Abstract
Objective During the coronavirus disease 2019 pandemic, as a safety-net organization with a substantial percentage of patients of color and with limited English proficiency (LEP), we were wary of furthering health disparities in our community. We analyzed gaps in telemedicine (telephone and video) delivery in our communities, quantified the effects of our tests of change, and began the process of accumulating evidence to create a road map for other organizations.
Methods We leveraged Lean problem-solving strategies to identify modifiable gaps across multiple domains that could inhibit equity in telemedicine. We implemented tests of change across domains of community engagement, technology, education, and access. We observed the proportion of telemedicine encounters across races and languages between April and November, 2020. Regression analyses tested the impact of race and language on telemedicine controlling for age, gender, insurance, and time.
Results Several rounds of changes and enhancements were associated with changes in telemedicine use of +5.5% ( p < 0.0001) for Hispanic, +4.0% ( p < 0.0001) for Spanish-speaking, −2.1% for Black ( p < 0.05), and −4.4% for White patients ( p < 0.001). African-American, Hispanic, and non-English-speaking patients had between 2.3 and 4.6 times the odds of preferring telephone to video encounters ( p < 0.0001), with increases in preferences for video use over time ( p < 0.05).
Conclusion Our roadmap to improve equitable delivery of telemedicine was associated with a significant improvement in telemedicine use among certain minority populations. Most populations of color used telephone more often than video. This preference changed over time and with equity-focused changes in telemedicine delivery.
Keywords: telemedicine, equity, Lean methods, minority populations, telemedicine and telehealth, implementation and deployment, outcome and process assessment, people, economic barriers (digital divide)
Background and Significance
The coronavirus disease 2019 (COVID-19) pandemic has changed the way health care is delivered in many ways. One of these is the broad adoption of telemedicine to more efficiently deliver care. There were several components that led to the broader adoption of telemedicine, including policy waivers by Centers for Medicare and Medicate Services that led to Medicare, Medicaid, and Children's Health Insurance Program offering payment for video and telephone encounters akin to what was already reimbursed by private insurance payers for video visits over the past many years. 1 Many private insurers subsequently included reimbursement for audio-only encounters taking place by telephone. Telemedicine, thus, became a viable option for many persons of color and limited English proficiency (LEP), who were now able to quickly, efficiently, and affordably access care. Due to the rapid uptake of telemedicine, health care systems were forced to build telemedicine platforms in a short period of time, often taking a “prefabricated” approach from electronic health record (EHR) developers relying on patient portals and singular pathways of connection. However, these types of services inherently disadvantage those with LEP or limited technical literacy. 2 These were some of the reasons our safety net organization had not previously pursued more robust telemedicine platforms.
Hennepin Healthcare System (HHS) is the largest safety net organization in Minnesota. In total, 60% of our patient population are persons of color, 9% have experienced homelessness, and 54% of our patients suffer from substance use or mental illness. 3 When the COVID-19 pandemic began, our health care system, like many others, felt the stress of an inability to contact our patients with clinic services temporarily closed. As we started to design processes and infrastructure around our telemedicine platform, we did so with equity (both equal access and usability) at the forefront of the conversation. As our telemedicine platform has matured, so has our ability to provide this modality of care in a more equitable fashion. Through Lean-focused process examination and careful observation with feedback from patients and staff, we have built a system that seeks to provide equitable health care by leveraging the advantages inherent in telemedicine: that is, improving basic access to affordable, high-quality health care. 4 5 Through this work, we have developed strategies and guidelines that may help health care organizations deliver telemedicine in ways that improve health equity rather than fueling further disparities. 6 7
The issue of equitable use of health care modalities (such as telemedicine) is of great importance to HHS, with 60% of our patients being persons of color. For reference, the 2010 U.S. Census declares that 63.8% of the population in Minneapolis, MN (where HHS resides) defined themselves as White. 8 In addition, only 73.5% of ambulatory encounters in these clinics were performed with English as the primary language, giving us one of the largest LEP patient populations in Minnesota. Because of the large populations of persons of color and patients with LEP, telemedicine seemed to contain too many barriers to be efficacious. One significant barrier was reimbursement, as HHS has one of the largest percentages of Medicaid patients in Minnesota. This barrier was broken down after Federal and State legislation provided funds for telemedicine reimbursement. The next barrier was the perception around access to the technology needed to participate in telemedicine 9 Other research has examined the role that general and technical literacy play in patients' ability to leverage technology to connect with health care providers. 10 Researchers at HHS studied the impact these factors would have on our community should telemedicine become a prominent mode of care delivery. A community needs survey examined (1) availability of technology needed to access care via video (internet-enabled device with a camera and access to broadband connection) and (2) our patents' willingness to receive health care via this modality. In a diverse cohort of respondents (including race, language, and homelessness), this was 89% (available) and 72% (willing), respectively. 11 With this information, our operations teams felt confident that telemedicine platforms should not be the insurmountable barriers they were previously felt to be. Like many health care systems, ours was asked to quickly deploy a telemedicine platform. We suspected that despite reliance on the patient portal and its inherent limitations, along with poor community awareness around telehealth, the process being deployed would still have the potential to deliver care equitably across our patient populations.
Objectives
This project began as an operational initiative to assure that we were striving for equitable delivery of care regardless of delivery modality. We defined equity as the unimpeded access to care irrespective of whatever demographic group one falls into. With the aforementioned characteristics of our patient population, there was apprehension about the ability to deliver telemedicine care equitably; telemedicine has been presumed to be challenging both at the delivery end (providers unaware and systems not well designed) and at the patient end (difficult for patients with less access to electronic technologies such as smartphones or patient portals). We focused on synchronous telemedicine modalities (telephone and video). Our objective was to quantify the equity of telemedicine delivery across races and languages so we could design interventions to improve equity. In particular, we analyzed gaps in equitable telemedicine (telephone and video) delivery, quantified the effects of our tests of change, and developed an evidence-based road map for other organizations. Our hypothesis was that these interventions would improve equitable care delivery, thus setting the stage for randomized controlled trials. After completing interventions and interval change analyses, we coalesced findings into a blueprint for the replication of our efforts by organizations struggling to deliver equitable care.
Methods
Thinking Lean
An important component of better understanding equity work is to be sure the perspectives of the patient populations being studied are accurately accounted for. We relied on Lean problem-solving strategies to understand the challenges in creating health equity in telemedicine care delivery. The key components of Lean methods used included the following: (1) several series of gap analyses, through interviews and observations, to examine root causes limiting more persons of color participating in telemedicine, (2) development of a fishbone diagram ( Fig. 1 ) that highlights key areas warranting particular focus around the provision of equitable telemedicine, and (3) deploying tests of change along all facets of the telemedicine patient experience including community awareness, scheduling, connecting and provider development ( Fig. 2 ).
Fig. 1.
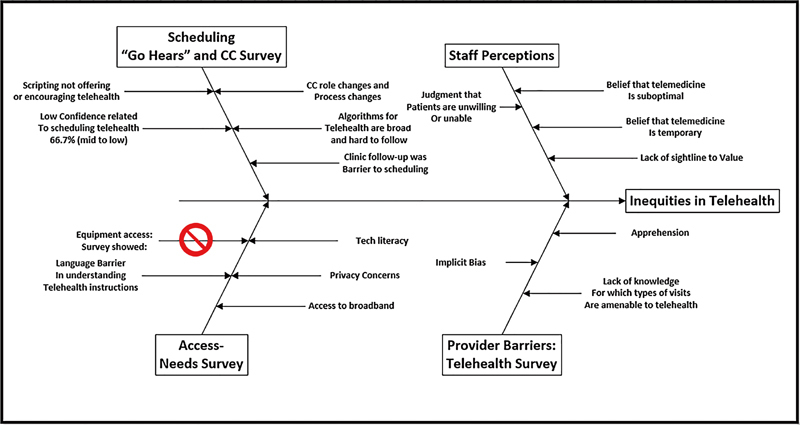
Key areas of focus for provision of equitable telemedicine.
Fig. 2.
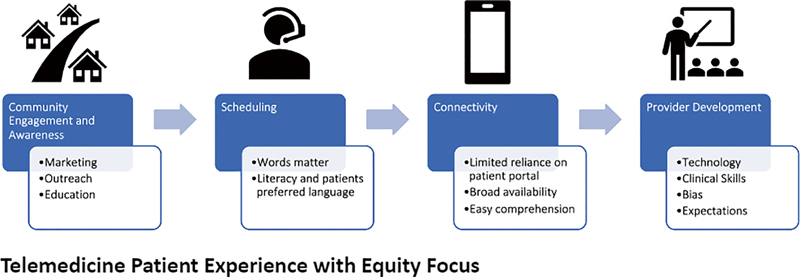
Roadmap to a more equitable telemedicine platform.
Community Awareness
The first area of focus was around the communities' awareness and knowledge of telemedicine. Part of our gap analysis included listening to recordings of patients attempting to schedule telemedicine visits. Analyses of these observations demonstrated a trend that if patients don't ask for telemedicine appointments, they are not typically scheduled for them. Most marketing at our organization is generally deployed in English. Knowing that many of our patients had no knowledge of telemedicine, we needed a way for patients to quickly access easily understandable information around this new care modality. We redesigned our public-facing Web site regarding telemedicine to include a toolkit. 12 The toolkit entailed a static document and videos defining telemedicine with detailed, step-by-step instructions on how to connect. The content was written maintaining a fourth grade literacy level and later translated into Spanish and Somali (the two predominant non-English languages in our community). The content was housed on a Web site that allows the viewer to select their preferred language resulting in the translation of all text-based content to any of the 16 languages we have as options.
Scheduling
The next phase of process improvement focused on scheduling of telemedicine visits via our connection center (CC), where patients are scheduled for upcoming visits. Through dozens of recorded observations, we elucidated that the words used to describe telemedicine matter to patients faced with deciding on how their care is delivered. Previously, the word “virtual” was used to describe both video and telephone visits. After conversations with our patients, interpreter services, and CC staff, we developed a revised script to describe and offer telemedicine to patients who may not have experienced it previously. The revised script kept in mind the general literacy level of the audience and the ability to easily translate these words into non-English languages.
Connecting via Telemedicine
One of the more crucial pieces of delivering equitable telemedicine is developing software that allows for the broadest reach without presenting barriers that fuel inequity. Patient portals have long been the primary method of connecting patients to video visits. Typically, patient portals are developed only in English and proficiency with these tools requires technical literacy. 13 We, thus, developed multiple pathways to access video visits. A custom solution was built to deploy a video visit solution that was fully integrated into the EHR that did not rely on the patient portal to establish access. This system developed a unique meeting ID upon scheduling a video visit. The hyperlink to access this meeting was pushed to the patient via SMS text message or email at the time of the visit with automatic translation into the patient's preferred language (Spanish, Somali or English). This allowed for “one-click connection” without the need for special accounts or software.
Supporting the Staff
We then focused our attention on providers who would staff the telemedicine appointments. Given the current gap in medical education around telemedicine, 14 we supported providers technically and also educated them on changes in their clinical workflows. We felt it was important to highlight areas in which telemedicine encounters were unique in comparison to face-to-face visits while acknowledging that most providers have never practiced telemedicine. Highlighting topics such as “webside” manner, expectation setting, tele-exam, and telediagnosis prepared our clinical team for telemedicine encounters. These efforts extended to graduate medical education cohorts through faculty providers. In conjunction with these efforts, we focused on sewing in the storyline of access equals equity and that, if designed accordingly, telemedicine can improve access to health care.
Data Collection and Analyses
Between April and November 2020, many improvements were rolled out in a staggered pattern across the various ambulatory care centers with the goal of improving equitable access to telemedicine visits. We used face-to-face encounters as a benchmark for current access to care within our health care system. Patient and visit data were collected from our EHR system. Patients self-reported their primary race when registering as either White, Black, Asian, Hispanic, or other. We identified all face-to-face and telemedicine visits from April 1st 2020 to November 30th 2020 across all ambulatory departments, excluding missed appointments and cancellations. Telemedicine visits were limited to telephone and video visits. Visits with patients who declined having their data used for research studies when registering were removed from the dataset. Statistical analyses were performed using SAS Enterprise Guide version 4.3. Chi-squared statistics determined differences between categorical variables. Multivariable modeling was performed to assess telemedicine use in different age categories and to determine the impact of race on using telephone versus video modality for the visit, controlling for age gender, insurance coverage, and time period. Statistical significance was measured at values ≤0.05
The project was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research In Human Subjects. The study was determined to be quality improvement and not subject to full Institutional Review Board review at our organization.
Results
Table 1 shows the demographics of patients seen during the study period. The analyses included 98,357 unique patients seen by any delivery modality between April and November of 2020. Fewer older patients (>65) and fewer patients without portal access participated in telemedicine.
Table 1. Patient characteristics.
| Patients with a telemedicine visit a | |||
|---|---|---|---|
| Characteristic | Patients with any visit (in-person ortelemedicine) during the study period | Telephone visit | Video visit |
| Sample size | 98,357 | 11,857 | 7,916 |
| Age in years | |||
| <18 | 17,649 (17.9%) | 667 (5.6%) | 831 (10.5%) |
| 18–44 | 47,217 (48.0%) | 4,527 (38.2%) | 3,856 (48.7%) |
| 45–64 | 24,138 (24.5%) | 4,362 (36.8%) | 2,108 (26.6%) |
| ≥65 | 9,353 (9.5%) | 2,301 (19.4%) | 1,121 (14.2%) |
| Language | |||
| English | 72,267 (73.5%) | 9,517 (80.3%) | 7,304 (92.3%) |
| Spanish | 14,596 (14.8%) | 1,606 (13.5%) | 461 (5.8%) |
| Somali | 3,465 (3.5%) | 400 (3.4%) | 72 (0.9%) |
| Other | 8,029 (8.2%) | 334 (2.8%) | 79 (1.0%) |
| MyChart (portal) status | |||
| Activated | 65,481 (66.6%) | 7,408 (62.5%) | 6,837 (86.4%) |
| Race | |||
| Asian | 3,900 (4.0%) | 364 (3.1%) | 270 (3.4%) |
| Black (African American or African) | 25,929 (26.4%) | 4,364 (36.8%) | 2,046 (25.8%) |
| Hispanic (Latino) | 19,611 (19.9%) | 2,124 (17.9%) | 921 (11.6%) |
| Other | 10,608 (10.8%) | 317 (2.7%) | 168 (2.1%) |
| White (Caucasian, Non-Hispanic) | 38,309 (38.9%) | 4,688 (39.5%) | 4,511 (57.0%) |
| Sex | |||
| Female | 51,065 (51.9%) | 6,672 (56.3%) | 4,489 (56.7%) |
| Insurance product | |||
| Commercial | 37,823 (38.5%) | 3,110 (26.2%) | 3,242 (41.0%) |
| Medicaid | 30,115 (30.6%) | 4,252 (35.9%) | 2,633 (33.3%) |
| Medicare | 10,540 (10.7%) | 3,186 (26.9%) | 1,434 (18.1%) |
| MNCare b | 3,496 (3.6%) | 500 (4.2%) | 267 (3.4%) |
| Other | 6,652 (6.8%) | 154 (1.3%) | 223 (2.8%) |
| Self/Unknown | 18,082 (18.4%) | 994 (8.4%) | 366 (4.6%) |
Patients who had a telephone and a video visit were counted in both columns.
MNCare is a health plan available to low-income Minnesotans who do not qualify for medical assistance.
As it relates to race ( Fig. 3 ), prior to any intervention, we saw that telemedicine visits for White, Black, and Hispanic populations were 53, 30, and 11%, respectively ( n = 3,366). This was a notable deviation from the number of face-to-face visits during that time (34, 37, and 19% n = 8,576). These discrepancies were even more prevalent in terms of language ( Fig. 4 ) with English-speaking, Spanish-speaking, and Somali-speaking patients comprising 90, 7, and 1% of telemedicine visits in April 2020, respectively. Over the period of time in which we deployed multiple tests of change with the intention of improving equity, we saw significant changes in the frequency of telemedicine visits in multiple demographics. In November 2020 White, Black, and Hispanic populations accounted for 50, 28, and 17% of telemedicine visits, respectively ( n = 3,640). There was a statistically significant percent change of −3.76 ( p = 0.0004), −2.11 ( p = 0.0295), and +5.48% ( p < 0.0001) respectively compared with baseline ( Table 2 ). Similar changes were seen with language showing a percent change from April to November of 2020 of –4.3, +3.98, +0.18% for English-speaking, Spanish-speaking, and Somali-speaking patients, respectively demonstrating statistical significance for English and Spanish speakers ( p < 0.0001).
Fig. 3.
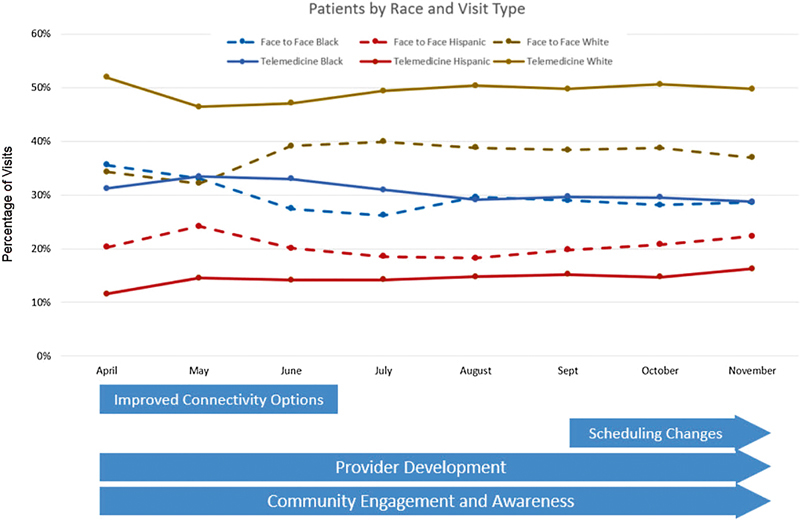
Percentage of visits by race in face-to-face visits and telemedicine visits.
Fig. 4.
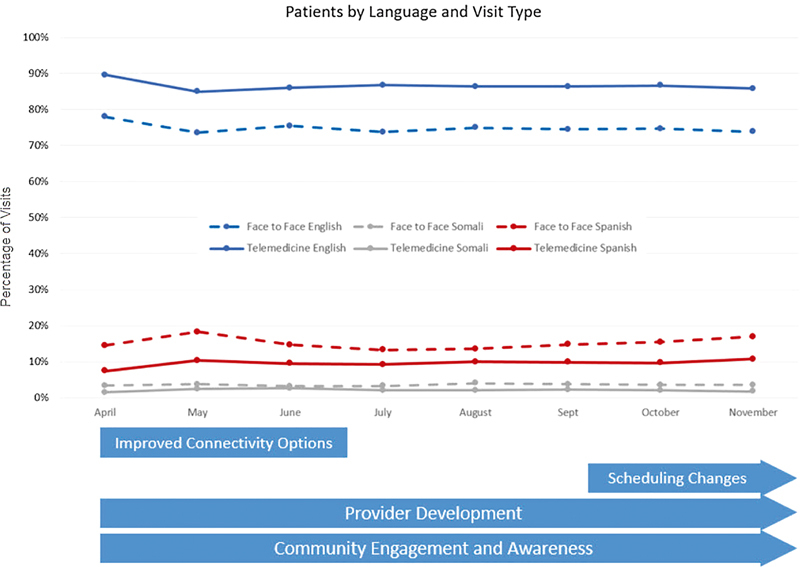
Percentage of visits by language in face-to-face visits and telemedicine visits.
Table 2. Differences in the use of telemedicine visits.
| Demographic variable | April 2020 | November 2020 | Change in percentage | ||
|---|---|---|---|---|---|
| Number of telemedicine visits | Percent of telemedicine visits ( n = 4,055) | Number of telemedicine visits | Percent of telemedicine visits ( n = 4,729) | ||
| Race | |||||
| Asian | 86 | 2.1% | 124 | 2.6% | 0.5% |
| Black (African American or African) | 1,228 | 30.3% | 1,332 | 28.2% | −2.1% a |
| Hispanic (Latino) | 450 | 11.1% | 784 | 16.6% | 5.5% a |
| White (Caucasian, Non-Hispanic) | 2,165 | 53.4% | 2,347 | 49.6% | −3.8% a |
| Language | |||||
| English | 3,669 | 90.5% | 4,071 | 86.1% | −4.4% a |
| Spanish | 277 | 6.8% | 511 | 10.8% | 4.0% a |
| Somali | 56 | 1.4% | 74 | 1.6% | 0.2% |
p < 0.05.
When looking at age categories within different race and language demographic groups ( Table 3 ), we found that the most notable changes in the percentage of telemedicine encounters (telephone plus video) from April to November 2020 were in the 18 to 44 year age category in Black, Hispanic, English, and Spanish demographic groups ( p 's < 0.05). A significant increase in telemedicine use was also seen in Hispanic patients <18 years old (odds ratio [OR] 1.76, p < 0.05).
Table 3. Change in telemedicine use from April to November 2020 across race and language broken down into age categories.
|
Notes: Yellow boxes indicate those reaching statistical significance of p < 0.05.
Notes: Multivariate logistic regression run by each race or language separately, controlling for race, language, age, gender, insurance, and time.
In terms of the odds of choosing telephone versus video ( Table 4 ), most non-Whites, non-English-speaking demographic groups carried a higher likelihood of relying on telephone versus video. Non-English-speaking patients had the highest likelihood (OR 4.62, p < 0.0001) to choose telephone. Preference for telephone over video was also shown for African-American and Hispanic patients, Medicare and Medicaid users, and older patients (all p 's < 0.0001). These multivariate models also showed that over time, there was a significant increase in several groups' preference for video visits.
Table 4. Likelihood of using telephone versus video in patients with telemedicine visits.
| Odds ratio estimates | ||||
|---|---|---|---|---|
| Effect | Odds ratio | 95% | p -Value | |
| Confidence intervals | ||||
| Black | 3.512 | 3.013 | 4.094 | <0.0001 |
| Hispanic | 2.35 | 1.753 | 3.149 | <0.0001 |
| Asian | 1.607 | 0.987 | 2.617 | 0.0564 |
| Non-English Speaking | 4.624 | 3.333 | 6.414 | <0.0001 |
| Medicaid | 1.308 | 1.173 | 1.459 | <0.0001 |
| Medicare | 1.346 | 1.176 | 1.541 | <0.0001 |
| All patients in November | 1.858 | 1.636 | 2.111 | <0.0001 |
| Female | 0.935 | 0.853 | 1.026 | 0.1571 |
| Age | 1.023 | 1.02 | 1.026 | <0.0001 |
| Black in November | 0.638 | 0.518 | 0.786 | <0.0001 |
| Hispanic in November | 0.638 | 0.441 | 0.925 | 0.0176 |
| Asian in November | 0.905 | 0.485 | 1.687 | 0.7523 |
| Non-English in November | 0.514 | 0.341 | 0.774 | 0.0015 |
Notes: Multivariable logistic regression model defined likelihood of using telephone for telemed encounter versus video (outcome) with race as predictor, controlling for age, gender, insurance coverage, and time period.
Discussion
In this preliminary study of diverse patients in a safety net setting during 8 months of the COVID-19 pandemic, we found that commitment to telehealth equity using several basic assumptions and methods was associated with an increased percentage of Hispanic and Spanish-speaking patients participating in telemedicine visits. Our team set out to demonstrate that with an emphasis on equity, a health care organization with a diverse and underserved patient population could deliver care more equitably via telemedicine across certain racial and language demographics. While we have not fully achieved our goal of equitable access to telemedicine, we have shown that with thoughtful design and process analysis, it is possible to move the needle closer to the benchmarks established by face-to-face visits within those same populations.
Over the past year, much has been published around the advancement and explosion of telemedicine as a modality of care delivery. 15 16 Historically, much has been studied around telemedicine as it relates to health care disparities among rural patient populations. Telemedicine as a platform has only recently become a phenomenon among the urban patient populations. Thus, there are fewer examinations of its effect on the urban underserved. It has only been in the past several months that we have begun to see more publications highlighting the inequities that have been observed with rapid telemedicine rollouts across urban health care organizations. 17 18 Many of those studies have identified the areas of need for future research, advocacy, and consideration. To our knowledge, when this article was initially written this is the first study that outlines an evidence-based roadmap to more equitable telemedicine access. Our hope is that this work will further highlight the inequities among patients attempting to access telemedicine while providing a framework for organizations to address these disparities.
Figs. 3 and 4 show that over time we were able to realize an expansion of telemedicine adoption within our Hispanic and Spanish-speaking communities. While it is reasonable to expect that these communities would be slower to adopt telemedicine given their limited exposure to this delivery modality, the expansion tracks well with our organizational efforts and deployed tests of change. This demonstrates that reliance on a “one size fits all” solution to telemedicine may be contributing to progressive disparities highlighting the digital divide in those communities. Our results suggest that solutions embracing multilingual support can provide new opportunities to expand access to health care. These figures also show that we did not make significant improvements within the Black communities regarding access to telemedicine. One of the likely reasons for this is that Black as a racial category is monolithic and not representative of the communities in which those patients reside. The Twin Cities area is home to a large English-speaking and non-English-speaking Somali population in addition to African-American communities. The cultural gaps between these two ethnicities are sizeable and likely warrant different solutions to further telemedicine adoption. As we move forward with this research, we need better capture of patient ethnicity in the EHR rather than monolithic racial categorizations.
Interestingly, we found most of the uptake in telemedicine was within the 18 to 44 year-old range, as well as the pediatric Hispanic population. This may reflect more comfort with technology and higher levels of digital literacy. Future research will be needed to determine if different interventions are needed for different age groups and ethnicities
There are multiple modalities within telemedicine, most notably telephone and video. There continues to be debate around the appropriate clinical applications of these modalities. The data displayed in Table 4 demonstrate findings consistent with results published elsewhere in that minority populations are more reliant on telephone when accessing care via telemedicine. 19 This highlights the importance of maintaining the telephone as a viable option that is reimbursed outside of the public health emergency. This also highlights the importance of better evaluating and understanding what keeps these groups from accessing telemedicine via video at rates comparable to their white, English-speaking peers. Digital literacy levels and lack of access to instructions in their native language may be reasons why Non-English speaking patients prefer telephone. The significant increase in video use with time in many minority populations may reflect our focus on improving access in this manner but will await further comparison trials to ascertain if these interventions did indeed lead to this change. We view our study and the roadmap generated from it as a first step toward fixing these inequities.
Fig. 2 outlines the roadmap that our organization developed to deliver a more equitable telemedicine platform. This figure aims to highlight key areas across the spectrum of the patient experience related to telemedicine access that we feel are crucial to the success of equitable care delivery. This roadmap was designed with reproducibility in mind. No piece of this roadmap is specific to any individual race, ethnic group, or language; rather, we provide broad recommendations that can be applied to any community seeking to design a more equitably distributed and utilized telemedicine platform.
There are limitations to our work. First, face-to-face visits may not be the best marker for equity as we know that these are fraught with discrepancies among minority populations. 20 Without a more robust public health analysis, we did not feel confident establishing these benchmarks based on existing data. 19 21 Next, this project was initially designed with intention of driving organizational goals around equity and access to care during the pandemic. Because of this, many of our interventions overlap and have continued to evolve and increase in scope. This design makes more robust analysis around the discrete contributions of specific interventions more difficult. Lastly, there are several confounding variables that may be contributing to the changes in telemedicine volumes that we saw during the study period. These include increased public awareness and familiarity of this modality along with increased pressure to stay socially distant during surges in the COVID-19 pandemic. While the gains we saw across various demographics were statistically significant, they were modest changes in comparison to the equity gaps that exist. Because of these limitations and potential confounders, further research and randomized controlled trials will be needed to elicit any degree of causation regarding these interventions' ability to improve equitable access to telemedicine.
Conclusion
While telemedicine as a means of delivering high-quality health care is not novel, the broad availability in urban communities of persons of color and those with LEP is a new development. Without careful examination of processes and the technologies behind them, this modality has the potential to broaden health care disparities already present among communities of color. We have demonstrated several Lean-process improvements aiming to establish telemedicine programs in a more equitable manner. In two related communities, those of Hispanic and Spanish-speaking patients, we have shown some early success. We present evidence upon which others can construct their own roadmaps for building systems with more equitable delivery of telemedicine. Despite our efforts, there remains a sizeable gap in the equitable distribution of telemedicine and careful attention should be paid to what modality of telemedicine patients are selecting. We believe telemedicine should be viewed as a means to break down access barriers to health care and a tool used to further the goal of broad health care equity across our communities. Future studies are required to rewrite the narrative around telemedicine as a tool to drive health equity rather than just another technological advancement in health care.
Clinical Relevance Statement
As telemedicine becomes more common as a means of providing quality medical care, health care providers and organizations will need to be mindful that it is being made available in an equitable manner. The digital divide is already present in our country and has the potential to broaden health care disparities. The research shows the value and importance of emphasizing equity in informatics work as it relates to accessing health care.
Multiple Choice Questions
-
Which community (race or language) saw the largest positive impact in the provision of equity-focused design around the provision of telemedicine in this research?
Black
Hispanic
Somali
Native American
Correct Answer: The correct answer is option b. The Hispanic and Spanish-speaking populations were the communities in which we found a significant change in how frequently telemedicine was used. We feel that many of our efforts to make telemedicine more accessible resonated well in those communities where the barriers addressed in this paper are covered. The inclusion of other languages to much of our marketing and education work resonates well with Spanish-speaking communities who often are not afforded access to these materials. While we did not see significant positive growth in Black populations, we postulate that this is largely due to the monolithic categorization of this racial group. In our communities, we have several different African immigrant communities that have very different needs and pose very different health equity challenges than our African American ethnic groups. Better capture and reporting mechanisms of ethnicity are needed to obtain more nuanced data that will allow health care organizations to solve these dilemmas.
-
Which of the following was NOT a strategy utilized in the roadmap to equitable telemedicine delivery researched by this organization?
The availability of alternate pathways that do not require the use of patient portals
Care use of language when introducing telemedicine to patients for the first time
Incentives to minority populations to try telemedicine for the first time
Toolkits designed to bridge tech literacy gaps available in multiple languages
Correct Answer: The correct answer is option c. No incentives were given to any populations in this retrospective analysis. Our informatics and operations teams made changes to our telemedicine workflows that we felt would maximize the equitable delivery of telemedicine. These strategies included the other answer choices and are further detailed in Fig. 2 .
Funding Statement
Funding M.L. is supported in his work in burnout reduction through the National Institutes of Health.
Conflict of Interest None declared.
Protection of Human and Animal Subjects
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects. This work was determined to be quality improvement work and not subject to full IRB review at our organization.
References
- 1.Medicare Telemedicine Health Care Provider Fact Sheet | CMSPublished January 20, 2021. Accessed January 20, 2021 at:https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 2.Antonio M G, Petrovskaya O, Lau F.Is research on patient portals attuned to health equity? A scoping review J Am Med Inform Assoc 201926(8-9):871–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garrett N, Bikah Bi Nguema Engoang J A, Rubin S, Vickery K D, Winkelman T NA. Health system resource use among populations with complex social and behavioral needs in an urban, safety-net health system. Healthc (Amst) 2020;8(03):100448. doi: 10.1016/j.hjdsi.2020.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batsis J A, DiMilia P R, Seo L M. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019;67(08):1737–1749. doi: 10.1111/jgs.15959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khairat S, Haithcoat T, Liu S.Advancing health equity and access using telemedicine: a geospatial assessment J Am Med Inform Assoc 201926(8–9):796–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaffe D H, Lee L, Huynh S, Haskell T P. Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag. 2020;23(05):368–377. doi: 10.1089/pop.2020.0186. [DOI] [PubMed] [Google Scholar]
- 7.Ye S, Kronish I, Fleck E. Telemedicine expansion during the COVID-19 pandemic and the potential for technology-driven disparities. J Gen Intern Med. 2021;36(01):256–258. doi: 10.1007/s11606-020-06322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United States Census Bureau 2010 Census United States Census BureauAccessed January 21, 2021. Accessed May 05, 2022 at:https://data.census.gov/cedsci/
- 9.Bommakanti K K, Smith L L, Liu L. Requiring smartphone ownership for mHealth interventions: who could be left out? BMC Public Health. 2020;20(01):81. doi: 10.1186/s12889-019-7892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey S C, O'Conor R, Bojarski E A. Literacy disparities in patient access and health-related use of Internet and mobile technologies. Health Expect. 2015;18(06):3079–3087. doi: 10.1111/hex.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Covid-10 Impact and Basic Needs Survey. Hennepin Healthcare 2020. Accessed January 20, 2021 at:https://hennepinhealthcare.org/wp-content/uploads/2020/09/COVID_Results_Packet_R10_Final.pdf
- 12.Hennepin Healthcare Video Visits Landing page and ToolkitsAccessed May 05, 2022 at:Hennepinhealthcare.org/videovisits
- 13.Casillas A, Abhat A, Mahajan A. Portals of change: How patient portals will ultimately work for safety net populations. J Med Internet Res. 2020;22(10):e16835. doi: 10.2196/16835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rutledge C, Hawkins E J, Bordelon M, Gustin T S. Telehealth education: An interprofessional online immersion experience in response to COVID-19. J Nurs Educ. 2020;59(10):570–576. doi: 10.3928/01484834-20200921-06. [DOI] [PubMed] [Google Scholar]
- 15.Patel S Y, Mehrotra A, Huskamp H A, Uscher-Pines L, Ganguli I, Barnett M L. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood) 2021;40(02):349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eberly L A, Kallan M J, Julien H M. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chunara R, Zhao Y, Chen J. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28(01):33–41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilson S F, Umscheid C A, Laiteerapong N, Ossey G, Nunes K J, Shah S D. Growth of ambulatory virtual visits and differential use by patient sociodemographics at one urban academic medical center during the COVID-19 pandemic: Retrospective analysis. JMIR Med Inform. 2020;8(12):e24544. doi: 10.2196/24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez J A, Betancourt J R, Sequist T D, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(01):21–26. doi: 10.37765/ajmc.2021.88573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franks P, Fiscella K, Meldrum S. Racial disparities in the content of primary care office visits. J Gen Intern Med. 2005;20(07):599–603. doi: 10.1111/j.1525-1497.2005.0109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinsky C, Linzer M. Practice and policy reset post-COVID-19: reversion, transition, or transformation? Health Aff (Millwood) 2020;39(08):1405–1411. doi: 10.1377/hlthaff.2020.00612. [DOI] [PubMed] [Google Scholar]


