Abstract
Simple Summary
Acute myeloid leukemia (AML) is the most common blood cancer in the elderly, which progresses rapidly and is often fatal. The prognosis for AML remains poor in most older patients: only about 15% of patients over 60 years of age can recover. Our aim is to determine new potential AML clinical treatment prognosis markers. We analyzed certain genes, proteins and the epigenome profile in therapy-resistant and responsive AML patients at diagnosis stage and after clinical treatment. We determined that MYC, WT1, IDH1, CDKN1A, HDAC2, TET1, KAT6A and GATAD2A gene expression changes might characterize refractory AML. Therefore, these genes could have an impact for AML prognosis.
Abstract
Acute myeloid leukemia (AML) is a heterogeneous disease. A significant proportion of AML patients is refractory to clinical treatment or relapses. Our aim is to determine new potential AML clinical treatment prognosis markers. We investigated various cell fate and epigenetic regulation important gene level differences between refractory and responsive AML patient groups at diagnosis stage and after clinical treatment using RT-qPCR. We demonstrated that oncogenic MYC and WT1 and metabolic IDH1 gene expression was significantly higher and cell cycle inhibitor CDKN1A (p21) gene expression was significantly lower in refractory patients’ bone marrow cells compared to treatment responsive patients both at diagnosis and after clinical treatment. Moreover, we determined that, compared to clinical treatment responsive patients, refractory patients possess a significantly higher gene expression of histone deacetylase 2 (HDAC2) and epigenetic DNA modulator TET1 and a significantly lower gene expression of lysine acetyltransferase 6A (KAT6A) and nucleosome remodeling and deacetylase (NuRD) complex component GATAD2A. We suggest that MYC, WT1, IDH1, CDKN1A, HDAC2, TET1, KAT6A and GATAD2A gene expression changes might characterize refractory AML. Thus, they might be useful for AML prognosis. Additionally, we suggest that epigenetic modulation might be beneficial in combination with standard treatment.
Keywords: acute myeloid leukemia (AML), prognostic markers, epigenetic regulation
1. Introduction
Acute myeloid leukemia (AML) is characterized by the uncontrolled proliferation of neoplastic myeloid cells, which leads to the disruption of hematopoiesis [1]. This disease is very heterogeneous: its cytogenetic heterogeneity was identified decades ago; however, the scale and prognostic importance of its molecular heterogeneity has become evident only during the last two decades [2]. Although karyotype is the strongest prognostic parameter in AML patients, approximately 45% of AML patients feature a normal karyotype [3]. Thus, next-generation sequencing technologies were applied to detect somatic mutations, which help to predict AML risk [4]. The mutations affecting FLT3, NPM1, CEBPA and RUNX1 genes are among the most clinically important mutations in AML [3]. Epigenetic dysregulation also plays an important role in AML. It was demonstrated that a great proportion of AML cases had mutations in epigenetic regulators, of which 44 % were detected in DNA methylation-related genes and 43% in chromatin modifier or cohesin-complex genes [4].
Treatment outcome is influenced not only by genetic profile, but also by age. Another important prognostic factor is patient ability to respond to intensive induction chemotherapy—failure to respond estimates poor prognosis [5]. Conventional chemotherapy 7 + 3 (7 days of cytarabine + 3 days of anthracycline) cures approximately 40% of younger and 15% of older adult AML patients. The survival rate for patients who are refractory to the treatment or relapse is only approximately 10% [6]. For intermediate and poor prognosis patients who manage to achieve remission, hematopoietic stem cell transplantation (HSCT) is often used; however, the long-term survival rate remains low [7].
Thus, AML is still a challenge: not only new treatment approaches, but also better understanding of this disorder, are necessary. In this study, we split AML patients into two groups depending on their response to the clinical treatment and compared the expression levels of the tested genes between them. After a thorough literature analysis, we chose the genes that have been shown to have an important role in AML pathogenesis. Therefore, we chose to analyze cell cycle, apoptosis, metabolism and epigenetic-regulation-related genes, such as genes that tend to be deregulated in cancerous cells.
2. Materials and Methods
2.1. Patients
Bone marrow samples were obtained by aspiration from treatment-responsive (n = 15) and treatment-resistant (n = 16) adult AML patients at diagnosis and after treatment (their diagnosis and treatment are provided in Supplementary Table S1). Mononuclear cells were purified using Ficoll-Paque PLUS density gradient centrifugation (GE Healthcare Chicago, IL, USA). The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Vilnius Regional Biomedical Research Ethics Committee (Approval No. 158200-16-824-356). Informed consent was obtained from all individual participants included in the study.
2.2. Gene Expression Analysis by RT-qPCR
Total RNA was purified using RNeasy Mini Kit (QIAGEN, Hilden, Germany), cDNA was synthesized using SensiFAST™ cDNA Synthesis Kit (Bioline, Memphis, TN, USA) and qPCR was performed using SensiFAST™ SYBR® No-ROX Kit (Bioline) on the RotorGene 6000 system (Corbett Life Science, QIAGEN) according to manufacturers’ instructions. Primer sequences (Metabion international AG, Planegg/Steinkirchen, Germany) are outlined in Supplementary Table S2. Relative gene expression was calculated using ∆∆Ct method. mRNA levels were normalized to GAPDH expression.
2.3. Statistical Analysis
Results are presented as mean ± standard deviation (S.D.); grey data points indicate outliers. Mann–Whitney U test was used to determine the significance of difference between groups of different patients’ samples, and significance was set at p ≤ 0.05 (*). Outliers were determined by ROUT (Q = 5%). Statistical analysis was performed using GraphPad Prism version 8.0.1 for Windows (GraphPad Software, San Diego, CA, USA).
3. Results
3.1. Cell-Fate-Important Gene Expression in AML Patients
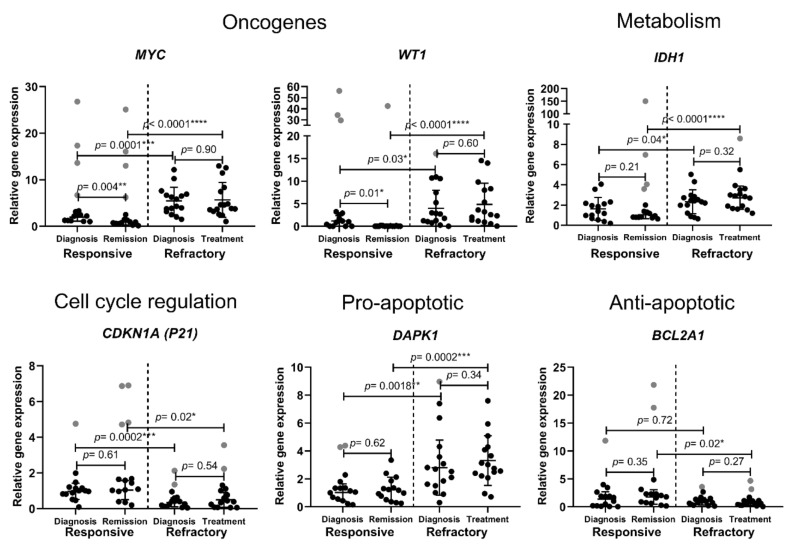
AML patients were split into two groups: the ones who responded to clinical treatment and reached remission (n = 15) and the ones who showed resistance to the used clinical treatment (n = 16). The samples were collected at diagnosis stage and after the clinical treatment. Mononuclear cells were purified and used for gene expression analysis by RT-qPCR. We analyzed some cell-fate-important gene expression differences between treatment-resistant and treatment-responsive patients at diagnosis and after clinical treatment. The expression of the oncogenes MYC and WT1 was significantly higher in refractory patients at diagnosis compared to responsive patients. Moreover, it significantly decreased after successful treatment, while remaining unchanged in refractory patients (Figure 1). Isocitrate dehydrogenase 1 coding gene (IDH1) expression was also demonstrated to be significantly higher in refractory AML patients. Meanwhile, cell-cycle-inhibitor CDKN1A (p21) gene expression was significantly higher in the treatment-responsive patient group before and after the treatment. Interestingly, pro-apoptotic gene DAPK1 expression was demonstrated to be significantly higher, while anti-apoptotic BCL2A1 expression showed a tendency to be lower in refractory patients (Figure 1). We did not find any significant differences between the tested patient groups in the gene expression of the anti-apoptotic genes BCL2, BCL2L1, BCL2L2 and MCL1; the pro-apoptotic genes APAF1, BAK1, BAX and P53; and also some other cell-fate-important genes, including TGFBR1, ABCB1, BECN1 and IDH2 (Supplementary Figure S1). In brief, the presented results show that refractory AML patients demonstrate significantly higher oncogenic MYC and WT1, metabolic IDH1 and pro-apoptotic DAPK1 gene expression and significantly lower cell-cycle-inhibitor CDKN1A (p21) gene expression both at diagnosis and after clinical treatment.
Figure 1.
Cell-fate-important gene expression analysis in treatment-responsive and -refractory AML patients. Cell samples were collected at diagnosis stage and after treatment. Relative gene expression analysis was performed using the RT-qPCR ΔΔCt method; GAPDH was used as a “housekeeping” gene. Mean ± standard deviation is presented; grey data points indicate outliers. Mann–Whitney U test was used to determine the significance of difference between the groups of different patients’ samples, and significance was set at p ≤ 0.05 (*). Outliers were determined by ROUT (Q = 5%).
3.2. Chromatin-Remodeling-Related Gene Expression in AML Patients
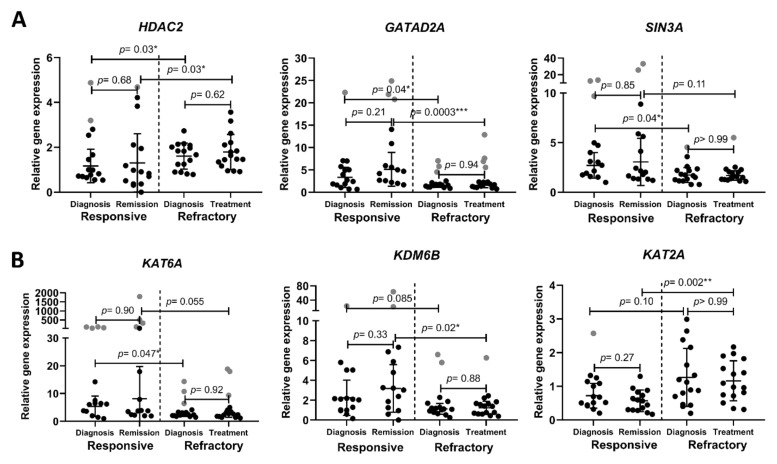
We also revealed some significant differences in epigenetic-regulation-related gene expression between treatment-refractory and treatment-responsive patients. Histone deacetylase 2 is a class I deacetylase coded by gene HDAC2; it causes transcriptional repression by acetyl group removal from histone-specific lysine residues [8]. GATA Zinc Finger Domain Containing 2A (GATAD2A, also known as p66α) is a subunit of the nucleosome remodeling and deacetylase (NuRD) complex. NuRD is highly conserved chromatin-remodeling complex that participates in DNA-damage-induced transcriptional repression [9]. The chromatin remodeling complex NuRD role in tumorigenesis was demonstrated to depend on context: it might either promote or suppress tumorigenesis [10]. SIN3A represses gene transcription by recruiting histone deacetylases to modify chromatin at particular sites of the genome [11]. We evaluated gene expression differences of these transcription repressors in AML patients and determined that HDAC2 gene expression was significantly higher, while GATAD2A was significantly lower in refractory AML patients compared to clinical-treatment-responsive patients. Additionally, in refractory AML patients, SIN3A gene expression was lower at diagnosis compared to responsive patients (Figure 2A).
Figure 2.
Chromatin-remodeling-related gene expression analysis in treatment-responsive and -refractory AML patients. (A) Gene expression changes of transcription-repressing histone modificators; (B) gene expression changes of transcription-activating histone modificators. Cell samples were collected at diagnosis stage and after treatment. Relative gene expression analysis was performed using the RT-qPCR ΔΔCt method; GAPDH was used as a “housekeeping” gene. Mean ± standard deviation is presented; grey data points indicate outliers. Mann–Whitney U test was used to determine the significance of difference between groups of different patients’ samples, and significance was set at p ≤ 0.05 (*). Outliers were determined by ROUT (Q = 5%).
We also demonstrated differences between AML patient groups in transcription-activating histone modificators. Lysine acetyltransferase 6A (KAT6A, also known as MOZ or MYST3) is a histone acetyltransferase required for H3K9 acetylation at target loci [1]. It participates in the regulation of various fundamental cellular processes, including cell cycle progression and stem cell maintenance [12,13,14]. In our study, KAT6A gene expression was significantly lower in refractory AML patients compared to responsive patients (Figure 2B). Lysine demethylase 6B (KDM6B, also known as JMJD3) is a H3K27me3-specific demethylase. It acts as a competitor of the polycomb-repressive complex 2 (PRC2), which adds methyl groups to H3K27. Thus, KDM6B activates gene transcription [15]. We showed that KDM6B gene expression had a tendency to be lower in refractory AML patients compared to the responsive patient group. Lysine acetyltransferase 2A (KAT2A) enhance transcriptional activity through histone and other target protein acetylation [16,17]. In our study, KAT2A gene expression showed a tendency to be higher in patients that are refractory to the treatment. We also evaluated EZH2, HDAC1, MTA1 and MTA2 and KAT2B gene expression, but they did not show any significant differences between tested groups (Supplementary Figure S1). In short, the histone-modification-related gene expression analysis revealed that refractory AML patients are characterized by significantly higher HDAC2 and significantly lower GATAD2A and KAT6A expression. Additionally, SIN3A gene expression was significantly lower at refractory patient diagnosis.
3.3. Epigenetic DNA Modification-Related Gene Expression in AML Patients
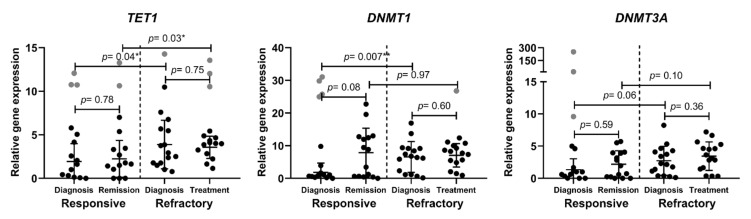
DNA methylation status also has an important role in cancer progression. Thus, we investigated the gene expression of several players participating in DNA methylation. TET1 is a dioxygenase that catalyzes 5-mC conversion to 5-hmC (5-hydroxymethylcytosine) and, therefore, participates in the DNA demethylation process [18]. Meanwhile, DNMT1 and DNMT3A are DNA methyltransferases that catalyze DNA methylation. DNMT3A catalyzes de novo DNA methylation, while DNMT1 preserves DNA methylation patterns during cell division [19]. In the present study, we determined that TET1 gene expression was significantly higher in refractory AML patients compared to treatment-responsive AML patients. Similarly, DNMT1 gene expression level was significantly higher at diagnosis in refractory patients. DNMT3A gene expression shows a slight tendency to be upregulated in refractory patients (Figure 3). TET2 and TET3 expression analysis did not show any significant differences between the tested groups (Supplementary Figure S1).
Figure 3.
Epigenetic DNA modification-related gene expression analysis in treatment-responsive and -refractory AML patients. Cell samples were collected at diagnosis stage and after treatment. Relative gene expression analysis was performed the using RT-qPCR ΔΔCt method; GAPDH was used as a “housekeeping” gene. Mean ± standard deviation is presented; grey data points indicate outliers. Mann–Whitney U test was used to determine the significance of difference between groups of different patients’ samples, and significance was set at p ≤ 0.05 (*). Outliers were determined by ROUT (Q = 5%).
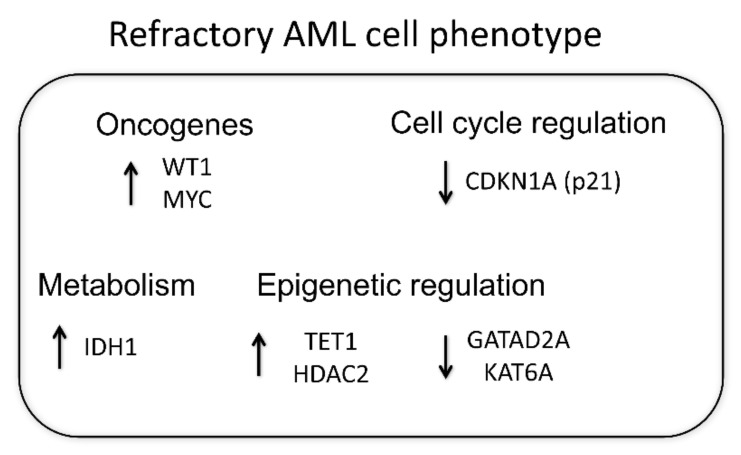
To conclude our obtained results, all detected gene expression differences are outlined in Figure 4 by presenting the proposed refractory AML phenotype.
Figure 4.
Proposed refractory AML phenotype. AML patients were split into two groups depending on their response to the clinical treatment. Relative gene expression analysis was performed using the RT-qPCR ΔΔCt method; GAPDH was used as a “housekeeping” gene. The determined statistically significant gene expression differences between refractory and responsive patients are presented.
4. Discussion
In the study, we analyzed gene level differences between clinical-treatment-responsive and -refractory AML patients at diagnosis and after the treatment. We revealed that oncogenic MYC and WT1 and metabolic IDH1 expression was significantly higher in the refractory patient group. WT1 and MYC overexpression is known to be associated with carcinogenesis, thus they are called oncogenes. WT1 is overexpressed in approximately 90% of AML patients and it is already being suggested as possible prognostic marker for relapse prediction [20]. Similarly, MYC activation is indicated as a molecular hallmark of cancer [21]. Its overexpression has also been linked with AML [22]. IDH1 is recognized to be mutated in 7–14% of AML. There is even a drug approved by the FDA to inhibit mutated IDH1 [23]. Moreover, a high IDH1 expression was demonstrated to be associated with poor cytogenetically normal AML prognosis [24]. Thus, our findings comply with previously shown data. Our results do not reveal any correlation between classical AML genes, such as TP53, TET2, IDH2, and EZH2, expression and patient response to the treatment. These genes are well known to be mutated in AML. For example, TP53 is a tumor suppressor gene; thus, its loss-of-function mutation is associated with the poor survival of AML [25]. Since we did not detect any significant differences between responsive and refractory patients’ TP53, TET2, IDH2, EZH2 expression, we suggest that the expression of these classically mutated AML genes is not a feature of AML and could not be used for its prognosis. Furthermore, two patients in our resistant patients’ group had a TP53 mutation, but, in our study, mutated TP53 expression was very similar to unmutated TP53 gene expression. We demonstrated that CDKN1A (p21) gene expression was significantly lower in refractory patients both at diagnosis and after clinical treatment. Since p21 is a cell cycle inhibitor, it is responsible for cell growth and proliferation control [26]. It was demonstrated that increased CDKN1A expression and decreased MYC expression contribute to the strong antileukemic effects of the transcription factor KLF4 [27]. Thus, the lower expression of p21 might be a marker of poor AML treatment prognosis. A dysregulated apoptosis mechanism is among the most important mechanisms used by cancerous cells. There are several pharmaceutical agents targeting the apoptosis pathway developed for AML treatment [28]. Interestingly, according to our results, resistance to apoptosis does not appear to be the main reason of AML resistance to clinical treatment. We tested various apoptosis-related gene expressions (Supplementary Figure S1) and significant differences were detected only in pro-apoptotic DAPK1. Oppositely to what was expected, pro-apoptotic DAPK1 expression was higher and anti-apoptotic BCL2A1 expression showed a tendency to be lower in refractory patients (Figure 1). It indicates that some treatment-refractory AML patients might even activate apoptosis induction mechanisms to overcome factors that cause cell resistance to clinical treatment.
Since epigenetic changes participate in the pathogenesis of AML, we compared the epigenetic-regulation-related gene expression between refractory and responsive patient groups. For example, various tumors demonstrate aberrant HDAC expression. It is well known that the inhibition of HDACs leads to anti-cancerous changes, such as decreased cell proliferation and induced apoptosis. Therefore, HDAC inhibitors are being developed for cancer, including AML, treatment. Although HDAC inhibitors are not sufficient as a monotherapy, they show promising results while used in combination with standard therapeutics [29]. The gene expression profiling of AML cells after HDAC1/2 selective inhibition alone and after HDAC1/2 selective inhibition together with treatment with azacytidine relieved particular transcription and cell-cycle-regulation-related genes that might be responsible for the mediation of combinatorial effect [30]. Moreover, it was demonstrated in some cancers that higher HDAC expression might be associated with poor prognosis—for example, in prostate carcinoma, a higher HDAC2 expression is associated with shorter relapse time [31]. We evaluated HDAC1 (Supplementary Figure S1) and HDAC2 (Figure 2A) expression in both treatment-resistant and -responsive AML patient groups and revealed that HDAC2 expression was significantly increased in refractory group. We also demonstrated that two other our tested transcription repressors SIN3A and GATAD2A showed significant differences between treatment-refractory and -responsive AML patient groups: their expression was lower in the refractory group. It was demonstrated that the lower expression of SIN3A was associated with more aggressive lung cancer progression [32]. Additionally, SIN3A knockdown increased the metastatic potential of breast cancer cells [11]. GATAD2A can have either cancer suppressive or cancer promotive role depending on the context since it is a nucleosome remodeling and deacetylase (NuRD) complex subunit. NuRD complex function depends largely on its interaction with other proteins [10]. Thus, more comprehensive studies are required to better understand GATAD2A role in AML tumorigenesis and treatment.
Transcription activating histone modificators also play an important role in carcinogenesis. We demonstrated that histone acetyltransferase KAT6A gene expression was significantly lower in the refractory patient group. This enzyme was shown to be often involved in carcinogenesis. Chromosome rearrangements resulting in fusion proteins, such as KAT6A-CBP or KAT6A-TIF2, have been identified in AML [13]. In addition, the overexpression of KAT6A was demonstrated to enhance PI3K/AKT signaling and tumorigenesis in glioblastoma cells [14]. Thus, KAT6A inhibitors are being developed for cancer therapy [33]. However, this histone acetyltransferase participates in the differentiation of erythroid and myeloid cells. KAT6A interacts with AML1 and acts as a transcriptional coactivator, but fusion protein KAT6A-CBP inhibits AML1-mediated transcription [34]. Thus, KAT6A role in tumorigenesis might depend on the type of cancer and on the presence of aberration. Moreover, it was demonstrated that KAT6A is essential for the ability of hematopoietic stem cells to reconstitute the hematopoietic system of a recipient after transplantation [35]. Our findings that KAT6A expression was higher in the treatment-responsive patient group prove its importance for healthy haematopoiesis.
Similarly, lysine demethylase 6B (KDM6B) has a complex role in tumorigenesis. Our results show that KDM6B gene expression had a tendency to be downregulated in the refractory AML patient group. However, this gene overexpression was detected in various blood disorders, including myelodysplastic syndromes (MDS), Hodgkin’s lymphoma (HL), multiple myeloma (MM) and T-cell acute lymphoblastic leukemia (T-ALL), implying the need to inhibit KDM6B for successful cancer therapy [36,37,38]. Furthermore, there are ongoing studies working on the development of KDM6B inhibitors for the treatment of hematopoietic disorders, including AML [39]. In contrast, other investigators demonstrated that KDM6B relieves the differentiation arrest of certain subtypes of AML cells. The authors determined that this histone demethylase activates the expression of a number of key myelopoietic regulatory genes by directly modulating H3K4 and H3K27 methylation levels, which indicates KDM6B onco-repressive activity. They determined that KDM6B downregulation correlates with poor clinical outcomes in certain AML subtypes [15]. Thus, KDM6B role in leukemogenesis might depend on the phase and linage of the disease [15,36].
Meanwhile, our tested transcription activating modificatory lysine acetyltransferase 2A (KAT2A) showed a tendency to be upregulated in refractory AML patients. This enzyme also plays different roles in different cancer types. For example, it was revealed that high KAT2A expression is associated with poor prognosis in breast, lung and colon cancers; however, it is associated with good prognosis in pancreatic adenocarcinoma and glioma. Its oncogenic role might be explained by causing the histone acetylation-mediated activation of E2F and MYC targets that participate in maintaining cell proliferation and survival. In AML, it was demonstrated that KAT2A helps to maintain undifferentiated leukemic cells. Additionally, KAT2A knock-out in leukemia stem-like cells lost repopulating capacity [40]. Thus, our findings that the higher expression of KAT2A might predict poor AML prognosis conforms to previous research.
We also determined differences between refractory and responsive AML patient groups in DNA methylation related gene expression—TET1 and DNMT1 were up-regulated in the refractory group. One scientist group determined that TET1 expression was significantly reduced in AML patients [18]. Other scientist group performed RNA expression profiling in AML patients possessing high/low TET1 expression and revealed that high TET1 expression predicts poor survival in two tested cytogenetically normal AML cohorts and is associated with a short survival time [41]. Thus, our results conform to the latter group’s results. DNMT1 and DNMT3A expression was shown to be increased in AML compared to bone marrow cells from healthy donors previously [42]. Additionally, DNMT1 expression was upregulated in multi-drug resistant HL60/ATRA cells in vitro [43]. Our results in ex vivo studies also indicate that an elevated DNMT1 expression might be a sign of AML resistance to treatment. One of the possible DNMT1 oncogenicity explanations is that it causes tumor suppressor p15 downregulation [42].
5. Conclusions
In conclusion, we evaluated gene expression differences between refractory and responsive AML patient groups and determined that refractory AML patients showed significantly higher oncogenic MYC and WT1, metabolic IDH1 and pro-apoptotic DAPK1 gene expression and significantly lower cell-cycle-inhibitor CDKN1A (p21) gene expression both at diagnosis and after clinical treatment. Moreover, we demonstrated significant differences in epigenetic-regulation-related gene expression: HDAC2 and TET1 gene expression was significantly higher, while GATAD2A and KAT6A was significantly lower in refractory AML patients compared to the responsive patients’ group (Figure 4). Our results reveal that the epigenetic landscape plays an important role in maintaining refractory AML. Our detected gene expression changes might be useful for AML prognosis. Additionally, we suggest that epigenetic modulators, when used in combination with standard treatment, could be useful for refractory AML clinical treatment.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers14112752/s1, Figure S1: Gene expression analysis in treatment-responsive and -refractory AML patients; Table S1: Diagnosis and treatment strategies of AML patients. Response evaluation was based on the European Leukemia Network (ELN) 2017 recommendations. Table S2: Primers used for RT-qPCR analysis.
Author Contributions
All authors (A.V., G.S., A.Ž., V.B. and R.N.) contributed to the study conception and design. Material preparation, data collection and analysis were performed by A.V., G.S., A.Ž. and V.B. The first draft of the manuscript was written by A.V. and all authors (G.S., A.Ž., V.B. and R.N.) commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee (Vilnius Regional Biomedical Research Ethics Committee Approval No. 158200-16-824-356) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the Research Council of Lithuania (grant number S-SEN-20-2).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liu X.-L., Liu H.-Q., Li J., Mao C.-Y., He J.-T., Zhao X. Role of Epigenetic in Leukemia: From Mechanism to Therapy. Chem. Biol. Interact. 2020;317:108963. doi: 10.1016/j.cbi.2020.108963. [DOI] [PubMed] [Google Scholar]
- 2.Döhner H., Weisdorf D.J., Bloomfield C.D. Acute Myeloid Leukemia. N. Engl. J. Med. 2015;373:1136–1152. doi: 10.1056/NEJMra1406184. [DOI] [PubMed] [Google Scholar]
- 3.Lagunas-Rangel F.A., Chávez-Valencia V. FLT3-ITD and Its Current Role in Acute Myeloid Leukaemia. Med. Oncol. 2017;34:114. doi: 10.1007/s12032-017-0970-x. [DOI] [PubMed] [Google Scholar]
- 4.Cai S.F., Levine R.L. Genetic and Epigenetic Determinants of AML Pathogenesis. Semin. Hematol. 2019;56:84–89. doi: 10.1053/j.seminhematol.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schlenk R.F., Müller-Tidow C., Benner A., Kieser M. Relapsed/Refractory Acute Myeloid Leukemia: Any Progress? Curr. Opin. Oncol. 2017;29:467–473. doi: 10.1097/CCO.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 6.Bose P., Vachhani P., Cortes J.E. Treatment of Relapsed/Refractory Acute Myeloid Leukemia. Curr. Treat. Options Oncol. 2017;18:17. doi: 10.1007/s11864-017-0456-2. [DOI] [PubMed] [Google Scholar]
- 7.Staudt D., Murray H.C., McLachlan T., Alvaro F., Enjeti A.K., Verrills N.M., Dun M.D. Targeting Oncogenic Signaling in Mutant FLT3 Acute Myeloid Leukemia: The Path to Least Resistance. Int. J. Mol. Sci. 2018;19:E3198. doi: 10.3390/ijms19103198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levidou G., Gajdzis P., Cassoux N., Donizy P., Masaoutis C., Gajdzis M., Gardrat S., Pergaris A., Danas E., Klijanienko J., et al. Histone Deacetylase (HDAC)-1, -2, -4, and -6 in Uveal Melanomas: Associations with Clinicopathological Parameters and Patients’ Survival. Cancers. 2021;13:4763. doi: 10.3390/cancers13194763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spruijt C.G., Luijsterburg M.S., Menafra R., Lindeboom R.G.H., Jansen P.W.T.C., Edupuganti R.R., Baltissen M.P., Wiegant W.W., Voelker-Albert M.C., Matarese F., et al. ZMYND8 Co-Localizes with NuRD on Target Genes and Regulates Poly(ADP-Ribose)-Dependent Recruitment of GATAD2A/NuRD to Sites of DNA Damage. Cell Rep. 2016;17:783–798. doi: 10.1016/j.celrep.2016.09.037. [DOI] [PubMed] [Google Scholar]
- 10.Lai A.Y., Wade P.A. Cancer Biology and NuRD: A Multifaceted Chromatin Remodelling Complex. Nat. Rev. Cancer. 2011;11:588–596. doi: 10.1038/nrc3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis M.J., Liu J., Libby E.F., Lee M., Crawford N.P.S., Hurst D.R. SIN3A and SIN3B Differentially Regulate Breast Cancer Metastasis. Oncotarget. 2016;7:78713–78725. doi: 10.18632/oncotarget.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheikh B.N., Yang Y., Schreuder J., Nilsson S.K., Bilardi R., Carotta S., McRae H.M., Metcalf D., Voss A.K., Thomas T. MOZ (KAT6A) Is Essential for the Maintenance of Classically Defined Adult Hematopoietic Stem Cells. Blood. 2016;128:2307–2318. doi: 10.1182/blood-2015-10-676072. [DOI] [PubMed] [Google Scholar]
- 13.Huang F., Abmayr S.M., Workman J.L. Regulation of KAT6 Acetyltransferases and Their Roles in Cell Cycle Progression, Stem Cell Maintenance, and Human Disease. Mol. Cell. Biol. 2016;36:1900–1907. doi: 10.1128/MCB.00055-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lv D., Jia F., Hou Y., Sang Y., Alvarez A.A., Zhang W., Gao W.-Q., Hu B., Cheng S.-Y., Ge J., et al. Histone Acetyltransferase KAT6A Upregulates PI3K/AKT Signaling through TRIM24 Binding. Cancer Res. 2017;77:6190–6201. doi: 10.1158/0008-5472.CAN-17-1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu S.-H., Zhu K.-Y., Chen J., Liu X.-Z., Xu P.-F., Zhang W., Yan L., Guo H.-Z., Zhu J. JMJD3 Facilitates C/EBPβ-Centered Transcriptional Program to Exert Oncorepressor Activity in AML. Nat. Commun. 2018;9:3369. doi: 10.1038/s41467-018-05548-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu D., Song Y., Yu Y., Wang D., Liu B., Chen L., Li X., Li Y., Cheng L., Lv F., et al. KAT2A-Mediated AR Translocation into Nucleus Promotes Abiraterone-Resistance in Castration-Resistant Prostate Cancer. Cell Death Dis. 2021;12:787. doi: 10.1038/s41419-021-04077-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou X., Wang N., Zhang Y., Yu H., Wu Q. KAT2B Is an Immune Infiltration-Associated Biomarker Predicting Prognosis and Response to Immunotherapy in Non-Small Cell Lung Cancer. Investig. New Drugs. 2022;40:43–57. doi: 10.1007/s10637-021-01159-6. [DOI] [PubMed] [Google Scholar]
- 18.Zhang T., Zhao Y., Zhao Y., Zhou J. Expression and Prognosis Analysis of TET Family in Acute Myeloid Leukemia. Aging. 2020;12:5031–5047. doi: 10.18632/aging.102928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong K.K., Lawrie C.H., Green T.M. Oncogenic Roles and Inhibitors of DNMT1, DNMT3A, and DNMT3B in Acute Myeloid Leukaemia. Biomark. Insights. 2019;14:6454. doi: 10.1177/1177271919846454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rein L.A.M., Chao N.J. WT1 Vaccination in Acute Myeloid Leukemia: New Methods of Implementing Adoptive Immunotherapy. Expert Opin. Investig. Drugs. 2014;23:417–426. doi: 10.1517/13543784.2014.889114. [DOI] [PubMed] [Google Scholar]
- 21.Gabay M., Li Y., Felsher D.W. MYC Activation Is a Hallmark of Cancer Initiation and Maintenance. Cold Spring Harb. Perspect. Med. 2014;4:a014241. doi: 10.1101/cshperspect.a014241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trop-Steinberg S., Azar Y. Is Myc an Important Biomarker? Myc Expression in Immune Disorders and Cancer. Am. J. Med. Sci. 2018;355:67–75. doi: 10.1016/j.amjms.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Megías-Vericat J.E., Ballesta-López O., Barragán E., Montesinos P. IDH1-Mutated Relapsed or Refractory AML: Current Challenges and Future Prospects. Blood Lymphat. Cancer. 2019;9:19–32. doi: 10.2147/BLCTT.S177913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma Q.-L., Wang J.-H., Wang Y.-G., Hu C., Mu Q.-T., Yu M.-X., Wang L., Wang D.-M., Yang M., Yin X.-F., et al. High IDH1 Expression Is Associated with a Poor Prognosis in Cytogenetically Normal Acute Myeloid Leukemia. Int. J. Cancer. 2015;137:1058–1065. doi: 10.1002/ijc.29395. [DOI] [PubMed] [Google Scholar]
- 25.Gu R., Yang X., Wei H. Molecular Landscape and Targeted Therapy of Acute Myeloid Leukemia. Biomark. Res. 2018;6:32. doi: 10.1186/s40364-018-0146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Deiry W.S. P21(WAF1) Mediates Cell-Cycle Inhibition, Relevant to Cancer Suppression and Therapy. Cancer Res. 2016;76:5189–5191. doi: 10.1158/0008-5472.CAN-16-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris V.A., Cummings C.L., Korb B., Boaglio S., Oehler V.G. Deregulated KLF4 Expression in Myeloid Leukemias Alters Cell Proliferation and Differentiation through MicroRNA and Gene Targets. Mol. Cell. Biol. 2016;36:559–573. doi: 10.1128/MCB.00712-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi J.H., Bogenberger J.M., Tibes R. Targeting Apoptosis in Acute Myeloid Leukemia: Current Status and Future Directions of BCL-2 Inhibition with Venetoclax and Beyond. Target. Oncol. 2020;15:147–162. doi: 10.1007/s11523-020-00711-3. [DOI] [PubMed] [Google Scholar]
- 29.San José-Enériz E., Gimenez-Camino N., Agirre X., Prosper F. HDAC Inhibitors in Acute Myeloid Leukemia. Cancers. 2019;11:1794. doi: 10.3390/cancers11111794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Min C., Moore N., Shearstone J.R., Quayle S.N., Huang P., van Duzer J.H., Jarpe M.B., Jones S.S., Yang M. Selective Inhibitors of Histone Deacetylases 1 and 2 Synergize with Azacitidine in Acute Myeloid Leukemia. PLoS ONE. 2017;12:e0169128. doi: 10.1371/journal.pone.0169128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weichert W., Röske A., Gekeler V., Beckers T., Stephan C., Jung K., Fritzsche F.R., Niesporek S., Denkert C., Dietel M., et al. Histone Deacetylases 1, 2 and 3 Are Highly Expressed in Prostate Cancer and HDAC2 Expression Is Associated with Shorter PSA Relapse Time after Radical Prostatectomy. Br. J. Cancer. 2008;98:604–610. doi: 10.1038/sj.bjc.6604199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suzuki H., Ouchida M., Yamamoto H., Yano M., Toyooka S., Aoe M., Shimizu N., Date H., Shimizu K. Decreased Expression of the SIN3A Gene, a Candidate Tumor Suppressor Located at the Prevalent Allelic Loss Region 15q23 in Non-Small Cell Lung Cancer. Lung Cancer. 2008;59:24–31. doi: 10.1016/j.lungcan.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Baell J.B., Leaver D.J., Hermans S.J., Kelly G.L., Brennan M.S., Downer N.L., Nguyen N., Wichmann J., McRae H.M., Yang Y., et al. Inhibitors of Histone Acetyltransferases KAT6A/B Induce Senescence and Arrest Tumour Growth. Nature. 2018;560:253–257. doi: 10.1038/s41586-018-0387-5. [DOI] [PubMed] [Google Scholar]
- 34.Katsumoto T., Aikawa Y., Iwama A., Ueda S., Ichikawa H., Ochiya T., Kitabayashi I. MOZ Is Essential for Maintenance of Hematopoietic Stem Cells. Genes Dev. 2006;20:1321–1330. doi: 10.1101/gad.1393106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thomas T., Corcoran L.M., Gugasyan R., Dixon M.P., Brodnicki T., Nutt S.L., Metcalf D., Voss A.K. Monocytic Leukemia Zinc Finger Protein Is Essential for the Development of Long-Term Reconstituting Hematopoietic Stem Cells. Genes Dev. 2006;20:1175–1186. doi: 10.1101/gad.1382606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mallaney C., Ostrander E.L., Celik H., Kramer A.C., Martens A., Kothari A., Koh W.K., Haussler E., Iwamori N., Gontarz P., et al. Kdm6b Regulates Context-Dependent Hematopoietic Stem Cell Self-Renewal and Leukemogenesis. Leukemia. 2019;33:2506–2521. doi: 10.1038/s41375-019-0462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ohguchi H., Harada T., Sagawa M., Kikuchi S., Tai Y.-T., Richardson P.G., Hideshima T., Anderson K.C. KDM6B Modulates MAPK Pathway Mediating Multiple Myeloma Cell Growth and Survival. Leukemia. 2017;31:2661–2669. doi: 10.1038/leu.2017.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wei Y., Zheng H., Bao N., Jiang S., Bueso-Ramos C.E., Khoury J., Class C., Lu Y., Lin K., Yang H., et al. KDM6B Overexpression Activates Innate Immune Signaling and Impairs Hematopoiesis in Mice. Blood Adv. 2018;2:2491–2504. doi: 10.1182/bloodadvances.2018024166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Y., Zhang M., Sheng M., Zhang P., Chen Z., Xing W., Bai J., Cheng T., Yang F.-C., Zhou Y. Therapeutic Potential of GSK-J4, a Histone Demethylase KDM6B/JMJD3 Inhibitor, for Acute Myeloid Leukemia. J. Cancer Res. Clin. Oncol. 2018;144:1065–1077. doi: 10.1007/s00432-018-2631-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arede L., Pina C. Buffering Noise: KAT2A Modular Contributions to Stabilization of Transcription and Cell Identity in Cancer and Development. Exp. Hematol. 2021;93:25–37. doi: 10.1016/j.exphem.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 41.Wang J., Li F., Ma Z., Yu M., Guo Q., Huang J., Yu W., Wang Y., Jin J. High Expression of TET1 Predicts Poor Survival in Cytogenetically Normal Acute Myeloid Leukemia from Two Cohorts. EBioMedicine. 2018;28:90–96. doi: 10.1016/j.ebiom.2018.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mizuno S., Chijiwa T., Okamura T., Akashi K., Fukumaki Y., Niho Y., Sasaki H. Expression of DNA Methyltransferases DNMT1, 3A, and 3B in Normal Hematopoiesis and in Acute and Chronic Myelogenous Leukemia. Blood. 2001;97:1172–1179. doi: 10.1182/blood.V97.5.1172. [DOI] [PubMed] [Google Scholar]
- 43.Li S., Jin X., Wu H., Wang Y., Li X., Guo Y., Liang S. HA117 Endows HL60 Cells with a Stem-like Signature by Inhibiting the Degradation of DNMT1 via Its Ability to down-Regulate Expression of the GGL Domain of RGS6. PLoS ONE. 2017;12:e0180142. doi: 10.1371/journal.pone.0180142. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.