Abstract
The two studies reported in the paper examined (1) the extended parallel process model’s (EPPM; Witte 1992) ability to predict and explain college students’ COVID-19 vaccination behavior, and (2) the EPPM-related reasons for college students’ COVID-19 vaccine hesitancy. Study 1 was a longitudinal study that measured the EPPM constructs at Time 1 and COVID-19 vaccine behavior two months later at Time 2. For danger control, results indicate that perceived threat and perceived efficacy positively predicted intentions and that intentions positively predicted behavior. For fear control, results indicate that perceived threat positively predicted fear, that perceived efficacy did not predict fear, and that fear negatively predicted defensive avoidance, reactance, and fatalism. Study 2 was a cross-sectional survey that assessed EPPM-related reasons for vaccine hesitancy. Results indicate that the main reasons for vaccine hesitancy were related to response efficacy (i.e., participants were concerned about the safety and effectiveness of the vaccine). The theoretical and practical implications of these results are discussed.
Keywords: Extended parallel process model (EPPM), COVID-19 vaccine, Danger control, Fear control
Introduction
The COVID-19 global pandemic has infected 213 million people and has taken the life of 4.45 million people globally since its first identification in 2019 (John Hopkins University, 2021). In addition to preventative measures such as wearing face masks and social distancing, several vaccines have been developed and approved for use since December 2020. As of March 29, 2022, 65.53% of the population in the United States have been fully vaccinated (Mathieu et al., 2021). However, many people remain uncertain or resistant toward the vaccine. SteelFisher et al. (2021) examined 39 nationally representative, randomized polls with publicly available tabulations that were conducted between August 2020 and February 2021 and found that 32% of respondents did not plan to get the vaccine.
Young adults are particularly hesitant toward vaccines. Diesel et al. (2021) found that 18- to 29-year-olds had the lowest COVID-19 vaccination coverage (38.3%), especially compared to other adult age groups such as those aged 65 or above (80%). The low COVID-19 vaccination rate is not surprising given that college students have been found to also have low flu vaccination rates ranging from 8 to 46% (National Foundation for Infectious Diseases, 2016, 2017). As new strains of the COVID-19 such as the Delta and the Omicron variants increase its rate of transmission, evidence has shown that vaccines are effective in preventing hospitalization and death (Centers for Disease Control & Prevention, 2021).
As many higher educational institutions resume in-person instructions, vaccination has become an important measure to help keep a safe campus life in such population condensed environments. Thomason and O’Leary (2021) identified 773 U.S. college campuses that mandate vaccination as of August 24, 2021. However, many other college campuses have not given any requirement on vaccination. This paper aimed to help higher education administrators develop effective communication strategies to encourage COVID-19 vaccination. Specifically, we examined how well the extended parallel process model (EPPM) predicts college students’ protective action of getting the COVID-19 vaccines and defensive reactions including defensive avoidance, reactance, and fatalism.
The extended parallel process model
Witte (1992) advanced the EPPM to help explain the effects of perceived threat and perceived efficacy on intentions and behavior. Perceived threat involves a person’s beliefs about a danger that exists in their environment. According to the EPPM, perceived threat includes two components: severity and susceptibility. Perceived severity involves beliefs about the seriousness of a health threat (i.e., “COVID-19 is a serious health problem”), and perceived susceptibility involves beliefs about the likelihood that one will experience a health threat (i.e., “it is possible that I will get COVID-19”). According to the EPPM, both perceived severity and perceived susceptibility must be high for perceived threat to be high.
Perceived efficacy involves a person’s beliefs about the effectiveness and ease with which a recommended response can prevent a threat. According to the EPPM, perceived efficacy also includes two components: response efficacy and self-efficacy. Perceived response efficacy traditionally focuses on the perceived effectiveness of the recommended response (i.e., “getting the COVID-19 vaccine is an effective way to prevent COVID-19”). In this study we added another aspect of response efficacy—perceived safety of the recommended response, which is an important and related assessment for vaccines. Perceived self-efficacy, on the other hand, focuses on one’s ability to perform the recommended behavior under various challenging circumstances (i.e., “it would be easy for me to get the COVID-19 vaccine if I wanted to). Again, according to the EPPM, both perceived response efficacy and perceived self-efficacy must be high for perceived efficacy to be high.
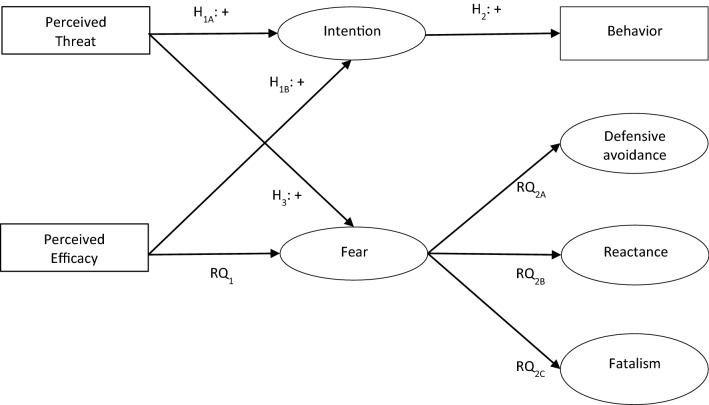
Finally, the EPPM posits that different combinations of perceived threat and perceived efficacy will lead to adaptive (i.e., danger control) or maladaptive (i.e., fear control) responses. A discussion of the conditions expected to elicit each type of response follows, and a visual summary of all hypotheses and research questions is provided in Fig. 1.
Fig. 1.
Structural model of predicted relationships for study 1
Adaptive danger control response
Danger control is a cognitive, problem-solving process where individuals strive to reduce a threat. Generally speaking, the EPPM predicts that individuals will engage in danger control when both perceived threat and perceived efficacy are high. To illustrate, if a person believes (1) that COVID-19 represents a personally relevant and serious problem (i.e., high threat), and (2) that the COVID-19 vaccine is an effective and easy way to reduce the threat (i.e., high efficacy), then they should engage in danger control and get vaccinated against COVID-19. However, questions about the exact nature of the relationship between threat and efficacy have been raised in the past two decades (i.e., is the relationship between threat and efficacy multiplicative or additive?). However, three recent meta-analyses indicate that that the relationship between threat and efficacy is additive (Sheeran et al., 2014; Tannenbaum et al., 2015; Witte & Allen, 2000), so that is what we predict in this study:
H1
(A) Perceived threat and (B) perceived efficacy will positively predict intentions to get the COVID-19 vaccine.
The EPPM also posits that when both perceived threat and perceived efficacy are high, a person should experience greater protection motivation (i.e., intention) and ultimately adaptive changes (i.e., behavior). The proposed relationship between intention and behavior is consistent with and has been well-studied by numerous other theoretical perspectives including social cognitive theory (Bandura, 2004) and the reasoned action approach (Fishbein & Ajzen, 2010). Results from numerous meta-analyses suggest that the intention-behavior relationship should be strong (e.g., McEachan et al., 2016; Rich et al., 2015). Thus, the following hypothesis is advanced:
H2
Intentions to get the COVID-19 vaccine will positively predict COVID-19 vaccine behavior.
Maladaptive fear control response
Conversely, fear control is an emotional coping process or psychological defense tactic designed to reduce fear rather than the actual threat. To illustrate, if an individual believes (1) that COVID-19 represents a personally relevant and serious problem (i.e., high threat), but (2) that the COVID-19 vaccine is not an effective or easy way to reduce the threat (i.e., low efficacy), then they will engage in fear control. Put differently, “when individuals see no efficacious means of eliminating danger, they turn to the defensive reactions as a means of reducing their fear” (Dillard et al., 2018, p. 974).
Dillard et al. (2018) investigated how defensive reactions are structured regarding one another. They concluded (1) that defensive reactions cannot be reduced to a single phenomenon, and (2) that individuals regularly experience multiple defensive reactions. Thus, this study focuses on three different defensive reactions: defensive avoidance, reactance, and fatalism. Defensive avoidance involves conscious efforts to ignore an issue. For example, an individual may refuse to think about or attempt to minimize their feelings about COVID-19. Reactance involves criticizing or rejecting the message or the source of the message. For example, an individual might believe that a message exaggerates the threat posed by COVID-19 or attempt to find flaws in the arguments or evidence. Fatalism involves a “calm and resigned acceptance of risk” (Dillard et al., 2018, p. 989). For example, an individual may believe that risks are normal or that they might contract COVID-19 no matter what they do.
The EPPM makes several specific predictions regarding the fear control process. Unfortunately, far fewer studies have investigated the fear control portion of the EPPM, and those that do often report inconsistent or contradictory results. The balance of this section will discuss each of the links in the fear control portion of the EPPM.
Witte (1992) notes that, “the greater the threat, the greater the fear aroused” (p. 339). Results from three meta-analysis are consistent with this prediction and indicate that the threat-fear relationship typically hovers around the r = 0.30 to 0.36 range (Boster & Mongeau, 1984; Mongeau, 1998; Witte & Allen, 2000). Thus, the following hypothesis is advanced:
H3
Perceived threat will positively predict fear.
Witte (1992) also notes that, “if efficacy is believed to be low, fear is increased further.” (p. 343). Unfortunately, fewer studies (and no meta-analyses that we are aware of) have explicitly examined the relationship between perceived efficacy and fear, and the studies that do exist offer conflicting results. For example, Dillard and colleagues (Dillard et al., 2017; Meczkowski et al., 2016) report that while (1) fear significantly decreased following exposure to an efficacy message (2) fear had little or no association with efficacy in their overall SEM models. A similar pattern was observed by Birmingham et al. (2015). Given these inconsistencies between theory and research, the following research question is advanced:
RQ1
What is the relationship between perceived efficacy and fear?
Finally, regarding the fear-fear control relationship, Witte (1992) predicts that, “fear causes maladaptive responses” (p. 343). Unfortunately, most EPPM studies either do not include fear control or focus on a single fear control outcome. Further, when fear control is studied, results are often inconsistent with EPPM predictions (Papova, 2012). However, the preponderance of evidence suggests that fear is negatively related to fear control (Roberto et al., 2021; Birmingham et al., 2015; De Meulenaer et al., 2015; Popova, 2012; Yang & Kahlor, 2012). Again, given the inconsistencies in theory and research, the following research question is advanced:
RQ2
What is the relationship between fear and (A) defensive avoidance, (B) reactance, and (C) fatalism?
Notably, the EPPM is not specific about which defensive reactions people will select; it simply states that individuals will engage in some sort of defensive response when perceived threat is high and perceived efficacy is low. Thus, the data will be considered consistent with the EPPM if fear positively relates to one or more of the defensive reactions included in this study.
EPPM-related reasons for COVID-19 vaccine hesitancy among college students
Finally, the EPPM provides a list of potential targets for messages design to persuade the vaccine hesitance (i.e., perceived severity, perceived susceptibility, perceived self-efficacy, and perceived response-efficacy). Thus, participants who (1) had not been vaccinated and (2) did intend to get vaccinated in the future responded to items designed to answer the following research question.
RQ3
What are the key reasons for COVID-19 vaccine hesitancy among college students?
Overview of studies
Two studies were conducted during the Spring 2021 semester to test the aforementioned hypotheses and research questions. More specifically, Study 1 employed a longitudinal design to test both hypotheses and to answer research questions 1 and 2, while Study 2 used a cross-sectional designed to answer research question 3.
Study 1
Method
Procedure and participants
Data were collected at two points in time using Qualtrics Survey Software. Participants were recruited from four undergraduate communication classes at Arizona State University. Participants received a small amount of extra credit for completing the Time 1 survey, and a small amount of extra credit or a $5 gift card for completing the Time 2 survey. All procedures were approved by the sponsoring university’s institutional review board.
Time 1 data were collected in early February 2021, or approximately two months after the U.S. Food and Drug Administration approved the first COVID-19 vaccine for emergency use on December 11, 2020 (U.S. Food and Drug Administration, 2021). Therefore, unless a college student met certain age, occupation, or health requirements, they were unable to get the vaccine in the state of Arizona at Time 1 data collection. Two-hundred and fifty-two individuals completed the Time 1 survey. Two participants indicated that they had already received both doses of the vaccine before Time 1 data collection took place (possibly because they met the criteria for vaccine emergency use) and were therefore excluded from all analyses.
Time 2 data collection took place in late April 2021, or approximately one month after the state of Arizona opened COVID-19 vaccine eligibility to anyone aged 16 and older on March 23, 2021 (Innes & Steinbach, 2021). One hundred and fifty-seven participants (62.8% of those participated in Time 1 survey) completed the Time 2 survey.
Thus, the final sample consisted of 157 participants. Participants were 44.7% male, 54.7% female, and 0.6% other, with a mean age of 19.55 (SD = 2.11). The sample was 61.1% white, 22.9% Asian, 6.4% black or African American, and 9.6% other. Finally, 19.5% of the sample identified as Hispanic or Latino/a, and 76.1% of participants were U.S. citizens.
Non-response analysis was conducted to see if there were any differences between those who did and did not respond to the Time 2 survey for any of the variables under investigation using the Time 1 data. Independent sample t-tests revealed no differences for susceptibility (t = − 1.24, df = 248; p = 0.22), self-efficacy (t = 1.44, df = 248, p = 0.20), or intention (t = − 0.89, df = 248, p = 0.37). However, for severity (t = − 2.87, df = 248; p = 0.004), response efficacy (t = − 3.02, df = 248; p = 03), and fear (t = − 2.27, df = 244; p = 0.02), those who responded at both points in time tended to score higher than participants who only responded at Time 1. Conversely, for defensive avoidance (t = 3.11, df = 24; p = 0.005), reactance (t = 2.29, df = 247; p = 0.02), and fatalism (t = 2.86, df = 247; p = 0.005), those who responded at both points in time tended to score lower than participants who only responded at Time 1. The implications of the non-response analysis results will be reviewed in the discussion section.
Instrumentation
A detailed discussion of each measure follows. All variables were measured at Time 1, except for behavior which was measured at Time 2. Means, standard deviations, scale items, and Cronbach’s alphas for all Time 1 variables are presented in Table 1.
Table 1.
Descriptive statistics and scale items for All EPPM constructs from study 1
| Variable | Scale M (SD) | Scale α | Scale Items |
|---|---|---|---|
| Severity | 4.18 (.79) | .92 |
COVID-19 is a severe health issue COVID-19 is a dangerous illness COVID-19 can lead to harmful health problems COVID-19 has serious health consequences |
| Susceptibility | 3.81 (.78) | .83 |
It is possible that I will get the COVID-19 Getting the COVID-19 is something that could happen to me I am at risk of getting the COVID-19 I am susceptible to getting COVID-19 |
| Self-efficacy | 3.14 (.86) | .85 |
I would know how to get the COVID-19 vaccine if I wanted to It would be easy for me to get the COVID-19 vaccine if I wanted to I would be able to get the COVID-19 vaccine if I wanted to It would be simple for me to get the COVID-19 vaccine if I wanted to It would be difficult for me get the COVID-19 vaccine. (Reversed) |
| Response-efficacy | 3.86 (.75) | .89 |
If I get the COVID-19 vaccine, I am less likely to get COVID-19 Getting the COVID-19 vaccine can decrease my chances of getting COVID-19 The COVID-19 vaccine is a safe way to prevent COVID-19 The COVID-19 vaccine protects people from getting COVID-19 |
| Fear | 2.69 (1.17) | .93 |
How do you feel when you think about getting COVID-19? Anxious Scared Fearful |
| Intention | 3.24 (1.16) | .96 |
I plan to get the COVID-19 vaccine in the NEXT 2 months (i.e., during the Spring 2021 semester) I will try to get the COVID-19 vaccine in the NEXT 2 months (i.e., during the Spring 2021 semester) I intend to get the COVID-19 vaccine in the NEXT 2 months (i.e., during the Spring 2021 semester) I am likely to get the COVID-19 vaccine in the NEXT 2 months (i.e., during the Spring 2021 semester) |
| Defensive Avoidance | 2.71 (.78) | .83 |
I try NOT to think about COVID-19 I avoid thinking about COVID-19 If thoughts about COVID-19 come to mind, I try to think about something else |
| Reactance | 2.54 (.81) | .81 |
The media have blown the COVID-19 issue all out of proportion In general, people are overreacting to COVID-19 Most of what I hear about the dangers of COVID-19 is exaggerated |
| Fatalism | 3.22 (.75) | .75 |
No matter what they do, some people are going to catch COVID-19 Some people are going to get COVID-19 no matter what Some people are destined to get COVID-19: There is really nothing you can do about it |
All variable except fear were measured on a five-point scale ranging from (1) “strongly disagree” to (5) “strongly agree.” Fear was measured on a five-point scale ranging from (1) “none of this emotion” to (5) “a great deal of this emotion”
Perceived Threat and Perceived Efficacy
The threat and efficacy measures were adapted from the Witte et al.’s (1996) Risk Behavior Diagnostic Scale (RBDS) and utilized five-point Likert-type items (i.e., “strongly disagree” to “strongly agree”). Specifically, perceived severity, perceived susceptibility, and perceived response efficacy were each measured using four items, and perceived self-efficacy was measured using five items. Existing theory and research suggest that perceived severity and perceived susceptibility interact to produce one’s overall perceived threat, and that perceived response efficacy and perceive self-efficacy interact to produce one’s overall perceived efficacy (e.g., Sheeran et al., 2014; Weinstein, 2000; Witte, 1992). Thus, we operationalized perceived threat (M = 16.08, SD = 4.91) as the product of perceived severity and susceptibility, and perceived efficacy (M = 12.11, SD = 4.21) as the product of perceived self-efficacy and perceived response efficacy.
Fear Fear
was measured using procedures outlined by Witte (1994). Specifically, participants were asked how getting COVID-19 made them feel using the following three items: “fearful,” “scared,” and “anxious.” Response categories for these items ranged from “none of this feeling” to “a great deal of this feeling.”
Danger Control Outcomes
The intention and behavior measures were developed using procedures outlined by Fishbein and Ajzen (2010). Specifically, intention was measured using four five-point Likert-type items ranging from “strongly disagree” to “strongly agree.” Behavior was measured at Time 2 by asking, “How many doses of the COVID-19 vaccine have you received in the past 2 months (i.e., during the Spring 2021 semester)?” The response categories for the behavior item were, “I received zero/no doses of the COVID-19 vaccine in the past 2 months,” “I received one of the two doses of the COVID-19 vaccine in the past 2 months,” and “I received both doses of the COVID-19 vaccine in the past 2 months.” The percentage of participants selecting each response are presented in Table 2.
Table 2.
Descriptive statistics for behavior measure from study 1 and study 2
| Study 1 (N = 157) (%) | Study 2 (N = 567) (%) | |
|---|---|---|
| Zero doses of COVID-19 vaccine | 50.3 | 51.7 |
| One dose of COVID-19 vaccine | 32.5 | 24.9 |
| Two doses of COVID-19 vaccine | 17.2 | 23.5 |
The behavior question asked, “How many doses of the COVID-19 vaccine have you received in the past 2 months (i.e., during the Spring 2021 semester)?”
Fear Control Outcomes
The defensive avoidance, reactance, and fatalism items were adapted from Dillard et al. (2018). These three variables were assessed using five-point Likert items ranging from “strongly disagree” to “strongly agree.”
Linking Questions
The Time 1 and Time 2 responses were linked using a self-generated identification code (Schnell et al., 2010) that was created using the answers to the following questions: (1) “On what day of the month were you born”, (2) “what are the last two numbers of your phone number”, and (3) “what is the last digit of your student ID?” In the few cases where identical codes were generated for multiple participants, responses to questions regarding gender, age, ethnicity, and citizenship were used to match participants’ responses.
Data analytic plan
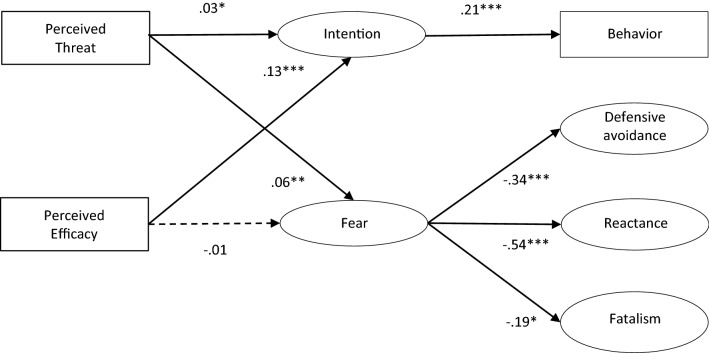
Structural equation modeling (SEM) was used to assess the data fit to the proposed theoretical model using the “lavaan” package (Rosseel, 2012) in R (RStudio Team, 2020). We followed a two-step procedure by first specifying the measurement models through confirmatory factor analysis and then completing the estimation of structural models (Kline, 2016). Full Information Maximum Likelihood (FIML) was used to address missing data (Enders, 2010). The following fit indices were used to evaluate model fit: the χ2/df ratio, the comparative fit indices (CFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). An acceptably fit model must meet the following criteria: the χ2/df ratio ≤ 5, CFI ≥ 0.90, RMSEA ≤ 0.08, and SRMR ≤ 0.08 (Hu & Bentler, 1999; Kline, 2016). Fit indices of the measurement models and final structural models are reported in Fig. 2.
Fig. 2.
Results for structural model for study 1. Solid lines indicate significant paths (*p < .05, **p < .01, ***p < .001). Dashed line indicates insignificant path
Results
The confirmatory factor analysis showed that the measurement model fit the data well (χ2/df = 1.54, CFI = 0.97, RMSEA = 0.06, SRMR = 0.06). The final structural model also demonstrated an acceptable fit to the data (χ2/df = 1.96, CFI = 0.94, RMSEA = 0.08, SRMR = 0.13). Path coefficients of the structural model are reported in Fig. 2. Overall, the EPPM constructs explained 11% of the variance in intention, 49% of the variance in behavior, 10% of the variance in defensive avoidance, 35% of the variance in reactance, and 27% of variance in fatalism.
Hypotheses and research questions
Hypothesis 1 proposed that (A) perceived threat and (B) perceived efficacy would positively predict intentions to get the COVID-19 vaccine. As expected, perceived threat (β = 0.03, p < 0.05) and perceived efficacy (β = 0.13, p < 0.001) significantly and positively predicted intention to get the COVID-19 vaccine. Hypothesis 2 proposed that the intention to get the COVID-19 vaccine would positively predict COVID-19 vaccine behavior. As expected, intention (β = 0.21, p < 0.001) significantly and positively predicted COVID-19 vaccine behavior at Time 2. Thus, the data were consistent with the danger control portion of the EPPM.
Hypothesis 3 proposed that perceived threat would positively predict fear. Results show that participants’ perceived threat (β = 0.06, p < 0.01) significantly and positively predicted their fear. Research question 1 asked about the relation between perceived efficacy and fear. We found that perceived efficacy (β = − 0.01, p = 0.490) was not associated with fear. Further, we also asked research questions 2 about the relation between fear and defensive reactions [i.e., (A) defensive avoidance, (B) reactance, or (C) fatalism]. Our results show that fear significantly and negatively predicted (A) defensive avoidance (β = − 0.34, p < 0.001), (B) reactance (β = − 0.54, p < 0.001), and (C) fatalism (β = − 0.19, p < 0.05). Therefore, the data were inconsistent with EPPM predictions, but consistent with other research in this area.
Study 2
Method
Procedures and participants
The data for Study 2 were collected using Qualtrics Survey Software. Participants were recruited from a total of six undergraduate communication classes at Arizona State University. They received a small amount of extra credit or a $5 gift card for completing this survey. All procedures were approved by the sponsoring university’s institutional review board.
Data collection for Study 2 took place at the same time as the Time 2 data collection for Study 1 (i.e., in late April 2021). The final sample for Study 2 included 567 individuals, including the 157 individuals from the Study 1, plus an additional 410 individuals that participated in other research project.1 These participants were 48.8% male, 50.7% female, and 0.5% other, with a mean age of 19.34 (SD = 2.14). The sample was 63% white, 22% Asian, 5.9% black or African American, and 9.1% other. Finally, 23.5% of the sample identified as Hispanic or Latino/a, and 80.7% of participants were U.S. citizens. As a reminder, this sample was used to answer our research question regarding the key reasons for COVID-19 vaccine hesitancy among college students who did not plan to get the COVID-19 vaccine in the future.
Instrumentation
Behavior Behavior
was measured using the same item from Study 1. As a reminder, this question asked, “How many doses of the COVID-19 vaccine have you received in the past 2 months (i.e., during the Spring 2021 semester)?” The response categories for this behavior item were, “I received zero/no doses of the COVID-19 vaccine in the past 2 months,” “I received one of the two doses of the COVID-19 vaccine in the past 2 months,” and “I received both doses of the COVID-19 vaccine in the past 2 months.” The percentage of participants selecting each response is presented in Table 2.
Intention
In addition, for Study 2, participants who reported receiving zero doses of the COVID-19 vaccine in the past two months were asked a follow-up question about their intention to do so in the future (i.e., “You indicate that you received zero/no doses of the COVID-19 vaccine in the past 2 months. Which of the following best describes your plans to get the COVID-19 vaccine in the future?”). The response categories for this item were, “I plan to get the COVID-19 vaccine in the future, and I have already set up an appointment to do so,” “I plan to get the COVID-19 vaccine in the future, but I have not set up and appointment to do so,” and “I do not plan to get the COVID-19 vaccine in the future.”
Vaccine hesitancy
Finally, those indicating that they both had not received the COVID-19 vaccine and did not plan to get the COVID-19 vaccine in the future were asked a follow-up question regarding why, followed by a list of eight EPPM-related reasons (along with an open-ended “other” option) and asked to check all that apply. The full list of response options is presented in Table 3.
Table 3.
EPPM related reasons for COVID-19 vaccine hesitancy among college students from study 2
| Reason | N (%) |
|---|---|
| I do not think I am likely to get COVID-19 | 31 (28.9%) |
| I do not think the people I care about are likely to get COVID-19 | 9 (8.4%) |
| I do not think COVID-19 is a serious health issue | 31 (29.0%) |
| I have concerns about the safety of the COVID-19 vaccine | 81 (75.7%) |
| I have concerns about the effectiveness of the COVID-19 vaccine | 57 (53.3%) |
| I do not have the time to get the COVID-19 vaccine | 9 (8.4%) |
| I do not have the ability to pay for the COVID-19 vaccine | 5 (4.7%) |
| I oppose vaccinations in general | 16 (15.0%) |
Results
Of the 293 participants who reported receiving zero doses of the COVID-19 vaccine in the past two months, 6.2% (n = 18) had already set up an appointment to get the COVIID-19 vaccine, 57.2% (n = 167) planned to get the COVID-19 vaccine in the future, and 36.6% (n = 107) did not plan to get the COVID-19 vaccine in the future.
Research question three asked, what are the key reasons for COVID-19 vaccine hesitancy among college students who do not plan to get the COVID-19 vaccine in the future? This question was answered using the 107 participants from Study 2 who had not yet received the COVID-19 vaccine and did not plan to get the COVID-19 vaccine in the future. Results are presented in Table 3. A glance at this table reveals that the most selected reasons for vaccine hesitancy were related to response efficacy (i.e., participants expressed concerns about the safety and the effectiveness of the COVID-19 vaccine). A smaller but still substantial number of participants reported being hesitant because they did not think COVID-19 was a serious health issue (i.e., low severity) or because they did not think they were likely to get COVID-19 (low susceptibility). Notably, self-efficacy appeared to play a relatively minor role in vaccine hesitancy (i.e., very few individuals reported not having the time to get or ability to pay for the COVID-19 vaccine).
Of the 18 (3.2%) individuals that selected “other” option, only two provided reasons that were not easily coded into one of the eight categories included in Table 3. These reasons include (1) “I am terrified of needles,” and (2) “my mom forbid me.” Of the other 18 reasons (i.e. a few participants provided multiple reasons), eight focused on susceptibility to self (e.g., “I had COVID-19 in August 2020 and tested positive for antibodies so I do not think I need the vaccine”), two focused on susceptibility to others (e.g., “everyone around me that is at risk is getting the vaccine so there I no reason for me to get it”), and eight focused on the safety of the vaccine (e.g., “the serious side effects and short introduction period to the vaccine are particularly concerning”). Thus, these responses were included in their respective categories when calculating numbers and percentages included in Table 3 (unless the relevant closed-ended option was already selected by the participant making the comment).
Discussion
One goal of this study was to assess the EPPM’s ability to predict and explain college students protective and defensive reactions to the COVID-19 vaccine. Results from Study 1 indicate the EPPM was consistent with the data and explained substantial amounts of variance in danger control (i.e., intention and behavior). For fear control (i.e., defensive avoidance, reactance, and fatalism) processes, however, the data were largely inconsistent with EPPM. Another goal of this study was to identify EPPM-related reasons for COVID-19 vaccine hesitancy among college students. By far the most common reasons related to response-efficacy (i.e., hesitant college students were concerned about the safety and effectiveness of the COVID-19 vaccine). A discussion of the theoretical and practical implications of these findings follows.
Theoretical implications
Results were consistent with the EPPM’s predictions regarding danger control. More specifically, perceived threat and perceived efficacy predicted intention, and intention predicted behavior. In short, our results support the notion that high-threat/high-efficacy messages should be an effective way to change college students’ COVID-19 vaccine behavior. We will return to this idea in the practical application section that follows.
Results were largely inconsistent with the EPPM’s predictions regarding fear control. More specifically, the EPPM predicts that (1) threat should positively predict fear, (2) efficacy should negatively predict fear, and (3) fear should positively predict fear control. However, our results indicate that while (1) threat did positively predict fear, (2) efficacy was unrelated to fear, and (3) fear was negatively related to fear control. Notably, these results are consistent with the growing body of literature suggesting that fear is negatively related to numerous fear control processes, (e.g., Roberto et al., 2021; Birmingham et al., 2015; De Meulner et al., 2015; Popova, 2012; Yang & Kahlor, 2012). The reasons for these discrepancies between theory and research remain unclear but indicate that fear control portion of the EPPM needs to be more clearly explicated and perhaps respecified.
Finally, a growing body of literature suggests that threat to others (instead of or in addition to threat to self) can impact intentions and behavior (see Roberto et al., 2009 for a review). To illustrate, Roberto and Goodall (2009) found that perceived threat to patients was associated with primary care physicians’ intention and behavior to test their patients’ level of kidney functioning. Goei et al. (2010) report that threat-to-other messages significantly increased school workers intentions to engage in a variety of behaviors meant to help manage asthma in their students. Chen and Chen (2021) report that other-oriented threat messages significantly increased Chinese smokers’ cessation intentions. In Study 2, 8.4% of COVID-19 vaccine hesitant college students reported low threat to others (i.e., I do not think the people I care about are likely to get COVID-19) as one of the reasons for vaccine hesitancy. Unfortunately, the full extent of the role of threat to others plays in COVID-19 vaccine decisions remains unknown as it was assessed using one check-all-that-apply follow-up item in this study (and only college students who indicated they did not plan to get the COVID-19 vaccine received this item). Thus, this remains a ripe are for additional research, especially in the context of infectious health risks, and we recommend that future studies use full scales to measure both threat to self and threat to other (sample threat-to-other scales are reported in Roberto & Goodall, 2009 and Goei et al., 2010).
Practical implications
Our results indicate that college student’s perceived severity, susceptibility, self-efficacy, and response efficacy hovered around 3–4 on a 5-point scale. On the one hand, these results are encouraging because they suggest that college students tend to view COVID-19 as moderately threatening and the COVID-19 vaccine as moderately efficacious. On the other hand, these results also suggest that there is still room for improvement and that messages targeting perceived threat and especially perceived efficacy could yield meaningful reductions in vaccine hesitancy among college students.
On a related note, it is encouraging that even though the vaccine had been available for only a short time, nearly one-half of participants received one or two doses of the COVID-19 vaccine by the time data collection took place in late April 2021. It is also encouraging that nearly one-third of participants planned to get the vaccine in the future. Concerning is the fact that nearly one-fifth of participants had not yet received the COVID-19 vaccine and did not plan to get vaccinated in the future. The research question focused on the reasons COVID-19 vaccine hesitancy among this latter group. By far the two leading reasons related to response-efficacy. That is, three-quarters of participants who were not planning to get vaccinated expressed concerns about the safety of the COVID-19 vaccine, and over one-half of those who were not planning to get vaccinated expressed concerns about the effectiveness of the COVID-19 vaccine. This suggest that response efficacy should be a prime target for those wishing to convert the vaccine hesitant. A distant third and fourth reasons concerned perceived severity and susceptibility. This suggests that continuing to include these elements in COVID-19 vaccine messaging will also be worthwhile.
Finally, regarding the number and types of defensive reactions college students experience with respect to COVID-19 and the COVID-19 vaccine, results indicate that they experienced all three defensive reactions under investigation to some extent. Further, fatalism appears to be employed more often than either defensive avoidance or reactance.2 This suggests that message creators must consider ways to overcome various defensive reactions, especially fatalism. As a reminder, defensive avoidance involves conscious efforts to refrain from thinking about an issue, reactance involves criticizing the message or the source of a message, and fatalism involves accepting or believing that little can be done to prevent a risk (Dillard et al., 2018). Thus, COVID-19 prevention messages should also include components that minimize colleges students’ motivation and ability to engage in such defensive reactions. This might be done by making sure the message (1) is difficult to avoid or forget, (2) is delivered by sources that college students find credible, and (3) stresses how taking simple steps such as social distancing, wearing masks, and getting the COVID-19 vaccine can meaningfully reduce the risk to both an individual and those around them.
Strengths and limitations
The key strengths of this study include (1) being guided by a well-respected theory—the EPPM, (2) assessing both danger control and fear control outcomes, (3) employing a longitudinal research design that included future behavior, (4) using well-established measures that yielded reliability estimates in the very good to excellent range, and (5) providing practically important insights regarding some of the key factors that influence college student’s COVID-19 vaccination intention and behavior. As is the case for any investigation, some limitations must also be noted.
The first potential limitation is attrition. Two-hundred and fifty participants responded at Time 1, of which 157 (62.8%) also responded at Time 2. Fortunately, we anticipated this might happen (i.e., attrition is common in longitudinal research), and made sure to start with a sample that was large enough to lead to a dataset from which meaningful conclusions could still be drawn (Schreiber et al., 2006). Further, this response rate is similar to or better than other longitudinal studies conducted with college student samples during and about the COVID-19 pandemic (e.g., Roberto et al., 2021; Fruehwirth et al., 2021; Ryerson et al., 2021; Zimmermann et al., 2021). Unfortunately, the non-response analyses indicate that there were some differences between those who did and did not respond to the Time 2 survey (i.e., those who dropped out of the study reported lower perceived severity, response efficacy, and fear, and greater defensive avoidance, reactance, and fatalism). Thus, some of these results might be interpreted with caution as some of these constructs may be higher or lower for college students in general.
The second potential limitation involves the use of a convenience sample of college students, which potentially limiting their generalizability to other populations. However, Yang (2012) notes that infectious diseases such as COVID-19 have a greater potential to spread in the high-density living environment on college campuses. Indeed, at the time this article was written in early-September 2021, there were already over 700,000 coronavirus cases at colleges and universities across the U.S., and a large number of universities that began with in-person classes have since moved remote learning (The New York Times, 2021). Further, our results offer meaningful insights for those wishing to influence individuals in this context. That said, this line of inquiry will clearly benefit from future research with nonstudent participants.
A third limitation is that it focused on four individual factors believed to impact intention and behavior (i.e., severity, susceptibility, self-efficacy, and response-efficacy). It does not address how relationship, community, and societal factors also influence behavior. Ecological models, on the other hand, view behavior as part of a larger system and explore how individual, relationship, community, and societal factors interact to produce behavior (Green & Kreuter, 2005). Thus, future research might look at role norms, employer and business mandates, and local, state, and national laws and guidelines play in encouraging or discouraging COVID-19 vaccination behavior.
A fourth limitation is the measurement of fatalism. We adapted items from Dillard et al. (2018) to measure fatalism. These items include “No matter what they do, some people are going to catch COVID-19,” “Some people are going to get COVID-19 no matter what,” and “Some people are destined to get COVID-19: There is really nothing you can do about it.” All three items focus on risk perception for other people, rather than for oneself. In other words, the way we measured fatalism represented an individual’s general belief that “some people” will get COVID-19 no matter what they do, but it is unclear whether or not an individual would consider him or herself included in “some people.” Even though fatalism has acceptable reliability (0.75) and all three items load to one factor in our study, the belief that “some people will get COVID-19 but not myself” is different from the belief that “some people will get COVID-19 including myself,” and may lead to different risk management behaviors. Future research should explore the notion of fatalism by specifying how such belief is related to oneself and how it is related to other EPPM variables.
Conclusion
In conclusion, this paper examined the EPPM’s ability to predict and explain both danger control and fear control outcomes regarding COVID-19 and the COVID-19 vaccine. Results were consistent with expectations for all danger control predictions, but inconsistent with expectations for most fear control predictions. In tandem, these results suggest there may be few downsides to using high-threat/high-efficacy messages to persuade colleges students to get the COVID-19 vaccine. These results also highlight the importance of additional research focusing on the fear control portion of the EPPM.
Author's contribution
AJR was primarily responsible for study design, data collection, writing the theory, method, and discussion sections, and also contributed to data analysis and writing the results section. XZ was primarily responsible for data analysis, writing the results section, and also contributed to the study design and writing the theory, method, and discussion sections.
Funding
None.
Data availability
Data and materials are available upon request.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were approved by the sponsoring university’s institutional review board (STUDY00013143).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
We conducted two different longitudinal studies using two different samples during the Spring 2021 semester: (1) the EPPM study reported here – conducted in early February 2021 and late April 2021, and (2) one on information seeking regarding the COVID-19 vaccine – conducted in January 2021 and late April 2021. Though each study had a different sample and a different focus, they both included the same measure of vaccine behavior and vaccine hesitancy at Time 2. The vaccine hesitancy results are reported in only this manuscript.
Post-hoc analyses indicate that our convenience sample of college students was more likely to use fatalism than either defensive avoidance, t (157) = 5.65, p < .001, or reactance, t (157) = 7.30, p < .001, and that defensive avoidance and reactance tended to be used equally, t (157) = 1.49, p < .14 (i.e., fatalism > defensive avoidance = reactance).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Birmingham WC, Hung M, Boonyasiriwat W, Kohlmann W, Walters ST, Burt RW, Stroup AM, Edwards SL, Schwartz MD, Lowery JT, Hill DA, Wiggins CL, Higginbotham JC, Tang P, Hon SD, Franklin JD, Vernon S, Kinney AY. Effectiveness of the extended parallel process model in promoting colorectal cancer screening. Psycho-Oncology. 2015;24:1265–1278. doi: 10.1002/pon.3899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boster FJ, Mongeau P. Fear-arousing persuasive messages. In: Bostrom RN, editor. Communication yearbook 8. Sage; 1984. pp. 330–375. [Google Scholar]
- Chen M, Chen L. Promoting smoking cessation in China: Using an expansion of the EPPM with other-oriented threat. Journal of Health Communication. 2021;26:174–183. doi: 10.1080/10810730.2021.1906360. [DOI] [PubMed] [Google Scholar]
- De Meulenaer S, De Pelsmacker P, Dens N. Have no fear: How individuals differing in uncertainty avoidance, anxiety, and chance belief process health risk messages. Journal of Advertising. 2015;44:114–125. doi: 10.1080/00913367.2015.1018465. [DOI] [Google Scholar]
- Diesel J, Sterrett N, Dasgupta S, Kriss JL, Barry V, Esschert KV, Whitement A, Cadwell BL, Weller D, Qualters JR, Harris L, Bhatt A, Williams C, Fox LM, Delman DM, Black CL, Barbour KE. COVID-19 vaccination coverage among adults—United States, December 14, 2020–May 22, 2021. Morbidity and Mortality Weekly Report. 2021;70(25):922–927. doi: 10.15585/mmwr.mm7025e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillard JP, Li R, Meczkowski E, Yang C, Shen Li. Fear responses to threat appeals: Functional form, methodological considerations, and correspondence between static and dynamic data. Communication Research. 2017;44(7):997–1018. doi: 10.1177/0093650216631097. [DOI] [Google Scholar]
- Dillard JP, Meczkowski E, Yang C. Defensive reactions to threatening health messages: Alternative structures and next questions. International Journal of Communication. 2018;12:973–995. [Google Scholar]
- Enders CK. Applied missing data analysis. Guilford Press; 2010. [Google Scholar]
- Fruehwirth JC, Biswas S, Perreira KM. The Covid-19 pandemic and mental health of first-year college students: Examining the effect of Covid-19 stressors using longitudinal data. PLoS ONE. 2021;16:e0247999. doi: 10.1371/journal.pone.0247999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goei R, Boyson AR, Lyon-Callo SK, Schott C, Wasilevich E, Cannarile S. An examination of EPPM predictions when threat is perceived externally: An asthma intervention with school workers. Health Communication. 2010;25:333–344. doi: 10.1080/10410231003775164. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- McEachan R, Taylor N, Harrison R, Lawton R, Gardner P, Conner M. Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Annals of Behavioral Medicine. 2016;50(4):592–612. doi: 10.1007/s12160-016-9798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meczkowski EJ, Dillard JP, Shen L. Threat appeals and persuasion: Seeking and finding the elusive curvilinear effect. Communication Monographs. 2016;83(3):373–395. doi: 10.1080/03637751.2016.1158412. [DOI] [Google Scholar]
- Mongeau PA. Another look at fear-arousing persuasive appeals. In: Allen M, Preiss RW, editors. Persuasion: Advances through meta-analysis. Hampton Press; 1998. pp. 53–68. [Google Scholar]
- Popova L. The extended parallel process model: Illuminating the gaps in research. Health Education and Behavior. 2012;39:455–473. doi: 10.1177/1090198111418108. [DOI] [PubMed] [Google Scholar]
- Rich A, Brandes K, Mullan B, Hagger MS. Theory of planned behavior and adherence in chronic illness: A meta-analysis. Journal of Behavioral Medicine. 2015;38:673–688. doi: 10.1007/s10865-015-9644-3. [DOI] [PubMed] [Google Scholar]
- Roberto AJ, Goodall CE. Using the extended parallel process model to explain physicians’ decisions to test their patients for kidney disease. Journal of Health Communication. 2009;14:400–412. doi: 10.1080/10810730902873935. [DOI] [PubMed] [Google Scholar]
- Roberto AJ, Goodall CE, Witte K. Raising the alarm and calming fears: Perceived threat and efficacy during risk and crisis. In: Heath R, O’Hair D, editors. Handbook of risk and crisis communication. Routledge; 2009. pp. 287–303. [Google Scholar]
- Roberto AJ, Zhou X, Lu AH. The effects of perceived threat and efficacy on college students’ social distancing behavior during the COVID-19 pandemic. Journal of Health Communication. 2021;26:264–271. doi: 10.1080/10810730.2021.1903628. [DOI] [PubMed] [Google Scholar]
- Rosseel Y. Lavaan: An R package for structural equation modeling and more. Version 0.5-12 (BETA) Journal of Statistical Software. 2012;48:1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- Ryerson NC, Wilson OW, Pena A, Duffy M, Bopp M. What happens when the party moves home? The effect of the COVID-19 pandemic on US college student alcohol consumption as a function of legal drinking status using longitudinal data. Translational Behavioral Medicine. 2021;11:772–774. doi: 10.1093/tbm/ibab006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnell R, Bachteler T, Reiher J. Improving the use of self-generated identification codes. Evaluation Review. 2010;34:391–418. doi: 10.1177/0193841X10387576. [DOI] [PubMed] [Google Scholar]
- Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research. 2006;99:323–338. doi: 10.3200/JOER.99.6.323-338. [DOI] [Google Scholar]
- Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychological Bulletin. 2014;140:511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- SteelFisher GK, Blendon RJ, Caporello H. An uncertain public—encouraging acceptance of Covid-19 vaccines. The New England Journal of Medicine. 2021;384:1483–1487. doi: 10.1056/NEJMp2100351. [DOI] [PubMed] [Google Scholar]
- Tannenbaum MB, Hepler J, Zimmerman RS, Saul L, Jacobs S, Wilson K, Albarracín D. Appealing to fear: A meta-analysis of fear appeal effectiveness and theories. Psychological Bulletin. 2015;141:1178–1204. doi: 10.1037/a0039729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND. Perceived probability, perceived severity, and health-protective behavior. Health Psychology. 2000;19:65–74. doi: 10.1037/0278-6133.19.1.65. [DOI] [PubMed] [Google Scholar]
- Witte K. Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs. 1992;59:329–349. doi: 10.1080/03637759209376276. [DOI] [Google Scholar]
- Witte K. Fear control and danger control: A test of the extended parallel process model (EPPM) Communications Monographs. 1994;61:113–134. doi: 10.1080/03637759409376328. [DOI] [Google Scholar]
- Witte K, Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior. 2000;27(5):591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- Witte K, Cameron KA, McKeon JK, Berkowitz JM. Predicting risk behaviors: Development and validation of a diagnostic scale. Journal of Health Communication. 1996;1:317–341. doi: 10.1080/108107396127988. [DOI] [PubMed] [Google Scholar]
- Yang ZJ. Too scared or too capable? Why do college students stay away from the H1N1 vaccine? Risk Analysis: An International Journal. 2012;32:1703–1716. doi: 10.1111/j.1539-6924.2012.01799.x. [DOI] [PubMed] [Google Scholar]
- Yang ZJ, Kahlor L. What, me worry? The role of affect in information seeking and avoidance. Science Communication. 2012;35:189–212. doi: 10.1177/1075547012441873. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2021). Delta variant: What we know about the science. https://www.cdc.gov/coronavirus/2019-ncov/variants/delta-variant.html.
- Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach. Psychology Press.
- Green, L. W., & Kreuter, M. W. (2005). Health promotion planning: An educational and ecological approach (4th ed.). McGraw-Hill.
- Innes, S., & Steinbach, A. (2021). State-operated vaccine cites open for Arizonans 16 and older. The Arizona Republic.https://www.azcentral.com/story/news/local/arizona-health/2021/03/22/arizona-opening-up-state-operated-sites-coronavirus-vaccines-16-and-older/4802159001/.
- Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). Guilford Press.
- Mathieu, E., Ritchie, H., Ortiz-Ospina, E. Roser, M., Hasell, J., Appel, C., Giattino, C., & Rodes-Guirao, L. (2021). A global database of COVID-19 vaccinations. Nature Human Behavior, 5, 947–953. [DOI] [PubMed]
- National Foundation for Infectious Diseases. (2016). Addressing the challenges of influenza vaccination on U.S. college campuses. https://www.nfid.org/wp-content/uploads/2019/08/college-flu-summit-report-2.pdf.
- National Foundation for Infectious Diseases. (2017). National survey on college students and flu. http://www.nfid.org/idinfo/influenza/college-students-flu-survey.html.
- RStudio Team. (2020). RStudio: Integrated development environment for R. RStudio, PBC. http://www.rstudio.com/.
- The New York Times. (2021), Tracking coronavirus cases at U.S. colleges and universities. https://www.nytimes.com/interactive/2020/us/covid-college-cases-tracker.html.
- Thomason, A., & O’Leary, B. (2021). Here’s a list of colleges that require students or employees to be vaccinated against Covid-19. The Chronicle of Higher Education. https://www.chronicle.com/blogs/live-coronavirus-updates/heres-a-list-of-colleges-that-will-require-students-to-be-vaccinated-against-covid-19.
- U.S. Food and Drug Administration. (2021). Pfizer-BioNTech COVID-19 vaccine. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine#additional.
- Zimmermann, M., Bledsoe, C., & Papa, A. (2021). The impact of the COVID-19 pandemic on college student mental health: A longitudinal examination of risk and protective factors. https://psyarxiv.com/2y7hu. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials are available upon request.