Abstract
Simple Summary
Cancer is a multifaceted, life-threatening, and genomically complex disease. The worldwide prevalence of cancer is so high that one in three people will develop cancer during their lifetime. Although the use of RNA therapy is promising to fight cancer, its efficient and safe delivery is still one of the significant challenges hampering its therapeutic application. Thus, the aim of the present review was to highlight the most recent developments in the field of nanomedicine RNA-associated therapies to fight cancer.
Abstract
The complexity, and the diversity of the different types of cancers allied to the tendency to form metastasis make treatment efficiency so tricky and often impossible due to the advanced stage of the disease in the diagnosis. In recent years, due to tremendous scientific breakthroughs, we have witnessed exponential growth in the elucidation of mechanisms that underlie carcinogenesis and metastasis. The development of more selective therapies made it possible to improve cancer treatment. Although interdisciplinary research leads to encouraging results, scientists still have a long exploration journey. RNA technology represents a promise as a therapeutic intervention for targeted gene silencing in cancer, and there are already some RNA-based formulations in clinical trials. However, the use of RNA as a therapeutic tool presents severe limitations, mainly related to its low stability and poor cellular uptake. Thus, the use of nanomedicine employing nanoparticles to encapsulate RNA may represent a suitable platform to address the major challenges hampering its therapeutic application. In this review, we have revisited the potential of RNA and RNA-associated therapies to fight cancer, also providing, as support, a general overview of nanoplatforms for RNA delivery.
Keywords: cancer, drug delivery systems, RNA, nanoparticles
1. Introduction
With increasing awareness of the interdisciplinarity needed for a comprehensive characterization of the underlying mechanisms of cancer research, we have witnessed groundbreaking discoveries in various facets of molecular oncology. Compelling experimental evidence obtained from high-throughput technologies has offered a window into previously intractable problems in our comprehension of cancer genetics/epigenetics, deregulated cell signaling pathways, noncoding genome, and tumor heterogeneities and provided new insights into therapeutic options. Rapidly evolving understanding has shown that by gaining deeper insights into nano-bio interactions and personalization of nanomedicines, and through the applications of nanotechnology to emerging and existing therapeutic modalities, we have started to realize the true potential of nanomedicines in cancer [1,2,3,4].
Recent studies have provided evidence of an upsurge in cytokines after the administration of positively charged nanoparticles. There is sufficient proof of the correlation of Compliment activation with nanoparticle administration. Importantly, nanoparticles with a positive surface charge triggered activation of the classical compliment pathways, whereas negatively charged particles “switched on” the alternative (lectin) pathways [5,6].
It is becoming sequentially more understandable that after intense experimental and clinical evaluation of protein biologics and small molecules, gene therapy and RNA medicines represent promising models of drug innovation. RNA vaccines against different cancers showcase an efficient technology, as they are easier and faster to develop and manufacture compared to conventional vaccines. Importantly, RNA vaccines are completely synthetic and do not require cell cultures.
In this review, we have attempted to highlight the most recent developments in the field of nanomedicine.
2. RNA for Cancer Therapy
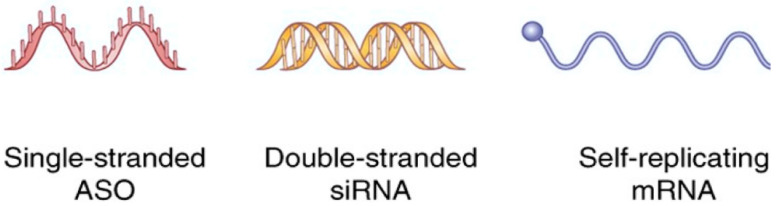
RNA therapy acts on messenger RNA (mRNA) by using oligonucleotides that can interfere with different metabolic processes of a polynucleotide, such as splicing, the mature process starting from pre-mRNA, transport, translation, and degradation [1] Differently from standard chemotherapy, RNA therapy harbors high specificity and may be used to target multiple critical oncogenic drivers, reduce drug resistance of tumor cells, and arrest growth of advanced-stage tumors [2]. RNA therapeutics may act through several mechanisms. They can inhibit the proliferation and induce apoptosis of tumor cells, prevent the metastasization process, disrupt the gene’s expression, inhibit angiogenesis, reconstruct the tumor environment, reprogram, and decrease drug resistance of tumor cells [2] RNA therapy may be divided into three major classes: antisense oligonucleotides (ASO), RNA interference (RNAi) therapies, and messenger (mRNA) therapy (Figure 1 and Table 1). ASO are single-stranded sequences of 15–25 nucleotides that bind specifically to target mRNA by complementary base pairing. Because of ASO’s weak hydrophilicity, a common modification is thiolization to increase diffusion in tissues and absorption.
Figure 1.
Main RNA used for cancer therapy.
Table 1.
Main classes of RNA therapy.
| Class of RNA Therapy | Features | Example in Cancer Therapy (Formulation) |
Target | Indication | References |
|---|---|---|---|---|---|
| ASO | 12–25 nucleotides Single-stranded Chemically modified (3 classes) |
Danvatirsen | STAT3 (downregulation) |
Advanced/recurrent solid tumors or lymphoma | [8] |
| siRNAs | 20–25 nucleotides Double-stranded Incorporated in RISC | ALN-VSP02 (lipid nanoparticle-formulated) |
VEGF and KSP (downregulation) |
Solid tumors with liver involvement | [9] |
| miRNAs | 18–25 nucleotides Single-stranded Incorporated in RISC |
miR-29b (cationic lipoplexes) |
CDK6, DNMT3B, MCL1 (downregulation) |
Lung cancer | [10] |
| miRNA mimics |
18–25 nucleotides Single-stranded Incorporated in RISC |
miR-4689 |
KRAS, AKT (downregulation) |
KRAS mutant colorectal cancer | [11] |
| anti-miR | 18–25 nucleotides Single-stranded Incorporated in RISC |
Anti-miR-155 | miR-155 (downregulation) |
Colorectal cancer | [12] |
| shRNA | 80 nucleotides Double-stranded with a loop sequence Incorporated in plasmid vectors |
hTERT-shRNA (plasmid) |
hTERT (downregulation) |
Colorectal cancer | [13] |
| mRNA | Single-stranded Less stable than DNA |
AGS-003 (dendritic cells) |
CD40L RNA tumor RNA |
Renal cancer | [14] |
Legend: RNAs; shRNA: short hairpin RNA; siRNA: small interfering RNA; RISC: RNA-inducing silencing complex.
Their easy diffusion and absorption through tissues allows them to directly bind to targets after being injected into patients [7].
ASO may act at their target mRNAs by activating RNase H or inhibiting translation by preventing ribosomes’ action through a steric effect [2]. ASO may act by correcting an altered spliceosome of proteins, repairing defective RNAs, restoring proteins, or downregulating genes’ expression [2]. Among ASO, some act as miRNA inhibitors. These oligonucleotides bind to the active chains of endogenous miRNAs with gene-silencing effects. Therefore, they enhance gene expression [2]. In contrast, RNA interference (RNAi) therapy is triggered by double-stranded RNA (dsRNA). RNAi therapy acts by knocking down the expression of the genes of interest by promoting short interfering RNAs (siRNAs). Some molecules are of synthetic manufacturing (siRNA and specific RNAi sequences). Moreover, RNAi therapy may be delivered through short hairpin RNAs (shRNAs) and microRNAs (miRNAs) [2]. siRNAs are double-stranded RNA molecules, 20–25 nucleotides in length. They are made from cutting a long dsRNA and disrupting mRNA before translation by binding it with 100% complementarity and high target specificity. Short hairpin RNAs (shRNAs) are sequences of RNA, typically about 80 base pairs in length, that include a region of internal hybridization that creates a loop structure. shRNA molecules are processed within the cell upon transcription to form a double-stranded siRNA, which knocks down gene expression.
The benefit of shRNA is that it can be incorporated into specific plasmid vectors, permitting cell-type-specific or inducible promoters integrated into genomic DNA for longer-term or stable expression, and thus more prolonged knockdown of the target mRNA [3]. miRNAs are short-endogenous non-coding RNA molecules that limit gene expression by restricting mRNA from translation and promoting mRNA decay. MiRNAs are integrated with siRNAs and proteins in the RNA-induced silencing complex (RISC). They regulate gene expression based on pairing with the target mRNA’s 3′ untranslated region (UTR). When binding with complementary mRNA occurs, RISC activates its RNase component and degrades its target. On the other hand, miRNAs come from single-stranded RNA. Folding miRNAs create stem-loops, small, folded areas of dsRNA [4]. Due to imperfect base pairing, miRNA action can affect hundreds of less specific genes. Moreover, miRNA may influence the CpG island methylation of gene promoters and regulate gene expression at the transcriptional level [2]. Among RNAi techniques, miRNA mimics function similarly to endogenous miRNAs. Their action may restore altered miRNA maturation mechanisms or enhance the function of specific tumor suppressor miRNAs [5]. In contrast, miRNA competitive agonists block the binding of endogenous miRNAs to RISC. In this way, they upregulate the expression of related proteins [6]. mRNA therapy is an alternative to DNA therapy and consists of the injection of a specific RNA messenger into a patient’s body to promote protein synthesis in cells [15]. mRNA is less stable than DNA and is an easy target of endogenous nucleases, with possible immune responses given by high numbers of neoantigens. To reduce these events, modification of the nucleoside portion of the uracil ribose has been evaluated with the creation of an immune-evasive “pseudouracil” [16]. Both siRNAs and miRNAs have hydrophilic nature, negative charge, and relatively high molecular weight (14–15 kDa), which make them poorly permeable across biological membranes. However, encapsulation of siRNAs into vesicles or conjugation to certain ligands can help deliver them to desired tissues or cells and, at the same time, avoid renal clearance [17]. With respect to siRNAs and miRNAs, mRNAs have higher and heterogeneous molecular weights and are negatively charged. Unlike drugs that can cross the lipid bilayer, the vast majority of RNA-based therapeutics are too charged and/or too large to enter cells, and demand a delivery agent. Nanoparticles (such as liposomes, polymers, and peptides) have been used to shuttle mRNA to the cell cytosol [18]. In addition, the use of lipid nanoparticles (LNPs) as a delivery system for mRNA allows the extended time of drug action, reduced drug toxicity, and improved drug stability [19]. Table 1 shows the different classes of RNA therapies and gives examples for each of them.
3. Nanoparticles for the Delivery of RNA
The development of RNA-based therapeutics has experienced a boost since the 1990s owing to the increasing knowledge of nucleic acid chemistry and the decline in production costs of mRNA [20].
The therapeutic potential of RNA largely depends on its ability to reach the desired target cells and express the proteins of interest. However, RNA presents limited stability in serum, suffers from rapid blood clearance, off-target effects, and poor cellular uptake, and may activate immune responses [21,22,23]. Therefore, the efficient and safe delivery of RNA is still one of the significant challenges hampering its therapeutic application.
The translation efficiency and stability of exogenous RNA can be enhanced by several methods, such as UTR (untranslated regions) manipulation, codon optimization, and chemical modification of the poly(A)tail of RNA [24,25]. Furthermore, its immunogenicity can be reduced through high-performance liquid chromatography purification and chemical manipulation [26,27,28,29,30,31,32,33]. Nevertheless, the optimized RNA still has to avoid enzymatic degradation, interact with the target cell, cross the cytoplasmic membrane, and diffuse in the cytoplasm to reach the ribosomes. Despite these modifications, RNA therapeutics fail to show efficient and specific uptake by tumor cells. Recent advances in nanotechnology have led to new opportunities in cancer prevention and treatment. Novel formulations of RNA in nanosystems or vectors were developed [34]. The use of viral and non-viral delivery systems resulted in improved stability and toxicity, tumor-specific delivery, and reduced immunogenicity. Viral delivery systems (retroviruses, lentiviruses, adenoviruses) make up about two-thirds of clinical trials with nucleic acids performed to date. Although effective in targeted cellular delivery, these systems raise some safety concerns related to immune responses, have a reduced cargo capacity, and are difficult to scale up manufacturing [35,36,37,38]. Non-viral delivery systems have emerged as a safer alternative for cancer therapy, as they are less immunogenic, less toxic, and less oncogenic. In addition, their production is more cost-effective and easier to scale up [39]. However, these systems’ low nucleic acid delivery efficiency hampers their translation into clinical practice and represents a problem that still needs to be addressed [40]. Nowadays, there exists a vast array of non-viral nanocarriers for RNA delivery, with distinctive compositions and thus unique properties. Some essential nanoparticle platforms are liposomes, exosomes, polymers, dendrimers, nanogels, and inorganic nanoparticles, such as carbon nanotubes and gold and magnetic nanoparticles (Figure 2) [41].
Figure 2.
Schematic representation of nanoparticles used in RNA delivery.
3.1. Lipids or Lipid-Based Nanoparticles
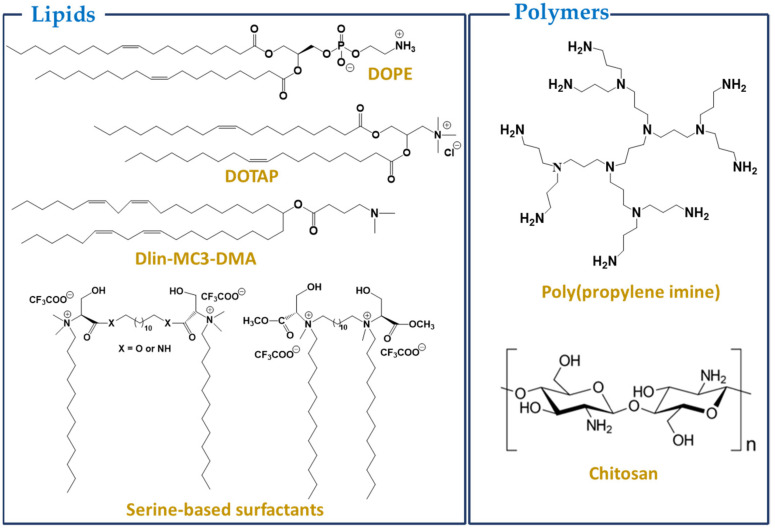
One of the most advanced RNA delivery methods is co-formulation into lipid nanoparticles (LNP) [42,43]. LNP for RNA delivery mainly comprises a cationic or ionizable lipid bearing a tertiary or quaternary ammonium group, which encapsulates the polyanionic RNA, protecting it from degradation and increasing its stability in blood circulation (Figure 3). In addition to the cationic/ionizable lipid, these formulations typically contain a zwitterionic lipid (helper lipid, e.g., 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine, DOPE) mimicking cell membrane lipids, cholesterol for the stabilization of the lipid bilayer of the nanoparticle, and a polyethene glycol (PEG), meant to improve colloidal stability and reduce protein absorption [44,45]. Cationic lipids frequently used in lipoplexes include N-[1-(2,3-dioleyloxy)propyl-N,N,N-trimethylammonium chloride (DOTMA) and N-[1-(2,3-dioleoyloxy)propyl]-N,N,N-trimethyl-ammonium chloride (DOTAP). The use of cationic lipids for lipoplex formation enhances the uptake of RNA through the interaction of the positively charged complexes with the negatively charged cell membranes. Several cationic LNP have been successfully used as RNA carriers in targeted cancer therapy, leading to higher accumulation and increased protein expression, which resulted in suppressed/blocked tumor growth [10,46].
Figure 3.
Structures of some common lipids/polymers used for preparing nanoparticles.
The inclusion of helper lipids, such as DOPE or cholesterol, generally increases the in vitro transfection efficiency of the lipoplexes [47]. However, most of these positively charged systems are highly cytotoxic in vivo, and the formulations have to be carefully adjusted to maintain cellular viability [48,49,50,51].
More recent studies have focused on using LNP based on pH-dependent ionizable cationic lipids, which have been shown to efficiently transfect mRNA to express therapeutic proteins. These lipids are positively charged at acidic pH but neutral at physiological pH. The resulting LNP display low surface charge at physiological pH and are relatively non-toxic and non-immunogenic. The structure of pH-dependent nanoparticles may be destabilized in environments with pH values lower than 6.5, facilitating the release of encapsulated cargoes within the more acidic tumor microenvironment [52,53,54]. In fact, the first siRNA drug approved by the FDA, Onpattro, is based on ionizable lipid (6Z,9Z,28Z,31Z)-heptatriaconta-6,9,28,31-tetraen-19-yl-4-(dimethylamino) butanoate (DLin-MC3-DMA, MC3) [55]. Several MC3-based LNP have then been tested for mRNA therapeutics [56,57]. Ethanolamine was identified as a favorable headgroup. The incorporation of biodegradable lipids resulted in nanoparticles with reduced toxicity and better delivery efficacy [58,59]. Biodegradability may be conferred by the presence of an ester bond on the hydrophobic tail or on the linker, which accelerates liver clearance. In addition, the release of the cargo may be triggered through cleavage of the labile ester bond (pH, nucleases) and consequent modification of the aggregate structure [58,59,60].
Further, the use of unsaturated lipid tails in the lipid structure has been shown to increase fluidity and introduce structural defects in the cell membrane, facilitating fusion of the LNP with the cell membrane, as well as endosomal escape [61]. However, a rational balance of unsaturation and biodegradability is of the utmost importance, since these two factors seem to strongly affect the degree and site of protein expression [62,63].
The development of lipid nanoparticles based on serine-derived gemini surfactants and monoolein (MO) as helper lipids for siRNA delivery has also been reported. The use of amino acids as polar headgroups in the design of surfactants leads to enhanced biological properties (biocompatibility and toxicity) compared to conventional quaternary ammonium-based surfactants [64]. The lipoplexes formed (gemini/MO/siRNA) were found to have sizes of 100–250 nm and were suitable for intravenous administration. The systems were effective in RNA complexation and gene silencing and presented no significant cytotoxicity. The transfection efficiency was shown to be dependent on the content of the MO.
Solid lipid nanoparticles (SLN) containing cationic lipids were also reported as RNA carriers for cancer therapy. They can be produced without the need for organic solvents, lyophilized, and the dehydrated SLN are stable for up to 9 months when stored at temperatures up to 30 °C [65]. In addition, the lyophilized SLN maintained their transfection efficacy over time [66]. Although effective as delivery systems, several problems associated with the positive charge of the lipids (e.g., toxicity) precluded their development and clinical use [67]. When neutral lipids were used to replace cationic ones, significant RNA accumulation, target genes’ downregulation, and tumor growth inhibition were achieved without inducing toxicity. However, these neutral lipid SLN suffer from lower loading capacity and lower transfection efficiency compared to the cationic lipid SLN.
More recently, miRNA-loaded exosomes have been engineered as cancer therapeutics (endometrial cancer, breast cancer, colorectal cancer, liver cancer) [68,69,70,71,72]. Exosomes are small (50–150 nm) endogenous membrane vesicles secreted from several mammalian cell types. These extracellular vesicles (EV) can fuse with the membrane of target cells and deliver exosome surface proteins, carbohydrates, lipids, and nucleic acids. They are non-immunogenic and non-oncogenic, present negligible toxicity, and thus stand as a promising and innovative platform for miRNA delivery [73]. Shtam et al. have shown that exosomes can efficiently deliver siRNA into target cancer cells, leading to gene silencing and cancer cell death [74]. However, there are still several limitations to implementing an EV-mediated miRNA cancer therapy, mainly related to the large-scale production, isolation, and characterization of EV suitable for clinical translation studies. In addition, the determination of the RNA content in the EV faces some problems. Finally, the dosage must be accurately defined, and routes of administration must be better explored since most systemically injected EV are delivered to the liver [75].
3.2. Polymers
Polymeric-based non-viral vectors represent another class of nanoscale platforms for RNA delivery. Specifically, cationic polymers can bind to nucleic acids to form polyplexes. Polymers can efficiently protect RNA from nucleases and promote cellular uptake and endosomal escape, leading to higher RNA delivery efficiency. Representative polymers of this class include chitosans, polyethyleneimine (PEI), dendrimers, and nanogels (Figure 2).
Chitosans are naturally derived cationic polysaccharides, differing in the degree of N-acetylation and molecular weight (50–2000 kDa). They are readily available, biodegradable, easy to modify, and possess unique biological properties associated with their polycationic nature [76,77,78]. Chitosan is only poorly water-soluble and exhibits low transfection efficacy. However, it can be derivatized to increase nucleic acid delivery efficiency by chitosan vectors. Strategies for derivatization include structural modifications–like (i) copolymerization: polyethylene glycol, PEG, and polyethyleneimine, PEI, are commonly used, although other chitosan graft copolymers are being studied as nucleic acid carriers [79]; and (ii) functional group modification: N-alkylation and quaternization enhance colloidal stability and transfection efficacy of the nanoparticles–and ligand conjugation–peptides, proteins, and non-proteinaceous ligands, like carbohydrates, folic acid and hyaluronic acid are commonly used for chitosan vector conjugation [80,81]. Although non-proteinaceous ligands are usually less immunogenic and produce more stable vectors, proteinaceous ligands offer a vast diversity of choices with favorable functionalities to vector conjugation for nucleic acid delivery [82]. Chitosan-based nanoparticles simultaneously encapsulating siRNA and the anticancer drug doxorubicin were shown to decrease the viability, growth, proliferation, and migration of breast [83] and colorectal [84,85] cancer cells and induce their apoptosis.
PEI is a cationic polymer that has been widely used in gene therapy [86]. It is highly efficient in the compaction of nucleic acids and promotes endosomal escape via the proton sponge effect [87]. The transfection efficiency of PEI-mRNA polyplexes in several types of cells has been reported, but cytotoxicity from PEI hinders its therapeutic application [44,48,88].
Incorporating PEI into polymers (as above for chitosan) has been reported to decrease its toxicity. For example, PEI-β-cyclodextrin conjugates show low toxicity while being highly efficient in promoting cell uptake and endosomal escape, leading to enhanced transfection efficiency [89].
Chemical modification of low molecular weight PEI (<2 kDa) with salicylamide or stearic acid has also been reported to reduce the toxicity and enhance transfection efficiency of the resulting polyplexes/micelles [90,91].
Dendrimers are polymeric materials with a highly branched 3D structure [92]. They consist of a central core, many layers of repeating units, and multiple functional groups on the surface. Due to their unique structure, they possess various interesting physical properties, such as good water-solubility, nanoscale uniform size, symmetrical shapes, internal cavities, good biocompatibility, stability, and high drug-loading capacity. Their toxicity is generally low but depends on the number of terminal amino groups and positive charge density. Dendrimer-based organic and inorganic nanoparticles have been widely studied and exhibited high potential in cell targeting and drug delivery [93,94,95]. Dendrimer-based iron oxide nanoparticles (IONP) show reduced toxicity, enhanced biocompatibility and safety, enhanced escape from the reticuloendothelial system (RES), and enhanced MRI properties compared to non-functionalized IONP. Dendronized magnetic IONP have been applied in gene delivery as magnetoplexes for magnetofection, leading to high-level transgene expression after a short incubation time using low doses of nucleic acid and a small amount of NP [96,97,98].
Dendrimers have also been used as templates for gold nanoparticles (AuNPs) to control their size and shape, which are known to influence the efficiency of AuNPs in biological systems highly [99,100].
Nanogels (NG) are gel particles with a three-dimensional hydrophilic network structure. They are commonly made up of polyacrylic acid, polyacrylamides, polyaminoacids, and other high molecular weight polymers. NG-based drug delivery systems possess a large surface area, structural stability, and the ability to swell. They present a high loading capacity, encapsulating either hydrophobic or hydrophilic drugs. Their shape and size can be finely tuned, and they are sensitive to pH, temperature, ionic strength, and other external stimuli, which confers them adequate controlled drug release capacities [101,102,103].
A thiolated PEI-dextrin NG was shown to efficiently deliver siRNA to cancer cells without inducing compromising toxicity. In any case, the variable morphology of the nanoparticles, as well as their size distribution, allied to the lack of data on their clinical safety and efficacy, are issues to be overcome for a broad application of this nanoplatform to be feasible [104].
3.3. Inorganic Nanoparticles
Inorganic nanomaterials (derived from gold, carbon, silica, etc.) are promising carrier platforms for RNA delivery due to their unique physicochemical properties, which endow them exciting attributes, such as long-term stability, high loading capacity, and optical responsiveness. These inorganic nanoparticles are usually easier to synthesize and scale up than organic-based ones and have been the subject of much research concerning their potential as nanocarriers for nucleic acid delivery.
The calcium phosphate (CaP) composite is the oldest non-viral gene carrier, introduced in 1973. It is biocompatible and biodegradable and forms complexes with nucleic acids, successfully delivering them to cells [105]. However, the size of the CaP precipitates is challenging to control, which constitutes a severe limitation to their use. Pegylation and lipid coating improve these nanocarriers’ colloidal stability, which shows relevant in vivo efficacies [106,107,108,109]. The calcium-phosphate core is responsible for endosomal escape and cargo release into the cytosol. Furthermore, these nanoparticles can efficiently co-deliver siRNA and mRNA [110].
Gold nanoparticles, AuNPs, possess high chemical stability and attractive optical properties, are easy to functionalize, and are of particular interest for biomedical applications [111]. They have been applied as therapeutics in drug delivery, diagnostics, and imaging [112]. Their efficiency in biological systems depends mainly on their shape, size, and size distribution, and many approaches have been made to optimize these parameters [99,100,113]. Gold can be directly conjugated via electrostatic and/or covalent interactions to thiolated compounds to form stabilized monolayer-coated NP, whose properties can easily be tuned through functionalization to meet specific needs. For example, Ghosh et al. developed efficient nanocarriers based on cysteamine-functionalized AuNP to deliver miRNA to cancer cells, using neuroblastoma and ovarian cancer cell lines [114].
Carbon nanotubes (CNT) can be categorized into single-, double-, or multi-walled (SWNT, DWNT, and MWNT) according to the number of graphene layers in their structure. They are promising nanocarriers for nucleic acid delivery, as they can avoid the endosomal barrier through an endocytosis-independent cell penetration pathway. CNT are poorly water-soluble; however, they offer a large surface area, which can be modified with functional groups and loaded with drugs or nucleic acids, thus enhancing their aqueous dispersibility [115,116]. CNT-mediated delivery of siRNA may be accomplished either by chemical conjugation of the nucleic acid to the CNT or the material used to coat them [117] or through formation of non-covalent complexes between chemically functionalized cationic CNT and the negatively charged siRNA [118,119,120,121]. Surface modification of CNT using dendrimers has been reported to enhance their aqueous dispersibility. These nanocarriers have been shown to efficiently complex siRNA and mediate its intracellular delivery with minimal induced cytotoxicity, and may thus be good candidate vectors for in vivo gene silencing [122].
Mesoporous silica-based nanoparticles (MSNP) were first applied for drug delivery in 2001 [123]. They present low toxicity, large surface area, and thus an enhanced loading capacity. However, they cannot induce endosomal escape and must be chemically modified to enhance their transfection efficacy in vivo [124,125]. Ngamcherdtrakul et al. modified siRNA loaded MSNP by adding PEI to promote endosomal escape, and PEG, to protect the siRNA from degradation, and reduce the toxicity induced by the PEI. The modified nanoparticles were shown to induce apoptosis in breast cancer cells in vitro [126]. Functionalization of MSNP with cyclodextrin-grafted PEI has also been reported to enhance the loading capacity of siRNA and enable its effective endosomal escape [127]. Furthermore, silica nanoparticles conjugated to a disialoganglioside antibody were used to deliver miRNA to neuroblastoma, with promising results [128].
Iron oxide magnetic nanoparticles have also been proposed as vehicles for the delivery of nucleic acids [129]. Magnetic nanoparticles coated with positively charged polymers, such as PEI, have been shown to significantly increase transfection efficiency compared to cationic polymers/surfactants or lipids alone [130]. This technique, known as magnetofection, relies on the combination of magnetic nanoparticles with a positively charged coating and nucleic acids to form the corresponding complexes, which upon applying a magnetic field adhere to the cell surface and internalize by endocytosis [131,132]. Nanoparticle coating has been reported to protect nucleic acid from degradation by nucleases. Superparamagnetic iron oxide nanoparticles (SPION) are effective vehicles for the delivery of nucleic acids and offer the possibility of monitoring biodistribution. Luo et al. reported the use of a folic acid functionalized polyethyleneimine SPION for siRNA delivery to gastric cancer cells [133].
The methods described above represent some of the most used nanoplatforms for RNA delivery. Still, others exist that were not referred to, as the aim was to provide a general, although not extensive, overview of the wide variety of available delivery systems, specifically for RNA delivery. The classifications of the delivery systems may sometimes overlap, as, e.g., in the case of inorganic gold nanoparticles functionalized with polymers. Whether they fit in the class of AuNP, or of polymers, or may be considered as hybrid nanoparticles, the most important thing is to be aware of the many considerations that have to be taken into account when designing novel vectors for biomedical applications. Efficacy concerning the proposed aim must go hand-in-hand with biocompatibility and safety; otherwise, translation into clinical use may be at cost.
In Table 2, some of the advantages and disadvantages of the above-mentioned nanosystems are summarized.
Table 2.
Advantages and disadvantages of nanosystems used for RNA delivery.
| Nanosystems | Advantages | Disadvantages | References | |
|---|---|---|---|---|
| Lipid-based nanosystems | Liposomes |
|
|
[43] |
| SLN |
|
|
[43,65,66] | |
| Exosomes |
|
|
[72] | |
| Polymeric systems |
|
|
[134] | |
| Inorganic nanoparticles | Metallic (Au, iron) |
|
|
[113,135,136] |
| Carbon nanotubes |
|
|
[115,116] | |
| Silica |
|
|
[124,125] | |
4. Ongoing Clinical Trials Using RNA-Loaded NPs for Cancer Therapy
Lipid-based nanoparticles (LNPs) that include liposomes and lipid NPs have been tested in animal models of tumors with promising results [9]. Therefore, clinical studies evaluating the role of RNA molecules encapsulated in LNPs have been conducted. So far, only LNPs, and no other type of nanoparticles have entered clinical trials for the delivery of RNA. Few studies have been concluded and have results, while a discrete number of trials are ongoing. In 2013, the results of the first-in-man phase I trial involving cancer patients with liver involvement treated with RNA interference (RNAi) molecules encapsulated in LNPs were published. Patients received a combination of two different short interfering RNAs (siRNAs), ALN, and VSP, targeting vascular endothelial growth factor-A (VEGF-A) and kinesin spindle protein encoded by the KIF11 gene (KPS). Similar to other liposomes of the same size (80–100 nm), ALN-VSP distributes primarily to the liver and spleen because of the fenestrated endothelium of these organs. Patients were enrolled in seven dose levels (0.1–1.5 mg/kg) in the dose-escalation phase, followed by an expansion phase. Therapy was administered intravenously every two weeks. Thirty-seven patients were evaluated for tumor response, and four had disease control over six months, with doses ≥ 0.7 mg/kg. A complete response occurred in a patient with endometrial cancer and multiple hepatic and abdominal lymph node metastases, with 50 doses of treatment received over 26 months. Seven patients had a long, stable disease and were treated for an average of 11.3 months. Some of these patients had VEGF-overexpressing primaries, such as renal, endometrial, pancreatic neuroendocrine tumors and angiosarcomas. Two patients with renal cancer experiencing progressive disease during VEGF pathway inhibitors had stable disease for 8–12 months. A patient with a primitive neuro-ectodermal tumor (PNET) and multiple liver metastases had disease stabilization for 18 months. Dynamic contrast-enhanced magnetic resonance imaging (MRI) showed a reduction in blood flow and capillary permeability following ALN-VSP treatment in 13 of the 28 evaluable patients. Moreover, biopsies were performed to look for evidence of RNAi. Among the 12 evaluable patients, all had detectable VEGF siRNA post-dose, and 11 of 12 had detectable KSP siRNA. Two patients had 96–100% viable tumor biopsies, suggesting selective drug delivery to the tumor. Treatment was well tolerated, with the most frequent adverse events being low-grade fatigue/asthenia, nausea/vomiting and fever occurring in 15–24% of patients. Liver function tests were normal in almost all patients, while one patient developed hepatic failure several days after the second dose and subsequently died. Data with ALN-VSP suggest that dual targeting of VEGF and KSP occurs at molecular and clinical levels. These preliminary data provide the basis for further development of ALN-VSP in anti-VEGF responsive malignancies, such as endometrial cancer, PNET, renal cell cancer, and hepatocellular carcinoma (HCC) [9]. Another phase I trial evaluated the activity of polo-like kinase 1 (PLK1) siRNA (TKM-080301) in patients with refractory adrenocortical cancer. The drug was evaluated in a dose-escalation plus expansion cohort and administered an intravenous infusion once a week for three consecutive weeks, repeated every 28 days. Sixteen patients were treated at 0.6 or 0.75 mg/kg/week for up to 18 cycles. Eight patients received at least two cycles and were evaluated for tumor response. Four patients had stable disease, while one patient had a partial response; evaluation of tumor tissue revealed mutations of TP53, NF1, and ARID1A. Moreover, RNA sequencing showed elevated expression of PLK1 compared to the normal adrenal RNA control. Two patients completed at least six cycles. Treatment was well tolerated, with the most frequent adverse events (AEs) being pyrexia (56%), chills (50%), back pain (31%), infusion reaction (31%), and nausea (25%) [137]. Later, TKM-080301 was evaluated in 43 HCC patients. Patients were enrolled in a 3 + 3 dose escalation plus expansion cohort. The maximum tolerated dose was 0.6 mg/kg. Of the 39 patients receiving a dose of at least 0.3 mg/kg, 18 subjects had stable disease according to RECIST 1.1 criteria, while eight subjects had a partial response according to Choi criteria. The median progression-free survival (PFS) was 2.04 months, while the median survival (mOS) for the whole population was 7.5 months. Treatment was well tolerated but did not improve OS compared to historical control for HCC [138].
The MYC oncogene has also been a target of the siRNA therapeutic approach. Dicerna Pharmaceutical developed DCR-MYC, a lipid particle with double-stranded RNA targeting the MYC oncogene and suppressing cancer progression [139]. DCR-MYC was administered in a phase I dose-escalation study as a two-hour intravenous infusion on days 1 and 8 of a 21-day cycle. Nineteen patients with advanced solid tumors, multiple myeloma, and lymphoma were enrolled. Considering the role played by MYC in cancer metabolism, FDG-PET was performed after one cycle to evaluate metabolic responses. At the same time, tumor shrinkage measured with RECIST criteria was assessed every two cycles. A patient with PNET had dose-limiting toxicity after one cycle at 0.1 mg/kg with a transient increase of aspartate aminotransferase and fatigue. However, this patient obtained a complete metabolic response sustained for more than eight months without further treatment. The most common AEs were fatigue, nausea, and infusion reactions [140]. DCR-MYC was also evaluated in a phase I study of patients with HCC (NCT02314052). However, the producing company has stopped clinical studies with DCR-MYC due to unsatisfactory clinical results [139].
Some trials using RNA-loaded NPs are ongoing. A nanoliposomal targeted therapeutic against EphA2 has been developed to reduce cancer cell proliferation and slow tumor growth. EphA2 is a tyrosine-kinase receptor with overexpression in breast, lung, prostate, ovarian, pancreatic, and endometrial cancer. A phase I study evaluating the role of EphA2 siRNA in patients with advanced solid tumors is currently active but not recruiting (NCT01591356). The companies ModernaTX and AstraZeneca have developed LPNs loaded with mRNA-2752. This mRNA encodes for OX40L, a T-cell co-stimulator. Patients with solid tumors have received mRNA-2752 or a combination with durvalumab. Responses in the preclinical setting using mRNA-2752 in monotherapy or in combination with durvalumab led to a phase I study activation in participants with relapsed/refractory solid tumor malignancies or lymphoma recruiting (NCT03739931).
Another LNP encapsulating mRNA, mRNA-2416, is being evaluated in treating patients with solid malignancies in a phase I-II study alone and in combination with fixed doses of durvalumab (NCT03323398). MRNA-2416 targets OX40, which strongly activates T-cell responses against tumoral cells. Lipo-MERIT is a cancer vaccine of four mRNAs encoding for NY-ESO-1, MAGE-A3, tyrosinase, and PTE. Lipo-MERIT has a splenic tropism, is taken up by dendritic cells and macrophages, and activates NK, B, CD4+ and CD8+ T-cells. Lipo-MERIT is now under evaluation in a phase I study of patients with advanced melanoma (NCT02410733). The mRNA-4157 LNP cancer vaccine is being tested in a phase I study (KEYNOTE-603) alone in patients with resected solid tumors and in combination with pembrolizumab in patients with unresectable solid tumors. After administration, this LNP is uptaken by antigen-presenting cells and induces cytotoxic T-lymphocyte and memory T-cell-dependent immune activation (NCT03313778). In contrast, KEYNOTE-942 is testing mRNA-4157 LNP together with pembrolizumab in patients with cutaneous melanoma completely resected and with a high risk of recurrence (NCT03897881). The OLIVIA trial is a phase-I study currently evaluating a combination of three ovarian cancer tumor-associated antigen mRNAs encapsulated in a liposome. Patients with ovarian cancer are vaccinated during neoadjuvant and adjuvant chemotherapy (e.g., carboplatin-paclitaxel) to increase the T-cell-mediated systemic immune response against cancer cells (NCT04163094). Another phase I study (TNBC-MERIT), currently active but not recruiting, is evaluating the treatment outcome with a combination of immunotherapy with patient-specific RNA-liposome complexes tailored to the antigen-expression profile of any given patient’s tumor (WAREHOUSE immunotherapy–IVAC_W_bre1_uID) and de novo synthesized RNAs targeting up to 20 individual tumor mutations (IVAC® MUTANOME immunotherapy–IVAC_M_uID). The scientific rationale for combining the two IVAC® approaches assumes that immunotherapies that acknowledge tumor heterogeneity on a single-patient level and target the whole range of antigens selectively expressed on tumors bear the highest potential to constitute an effective treatment (NCT02316457). Table 3 lists the major features of the ongoing studies in this field.
Table 3.
Ongoing studies with RNA-loaded nanoparticles.
| Study Name | Phase/Status | Drug | Target | Indication |
|---|---|---|---|---|
| NCT01591356 | I/Active, not recruiting | EphA2 siRNA | EphA2 | advanced/recurrent solid tumors |
| NCT03739931 | I/Active and recruiting | mRNA-2752 LNP | OX40L T cell | relapsed/refractory solid tumor or lymphoma |
| NCT03323398 | I-II/Active, not recruiting | mRNA-2416 LNP alone or + durvalumab | OX40L T cell | relapsed/refractory solid tumor or lymphoma |
|
NCT02410733 Lipo-MERIT |
I/Active, not recruiting | mRNA RBL001.1, RBL002.2, RBL003.1, RBL004 LIP | NY-ESO-1, MAGE-A3, tyrosinase and TPTE |
advanced melanoma |
| NCT03313778 KEYNOTE-603 | I/Active and recruiting | mRNA-4157 LNP alone or +pembrolizumab | 20 TAA | unresectable solid tumor |
|
NCT03897881 KEYNOTE-942 |
I/Active and recruiting | mRNA-4157 LNP + pembrolizumab | 20 TAA | resected and high-risk melanoma |
|
NCT04163094 OLIVIA |
I/Active and recruiting | W_ova1 | 3 TAA | resectable ovarian cancer (neoadjuvant and adjuvant) |
5. Conclusions
For clinical translatability of promising nano-enabled technologies, well-defined initiatives have already been initiated aiming to improve patient-specific therapeutic outcomes. We have witnessed encouraging results in laboratory settings related to delivery strategies for RNA molecules. However, delivery of tumor suppressor non-coding RNAs is still in its infancy. There is a need to identify highly promising miRNAs, lncRNAs, and circular RNAs for delivery in animal models for disease prevention and treatment. Through continuous and tireless investigation of nanoparticle delivery technologies in laboratory settings, researchers have unique opportunities to conceptually interpret and analyze outcomes to add to an ever-expanding library of known design-function relationship trends in the rapidly evolving field of nanomedicine. However, it is worthwhile that the trends observed at the benchtop must be contextualized before making any attempt to generalize experimental evidence broadly, as minor differences in nanoparticle compositions, animal models, and disease pathology may modify the functions of nanoparticles and must be considered during the clinical translation of nanoparticle technology.
Acknowledgments
Sandra G. Silva and Marina Pinheiro thank FCT (Fundação para a Ciência e Tecnologia) for funding through the Individual Call to Scientific Employment Stimulus (CEEC Individual grant CEECIND/01932/2017) and through program DL 57/2016–Norma transitória, respectively.
Author Contributions
Conceptualization, M.G., S.G.S., J.E., M.L.C.d.V., A.A.F. and M.P.; methodology, M.G., S.G.S., J.E., M.L.C.d.V., A.A.F. and M.P.; investigation, M.G., S.G.S., J.E., M.L.C.d.V., A.A.F. and M.P; writing—original draft preparation, M.G., S.G.S., J.E., M.L.C.d.V., A.A.F. and M.P.; writing—review and editing, M.G., S.G.S., J.E., M.L.C.d.V., A.A.F. and M.P.; supervision, M.P.; funding acquisition, S.G.S., M.L.C.d.V., A.A.F. and M.P. All authors have read and agreed to the published version of the manuscript.
Memorial
This manuscript is dedicated in honour of José Luís Fontes da Costa Lima. José Luís Fontes da Costa Lima will be remembered forever as an inspiring and pioneering chemist scientist, educator, friend, and mentor of the Faculty of Pharmacy of the University of Porto.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work received financial support from PT national funds (FCT/MCTES, Fundação para a Ciência e Tecnologia and Ministério da Ciência, Tecnologia e Ensino Superior) through project UIDB/50006/2020.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bumcrot D., Manoharan M., Koteliansky V., Sah D.W. RNAi therapeutics: A potential new class of pharmaceutical drugs. Nat. Chem. Biol. 2006;2:711–719. doi: 10.1038/nchembio839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang X., Li D., Leng S., Zhu X. RNA-based pharmacotherapy for tumors: From bench to clinic and back. Biomed. Pharmacother. 2020;125:109997. doi: 10.1016/j.biopha.2020.109997. [DOI] [PubMed] [Google Scholar]
- 3.Sliva K., Schnierle B.S. Selective gene silencing by viral delivery of short hairpin RNA. Virol. J. 2010;7:248. doi: 10.1186/1743-422X-7-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinel K., Diver L.A., White K., McDonald R.A., Baker A.H. Substantial Dysregulation of miRNA Passenger Strands Underlies the Vascular Response to Injury. Cells. 2019;8:83. doi: 10.3390/cells8020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weng Y., Xiao H., Zhang J., Liang X.J., Huang Y. RNAi therapeutic and its innovative biotechnological evolution. Biotechnol. Adv. 2019;37:801–825. doi: 10.1016/j.biotechadv.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Setten R.L., Rossi J.J., Han S.P. The current state and future directions of RNAi-based therapeutics. Nat. Rev. Drug Discov. 2019;18:421–446. doi: 10.1038/s41573-019-0017-4. [DOI] [PubMed] [Google Scholar]
- 7.Crooke S.T., Witztum J.L., Bennett C.F., Baker B.F. RNA-Targeted Therapeutics. Cell Metab. 2018;27:714–739. doi: 10.1016/j.cmet.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Hong D., Kurzrock R., Kim Y., Woessner R., Younes A., Nemunaitis J., Fowler N., Zhou T., Schmidt J., Jo M., et al. AZD9150, a next-generation antisense oligonucleotide inhibitor of STAT3 with early evidence of clinical activity in lymphoma and lung cancer. Sci. Transl. Med. 2015;7:314ra185. doi: 10.1126/scitranslmed.aac5272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tabernero J., Shapiro G.I., LoRusso P.M., Cervantes A., Schwartz G.K., Weiss G.J., Paz-Ares L., Cho D.C., Infante J.R., Alsina M., et al. First-in-humans trial of an RNA interference therapeutic targeting VEGF and KSP in cancer patients with liver involvement. Cancer Discov. 2013;3:406–417. doi: 10.1158/2159-8290.CD-12-0429. [DOI] [PubMed] [Google Scholar]
- 10.Wu Y., Crawford M., Mao Y., Lee R.J., Davis I.C., Elton T.S., Lee L.J., Nana-Sinkam S.P. Therapeutic Delivery of MicroRNA-29b by Cationic Lipoplexes for Lung Cancer. Mol. Ther. Nucleic Acids. 2013;2:e84. doi: 10.1038/mtna.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hiraki M., Nishimura J., Takahashi H., Wu X., Takahashi Y., Miyo M., Nishida N., Uemura M., Hata T., Takemasa I., et al. Concurrent Targeting of KRAS and AKT by MiR-4689 Is a Novel Treatment Against Mutant KRAS Colorectal Cancer. Mol. Ther. Nucleic Acids. 2015;4:e231. doi: 10.1038/mtna.2015.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y., Duo Y., Bi J., Zeng X., Mei L., Bao S., He L., Shan A., Zhang Y., Yu X. Targeted delivery of anti-miR-155 by functionalized mesoporous silica nanoparticles for colorectal cancer therapy. Int. J. Nanomed. 2018;13:1241–1256. doi: 10.2147/IJN.S158290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu A.Q., Ge L.Y., Lu X.L., Luo X.L., Cai Y.L., Ye X.Q., Geng F.F. Silencing of the hTERT gene by shRNA inhibits colon cancer SW480 cell growth in vitro and in vivo. PLoS ONE. 2014;9:e107019. doi: 10.1371/journal.pone.0107019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amin A., Dudek A.Z., Logan T.F., Lance R.S., Holzbeierlein J.M., Knox J.J., Master V.A., Pal S.K., Miller W.H., Jr., Karsh L.I., et al. Survival with AGS-003, an autologous dendritic cell-based immunotherapy, in combination with sunitinib in unfavorable risk patients with advanced renal cell carcinoma (RCC): Phase 2 study results. J. Immunother. Cancer. 2015;3:14. doi: 10.1186/s40425-015-0055-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weissman D., Kariko K. mRNA: Fulfilling the Promise of Gene Therapy. Mol. Ther. 2015;23:1416–1417. doi: 10.1038/mt.2015.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kariko K., Buckstein M., Ni H., Weissman D. Suppression of RNA recognition by Toll-like receptors: The impact of nucleoside modification and the evolutionary origin of RNA. Immunity. 2005;23:165–175. doi: 10.1016/j.immuni.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 17.Lam J.K.W., Chow M.Y.T., Zhang Y., Leung S.W.S. siRNA Versus miRNA as Therapeutics for Gene Silencing. Mol. Ther. Nucleic Acids. 2015;4:e252. doi: 10.1038/mtna.2015.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoecke L., Roose K. How mRNA therapeutics are entering the monoclonal antibody field. J. Transl. Med. 2019;17:54. doi: 10.1186/s12967-019-1804-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ickenstein L.M., Garidel P. Lipid-based nanoparticle formulations for small molecules and RNA drugs. Exp. Opin. Drug Deliv. 2019;16:1205–1226. doi: 10.1080/17425247.2019.1669558. [DOI] [PubMed] [Google Scholar]
- 20.Han X., Mitchell M.J., Nie G. Nanomaterials for Therapeutic RNA Delivery. Matter. 2020;3:1948–1975. doi: 10.1016/j.matt.2020.09.020. [DOI] [Google Scholar]
- 21.Yu B., Zhao X., Lee L.J., Lee R.J. Targeted Delivery Systems for Oligonucleotide Therapeutics. AAPS J. 2009;11:195–203. doi: 10.1208/s12248-009-9096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Y., Gao D.-Y., Huang L. In vivo delivery of miRNAs for cancer therapy: Challenges and strategies. Adv. Drug Deliv. Rev. 2015;81:128–141. doi: 10.1016/j.addr.2014.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Houseley J., Tollervey D. The many pathways of RNA degradation. Cell. 2009;136:763–776. doi: 10.1016/j.cell.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 24.Hajj K.A., Whitehead K.A. Tools for translation: Non-viral materials for therapeutic mRNA delivery. Nat. Rev. Mater. 2017;2:17056. doi: 10.1038/natrevmats.2017.56. [DOI] [Google Scholar]
- 25.Xiong Q., Lee G.Y., Ding J., Li W., Shi J. Biomedical applications of mRNA nanomedicine. Nano Res. 2018;11:5281–5309. doi: 10.1007/s12274-018-2146-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meng C., Chen Z., Li G., Welte T., Shen H. Nanoplatforms for mRNA Therapeutics. Adv. Ther. 2021;4:2000099. doi: 10.1002/adtp.202000099. [DOI] [Google Scholar]
- 27.Stepinski J., Waddell R., Stolarski R., Darzynkiewicz E., Rhoads R.E. Synthesis and properties of mRNAs containing the novel “anti-reverse” cap analogs 7-methyl(3′-O-methyl)GpppG and 7-methyl (3′-deoxy)GpppG. RNA. 2001;7:1486–1495. [PMC free article] [PubMed] [Google Scholar]
- 28.Beverly M., Hagen C., Slack O. Poly A tail length analysis of in vitro transcribed mRNA by LC-MS. Anal. Bioanal. Chem. 2018;410:1667–1677. doi: 10.1007/s00216-017-0840-6. [DOI] [PubMed] [Google Scholar]
- 29.Holtkamp S., Kreiter S., Selmi A., Simon P., Koslowski M., Huber C., Türeci Ö., Sahin U. Modification of antigen-encoding RNA increases stability, translational efficacy, and T-cell stimulatory capacity of dendritic cells. Blood. 2006;108:4009–4017. doi: 10.1182/blood-2006-04-015024. [DOI] [PubMed] [Google Scholar]
- 30.Suknuntha K., Tao L., Brok-Volchanskaya V., D’Souza S.S., Kumar A., Slukvin I. Optimization of Synthetic mRNA for Highly Efficient Translation and its Application in the Generation of Endothelial and Hematopoietic Cells from Human and Primate Pluripotent Stem Cells. Stem Cell Rev. Rep. 2018;14:525–534. doi: 10.1007/s12015-018-9805-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Russell J., Liebhaber S. The stability of human beta-globin mRNA is dependent on structural determinants positioned within its 3′ untranslated region. Blood. 1996;87:5314–5323. doi: 10.1182/blood.V87.12.5314.bloodjournal87125314. [DOI] [PubMed] [Google Scholar]
- 32.Chung B.K., Lee D.Y. Computational codon optimization of synthetic gene for protein expression. BMC Syst. Biol. 2012;6:134. doi: 10.1186/1752-0509-6-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karikó K., Muramatsu H., Ludwig J., Weissman D. Generating the optimal mRNA for therapy: HPLC purification eliminates immune activation and improves translation of nucleoside-modified, protein-encoding mRNA. Nucleic Acids Res. 2011;39:e142. doi: 10.1093/nar/gkr695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mirzaei S., Gholami M.H., Ang H.L., Hashemi F., Zarrabi A., Zabolian A., Hushmandi K., Delfi M., Khan H., Ashrafizadeh M., et al. Pre-Clinical and Clinical Applications of Small Interfering RNAs (siRNA) and Co-Delivery Systems for Pancreatic Cancer Therapy. Cells. 2021;10:3348. doi: 10.3390/cells10123348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Somia N., Verma I.M. Gene therapy: Trials and tribulations. Nat. Rev. Genet. 2000;1:91–99. doi: 10.1038/35038533. [DOI] [PubMed] [Google Scholar]
- 36.Bouard D., Alazard-Dany N., Cosset F.-L. Viral vectors: From virology to transgene expression. Br. J. Pharmacol. 2009;157:153–165. doi: 10.1038/bjp.2008.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thomas C.E., Ehrhardt A., Kay M.A. Progress and problems with the use of viral vectors for gene therapy. Nat. Rev. Genet. 2003;4:346–358. doi: 10.1038/nrg1066. [DOI] [PubMed] [Google Scholar]
- 38.Bessis N., GarciaCozar F.J., Boissier M.C. Immune responses to gene therapy vectors: Influence on vector function and effector mechanisms. Gene Ther. 2004;11:S10–S17. doi: 10.1038/sj.gt.3302364. [DOI] [PubMed] [Google Scholar]
- 39.Yin H., Kanasty R.L., Eltoukhy A.A., Vegas A.J., Dorkin J.R., Anderson D.G. Non-viral vectors for gene-based therapy. Nat. Rev. Genet. 2014;15:541–555. doi: 10.1038/nrg3763. [DOI] [PubMed] [Google Scholar]
- 40.Sainz-Ramos M., Gallego I., Villate-Beitia I., Zarate J., Maldonado I., Puras G., Pedraz J.L. How Far Are Non-Viral Vectors to Come of Age and Reach Clinical Translation in Gene Therapy? Int. J. Mol. Sci. 2021;22:7545. doi: 10.3390/ijms22147545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peer D., Karp J.M., Hong S., Farokhzad O.C., Margalit R., Langer R. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007;2:751–760. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 42.Hou X., Zaks T., Langer R., Dong Y. Lipid nanoparticles for mRNA delivery. Nat. Rev. Mater. 2021;6:1078–1094. doi: 10.1038/s41578-021-00358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tenchov R., Bird R., Curtze A.E., Zhou Q. Lipid Nanoparticles─From Liposomes to mRNA Vaccine Delivery, a Landscape of Research Diversity and Advancement. ACS Nano. 2021;15:16982–17015. doi: 10.1021/acsnano.1c04996. [DOI] [PubMed] [Google Scholar]
- 44.Rejman J., Tavernier G., Bavarsad N., Demeester J., De Smedt S.C. mRNA transfection of cervical carcinoma and mesenchymal stem cells mediated by cationic carriers. J. Control. Release. 2010;147:385–391. doi: 10.1016/j.jconrel.2010.07.124. [DOI] [PubMed] [Google Scholar]
- 45.Gomes-da-Silva L.C., Fonseca N.A., Moura V., Pedroso de Lima M.C., Simões S., Moreira J.N. Lipid-Based Nanoparticles for siRNA Delivery in Cancer Therapy: Paradigms and Challenges. Acc. Chem. Res. 2012;45:1163–1171. doi: 10.1021/ar300048p. [DOI] [PubMed] [Google Scholar]
- 46.Wu Y., Crawford M., Yu B., Mao Y., Nana-Sinkam S.P., Lee L.J. MicroRNA delivery by cationic lipoplexes for lung cancer therapy. Mol. Pharm. 2011;8:1381–1389. doi: 10.1021/mp2002076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng X., Lee R.J. The role of helper lipids in lipid nanoparticles (LNPs) designed for oligonucleotide delivery. Adv. Drug Deliv. Rev. 2016;99:129–137. doi: 10.1016/j.addr.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 48.Lv H., Zhang S., Wang B., Cui S., Yan J. Toxicity of cationic lipids and cationic polymers in gene delivery. J. Control. Release. 2006;114:100–109. doi: 10.1016/j.jconrel.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 49.Hess P.R., Boczkowski D., Nair S.K., Snyder D., Gilboa E. Vaccination with mRNAs encoding tumor-associated antigens and granulocyte-macrophage colony-stimulating factor efficiently primes CTL responses, but is insufficient to overcome tolerance to a model tumor/self antigen. Cancer Immunol. Immunother. 2006;55:672–683. doi: 10.1007/s00262-005-0064-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Verbeke R., Lentacker I., Wayteck L., Breckpot K., Van Bockstal M., Descamps B., Vanhove C., De Smedt S.C., Dewitte H. Co-delivery of nucleoside-modified mRNA and TLR agonists for cancer immunotherapy: Restoring the immunogenicity of immunosilent mRNA. J. Control. Release. 2017;266:287–300. doi: 10.1016/j.jconrel.2017.09.041. [DOI] [PubMed] [Google Scholar]
- 51.Landesman-Milo D., Peer D. Toxicity profiling of several common RNAi-based nanomedicines: A comparative study. Drug Deliv. Transl. Res. 2014;4:96–103. doi: 10.1007/s13346-013-0158-7. [DOI] [PubMed] [Google Scholar]
- 52.Hajj K.A., Ball R.L., Deluty S.B., Singh S.R., Strelkova D., Knapp C.M., Whitehead K.A. Branched-Tail Lipid Nanoparticles Potently Deliver mRNA In Vivo due to Enhanced Ionization at Endosomal pH. Small. 2019;15:e1805097. doi: 10.1002/smll.201805097. [DOI] [PubMed] [Google Scholar]
- 53.Semple S.C., Akinc A., Chen J., Sandhu A.P., Mui B.L., Cho C.K., Sah D.W.Y., Stebbing D., Crosley E.J., Yaworski E., et al. Rational design of cationic lipids for siRNA delivery. Nat. Biotechnol. 2010;28:172–176. doi: 10.1038/nbt.1602. [DOI] [PubMed] [Google Scholar]
- 54.Oberli M.A., Reichmuth A.M., Dorkin J.R., Mitchell M.J., Fenton O.S., Jaklenec A., Anderson D.G., Langer R., Blankschtein D. Lipid Nanoparticle Assisted mRNA Delivery for Potent Cancer Immunotherapy. Nano Lett. 2017;17:1326–1335. doi: 10.1021/acs.nanolett.6b03329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Akinc A., Maier M.A., Manoharan M., Fitzgerakd K., Jayaraman M., Barros S., Ansell S., Du X., Hope M.J., Madden T.D., et al. The Onpattro story and the clinical translation of nanomedicines containing nucleic acid-based drugs. Nat. Nanotechnol. 2019;14:1084–1087. doi: 10.1038/s41565-019-0591-y. [DOI] [PubMed] [Google Scholar]
- 56.Veiga N., Goldsmith M., Granot Y., Rosenblum D., Dammes N., Kedmi R., Ramishetti S., Peer D. Cell specific delivery of modified mRNA expressing therapeutic proteins to leukocytes. Nat. Commun. 2018;9:4493. doi: 10.1038/s41467-018-06936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jain R., Frederick J.P., Huang E.Y., Burke K.E., Mauger D.M., Adrianova E.A., Farlow S.J., Siddiqui S., Pimentel J., Cheumg-Ong K., et al. MicroRNAs Enable mRNA Therapeutics to Selectively Program Cancer Cells to Self-Destruct. Nucleic Acid Ther. 2018;28:285–296. doi: 10.1089/nat.2018.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sabnis S., Kumarasinghe E.S., Salerno T., Mihai C., Ketova T., Senn J.J., Lynn A., Bulychev A., McFadyen I., Chan J., et al. A Novel Amino Lipid Series for mRNA Delivery: Improved Endosomal Escape and Sustained Pharmacology and Safety in Non-human Primates. Mol. Ther. 2018;26:1509–1519. doi: 10.1016/j.ymthe.2018.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Maier M.A., Jayaraman M., Matsuda S., Liu J., Barros S., Querbes W., Tam Y.K., Ansell S.M., Kumar V., Qin J., et al. Biodegradable lipids enabling rapidly eliminated lipid nanoparticles for systemic delivery of RNAi therapeutics. Mol. Ther. 2013;21:1570–1578. doi: 10.1038/mt.2013.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hassett K.J., Benenato K.E., Jacquinet E., Lee A., Woods A., Yuzhakoy O., Himansu S., Deterling J., Geilich B.M., Ketova T., et al. Optimization of Lipid Nanoparticles for Intramuscular Administration of mRNA Vaccines. Mol. Ther. Nucleic Acids. 2019;15:1–11. doi: 10.1016/j.omtn.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Heyes J., Palmer L., Bremner K., MacLachlan I. Cationic lipid saturation influences intracellular delivery of encapsulated nucleic acids. J. Control. Release. 2005;107:276–287. doi: 10.1016/j.jconrel.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 62.Fenton O.S., Kauffman K.J., McClellan R.L., Appel E.A., Dorkin J.R., Tibbitt M.W., Heartlein M.W., DeRosa F., Langer R., Anderson D.G. Bioinspired Alkenyl Amino Alcohol Ionizable Lipid Materials for Highly Potent In Vivo mRNA Delivery. Adv. Mater. 2016;28:2939–2943. doi: 10.1002/adma.201505822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fenton O.S., Kauffman K.J., Kaczmarek J.C., McClellam R.L., Jhunjhunwala S., Tibbitt M.W., Zeng M.D., Appel E.A., Dorkin J.R., Mir M.W., et al. Synthesis and Biological Evaluation of Ionizable Lipid Materials for the In Vivo Delivery of Messenger RNA to B Lymphocytes. Adv. Mater. 2017;29:1606944. doi: 10.1002/adma.201606944. [DOI] [PubMed] [Google Scholar]
- 64.Costa C., Oliveira I.S., Silva J.P.N., Silva S.G., Botelho C., do Vale M.L.C., Real Oliveira M.E.C.D., Gomes A.C., Marques E.F. Effective cytocompatible nanovectors based on serine-derived gemini surfactants and monoolein for small interfering RNA delivery. J. Colloid Interface Sci. 2021;584:34–44. doi: 10.1016/j.jcis.2020.09.077. [DOI] [PubMed] [Google Scholar]
- 65.Ezzati Nazhad Dolatabadi J., Valizadeh H., Hamishehkar H. Solid Lipid Nanoparticles as Efficient Drug and Gene Delivery Systems: Recent Breakthroughs. Adv. Pharm. Bull. 2015;5:151–159. doi: 10.15171/apb.2015.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.del Pozo-Rodríguez A., Solinís M.A., Gascón A.R., Pedraz J.L. Short- and long-term stability study of lyophilized solid lipid nanoparticles for gene therapy. Eur. J. Pharm. Biopharm. 2009;71:181–189. doi: 10.1016/j.ejpb.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 67.Scioli Montoto S., Muraca G., Ruiz M.E. Solid Lipid Nanoparticles for Drug Delivery: Pharmacological and Biopharmaceutical Aspects. Front. Mol. Biosci. 2020;7:319. doi: 10.3389/fmolb.2020.587997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu T., Zhang X., Du L., Wang Y., Liu X., Tian H., Wang L., Li P., Zhao Y., Duan W., et al. Exosome-transmitted miR-128-3p increase chemosensitivity of oxaliplatin-resistant colorectal cancer. Mol. Cancer. 2019;18:43. doi: 10.1186/s12943-019-0981-7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 69.Baldari S., Di Rocco G., Magenta A., Picozza M., Toietta G. Extracellular Vesicles–Encapsulated MicroRNA-125b Produced in Genetically Modified Mesenchymal Stromal Cells Inhibits Hepatocellular Carcinoma Cell Proliferation. Cells. 2019;8:1560. doi: 10.3390/cells8121560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yuan L., Liu Y., Qu Y., Liu L., Li H. Exosomes Derived From MicroRNA-148b-3p-Overexpressing Human Umbilical Cord Mesenchymal Stem Cells Restrain Breast Cancer Progression. Front. Oncol. 2019;9:1076. doi: 10.3389/fonc.2019.01076. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.Li X., Liu L.L., Yao J.L., Wang K., Ai H. Human Umbilical Cord Mesenchymal Stem Cell-Derived Extracellular Vesicles Inhibit Endometrial Cancer Cell Proliferation and Migration through Delivery of Exogenous miR-302a. Stem Cells Int. 2019;2019:8108576. doi: 10.1155/2019/8108576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gilligan K.E., Dwyer R.M. Engineering Exosomes for Cancer Therapy. Int. J. Mol. Sci. 2017;18:1122. doi: 10.3390/ijms18061122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ingenito F., Roscigno G., Affinito A., Nuzzo S., Scognamiglio I., Quintavalle C., Condorelli G. The Role of Exo-miRNAs in Cancer: A Focus on Therapeutic and Diagnostic Applications. Int. J. Mol. Sci. 2019;20:4687. doi: 10.3390/ijms20194687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shtam T.A., Kovalev R.A., Varfolomeeva E.Y., Makarov E.M., Kil Y.V., Filatov M.V. Exosomes are natural carriers of exogenous siRNA to human cells in vitro. Cell Commun. Signal. 2013;11:88. doi: 10.1186/1478-811X-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Allan D., Tieu A., Lalu M., Burger D. Mesenchymal stromal cell-derived extracellular vesicles for regenerative therapy and immune modulation: Progress and challenges toward clinical application. Stem Cells Transl. Med. 2019;9:39–46. doi: 10.1002/sctm.19-0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang E., Xing R., Liu S., Qin Y., Li K., Li P. Advances in chitosan-based nanoparticles for oncotherapy. Carbohy. Polym. 2019;222:115004. doi: 10.1016/j.carbpol.2019.115004. [DOI] [PubMed] [Google Scholar]
- 77.Garcia-Fuentes M., Alonso M.J. Chitosan-based drug nanocarriers: Where do we stand? J. Control. Release. 2012;161:496–504. doi: 10.1016/j.jconrel.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 78.Ashrafizadeh M., Delfi M., Hashemi F., Zabolian A., Saleki H., Bagherian M., Azami N., Farahani M.V., Sharifzadeh S.O., Hamzehlou S., et al. Biomedical application of chitosan-based nanoscale delivery systems: Potential usefulness in siRNA delivery for cancer therapy. Carbohydr. Polym. 2021;260:117809. doi: 10.1016/j.carbpol.2021.117809. [DOI] [PubMed] [Google Scholar]
- 79.Chen H., Cui S., Zhao Y., Zhang C., Zhang S., Peng X. Grafting Chitosan with Polyethylenimine in an Ionic Liquid for Efficient Gene Delivery. PLoS ONE. 2015;10:e0121817. doi: 10.1371/journal.pone.0121817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lu H., Lv L., Dai Y., Wu G., Zhao H., Zhang F. Porous chitosan scaffolds with embedded hyaluronic acid/chitosan/plasmid-DNA nanoparticles encoding TGF-β1 induce DNA controlled release, transfected chondrocytes, and promoted cell proliferation. PLoS ONE. 2013;8:e69950. doi: 10.1371/journal.pone.0069950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ragelle H., Vandermeulen G., Préat V. Chitosan-based siRNA delivery systems. J. Control. Release. 2013;172:207–218. doi: 10.1016/j.jconrel.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 82.Wang J.J., Zeng Z.W., Xiao R.Z., Xie T., Zhou G.L., Zhan X.R., Wang S.L. Recent advances of chitosan nanoparticles as drug carriers. Int. J. Nanomed. 2011;6:765–774. doi: 10.2147/IJN.S17296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alinejad V., Somi M.H., Baradaran B., Akbarzadeh P., Atyabi F., Kazerooni H., Kafil B., Maleki L.A., Mansouri H.S., Yousefi M. Co-delivery of IL17RB siRNA and doxorubicin by chitosan-based nanoparticles for enhanced anticancer efficacy in breast cancer cells. Biomed. Pharmacother. 2016;83:229–240. doi: 10.1016/j.biopha.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 84.Sadreddini S., Safaralizadeh R., Baradaran B., Aghebati-Maleki L., Hosseinpour-Feizi M., Shanehbandi D., Jadidi-Niaragh F., Sadreddini S., Kafil H.S., Younesi V., et al. Chitosan nanoparticles as a dual drug/siRNA delivery system for treatment of colorectal cancer. Immunol. Lett. 2017;181:79–86. doi: 10.1016/j.imlet.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 85.Siahmansouri H., Somi M.H., Babaloo Z., Baradaran B., Jadidi-Niaragh F., Atyabi F., Mohammadi H., Ahmadi M., Yousefi M. Effects of HMGA2 siRNA and doxorubicin dual delivery by chitosan nanoparticles on cytotoxicity and gene expression of HT-29 colorectal cancer cell line. J. Pharm. Pharmacol. 2016;68:1119–1130. doi: 10.1111/jphp.12593. [DOI] [PubMed] [Google Scholar]
- 86.Neu M., Fischer D., Kissel T. Recent advances in rational gene transfer vector design based on poly(ethylene imine) and its derivatives. J. Gene Med. 2005;7:992–1009. doi: 10.1002/jgm.773. [DOI] [PubMed] [Google Scholar]
- 87.Akinc A., Thomas M., Klibanov A.M., Langer R. Exploring polyethylenimine-mediated DNA transfection and the proton sponge hypothesis. J. Gene Med. 2005;7:657–663. doi: 10.1002/jgm.696. [DOI] [PubMed] [Google Scholar]
- 88.Johler S.M., Rejman J., Guan S., Rosenecker J. Nebulisation of IVT mRNA Complexes for Intrapulmonary Administration. PLoS ONE. 2015;10:e0137504. doi: 10.1371/journal.pone.0137504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tan L., Zheng T., Li M., Zhong X., Tang Y., Qin M., Sun X. Optimization of an mRNA vaccine assisted with cyclodextrin-polyethyleneimine conjugates. Drug Deliv. Transl. Res. 2020;10:678–689. doi: 10.1007/s13346-020-00725-4. [DOI] [PubMed] [Google Scholar]
- 90.Chiper M., Tounsi N., Kole R., Kichler A., Zuber G. Self-aggregating 1.8 kDa polyethylenimines with dissolution switch at endosomal acidic pH are delivery carriers for plasmid DNA, mRNA, siRNA and exon-skipping oligonucleotides. J. Control. Release. 2017;246:60–70. doi: 10.1016/j.jconrel.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 91.Zhao M., Li M., Zhang Z., Gong T., Sun X. Induction of HIV-1 gag specific immune responses by cationic micelles mediated delivery of gag mRNA. Drug Deliv. 2016;23:2596–2607. doi: 10.3109/10717544.2015.1038856. [DOI] [PubMed] [Google Scholar]
- 92.Svenson S., Tomalia D.A. Dendrimers in biomedical applications—reflections on the field. Adv. Drug Deliv. Rev. 2012;64:102–115. doi: 10.1016/j.addr.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 93.Shan Y., Luo T.L., Peng C., Sheng R., Cao A., Shen M., Guo R., Tomás H., Shi X. Gene delivery using dendrimer-entrapped gold nanoparticles as nonviral vectors. Biomaterials. 2012;33:3025–3035. doi: 10.1016/j.biomaterials.2011.12.045. [DOI] [PubMed] [Google Scholar]
- 94.Khandare J., Calderón M., Dagia N.M., Haag R. Multifunctional dendritic polymers in nanomedicine: Opportunities and challenges. Chem. Soc. Rev. 2012;41:2824–2848. doi: 10.1039/C1CS15242D. [DOI] [PubMed] [Google Scholar]
- 95.Liu X., Liu C., Zhou J., Chen C., Qu F., Rossi J.J., Rocchi P., Peng L. Promoting siRNA delivery via enhanced cellular uptake using an arginine-decorated amphiphilic dendrimer. Nanoscale. 2015;7:3867–3875. doi: 10.1039/C4NR04759A. [DOI] [PubMed] [Google Scholar]
- 96.Chandra S., Mehta S., Nigam S., Bahadur D. Dendritic magnetite nanocarriers for drug delivery applications. New J. Chem. 2010;34:648–655. doi: 10.1039/b9nj00609e. [DOI] [Google Scholar]
- 97.Liu W.-M., Xue Y.-N., Peng N., He W.-T., Zhuo R.-X., Huang S.-W. Dendrimer modified magnetic iron oxide nanoparticle/DNA/PEI ternary magnetoplexes: A novel strategy for magnetofection. J. Mater. Chem. 2011;21:13306–13315. doi: 10.1039/c1jm11460c. [DOI] [Google Scholar]
- 98.Pan B., Cui D., Sheng Y., Ozkan C., Gao F., He R., Li Q., Xu P., Huang T. Dendrimer-modified magnetic nanoparticles enhance efficiency of gene delivery system. Cancer Res. 2007;67:8156–8163. doi: 10.1158/0008-5472.CAN-06-4762. [DOI] [PubMed] [Google Scholar]
- 99.Shi X., Wang S., Sun H., Baker J.R., Jr. Improved biocompatibility of surface functionalized dendrimer-entrapped gold nanoparticles. Soft Matter. 2006;3:71–74. doi: 10.1039/B612972B. [DOI] [PubMed] [Google Scholar]
- 100.Shi X., Wang S., Meshinchi S., Van Antwerp M.E., Bi X., Lee I., Baker J.R., Jr. Dendrimer-entrapped gold nanoparticles as a platform for cancer-cell targeting and imaging. Small. 2007;3:1245–1252. doi: 10.1002/smll.200700054. [DOI] [PubMed] [Google Scholar]
- 101.Pinelli F., Perale G., Rossi F. Coating and Functionalization Strategies for Nanogels and Nanoparticles for Selective Drug Delivery. Gels. 2020;6:6. doi: 10.3390/gels6010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li Y., Maciel D., Rodrigues J., Shi X., Tomás H. Biodegradable Polymer Nanogels for Drug/Nucleic Acid Delivery. Chem. Rev. 2015;115:8564–8608. doi: 10.1021/cr500131f. [DOI] [PubMed] [Google Scholar]
- 103.Zhang H., Zhai Y., Wang J., Zhai G. New progress and prospects: The application of nanogel in drug delivery. Mater. Sci. Eng. C Mater. Biol. Appl. 2016;60:560–568. doi: 10.1016/j.msec.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 104.Li H., Yang X., Gao F., Qian C., Li C., Oupicky D., Sun M. Bioreduction-ruptured nanogel for switch on/off release of Bcl2 siRNA in breast tumor therapy. J. Control. Release. 2018;292:78–90. doi: 10.1016/j.jconrel.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 105.Roy I., Mitra S., Maitra A., Mozumdar S. Calcium phosphate nanoparticles as novel non-viral vectors for targeted gene delivery. Int. J. Pharm. 2003;250:25–33. doi: 10.1016/S0378-5173(02)00452-0. [DOI] [PubMed] [Google Scholar]
- 106.Li J., Yang Y., Huang L. Calcium phosphate nanoparticles with an asymmetric lipid bilayer coating for siRNA delivery to the tumor. J. Control. Release. 2012;158:108–114. doi: 10.1016/j.jconrel.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yang Y., Hu Y., Wang Y., Li J., Liu F., Huang L. Nanoparticle Delivery of Pooled siRNA for Effective Treatment of Non-Small Cell Lung Caner. Mol. Pharm. 2012;9:2280–2289. doi: 10.1021/mp300152v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Li J., Chen Y.C., Tseng Y.C., Mozumdar S., Huang L. Biodegradable calcium phosphate nanoparticle with lipid coating for systemic siRNA delivery. J. Control. Release. 2010;142:416–421. doi: 10.1016/j.jconrel.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xie Y., Chen Y., Sun M., Ping Q. A mini review of biodegradable calcium phosphate nanoparticles for gene delivery. Curr. Pharm. Biotechnol. 2013;14:918–925. doi: 10.2174/1389201014666131226145441. [DOI] [PubMed] [Google Scholar]
- 110.Wang Y., Zhang L., Xu Z., Miao L., Huang L. mRNA Vaccine with Antigen-Specific Checkpoint Blockade Induces an Enhanced Immune Response against Established Melanoma. Mol. Ther. 2018;26:420–434. doi: 10.1016/j.ymthe.2017.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shukla R., Bansal V., Chaudhary M., Basu A., Bhonde R.R., Sastry M. Biocompatibility of Gold Nanoparticles and Their Endocytotic Fate Inside the Cellular Compartment: A Microscopic Overview. Langmuir. 2005;21:10644–10654. doi: 10.1021/la0513712. [DOI] [PubMed] [Google Scholar]
- 112.Ali H.S., El-Haj B.M., Saifullah S., Kawish M. Chapter 4—Gold nanoparticles in cancer diagnosis and therapy. In: Shah M.R., Imran M., Ullah S., editors. Metal Nanoparticles for Drug Delivery and Diagnostic Applications. Elsevier; Amsterdam, The Netherlands: 2020. pp. 43–58. [Google Scholar]
- 113.Mendes R., Fernandes A.R., Baptista P.V. Gold Nanoparticle Approach to the Selective Delivery of Gene Silencing in Cancer—The Case for Combined Delivery? Genes. 2017;8:94. doi: 10.3390/genes8030094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ghosh R., Singh L.C., Shohet J.M., Gunaratne P.H. A gold nanoparticle platform for the delivery of functional microRNAs into cancer cells. Biomaterials. 2013;34:807–816. doi: 10.1016/j.biomaterials.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 115.Foldvari M., Bagonluri M. Carbon nanotubes as functional excipients for nanomedicines: II. Drug delivery and biocompatibility issues. Nanomed. Nanotechnol. Biol. Med. 2008;4:183–200. doi: 10.1016/j.nano.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 116.Bates K., Kostarelos K. Carbon nanotubes as vectors for gene therapy: Past achievements, present challenges and future goals. Adv. Drug Deliv. Rev. 2013;65:2023–2033. doi: 10.1016/j.addr.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 117.Kam N.W.S., Liu Z., Dai H. Functionalization of Carbon Nanotubes via Cleavable Disulfide Bonds for Efficient Intracellular Delivery of siRNA and Potent Gene Silencing. J. Am. Chem. Soc. 2005;127:12492–12493. doi: 10.1021/ja053962k. [DOI] [PubMed] [Google Scholar]
- 118.Krajcik R., Jung A., Hirsch A., Neuhuber W., Zolk O. Functionalization of carbon nanotubes enables non-covalent binding and intracellular delivery of small interfering RNA for efficient knock-down of genes. Biochem. Biophys. Res. Commun. 2008;369:595–602. doi: 10.1016/j.bbrc.2008.02.072. [DOI] [PubMed] [Google Scholar]
- 119.Zhang Z., Yang X., Zhang Y., Zeng B., Wang S., Zhu T., Roden R.B., Chen Y., Yang R. Delivery of telomerase reverse transcriptase small interfering RNA in complex with positively charged single-walled carbon nanotubes suppresses tumor growth. Clin. Cancer Res. 2006;12:4933–4939. doi: 10.1158/1078-0432.CCR-05-2831. [DOI] [PubMed] [Google Scholar]
- 120.Wang X., Ren J., Qu X. Targeted RNA Interference of Cyclin A2 Mediated by Functionalized Single-Walled Carbon Nanotubes Induces Proliferation Arrest and Apoptosis in Chronic Myelogenous Leukemia K562 Cells. ChemMedChem. 2008;3:940–945. doi: 10.1002/cmdc.200700329. [DOI] [PubMed] [Google Scholar]
- 121.Podesta J.E., Al-Jamal K.T., Herrero M.A., Tian B., Ali-Boucetta H., Hegde V., Bianco A., Prato M., Kostarelos K. Antitumor Activity and Prolonged Survival by Carbon-Nanotube-Mediated Therapeutic siRNA Silencing in a Human Lung Xenograft Model. Small. 2009;5:1176–1185. doi: 10.1002/smll.200801572. [DOI] [PubMed] [Google Scholar]
- 122.Al-Jamal K.T., Toma F.M., Yilmazerm A., Ali-Boucetta H., Nunes A., Herrero M.-A., Tian B., Eddaoudi A., Al-Jamal W., Bianco A., et al. Enhanced cellular internalization and gene silencing with a series of cationic dendron-multiwalled carbon nanotube:siRNA complexes. FASEB J. 2010;24:4354–4365. doi: 10.1096/fj.09-141036. [DOI] [PubMed] [Google Scholar]
- 123.Vallet-Regi M., Rámila A., del Real R.P., Pérez-Pariente J. A New Property of MCM-41: Drug Delivery System. Chem. Mater. 2001;13:308–311. doi: 10.1021/cm0011559. [DOI] [Google Scholar]
- 124.Hom C., Lu J., Liong M., Luo H., Li Z., Zink J.I., Tamanoi F. Mesoporous silica nanoparticles facilitate delivery of siRNA to shutdown signaling pathways in mammalian cells. Small. 2010;6:1185–1190. doi: 10.1002/smll.200901966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Slowing I.I., Vivero-Escoto J.L., Wu C.-W., Lin V.S.Y. Mesoporous silica nanoparticles as controlled release drug delivery and gene transfection carriers. Adv. Drug Deliv. Rev. 2008;60:1278–1288. doi: 10.1016/j.addr.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 126.Ngamcherdtrakul W., Morry J., Gu S., Castro D.J., Goodyear S.M., Sangvanich T., Reda M.M., Lee R., Mihelic S., Beckman B.L., et al. Cationic Polymer Modified Mesoporous Silica Nanoparticles for Targeted siRNA Delivery to HER2+ Breast Cancer. Adv. Funct. Mater. 2015;25:2646–2659. doi: 10.1002/adfm.201404629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shen J., Kim H.-C., Su H., Wang F., Wolfram J., Kirui D., Mai J., Mu C., Ji L.-N., Mao Z.-W., et al. Cyclodextrin and polyethylenimine functionalized mesoporous silica nanoparticles for delivery of siRNA cancer therapeutics. Theranostics. 2014;4:487–497. doi: 10.7150/thno.8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tivnan A., Orr W.S., Gubala V., Nooney R., Williams D.E., McDonagh C., Prenter S., Harvey H., Domingo-Fernández R., Bray I.M., et al. Inhibition of neuroblastoma tumor growth by targeted delivery of microRNA-34a using anti-disialoganglioside GD2 coated nanoparticles. PLoS ONE. 2012;7:e38129. doi: 10.1371/journal.pone.0038129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Pankhurst Q.A., Connolly J., Jones S.K., Dobson J. Applications of magnetic nanoparticles in biomedicine. J. Phys. D Appl. Phys. 2003;36:R167–R181. doi: 10.1088/0022-3727/36/13/201. [DOI] [Google Scholar]
- 130.Gupta A.K., Gupta M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 2005;26:3995–4021. doi: 10.1016/j.biomaterials.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 131.Cruz-Acuña M., Halman J.R., Afonin K.A., Dobson J., Rinaldi C. Magnetic nanoparticles loaded with functional RNA nanoparticles. Nanoscale. 2018;10:17761–17770. doi: 10.1039/C8NR04254C. [DOI] [PubMed] [Google Scholar]
- 132.Plank C., Zelphati O., Mykhaylyk O. Magnetically enhanced nucleic acid delivery. Ten years of magnetofection—Progress and prospects. Adv. Drug Deliv. Rev. 2011;63:1300–1331. doi: 10.1016/j.addr.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Luo X., Peng X., Hou J., Wu S., Shen J., Wang L. Folic acid-functionalized polyethylenimine superparamagnetic iron oxide nanoparticles as theranostic agents for magnetic resonance imaging and PD-L1 siRNA delivery for gastric cancer. Int. J. Nanomed. 2017;12:5331–5343. doi: 10.2147/IJN.S137245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rai R., Alwani S., Badea I. Polymeric Nanoparticles in Gene Therapy: New Avenues of Design and Optimization for Delivery Applications. Polymers. 2019;11:745. doi: 10.3390/polym11040745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kus-Liśkiewicz M., Fickers P., Ben Tahar I. Biocompatibility and Cytotoxicity of Gold Nanoparticles: Recent Advances in Methodologies and Regulations. Int. J. Mol. Sci. 2021;22:10952. doi: 10.3390/ijms222010952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Arias L.S., Pessan J.P., Vieira A.P.M., Lima T.M.T.d., Delbem A.C.B., Monteiro D.R. Iron Oxide Nanoparticles for Biomedical Applications: A Perspective on Synthesis, Drugs, Antimicrobial Activity, and Toxicity. Antibiotics. 2018;7:46. doi: 10.3390/antibiotics7020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Demeure M.J., Armaghany T., Ejadi S., Ramanathan R.K., Elfiky A., Strosberg J.R., Smith D.C., Whitsett T., Liang W.S., Sekar S., et al. A phase I/II study of TKM-080301, a PLK1-targeted RNAi in patients with adrenocortical cancer (ACC) J. Clin. Oncol. 2016;34:2547. doi: 10.1200/JCO.2016.34.15_suppl.2547. [DOI] [Google Scholar]
- 138.El Dika I., Lim H.Y., Yong W.P., Lin C.-C., Yoon J.-H., Modiano M., Freilich B., Choi H.J., Chao T.-Y., Kelley R.K., et al. An Open-Label, Multicenter, Phase I, Dose Escalation Study with Phase II Expansion Cohort to Determine the Safety, Pharmacokinetics, and Preliminary Antitumor Activity of Intravenous TKM-080301 in Subjects with Advanced Hepatocellular Carcinoma. Oncologist. 2019;24:747-e218. doi: 10.1634/theoncologist.2018-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Thi T.T.H., Suys E.J.A., Lee J.S., Nguyen D.H., Park K.D., Truong N.P. Lipid-Based Nanoparticles in the Clinic and Clinical Trials: From Cancer Nanomedicine to COVID-19 Vaccines. Vaccines. 2021;9:359. doi: 10.3390/vaccines9040359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tolcher A.W., Papadopoulos K.P., Patnaik A., Rasco D.W., Martinez D., Fielman D.L.W., Sharma M., Janisch L.A., Brown B.D., Bhargavam P., et al. Safety and activity of DCR-MYC, a first-in-class Dicer-substrate small interfering RNA (DsiRNA) targeting MYC, in a phase I study in patients with advanced solid tumors. J. Clin. Oncol. 2015;33:11006. doi: 10.1200/jco.2015.33.15_suppl.11006. [DOI] [Google Scholar]