Abstract
This study examined the associations of moderate-to-vigorous intensity physical activity (MVPA) trajectories in adolescence through young adulthood with adiposity in young adults. Participants from The Iowa Bone Development Study cohort were longitudinally assessed (N = 297; 57% female). Accelerometry-measured MVPA (min/day) at ages 15 through 23 years, and fat mass and visceral adipose tissue mass indices (kg/m2, g/m2) derived from dual-energy X-ray absorptiometry scans at age 23 years were analyzed. Latent trajectory analyses classified MVPA into two patterns. Multivariable linear regression analyses showed that being in the high MVPA trajectory group was associated with lower fat mass index z-scores. Individuals who were consistently active with high MVPA (vs. moderately active with decreasing MVPA) during adolescence up until early young adulthood had less accumulation of total body adiposity in young adulthood. This study suggests that adopting a consistently active lifestyle throughout adolescence can result in healthier body composition in young adulthood.
Keywords: Physical activity, Trajector, Young adulthood, Fat mass index
Introduction
Moderate-to-vigorous intensity physical activity (MVPA) has been widely recommended as a critical lifestyle behavior for maintaining health in people of all ages, including youth. The US federal physical activity guidelines recommend a minimum of 60 min/day of MVPA in youth; (Powell et al., 2019) however, the majority of youth in the U.S. (approximately 75%) do not meet the guidelines (Katzmarzyk et al., 2016; Troiano et al., 2008) and obesity prevalence in youth has been steadily increasing (Hales et al., 2017). Previous studies suggest that habitual MVPA is associated negatively with adiposity status in youth (Janz et al., 2017; Katzmarzyk et al., 2015; Kwon et al., 2013, 2015), and maintaining adequate levels of MVPA in youth could be a critical determinant in avoiding the development of adulthood obesity (Nelson et al., 2008).
Young adulthood is a unique transitional point in life where young adults experience dramatic changes in body weight (Hebden et al., 2012) and when lifelong health behaviors (e.g., dietary intake, physical activity) are established (Nelson et al., 2008); however, little is known about the longitudinal associations of health behaviors with body composition and health outcomes in young adults (Nanney et al., 2015). Most young adults leave their parents’ homes and this can result in an unhealthy lifestyle (e.g., increased TV viewing, alcohol consumption, and poor diet quality) (Nanney et al., 2015; Nelson et al., 2008). In addition, the prevalence of obesity accelerates in late adolescence through young adulthood in their 20 s and 30 s, compared to other age ranges (Gordon-Larsen et al., 2010; Hebden et al., 2012), and young adults gain body weight faster than other age groups (Hebden et al., 2012). Despite the evidence demonstrating the lifestyle-based transitions that take place during young adulthood, the associations between MVPA patterns and adiposity development remain unclear in this population. Several longitudinal studies examining physical activity behavior changes from childhood to adolescence have demonstrated declines of habitual MVPA in youth over time in both males and females (Farooq et al., 2018; Kwon et al., 2015; Pate et al., 2019). Robust evidence shows that MVPA has a beneficial role in adiposity indicators and health outcomes in youth and young adulthood; however, it is unclear whether changes in MVPA in adolescence and early young adulthood predict or alter adiposity in young adulthood.
Researchers frequently have used body mass index and percent body fat in health research. However, these methods have been acknowledged as suboptimal approaches for representing true body fatness or studying health risks because body mass index (body weight divided by height squared) does not differentiate body fat from body fat-free mass (Lavie et al., 2010) and relies on height (i.e., not appropriately adjusting for body size) (Schooling et al., 2007), and percent body fat cannot be determined independent of body fat-free mass (Ellis et al., 1999). Therefore, fat mass index (FMI) seems to be a better screening method than body mass index or percent body fat as a total body adiposity index in health outcomes research (Kyle et al., 2003; Liu et al., 2013), because it acknowledges fat-free mass and adjusts body size by height (VanItallie et al., 1990). In addition, the type or location of body fat is important for health outcomes, because abdominal visceral adipose tissue (VAT) is metabolically more active (e.g., secretes more inflammatory cytokines or free fatty acids) than other types of fat depots and is closely-associated with many chronic diseases (Smith et al., 2001). In this study, we used FMI as a primary outcome and, to the best of our knowledge, this study is the first investigation to use VAT mass index (VAT mass divided by height squared) in a manner analogous to FMI. We hypothesize that a new application of VAT mass index, in addition to FMI (using a two-compartment model), will be a better indicator of adiposity for health research.
Few longitudinal studies (Farooq et al., 2018; Kwon et al., 2015; Pate et al., 2019) employing group-based trajectory modeling have shown physical activity patterns over time in childhood and adolescence. Pate et al. (2019) found three different shapes of trajectory (two gradually decreased and one gradually increased) of overall physical activity (not sex-specific) in youth ages 10–16 years and Farooq et al. (2018) reported three (in boys) and four (in girls) trajectories (all were gradually decreased from the different starting points) of MVPA in youth ages 7–15 years. The Kwon study (2015), which included children up to young adults ages 5–19 years, reported two maintained and two gradually decreased patterns of MVPA trajectories (not sex-specific). Overall trends of physical activity indicated by trajectory modeling reported in the previous studies were very similar over time (i.e., MVPA gradually decreased with age). Consistent with the previous studies, a recent review and meta-analysis (tracking longitudinally-observed MVPA in youth) published by Farooq et al. (2020) showed decreased MVPA patterns in youth, and also this review study suggested that there are ‘far fewer’ studies examining MVPA patterns especially in late adolescence (i.e., above 15 years old). Despite the evidence that a decline in MVPA during adolescence (Corder et al., 2016; Dumith et al., 2011; Farooq et al., 2018; Li et al., 2016; Pate et al., 2019) could be a risk factor for future obesity (Yang et al., 2006), the evidence is inconclusive on the relationships between distinct MVPA patterns and adiposity in young adulthood.
The objective of this study was to examine the associations between MVPA patterns assessed longitudinally from ages 15–23 years and adiposity indicators (i.e., FMI and VAT mass indices) at age 23 years. We hypothesized that individuals with a healthy MVPA trajectory (i.e., increased, or being consistently active) from adolescence to early young adulthood will have lower levels of adiposity indicators at age 23 years when compared to individuals with a less healthy MVPA trajectory.
Methods
Study participants
Study participants were a subset of Midwestern residents (recruited through their parents when they were approximately 5 years of age between 1998 and 2001) from a cohort of 890 families then participating in the Iowa Fluoride Study. This subset of the Iowa Fluoride Study cohort participated in The Iowa Bone Development Study (IBDS), a longitudinal cohort study investigating levels of physical activity, bone health, body composition, and other factors during childhood, adolescence, and young adulthood. Among the IBDS cohort of 630 individuals (approximately 50% female), approximately 95% of participants were white and 72% of their parents had college degrees or higher education. Additional information about the IBDS study participants and design can be found elsewhere (Janz et al., 2005). This report uses the data collected between 2007 and 2017 when participants were approximately 15, 17, 19, 21, and 23 years of age (data collection waves 5–9, respectively). The University of Iowa Institutional Review Board approved the IBDS and written informed consent was obtained from all participants and their parents (when participants were aged 15 and 17 years).
Measurements
Physical activity
MVPA (min/day) was measured by ActiGraph accelerometers (Pensacola, FL, USA) using the model GT1m for wave 5 (approximately aged 15 years) and GT3x + for waves 6–9 (approximately aged 17–23 years). Accelerometers were mailed to participants and collected during the autumn season (September–November). They were asked to wear the accelerometer on their waist during waking hours for 5 consecutive days, including both weekend days. Accelerometer data were considered valid if participants wore the monitor for ≥ 4 days and ≥ 10 h/day, consistent with the NHANES criteria (Evenson et al., 2008). The 2-regression equation model from Crouter et al. (2010) was applied to estimate physical activity intensity. MVPA was defined as an activity count ≥ 297 counts per 10-s (Crouter et al., 2010). Activities were measured by 10-s epochs within each minute, and the combinations of 6 continuous 10-s epochs were converted to 1-min epochs (Crouter et al., 2010). The 2-regression equation model developed by Crouter et al. (2010) distinguishes between sporadic lifestyle activity and consecutive ambulatory activity, thus reducing the limitations of single regression equations developed using either walking and running (Brage et al., 2003; Freedson et al., 1998; Leenders et al., 2003) or moderate-intensity lifestyle activities (Hendelman et al., 2000). In general, the previously-developed single regression equations for walking and jogging slightly overestimate the energy expenditure of walking and light-intensity activities, and they greatly underestimate the energy expenditure of moderate-intensity lifestyle activities (Crouter et al., 2010). In addition, evidence in the literature demonstrated that a 1-min epoch (vs. a short-interval epoch) would significantly underestimate activity intensity (Welk, 2002).
Anthropometry and adiposity
Participants’ height (cm) and weight (kg) were assessed by trained nurses using a Harpenden stadiometer (Holtain Ltd., Crosswell, UK) and a Healthometer physician’s scale (Continental, Bridgeview, IL), respectively, during each study visit. Total body fat and VAT were obtained from the analysis of whole-body scans using dual-energy X-ray absorptiometry (DXA) obtained with the Hologic QDR 4500 and Discovery (Delphi upgrade, Hologic, Inc., Waltham, MA) for wave 5 and 9 (at approximately aged 15 and 23 years). Both scans at waves 5 and 9 were analyzed with the NHANES calibration method for fat mass estimation (Kelly et al., 2009), and VAT was estimated using APEX 4.0 software version. FMI and VAT mass index were calculated as fat mass (kg) and VAT mass (g), respectively, divided by height squared (m2). The DXA was registered in the state of Iowa, and safety compliance was confirmed by the Health Protection Office at the University of Iowa.
Diet (covariate)
Diet quality was estimated at waves 8 and 9 (at approximately aged 21 and 23 years, respectively) using the Healthy Eating Index (HEI) (Guo et al., 2004) score (0–100; higher score indicates a healthier diet pattern) derived from the Diet History Questionnaire (Block et al., 1990; Cullen et al., 2008), which has been consistently associated with health outcomes and adiposity (Guo et al., 2004; Togo et al., 2001). We included HEI scores when participants were aged 23 years (wave 9) in our regression models as a potential confounder in the associations between MVPA and adiposity.
Statistical analyses
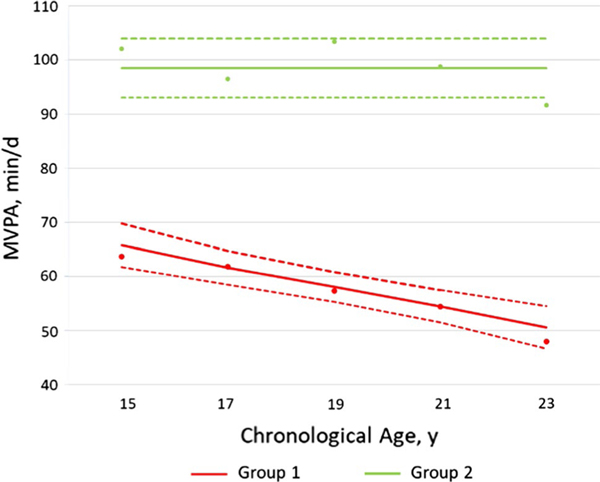
Mean MVPA (min/day) by sex, wave (age), and MVPA trajectory groups were calculated. Sex-specific descriptive analyses were conducted to describe body composition, FMI, and VAT at age 23 years. Comparisons by sex were performed using either independent samples t test or the Mann–Whitney–Wilcoxon test as appropriate. Sex-specific linear models (SAS MIXED procedure, version 9.4; SAS Institute, Inc, Cary, NC) with age polynomials as predictors and autoregressive residual covariance structure for repeated observation on the subject over time were used to describe the overall MVPA trends across late adolescence and early adulthood. Autoregressive residual covariance structure was appropriate because based on our analysis, the correlation between PA estimates weakens as time between measurements increases. First-degree polynomials (linear models) were found adequate for the overall trend description. Each participant’s MVPA data from approximate ages 15 through 23 years (waves 5–9) were used to identify distinct physical activity patterns using group-based trajectory analyses software (SAS TRAJ procedure, version 9.4; SAS Institute, Inc, Cary, NC, USA) (Jones & Nagin, 2007). Trajectory analyses included all participants with at least three estimates of MVPA, with the first at wave 5 or 6 (age 15 and 17) and last at wave 8 or 9 (age 21 and 23). As recommended by Nagin (2005), we used a two-step approach to find the best possible solution for determining the number of groups. First, we identified an adequate number of groups, and a quadratic model was initially used for trajectory shapes for all groups. We created 4, 3, and 2-group solution by comparing values of the Bayesian Information Criterion (BIC) and the proportion of cohort members in each group. While BIC values were somewhat better in 4-group solution (BIC: − 4531.1) or 3-group solution (BIC: − 4527.9) when compared with 2-group solution (BIC: − 4556.2), additional groups had very small sample sizes (the smallest with < 1% of total cohort members). For reference, additional statistics for the trajectory group selection process are presented in Supplementary Table. Therefore, we proceeded to the next step in the model selection process with 2 groups. At that step, the degree of the polynomial for each group (i.e., quadratic, linear, and constant) was reduced until the parameter estimate for the highest degree polynomial effect had an associated p-value < 0.01. Model adequacy was tested using the diagnostic measures: the average posterior probability of assignment for each group is ≥ 0.7; odds of correct classification are ≥ 5 for group membership; and the difference between estimated group probabilities (or reasonably close correspondence between a group’s estimated probability) and the proportion of individuals assigned to the group using the maximum posterior probability rule (Nagin, 2005; Niyonkuru et al., 2013). Each participant was assigned to the trajectory group with the highest posterior membership probability. The two homogeneous (latent) trajectory groups were characterized as follows: group 1 as a reference = ‘moderately-active with decreasing MVPA’ and group 2 = ‘consistently-active with high MVPA’ (Fig. 1). To examine whether latent groups were predictive of FMI and VAT mass index, multivariable linear regression analyses were performed. FMI and VAT mass index variables both at ages 15 and 23 were converted to z-scores within each sex, and then we combined all the samples to obtain a larger overall sample size in regression models instead of sex-specific analyses. FMI and VAT mass indices z-scores at age 15 years were included as covariates to test whether there were associations between study variables, regardless of adiposity levels at age 15 years. To ensure that the wear time of the activity monitor did not bias our study results, we further conducted analyses using different indicators of MVPA (e.g., proportion of MVPA time in total wear time). A p-value < 0.05 was considered significant and SPSS version 25 (IBM Corp. in Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) were used for statistical analyses.
Fig. 1.
Moderate-to-vigorous intensity physical activity (MVPA) trajectory groups (Both sexes combined). Dots indicate actual mean MVPA minutes, solid lines indicate estimated MVPA minutes, and dotted lines indicate 95% confidence intervals of estimated MVPA minutes. Group 1, ‘moderately-active with decreasing MVPA’; Group 2, ‘consistently-active with high MVPA’
Results
Table 1 shows mean MVPA (min/day) in adolescence through young adulthood (waves 5–9). Levels of MVPA in males were greater than those of females throughout all waves within the same trajectory group (1 or 2). Participant characteristics including body size, body composition, and adiposity variables are presented in Table 2. Means FMI of females and males were 10.1 kg/m2 and 8.4 kg/m2, respectively. Based on the FMI cutoff values for defining ‘overfat’ status (i.e., 11.8 kg/m2 for women and 8.3 kg/m2 for men, respectively) (Kyle et al., 2003), 31% of females and 40% of males were obese, respectively. In comparison, based on the body mass index cutoff value for defining body fatness (body mass index ≥ 30.0 kg/m2), 24.8% of females and 35.9% of males were obese, respectively. Males also had higher VAT mass indices than females (mean 127.3 g/m2 vs. 112.1 g/m2).
Table 1.
Descriptions of age and MVPA levels by sex and MVPA trajectory groups
| Age (years) | Group 1 |
Group 2 |
|||
|---|---|---|---|---|---|
| MVPA (min/day) | n | MVPA (min/day) | n | ||
|
| |||||
| Female | |||||
| Wave 5 | 15.0 (0.3) | 60.4 (26.1) | 123 | 99.4 (24.9) | 10 |
| Wave 6 | 17.2 (0.5) | 56.2 (21.0) | 129 | 84.9 (24.2) | 11 |
| Wave 7 | 19.5 (0.5) | 52.9 (21.6) | 130 | 116.8 (48.3) | 15 |
| Wave 8 | 21.4 (0.5) | 51.0 (21.5) | 133 | 98.5 (31.8) | 14 |
| Wave 9 | 23.1 (0.3) | 43.8 (22.1) | 138 | 88.5 (38.0) | 16 |
|
Male
Wave 5 |
15.0 (0.3) | 69.5 (27.4) | 69 | 104.2 (34.9) | 38 |
| Wave 6 | 17.2 (0.4) | 73.4 (26.3) | 65 | 101.5 (32.9) | 37 |
| Wave 7 | 19.5 (0.6) | 65.9 (25.8) | 58 | 100.6 (39.3) | 36 |
| Wave 8 | 21.4 (0.5) | 59.2 (19.2) | 72 | 102.5 (45.3) | 40 |
| Wave 9 | 23.2 (0.4) | 55.4 (23.9) | 66 | 96.4 (34.9) | 34 |
Data are mean (standard deviation). MVPA, Moderate-to-vigorous intensity physical activity; Group 1, moderately-active with decreasing MVPA; Group 2, consistently-active with high MVPA
Table 2.
Body size, composition, and regional adiposities at age 23
| Females (n = 129) | Males (n = 92) | Mean difference (95% CI) | |
|---|---|---|---|
|
| |||
| Age (years) | 23.4 (0.5) | 23.4 (0.6) | 0.0 (− 0.1, 0.2) |
| Height (cm) | 166.3 (6.6) | 179.8 (7.8) | − 13.5 (− 15.5, − 11.6) |
| Weight (kg) | 73.1 (19.2) | 92.4 (22.9) | − 19.3 (− 24.9, − 13.7) |
| BMI (kg/m2) | 26.4 (6.4) | 28.5 (6.4) | − 2.1 (− 3.8, − 0.4) |
| Total fat mass (kg) | 28.1 (12.5) | 27.2 (14.0) | 0.8 (− 27.1, 43.7) |
| Lean body mass (kg) | 46.8 (8.1) | 66.9 (11.7) | − 20.1 (− 22.9, − 17.3) |
| VAT mass (g) | 309.1 (210.4) | 410.5 (190.4) | − 101.4 (− 155.8, − 47.0) |
| FMI (kg/m2) | 10.1 (4.4) | 8.4 (4.1) | 1.7 (0.6, 2.9) |
| VAT mass index (g/m2) | 112.1 (76.0) | 127.3 (59.0) | − 15.2 (− 33.2, 2.7) |
| Total fat mass at age 15 (kg) | 19.6 (8.8) | 17.0 (10.3) | 2.6 (− 0.1, 5.3) |
| VAT mass at age 15 (g) | 179.6 (127.6) | 250.6 (128.4) | − 71.1 (− 108.6, 33.5) |
Data are mean (standard deviation)
CI confidence interval, BMI body mass index, VAT visceral adipose tissue, FMI fat mass index
Two different patterns of MVPA (both sexes combined latent trajectories; total N = 297; 57% Female) are presented in Fig. 1. The first corresponds to a group of moderately-active participants with decreasing MVPA (63.7, 61.8, 57.3, 54.4, 47.9 min/day, respectively; mean = 57.0 min/day) and the second was a group of consistently-active participants with high MVPA (102.1, 96.5, 103.4, 98.8, 91.6 min/day, respectively; mean = 98.5 min/day). MVPA trajectories by sex and latent group indicate actual means of MVPA (min/day) by dots, estimated MVPA by solid lines, and 95% confidence intervals of estimated MVPA by dotted lines. As presented in the Supplementary Figure, MVPA trajectories by sex showed that mean MVPA min/day from wave 5 to 9 (age 15–23 years) consistently declined over time in both females (62.9, 58.6, 56.1, 56.3, 46.4 min/day, respectively) and males (81.2, 83.7, 78.8, 73.2, 69.5 min/day, respectively).
A multivariable linear regression model (both sexes combined) showed that the trajectory membership was negatively associated with FMI z-score, independent of FMI z-score at age 15 years and HEI score at age 23 years (Table 3). The regression model revealed that group 2 had a 0.36 lower FMI z-score (standard deviation) compared to group 1 (p = 0.007, model R2 = 0.51), assuming all other variables are held constant. However, VAT mass index z-score was not predicted by the trajectory group membership (p = 0.841).
Table 3.
Associations of MVPA trajectory from ages 15 to 23 years with FMI and VAT mass index z-scores at age 23 years
| FMI z-score | β | SE | p | R2 |
|---|---|---|---|---|
|
| ||||
| (Intercept) | 0.72 | 0.31 | 0.022 | 0.51 |
| FMI z-score at age 15 | 0.72 | 0.05 | < 0.001 | |
| HEI | 0.00 | 0.00 | 0.314 | |
| MVPA_Group | − 0.36 | 0.13 | 0.007 | |
|
| ||||
| VAT mass index z-score | ||||
|
| ||||
| (Intercept) | 0.65 | 0.30 | 0.034 | 0.55 |
| VAT mass index z-score at age 15 | 0.76 | 0.05 | < 0.001 | |
| HEI | − 0.01 | 0.00 | 0.017 | |
| MVPA_Group | − 0.03 | 0.13 | 0.841 | |
HEI, Healthy Eating Index (at age 23 years); MVPA, Moderate-to-vigorous intensity physical activity; MVPA_Group, MVPA trajectory latent group (1 = reference ‘moderately-active with decreasing MVPA’ or 2 = ‘consistently-active with high MVPA’); FMI, Fat mass index; VAT, visceral adipose tissue; β, regression coefficient; SE, Standard error
Discussion
Using objectively-measured physical activity data obtained at five assessments over 9 years, the current study identified a significant negative association between MVPA and FMI levels. Specifically, accelerometer-estimated MVPA trajectories from adolescence to young adulthood were related to FMI levels in young adulthood. Group-based trajectory models may provide additional insight by showing patterns and quantifying the cumulative effect of variables in comparison to other traditional longitudinal analytic approaches which generally examine physical activity behaviors by two-time points (i.e., baseline and follow-up). Thus, the group-based trajectory approach enables researchers to examine the heterogeneity of the study population by dividing them into distinct subgroups (Nagin & Odgers, 2010). Therefore, this study using trajectory models expands the current knowledge of the developmental associations between MVPA and adiposity in young adulthood by using a rich, longitudinal data source that provides unique insight between patterns of lifestyle behaviors and health outcomes over an extended period of time.
The primary finding of this study was that individuals who were consistently-active and maintained high MVPA levels (group 2) during adolescence and young adulthood had significantly lower FMI z-score at 23 years of age, independent of FMI at age 15 years, when compared to individuals who were moderately-active and had decreased MVPA levels (group 1). On average, the observed difference in FMI z-score (0.36) between the two trajectory groups was equal to a 1.6 kg/m2 difference in FMI raw value for both sexes. This indicates that 41.5 min/day more MVPA throughout adolescence and early young adulthood is associated with a 1.6 kg/m2 less FMI at young adulthood. Although there is no strong evidence about reference values associated with a clinically-meaningful change in FMI and their health implications, the 1.6 kg/m2 difference in FMI from the protective daily minutes (i.e., 41.5 min/day of MVPA) could be significant as a preventive advantage. Toomey et al. (2017) suggested that a 1 kg/m2 FMI difference could result in negative obesity consequences and increased risk for chronic disease in adults. For a reference, we found that a 1.6 kg/m2 difference in FMI corresponds to a 19% and 16% variation from the mean FMI for male (8.4 kg/m2) and female participants (10.1 kg/m2), respectively.
To our knowledge, this study is the first to investigate the effect of MVPA patterns (i.e., longitudinal changes) in adolescence through young adulthood on FMI in young adulthood. Although the negative associations of MVPA with adiposity indicators and cardiometabolic health outcomes (e.g., waist circumference, body mass index, systolic blood pressure, triglycerides) have been well-demonstrated in many studies of children through adolescents (Carson et al., 2014; Ekelund et al., 2012; Evenson et al., 2008; Marques et al., 2016; Mitchell et al., 2013) and also one in adults (Maher et al., 2013) from large cohort data sets, the studies are limited by cross-sectional designs or short follow-up periods (1–2 years). Utilizing the multiple measures of MVPA and understanding the relationships between longitudinally measured MVPA and adiposity outcomes in health research have recently become available. For example, Janz et al. (2017) examined the relationship between accelerometer-estimated MVPA and adiposity from early childhood to late adolescence (aged 5–19 years) among participants in the IBDS using multilevel growth models. However, Janz et al. (2017) could not identify a trend in the developmental pattern of MVPA over time. Moreover, the longitudinal associations between physical activity patterns in youth and adiposity outcomes in young adulthood were not examined. One of the few studies using the same general analytical approach as the present study (i.e., trajectory analyses) was published by Kwon et al. (2015) where they investigated the longitudinal associations between MVPA trajectories and percent body fat developments throughout childhood to adolescence (aged from 5 to 19 years), also using data from the IBDS cohort. They concluded that individuals who were active but had decreased MVPA with age, compared to individuals who were consistently active, throughout childhood and adolescence, were more likely to become obese. Kwon et al. (2015) suggested that adiposity development at age 13 or younger may be crucial to determining obesity (assessed by a dichotomous variable of percent body fat) in late adolescence and early young adulthood. However, it is unclear as to what extent the developmental patterns of MVPA in adolescents through the early 20 s would be associated with FMI development in college-age young adults. Our findings complement those of Kwon et al. (2015), but differed in that our study demonstrated that the amount of MVPA in adolescence (independent of FMI at age 15 years) was associated with FMI in early young adulthood, which is known as emerging adulthood (Nelson et al., 2008). Our findings elucidate the importance of MVPA patterns during adolescence up until young adulthood on adiposity accumulations in young adulthood and support current public health efforts to optimize health outcomes in early young adulthood.
Unexpectedly, we did not find a significant association between MVPA trajectory and VAT mass index (p = 0.841). Consistent with this finding, Janz et al. (2017) reported that there was no significant association between lower levels of MVPA and higher levels of VAT in the IBDS cohort (aged 5–19 years). Similar to the assumption from Janz et al. (2017), we also assume the lower levels and less variability in MVPA and/or VAT in females could result in this nonsignificant finding. Females represented a small proportion of those included in the consistently-active with high MVPA trajectory group (7.8% of the sample) and females had significantly lower levels of VAT mass than males. This may explain the null finding in the association between our MVPA trajectory models and VAT at 23 years. VAT is a stronger pathogenic risk factor than total body adiposity, which has been more strongly associated with chronic diseases independent of obesity status (Rosito et al., 2008), and accelerometry-measured MVPA has been negatively-associated with VAT in middle-aged adults (Murabito et al., 2015) and youth (Janz et al., 2017). To our knowledge, little is known about whether MVPA patterns in youth predict VAT deposition in young adulthood. Further investigation is warranted to examine the associations between developmental MVPA patterns and VAT during youth and young adulthood in a larger population where associations can be examined separately for males and females.
One noteworthy finding was that our study participants were active, compared to the similar age group of the general population [approximately two-thirds of youth do not meet the physical activity guidelines (Katzmarzyk et al., 2016; Troiano et al., 2008)]. The mean MVPA of the IBDS participants was 64.8 min/day (group 2 and group 1 had 99.3 min/day and 56.3 min/day, respectively), which is greater than the recommended federal MVPA guidelines of 60 min/day (for youth) and corresponds to at least 150–300 min/week of moderate intensity physical activity, or 75–150 min/week of vigorous intensity physical activity, or an equivalent combination of moderate- and vigorous-intensity physical activity (for adults) (Powell et al., 2019). The average percentage of study participants at waves 5–7 (ages between 15 and 19 years) who met the federal MVPA guidelines of 60 min/day for youth was approximately 57% (data not shown). An important observation from our study results is that the association between a sustained-active lifestyle and lower levels of adiposity in early young adulthood was found in a relatively-active population. Our findings based on accelerometry-measured physical activity can support future federal physical activity guidelines (evidence is mostly obtained by self-report physical activity data) to develop MVPA recommendations for young adulthood for healthy body composition. However, it is important to note that the application of the updated 2-regression equation from Crouter et al. (2010) to analyze physical activity data could have resulted in higher estimates of MVPA than other cutoff values. Using the data from NHANES, Troiano et al. (2008) reported an average accelerometer-estimated MVPA in U.S. children through adults. MVPA levels in the NHANES data in a similar age range with our participants were noticeably lower than MVPA levels of our participants. However, Troiano et al. (2008) applied higher activity intensity cutoff values for youth (ages 6–17 years): 4 metabolic equivalent task (METs) for moderate intensity and 7 METs for vigorous intensity compared to the usual adult values of 3 and 6 METs, respectively. Thus, this may result in lower MVPA values. Furthermore, Crouter et al. (2013) compared the validity of assessing free-living physical activity using the Crouter algorithm (2010) with the NHANES accelerometry data estimated by the Troiano cut-points (Troiano et al., 2008) with indirect calorimetry in young adults (mean age = 25 years). Crouter et al. (2013) reported that NHANES cutpoints underestimated MVPA by 50.4–56.7%, whereas the Crouter algorithm overestimated light, moderate, and vigorous intensity physical activities by 9.0–44.5%. Again, the previously-used single regression equations are limited, given these methods underestimate the energy cost of moderate-intensity activities (Crouter et al., 2010); and, therefore, the 2-regression equation using a shorter interval epoch (10-s) is arguably a better estimate of MVPA, especially in healthy young populations (Welk, 2002). This observation emphasized the need for more longitudinal studies examining accelerometer-estimated MVPA using the updated 2-regression Crouter algorithm (Crouter et al., 2010) and adiposity development in young adults in a large population.
Sex-specific MVPA trajectories (supplementary figure) showed consistent declines throughout adolescence and early young adulthood in both males and females. In agreement with findings in previous studies (Dumith et al., 2011; Farooq et al., 2018; Kwon et al., 2015; Nader et al., 2008; Nelson et al., 2008; Troiano et al., 2008), we found age-related reductions of MVPA in both girls and boys, and boys were more active than girls throughout adolescence and young adulthood. In addition, our results support the evidence with objectively-measured physical activity data that the decline of MVPA continued through young adulthood. To date, noticeable reductions of physical activity and their patterns in children and adolescents have been reported by objective measurements (Kwon et al., 2015; Pate et al., 2019); however, the decline in young adults mostly has been demonstrated by self-reported measurement from survey design studies (Caspersen et al., 2000; Gordon-Larsen et al., 2004). Our results also indicate that MVPA trajectories declined more sharply in females than males throughout the collected ages. In agreement with this finding, the literature has shown that females exhibited steeper declines in MVPA than males during adolescence (Craggs et al., 2011). Since there might be many factors causing the difference between males and females, sex per se may not be the factor that accounts for the disparity in physical activity patterns between girls and boys (Craggs et al., 2011). Various alternate factors, such as individual, social, and environmental factors for female vs. male adolescents might presumably explain the declining pattern of physical activity (Zook et al., 2014). For example, Kwon et al. (2017) suggested that physical activity growth patterns in childhood are more persistent in females than males, and there was a greater sport participation rate in males within the same age range in youth. Additional investigations to better understand the determinants of physical activity patterns in females from youth to young adulthood are warranted. However, importantly, we confirmed that there was a subset of female participants in the study who maintained high levels of MVPA (7.8% of the total females).
This study has strengths in terms of the application of analyses of the behavioral process using the group-based trajectory modeling from objectively-measured physical activity data and criterion-referenced measurement of adiposity. However, several limitations should also be acknowledged in this study. First, our findings may not be generalizable to other populations, as study participants were active and largely homogenous Caucasian Midwestern residents of relatively high socioeconomic status. Therefore, generalization to other racial/ethnic groups, different regions, and diverse socioeconomic status needs to be done with caution. Second, group 2 had a very small sample size of females. Future studies should utilize larger and more diverse samples to investigate whether the findings from our study are applicable to other populations. However, we believe that this small portion of females in group 2 would reflect the true distribution of physical activity behaviors in real life (i.e., only a small portion of females would be active) (Zook et al., 2014). Lastly, we are aware that not all participants in each group perfectly followed their assigned group trajectory because group membership was determined based on estimated probabilities from maximum likelihood estimation. The average posterior probabilities of our study participants for our trajectory groups 1 and 2 were 96.8% and 87.1%, respectively. In addition, the sample size variation over time might affect our findings. However, the majority of participants who participated in the latest wave (9; year 23) have consistently participated in previous waves. Therefore, we assume that the small variation in sample size in each wave minimally affected our main finding. We used the posterior probability-based classification which does not explain the uncertainty in group allocation (Roeder et al., 1999); however, it provides a straightforward basis for producing profiles of trajectory group members and an easy and transparent communication of the findings (Nagin & Odgers, 2010).
Conclusions
Accelerometer-estimated physical activity data were analyzed to predict adiposity by latent group-based trajectory models in a sample of U.S. youth as they transitioned from adolescence to early young adulthood. The mean difference in daily MVPA (from adolescence to young adulthood) between the trajectory groups 1 and 2 was 41.5 min/day, and this difference in MVPA was associated with a 1.6 kg/m2 difference in FMI in young adults. Therefore, we conclude that individuals who are consistently-active with maintaining their high MVPA level during adolescence through early young adulthood are less likely to accumulate total body fat in young adulthood, as assessed by FMI. This study suggests that a sustained-active lifestyle throughout adolescence and young adulthood will support a healthy transition in body composition during this period in life.
Supplementary Material
Acknowledgements
We thank the study participants and staff of The Iowa Bone Development Study. We thank the study participants and staff of The Iowa Bone Development Study. This work was supported by the National Institutes of Health (R01-DE12101, R01-DE09551, M01-RR00059, UL1-RR024979, UL1-TR000442, and U54-TR001013), and research funds by the Roy J. Carver Charitable Trust and Delta Dental of Iowa Foundation.
Footnotes
Compliance with ethical standards
Conflict of interest Minsuk Oh, Dong Zhang, Kara M. Whitaker, Elena M. Letuchy, Kathleen F. Janz, and Steven M. Levy declare that they have no conflict of interest.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights and Informed Consent All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10865-020-00190-x) contains supplementary material, which is available to authorized users.
References
- Block G, Woods M, Potosky A, & Clifford C (1990). Validation of a self-administered diet history questionnaire using multiple diet records. Journal of Clinical Epidemiology, 43, 1327–1335. [DOI] [PubMed] [Google Scholar]
- Brage S, Wedderkopp N, Franks PW, Andersen LB, & Froberg K (2003). Reexamination of validity and reliability of the CSA monitor in walking and running. Medicine and Science in Sports and Exercise, 35, 1447–1454. [DOI] [PubMed] [Google Scholar]
- Carson V, Rinaldi R, Torrance B, Maximova K, Ball G, Majumdar S, & Wozny P (2014). Vigorous physical activity and longitudinal associations with cardiometabolic risk factors in youth. International Journal of Obesity, 38, 16–21. [DOI] [PubMed] [Google Scholar]
- Caspersen CJ, Pereira MA, & Curran KM (2000). Changes in physical activity patterns in the United States, by sex and cross-sectional age. Medicine and Science in Sports and Exercise, 32, 1601–1609. [DOI] [PubMed] [Google Scholar]
- Corder K, Sharp SJ, Atkin AJ, Andersen LB, Cardon G, Page A, & Janz KF (2016). Age-related patterns of vigorous-intensity physical activity in youth: The International Children’s Accelerometry Database. Preventive Medicine Reports, 4, 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craggs C, Corder K, Van Sluijs EM, & Griffin SJ (2011). Determinants of change in physical activity in children and adolescents: A systematic review. American Journal of Preventive Medicine, 40, 645–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouter SE, DellaValle DM, Haas JD, Frongillo EA, & Bassett DR (2013). Validity of ActiGraph 2-regression model, Matthews cut-points, and NHANES cut-points for assessing free-living physical activity. Journal of Physical Activity and Health, 10, 504–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouter SE, Kuffel E, Haas JD, Frongillo EA, & Bassett DR Jr. (2010). A refined 2-regression model for the actigraph accelerometer. Medicine and Science in Sports and Exercise, 42, 1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen KW, Watson K, & Zakeri I (2008). Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. Journal of the American Dietetic Association, 108, 862–866. [DOI] [PubMed] [Google Scholar]
- Dumith SC, Gigante DP, Domingues MR, & Kohl HW III. (2011). Physical activity change during adolescence: A systematic review and a pooled analysis. International Journal of Epidemiology, 40, 685–698. [DOI] [PubMed] [Google Scholar]
- Ekelund U, Luan J, & Sherar LB, Esliger DW, Griew P, Cooper A, & Collaborators, I. C. s. A. D. . (2012). Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA, 307, 704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis KJ, Abrams SA, & Wong WW (1999). Monitoring childhood obesity: Assessment of the weight/height2 index. American Journal of Epidemiology, 150, 939–946. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, & McMurray RG (2008). Calibration of two objective measures of physical activity for children. Journal of Sports Sciences, 26, 1557–1565. [DOI] [PubMed] [Google Scholar]
- Farooq A, Martin A, Janssen X, Wilson MG, Gibson AM, Hughes A, & Reilly JJ (2020). Longitudinal changes in moderate-to-vigorous-intensity physical activity in children and adolescents: A systematic review and meta-analysis. Obesity Reviews, 21, e12953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq MA, Parkinson KN, Adamson AJ, Pearce MS, Reilly JK, Hughes AR, & Reilly JJ (2018). Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. British Journal of Sports Medicine, 52, 1002–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, & Sirard J (1998). Calibration of the Computer Science and Applications, Inc. accelerometer. Medicine and Science in Sports and Exercise, 30, 777–781. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, & Popkin BM (2004). Longitudinal physical activity and sedentary behavior trends: Adolescence to adulthood. American Journal of Preventive Medicine, 27, 277–283. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, The NS, & Adair LS (2010). Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity, 18, 1801–1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X, Warden B, Paeratakul S, & Bray G (2004). Healthy eating index and obesity. European Journal of Clinical Nutrition, 58, 1580–1586. [DOI] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, & Ogden CL (2017). Prevalence of obesity among adults and youth: United States, 2015–2016. Centers for Disease Control and Prevention (NCHS Data Brief), 288. [PubMed] [Google Scholar]
- Hebden L, Chey T, & Allman-Farinelli M (2012). Lifestyle intervention for preventing weight gain in young adults: A systematic review and meta-analysis of RCTs. Obesity Reviews, 13, 692–710. [DOI] [PubMed] [Google Scholar]
- Hendelman D, Miller K, Baggett C, Debold E, & Freedson P (2000). Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Medicine and Science in Sports and Exercise, 32, S442–S449. [DOI] [PubMed] [Google Scholar]
- Janz KF, Boros P, Letuchy EM, Kwon S, Burns TL, & Levy SM (2017). Physical activity, not sedentary time, predicts dual-energy X-ray absorptiometry-measured adiposity age 5 to 19 years. Medicine and Science in Sports and Exercise, 49, 2071–2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz KF, Burns TL, & Levy SM (2005). Tracking of activity and sedentary behaviors in childhood: The Iowa Bone Development Study. American Journal of Preventive Medicine, 29, 171–178. [DOI] [PubMed] [Google Scholar]
- Jones BL, & Nagin DS (2007). Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods and Research, 35, 542–571. [Google Scholar]
- Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput J-P, Fogelholm M, & Kurpad A (2015). Physical activity, sedentary time, and obesity in an international sample of children. Medicine and Science in Sports and Exercise, 47, 2062–2069. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Denstel KD, Beals K, Bolling C, Wright C, Crouter SE, & Staiano AE (2016). Results from the United States of America’s 2016 report card on physical activity for children and youth. Journal of Physical Activity and Health, 13, S307–S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly TL, Wilson KE, & Heymsfield SB (2009). Dual energy X-ray absorptiometry body composition reference values from NHANES. PLoS ONE, 4, e7038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon S, Burns TL, Levy SM, & Janz KF (2013). Which contributes more to childhood adiposity-high levels of sedentarism or low levels of moderate-through-vigorous physical activity? The Iowa Bone Development Study. The Journal of Pediatrics, 162, 1169–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon S, Janz KF, Letuchy EM, Burns TL, & Levy SM (2015). Active lifestyle in childhood and adolescence prevents obesity development in young adulthood. Obesity, 23, 2462–2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon S, Janz KF, Letuchy EM, Burns TL, & Levy SM (2017). Association between body mass index percentile trajectories in infancy and adiposity in childhood and early adulthood. Obesity, 25, 166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyle UG, Schutz Y, Dupertuis YM, & Pichard C (2003). Body composition interpretation: Contributions of the fat-free mass index and the body fat mass index. Nutrition, 19, 597–604. [DOI] [PubMed] [Google Scholar]
- Lavie CJ, Milani RV, Ventura HO, & Romero-Corral A (2010). Body composition and heart failure prevalence and prognosis: Getting to the fat of the matter in the “obesity paradox”. Paper presented at the mayo clinic proceedings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leenders N, Nelson T, & Sherman W (2003). Ability of different physical activity monitors to detect movement during treadmill walking. International Journal of Sports Medicine, 24, 43–50. [DOI] [PubMed] [Google Scholar]
- Li K, Haynie D, Lipsky L, Iannotti RJ, Pratt C, & Simons-Morton B (2016). Changes in moderate-to-vigorous physical activity among older adolescents. Pediatrics, 138, e20161372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P, Ma F, Lou H, & Liu Y (2013). The utility of fat mass index vs. body mass index and percentage of body fat in the screening of metabolic syndrome. BMC Public Health, 13, 629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher CA, Mire E, Harrington DM, Staiano AE, & Katzmarzyk PT (2013). The independent and combined associations of physical activity and sedentary behavior with obesity in adults: NHANES 2003–06. Obesity, 21, E730–E737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques A, Minderico C, Martins S, Palmeira A, Ekelund U, & Sardinha LB (2016). Cross-sectional and prospective associations between moderate to vigorous physical activity and sedentary time with adiposity in children. International Journal of Obesity, 40, 28–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J, Pate R, España-Romero V, O’Neill J, Dowda M, & Nader P (2013). Moderate-to-vigorous physical activity is associated with decreases in body mass index from ages 9 to 15 years. Obesity, 21, E280–E286. [DOI] [PubMed] [Google Scholar]
- Murabito JM, Pedley A, Massaro JM, Vasan RS, Esliger D, Blease SJ, & Fox CS (2015). Moderate-to-vigorous physical activity with accelerometry is associated with visceral adipose tissue in adults. Journal of the American Heart Association, 4, e001379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader PR, Bradley RH, Houts RM, McRitchie SL, & O’Brien M (2008). Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA, 300, 295–305. [DOI] [PubMed] [Google Scholar]
- Nagin DS (2005). Group-based modeling of development. London: Harvard University Press. [Google Scholar]
- Nagin DS, & Odgers CL (2010). Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology, 6, 109–138. [DOI] [PubMed] [Google Scholar]
- Nanney MS, Lytle LA, Farbakhsh K, Moe SG, Linde JA, Gardner JK, & Laska MN (2015). Weight and weight-related behaviors among 2-year college students. Journal of American College Health, 63, 221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson MC, Story M, Larson NI, Neumark-Sztainer D, & Lytle LA (2008). Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity, 16, 2205–2211. [DOI] [PubMed] [Google Scholar]
- Niyonkuru C, Wagner AK, Ozawa H, Amin K, Goyal A, & Fabio A (2013). Group-based trajectory analysis applications for prognostic biomarker model development in severe TBI: A practical example. Journal of Neurotrauma, 30, 938–945. [DOI] [PubMed] [Google Scholar]
- Pate RR, Schenkelberg MA, Dowda M, & McIver KL (2019). Group-based physical activity trajectories in children transitioning from elementary to high school. BMC Public Health, 19, 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell KE, King AC, Buchner DM, Campbell WW, DiPietro L, Erickson KI, & Katzmarzyk PT (2019). The scientific foundation for the Physical Activity Guidelines for Americans. Journal of Physical Activity and Health, 16, 1–11. [DOI] [PubMed] [Google Scholar]
- Roeder K, Lynch KG, & Nagin DS (1999). Modeling uncertainty in latent class membership: A case study in criminology. Journal of the American Statistical Association, 94, 766–776. [Google Scholar]
- Rosito G, Massaro J, & Hoffmann U (2008). Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: The Framingham heart study. Circulation, 117, 605. [DOI] [PubMed] [Google Scholar]
- Schooling CM, Thomas GN, Leung GM, Ho SY, Janus ED, & Lam TH (2007). Is height associated with cardiovascular risk in Chinese adults? Epidemiology, 18, 274–278. [DOI] [PubMed] [Google Scholar]
- Smith SR, Lovejoy JC, Greenway F, Ryan D, deJonge L, de la Bretonne J, & Bray GA (2001). Contributions of total body fat, abdominal subcutaneous adipose tissue compartments, and visceral adipose tissue to the metabolic complications of obesity. Metabolism-Clinical and Experimental, 50, 425–435. [DOI] [PubMed] [Google Scholar]
- Togo P, Osler M, Sørensen TI, & Heitmann B (2001). Food intake patterns and body mass index in observational studies. International Journal of Obesity, 25, 1741–1751. [DOI] [PubMed] [Google Scholar]
- Toomey CM, Whittaker JL, Nettel-Aguirre A, Reimer RA, Woodhouse LJ, Ghali B, & Emery CA (2017). Higher fat mass is associated with a history of knee injury in youth sport. Journal of Orthopaedic and Sports Physical Therapy, 47, 80–87. [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise, 40, 181. [DOI] [PubMed] [Google Scholar]
- VanItallie T, Yang M-U, Heymsfield SB, Funk RC, & Boileau RA (1990). Height-normalized indices of the body’s fat-free mass and fat mass: Potentially useful indicators of nutritional status. The American Journal of Clinical Nutrition, 52, 953–959. [DOI] [PubMed] [Google Scholar]
- Welk G (2002). Physical activity assessments for health-related research. New York: Human Kinetics. [Google Scholar]
- Yang X, Telama R, Viikari J, & Raitakari OT (2006). Risk of obesity in relation to physical activity tracking from youth to adulthood. Medicine and Science in Sports and Exercise, 38, 919. [DOI] [PubMed] [Google Scholar]
- Zook KR, Saksvig BI, Wu TT, & Young DR (2014). Physical activity trajectories and multilevel factors among adolescent girls. Journal of Adolescent Health, 54, 74–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.