Abstract
Objective
Frontline healthcare workers (FHCWs) responding to the COVID-19 pandemic develop posttraumatic stress disorder (PTSD), major depressive disorder (MDD) and generalized anxiety disorder (GAD) symptoms. Such symptoms are associated with burnout, occupational and relational difficulties. In the current study, we examined the prospective association between acute transdiagnostic COVID-19-related PTSD, MDD, and GAD symptoms at pandemic outset, and burnout and functional difficulties several months later in FHCWs in New York City.
Methods
Wave 1 symptoms of COVID-19-related PTSD, MDD, and GAD, were assessed in 787 FHCWs from April 14 to May 11th, 2020. Burnout and occupational difficulties were assessed at wave 1 and wave 2, approximately 7 months later.
Results
After adjusting for wave 1 burnout, wave 1 MDD symptoms, particularly sleep difficulties, loss of interest, and feeling tired/having little energy, collectively explained 42% incremental variance in this outcome. After adjusting for wave 1 work difficulties, MDD and PTSD symptoms, particularly feeling tired/having little energy, loss of interest, and negative expectations of self/world, collectively explained 42% incremental variance in this outcome. After adjusting for wave 1 relationship difficulties, MDD, GAD, and PTSD symptoms, particularly depressed mood, irritability, and appetite disturbance, explained 26% incremental variance in this outcome.
Conclusions
Results highlight psychiatric symptoms assessed during the acute phase of the COVID-19 pandemic that may help predict burnout and work and relationship difficulties in FHCWs. Early interventions aimed at ameliorating transdiagnostic symptoms of MDD, PTSD, and GAD may help mitigate risk for burnout and functional difficulties in this population.
Keywords: SARS COVID-19, Frontline healthcare workers, Mental health impact, Burnout, Relationship outcomes, Occupational outcomes
1. Introduction
Since the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), first in Wuhan, China in December 2019, and subsequently the in the rest of the world including the U.S., researchers have sought to document the mental health impact on frontline healthcare workers (FHCWs). Findings from such studies showed that FHCWs exhibited increases in depressive, anxiety, and posttraumatic stress symptoms, in addition to overall psychological distress (see Moitra et al., 2021). In previous studies of the mental health impact of the COVID-19 pandemic on FHCWs in the greater New York City area, an area that was particularly hard-hit in the early stages the pandemic, we showed that approximately 25% of the individuals in our sample screened positive for COVID-19-related symptoms of posttraumatic stress disorder (PTSD), major depressive disorder (MDD), or generalized anxiety disorder (GAD; Feingold et al., 2021; Kachadourian et al., 2021). We also showed that approximately 40% of FHCWs working directly with patients diagnosed with COVID-19 screened positive for burnout and reported work and relationship difficulties.
As the pandemic continues beyond two years in duration, research has shifted to considering the longer-term mental health impact that the pandemic has had on the lives of FHCWs. To date, however, most studies have been cross-sectional in nature or have had short-term follow-up periods (i.e., four to eight weeks; Van Steenkiste et al., 2021). Previous studies on the long-term impact of other disease outbreaks on the lives of FHCWs have shown that the impact can be significant and chronic in nature. For example, one study examining the occupational impact of the 2003 severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) outbreak found that healthcare workers who treated SARS patients indicated significantly more missed work shifts because of stress or illness as well as decreases in face-to-face patient contact compared to healthcare workers who did not treat SARS patients, 13–26 months after the outbreak (Maunder et al., 2006). They also found that FHCWs reported significantly higher levels of burnout and overall psychological distress.
In addition to a lack of research on the longer-term mental health impact of the COVID-19 pandemic on FHCWs, little is known about which psychiatric symptoms experienced during the initial pandemic surge are linked to greater risk of burnout and functional difficulties (e.g. workplace and relational challenges) in this population. Focusing on individual symptoms of distinct diagnoses (e.g., PTSD, MDD, GAD) is important as symptoms within each disorder may contribute more strongly to different aspects of functioning than others (Fried and Nesse, 2014). Such a ‘symptomics’ approach allows for a more nuanced understanding of the impact of individual psychological symptoms and outcomes of relevance to stress-exposed populations. In our previous study (Kachadourian et al., 2021), we examined cross-sectional associations between transdiagnostic pandemic-related PTSD, MDD, and GAD symptoms, and burnout and functional difficulties. Results revealed that tiredness/low energy, irritability, and feeling nervous showed the strongest associations with burnout. Further, having negative expectations of oneself or the world, concentration difficulties, and irritability showed the strongest association with work difficulties, while irritability, having negative expectations about oneself or the world, and feeling bad about oneself showed the strongest association with relationship difficulties.
To date, no known longitudinal study has examined which transdiagnostic pandemic-related PTSD, MDD, and GAD symptoms predict burnout, work and relationship functioning over time in FHCWs. As such, we sought to build on our previous study (Kachadourian et al., 2021) and examine longitudinal associations between these transdiagnostic symptoms, assessed during the initial pandemic surge in New York City, and burnout, work and relationship functioning seven months later. Using a novel analytic approach that accounts for intercorrelations among baseline measures of these outcomes and these symptoms, we also sought to examine which Wave 1 symptoms of PTSD, MDD, and GAD were the strongest determinants of these outcomes.
2. Methods
2.1. Participants and procedure
The study sample included health care workers working at The Mount Sinai Hospital (MSH), an urban tertiary care hospital in New York City. Hospital and administrative leaders helped to identify the groups most likely to be involved in frontline care prior to procuring contact information for study invitation. The sample included attending-level physician faculty and house staff from various departments, patient-facing nurses and nurse practitioners, physician assistants, hospital chaplains, psychologists, social workers, and dietitians. An electronically-administered anonymous survey was then sent to those FHCWs most likely to be directly involved in the care of patients infected with COVID-19, either as a result of their standard practice or anticipated redeployment within the study period. Participants were excluded if email invitations went undelivered to addresses on file.
Wave 1 data were collected between April 14th and May 11th, 2020. This period corresponded with the initial peak and downward slope of the epidemic curve at MSH, as defined by COVID-19 inpatient census data. Participants were eligible to receive a $25 gift card after survey completion, based on filling out a separate form to endorse study participation that was not linked to the study survey. Self-generating research codes were used to enable data linkage to future surveys while preserving anonymity. The entire sample was re-contacted seven months later to complete a wave 2 follow-up assessment and were eligible to receive an iPad, AirPods, or Apple watch via raffle. No participants were contacted between waves 1 and 2. The study was approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai.
Of the 6026 presumed FHCWs, 3360 completed the wave 1 survey (55.8%), of which 2579 (76.8%) endorsed having frontline responsibilities; median completion date = 04/21/20; range = 04/14/20–05/11/20. For wave 2, 787 (30.5%) completed the follow-up assessment (median completion date = 12/6/20; range = 11/19/20–1/10/21). Distributions of age, sex, profession, marital and parental status, leadership and redeployment status, and pre-pandemic psychiatric history between wave 2 completers and non-completers did not differ (all χ2<1.32, all p's > 0.20).
2.2. Study instruments
The wave 1 survey included validated instruments to assess demographic characteristics, psychological symptoms, burnout, and functional difficulties. A full description of wave 1 data is available elsewhere and is provided in Supplemental Table 1.
COVID-19-related PTSD Symptoms. Wave 1 symptoms of PTSD were assessed using a 4-item PTSD-Checklist (Geier et al., 2020), an abbreviated version of the PTSD-Checklist for DSM-5 (PCL-5; Weathers et al., 2013 ), with questions modified to assess PTSD symptoms related to COVID-19 exposure. (e.g., “Over the past two weeks, how often were you bothered by repeated, disturbing, and unwanted memories of your experiences related to the COVID-19 pandemic?”) A positive screen for significant COVID-19-related PTSD symptoms was defined by a score ≥8, which showed the highest efficiency (90.4%; sensitivity = 0.81, specificity = 0.94) in diagnosing PTSD (Geier et al., 2020) Cronbach's α = 0.82.
Major Depressive Disorder Symptoms. Wave 1 symptoms of MDD were assessed using the Patient Health Questionnaire-8 (Kroenke et al., 2009 ), an eight-item measure that assesses symptoms of MDD experienced over the previous 2 weeks. A positive screen for significant MDD symptoms was defined by a score ≥10, which yields comparable estimates of the prevalence of current major depressive or other depressive disorders relative to diagnostic interviews. Cronbach's α = 0.87.
Generalized Anxiety Disorder Symptoms. Wave 1 symptoms of GAD were assessed using the Generalized Anxiety Disorder-7 (Spitzer et al., 2006), a seven-item measure that assesses symptoms of GAD experienced over the past 2 weeks. A positive screen for significant GAD symptoms was defined by a score ≥10, which has a sensitivity of 0.89 and specificity of 0.82 in diagnosing GAD. Cronbach's α = 0.91.
Burnout. Burnout was assessed at wave 1 and wave 2 using a slightly modified single-item Mini-Z measure, which is rated on a 5-point scale and asks participants to choose the best answer (1–5) as it relates to their work experience (Rohland et al., 2004). Options are “I enjoy my work. I have no symptoms of burnout” (score of 1) to “I feel completely burnt out. I am at the point where I may need to seek help.” (score of 5). This item was modified to include a definition of burnout, as follows: “Burnout is a long-term stress reaction characterized by depersonalization, including cynical or negative attitudes toward patients, emotional exhaustion, a feeling of decreased personal achievement and a lack of empathy for patients.” A positive screen for burnout was operationalized as a score of 3 (“I am definitely burning out and have one or more symptoms of burnout, e.g., emotional exhaustion”); 4 (“The symptoms of burnout that I am experiencing won't go away. I think about work frustrations a lot”); or 5 (“I feel completely burned out. I am at the point where I may need to seek help”). The Mini-Z has been validated against the emotional exhaustion subscale of the Maslach Burnout Inventory (MBI) with a correlation of 0.64 (p < 0.001; Rohland et al., 2004).
Functional difficulties. The Brief Inventory of Psychosocial Functioning (B-IPF; Marx et al., 2019) was used to assess functional impairment in seven functional domains, including romantic relationships, family relationships, work, friendships and socializing, self-care, education, and parenting. Scores on items reflecting work difficulties (e.g., “I had trouble at work”) and relationship difficulties (e.g., “I had trouble with my family relationships”) were analyzed separately.
2.3. Data analysis
Data analyses proceeded in three steps. First, we computed descriptive statistics to summarize sociodemographic and clinical characteristics of the sample. Second, to identify individual wave 1 COVID-19-related PTSD, MDD, and GAD symptoms associated with wave 2 burnout, and work and relationship difficulties, we conducted three sets of multiple regression analyses (logistic regression for burnout, and linear regressions for work and relationship difficulties); age, gender, profession (registered nurse ([RN] vs. other), and wave 2 burnout screening status and functional difficulties were adjusted for in these analyses. These analyses included symptoms from all three of these disorders. Third, we conducted relative importance (RI) analyses using the R package relaimpo (Groemping, 2006) to assess the unique proportion of variance in these outcomes associated with each PTSD, MDD, and GAD symptom. These analyses partition the explained variance (i.e., R2) in a dependent variable that is explained by each independent variable while simultaneously accounting for intercorrelations among these independent variables. The LMG metric was used to estimate the relative importance of each PTSD, MDD, and GAD symptom by dividing the total R2 into individual values of explained variance for each symptom, which sums to the total explained R2. These values were then rescaled to range from 0 to 100% of the total explained variance. Bootstrapped 95% confidence intervals (10,000 samples) and P values of the RI coefficients were also computed to determine which wave 1 PTSD, MDD, and/or GAD symptoms were significantly associated with wave 2 burnout, and work and relationship difficulties.
3. Results
Description of the sample show that the following were <35 years of age (n = 464, 59%); female (n = 571, 72.6%); white, non-Hispanic (n = 416, 52.9%), Asian (n = 201, 25.6%), or Hispanic (n = 46, 5.9%); married/partnered (n = 569, 72.4%); and did not have children (n = 551, 70.1%). With regard to profession, 267 (34.0%) were registered nurses, 184 (23.4%) residents/fellows, 183 (23.3%) attending physicians, 114 (14.5%), mid-level providers (advanced practice registered nurse or physician assistant), and 38 (4.8%) other (e.g., clinical psychologist, social worker). At wave 2, a total of 351 FHCWs (44.7%) screened positive for burnout.
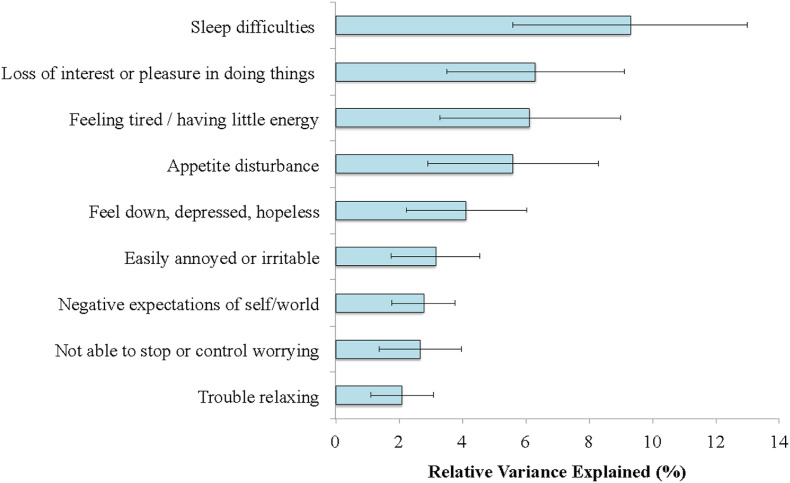
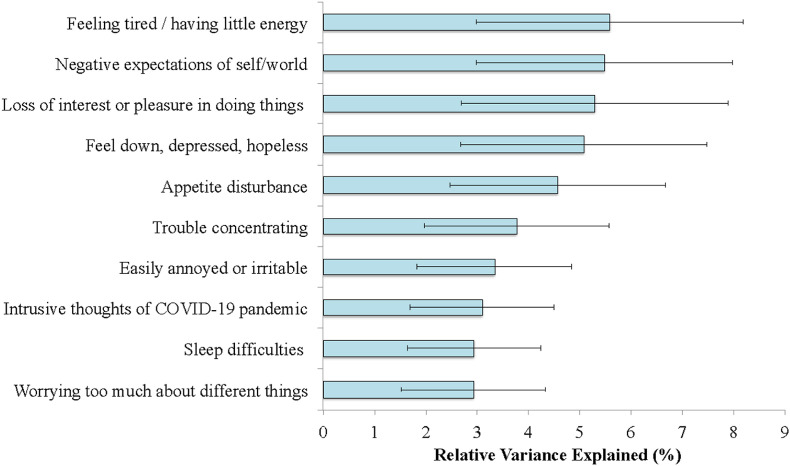
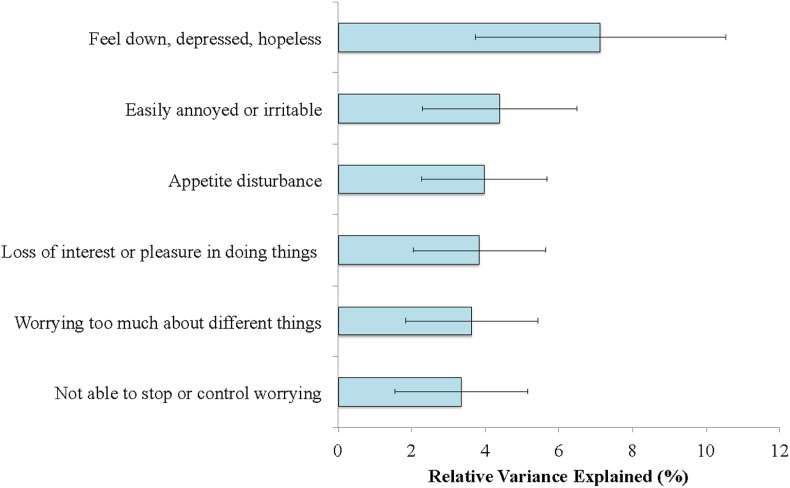
Table 1 provides descriptive statistics of wave 1 PTSD, MDD, and GAD symptoms, as well as burnout, work and relationship difficulties. Fig. 1, Fig. 2, Fig. 3 show results of relative importance analyses of wave 1 variables that significantly predicted wave 2 burnout, and work and relationship difficulties, respectively.
Table 1.
Descriptive statistics of Wave 1 PTSD, MDD, and GAD symptoms in frontline health care workers.
| Mean (SD) or n (%) |
Range |
|
|---|---|---|
| Wave 1 Symptoms | ||
| COVID-19-related PTSD symptoms (PCL4-5) | 3.8 (3.5) | 0–16 |
| Intrusive thoughts of COVID-19 pandemic | 1.2 (1.1) | 0–4 |
| Avoidance of reminders of COVID-19 pandemic | 1.1 (1.2) | 0–4 |
| Negative expectations of self/world | 0.7 (1.0) | 0–4 |
| Exaggerated startle response | 0.7 (1.0) | 0–4 |
| MDD Symptoms (PHQ-8) | 6.2 (5.0) | 0–24 |
| Feel down, depressed, hopeless | 0.7 (0.8) | 0–3 |
| Loss of interest or pleasure in doing things | 0.7 (0.8) | 0–3 |
| Sleep difficulties | 1.2 (1.0) | 0–3 |
| Feeling tired/having little energy | 1.3 (1.0) | 0–3 |
| Appetite disturbance | 1.0 (1.0) | 0–3 |
| Feeling bad about oneself | 0.4 (0.8) | 0–3 |
| Trouble concentrating | 0.6 (0.9) | 0–3 |
| Psychomotor disturbance | 0.2 (0.6) | 0–3 |
| GAD Symptoms (GAD-7) | 6.0 (5.2) | 0–21 |
| Feeling nervous, anxious, on edge | 1.2 (1.0) | 0–3 |
| Not able to stop or control worrying | 0.9 (1.0) | 0–3 |
| Worrying too much about different things | 0.8 (0.9) | 0–3 |
| Trouble relaxing | 1.0 (1.0) | 0–3 |
| Restlessness | 0.5 (0.8) | 0–3 |
| Easily annoyed or irritable | 0.9 (0.9) | 0–3 |
| Feel afraid something awful might happen | 0.8 (0.9) | 0–3 |
| Wave 1 burnout | 306 (38.9%) | – |
| Wave 1 work difficulties | 19.9 (21.9) | 0–100 |
| Wave 1 relationship difficulties | 21.0 (22.5) | 0–100 |
Abbreviations: PTSD = posttraumatic stress disorder; MDD = major depressive disorder; GAD = generalized anxiety disorder. PCL4-5: 4-item PTSD Checklist for DSM-5; PHQ-8: Patient Health Questionnaire-8; GAD-7: Generalized Anxiety Disorder-7.
Fig. 1.
Wave 1 transdiagnostic psychiatric symptoms that significantly predicted Wave 2 burnout
Note. Nagelkerke R2 for full model = 0.33. Age, gender, profession, and Wave 1 burnout explained 5.0%, 2.9%, 0.8%, and 37.1% of the variance in Wave 2 burnout, respectively; age and Wave 1 burnout were statistically significant (p < 0.05).
Only Wave 1 MDD, GAD, and PTSD symptoms that were significant (p < 0.05) predictors of Wave 2 burnout are shown.
Error bars represent 95% confidence intervals.
Fig. 2.
Wave 1 transdiagnostic psychiatric symptoms that significantly predicted Wave 2 work difficulties
Note. R2 for full model = 0.24. Age, gender, profession, and Wave 1 work difficulties explained 1.2%, 0.4%, 0.8%, and 40.5% of the relative variance in Wave 2 work difficulties, respectively, none of which were significant.
Only Wave 1 MDD, GAD, and PTSD symptoms that were significant (p < 0.05) predictors of Wave 2 work difficulties are shown.
Error bars represent 95% confidence intervals.
Fig. 3.
Wave 1 transdiagnostic psychiatric symptoms that significantly predicted Wave 2 relationship difficulties
Note. R2 for full model = 0.24. Age, gender, profession, and Wave 1 relationship difficulties explained 0.1%, 0.1%, 0.2%, and 50.4% of the relative variance in Wave 2 relationship difficulties, respectively; only Wave 1 relationship difficulties were statistically significant. Only Wave 1 MDD, GAD, and PTSD symptoms that were significant (p < 0.05) predictors of Wave 2 relationship difficulties are shown.
Error bars represent 95% confidence intervals.
Wave 1 burnout explained 37.1% of the variance in wave 2 burnout. In addition, six MDD symptoms collectively explained an additional 42% of the variance in this outcome: sleep difficulties, loss of interest or pleasure in doing things (i.e., anhedonia), feeling tired/having little energy, appetite disturbance, feeling down/depressed/hopeless and being easily annoyed/irritable.
Wave 1 work difficulties explained 40.5% of the variance in Wave 2 work difficulties. Furthermore, five MDD symptoms (feeling tired/having little energy, loss of interest or pleasure in doing things, feeling down, depressed, hopeless, appetite disturbance, and trouble concentrating), two PTSD symptoms (negative expectations of the self/world, intrusive thoughts of the COVID-19 pandemic), and two GAD symptoms (being easily annoyed or irritable, worrying too much about different things) collectively explained an additional 42% of the variance in this outcome.
Wave 1 relationship difficulties explained 50.4% of the variance in Wave 2 relationship difficulties. Furthermore, four MDD symptoms (feeling down/depressed/irritable, appetite disturbance, loss of interest or pleasure in doing things, and feeling tired/having little energy), four GAD symptoms (being easily annoyed or irritable, worrying too much about different things, not able to stop or control worrying, and trouble relaxing), and one PTSD symptom (intrusive thoughts of the COVID-19 pandemic) collectively explained an additional 26.0% of the variance in this outcome.
4. Discussion
To our knowledge, this study is the first to employ a novel ‘symptomics’ approach to examine specific symptoms of COVID-19 pandemic-related PTSD, MDD, and GAD symptoms assessed during the initial surge of the pandemic that are associated with burnout, work and relationship difficulties over time. Results revealed that, as expected, wave 1 burnout, work, and relationship difficulties accounted for a significant amount of variance in wave 2 burnout, work, and relationship difficulties, respectively. However, wave 1 MDD, PTSD, and GAD symptoms explained a substantial proportion of incremental variance in these outcomes. Specifically, wave 1 symptoms of MDD explained incremental variance in wave 2 burnout; wave 1 symptoms of MDD and GAD explained incremental variance in wave 2 work difficulties; and wave 1 symptoms of MDD, PTSD, and GAD explained incremental variance in wave 2 relationship difficulties. Of note, for wave 2 burnout and work difficulties, these transdiagnostic symptoms collectively accounted for a greater amount of explained variance than wave 1 burnout and work and difficulties (42.2% versus 37.1% in predicting wave 2 burnout; 42.1% versus 40.5% in predicting wave 2 work difficulties).
These findings overlap somewhat with findings from our previous study examining the cross-sectional association between COVID-19-related symptoms of PTSD, MDD, and GAD with burnout, work and relationship difficulties during the initial pandemic surge in New York City (Kachadourian et al., 2021). Findings from that study similarly indicated that feeling tired/having little energy and feeling easily annoyed or irritable were strongly associated with burnout; holding negative expectations of oneself and the world, trouble concentrating, and feeling easily annoyed or irritable with work difficulties; and feeling annoyed/easily irritated with relationship difficulties. Results of the current longitudinal study extend these findings to identify acute psychiatric symptoms that may be important to consider in predicting these outcomes several months into the pandemic. Specifically, sleep difficulties, loss of interest, and tiredness/low energy emerged as strong predictors of wave 2 burnout; tiredness/low energy, negative expectations, and loss of interest as strong predictors of wave 2 work difficulties; and feeling depressed, easily annoyed/irritable, and appetite disturbance of wave 2 relationship difficulties.
The finding that sleep difficulties were strongly predictive of burnout aligns with prior work documenting a decline in sleep and increase in daytime sleepiness and insomnia during the first wave of the COVID-19 pandemic (Hassinger et al., 2021), as well as a link between sleep disturbance and psychological distress in FHCWs (Diaz et al., 2022; Kaye-Kauderer et al., 2021; Serrano-Ripoll et al., 2021). Loss of interest (or anhedonia)—a cardinal feature of MDD—emerged as an important predictor of wave 2 burnout as well as work difficulties. Anhedonia, defined in DSM-5 as reduced interest or loss of pleasure in all or almost all activities, is both a core symptom of MDD and a transdiagnostic symptom that may characterize other mood and anxiety disorders, PTSD, substance use disorders, and others (Der-Avakian et al., 2016). Clinically, the presence of anhedonia is generally considered a poor prognostic factor and is associated with poor response to treatment in individuals with MDD and is also associated with an increased risk of suicide (Spijker et al., 2010; Moos and Cronkite, 1999). Basic science has demonstrated anhedonic-like behavior as a key behavioral change resulting from chronic or severe stress, in part through maladaptive effects on reward systems in the brain (for review see Pizzagalli, 2014). The findings of the current study are consistent with our emerging understanding of anhedonia as an important negative outcome following stress exposure, in this case the occupational and psychosocial stress of the COVID-19 pandemic. Clinically, these findings underscore the potential utility of prevention and treatment efforts targeting vegetative symptoms such as sleep difficulties, fatigue/low energy, and appetite disturbance (e.g., Cheng et al., 2021; Nourian et al., 2021) as part of broader mental health and resilience initiatives. Doing so may help to mitigate risk for burnout and promote functioning and well-being in FHCWs.
Of note, several wave 1 transdiagnostic symptoms that showed strong associations with wave 2 burnout, work, and relationship difficulties were also linked to these outcomes at wave 1. For example, feeling tired/having low energy explained a significant amount of variance in burnout both cross-sectionally and longitudinally, while having negative expectations about oneself and the world explained a significant amount of variance in work difficulties, both during the initial pandemic surge and over time. Finally, feeling easily annoyed or irritable emerged as one of the strongest predictors of relationship difficulties, both cross-sectionally and over time.
These findings underscore the importance of assessment, monitoring, and treatment efforts targeting these specific psychiatric symptoms, as they are associated with both acute and long-term adverse professional and personal consequences in FHCWs. For example, reducing overtime and long shifts might help to address burnout-related problems like feeling tired and having little energy (Maunder et al., 2021). They further suggest that a more nuanced, symptom-level approach to assessing psychological distress—as opposed to simply assessing whether individuals do or do not screen positive for certain disorders—may provide a more targeted approach to guiding interventions designed to mitigate risk for burnout and functional difficulties in FHCWs.
Limitations of this study must be noted. First, the relatively lower response rate at wave 2 may limit generalizability of findings; nevertheless, the demographic composition of wave 2 responders vs. non-responders was similar. Second, although the longitudinal design of our study allowed us to examine the relation between wave 1 MDD, PTSD, and GAD symptoms, and wave 2 burnout and functional difficulties, conclusions about causality are limited given the dynamic nature of how these symptoms are linked with these outcomes over time. Third, all assessments were self-report and the assessment of PTSD in wave 1 was limited to 4 symptoms specific to pandemic-related stressors. Further research that employs clinician-administered structured interviews and that includes a more comprehensive assessment of all 20 symptoms of PTSD in addition to other mental health variables (e.g., substance use) would be important in more comprehensively identifying symptom-level associations with clinically relevant outcomes in FHCWs. Finally, given the enduring nature of the COVID-19 pandemic, further research employing longer follow-up periods is needed to identify transdiagnostic symptoms linked to longer-term trajectories of burnout, functioning, and related clinical outcomes.
These limitations notwithstanding, the current study is the first, to our knowledge, to identify transdiagnostic MDD, PTSD, and GAD that are prospectively associated with burnout and functional difficulties in FHCWs. Results suggest that these symptoms may provide incremental utility in predicting these outcomes, above and beyond baseline levels of burnout and functional difficulties, though additional research is needed to evaluate this possibility. They further suggest that a symptom-level approach to assessing psychological distress during the acute phase of a pandemic may provide a more targeted approach to the assessment, monitoring, and treatment of aspects of psychopathology that are most strongly linked to adverse professional and personal consequences. For example, interventions targeting sleep difficulties (e.g., cognitive behavioral treatment for insomnia) may help mitigate risk of burnout. Further research is needed to replicate these findings in other cohorts of FHCWs; identify transdiagnostic symptoms that predict longer-term trajectories of burnout, functional difficulties, and related outcomes; and evaluate the efficacy of prevention and treatment efforts targeting key drivers of adverse outcomes (e.g., vegetative symptoms) in mitigating risk for burnout and promoting overall well-being in this population.
Author statement
Lorig K. Kachadourian, PhD-conceptualization, writing-original draft, review and editing, James W. Murrough, MD, PhD-methodology, investigation, resources, writing-review and editing, funding acquisition, Jonathan DePierro, PhD-writing-review and editing, Carly Kaplan, BS- writing-review and editing, Sabrina Kaplan, BA-writing-review and editing, Jordyn H. Feingold, MD, MAPP- writing-review and editing, Adriana Feder, MD-writing-review and editing, Dennis Charney, MD-writing-review and editing, resources, data curation, funding acquisition, Steven M. Southwick, MD-writing-review and editing, Lauren Peccoralo, MD-writing-review and editing, resources, data curation, funding acquisition, Jonathan Ripp, MD, MPH- writing-review and editing, resources, data curation, funding acquisition, Robert H. Pietrzak, PhD, MPH-conceptualization, formal analysis, writing-original draft, review and editing.
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
We understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). He/she is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. We confirm that we have provided a current, correct email address which is accessible by the Corresponding Author and which has been configured to accept email from Lorig.kachadourian@Yale.edu.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2022.05.034.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- The Brief Inventory of Psychosocial Functioning (B-Ipf). [Measurement instrument]. Available from https://www.ptsd.va.gov.
- Cheng P., Casement M.D., Kalmbach D.A., Castelan A.C., Drake C.L. Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep. 2021;44(4) doi: 10.1093/sleep/zsaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Der-Avakian A., Barnes S.A., Markou A., Pizzagalli D.A. Translational assessment of reward and motivational deficits in psychiatric disorders. Curr Top Behav Neurosci. 2016;28:231–262. doi: 10.1007/7854_2015_5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz F., Cornelius T., Bramley S., et al. The association between sleep and psychological distress among New York City healthcare workers during the COVID-19 pandemic. J. Affect. Disord. 2022;298(Pt A):618–624. doi: 10.1016/j.jad.2021.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold J.H., Peccoralo L., Chan C.C., Kaplan C.A., Kaye-Kauderer H., Charney D., Verity J., Hurtado A., Burka L., Syed S.A., Murrough J.W., Feder A., Pietrzak R.H., Ripp J. Psychological impact of the COVID-19 pandemic on frontline health care workers during the pandemic surge in New York city. Chronic Stress (Thousand Oaks) 2021;5 doi: 10.1177/2470547020977891. Feb 1. 2470547020977891, PMID: 33598592; PMCID: PMC7863176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried Eiko, L, Nesse Randolph., M The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS One. 2014;28(9 (2)):e90311. doi: 10.1371/journal.pone.0090311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geier T.J., Hunt J.C., Hanson J.L., et al. Validation of abbreviated four- and eight-item versions of the PTSD checklist for DSM-5 in a traumatically injured sample. J. Trauma Stress. 2020;33(3):218–226. doi: 10.1002/jts.22478. [DOI] [PubMed] [Google Scholar]
- Groemping U. Relative importance for linear regression in R: the package relaimpo. J. Stat. Software. 2006;17(1):1–27. [Google Scholar]
- Hassinger A.B., Breuer R.K., Mishra A. Sleep patterns of US healthcare workers during the first wave of the COVID-19 pandemic. Sleep Breath. 2021:1–11. doi: 10.1007/s11325-021-02515-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kachadourian L.K., Feder A., Murrough J.W., et al. Transdiagnostic psychiatric symptoms, burnout, and functioning in frontline health care workers responding to the COVID-19 pandemic: a symptomics analysis. J. Clin. Psychiatr. 2021;82(3) doi: 10.4088/JCP.20m13766. [DOI] [PubMed] [Google Scholar]
- Kaye-Kauderer H., Loo G., Murrough J.W., et al. Effects of sleep, exercise, and leadership support on resilience in frontline healthcare workers during the COVID-19 pandemic. J. Occup. Environ. Med. 2021 doi: 10.1097/JOM.0000000000002460. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Marx, B. P., Schnurr, P. P., Lunney, C., Weathers, F. W., Bovin, M. J., & Keane, T. M. (2019).
- Maunder R.G., Lancee W.J., Balderson K.E., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Heeney N.D., Strudwick G., et al. Burnout in hospital-based healthcare workers during COVID-19. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(46) doi: 10.47326/ocsat.2021.02.46.1.0. [DOI] [Google Scholar]
- Moitra M, Rahman M, Collins P, et al. Mental Health Consequences for Healthcare Workers During the COVID-19 Pandemic: a Scoping Review to Draw Lessons for LMICs. Front. Psychiatr. 2021;27(12) doi: 10.3389/fpsyt.2021.602614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R.H., Cronkite R.C. Symptom-based predictors of a 10-year chronic course of treated depression. J. Nerv. Ment. Dis. 1999;187(6):360–368. doi: 10.1097/00005053-199906000-00005. [DOI] [PubMed] [Google Scholar]
- Nourian M., Nikfarid L., Khavari A.M., Barati M., Allahgholipour A.R. The impact of an online mindfulness-based stress reduction program on sleep quality of nurses working in COVID-19 care units: a clinical trial. Holist. Nurs. Pract. 2021;35(5):257–263. doi: 10.1097/HNP.0000000000000466. [DOI] [PubMed] [Google Scholar]
- Pizzagalli D.A. Depression, stress, and anhedonia: toward a synthesis and integrated model. Annu. Rev. Clin. Psychol. 2014;10:393–423. doi: 10.1146/annurev-clinpsy-050212-185606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohland B.M., Kruse G.R., Rohrer J.E. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75–79. [Google Scholar]
- Serrano-Ripoll M.J., Zamanillo-Campos R., Castro A., Fiol-de Roque M.A., Ricci-Cabello I. Insomnia and sleep quality in healthcare workers fighting against COVID-19: a systematic review of the literature and meta-analysis. Actas Esp. Psiquiatr. 2021;49(4):155–179. [PubMed] [Google Scholar]
- Spijker J., de Graaf R., Ten Have M., Nolen W.A., Speckens A. Predictors of suicidality in depressive spectrum disorders in the general population: results of The Netherlands Mental Health Survey and Incidence Study. Soc. Psychiatr. Psychiatr. Epidemiol. 2010;45(5):513–521. doi: 10.1007/s00127-009-0093-6. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Van Steenkiste E., Schoofs J., Gilis S., Messiaen P. Mental health impact of COVID-19 in frontline healthcare workers in a Belgian Tertiary care hospital: a prospective longitudinal study. Acta Clin. Belg. 2021:1–8. doi: 10.1080/17843286.2021.1903660. [DOI] [PubMed] [Google Scholar]
- Weathers F.W., Litz B.T., Keane T.M., Palmieri P.A., Marx B.P., Schnurr P.P. 2013. The PTSD Checklist for DSM-5 (PCL-5) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.