Abstract
Antibodies play a crucial role in the immune response, in fighting off pathogens as well as helping create strong immunological memory. Antibody-dependent enhancement (ADE) occurs when non-neutralising antibodies recognise and bind to a pathogen, but are unable to prevent infection, and is widely known and is reported as occurring in infection caused by several viruses. This narrative review explores the ADE phenomenon, its occurrence in viral infections and evaluates its role in infection by SARS-CoV-2 virus, which causes coronavirus disease 2019 (COVID-19). As of yet, there is no clear evidence of ADE in SARS-CoV-2, though this area is still subject to further study.
Keywords: coronavirus, SARS-CoV-2, antibody-dependent enhancement, COVID-19
1. Overview of SARS-CoV-2 Virus
1.1. The SARS-CoV-2 Virus Structure and Function
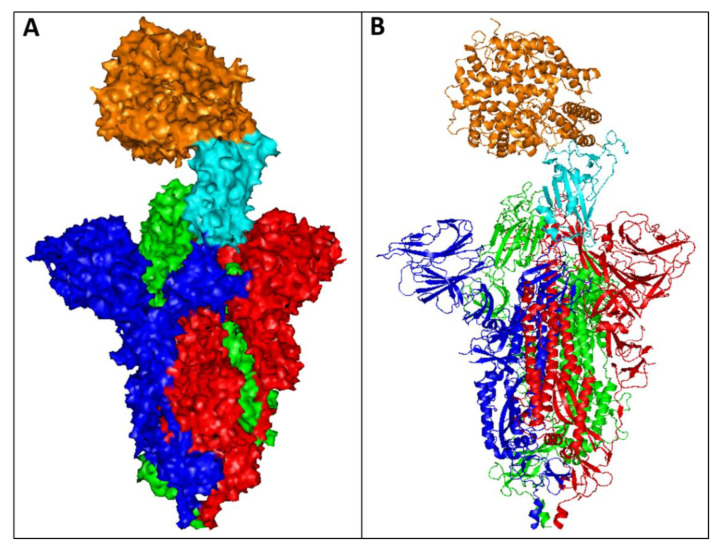
The causative agent of the COVID-19 pandemic is a previously unidentified virus strain, denoted as SARS-CoV-2 [1]. COVID-19 is generally associated with different symptoms including: fever, persistent dry cough, shortness of breath, and loss of taste and/or smell, and in many cases this disease has been fatal [2]. Consequently, the development of novel therapies has been a global priority for researchers. SARS-CoV-2 is composed of different structural proteins: the spike (S), membrane (M), envelope (E), and nucleocapsid (N) proteins [3]. SARS-CoV-2 infects human cells through binding of the virus receptor binding domain (RBD), located at the tip of the S protein (Figure 1), to the angiotensin-converting enzyme 2 (ACE2) receptor on human cell surfaces to facilitate the entry process and infection. Therefore, most anti-SARS-CoV-2 therapies have focussed on targeting the S protein, with the aim of inhibiting its binding to the ACE2 receptor.
Figure 1.
The crystal structure of SARS-CoV-2 S protein complexed with ACE2 receptor retrieved from the Protein Data Bank (PDB), PDB entry 7DF4. The structure was visualised by PyMOL (The PyMOL Molecular Graphics System, Version 1.7.4 Schrödinger, LLC.). The complex is displayed as (A) surface and (B) loops. The S protein assembles into trimers (coloured red, blue, and green) on the virion surface to form a distinctive “corona”. The RBD domain of the S protein (cyan) binds to the human ACE2 receptor (orange) to promote attachment and fusion.
Upon entry, two open reading frames (ORFs) 1a and 1b translate to two polypeptides, known as ORF 1a and 1b. This further encodes two proteases; the main protease (Mpro), that is also identified as chymotrypsin-like cysteine protease (3CLpro), and papain-like protease (PLpro) [4]. The polypeptides 1a and 1ab invade host-cellular ribosomes to facilitate their translation, where they are processed by Mpro and PLpro, encoding several non-structural proteins (nsPs). The nsPs help the structural proteins (S, M, N, and E) enter the endoplasmic reticulum/golgi apparatus, and are involved in viral assembly and packaging [5]. The viral genome binds to the N protein, resulting in the formation of a ribonucleoprotein complex that facilitates viral replication [6]. NsP12 is an RNA-dependent RNA polymerase (RdRp), which plays a critical role in the assembly of the entire RNA polymerase replicative machinery, and is a key enzyme mediating the synthesis of all viral RNA molecules [7], making it a potential therapeutic target. In addition, guanine N7-methyltransferase (N7-MTase), found at the C-terminal of SARS-CoV-2 nsP14, is crucial for exonuclease activity [8]. Inhibition of this target could interfere with enzyme catalysis and prevent capping of the 5′-ends of viral genomic RNA and sub-genomic RNA, that is crucial in SARS-CoV-2 evasion of the host immune response [9]. Failure of RNA capping leads to viral RNA degradation, and interference with the replication cycle [10].
Other potential therapeutic targets include Mpro and PLpro, since their inhibition can stop the production of nsPs, which are critical to viral transcription and replication. Grotessi et al. [11] studied the conformational arrangements of Mpro, and found that the protein is composed of three parts: domain 1 (residues 8–101), domain 2 (residues 102–184), and domain 3 (residues 201–303). The protease catalytic site is formed by a Cys-His dyad found in a pocket between domains 1 and 2. A molecular dynamics (MD) simulation study has predicted the interaction as an induced fit model [11]. Therefore, blocking the functional unit that cleaves the polyprotein could represent a compelling target for the development of new therapeutics. One possible method for blocking these targets, especially the S protein, could be achieved by antibodies.
1.2. Immune Responses to Viruses: The SARS-CoV-2 Case
The innate immune response (IIR) is the first line of defence against viral infection, and it is rapidly induced, but is of low specificity. Some evidence suggests the importance of IIR in early life when adaptive functions are not completely developed [12]. The innate immune cells express pathogen-recognition receptors (PRRs), such as C-type lectin receptors, NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), and Toll-like receptors (TLRs) [13]. These receptors sense pathogen-associated molecular patterns (PAMPs) that include different viral structures like nucleic acid. RNA from coronavirus and other respiratory viruses are recognised by cytosolic and endosomal RNA receptors like RIG-I or TLR 3 and 7 [14]. Overall, the innate immune system senses foreign viral material and triggers downstream signalling, which induces transcription factors in the nucleus (NF-KB) that stimulate the expression of cytokines and interferons (IFNs) to fight against an infection [15].
IFNs play a major role in antiviral activities and are divided into three families (type I, type II and type III) based on their homology and biological activities [16]. Type I IFNs (e.g IFNα, INFβ, etc) are one of the first cytokines produced during viral infections, and their functions include inhibition of cellular translational function to prevent virion release, prevention of virus entry, and inhibition of virus transcription [17]. Type II IFNs are structurally unrelated to the other two classes of IFN genes and are produced by NK cells during antiviral IIR. IFN-γ improves the antiviral effect of NK cells and macrophages, but also has a great impact on the maturation and activation of antigen presenting cells (APCs). This effect drives stimulation of the adaptive antiviral response to clear the infection and generate memory to further fuel responses against the pathogen [17].
Type III IFNs also have an important role in tissue-specific IFN responses, and recent studies have shown that type III IFNs are better than the other two types of IFN. Type III IFNs are lower in magnitude, less inflammatory, and concentrated in regions of anatomic barrier signalling [18]. The antiviral effects of type III IFNs are especially evident at epithelial barriers, such as the gastrointestinal, respiratory, and reproductive tracts [19]. Type I and III IFNs are also considered to be crucial in antiviral responses, and SARS-CoV-2 has been shown to be sensitive to pre-treatment with IFN-I and III in in vitro assays [20,21]. The suppression of IFN responses in the early stages of COVID-19, reduces the host’s capacity to eliminate the virus and its spread [22]. However, IFN responses may also cause immunopathies, mainly if the immune response is not activated at the right time or intensity [23]. Overall, the early stages of type I IFN deficiency and the late stage of IFN persistence, could be a hallmark of severe COVID-19 infection [19,20,21,22,23,24]. In contrast, type III IFN responses are restrictively mucosa-specific, and the antiviral defences are weaker than those induced by pro-inflammatory responses. So far, many studies have investigated the immunomodulatory and antiviral roles of both type I and type III IFNs in SARS-CoV-2 infection, and it is imperative for IFN-based prophylactic development [24].
The adaptive immune response (AIR) is considered the main mechanism to limit viral replication and spread. AIR is led by the induction of proinflammatory cytokines and the activation of CD4+/CD8+ T cells, and B cells [25,26]. Chen et al. (2010) demonstrated that CD4+ T cells were very important for controlling SARS-CoV replication in disease T cell knock out mice. Recently, T cell studies demonstrated that CD8+ and CD4+ memory T cells are induced in SARS-CoV 2 convalescent patients and may have a major role in host protection [27]. However, in COVID-19, total CD4+ and CD8+ T cells are significantly reduced [28]. The importance of T cell responses is notable in that T cells may be sufficient to clear the virus in the absence of antibodies [29].
The induction of neutralising antibodies is an important effector mechanism to clear infections against viral diseases like influenza, dengue and COVID-19. More than 90% of infected patients with SARS-CoV-2 seroconvert between 5–15 days and the primary antigen for seroconversion is the spike protein (S) from the virus envelope [30]. The receptor binding domain (RBD) of S protein is the target of >90% of neutralising antibodies in COVID-19 cases [31]. Interestingly, SARS-CoV-2 neutralising antibodies have little to no somatic hypermutation (a process in which point mutations accumulate in the antibody variable regions to enhance their ability to bind foreign pathogens) [32,33]. These data indicate that the development of neutralising antibodies against SARS-CoV-2 is triggered by T cell independent mechanisms, as it can be accomplished by many B cells with little or no affinity maturation required. Work by Anderson et al. (2020) [34] and Shrock et al. (2020) [35], suggests that neutralising antibody responses generally develop from naive B cells, and not from pre-existing memory B cells.
The T cell response against COVID-19 has been underestimated, and recent data shows its importance in inducing memory and highly protective response. SARS-CoV-2-specific CD4+ and CD8+ T cells have been correlated with reduced disease severity, while neutralising antibodies in the same individuals did not [36]. It is also known that administration of high doses of SARS-CoV-2 neutralising monoclonal antibodies into SARS-CoV-2-infected patients had relatively limited effects on COVID-19 in clinical trials [37,38]. Altogether, these data highlight the importance of inducing high quality antibodies and memory B cells for appropriate protection against SARS-CoV-2. Probably with the cooperation of CD4+ cells and induction of B cell responses through T cell dependent mechanisms. New vaccine candidates are focused on the use of immune stimulating adjuvants and vaccine formulations, to elicit long lasting and highly neutralising responses against the virus through T cell activation [39].
Coronaviruses infect cells by multiple approaches, mediated by direct/indirect antibody Fc receptors or through targeting of the RBD to the ACE2 receptor. Infection of immune cells like macrophages and mast cells is possible if they express the target receptor. In fact, the exacerbated activation of macrophages and mass induction of cytokines supports the pathogenesis and inflammatory reactions in the severe forms of the disease [40]. Results from Maemura et al. [41] suggest that the Antibody-dependent enhancement (ADE) mechanism requires both Fc receptor engagement and ACE2 activation, although it is not clear that ADE inducing antibodies have a direct role in stimulating the cytokine storm. On the other hand, the quality and quantity of the SARS-CoV viruses infecting macrophages seems to be more related to the hyper-inflammation process. Therefore, to discover the mechanisms underlying SARS-Cov2 cytokine production it is important to develop new drugs to block the pathological process [42]. In addition, many groups are focusing their efforts on developing new vaccines inducing T cell responses, which may be more effective in controlling and reducing the viruses in the host cells than the currently approved COVID vaccines, which mainly induce a neutralising antibody response [43].
1.3. The Role of Antibodies against SARS-CoV-2 Virus
Passive immunisation has been routinely used for over a century to prevent diseases such as rabies, hepatitis B, and tetanus [44]. Another aspect of protection is based on utilising antibodies to block virus infection by a process called neutralisation. Virus neutralisation inhibits the acquisition of a pathogen or limits its pathogenesis. This can be achieved through pre-attachment neutralisation, by antibody binding to micro-organisms, and aggregation of antibodies may allow more efficient entrapment of pathogens in mucous, enhancing their subsequent clearance [45]. Virus neutralisation can also take the shape of interference with the viral attachment through binding to ligands vital for attachment of the pathogen to its host receptor through steric hindrance [46]. Post-attachment neutralisation can be based on inhibition of fusion/entry [47]; or inhibition of other steps in the organism’s lifecycle once it has successfully entered host cells by engineering cells to express intracellular antibodies (intrabodies) [48]. Consequently, virus neutralisation by antibodies could be exploited to protect against the SARS-CoV-2 virus. NHS England, for example, has provided a list of symptomatic, non-hospitalised COVID-19 patients who are showing no sign of clinical recovery and have priority for treatment with mAbs [49].
Several biopharmaceutical companies and academic institutions have co-operated to develop monoclonal antibodies (mAbs) for the treatment of COVID-19 and protection from infection against the SARS-CoV-2 virus. These efforts were based on previous experience in developing mAbs against pathogens such as syncytial virus (Palivizumab) [50], Ebola virus (Ansuvimab-zykl) [51], and Bacillus anthracis (Obiltoxaximab) [52]. Numerous SARS-CoV-2 mAbs have entered clinical trials for the treatment of patients with varying degrees of SARS-CoV-2 infection. There are currently 39 antibodies at different stages of clinical trials (Table 1). On 9 November 2020, the U.S. Food and Drug Administration (FDA) issued an emergency use authorisation for Bamlanivimab for the treatment of mild-to-moderate COVID-19 in adult and paediatric patients [53]. Regeneron REGN-COV2 (Casirivimab and Imdevimab) was also approved by the FDA (on 21st November 2020) in adults with mild-to-moderate COVID-19 who are at high risk for poor outcomes [53]. However, in January 2022, the FDA has limited the use of Bamlanivimab and Etesevimab, due to the Omicron Variant, to only when the patient is likely to have been infected with or exposed to a variant that is susceptible to these two antibodies [1].
Table 1.
List of antibodies currently in clinical development. Data were extracted from National Institutes of Health databank (https://clinicaltrials.gov/; accessed on 20 April 2022), and the Antibody Society (https://www.antibodysociety.org/covid-19-biologics-tracker/; accessed on 10 May 2022).
| Antibody | Company and Country | Clinical Trial Stage and ID | |
|---|---|---|---|
| 1 | REGN-COV2, a cocktail of two mAbs: REGN10987 (Imdevimab) and REGN10933 (Casirivimab) | Regeneron Pharmaceuticals, Westchester County, USA | Emergency Use Authorization granted in the USA; Approved in Japan, UK, EU, and Australia |
| 2 | LY-CoV555 (Bamlanivimab) and LY-CoV016 (Etesevimab) | AbCellera, Vancouver, Canada and Eli Lilly, Indianapolis, USA | Emergency Use Authorization granted in the USA in 2020, but limited the authorisation in 2022. |
| 3 | VIR-7831/ GSK4182136 (Sotrovimab) |
Vir Biotechnology, San Francisco, USA and GSK, Middlesex, UK | Emergency Use Authorization granted in the USA; Approved in Australia, UK, and EU. |
| 4 | CT-P59 (Regdanvimab) | Celltrion Group, Incheon, South Korea | Emergency Use Authorization granted in South Korea and EU. |
| 5 | AZD7442 (AZD8895/Tixagevimab and AZD1061/Cilgavimab) | AstraZeneca, Macclesfield, UK | Emergency Use Authorization granted in the USA |
| 6 | TY027 | Tychan, National University of Singapore | Phase 3 (NCT04429529 and NCT04649515) |
| 7 | BRII-196/ BRII-198 (Amu-barvimab/Romlusevimab) | Brii Bio, Durham, USA/TSB Therapeutics/Tsinghua University, China | Approved in China Phase 3 (NCT04501978, NCT04479631, and NCT04479644) |
| 8 | ADG20 | Adagio Therapeutics, Waltham, USA | Phase 2/3 (NCT04805671 and NCT04859517) |
| 9 | SCTA01 | Sinocelltech, China | Phase 2/3 (NCT04483375 and NCT04644185) |
| 10 | C144-LS and C-135-LS | Bristol-Myers Squibb, New York City, USA | Phase 2/3 (NCT04700163 and Activ-2 study) |
| 11 | ADM03820 | Ology Bioservices, Alachua, USA | Phase 2/3 (NCT05142527) |
| 12 | REGN14256 + imdevimab | Regeneron, Westchester County, USA | Phase ½/3 (NCT05081388) |
| 13 | MAD0004J08 | Toscana Life Sciences Sviluppo s.r.l, Siena, Italy | Phase 2/3 (NCT04932850 and NCT04952805) |
| 14 | MW33 | Mabwell Bioscience Co, Zhangjiang Hi-tech Park, Shanghai | Phase 2 (NCT04533048 and NCT04627584) |
| 15 | Etesevimab (JS016, LY3832479, LY-CoV016) | Junshi Biosciences, China and Eli Lilly, Indianapolis, USA | Phase 2 (NCT04441918, NCT04441931, and NCT04427501) |
| 16 | BGB-DXP593 | BeiGene, Beijing, China | Phase 2 (NCT04551898 and NCT04532294) |
| 17 | COVI-AMG (STI-2020) | Sorrento Therapeutics, San Diego, USA | Phase 2 (NCT04734860) |
| 18 | LY-CoV1404, LY3853113 | AbCellera, Vancouver, Canada and Eli Lilly, Indianapolis, USA | Phase 2 (NCT04634409) |
| 19 | IBIO-123 | Immune Biosolutions, Sherbrooke, Canada | Phase 2 (Not Available) |
| 20 | VIR-7832 | Vir Biotechnology, San Francisco, USA | Phase 1/2 (NCT04746183) |
| 21 | COR-101 | CORAT Therapeutics, Braunschweig, Germany | Phase 1/2 trial (NCT04674566) |
| 22 | DZIF-10c, BI 767551 | University of Cologne, Germany | Phase 1/2 (NCT04631666 and NCT04631705) |
| 23 | XVR011 | Exevir Bio BV, Belgium | Phase 1/2 (NCT04884295) |
| 24 | HLX70 | Hengenix Biotech Inc., Milpitas, USA | Phase 1 (NCT04561076) |
| 25 | DXP-604 | BeiGene, Beijing, China | Phase 1 (NCT04669262) |
| 26 | ZRC-3308 | Zydus Cadila, Ahmedabad, India | Phase 1 (Not Available) |
| 27 | HFB30132A | HiFiBiO Therapeutics, Cambridge, USA | Phase 1 (NCT04590430) |
| 28 | ABBV-47D11 | Abbvie, North Chicago, USA | Phase 1 (NCT04644120) |
| 29 | C144-LS and C-135-LS | Bristol-Myers Squibb, New York City, USA | Phase 1 (NCT04700163) |
| 30 | JMB2002 | Jemincare Group, Shanghai | Phase 1 (ChiCTR2100042150) |
| 31 | IMM-BCP-01 | Immunome, Inc., Exton, USA | Phase 1 (Not Available) |
| 32 | SCTA01 | Sinocelltech, China | Phase 1 (NCT04483375) |
| 33 | MW33 | Mabwell Bioscience Co., Ltd., Shanghai | Phase 1 (NCT04533048) |
| 34 | Anti-SARS-CoV-2 mAb | Stanford University, Stanford, USA | Phase 1 (NCT04567810) |
| 35 | P2C-1F11 | Brii Biosciences, Durham, USA | Phase 1 (NCT04479631 and NCT04479644) |
| 36 | SCTA01 | Sinocelltech, China | Phase 1 (NCT04483375) |
| 37 | LY-CovMab | Luye Pharma Group, Princeton, USA | Phase 1 (NCT04973735) |
| 38 | CT-P63 | Celltrion Group, Incheon, South Korea | Phase 1 (NCT05017168) |
| 39 | IGM-6268 | IGM Biosciences, Mountain View, USA | Phase 1 (NCT05160402 and NCT05184218) |
All these clinical candidates are full length IgG antibodies targeting the SARS-CoV-2 S protein. In addition to these antibodies, various antibody formats are currently in pre-clinical development, including human mAbs [54], human single domain antibodies [55], llama-derived nanobodies [56], shark single-domain Variable New Antigen Receptors (VNARs) [57], humanised nanobodies [58], and human Fab [59], bi-specific or tri-specific antibodies [60], and nucleic acid encoding antibodies [61]. In addition, the route of administration could play an important role to surpass SARS-CoV-2 infection. For instance, Halwe et al. [62] have examined DZIF-10c, a mAb that could be administered intranasally to provide both prophylactic and therapeutic effects against COVID-19. DZIF-10c was able to abolish the infectious particles in SARS-CoV-2 infected mice, and mitigated lung pathology when administered prophylactically. DZIF-10c has completed phase 1 and 2 trial in healthy volunteers and SARS-CoV-2 infected individuals (ClinicalTrials.gov Identifier: NCT04631705).
The current success in developing antibodies against SARS-CoV-2 in a relatively short period was supported through the significant development of several laboratory and computational techniques. The antibody development process relies on techniques such as single B cell sorting, phage display, development of transgenic mice, high throughput sequencing, and modelling and computational analysis [53]. These techniques have the privilege to generate antibodies with exceptionally high affinity and superior neutralising function. Most of the isolated neutralising mAbs are developed using single B cells from individuals infected with COVID-19, as comprehensively detailed in [2]. These mAbs are specific to the RBD of the SARS-CoV-2 S protein, to compete with the ACE2 receptor to bind the RBD and neutralise infection. Moreover, these antibodies can also be engineered to remove or change the sites related to potential side effects, or can be engineered into multivalent or multi-specific neutralising antibodies. The selected antibodies can also be manufactured on an industrial scale to meet increasing clinic demands. The shark VNARs and llama nanobodies represent promising approaches for various therapeutic applications, since they could bind to cryptic epitopes that are inaccessible to full antibodies [63]. These variable domains could additionally bypass any potential ADE associated with SARS-CoV-2 infection, as they lack the Fc domain. Therefore, they could be considered an effective therapeutic option against coronaviruses.
Nevertheless, there are issues that should be considered related to dosing instructions, potential side effects, and drug interactions. Possible side effects of Casirivimab and Imdevimab include: anaphylaxis and infusion-related reactions, fever, chills, hives, itching, and flushing [53]. In addition, viral diversity and mutations could lead to the emergence of viruses with resistance mutations under the selective pressure of mAb treatment [54]. The latter point could be surpassed by selecting antibodies that are being developed to target conserved regions of the viral S protein, and a combination of different mAbs targeting various sites on the S protein were also considered to overcome these anticipated mutations [13]. Certain types of anti-viral antibodies could also be involved in a phenomenon known as ADE, where antibodies could enhance the infection and increase the severity of the resulting disease [64]. ADE, however, is a very complex process that involves different sophisticated factors that require comprehensive understanding prior to concluding whether a specific antibody is involved in this process or not.
2. Antibody-Dependent Enhancement (ADE)
2.1. The Principle of ADE
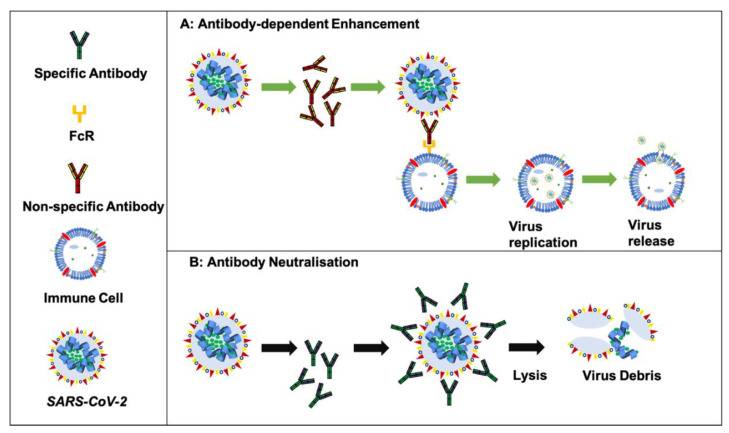
Antibodies involved in ADE may be generated from a previous infection or vaccination, and although virus-specific antibodies generally play a crucial role in infection control, sometimes the antibodies may aid viral replication [65]. This could occur upon infection with a different strain of the virus, when antibodies from a prior infection are still circulating or are induced by stimulation of memory cells (mainly B cells). These non-neutralising antibodies may bind to the virus and improve their uptake into the host cells. Further intracellular signalling could promote replication of the virus (Figure 2), and, as the virions are taken up by Fc-receptor bearing host cells [66], this results in wide-spread amplification of the original infection, resulting in severe and life-threatening viral infection [65].
Figure 2.
Schematic representation of antibody neutralisation versus ADE. Panel A indicates the extrinsic ADE mechanism, showing enhanced viral entry. The intrinsic ADE pathway leads to increased virus production by inhibition of the type1 interferon. Figure modified from Zhou et al. [67].
There are generally two mechanisms of ADE: (1) extrinsic ADE, which contributes to enhanced viral entry and occurs through Fc-receptor facilitated virus contact and entry following viral receptor-mediated endocytosis [68] and (2) intrinsic ADE, which results in increased virus production by inhibition of type1 interferon (IFN1) and activation of interleukin-10 (IL10) biosynthesis [69]. Various studies have acknowledged the involvement of Fcγ receptors (FcγRs), surface receptors expressed on immune cell surfaces to recognise the Fc portion of IgG antibodies and activate comprehensive effector functions, as crucial mediators of ADE [66].
2.2. ADE in Viruses
Numerous articles have examined the contribution of antibodies to ADE in various flaviviruses, such as Dengue virus, Zika virus, and the enhancement of Zika by West Nile virus (WNV) antibodies [70,71,72]. ADE was initially described in Dengue virus infection [70]. The mechanism of ADE in Dengue virus was proposed to be intrinsic, which includes alteration of innate immune effectors by internalised virus-immune complexes to favour enhanced replication and release [73]. The antibodies’ role was postulated when reports suggested that patients with a particularly severe Dengue virus infection were associated with prior infection with a different Dengue virus serotype and pre-existing, non-neutralising anti-Dengue virus antibodies [74]. Activating FcγRs, such as FcγRIIa and FcγRIIIa, could promote Dengue virus infection, while FcγRIIb could generate a negative regulator for the ADE process [75,76].
The envelope of the Dengue virus contains the surface proteins E and M. E glycoprotein has a crucial function in viral attachment to cells [77]. The M protein can be found in two forms: prM, an immature precursor of the M protein and mature extracellular virions with the M protein. PrM is cleaved during maturation to yield the full M protein, induced during primary Dengue infection; and prM specific antibodies are highly cross-reactive, infection-enhancing, and possess limited neutralisation properties [78]. In secondary infection, these antibodies can bind to the infecting virus and so are postulated to play a key role in Fc-mediated ADE [78]. FcγR-mediated entry and infection enhancement, as key immune evasion mechanisms for Dengue virus, were demonstrated both in vitro and in vivo [79,80]. In addition, abrogation of the Fc–FcγR binding resulted in diminishing the pathogenic activity of these antibodies [81], and patients with symptomatic Dengue virus infection possess elevated serum levels of Fc glycoforms, with improved affinity for FcγRIIIa [82], and increased allelic frequency affinity single nucleotide polymorphism (SNP) of FcγRIIa [83]. An SNP in FcγRIIa could result in altered affinity of the receptor for different subclasses of IgG antibodies, and is crucial in determining the protection from, or the susceptibility to, severe clinical infection of dengue. These results have collectively highlighted the role of activating FcγRs in modulating Dengue virus infection.
In addition to the role of antibodies in Dengue virus, Furuyama et al. [84] studied the mechanism of ADE in Ebola virus in vitro, and found that besides Fc-receptor mediated ADE, the virus could utilise complement component C1q for ADE of infection. The C1q mechanism is independent of Fc-receptor mediated ADE, and is driven by the cross-linking of virus-antibody C1q complexes to cell surface C1q receptors [84]. However, both animal and clinical studies have failed to support a pathogenic role for antibodies in these infections [66]. Administration of a subset of potently neutralising mAbs revealed no protection, and a subset of highly protective mAbs only showed moderate neutralising activity, suggesting neutralisation was not sufficient for protection or strong neutralising activity is not consistently essential for protection [85]. In addition, FcγR engagement was essential for their antiviral potency, as loss of their FcγR binding capacity was accompanied with considerable decline in their protective activity [86]. Furthermore, the therapeutic implementation of anti-Ebola virus mAb114, a single monoclonal antibody targeting the RBD of Ebola virus glycoprotein did not cause side effects related to disease enhancement [87].
Antibodies against Dengue virus have shown a wide variety of in vitro cross-reactivity with Zika virus, and West Nile virus (WNV), especially between the former [71,88,89,90]. Both viruses share immunodominant epitopes that can provoke cross-reactive T lymphocytes to create protective immune responses [91,92]. The enhancement of Zika virus infection by antibodies from humans with symptomatic or asymptomatic WNV infection was tested in vitro [72]. Antibody-positive sera failed to inhibit Zika virus, and was proposed to cause an enhancement of the infection, which was attributed to the presence of non-neutralising antibodies to E protein that bind the pathogen, but do not interfere with infectivity, stimulating Fc-receptor mediated ADE [72]. The majority of specific antibodies against Zika virus were able to increase heterotypic viral replication in vitro [93,94]. Moreover, this proposed ADE process was prevented through blockage of Fc-FcγR interaction by antibody mutation [95] or pre-treatment with α-FcR antibodies [95,96]. Likewise, antibodies against WNV have enhanced Zika virus infection [71]. These in vitro data, nevertheless, were difficult to be extrapolated in vivo, as animal studies have shown conflicting outcomes [71,95,97]. Consequently, these results exemplify the divergence between in vitro and in vivo evaluation that adds huge complexity to the ability to understand and confirm whether a specific antibody contributes to the ADE process.
2.3. ADE in SARS-CoV
ADE in coronaviruses could be driven by FcγR bearing cells, and involves the key structural proteins found in these viruses, especially the S and N proteins that represent the core mechanism through which viral entry and infection occur [98]. Therefore, it is important to study the interactions of these proteins when developing vaccines against coronaviruses to ensure maximum efficacy, and minimise the possibility of ADE. Antibodies generated by the human immune system in response to SARS-CoV infections target the S protein, and these may contribute to the Fcγ-mediated ADE of the SARS-CoV virus [98]. A study in mice has attributed ADE in SARS-CoV infection to be driven by IgG1 antibodies against the S protein, while anti-S protein IgG2a antibodies neutralised the virus, without the generation of ADE [99]. A further study in mice showed that immunisation with the SARS-CoV S protein aggravated the infection by causing Th2-type immunopathologic lung symptoms [100]. In addition, Wang et al. [101] studied different peptides of the SARS-CoV S protein and concluded that peptide-based vaccines could be designed to avoid ADE via elimination of the S597–603 epitope. It is noteworthy that cytokines secreted by Th1 and Th2 cells mediate isotype switching to IgG2a and IgG1, respectively [102]. In addition, the IgG1 and IgG2a ratio denotes the balance between humoral immunity (Th2 based) and cellular immunity (Th1 based) [103].
The in vitro mechanism of ADE against SARS-CoV varies considerably from the well-established mechanisms that govern ADE in Dengue virus. The antibodies produced against the S protein could increase the binding of the virus to FcyRII receptors, and lead to enhancement of uptake by host cells [104]. Dengue virus ADE depends on activating FcγRs like FcγRIIa and FcγRIIIa, whereas ADE mediated by SARS-CoV mAbs is dependent primarily on the inhibitory FcγRIIb, and has been shown to cause preferential infection of B cell (cell lines) in vitro [75,105]. Viral subunit vaccines frequently comprise immunodominant epitopes that are non-neutralising and could divert host immune responses, and these epitopes should be excluded in any prospective vaccine design. For instance, a vaccine developed for Middle East respiratory syndrome coronavirus (MERS-CoV) used an immunofocusing approach, through testing of the neutralising immunogenicity index, to specifically target the S1 domain of the virus RBD protein [106]. This resulted in a better immune response than targeting the full S protein, with notably high titres of neutralising antibodies for the S1 domain of the S protein [106]. Wan et al. [107] also investigated the ADE mechanism for MERS-CoV, and the antibody/Fc receptor complex was found to mimic the viral receptor involved in mediating viral entry.
A novel mechanism for ADE occurrence was found to involve a neutralising antibody binding to the S protein [107]. This was thought to trigger a conformational change of the S protein and mediate viral entry into FcγRs expressing cells through canonical viral-receptor-dependent-pathways [107]. Despite this possible entry mode, SARS-CoV can bind with high affinity to its entry receptor ACE2, so it is uncertain whether the virus needs to utilise low-affinity FcγRs, like FcγRIIb, for infection within the lung microenvironment. In Dengue virus, the situation was different because the lack of a specialised high-affinity entry receptor could force the virus to utilise the FcγR pathway [66]. In contrast to Dengue virus infections, cells expressing FcγR cannot withstand productive SARS-CoV infection, as these cell types are not tolerant for viral replication [108]. Yip et al. [109] demonstrated the occurrence of ADE in SARS-CoV Spike-pseudotyped lentiviral particles. ADE was seen to occur in different immune cell types, particularly in the monocytic cell lineage and the enhancement of infection in human macrophages by the presence of anti-viral antibodies. Furthermore, ADE of SARS-CoV infection was found to depend on the properties of the intracellular domain of FcγRII [109]. Consequently, the complexity of these observations should be considered, when developing new vaccines targeting SARS-CoV-2.
2.4. ADE in SARS-CoV-2
SARS-CoV-2 could follow an Fcγ-mediated ADE mechanism. Structural proteins S and N are likely to play a crucial role in any possible ADE, although there are not enough studies to verify this for the new virus [98]. A further study investigating antibodies against the N protein showed the opposite, suggesting the cross-reactive IgG presence is exclusive to the S protein [110]. As the SARS-CoV-2 pandemic has progressed, a compelling observation was noted in relation to the early appearance of IgG rather than IgM in certain patients [111]. This point could facilitate Fcγ-mediated ADE, and the early emergence of IgG could contribute to disease prognosis [111]. In addition, pre-existing anti-coronavirus IgG antibodies from a previous infection may cross react with SARS-CoV-2, and contribute to increased ADE and severity of COVID-19 disease [107]. There is evidence of cross-reactivity between SARS-CoV and other human coronaviruses (229E and OC43) [112]. Therefore, there might be a suggestion that any IgG induced or present from previous coronavirus infections could contribute to ADE and enhance disease progression in SARS-CoV-2. However, further understanding of the binding sites and the complexity of the immune system is crucially important as for instance, a SARS-CoV specific antibody, CR3022, was found to bind to the S protein of SARS-CoV-2, at an epitope that does not overlap with the ACE2 binding site [113]. Whilst another recent study has found a poor cross-neutralisation response between SARS-CoV and SARS-CoV-2, indicating the presence of non-neutralising antibodies that could contribute to the ADE process in SARS-CoV-2 [114]. The influence of a cross-neutralisation response is yet to be studied for SARS-CoV-2, but this phenomenon has previously been observed in other coronaviruses [98,100,115]. Consequently, further in vivo studies are required to confirm these points and to understand if antibodies could contribute to ADE following a SARS-CoV-2 infection. A further consideration for ADE in SARS-CoV-2 could be the influence of other coronaviruses [116]. The antigenic epitope heterogeneity occurring as a result of priming of infected individuals by prior coronavirus exposure could lead to the enhancement of COVID-19. This phenomenon has been observed previously, where SARS-CoV was said to be the cause of high mortality in China [117], with the priming virus a previous mild strain of coronavirus—229E [117].
Preclinical studies of inactivated vaccine candidates against SARS-CoV-2 in rodents and non-human primates demonstrated the stimulation of protective IgG responses, without sign of ADE [118]. Furthermore, sequence variability in coding genes for FcγR, along with extensive interspecies differences in the structure and function of FcγR could hinder our ability to understand data from these different animal models [119]. Passive transfer of convalescent plasma to serious cases of COVID-19 had a satisfactory safety profile, which demonstrates that IgG antibodies do not have pathogenic concerns and instead provide important clinical benefits [120]. This was substantiated by a study of 20,000 patients suffering severely from COVID-19, as they showed an adverse event incidence of 1–3% [121], while the occurrence of ADE has been linked to reduced titres of neutralising antibodies [122]. Another factor to consider when studying ADE in SARS-CoV-2 is mutations. There have been several new strains such as the Delta strain, which is around 60% more transmissible than the Alpha variant [123], and the Omicron variant, which 3x more transmissible than the Delta strain [124], as of yet though, there is as yet no clear-cut evidence of ADE in SARS-CoV-2. Furthermore, new viral strains are continuing to develop in other animal species and we need to remain vigilant for other emerging zoonotic strains and their consequences on human health. This might be due to the way the virus interacts with the immune system, the virus may be sufficiently adapted to humans [125], and if it were to interact with non-neutralising antibodies, the interaction may not be strong enough to cause ADE. Furthermore, even though ADE has previously been observed with SARS-CoV [98] and MERS-CoV [107] clinical data has not yet established a role for ADE in SARS-CoV-2 [126]. There has also been no sign of vaccine-mediated disease enhancement in the clinical trials for the COVID-19 vaccines [127,128]. The ongoing development in COVID-19 research field is additionally leading to the enhancement of our understanding of ADE. Okuya et al. [129] recently reported ADE antibodies are produced by the SARS-CoV-2 virus, after ADE antibodies were found in 41.4% of the tested COVID-19 patients. The occurrence of ADE in SARS-CoV-2 can be mediated by two different mechanisms, the FcγR and C1q, and the latter has also been previously reported in Ebola virus [84]. Due to the expression of FcγR on immune cells and the SARS-CoV-2 virus primarily targeting respiratory epithelial cells, ADE in SARS-CoV-2 is more likely to occur by the C1q mechanism found in respiratory epithelial cells [129]. Furthermore, by using convalescent-phase plasma and baby hamster kidney cells expressing FcγRs, Maemura et al. [41] found FcγRIIA and FcγRIIIA facilitated ADE infection in SARS-CoV-2. It is crucially important to extend these studies to include a larger number of COVID-19 patient samples to confirm the clinical significance of ADE in SARS-CoV-2 infection.
3. Conclusions and Future Considerations
This narrative review has focussed on the potential for ADE in SARS-CoV-2 in humans. This field is ever-evolving, and currently, there is limited evidence supporting ADE in COVID-19. ADE could appear following an infection with a different strain of the virus, when antibodies from a prior infection are regenerated, but cannot effectively neutralise the pathogen. FcγR-mediated entry and infection enhancement is a key mechanism that could contribute to ADE. However, the divergence between in vitro and in vivo data has added significant difficulty in our ability to understand and confirm whether a specific antibody or mechanism can contribute to the ADE process. Therefore, careful considerations should be dedicated to this phenomenon throughout the development of anti-viral antibodies. ADE mitigation strategies like targeted vaccine development, or the development of immunotherapeutics specifically targeting RBD, could be useful in the case of COVID-19 [130]. This is due to the previously aforementioned lessons learnt from SARS-CoV and MERS-CoV. Another approach could be directed to block certain epitopes on SARS-CoV-2 by glycosylation [131]. This means leaving only the RBD on the S protein free, which would only produce neutralising antibodies, preventing the development of non-neutralising antibodies and minimising the risk of ADE [131]. Alternatively, an immunofocussed approach could be taken, as previously reported for MERS-CoV [106], which works by developing therapeutics targeting only the receptor binding motifs in RBD, producing a better immune response and therefore a higher quantity of neutralising antibodies [106].
On the other hand, mAbs may be engineered to selectively target the motifs in RBD involved in the production of neutralising antibodies, minimising the chance of ADE and protecting the host from COVID-19 [132]. Additionally, the Fc region of an antibody could be engineered to reduce binding to the FcγR on cells, minimising ADE and specifically treating disease. This approach has been utilised previously in the successful generation of mAbs with preferential binding to treat another disease [133]. This methodology has also been trialled previously, where glycoengineered Fc-domain variants exhibited unique binding properties, and could effectively work against ADE [134,135]. Fab antibody fragments or single domain antibodies (nanobodies) could also be used in the development of effective treatments, as a lack of a Fc domain means there would be no risk of ADE [136]. However, this would result in these antibodies having a reduced half-life, requiring multiple doses for the same effect, or alternative engineering approaches to extend their longevity. The small size of these antibody fragments could enable them to interact with cryptic (hidden or sequestered) epitopes and inhibit virus attachment to host cells through steric hindrance [63]. These precautionary approaches, along with increasing knowledge in Fcγ pathways could provide a firm foundation for the development of effective antibody-based therapeutics without inducing ADE, as well as providing improved therapeutic efficacy.
For instance, AstraZeneca has recently announced the results of primary completion of a Phase 3 trial (PROVENT), in which 5197 people globally, with various immune deficiencies received a dose of either a mAbs-based cocktail (AZD7442) or a placebo (Clinical trial ID: NCT04625725). AZD7442 reduced risk of developing symptomatic COVID-19 by 77% and was the first antibody combination to potentially provide long-lasting protection against COVID-19 [137]. Similarly, Eli Lilly has announced the successful completion of their Phase 3 trial on 1035 participants (Clinical trial ID: NCT04427501). The study tested the efficacy and safety of LY-CoV555 (Bamlanivimab) and LY-CoV016 (Etesevimab) mAbs in preventing severe SARS-CoV-2 infection among infected high-risk ambulatory patients. The mAbs given in combination led to a lower incidence of COVID-19 related hospitalisation and death than the placebo [138]. Reaching positive outcomes from these trials will support the chance of using these mAbs to protect immunocompromised patients or elderly people who can generate insufficient natural antibodies in response to the vaccine. These antibody therapeutics have the potential to be highly beneficial for COVID-19 patients that cannot obtain full protection through currently approved vaccines. In addition, anti-SARS-CoV-2 antibodies could be highly valuable in immunocompromised patients, such as those with AIDS, or patients receiving anticancer drugs, radiation therapy, and stem cell or organ transplant.
Author Contributions
M.M.A.Q. conceptualised the paper. This was developed with M.A.H.F. and R.A. and the former also led the overall writing activities. The article was designed and revised critically by V.A.F. and P.A.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
M.A.H.F. is funded by BBSRC UK grant number BB/T508792/1. M.M.A.Q. acknowledges financial support from the EPSRC grant No. EP/R51178X/1.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hanley B., Naresh K., Roufosse C., Nicholson A.G., Weir J., Cooke G.S., Thursz M., Manousou P., Corbett R., Goldin R., et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: A post-mortem study. Lancet Microbe. 2020;1:e245–e253. doi: 10.1016/S2666-5247(20)30115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farouq M.A.H., Al Qaraghuli M.M., Kubiak-Ossowska K., Ferro V.A., Mulheran P.A. Biomolecular interactions with nanoparti-cles: Applications for COVID-19. Curr. Opin. Colloid Interface Sci. 2021;54:101461. doi: 10.1016/j.cocis.2021.101461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shin D., Mukherjee R., Grewe D., Bojkova D., Baek K., Bhattacharya A., Schulz L., Widera M., Mehdipour A.R., Tascher G., et al. Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity. Nature. 2020;587:657–662. doi: 10.1038/s41586-020-2601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alsaadi E.A.J., Jones I.M. Membrane binding proteins of coronaviruses. Future Virol. 2019;14:275–286. doi: 10.2217/fvl-2018-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gui M., Liu X., Guo D., Zhang Z., Yin C.-C., Chen Y., Xiang Y. Electron microscopy studies of the coronavirus ribonucleoprotein complex. Protein Cell. 2017;8:219–224. doi: 10.1007/s13238-016-0352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mishra A., Rathore A.S. RNA dependent RNA polymerase (RdRp) as a drug target for SARS-CoV2. J. Biomol. Struct. Dyn. 2021:1–13. doi: 10.1080/07391102.2021.1875886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogando N.S., Zevenhoven-Dobbe J.C., van der Meer Y., Bredenbeek P.J., Posthuma C.C., Snijder E.J. The Enzymatic Activity of the nsp14 Exoribonuclease Is Critical for Replication of MERS-CoV and SARS-CoV-2. J. Virol. 2020;94:e01246-20. doi: 10.1128/JVI.01246-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pearson L.-A., Green C.J., Lin D., Petit A.-P., Gray D.W., Cowling V.H., Fordyce E.A. Development of a High-Throughput Screening Assay to Identify Inhibitors of the SARS-CoV-2 Guanine-N7-Methyltransferase Using RapidFire Mass Spectrometry. SLAS DISCOVERY Adv. Sci. Drug Discov. 2021;26:749–756. doi: 10.1177/24725552211000652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Selvaraj C., Dinesh D.C., Panwar U., Abhirami R., Boura E., Singh S.K. Structure-based virtual screening and molecular dynam-ics simulation of SARS-CoV-2 Guanine-N7 methyltransferase (nsp14) for identifying antiviral inhibitors against COVID-19. J. Biomol. Struct. Dyn. 2020;39:4582–4593. doi: 10.1080/07391102.2020.1778535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grottesi A., Bešker N., Emerson A., Manelfi C., Beccari A.R., Frigerio F., Lindahl E., Cerchia C., Talarico C. Computational Studies of SARS-CoV-2 3CLpro: Insights from MD Simulations. Int. J. Mol. Sci. 2020;21:5346. doi: 10.3390/ijms21155346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lambert L., Culley F.J. Innate Immunity to Respiratory Infection in Early Life. Front. Immunol. 2017;8:1570. doi: 10.3389/fimmu.2017.01570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tartey S., Takeuchi O. Pathogen recognition and Toll-like receptor targeted therapeutics in innate immune cells. Int. Rev. Immunol. 2017;36:57–73. doi: 10.1080/08830185.2016.1261318. [DOI] [PubMed] [Google Scholar]
- 14.Totura A.L., Whitmore A., Agnihothram S., Schäfer A., Katze M.G., Heise M.T., Baric R.S. Toll-like receptor 3 signaling via TRIF contributes to a protective innate immune response to severe acute severe acute respiratory syndrome coronavirus infection. mBio. 2015;6:e00638-15. doi: 10.1128/mBio.00638-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dosch S.F., Mahajan S.D., Collins A.R. SARS coronavirus spike protein-induced innate immune response occurs via activation of the NF-kappaB pathway in human monocyte macrophages in vitro. Virus Res. 2009;142:19–27. doi: 10.1016/j.virusres.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barrat F.J., Crow M.K., Ivashkiv L.B. Interferon target-gene expression and epigenomic signatures in health and disease. Nat. Immunol. 2019;20:1574–1583. doi: 10.1038/s41590-019-0466-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Majoros A., Platanitis E., Kernbauer-Hölzl E., Rosebrock F., Müller M., Decker T. Canonical and Non-Canonical Aspects of JAK–STAT Signaling: Lessons from Interferons for Cytokine Responses. Front. Immunol. 2017;8:29. doi: 10.3389/fimmu.2017.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells A., Coyne C.B. Type III Interferons in Antiviral Defenses at Barrier Surfaces. Trends Immunol. 2018;39:848–858. doi: 10.1016/j.it.2018.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kotenko S.V., Durbin J.E. Contribution of type III interferons to antiviral immunity: Location, location, location. J. Biol. Chem. 2017;292:7295–7303. doi: 10.1074/jbc.R117.777102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lokugamage K.G., Hage A., de Vries M., Valero-Jimenez A.M., Schindewolf C., Dittmann M., Rajsbaum R., Menachery V.D. Type I Interferon Susceptibility Distinguishes SARS-CoV-2 from SARS-CoV. J. Virol. 2020;94:e01410-20. doi: 10.1128/JVI.01410-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stanifer M.L., Kee C., Cortese M., Zumaran C.M., Triana S., Mukenhirn M., Kraeusslich H.-G., Alexandrov T., Bartenschlager R., Boulant S. Critical Role of Type III Interferon in Controlling SARS-CoV-2 Infection in Human Intestinal Epithelial Cells. Cell Rep. 2020;32:107863. doi: 10.1016/j.celrep.2020.107863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blanco-Melo D., Nilsson-Payant B.E., Liu W.C., Uhl S., Hoagland D., Møller R., Jordan T.X., Oishi K., Panis M., Sachs D., et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell. 2020;181:1036–1045.e9. doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hadjadj J., Yatim N., Barnabei L., Corneau A., Boussier J., Smith N., Péré H., Charbit B., Bondet V., Chenevier-Gobeaux C., et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee J.S., Shin E.-C. The type I interferon response in COVID-19: Implications for treatment. Nat. Rev. Immunol. 2020;20:585–586. doi: 10.1038/s41577-020-00429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kikkert M. Innate Immune Evasion by Human Respiratory RNA Viruses. J. Innate Immun. 2020;12:4–20. doi: 10.1159/000503030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen J., Lau Y.F., Lamirande E.W., Paddock C.D., Bartlett J.H., Zaki S.R., Subbarao K. Cellular immune responses to severe acute respira-tory syndrome coronavirus (SARS-CoV) infection in senescent BALB/c mice: CD4+ T cells are important in control of SARS-CoV infection. J. Virol. 2010;84:1289–1301. doi: 10.1128/JVI.01281-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peng Y., Mentzer A.J., Liu G., Yao X., Yin Z., Dong D., Dejnirattisai W., Rostron T., Supasa P., Liu C., et al. Broad and strong memory CD4(+) and CD8(+) T cells induced by SARS-CoV-2 in UK convalescent individuals following COVID-19. Nat. Immunol. 2020;21:1336–1345. doi: 10.1038/s41590-020-0782-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diao B., Wang C., Tan Y., Chen X., Liu Y., Ning L., Chen L., Li M., Liu Y., Wang G., et al. Reduction and Functional Exhaustion of T Cells in Patients with Coro-navirus Disease 2019 (COVID-19) Front. Immunol. 2020;11:827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gallais F., Velay A., Wendling M.-J., Nazon C., Partisani M., Sibilia J., Candon S., Fafi-Kremer S. Intrafamilial Exposure to SARS-CoV-2 Induces Cel-lular Immune Response without Seroconversion. Emerg. Infect. Dis. 2021;27:113–121. doi: 10.3201/eid2701.203611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marklund E., Leach S., Axelsson H., Nyström K., Norder H., Bemark M., Angeletti D., Lundgren A., Nilsson S., Andersson L.-M., et al. Serum-IgG responses to SARS-CoV-2 after mild and severe COVID-19 infection and analysis of IgG non-responders. PLoS ONE. 2020;15:e0241104. doi: 10.1371/journal.pone.0241104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piccoli L., Park Y.-J., Tortorici M.A., Czudnochowski N., Walls A.C., Beltramello M., Silacci-Fregni C., Pinto D., Rosen L.E., Bowen J.E., et al. Mapping Neutralizing and Immu-nodominant Sites on the SARS-CoV-2 Spike Receptor-Binding Domain by Structure-Guided High-Resolution Serol. Cell. 2020;183:1024–1042.e21. doi: 10.1016/j.cell.2020.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gaebler C., Wang Z., Lorenzi J.C.C., Muecksch F., Finkin S., Tokuyama M., Cho A., Jankovic M., Schaefer-Babajew D., Oliveira T.Y., et al. Evolution of Antibody Immunity to SARS-CoV-2. Nature. 2021;591:639–644. doi: 10.1038/s41586-021-03207-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robbiani D.F., Gaebler C., Muecksch F., Lorenzi J.C.C., Wang Z., Cho A., Agudelo M., Barnes C.O., Gazumyan A., Finkin S., et al. Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature. 2020;584:437–442. doi: 10.1038/s41586-020-2456-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson E.M., Goodwin E.C., Verma A., Arevalo C.P., Bolton M.J., Weirick M.E., Gouma S., McAllister C.M., Christensen S.R., Weaver J., et al. Seasonal human coronavirus antibodies are boosted upon SARS-CoV-2 infection but not associated with protection. Cell. 2021;184:1858–1864. doi: 10.1016/j.cell.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shrock E., Fujimura E., Kula T., Timms R.T., Lee I.-H., Leng Y., Robinson M.L., Sie B.M., Li M.Z., Chen Y., et al. Viral epitope profiling of COVID-19 patients reveals cross-reactivity and correlates of severity. Science. 2020;370:eabd4250. doi: 10.1126/science.abd4250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rydyznski M.C., Ramirez S.I., Dan J.M., Grifoni A., Hastie K.M., Weiskopf D., Belanger S., Abbott R.K., Kim C., Choi J., et al. Antigen-Specific Adaptive Im-munity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity. Cell. 2020;183:996–1012.e19. doi: 10.1016/j.cell.2020.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen P., Nirula A., Heller B., Gottlieb R.L., Boscia J., Morris J., Huhn G., Cardona J., Mocherla B., Stosor V., et al. SARS-CoV-2 Neutralizing Antibody LY-CoV555 in Outpa-tients with Covid-19. N. Engl. J. Med. 2021;384:229–237. doi: 10.1056/NEJMoa2029849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weinreich D.M., Sivapalasingam S., Norton T., Ali S., Gao H., Bhore R., Musser B.J., Soo Y., Rofail D., Im J., et al. REGN-COV2, a Neutralizing Antibody Cocktail, in Outpatients with Covid-19. N. Engl. J. Med. 2021;384:238–251. doi: 10.1056/NEJMoa2035002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wørzner K., Sheward D.J., Schmidt S.T., Hanke L., Zimmermann J., McInerney G., Hedestam G.B.K., Murrell B., Christensen D., Pedersen G.K. Adjuvanted SARS-CoV-2 spike protein elicits neutralizing antibodies and CD4 T cell responses after a single immunization in mice. EBioMedicine. 2021;63:103197. doi: 10.1016/j.ebiom.2020.103197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sánchez-Zuno G.A., Matuz-Flores M.G., González-Estevez G., Nicoletti F., Turrubiates-Hernández F.J., Mangano K., Munoz-Valle J.F. A review: Antibody-dependent enhancement in COVID-19: The not so friendly side of antibodies. Int. J. Immunopathol. Pharmacol. 2021;35:20587384211050199. doi: 10.1177/20587384211050199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maemura T., Kuroda M., Armbrust T., Yamayoshi S., Halfmann P.J., Kawaoka Y. Antibody-Dependent Enhancement of SARS-CoV-2 Infection Is Mediated by the IgG Receptors FcγRIIA and FcγRIIIA but Does Not Contribute to Aberrant Cytokine Production by Macrophages. mBio. 2021;12:e0198721. doi: 10.1128/mBio.01987-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Munnur D., Teo Q., Eggermont D., Lee H.H.Y., Thery F., Ho J., Wilhelmina van Leur S., Ng W.W.S., Siu L.Y.L., Beling A., et al. Altered ISGylation drives aberrant macrophage-dependent immune responses during SARS-CoV-2 infection. Nat. Immunol. 2021;22:1416–1427. doi: 10.1038/s41590-021-01035-8. [DOI] [PubMed] [Google Scholar]
- 43.Heitmann J.S., Bilich T., Tandler C., Nelde A., Maringer Y., Marconato M., Reusch J., Jäger S., Denk M., Richter M., et al. A COVID-19 peptide vaccine for the induction of SARS-CoV-2 T cell immunity. Nature. 2022;601:617–622. doi: 10.1038/s41586-021-04232-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sparrow E., Friede M., Sheikh M., Torvaldsen S. Therapeutic antibodies for infectious diseases. Bull. World Health Organ. 2017;95:235–237. doi: 10.2471/BLT.16.178061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brandtzaeg P. Induction of secretory immunity and memory at mucosal surfaces. Vaccine. 2007;25:5467–5484. doi: 10.1016/j.vaccine.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 46.Klasse P.J., Sanders R.W., Cerutti A., Moore J.P. How can HIV-type-1-Env immunogenicity be improved to facilitate anti-body-based vaccine development? AIDS Res. Hum. Retrovir. 2012;28:1–15. doi: 10.1089/aid.2011.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Edwards M.J., Dimmock N.J. Hemagglutinin 1-specific immunoglobulin G and Fab molecules mediate postattachment neu-tralization of influenza A virus by inhibition of an early fusion event. J. Virol. 2001;75:10208–10218. doi: 10.1128/JVI.75.21.10208-10218.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maciejewski J.P., Weichold F.F., Young N.S., Cara A., Zella D., Reitz M.S., Gallo R.C. Intracellular expression of antibody fragments directed against HIV reverse transcriptase prevents HIV infection in vitro. Nat. Med. 1995;1:667–673. doi: 10.1038/nm0795-667. [DOI] [PubMed] [Google Scholar]
- 49.England N. Interim Clinical Commissioning Policy: Antivirals or Neutralising Monoclonal Antibodies for Non-Hospitalised patients with COVID-19 (Version 5) 2022. [(accessed on 21 April 2022)]. Available online: https://www.england.nhs.uk/coronavirus/documents/c1603-interim-clinical-commissioning-policy-antivirals-or-neutralising-monoclonal-antibodies-for-non-hospitalised-patients-with-covid-19-version-5/
- 50.Andabaka T., Nickerson J.W., Rojas-Reyes M.X., Rueda J.D., Vrca V.B., Barsic B. Monoclonal antibody for reducing the risk of respiratory syncytial virus infection in children. Cochrane Database Syst. Rev. 2013;38:CD006602. doi: 10.1002/14651858.CD006602.pub4. [DOI] [PubMed] [Google Scholar]
- 51.Mulangu S., Dodd L.E., Davey R.T., Jr., Tshiani Mbaya O., Proschan M., Mukadi D., Lusakibanza Manzo M., Nzolo D., Tshomba Oloma A., Ibanda A., et al. A Randomized, Controlled Trial of Ebola Virus Disease Therapeutics. N. Engl. J. Med. 2019;381:2293–2303. doi: 10.1056/NEJMoa1910993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yamamoto B.J., Shadiack A.M., Carpenter S., Sanford D., Henning L.N., O’Connor E., Gonzales N., Mondick J., French J., Stark G.V., et al. Efficacy Projection of Obiltoxaximab for Treatment of Inhalational Anthrax across a Range of Disease Severity. Antimicrob. Agents Chemother. 2016;60:5787–5795. doi: 10.1128/AAC.00972-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.COVID-19 CotC FDA Authorizes Monoclonal Antibody for Treatment of COVID-19: FDA; 2020. [(accessed on 12 January 2021)]; Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-monoclonal-antibodies-treatment-covid-19.
- 54.Ju B., Zhang Q., Ge J., Wang R., Sun J., Ge X., Yu J., Shan S., Zhou B., Song S., et al. Human neutralizing antibodies elicited by SARS-CoV-2 infection. Nature. 2020;584:115–119. doi: 10.1038/s41586-020-2380-z. [DOI] [PubMed] [Google Scholar]
- 55.Wu Y., Li C., Xia S., Tian X., Kong Y.., Wang Z., Gu C., Zhang R., Tu C., Xie Y., et al. Identification of Human Single-Domain Antibodies against SARS-CoV-2. Cell Host Microbe. 2020;27:891–898.e5. doi: 10.1016/j.chom.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huo J., Le Bas A., Ruza R.R., Duyvesteyn H.M.E., Mikolajek H., Malinauskas T., Tan T.K., Rijal P., Dumoux M., Ward P.N., et al. Neutralizing nanobodies bind SARS-CoV-2 spike RBD and block interaction with ACE2. Nat. Struct. Mol. Biol. 2020;27:846–854. doi: 10.1038/s41594-020-0469-6. [DOI] [PubMed] [Google Scholar]
- 57.Ubah O.C., Lake E.W., Gunaratne G.S., Gallant J.P., Fernie M., Robertson A.J., Marchant J.S., Bold T.D., Langlois R.A., Matchett W.E., et al. Mechanisms of SARS-CoV-2 neutralization by shark variable new antigen receptors elucidated through X-ray crystallography. Nat. Commun. 2021;12:7325. doi: 10.1038/s41467-021-27611-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chi X., Liu X., Wang C., Zhang X., Li X., Hou J., Ren L., Jin Q., Wang J., Yang W. Humanized single domain antibodies neutralize SARS-CoV-2 by targeting the spike receptor binding domain. Nat. Commun. 2020;11:4528. doi: 10.1038/s41467-020-18387-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pinto D., Park Y.J., Beltramello M., Walls A.C., Tortorici M.A., Bianchi S., Jaconi S., Culap K., Zatta F., Marco A.D., et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature. 2020;583:290–295. doi: 10.1038/s41586-020-2349-y. [DOI] [PubMed] [Google Scholar]
- 60.Dong J., Huang B., Wang B., Titong A., Gallolu K.S., Jia Z., Wright M., Parthasarathy P., Liu Y. Development of humanized tri-specific nano-bodies with potent neutralization for SARS-CoV-2. Sci. Rep. 2020;10:17806. doi: 10.1038/s41598-020-74761-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Parzych E., Weiner D.B. Nucleic acid approaches to antibody-based therapeutics for COVID-19: A perspective. J. Allergy Clin. Immunol. 2020;146:537–540. doi: 10.1016/j.jaci.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Halwe S., Kupke A., Vanshylla K., Liberta F., Gruell H., Zehner M., Rohde C., Krähling V., Serra M.G., Kreer C., et al. Intranasal Administration of a Monoclonal Neutraliz-ing Antibody Protects Mice against SARS-CoV-2 Infection. Viruses. 2021;13:1498. doi: 10.3390/v13081498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Al Qaraghuli M.M., Ferro V.A. Analysis of the binding loops configuration and surface adaptation of different crystallized single-domain antibodies in response to various antigens. J. Mol. Recognit. 2017;30:e25923. doi: 10.1002/jmr.2592. [DOI] [PubMed] [Google Scholar]
- 64.Tirado S.M.C., Yoon K.-J. Antibody-Dependent Enhancement of Virus Infection and Disease. Viral Immunol. 2003;16:69–86. doi: 10.1089/088282403763635465. [DOI] [PubMed] [Google Scholar]
- 65.Kulkarni R. Dynamics of Immune Activation in Viral Diseases. Springer Science and Business Media LLC.; Berlin, Germany: 2020. Antibody-Dependent Enhancement of Viral Infections; pp. 9–41. [Google Scholar]
- 66.Bournazos S., Gupta A., Ravetch J.V. The role of IgG Fc receptors in antibody-dependent enhancement. Nat. Rev. Immunol. 2020;20:633–643. doi: 10.1038/s41577-020-00410-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhou Z., Wang X., Fu Y., Zhang X., Liu C. Letter to the editor: Neutralizing antibodies for the treatment of COVID-19. Acta Pharm. Sin. B. 2020;11:304–307. doi: 10.1016/j.apsb.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tsai T.-T., Chuang Y.-J., Lin Y.-S., Wan S.-W., Chen C.-L., Lin C.-F. An emerging role for the anti-inflammatory cytokine interleu-kin-10 in dengue virus infection. J. Biomed. Sci. 2013;20:40. doi: 10.1186/1423-0127-20-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tsai T.-T., Chuang Y.-J., Lin Y.-S., Chang C.P., Wan S.W., Lin S.H., Chen C.-L., Lin C.-F. Antibody-dependent enhancement infection facilitates den-gue virus-regulated signaling of IL-10 production in monocytes. PLoS Negl. Trop. Dis. 2014;8:e3320. doi: 10.1371/journal.pntd.0003320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Halstead S.B., Chow J.S., Marchette N.J. Immunological enhancement of dengue virus replication. Nat. New Biol. 1973;243:24–26. [PubMed] [Google Scholar]
- 71.Bardina S.V., Bunduc P., Tripathi S., Duehr J., Frere J.J., Brown J.A., Nachbagauer R., Foster G.A., Krysztof D., Tortorella D., et al. Enhancement of Zika virus pathogenesis by preexisting antiflavivirus immunity. Science. 2017;356:175–180. doi: 10.1126/science.aal4365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Garg H., Yeh R., Watts D.M., Mehmetoglu-Gurbuz T., Resendes R., Parsons B., Gonzales F., Joshi A. Enhancement of Zika virus infection by an-tibodies from West Nile virus seropositive individuals with no history of clinical infection. BMC Immunol. 2021;22:5. doi: 10.1186/s12865-020-00389-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Narayan R., Tripathi S. Intrinsic ADE: The Dark Side of Antibody Dependent Enhancement During Dengue Infection. Front. Cell. Infect. Microbiol. 2020;10:580096. doi: 10.3389/fcimb.2020.580096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Katzelnick L.C., Gresh L., Halloran M.E., Mercado J.C., Kuan G., Gordon A., Balmaseda A., Harris E. Antibody-dependent enhancement of severe dengue disease in humans. Science. 2017;358:929–932. doi: 10.1126/science.aan6836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chan K.R., Zhang S.L., Tan H.C., Chan Y.K., Chow A., Lim A.P., Vasudevan S.G., Hanson B.J., Ooi E.E. Ligation of Fc gamma receptor IIB inhibits anti-body-dependent enhancement of dengue virus infection. Proc. Natl. Acad. Sci. USA. 2011;108:12479–12484. doi: 10.1073/pnas.1106568108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thulin N.K., Brewer R.C., Sherwood R., Bournazos S., Edwards K.G., Ramadoss N.S., Taubenberger J.K., Memoli M., Gentles A.J., Jagannathan P., et al. Maternal Anti-Dengue IgG Fucosyla-tion Predicts Susceptibility to Dengue Disease in Infants. Cell Rep. 2020;31:107642. doi: 10.1016/j.celrep.2020.107642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bowden T.A., Jones E.Y., Stuart D.I. Cells under siege: Viral glycoprotein interactions at the cell surface. J. Struct. Biol. 2011;175:120–126. doi: 10.1016/j.jsb.2011.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guzman M.G., Vázquez S. The Complexity of Antibody-Dependent Enhancement of Dengue Virus Infection. Viruses. 2010;2:2649–2662. doi: 10.3390/v2122649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Diamond M.S., Edgil D., Roberts T.G., Lu B., Harris E. Infection of Human Cells by Dengue Virus Is Modulated by Different Cell Types and Viral Strains. J. Virol. 2000;74:7814–7823. doi: 10.1128/JVI.74.17.7814-7823.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pinto A.K., Brien J.D., Lam C.Y., Johnson S., Chiang C., Hiscott J., Sarathy V.V., Barrett A.D., Shresta S., Diamond M.S. Defining New Therapeutics Using a More Immunocompe-tent Mouse Model of Antibody-Enhanced Dengue Virus Infection. mBio. 2015;6:e01316-15. doi: 10.1128/mBio.01316-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Halper-Stromberg A., Lu C.-L., Klein F., Horwitz J.A., Bournazos S., Nogueira L., Eisenreich T.R., Liu C., Gazumyan A., Schaefer U., et al. Broadly Neutralizing Antibodies and Viral Inducers Decrease Rebound from HIV-1 Latent Reservoirs in Humanized Mice. Cell. 2014;158:989–999. doi: 10.1016/j.cell.2014.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang T.T., Sewatanon J., Memoli M.J., Wrammert J., Bournazos S., Bhaumik S.K., Pinsky B.A., Chokephaibulkit K., Onlamoon N., Pattanapanyasat K., et al. IgG antibodies to dengue enhanced for FcγRIIIA binding determine disease severity. Science. 2017;355:395–398. doi: 10.1126/science.aai8128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mohsin S.N., Saleem M., Ghafoor F., Raza S.M., Mahmood S., Amar A. Association of FcγRIIa Polymorphism with Clinical Outcome of Dengue Infection: First Insight from Pakistan. Am. J. Trop. Med. Hyg. 2015;93:691–696. doi: 10.4269/ajtmh.15-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Furuyama W., Nanbo A., Maruyama J., Marzi A., Takada A. A complement component C1q-mediated mechanism of anti-body-dependent enhancement of Ebola virus infection. PLoS Negl. Trop. Dis. 2020;14:e0008602. doi: 10.1371/journal.pntd.0008602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gunn B.M., Yu W.-H., Karim M.M., Brannan J.M., Herbert A.S., Wec A.Z., Halfmann P.J., Fusco M.L., Schendel S., Gangavarapu K., et al. A Role for Fc Function in Therapeutic Monoclonal Antibody-Mediated Protection against Ebola Virus. Cell Host Microbe. 2018;24:221–233.e5. doi: 10.1016/j.chom.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bournazos S., DiLillo D.J., Goff A.J., Glass P.J., Ravetch J.V. Differential requirements for FcγR engagement by protective anti-bodies against Ebola virus. Proc. Natl. Acad. Sci. USA. 2019;116:20054–20062. doi: 10.1073/pnas.1911842116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gaudinski M.R., Coates E.E., Novik L., Widge A., Houser K.V., Burch E., Holman L.A., Gordon I.J., Chen G.L., Carter C., et al. Safety, tolerability, pharmacokinetics, and immu-nogenicity of the therapeutic monoclonal antibody mAb114 targeting Ebola virus glycoprotein (VRC 608): An open-label phase 1 study. Lancet. 2019;393:889–898. doi: 10.1016/S0140-6736(19)30036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sapparapu G., Fernandez E.P.-A., Kose N., Cao B., Fox J., Bombardi R.G., Zhao H., Nelson C.A., Bryan A.L., Barnes T., et al. Neutralizing human antibodies prevent Zika virus replication and fetal disease in mice. Nature. 2016;540:443–447. doi: 10.1038/nature20564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kam Y.-W., Lee C.Y.-P., Teo T.-H., Howland S.W., Amrun S.N., Lum F.-M., See P., Kng N.Q.-R., Huber R.G., Xu M.-H., et al. Cross-reactive dengue human monoclonal anti-body prevents severe pathologies and death from Zika virus infections. JCI Insight. 2017;2:e92428. doi: 10.1172/jci.insight.92428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pantoja P., Pérez-Guzmán E.X., Rodríguez I.V., White L.J., González O., Serrano C., Giavedoni L., Hodara V., Cruz L., Arana T., et al. Zika virus pathogenesis in rhesus ma-caques is unaffected by pre-existing immunity to dengue virus. Nat. Commun. 2017;8:15674. doi: 10.1038/ncomms15674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Grifoni A., Pham J., Sidney J., O’Rourke P.H., Paul S., Peters B., Martini S.R., de Silva A.D., Ricciardi M.J., Magnani D.M., et al. Prior Dengue Virus Exposure Shapes T Cell Immunity to Zika Virus in Humans. J. Virol. 2017;91:e01469-17. doi: 10.1128/JVI.01469-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wen J., Tang W.W., Sheets N., Ellison J., Sette A., Kim K., Shresta S. Identification of Zika virus epitopes reveals immunodominant and protective roles for dengue virus cross-reactive CD8+ T cells. Nat. Microbiol. 2017;2:17036. doi: 10.1038/nmicrobiol.2017.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dejnirattisai W., Jumnainsong A., Onsirisakul N., Fitton P., Vasanawathana S., Limpitikul W., Puttikhunt C., Edwards C., Duangchinda T., Supasa S., et al. Cross-Reacting Antibodies Enhance Dengue Virus Infection in Humans. Science. 2010;328:745–748. doi: 10.1126/science.1185181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kawiecki A.B., Christofferson R.C. Zika Virus–Induced Antibody Response Enhances Dengue Virus Serotype 2 Replication In Vitro. J. Infect. Dis. 2016;214:1357–1360. doi: 10.1093/infdis/jiw377. [DOI] [PubMed] [Google Scholar]
- 95.Stettler K., Beltramello M., Espinosa D.A., Graham V., Cassotta A., Bianchi S., Vanzetta F., Minola A., Jaconi S., Mele F., et al. Specificity, cross-reactivity, and function of antibodies elicited by Zika virus infection. Science. 2016;353:823–826. doi: 10.1126/science.aaf8505. [DOI] [PubMed] [Google Scholar]
- 96.Paul L.M., Carlin E.R., Jenkins M.M., Tan A.L., Barcellona C.M., Nicholson C.O., Michael S.F., Isern S. Dengue virus antibodies enhance Zika virus infection. Clin. Transl. Immunol. 2016;5:e117. doi: 10.1038/cti.2016.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Martín-Acebes M.A., Saiz J.-C., Jiménez de Oya N. Antibody-Dependent Enhancement and Zika: Real Threat or Phantom Menace? Front. Cell. Infect. Microbiol. 2018;8:44. doi: 10.3389/fcimb.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang S.-F., Tseng S.-P., Yen C.-H., Yang J.-Y., Tsao C.-H., Shen C.-W., Chen K.-H., Liu F.-T., Liu W.-T., Chen Y.-M.A., et al. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem. Biophys. Res. Commun. 2014;451:208–214. doi: 10.1016/j.bbrc.2014.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jaume M., Yip M.S., Cheung C.Y., Leung H.L., Li P.H., Kien F., Dutry I., Callendret B., Escriou N., Altmeyer R., et al. Anti-Severe Acute Respiratory Syndrome Coronavirus Spike Antibodies Trigger Infection of Human Immune Cells via a pH- and Cysteine Protease-Independent FcγR Pathway. J. Virol. 2011;85:10582–10597. doi: 10.1128/JVI.00671-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tseng C.-T., Sbrana E., Iwata-Yoshikawa N., Newman P.C., Garron T., Atmar R.L., Peters C.J., Couch R.B. Immunization with SARS Coronavirus Vaccines Leads to Pulmonary Immunopathology on Challenge with the SARS Virus. PLoS ONE. 2012;7:e35421. doi: 10.1371/annotation/2965cfae-b77d-4014-8b7b-236e01a35492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang Q., Zhang L., Kuwahara K., Li L., Liu Z., Li T., Zhu H., Liu J., Xu Y., Xie J., et al. Immunodominant SARS Coronavirus Epitopes in Humans Elicited both Enhancing and Neutralizing Effects on Infection in Non-human Primates. ACS Infect. Dis. 2016;2:361–376. doi: 10.1021/acsinfecdis.6b00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rostamian M., Sohrabi S., Kavosifard H., Niknam H.M. Lower levels of IgG1 in comparison with IgG2a are associated with protective immunity against Leishmania tropica infection in BALB/c mice. J. Microbiol. Immunol. Infect. 2017;50:160–166. doi: 10.1016/j.jmii.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 103.Zhao F., Qu J., Wang W., Li S., Xu S. The imbalance of Th1/Th2 triggers an inflammatory response in chicken spleens after ammonia exposure. Poultry Sci. 2020;99:3817–3822. doi: 10.1016/j.psj.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pierson T.C., Fremont D.H., Kuhn R.J., Diamond M.S. Structural insights into the mechanisms of antibody-mediated neutralization of flavivirus infection: Implications for vaccine development. Cell Host Microbe. 2008;4:229–238. doi: 10.1016/j.chom.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kam Y.W., Kien F., Roberts A., Cheung Y.C., Lamirande E.W., Vogel L., Chu S.L., Tse J., Guarner J., Zaki S.R., et al. Antibodies against trimeric S glycoprotein protect hamsters against SARS-CoV challenge despite their capacity to mediate FcgammaRII-dependent entry into B cells in vitro. Vaccine. 2007;25:729–740. doi: 10.1016/j.vaccine.2006.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Du L., Tai W., Yang Y., Zhao G., Zhu Q., Sun S., Liu C., Tao X., Tseng X.T.C.-T.K., Perlman S., et al. Introduction of neutralizing immunogenicity index to the rational design of MERS coronavirus subunit vaccines. Nat. Commun. 2016;7:13473. doi: 10.1038/ncomms13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wan Y., Shang J., Sun S., Tai W., Chen J., Geng Q., He L., Chen Y., Wu J., Shi Z., et al. Molecular Mechanism for Antibody-Dependent Enhancement of Coronavirus Entry. J. Virol. 2020;94:e02015–e02019. doi: 10.1128/JVI.02015-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yip M.S., Leung N.H.L., Cheung C.Y., Li P.H., Lee H.H.Y., Daëron M., Peiris J.S.M., Bruzzone R., Jaume M. Antibody-dependent infection of human macrophages by severe acute respiratory syndrome coronavirus. Virol. J. 2014;11:82. doi: 10.1186/1743-422X-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yip M.S., Leung H.L., Li P.H., Cheung C.Y., Dutry I., Li D., Daëron M., Bruzzone R., Peiris J.S.M., Jaume M. Antibody-dependent enhancement of SARS coronavirus infection and its role in the pathogenesis of SARS. Hong Kong Med. J. 2016;22:25–31. doi: 10.1186/1753-6561-5-S1-P80. [DOI] [PubMed] [Google Scholar]
- 110.Tan W., Lu Y., Zhang J., Wang J., Dan Y., Tan Z., He X., Qian C., Sun Q., Hu Q., et al. Viral Kinetics and Antibody Responses in Patients with COVID-19. medRxiv. 2020 doi: 10.1101/2020.03.24.20042382. [DOI] [Google Scholar]
- 111.Long Q.-X., Deng H.-J., Chen J., Hu J.-L., Liu B.-Z., Liao P., Lin Y., Yu L.-H., Mo Z., Xu Y.-Y., et al. Antibody responses to SARS-CoV-2 in COVID-19 patients: The per-spective application of serological tests in clinical practice. medRxiv. 2020 doi: 10.1101/2020.03.18.20038018. [DOI] [Google Scholar]
- 112.Che X.-Y., Qiu L.-W., Liao Z.-Y., Wang Y.-D., Wen K., Pan Y.-X., Hao W., Mei Y.-B., Cheng V.C.C., Yuen K.-Y. Antigenic Cross-Reactivity between Severe Acute Respiratory Syndrome—Associated Coronavirus and Human Coronaviruses 229E and OC43. J. Infect. Dis. 2005;191:2033–2037. doi: 10.1086/430355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tian X., Li C., Huang A., Xia S., Lu S., Shi Z., Lu L., Jiang S., Yang Z., Wu Y., et al. Potent binding of 2019 novel coronavirus spike protein by a SARS corona-virus-specific human monoclonal antibody. Emerg. Microbes Infect. 2020;9:382–385. doi: 10.1080/22221751.2020.1729069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lv H., Wu N.C., Tsang O.T.-Y., Yuan M., Perera R.A.P.M., Leung W.S., So R.T.Y., Chan J.M.C., Yip G.K., Chik T.S.H., et al. Cross-reactive Antibody Response between SARS-CoV-2 and SARS-CoV Infections. Cell Rep. 2020;31:107725. doi: 10.1016/j.celrep.2020.107725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Weiss R.C., Scott F.W. Antibody-mediated enhancement of disease in feline infectious peritonitis: Comparisons with dengue hemorrhagic fever. Comp. Immunol. Microbiol. Infect. Dis. 1981;4:175–189. doi: 10.1016/0147-9571(81)90003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tetro J.A. Is COVID-19 receiving ADE from other coronaviruses? Microbes Infect. 2020;22:72–73. doi: 10.1016/j.micinf.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ho M.-S., Chen W.-J., Chen H.-Y., Lin S.-F., Wang M.-C., Di J., Lu Y.-T., Liu C.-L., Chang S.-C., Chao C.-L., et al. Neutralizing Antibody Response and SARS Severity. Emerg. Infect. Dis. 2005;11:1730–1737. doi: 10.3201/eid1111.040659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gao Q., Bao L., Mao H., Wang L., Xu K., Yang M., Li Y., Zhu L., Wang N., Lv Z., et al. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369:77. doi: 10.1126/science.abc1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bournazos S. IgG Fc Receptors: Evolutionary Considerations. Curr. Top Microbiol. Immunol. 2019;423:1–11. doi: 10.1007/82_2019_149. [DOI] [PubMed] [Google Scholar]
- 120.Joyner M.J., Wright R.S., Fairweather D., Senefeld J.W., Bruno K.A., Klassen S.A., Carter R.E., Klompas A.M., Wiggins C.C., Shepherd J.R.A., et al. Early Safety Indicators of COVID-19 Convalescent Plasma in 5000 Patients. J. Clin. Investig. 2020;130:4791–4797. doi: 10.1172/JCI140200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Joyner M.J., Bruno K.A., Klassen S.A., Kunze K.L., Johnson P.W., Lesser E.R., Wiggins C.C., Senefeld J.W., Klompas A.M., Hodge D.O., et al. Safety Update: COVID-19 Convalescent Plasma in 20,000 Hospitalized Patients. Mayo Clin. Proc. 2020;95:1888–1897. doi: 10.1016/j.mayocp.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Arvin A.M., Fink K., Schmid M.A., Cathcart A., Spreafico R., Havenar-Daughton C., Lanzavecchia A., Corti D., Virgin H.W. A perspective on potential anti-body-dependent enhancement of SARS-CoV-2. Nature. 2020;584:353–363. doi: 10.1038/s41586-020-2538-8. [DOI] [PubMed] [Google Scholar]
- 123.Mahase E. Delta variant: What is happening with transmission, hospital admissions, and restrictions? BMJ. 2021;373:n1513. doi: 10.1136/bmj.n1513. [DOI] [PubMed] [Google Scholar]
- 124.Nishiura H., Ito K., Anzai A., Kobayashi T., Piantham C., Rodríguez-Morales A.J. Relative Reproduction Number of SARS-CoV-2 Omicron (B.1.1.529) Compared with Delta Variant in South Africa. J. Clin. Med. 2022;11:30. doi: 10.3390/jcm11010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Choe H., Farzan M. How SARS-CoV-2 first adapted in humans. Science. 2021;372:466. doi: 10.1126/science.abi4711. [DOI] [PubMed] [Google Scholar]
- 126.Lee W.S., Wheatley A.K., Kent S.J., DeKosky B.J. Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies. Nat. Microbiol. 2020;5:1185–1191. doi: 10.1038/s41564-020-00789-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., Perez J.L., Pérez Marc G., Moreira E.D., Zerbini C., et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., Diemert D., Spector S.A., Rouphael N., Creech C.B., et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2020;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Okuya K., Hattori T., Saito T., Takadate Y., Sasaki M., Furuyama W., Marzi A., Ohiro Y., Konno S., Hattori T., et al. Multiple Routes of Antibody-Dependent Enhance-ment of SARS-CoV-2 Infection. Microbiol Spectr. 2022;10 doi: 10.1128/spectrum.01553-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yang L., Liu S., Liu J., Zhang Z., Wan X., Huang B., Chen Y., Zhang Y. COVID-19: Immunopathogenesis and Immunotherapeutics. Signal Transduct. Target. Ther. 2020;5:128. doi: 10.1038/s41392-020-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Liu L., Wang P., Nair M.S., Yu J., Rapp M., Wang Q., Luo Y., Chan J.F.-W., Sahi V., Figueroa A., et al. Potent neutralizing antibodies against multiple epitopes on SARS-CoV-2 spike. Nature. 2020;584:450–456. doi: 10.1038/s41586-020-2571-7. [DOI] [PubMed] [Google Scholar]
- 132.DeFrancesco L. COVID-19 antibodies on trial. Nat. Biotechnol. 2020;38:1242–1252. doi: 10.1038/s41587-020-0732-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.De Goeij B.E.C.G., Janmaat M.L., Andringa G., Kil L., Van Kessel B., Frerichs K.A., Lingnau A., Freidig A., Mutis T., Sasser A.K., et al. Hexabody-CD38, a Novel CD38 Antibody with a Hexamerization Enhancing Mutation, Demonstrates Enhanced Complement-Dependent Cytotoxicity and Shows Potent Anti-Tumor Activity in Preclinical Models of Hematological Malignancies. Blood. 2019;134:3106. doi: 10.1182/blood-2019-125788. [DOI] [Google Scholar]
- 134.Wang X., Mathieu M., Brezski R.J. IgG Fc engineering to modulate antibody effector functions. Protein Cell. 2017;9:63–73. doi: 10.1007/s13238-017-0473-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mimoto F., Katada H., Kadono S., Igawa T., Kuramochi T., Muraoka M., Wada Y., Haraya K., Miyazaki T., Hattori K. Engineered antibody Fc variant with selectively enhanced FcγRIIb binding over both FcγRIIa(R131) and FcγRIIa(H131) Protein Eng. Des. Sel. PEDS. 2013;26:589–598. doi: 10.1093/protein/gzt022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lu Q., Zhang Z., Li H., Zhong K., Zhao Q., Wang Z., Wu Z., Yang D., Sun S., Yang N., et al. Development of multivalent nanobodies blocking SARS-CoV-2 infec-tion by targeting RBD of spike protein. J. Nanobiotechnol. 2021;19:33. doi: 10.1186/s12951-021-00768-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.AZD7442 PROVENT Phase III Prophylaxis Trial Met Primary Endpoint in Preventing COVID-19 2021. [(accessed on 9 November 2021)]. Available online: https://www.astrazeneca.com/media-centre/press-releases/2021/azd7442-prophylaxis-trial-met-primary-endpoint.html.
- 138.Dougan M., Nirula A., Azizad M., Mocherla B., Gottlieb R.L., Chen P., Hebert C., Perry R., Boscia J., Heller B., et al. Bamlanivimab plus Etesevimab in Mild or Moderate Covid-19. N. Engl. J. Med. 2021;385:1382–1392. doi: 10.1056/NEJMoa2102685. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.