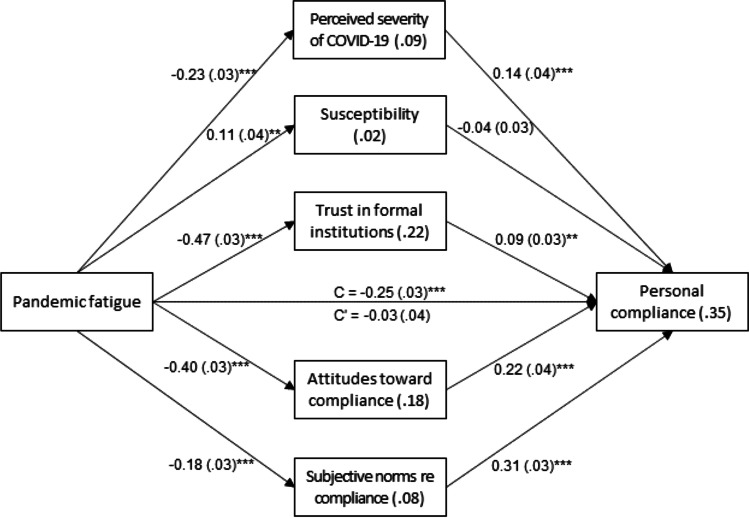
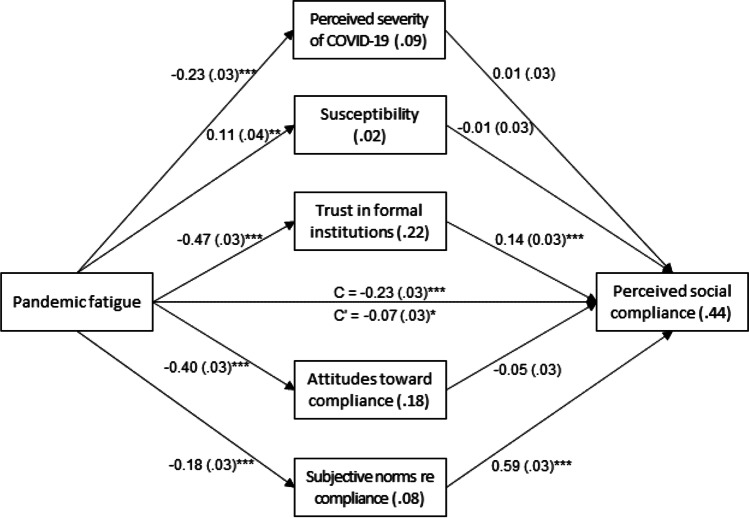
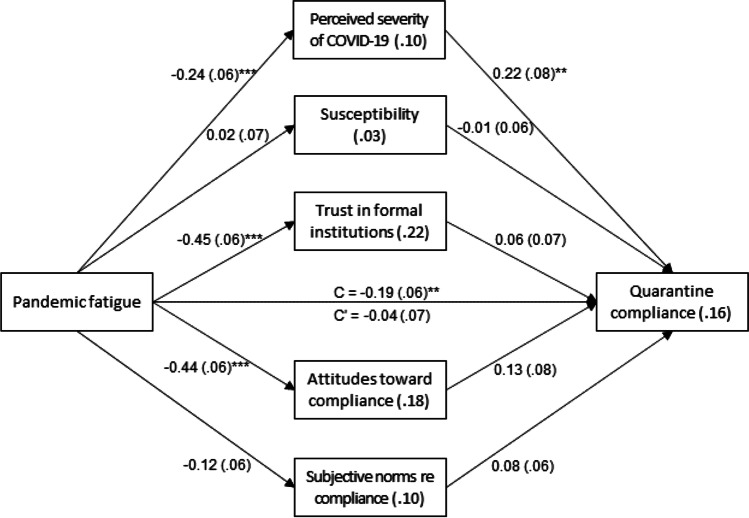
The negative relationship between pandemic fatigue and personal compliance was mediated by lower perceived severity of COVID-19, attitudes toward compliance, and subjective norms (p < .001). The negative relationship between pandemic fatigue and social network compliance was mediated by lower trust in institutions and subjective norms (p < .001). Lower perceived severity of COVID-19 mediated the relationship between higher pandemic fatigue and lower quarantine compliance (p = .003).
Conclusions
The results highlight the important of perception of the disease severity, social and subjective norms, and the central role of trust in determining adherence to guidelines. Thus, increasing trust on authorities and planning tailored-maid interventions can raise compliance with the preventive guidelines and prevent the spread of the virus. Such interventions will address the characteristics of minority populations and take into account the implications of the guidelines and the possibility that may lead to fatigue, which in turn will lead to non-compliance with those guidelines.
Keywords: Arab minority, Attitudes, Compliance, COVID-19, Quarantine, Pandemic fatigue, Subjective norms, Trust, Israel
Introduction
The novel coronavirus disease (COVID-19) broke out in China at the end of 2019. The World Health Organization (WHO) labeled the COVID-19 outbreak a “Public Health Emergency of International Concern” [1, 2] that constitutes a threat to the mental and physical health of the world’s population [3, 4]. The pandemic spread rapidly across the globe, accompanied by increasing morbidity and mortality rates [5, 6]. To stop the disease from spreading, the WHO recommends a series of preventive behaviors, including mask-wearing, hand hygiene, and social distancing or lockdowns [2]. Isolation and social distancing measures have proven to be the most effective strategy in containing the pandemic [7–9].
The effective control of outbreaks of epidemics relies on public compliance with guidelines [10–12]. Studies show that those who perceive a disease as serious and dangerous are more likely to comply with the guidelines [13–15]. During the Ebola epidemic, for example, Ajilore, Atakiti, and Onyenankeya [16] found that risk perceptions regarding the disease affected health behavior. According to the health belief model (HBM), risk perceptions are defined by a combination of two factors: (1) perceived threat of the disease, representing what individuals believe about their chances of contracting a certain disease or the likelihood that their health will deteriorate as a result of engaging in or refraining from health behaviors; and (2) perceived severity of the disease, representing individuals’ beliefs regarding the severity of a disease or a medical condition [17]. The HBM posits that perceived threat and perceived severity influence behavior; for example, people’s perceptions of the seriousness of contracting an illness or disease affect their motivation to avoid being infected [18, 19].
When this research was conducted (October 2020), the world was in the midst of the second wave of the COVID-19 pandemic. Israel had one of the highest morbidity rates globally during this wave [20]. In response, the government issued numerous guidelines to the Israeli population to cope with the consequences of COVID-19 infection and to prevent the virus from spreading. In June 2020, the number of new confirmed cases of COVID-19 reached 4000–6000 new cases a day in mid-September the number of deaths approached 1200 or 130 deaths per million. At this point, with roughly 180,000 confirmed cases, 50,000 of which were active. Throughout the pandemic, morbidity in Arab society fit to its proportion in the population (20%), and general society occupied a smaller volume than its proportion in the population of 54%. Although the total morbidity in Arab society fit to its proportion in the population, it was found that out of the total morbidity in the country, its proportion was significantly higher than the relative proportion in the population (30%), the general society constituting 69%, and the Arabs 59%. The relative number of patients in critical condition in Arab society was the highest in the country throughout the epidemic and was also dominant at younger ages compared to other societies [21].
In mid-September 2020, the government declared a second general lockdown that entailed physical and social distancing and isolation [21].
The Israeli Ministerial Committee for Coping with the Coronavirus and its Consequences recommended implementing a policy of differential treatment in fighting the spread of the disease. According to this policy, all cities in Israel were classified into one of four categories—red, orange, yellow, or green—depending on their morbidity and infection rates [22]. The cabinet recommended imposing differential restrictions on cities in accordance with their classification, up to imposing local lockdowns [22].
The COVID-19 pandemic has had major health and economic consequences for the global population. As has been the case in other disasters [23], ethnic minorities are more vulnerable to the physical, economic, and emotional consequences of the present pandemic [24]. They have borne a disproportional share of the disease in terms of hospitalizations and deaths [25–27]. In line with this, the COVID-19 pandemic has spread rapidly throughout the Arab localities in Israel, such that these localities top the list of cities classified as red [22].
The Arab citizens of Israel are an ethnic minority constituting 21% of the population. Ninety percent of the Arab citizens live in homogenous communities located in the peripheral region, which are characterized by overcrowded conditions [28]. They are classified as having a low socioeconomic status [29] and have been suffering from discrimination [30], limited access to healthcare services [31], and low levels of health literacy [31]. Furthermore, compared to the Jewish population of Israel, Arab men have a high prevalence of chronic lower respiratory diseases and smoking, and among Arabs of both sexes, the prevalence of diabetes, high blood pressure, and cardiac and vascular disease is higher [32]. Therefore, the Arab community is more vulnerable to the health consequences of COVID-19.
Previous epidemic studies reveal that trust in the government and the health system is related to compliance with guidelines for preventing the spread of disease [33–37]. High levels of trust are related to better compliance with COVID-19 guidelines issued by health and government authorities [38, 39]. Two other studies that examined adherence to social distancing among Israeli Jewish found that they reported more compliance with Ministry of Health (MOH) guidelines than Israeli Arabs [30, 40].
However, ethnic minorities tend to have lower levels of trust in governments and health authorities, leading to lower compliance with COVID-19 guidelines. For example, a study that examined adherence to COVID-19 preventive guidelines (including washing hands, social distancing, avoiding face touching, and wearing masks) among African Americans reported that they have lower than 80% adherence to these guidelines [41]. Furthermore, the Arab population in Israel is marked by a lack of trust in the government and a sense of alienation resulting from the government’s exclusionary policy and declarations. According to Lavie et al. [42], low levels of trust can affect the attitudes of the Arabs, causing them to comply less with the guidelines.
In addition, it is important to note that the second wave of COVID-19 in Israel coincided with the wedding season in Arab society. There was therefore a clash between the values, norms, and customs of this society and government guidelines for coping with this dangerous pandemic, affecting the extent of compliance. The gathering of many people at these weddings undoubtedly contributed to the high morbidity rates among Israel’s Arab population [43].
On top of all this, the longer the pandemic lasted, the more people lost their motivation to comply with the guidelines. Their motivation was affected by the feelings, experiences, and perceptions of others [3]. This diminishing motivation to comply with cautionary measures was apparent in Israel, compromising the government’s ability to decrease the high morbidity rates [17].
The WHO coined the term “pandemic fatigue” to describe the population’s general feelings of distress in response to an ongoing crisis whose end is nowhere in sight. People feel unmotivated to implement the recommended guidelines for protecting themselves and others against the virus [3]. To combat this, the WHO recommends involving the public in finding solutions to which they can commit themselves [3] as long-term restrictions are likely to be impossible to implement for everyone over time. The organization has issued a document outlining strategies, principles, and best practices to counter pandemic fatigue and reignite public support for maintaining protective measures. These strategies include understanding people, using proven evidence for policy implementation, targeting and tailoring interventions and media communication, and enabling people to live their lives while reducing the risks.
People’s behavior usually stems from their perceptions of what others in their environment think about their behavior and how others expect them to behave. According to the theory of reasoned action (TRA), people’s viewpoints about particular behaviors are also a consequence of their beliefs about the results of these behaviors [44]. Hence, individuals will have positive views regarding a particular behavior if they believe that it will, in most cases, have positive consequences for themselves [45]. Moreover, subjective norms are the outcome of what individuals believe regarding how others expect them to behave [46].
The above summary leads to the understanding that human behavior is a crucial factor in the transmission of SARS-Cov-2, the virus that causes COVID-19, and that behavioral change is essential in stopping the spread of the pandemic. Furthermore, minority populations are more vulnerable to pandemics in general and to the current pandemic in particular. The objective of the current study is to examine the factors influencing compliance with MOH guidelines among a minority population—the Arab population in Israel.
Study Hypotheses
(1) Variables of the HBM and TRA—lower perceived severity of and susceptibility to COVID-19, lower trust in formal institutions, negative attitudes toward compliance, and lower subjective norms, will be related to lower compliance with MOH guidelines.
(2) Variables of the HBM and TRA will serve as mediators between pandemic fatigue and compliance with MOH guidelines. Higher pandemic fatigue will be related to lower perceived severity of and susceptibility to COVID-19, lower trust in formal institutions, negative attitudes toward compliance, and lower subjective norms, which in turn will be related to lower compliance with MOH guidelines.
Material and Methods
Research Population
The current study entailed analyzing data collected by means of an online cross-sectional survey completed by 810 respondents from the Arab population in Israel during the period October 16–19, 2020, while Israel was under its second lockdown in an effort to prevent the spread of COVID-19. The respondents were at least 18 years old and identified themselves as Muslims, Christians, and Druze living in Israel. The survey was distributed via social media such as Facebook and WhatsApp, and participants were asked to send the survey link to their relatives and friends, thus generating a sample via snowball sampling. Participation in the survey was voluntary, and participants were not offered any compensation. The research protocol was approved by the Ethics Committee at the researchers’ academic institution (approval number YVC EMEK 2021–30).
Research Tools
The survey used validated questionnaires from previous studies as well as questionnaires based on the literature that were developed specifically for the current study. Questionnaire items that were originally in English were translated into Arabic and then back-translated into English to ensure questionnaire reliability. Two professionals in the field who are fluent in Arabic validated the translation. An explanation of the research topic and research population appeared at the beginning of the survey, together with information about maintaining participant confidentiality and an explanation that participants could refuse to complete the questionnaire or could stop filling it out at any time without any consequence to themselves.
Questionnaire Examining Compliance with Ministry of Health Guidelines
This questionnaire examined three levels of compliance: personal, social network, and quarantine compliance.
Personal Compliance with MOH Guidelines
Participants were asked to report their behavior by describing the extent to which they complied with MOH guidelines during the second wave of COVID-19. Compliance was assessed by 12 statements based on MOH guidelines [21]. Sample statements include: “I maintain a distance of 2 m from other people,” “I do not participate in crowded events such as weddings,” and “I always wear a mask that covers my nose and mouth whenever I leave home.”
Compliance of Social Network with MOH Guidelines
Respondents were asked to report their impressions of other individuals in their social networks in terms of compliance with MOH guidelines to avoid the spread of COVID-19. Four social circles were surveyed: the nuclear family (those who live with the respondent in the same home), the extended family (uncles, aunts, in-laws), and friends, the workplace, and the village/town of residence.
Compliance with Quarantine Guidelines
The questions included in this part were only answered by participants who had faced mandatory quarantine because they had tested positive for COVID-19, had been exposed to a confirmed case, or had returned from abroad. The respondents were asked to quantify the rate of compliance with MOH guidelines on seven components that were created according to MOH guidelines. For example, the respondents were asked to reply to the following item: “During quarantine, I stayed in a separate room/separate house/separate floor/government authorized hotel.”
Participants rated their compliance and that of their social network with MOH guidelines for preventing the spread of COVID-19 on a Likert scale ranging from 1 (not at all) to 5 (always). Mean scores were calculated for each participant, with higher total scores representing higher compliance with MOH guidelines. Cronbach’s α was 0.90, 0.69, and 0.80 for items measuring personal compliance, perceived compliance of social network, and compliance with quarantine guidelines, respectively.
Questionnaire Examining Trust in the Health System
The trust in the health system questionnaire based on the Multidimensional Trust in Health-Care System Scale questionnaire [47] examined the extent of respondents’ trust in the people and professional organizations leading the battle against COVID-19 in Israel. These included all eight professional organizations and individuals involved in handling the COVID-19 pandemic in Israel, among them the Prime Minister, the National Coronavirus Project Coordinator, and the MOH. Participants were asked to rate each statement on a scale ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s α was 0.87 for all items on the trust scale. Mean scores were calculated for each participant, with higher total scores representing greater trust in the healthcare system.
Questionnaire Examining Perceived Severity of and Susceptibility to COVID-19
To assess perceived susceptibility to and severity of COVID-19, we used the 17 items from the study by Prasetyo, Castillo, Salonga, and Seneta [46] that were based on a sub-scale of the HBM [48, 49]. Five items were used for assessing perceived susceptibility. Sample items include: “I think I am very susceptible to COVID-19” and “I think there’s a chance my family will be infected with COVID-19.” Twelve items were used to assess perceived severity. Sample items include the following: “In my opinion, COVID-19 is more serious than any other disease” and “I believe that COVID-19 may lead to death.” Participants were asked to rate each of these 17 items on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s α was acceptable at 0.79 and 0.88 for perceived susceptibility and perceived severity, respectively. Mean scores were calculated for each participant, with higher total scores representing a higher perceived susceptibility to and severity of COVID-19.
Questionnaire Examining Attitudes and Subjective Norms Regarding Compliance with Ministry of Health Guidelines
Attitudes and subjective norms regarding compliance with MOH guidelines were assessed using the questionnaires developed by Ajzen and Fishbein, and Ajzen and Madden [50, 51], which were adapted for this study. Six items were used to assess subjective norms. Sample items include: “Most people in my extended family believe in wearing masks outside the home to prevent the spread of the virus” and “Most people I know do not attend weddings.” Ten items were used to assess attitude. Sample items include: “I think that social distancing may prevent the spread of the disease.” Each item was rated on a five-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s α for attitudes toward compliance was 0.80, and for subjective norms about compliance, it was 0.92. Mean scores were calculated for all participants, with higher total scores representing positive subjective norms and attitudes toward compliance (i.e., a perception that the behavior is more acceptable in the respondent’s social network).
Questionnaire Examining Pandemic Fatigue
The questionnaire assessing pandemic fatigue was constructed based on a checklist published by the WHO designed to help countries devise appropriate policies to help people comply with guidelines [52]. The questionnaire included nine items. A sample item is: “Government and MOH leaders are not role models for me.” Participants were asked to rate each of these items on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s α was 0.80. Mean scores were calculated for each participant, with higher total scores representing higher perceived pandemic fatigue.
Demographic Questionnaire
Participants were asked to provide the following personal information: age; sex; religion (Muslim, Bedouin, Druze, or Christian); degree of religious observance (secular, traditional, religious, very religious); marital status; number of children; place of residence (north, south, or center of Israel); education (high school, post-secondary vocational, academic); type of employment (self-employed, salaried, unemployed); and income level (below average, average, above average).
Data Analysis
Data were analyzed using SPSS version 27. Categorical background characteristics and items of compliance with MOH guidelines were described using frequencies and percentages. Continuous variables were described using means and standard deviations. Internal consistencies were calculated using Cronbach α, and variables were computed using item means. Personal compliance, quarantine compliance, and attitudes toward compliance were negatively skewed and were thus exponentially transformed. Pearson correlations were calculated between contentious variables. Bonferroni correction for multiple comparisons was applied. Relationships between compliance with MOH guidelines and various demographic characteristics of the participants were examined using series of t tests. Further, a series of t tests was used to assess differences in the study variables according to the presence of quarantine. Multiple hierarchical linear regressions were calculated for the three dependent variables of compliance with MOH guidelines. Demographic characteristics were entered in the first step, pandemic fatigue in the second, and the other study variables in the third. Mediation effects were examined because the pandemic fatigue variable was significantly related to the study variables in the bivariate relationship, and in regression analysis, the relationship disappeared. Therefore, it was tested as an independent variable, and mediation effects were examined with the Process procedure, model no. 4, for parallel mediation [53]. Continuous variables were standardized, and 5000 bootstrap samples were used with a 95% confidence interval.
Results
Participants
A total of 810 Israeli Arab adults, women (n = 641, 79.1%) and men (n = 169, 20.9%), between the ages of 18 and 55 years participated in this study. The age groups were 18 to 25 years old (n = 145, 17.9%), 26 to 35 years old (n = 182, 22.5%), 36 to 45 years old (n = 460, 56.8%), and 46 to 55 years old (n = 23, 2.8%). Most were Muslim (n = 542, 68.2%), and others were Christian (n = 217, 27.3%) or Druze (n = 36, 4.5%). Almost half were religious (n = 388, 48.5%), and others were partly religious (n = 305, 38.1%) or secular (n = 107, 13.4%). Most were married or had an intimate relationship (n = 614, 76.3%), and others were single (n = 157, 19.5%) or divorced/widowed (n = 34, 4.2%). Most of the respondents had children (n = 596, 73.6%), with a maximum of 10 children (M=3.16, SD = 1.44). About two-thirds of them lived in rural areas (n = 537, 66.3%), and more than three-quarters lived in northern Israel (n = 625, 77.2%). Others lived in central Israel and Jerusalem (n = 37, 4.5%) or in southern Israel (n = 148, 18.3%).
About 70% of the participants had an academic degree (n = 557, 69.3%), and others had higher education (n = 140, 17.4%) or high school education (n = 107, 13.3%). Close to 70% of the participants were employed (n = 550, 68.4%), while others were unemployed (n = 87, 10.8%), on a leave of absence (n = 28, 3.5%), or retired/students/housewives (n = 139, 17.3%). Most reported a below average income (n = 393, 50.1%), followed by an above average income (n = 246, 31.4%) and then an average income (n = 145, 18.5%). Most were in good to excellent health (n = 757, 93.6%) and did not use medication regularly (n = 663, 82.0%).
Compliance with Ministry of Health Guidelines
The participants were generally compliant with MOH guidelines. Most of them avoided public places when they had respiratory symptoms or a fever (n = 761, 94.0%), wore a face mask when outside the home (n = 733, 90.5%), and avoided contact with people who showed respiratory symptoms (n = 707, 87.3%). To a lesser extent, they washed their hands often and for at least 20 s at a time (n = 569, 70.4%), avoided visiting family and friends (n = 537, 66.3%), and avoided touching their faces with unwashed hands (n = 530, 66.0%).
Participants perceived that their social networks were fairly compliant with MOH guidelines. The majority perceived that MOH guidelines were adhered to in their workplace at least most of the time (n = 661, 81.6%), as well as in their nuclear family (n = 656, 81.0%), and in their extended family (n = 503, 62.1%). Lower compliance was noted for the community in general (n = 240, 29.6%).
About a third of the participants (n = 262, 32.3%) were required to be in quarantine at some point. Mostly, these participants stayed indoors (n = 243, 92.8%), covered their mouth and nose when coughing (always, n = 241, 92.0%), and washed their hands frequently (n = 244, 93.1%). They avoided contact with other people in the home (n = 236, 90.1%) and generally stayed in a separate room (n = 195, 74.4%).
Table 1 presents the distribution of the study variables and their inter-correlations. The results show high means for personal compliance with MOH guidelines, as well as for compliance with quarantine guidelines. The mean for perceived compliance of the social network is somewhat lower. Means for perceived severity of COVID-19, susceptibility, pandemic fatigue, and trust in formal institutions are all around mid-scale, while means for attitudes toward compliance and subjective norms about compliance tend to be high. Significant correlations were found between the study variables. Both personal and perceived social network compliance were positively related to perceived severity of COVID-19, trust in formal institutions, attitudes toward compliance, and subjective norms about compliance, and negatively related to pandemic fatigue. Both were unrelated to susceptibility. Compliance with quarantine guidelines was positively related to perceived severity of COVID-19 and attitudes toward compliance. Further, perceived severity of COVID-19, trust in formal institutions, attitudes toward compliance, and subjective norms about compliance were positively interrelated. Susceptibility was positively related to perceived severity of COVID-19 and attitudes toward compliance. Pandemic fatigue was negatively related to perceived severity of COVID-19, trust in formal institutions, attitudes toward compliance, and subjective norms about compliance.
Table 1.
Means, standard deviations, and inter-correlations for the study variables (N = 810)
| M (SD) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Personal compliance | 4.25 (0.74) | .45* | .32* | − .28* | .39* | .02 | .28* | .39* | .43* |
| 2. Perceived social network compliance | 3.83 (0.70) | .12 | − .25* | .18* | − .06 | .32* | .12* | .64* | |
| 3. Quarantine compliance (n = 262) | 4.48 (0.68) | − .17 | .31* | .03 | .19 | .28* | .14 | ||
| 4. Pandemic fatigue | 3.29 (0.84) | − .25* | .10 | − .48* | − .41* | − .21* | |||
| 5. Severity of COVID-19 | 3.54 (0.84) | .30* | .26* | .57* | .24* | ||||
| 6. Susceptibility | 2.70 (0.92) | .02 | .15* | − .09 | |||||
| 7. Trust in formal institutions | 3.04 (0.98) | .30* | .26* | ||||||
| 8. Attitudes toward compliance | 3.93 (0.74) | .14* | |||||||
| 9. Subjective norms about compliance | 3.72 (0.91) |
Range: 1–5. Bonferroni correction for multiple comparisons was applied (p < .001)
Several relationships were found between compliance with MOH guidelines and the demographic characteristics of the participants. Personal compliance with MOH guidelines was higher among women (M = 4.33, SD = 0.66) than men (M = 3.93, SD = 0.94) (t (808) = 5.86, p < 0.001). It was also higher among participants older than 36 years (M = 4.32, SD = 0.76) than among younger participants (ages 18 to 35) (M = 4.14, SD = 0.71) (t (808) = 4.59, p < 0.001). Similarly, personal compliance with MOH guidelines was higher among participants who were parents (M = 4.30, SD = 0.76) than among those who did not have children (M = 4.10, SD = 0.68) (t (808) = 3.50, p < 0.001). Perceived compliance of the social network with MOH guidelines was found to be higher among non-Muslim participants (Christian and Druze) (M = 3.97, SD = 0.56) than among Muslim participants (M = 3.78, SD = 0.75) (t (634.36) = 3.88, p < 0.001). Other relationships between compliance with MOH guidelines and the demographic characteristics of the participants were not found significant when applying the Bonferroni correction for multiple comparisons (including level of education, income, religiosity, rural/urban living, and health status). In addition, having children was highly correlated with age (Phi = 0.55, p < 0.001). Thus, the study hypotheses were examined while controlling for gender (1: male, 0: female), age group (1:55-36, 0: 18–35), and religion (1: Muslim, 0: Christian or Druze).
Participants who had been quarantined (n = 262) reported feeling more susceptible to contracting the virus (M = 2.87, SD = 0.95) than those who had not (M = 2.61, SD = 0.89) (t (808) = 3.79, p < 0.001). All other differences, in terms of compliant behavior, perception of severity, pandemic fatigue, trust, attitudes, and subjective norms, were not significant.
Three multiple hierarchical linear regressions were calculated for the three dependent variables of compliance with MOH guidelines. Demographic characteristics were entered in the first step, pandemic fatigue in the second, and the other study variables in the third (see Table 2). The three models were found significant, with 35% of the variance in personal compliance explained, 43% of the variance in perceived social network compliance explained, and 12% of the variance in quarantine compliance explained. Bonferroni correction for multiple comparisons was applied regarding personal and perceived social network compliance (p = 0.005).
Table 2.
Multiple hierarchical linear regressions for compliance with MOH guidelines
| Personal compliance (n = 795) | Perceived social network compliance (n = 795) | Quarantine compliance (n = 256) | ||||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Step 1 | ||||||
| Gender (male) | − .21 | < .001 | − .06 | .078 | .03 | .619 |
| Age group (older) | .17 | < .001 | .05 | .125 | − .07 | .282 |
| Religion (Muslim) | − .04 | .283 | − .11 | .002 | − .13 | .047 |
| Adj.R2 | .07, p < .001 | .02, p < .001 | .01, p = .208 | |||
| Step 2 | ||||||
| Gender (male) | − .19 | < .001 | -.04 | .190 | .06 | .361 |
| Age group (older) | ·17 | < ·001 | .05 | .157 | − .07 | .253 |
| Religion (Muslim) | − .02 | .454 | − .10 | .003 | − .12 | .059 |
| Pandemic fatigue | − .25 | < .001 | − .23 | < .001 | − .18 | .004 |
| Adj.R2 | .13, p < .001 | .07, p < .001 | .03, p = .013 | |||
| Step 3 | ||||||
| Gender (male) | − .13 | < .001 | .03 | .227 | .11 | .077 |
| Age group (older) | .14 | < .001 | .06 | .039 | − .08 | .213 |
| Religion (Muslim) | .04 | .144 | − .01 | .854 | − .09 | .163 |
| Pandemic fatigue | − .03 | .403 | − .07 | .035 | − .04 | .618 |
| Severity of COVID-19 | .14 | < .001 | .01 | .779 | .22 | .007 |
| Susceptibility | − .04 | .148 | − .01 | .796 | − .01 | .981 |
| Trust in formal institutions | .09 | .009 | .14 | < .001 | .06 | .419 |
| Attitudes toward compliance | .22 | < .001 | -.05 | .175 | ·14 | .079 |
| Subjective norms about compliance | .31 | < .001 | .60 | < .001 | .08 | .207 |
| Adj. R2 | .35, p < .001 | .43, p < .001 | .12, p < .001 | |||
| F |
F(9, 785) = 47.44, p < .001 |
F(9, 785) = 68.30, p < .001 |
F(9, 246) = 5.04, p < .001 |
|||
Bonferroni correction for multiple comparisons was applied regarding personal and social network compliance (p = .005)
The results show that personal compliance was higher among females and older participants. Further, perceptions of higher severity of COVID-19, more supportive attitudes toward compliance, and higher subjective norms regarding compliance were related to greater personal compliance with MOH guidelines. Greater trust in formal institutions and higher subjective norms regarding compliance were related to higher perceived social network compliance. Finally, perceptions of higher severity of COVID-19 were related to higher compliance with quarantine guidelines. These results support hypotheses 1.
In all three models, pandemic fatigue had a negative and significant contribution in the second step, beyond the background variables, but lost its significance in the third step.
The role of perceived severity of COVID-19, susceptibility, trust in formal institutions, attitudes toward compliance, and subjective norms about compliance as mediators between pandemic fatigue and the three types of compliance with MOH guidelines was examined using three Process models [45]. A parallel mediation Process model (model no. 4) was calculated for each type of compliance with MOH guidelines. Pandemic fatigue was defined as the independent variable, and gender (1: male, 0: female), age group (1: older, 0: younger), and religion (1: Muslim, 0: other) as covariates. Bonferroni correction for multiple comparisons was applied regarding personal and perceived social network compliance (p = 0.005).
The three total indirect effects were found significant (see Table 3 and Figs. 1, 2, and 3). Regarding personal compliance, three mediators were found significant: perceived severity of COVID-19, attitudes toward compliance, and subjective norms about compliance. Higher pandemic fatigue was related to lower perceived severity of COVID-19, less positive attitudes toward compliance, and lower subjective norms about compliance, which were then related to lower personal compliance.
Table 3.
Mediation effects between pandemic fatigue and compliance with MOH guidelines
| Personal compliance (n = 795) | Perceived social networks compliance (n = 795) | Quarantine compliance (n = 256) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Effect (SE) | 95%CI | p | Effect (SE) | 95%CI | p | Effect (SE) | 95%CI | p | |
| Total indirect effect | -0.23 (0.03) |
-0.28, -0.17 |
< .001 | -0.16 (0.03) |
-0.22, -0.10 |
< .001 | -0.15 (0.05) |
-0.25, -0.05 |
.003 |
| Severity of COVID-19 | − 0.03 (0.01) |
− 0.06, − 0.01 |
.003 | − 0.01 (0.01) |
− 0.02, 0.02 |
.809 | − 0.05 (0.02) |
− 0.11, − 0.01 |
.024 |
| Susceptibility | − 0.01 (0.01) |
− 0.01, 0.01 |
.242 | − 0.01 (0.01) |
− 0.01, 0.01 |
.841 | − 0.01 (0.01) |
− 0.01, 0.01 |
.981 |
| Trust in formal institutions | − 0.04 (0.02) |
− 0.07, − 0.01 |
.017 | − 0.06 (0.02) |
− 0.10, − 0.03 |
< .001 | − 0.03 (0.03) |
− 0.10, 0.04 |
.939 |
| Attitudes toward compliance | − 0.09 (0.02) |
− 0.13, − 0.05 |
< .001 | 0.02 (0.01) |
− 0.01, 0.05 |
.163 |
− 0.06 (0.03) |
− 0.13, 0.01 |
.084 |
| Subjective norms about compliance | − 0.06 (0.01) |
− 0.09, − 0.03 |
< .001 | − 0.11 (0.02) |
− 0.16, − 0.06 |
< .001 | − 0.01 (0.01) |
− 0.03, 0.01 |
.923 |
Bonferroni correction for multiple comparisons was applied regarding personal and social network compliance (p = .005)
Fig. 1.
The mediating role of variables of the health belief model and variables of the theory of reasoned action in the relationship between pandemic fatigue and personal compliance with MOH guidelines. Note. Values on arrows: B(SE), values within rectangles: R.2, C = total effect, C’ = direct effect. *p < .05, **p < .01, ***p < .001
Fig. 2.
The mediating role of variables of the health belief model and variables of the theory of reasoned action in the relationship between pandemic fatigue and perceived social network compliance with MOH guidelines. Note. Values on arrows: B(SE), values within rectangles: R.2, C = total effect, C’ = direct effect. *p < .05, **p < .01, ***p < .001
Fig. 3.
The mediating role of variables of the health belief model and variables of the theory of reasoned action in the relationship between pandemic fatigue and quarantine compliance with MOH guidelines. Note. Values on arrows: B(SE), values within rectangles: R.2, C = total effect, C’ = direct effect. *p < .05, **p < .01, ***p < .001
Regarding perceived social network compliance, two mediators were found significant: trust in formal institutions and subjective norms about compliance. Higher pandemic fatigue was related to lower trust in formal institutions and lower subjective norms about compliance, which were then related to lower perceived social network compliance.
Regarding quarantine compliance, one mediator was found significant: perceived severity of COVID-19. Higher pandemic fatigue was related to lower perceived severity of COVID-19, which was then related to lower quarantine compliance. This support partially hypothesis 2.
Discussion
Adherence to MOH preventive measures by the ethnic Arab residents in Israel during the second wave of the COVID-19 pandemic was influenced by several factors. The present study examined the behavioral aspects (HBM, TRA) related to both personal and social network compliance, such as the perceived severity of COVID-19 and pandemic fatigue, among the minority Arab population, who are more vulnerable to crises due to their social characteristics. The findings of the present study were consistent with findings of previous studies [13–15, 54].
Participants of the current study were personally compliant with MOH guidelines. As mentioned before, most of the participants have higher education, and this can explain to some extend these results. Comparing to other Arabs countries, previous studies show also high compliance with the preventive guidelines, for example, Egypt [55], Jourdan [56], and Iraq [57].
On the other hand, they reported low levels of compliance among their social networks. This can be explained by other health related behaviors. The Arab Israeli population suffer from poor health compared to the Jewish population. They suffer from high incidence of road accidents and chronic smoking-related lower respiratory disease, growing of life expectancy gap between the two populations Arabs and Jews, especially for men. Diabetes also appears to be a major cause of mortality that distinguishes between the Arab Israeli and Jewish populations—accounting for a 2.25-fold difference in fatality rates [32].
Subjective norms among Arab participants, such as attending crowded events (i.e., weddings or funerals), have caused increased morbidity rates due to a lack of proper pandemic information dissemination or alternatives to such events. This implies that the customs and traditions of the community, as part of a “collective society” which stresses the importance of the community over the individual, have a stronger impact on individual behavior than compliance with MOH guidelines.
The demographic characteristics identified as contributing to compliance with MOH guidelines were age and gender (female) respondents and older participants expressed higher personal compliance. Demographic characteristics (for example, gender and age) are known as no-modifiable factors, and it cannot be changed, but it can be useful to develop tailor interventions targeting such subgroups. These interventions can help in raising levels of compliance with health related behaviors like COVID-19 guidelines.
Moreover, higher trust in institutions led to better adherence to guidelines as well as higher perceived severity of COVID-19. The latter was a significant factor related to personal compliance. Trust has been tested in several studies to predict adherence to health related guidance [54]. For better compliance with COVID-19 preventive guidelines, it is important to foster public trust in health system institutions in general, and especially among minority communities. Satran et al. [56] recently published a study attesting to the role of the perceived severity of COVID-19 and trust in the healthcare system among Israeli Arabs during the first wave. The participants also reported a high degree of perceived threat and a moderate level of trust in the healthcare system and very high adherence to guidelines. At that time, the Arab community’s morbidity rate was lower than that of the rest of the country [20, 57].
Pandemic fatigue, expressed as low personal compliance, and it was mediated by perceived severity of COVID-19, trust in formal institutions, and social norms. Previous study demonstrated that lower perceived social support was significantly associated with a higher level of active coping with COVID-19, and this was mediated by a higher level of risk perception [58]. Cross-sectional study [59] found that both higher level of perceived susceptibility and perceived severity of COVID-19, trust and pro-social orientation, were associated with protective behaviors, such as social distancing and more. Keeping these rules (of COVID-19 guidelines) like social distancing comes with individual costs and leading to pandemic fatigue. It is possible that pandemic fatigue will be expressed as stress, which could be associated with indifference to authority guidelines.
A limitation of this study was that it addressed the age group of 18–55 years old, excluding older respondents who are the most at risk. However, the chosen group of respondents represents the workforce age range, making them at risk of exposure to COVID-19 in the workplace.
Another limitation was that the demographic data reported only 21% male respondents, indicating their underrepresentation among the study participants compared to the wider Arab population. Additionally, the study sample included mainly academic women, which impairs the ability to generalize.
Nonetheless, we point out that electronic media was accessible during the lockdown and stay-at-home orders, with the survey link reaching more than 800 respondents over a short period of 4 days.
The study has several important implications for policy makers. The results highlight the important of social and subjective norms, as well as the central role of trust in determining adherence to guidelines. Thus, increasing trust on authorities can raise compliance with the preventive guidelines and prevent the spread of the virus.
Based on the results, it is recommended to plan tailored made interventions. Such interventions will address the characteristics of minority populations and take into account the implications of the guidelines and the possibility that may lead to fatigue, which in turn will lead to non-compliance with those guidelines.
Moreover, the findings highlight the importance of preparing ahead of time and planning for any other pandemic, medical crisis, or emergency that might materialize.
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ola Ali Saleh and Samira Obeid. The first draft of the manuscript was written by Ola Ali Saleh and Samira Obeid. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee at the Max Stern Yezreel Valley Academic College (approval number YVC EMEK 2021–30).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill 2020;25(5):pii–200131e. 10.2807/1560-7917.ES.2020.25.5.200131e [DOI] [PMC free article] [PubMed]
- 2.World Health Organization. Coronavirus disease (COVID -19) advice for the public. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [accessed 12 May 2021]
- 3.World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. 2020. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2 [accessed 12 May 2020]
- 4.Del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA. 2020;324(17):1723–1724. doi: 10.1001/jama.2020.19719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 7.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289:113098. doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Memon Z, Qureshi S, Memon BR. Assessing the role of quarantine and isolation as control strategies for COVID-19 outbreak: a case study. Chaos, Solitons Fractals. 2021;144:110655. doi: 10.1016/j.chaos.2021.110655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor S. I've spent years studying the psychology of pandemics. This is what you need to know about Covid-19. Independent 2020
- 11.https://www.independent.co.uk/voices/coronavirus-covid-19-pandemic-psychology-research-predictions-a9406876.html [accessed 3 May 2020]
- 12.Webster RK, Brooks SK, Smith LE, Woodland L, Wessely S, Rubin GJ. How to improve adherence with quarantine: rapid review of the evidence. Pub Health. 2020;182:163–169. doi: 10.1016/j.puhe.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoo KJ, Kwon S, Choi Y, Bishai DM. Systematic assessment of South Korea’s capabilities to control COVID-19. Health Policy. 2021;125(5):568–576. doi: 10.1016/j.healthpol.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maroldi MAC, Felix AM, Dias AAL, et al. Adherence to precautions for preventing the transmission of microorganisms in primary health care: a qualitative study. BMC Nurs. 2017;16(1):1–8. doi: 10.1186/s12912-017-0245-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Graves KD, Huerta E, Cullen J, et al. Perceived risk of breast cancer among Latinas attending community clinics: risk comprehension and relationship with mammography adherence. Cancer Causes Control. 2008;19(10):1373–1382. doi: 10.1007/s10552-008-9209-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luo Y, Cheng Y, Sui M. The moderating effects of perceived severity on the generational gap in preventive behaviors during the COVID-19 pandemic in the US. Int J Environ Res Public Health. 2021;18(4):2011. doi: 10.3390/ijerph18042011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ajilore K, Atakiti I, Onyenankeya K. College students’ knowledge, attitudes and adherence to public service announcements on Ebola in Nigeria: suggestions for improving future Ebola prevention education programs. Health Educ J. 2017;76(6):648–660. doi: 10.1177/0017896917710969. [DOI] [Google Scholar]
- 18.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–386. doi: 10.1177/109019817400200405. [DOI] [PubMed] [Google Scholar]
- 19.Hochbaum GM. Psychosocial aspects of smoking with special reference to cessation. Am J Public Health Nations Health. 1965;55(5):692–697. doi: 10.2105/ajph.55.5.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 21.Birenbaum-Carmeli D, Chassida J. Health and socio-demographic implications of the COVID-19 second pandemic wave in Israel, compared with the first wave. Int J Equity Health. 2021;20(1):1–2. doi: 10.1186/s12939-021-01445-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health, Israel. The novel coronavirus. https://govextra.gov.il/ministry-of-health/corona/corona-virus-en/guidelines/ [accessed 12 May 2020]
- 23.Prime Minister’s Office, Israel. The Israeli Ministerial Committee for coping with COVID-19 and its consequences. The traffic lights program to differential dealing with the COVID-19 epidemic. 2020. https://www.gov.il/he/departments/policies/dec388_2020 [accessed 12 May 2020]
- 24.Davidson TM, Price M, McCauley JL, Ruggiero KJ. Disaster impact across cultural groups: comparison of Whites, African Americans, and Latinos. Am J Community Psychol. 2013;52(1):97–105. doi: 10.1007/s10464-013-9579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Risk of Severe Illness or Death from COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-illness.html [PubMed]
- 26.Reyes C, Husain N, Gutowski C, St Clair S, Pratt G. Chicago’s coronavirus disparity: black Chicagoans are dying at nearly six times the rate of white residents, data show. Chicago Tribune. 2020 https://www.chicagotribune.com/coronavirus/ct-coronavirus-chicago-coronavirus-deaths-demographics-lightfoot-20200406-77nlylhiavgjzb2wa4ckivh7mu-story.html [accessed 3 May 2020]
- 27.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 28.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8(6):547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Central Bureau of Statistics. Statistical abstract of Israel 2015—no. 66. 2015. https://www.cbs.gov.il/en/publications/Pages/2015/Statistical-Abstract-of-Israel-2015-No66.aspx [accessed 03 May 2020]
- 30.Central Bureau of Statistics. Socio-economic index of local authorities. 2020. https://www.cbs.gov.il/en/subjects/Pages/Socio-Economic-Index-of-Local-Authorities.aspx [accessed 12 May 2020]
- 31.Daoud N, Soskolne V, Mindell JS, Roth MA, Manor O. Ethnic inequalities in health between Arabs and Jews in Israel: the relative contribution of individual-level factors and the living environment. Int J Public Health. 2018;63(3):313–323. doi: 10.1007/s00038-017-1065-3. [DOI] [PubMed] [Google Scholar]
- 32.Levin-Zamir D, Baron-Epel OB, Cohen V, Elhayany A. The association of health literacy with health behavior, socioeconomic indicators, and self-assessed health from a national adult survey in Israel. J Health Commun. 2016;21(Suppl. 2):61–68. doi: 10.1080/10810730.2016.1207115. [DOI] [PubMed] [Google Scholar]
- 33.Chernichovsky D, Bisharat B, Bowers L, Brill A, Sharony C. The health of the Arab Israeli population. State Nation Report 2017. https://www.taubcenter.org.il/wp-content/files_mf/healthofthearabisraelipopulation.pdf
- 34.Gilles I, Bangerter A, Clémence A, et al. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur J Epidemiol. 2011;26(3):203–210. doi: 10.1007/s10654-011-9577-2. [DOI] [PubMed] [Google Scholar]
- 35.Quinn SC, Parmer J, Freimuth VS, Hilyard KM, Musa D, Kim KH. Exploring communication, trust in government, and vaccination intention later in the 2009 H1N1 pandemic: results of a national survey. Biosecur Bioterror. 2013;11(2):96–106. doi: 10.1089/bsp.2012.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siegrist M, Zingg A. The role of public trust during pandemics: implications for crisis communication. Eur Psychol. 2014;19(1):23–32. doi: 10.1027/1016-9040/a000169. [DOI] [Google Scholar]
- 37.Teufel M, Schweda A, Dörrie N, et al. Not all world leaders use Twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J Public Health. 2020;42(3):644–646. doi: 10.1093/pubmed/fdaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khosravi M. Perceived risk of COVID-19 pandemic: the role of public worry and trust. Electron J Gen Med. 2020;17(4):em203. doi: 10.29333/ejgm/7856. [DOI] [Google Scholar]
- 39.Blair RA, Morse BS, Tsai LL. Public health and public trust: survey evidence from the Ebola virus disease epidemic in Liberia. Soc Sci Med. 2017;172:89–97. doi: 10.1016/j.socscimed.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 40.Vinck P, Pham PN, Bindu K, Bedford J, Nilles EJ. Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis. 2019;19(5):529–536. doi: 10.1016/S1473-3099(19)30063-5. [DOI] [PubMed] [Google Scholar]
- 41.Bord S, Schor A, Satran C, Ali Saleh O, Inchi L, Halperin D. Distancing adherence and negative emotions among the Israeli elderly population during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(16):8770. doi: 10.3390/ijerph18168770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Block R, Jr, Berg A, Lennon RP, Miller EL, Nunez-Smith M. African American adherence to COVID-19 public health recommendations. Health Lit Res Pract. 2020;4(3):e166–e170. doi: 10.3928/24748307-20200707-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lavie E, Elran M, Sawaed A, Moch M, Dallashi M. Israel’s Arab society and the coronavirus challenge. INSS Insight 2020;1288:1–5. https://www.inss.org.il/publication/coronavirus-and-the-israeli-arabs/
- 44.Brik S. The dark side of Gamzu’s plan. 2020. https://www.haaretz.co.il/debate/hebrew/1.9122135 [accessed 3 September 2020]
- 45.Terry DJ, Gallois C, McCamish M. (Eds.). The theory of reasoned action: its application to AIDS-preventive behavior. Abingdon-on-Thames: Routledge, 2015. https://www.routledge.com/The-Theory-of-Reasoned-Action-Its-application-to-AIDS-Preventive-Behaviour/Gallois-McCamish-Terry/p/book/9780415861823 [accessed 03 May 2020]
- 46.Ajzen I, Fishbein M. A Bayesian analysis of attribution processes. Psychol Bull. 1975;82(2):261–277. doi: 10.1037/h0076477. [DOI] [Google Scholar]
- 47.Prasetyo YT, Castillo AM, Salonga LJ, Sia JA, Seneta JA. Factors affecting perceived effectiveness of COVID-19 prevention measures among Filipinos during enhanced community quarantine in Luzon, Philippines: integrating protection motivation theory and extended theory of planned behavior. Int J Infect Dis. 2020;99:312–323. doi: 10.1016/j.ijid.2020.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Egede LE, Ellis C. Development and testing of the multidimensional trust in health care systems scale. J Gen Intern Med. 2008;23(6):808–15. doi: 10.1007/s11606-008-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nelms E, Wang L, Pennell M, et al. Trust in physicians among rural Medicaid-enrolled smokers. J Rural Health. 2014;30(2):214–220. doi: 10.1111/jrh.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 51.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs: Prentice-Hall; 1980. [Google Scholar]
- 52.Ajzen I, Madden JT. Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. J Exp Soc Psychol. 1986;22(5):453–474. doi: 10.1016/0022-1031(86)90045-4. [DOI] [Google Scholar]
- 53.World Health Organization. Pandemic fatigue: reinvigorating the public to prevent COVID-19: policy framework for supporting pandemic prevention and management: revised version November 2020 (No. WHO/EURO: 2020–1573–41324–56242). https://apps.who.int/iris/bitstream/handle/10665/337574/WHO-EURO-2020-1573-41324-56242-eng.pdf?sequence=1&isAllowed=y [accessed 3 May 2020]
- 54.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Press; 2018. [Google Scholar]
- 55.Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner CP, Gerger H. Trust in the health care professional and health outcome: a meta-analysis. PLoS ONE. 2017;12:e0170988. doi: 10.1371/journal.pone.0170988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soltan EM, El-Zoghby SM, Salama HM. Knowledge, risk perception, and preventive behaviors related to COVID-19 pandemic among undergraduate medical students in Egypt. SN Compr Clin Med. 2020;2(12):2568–2575. doi: 10.1007/s42399-020-00640-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khasawneh AI, Humeidan AA, Alsulaiman JW, Bloukh S, Ramadan M, Al-Shatanawi TN, et al. Medical students and COVID-19: knowledge, attitudes, and precautionary measures: a descriptive study from Jordan. Front Public Health. 2020;8(3):253–269. doi: 10.3389/fpubh.2020.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khalil NS, Al-Yuzbaki DB, Tawfeeq RS. COVID-19 knowledge, attitude and practice among medical undergraduate students in Baghdad city. Eurasian J Biosci. 2020;14(2):4179–4186. [Google Scholar]
- 59.Satran C, Ali-Saleh O, Mashiach-Eizenberg M, Bord S. Stress and perceived discrimination among the Arab population in Israel: the mediation role of the perceived COVID-19 threat and trust in the healthcare system. Ethn Health 2021;1–18. Online ahead of print. 10.1080/13557859.2021.1899139 [DOI] [PubMed]
- 60.Saban M, Shachar TA, Miron O, et al. Effect of socioeconomic and ethnic characteristics on COVID-19 infection: the case of the ultra-orthodox and the Arab communities in Israel. J Racial Ethn Health Disparities. 2020;9:581–588. doi: 10.1007/s40615-021-00991-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li DJ, Ko NY, Chang YP, Yen CF, Chen YL. Mediating effects of risk perception on association between social support and coping with COVID-19: an online survey. Int J Environ Res Public Health. 2021;18(4):1550. doi: 10.3390/ijerph18041550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Franzen A, Wöhner F. Fatigue during the COVID-19 pandemic: evidence of social distancing adherence from a panel study of young adults in Switzerland. PLoS ONE. 2021;16(12):e0261276. doi: 10.1371/journal.pone.0261276. [DOI] [PMC free article] [PubMed] [Google Scholar]