Abstract
The evidence regarding the intake of dietary folate, vitamin B6, and vitamin B12 in relation to mortality in the general population is limited. This study aimed to examine the relationship between dietary intakes of folate, vitamin B6, and vitamin B12 in relation to all-cause and cause-specific mortality in a large U.S. cohort. This study included a total of 55,569 adults from the Third National Health and Nutrition Examination Survey (NHANES III) and NHANES 1999–2014. Vital data were determined by linking with the National Death Index records through 31 December 2015. Cox proportional hazards models were used to investigate the relationships of all-cause and cause-specific mortality with dietary folate, vitamin B6, and vitamin B12 intake. Dietary intakes of folate and vitamin B6 were inversely associated with mortality from all-cause, cardiovascular disease, and cancer for men and with mortality from all-cause and cardiovascular disease for women. In men, the multivariable hazard ratios (95% confidence intervals) for the highest versus lowest quintiles of folate and vitamin B6 were 0.77 (0.71–0.85) and 0.79 (0.71–0.86) for all-cause mortality, 0.59 (0.48–0.72) and 0.69 (0.56–0.85) for CVD mortality, and 0.68 (0.56–0.84) and 0.73 (0.60–0.90) for cancer mortality, respectively. Among women, the multivariable hazard ratios (95% confidence intervals) for the highest versus lowest quintiles of folate and vitamin B6 were 0.86 (0.78–0.95) and 0.88 (0.80–0.97) for all-cause mortality and 0.53 (0.41–0.69) and 0.56 (0.44–0.73) for CVD mortality, respectively. No significant associations between dietary vitamin B12 and all-cause and cause-specific mortality were observed. In conclusion, higher dietary intakes of folate and vitamin B6 were significantly associated with lower all-cause and cardiovascular mortality. Our findings suggest that increasing the intake of folate and vitamin B6 may lower the mortality risk among U.S. adults.
Keywords: diet, folate, vitamin B6, vitamin B12, mortality
1. Introduction
Folate, vitamin B6, and vitamin B12 are essential B vitamin nutrients which play important roles in the degradation of homocysteine (Hcy) by acting as prerequisite substrate donors or as necessary coenzymes [1,2]. In addition, these B vitamins are important components of one-carbon metabolism, which contributes to DNA synthesis and DNA methylation, the synthesis of blood cells, and nerve function. The lack of these B vitamins is one of the key contributors to high blood homocysteine levels [3], DNA repair disruption [4], and gene expression [5].
Several epidemiologic studies have investigated the relationship between dietary folate, vitamin B6, or vitamin B12 intake and mortality risk. However, most of these studies were conducted among specific populations (e.g., older adults and participants with cancers), and limited information is available for general populations. In addition, the results were inconsistent. For example, Persson et al. [6] reported inverse associations between dietary folate and the risk of all-cause and liver-disease mortality in the American Association of Retired Persons Diet and Health Study. Li et al. observed an inverse association between dietary folate intake and all-cause mortality among patients with breast cancer [7]. Medrano et al. observed that a higher dietary intake of folate or vitamin B12 was associated with lower coronary mortality, but vitamin B6 intake was not associated with cardiovascular-disease (CVD) mortality in the Spanish population [8]. Cui et al. [9] observed in the Japan Collaborative Cohort Study that dietary folate and vitamin B6 intakes were inversely associated with mortality from stroke, coronary heart disease, and heart failure, while dietary vitamin B12 intake was positively associated with mortality from stroke in men. In contrast, Xu et al. [10] reported that dietary folate, vitamin B6, and vitamin B12 were neither associated with all-cause mortality nor cancer–specific mortality in participants with cancer. Non-significant relationships between folate supplementation and all-cause or CVD mortality were observed in a recent meta-analysis of randomized clinical trials (RCTs) [11], and even some RCTs demonstrated that folate or vitamin B12 supplementation was associated with higher all-cause mortality [12,13,14]. Large-scale cohort studies are thus needed to provide robust results and precise estimates in general populations. Therefore, utilizing the data from a nationally representative sample of the National Health and Nutrition Examination Survey (NHANES), we investigated whether dietary intakes of folate, vitamin B6, and vitamin B12 were in relation to the risk of all-cause and cause-specific mortality in the general U.S. adult population.
2. Materials and Methods
2.1. Study Population
The NHANES is a nationally representative survey conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention (CDC). Information on the methods of sampling and data collection has been described previously [15]. In brief, the NHANES adopted a complex, stratified, multistage probability sampling method to select a representative population in the U.S. Information on lifestyle factors and health and nutritional status was collected for each participant. The design and procedures of the NHANES survey have been described in detail elsewhere [16].
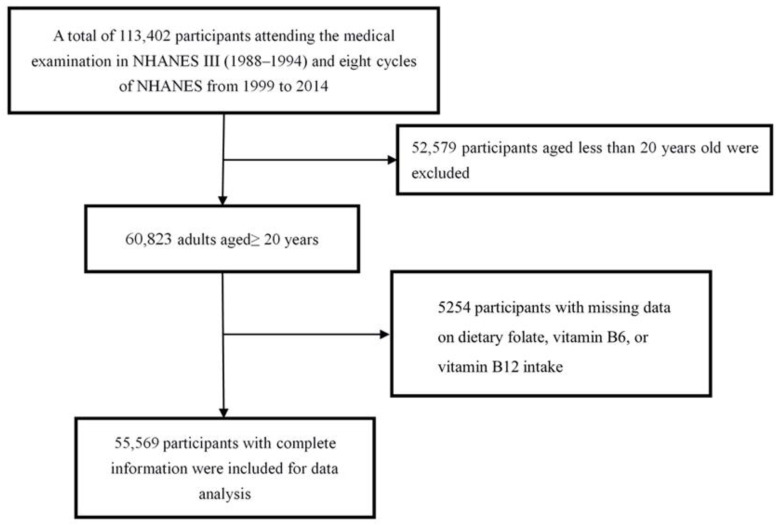
In the current study, we used data from NHANES III (1988–1994) and eight cycles of the NHANES from 1999 and 2014. Adult participants aged ≥ 20 years were included in the analysis. Figure 1 shows the procedure of participant selection. Briefly, 113,402 U.S residents attending the medical examination in the NHANES from 1988 to 2014 were initially included in this study. Among them, 52,579 participants were excluded due to them being younger than 20 years old, and 5254 participants with missing information on dietary folate, vitamin B6, or vitamin B12 intake were further excluded. Finally, 55,569 adults were included in the main analysis.
Figure 1.
Flowchart of participant selection.
2.2. Measurement of Dietary Folate, Vitamin B6, and Vitamin B12 Intake
The data on dietary folate, vitamin B6, and vitamin B12 intake from food were assessed using a 24 h diet recall conducted by trained interviewers. In NHANES III and the 1999–2002 survey cycles, one diet recall was collected from each person in the Mobile Examination Center (MEC). Since 2003, two dietary reviews were conducted. The first one was collected in the MEC, and the second collection was conducted by telephone after 3–10 days. The intakes of folate, vitamin B6, and vitamin B12 from food were evaluated using the United States Department of Agriculture (USDA) Food and Nutrient Database for Dietary Studies (FNDDS), versions 1.0–5.0, which provided the content of these vitamins in each food [17].
2.3. Ascertainment of Mortality
The NCHS has linked the NHANES survey data with all-cause and cause-specific mortality from the National Death Index (NDI). The restricted-use Linked Mortality File (LMF) has been updated with mortality follow-up data through 31 December 2015, which was also publicly available. The disease-specific death was determined by the 10th revision of the International Classification of Disease (ICD-10). The outcomes in this study were all-cause, cardiovascular, and cancer mortality. Cardiovascular mortality was defined as the ICD-10 codes of I00–I09, I11, I13, I20–I51, or I60–I69, and cancer mortality was defined as the ICD-10 codes of C00–C97. The time-to-event for each individual was calculated from the date of recruitment to the date of death or the censor date (31 December 2015), whichever came earlier.
2.4. Covariates
We used the information on age, sex (men or women), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, and other race—including multi-racial), smoking (never, former, or current), alcohol drinking (nondrinker, low-to-moderate drinker, or heavy drinker), the ratio of family income to poverty (≤1, 1–3, or >3), leisure time physical activity (defined as the product of metabolic equivalent value (MET)), and self-reported physician diagnosed cardiovascular disease (yes or no), hypertension (yes or no), type 2 diabetes (yes or no), and Body mass index (BMI) as the covariates.
2.5. Statistical Analysis
We used numbers (percentages) to depict the categorical variables and means (standard deviations) to describe the continuous variables. Multiple imputation was used to impute these covariates with missing values [18].
The Cox proportional hazards model was adopted to evaluate the relationships of dietary folate, vitamin B6, and vitamin B12 with all-cause and cause-specific mortality. The dietary nutrients (i.e., dietary folate, vitamin B6, and vitamin B12) were categorized into quartiles, and the first quartile was selected as the reference group. Two models were introduced: the Crude Model, which was not adjusted, and the Multivariable Model, which was adjusted for age, race/ethnicity, BMI, family income–poverty ratio, smoking status, drinking status, leisure-time physical activity, total energy intake, diabetes, hypertension, and cardiovascular disease.
Stratified analyses were conducted to evaluate the potential effect modification by age (<65 or ≥65 y), smoking status (yes or no), drinking status (yes or no), and BMI (<30 or ≥30 kg/m2). We examined each potential modifier separately by adding a multiplicative interaction term (i.e., continuous dietary nutrients intake parameters* potential modifier).
In order to examine the robustness of the relationships, we also conducted three sensitivity analyses: (1) restricting the analysis to participants free of cardiovascular disease at baseline; (2) excluding participants who died within the first 2 years of follow-up; (3) further adjusting the folate supplement.
All statistical analyses were conducted using R 4.0.2. (R Core Team, Vienna, Austria), and two-sided p values < 0.05 were considered statistically significant.
3. Results
3.1. General Characteristics
The general characteristics of the participants and the cases of all-cause death are presented in Table 1. A total of 55,569 participants with a mean age of 49.0 (SD: 18.6) years at baseline were included. During a median follow-up of 9.8 (interquartile range (IQR): 5.3–15.8) years, a total of 11,535 participants died, including 2411 deaths due to cardiovascular disease and 2482 deaths due to cancer. In comparison to the survivors, the dead participants were more likely to be older, female, and non-Hispanic white; more likely to have diabetes, hypertension, and cardiovascular disease; less likely to be current smokers; and had a lower family income and less leisure-time physical activity.
Table 1.
Baseline characteristics of the study population.
| Variables | Total Sample n = 55,569 |
Survivors n = 44,034 |
Death n = 11,535 |
|---|---|---|---|
| Age, year | 49.0 (18.6) | 44.4 (16.5) | 66.4 (15.7) |
| Sex | |||
| Female | 26,566 (47.81%) | 20,343 (46.2%) | 6223 (53.95%) |
| Male | 29,003 (52.19%) | 23,691 (53.8%) | 5312 (46.05%) |
| Race | |||
| Hispanic | 14,402 (25.92%) | 12,011 (27.28%) | 2391 (20.73%) |
| Non-Hispanic white | 25,249 (45.44%) | 18,973 (43.09%) | 6276 (54.41%) |
| Non-Hispanic black | 12,658 (22.78%) | 10,090 (22.91%) | 2568 (22.26%) |
| Other race—including multi-racial | 3260 (5.87%) | 2960 (6.72%) | 300 (2.6%) |
| Drinking | |||
| Never | 14,732 (26.51%) | 10,410 (23.64%) | 4322 (37.47%) |
| Low to moderate | 11,607 (20.89%) | 8984 (20.4%) | 2623 (22.74%) |
| Heavy | 29,230 (52.60%) | 24,640 (55.96%) | 4590 (39.79%) |
| Smoking | |||
| Never | 12,662 (22.79%) | 10,050 (22.82%) | 2612 (22.64%) |
| Former | 13,919 (25.05%) | 9779 (22.21%) | 4140 (35.89%) |
| Current | 28,988 (52.17%) | 24,205 (54.97%) | 4783 (41.47%) |
| Ratio of family income to poverty | |||
| ≤1 | 12,048 (21.68%) | 9353 (21.24%) | 2695 (23.36%) |
| 1–3 | 24,021 (43.23%) | 18,178 (41.28%) | 5843 (50.65%) |
| >3 | 19,500 (35.09%) | 16,503 (37.48%) | 2997 (25.98%) |
| Diabetes | 6469 (11.64%) | 3975 (9.03%) | 2494 (21.62%) |
| Hypertension | 10,078 (18.14%) | 5814 (13.2%) | 4264 (36.97%) |
| Cardiovascular disease | 5705 (10.27%) | 2806 (6.37%) | 2899 (25.13%) |
| BMI, kg/m2 | 28.1 (6.0) | 28.2 (6.0) | 27.5 (5.7) |
| Leisure-time physical activity, MET | 18.5 (28.3) | 19.2 (29.0) | 15.5 (25.5) |
Data were presented as means (standard deviations) or numbers (percentages). BMI, body mass index; MET, metabolic equivalent value.
3.2. Dietary Folate with All-Cause and Cause-Specific Mortality
The sex-specific relationships between dietary folate intake and all-cause and cause-specific mortality are presented in Table 2. Among men, we observed that dietary folate intake was inversely associated with death from all-cause, cardiovascular disease, and cancer. The multivariable hazard ratios (HRs) with 95% confidence intervals (CIs) for the highest versus lowest quintiles in men were 0.77 (0.71–0.85), 0.59 (0.48–0.72), and 0.68 (0.56–0.84) for all-cause, cardiovascular, and cancer mortality, respectively. Consistently, among women, dietary folate intake was inversely associated with all-cause and cardiovascular mortality. However, no significant relationship between dietary folate intake and cancer mortality was observed. The multivariable HRs (95% CIs) for the highest versus lowest quintiles in women were 0.86 (0.78–0.95), 0.53 (0.41–0.69), and 0.82 (0.66–1.03) for all-cause, cardiovascular, and cancer mortality, respectively.
Table 2.
Hazard Ratios (HRs) and 95% confidence intervals (CIs) for all-cause and cause-specific mortality according to the quintiles of dietary folate.
| Quartile of Nutrient Intake | Ptrend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Men | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.89 (0.84–0.95) |
0.77 (0.72–0.83) |
0.65 (0.60–0.71) |
<0.001 |
| Multivariable Model | Ref | 0.91 (0.86–0.97) |
0.86 (0.80–0.92) |
0.77 (0.71–0.85) |
<0.001 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.80 (0.71–0.91) |
0.64 (0.55–0.75) |
0.53 (0.44–0.63) |
<0.001 |
| Multivariable Model | Ref | 0.81 (0.71–0.92) |
0.71 (0.61–0.83) |
0.59 (0.48–0.72) |
<0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.82 (0.72–0.93) |
0.77 (0.66–0.89) |
0.57 (0.48–0.68) |
<0.001 |
| Multivariable Model | Ref | 0.87 (0.77–0.99) |
0.89 (0.77–1.04) |
0.68 (0.56–0.84) |
0.001 |
| Women | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 1.01 (0.94–1.07) |
0.91 (0.84–0.98) |
0.85 (0.78–0.93) |
<0.001 |
| Multivariable Model | Ref | 0.91 (0.85–0.97) |
0.87 (0.81–0.95) |
0.86 (0.78–0.95) |
<0.001 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.91 (0.79–1.05) |
0.71 (0.59–0.86) |
0.58 (0.46–0.71) |
<0.001 |
| Multivariable Model | Ref | 0.82 (0.70–0.95) |
0.69 (0.57–0.83) |
0.53 (0.41–0.69) |
<0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.97 (0.84–1.13) |
1.04 (0.88–1.24) |
0.79 (0.65–0.97) |
0.115 |
| Multivariable Model | Ref | 0.93 (0.80–1.08) |
1.05 (0.88–1.25) |
0.82 (0.66–1.03) |
0.342 |
Crude HR did not adjust for anything. Multivariable HR adjusted for age, race/ethnicity, BMI, family income–poverty ratio, smoking status, drinking status, leisure-time physical activity, total energy intake, diabetes, hypertension, and cardiovascular disease.
3.3. Dietary Vitamin B6 with All-Cause and Cause-Specific Mortality
The sex-specific relationships between dietary vitamin B6 intake and all-cause and cause-specific mortality are presented in Table 3. Among men, a higher dietary intake of vitamin B6 was associated with a lower risk of all-cause (HR (95% CI) 0.79 (0.71–0.86)), CVD (HR (95% CI) 0.69 (0.56–0.85)), and cancer mortality (HR (95% CI) 0.73 (0.60–0.90)). Among women, a higher dietary intake of vitamin B6 was associated with a lower risk of all-cause (HR (95% CI) 0.88 (0.80–0.97)) and CVD mortality (HR (95% CI) 0.56 (0.44–0.73)). No significant relationship between dietary vitamin B6 intake and cancer mortality was observed.
Table 3.
Hazard Ratios (HRs) and 95% confidence intervals (CIs) for all-cause and cause-specific mortality according to the quintiles of dietary vitamin B6.
| Quartile of Nutrient Intake | Ptrend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Men | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.76 (0.72–0.81) |
0.65 (0.61–0.70) |
0.57 (0.53–0.62) |
<0.001 |
| Multivariable Model | Ref | 0.94 (0.88–1.00) |
0.86 (0.80–0.93) |
0.79 (0.71–0.86) |
<0.001 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.71 (0.62–0.80) |
0.55 (0.47–0.64) |
0.51 (0.43–0.61) |
<0.001 |
| Multivariable Model | Ref | 0.87 (0.76–0.98) |
0.74 (0.63–0.86) |
0.69 (0.56–0.85) |
<0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.67 (0.59–0.76) |
0.70 (0.61–0.80) |
0.54 (0.45–0.64) |
<0.001 |
| Multivariable Model | Ref | 0.85 (0.74–0.97) |
0.95 (0.82–1.10) |
0.73 (0.60–0.90) |
0.013 |
| Women | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.93 (0.87–0.99) |
0.85 (0.79–0.91) |
0.83 (0.76–0.91) |
<0.001 |
| Multivariable Model | Ref | 0.93 (0.87–1.00) |
0.90 (0.84–0.98) |
0.88 (0.80–0.97) |
0.002 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.89 (0.77–1.03) |
0.71 (0.60–0.85) |
0.58 (0.47–0.72) |
<0.001 |
| Multivariable Model | Ref | 0.89 (0.77–1.03) |
0.77 (0.64–0.92) |
0.56 (0.44–0.73) |
<0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.98 (0.84–1.13) |
0.85 (0.71–1.00) |
0.82 (0.68–1.00) |
0.017 |
| Multivariable Model | Ref | 1.01 (0.87–1.17) |
0.91 (0.76–1.08) |
0.89 (0.72–1.10) |
0.182 |
Crude HR did not adjust for anything. Multivariable HR adjusted for age, race/ethnicity, BMI, family income–poverty ratio, smoking status, drinking status, leisure-time physical activity, total energy intake, diabetes, hypertension, and cardiovascular disease.
3.4. Dietary Vitamin B12 with All-Cause and Cause-Specific Mortality
Table 4 shows the HRs for dietary vitamin B12 intake in relation to all-cause and cause-specific mortality. We observed that vitamin B12 intake was not associated with death from all-cause, cardiovascular, or cancer mortality in either men or women. For men, the multivariable HRs (95% CIs) for the highest versus lowest quintiles were 1.01 (0.92–1.11), 0.93 (0.76–1.13), and 0.96 (0.79–1.16) for all-cause, cardiovascular, and cancer mortality, respectively. For women, the multivariable HRs (95% CIs) for the highest versus lowest quintiles were 1.07 (0.97–1.18), 1.05 (0.83–1.34), and 1.05 (0.84–1.31) for all-cause, cardiovascular, and cancer mortality, respectively.
Table 4.
Hazard Ratios (HRs) and 95% confidence intervals (CIs) for all-cause and cause-specific mortality according to the quintiles of dietary vitamin B12.
| Quartile of Nutrient Intake | Ptrend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Men | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.88 (0.82–0.93) |
0.79 (0.73–0.84) |
0.66 (0.61–0.72) |
<0.001 |
| Multivariable Model | Ref | 1.01 (0.95–1.08) |
1.01 (0.94–1.09) |
1.01 (0.92–1.11) |
0.719 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.78 (0.69–0.90) |
0.68 (0.59–0.79) |
0.56 (0.47–0.67) |
<0.001 |
| Multivariable Model | Ref | 0.92 (0.80–1.05) |
0.91 (0.77–1.07) |
0.93 (0.76–1.13) |
0.311 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.84 (0.73–0.96) |
0.85 (0.73–0.98) |
0.65 (0.55–0.77) |
<0.001 |
| Multivariable Model | Ref | 0.97 (0.84–1.11) |
1.08 (0.93–1.27) |
0.96 (0.79–1.16) |
0.895 |
| Women | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.88 (0.82–0.95) |
0.83 (0.77–0.89) |
0.77 (0.71–0.84) |
<0.001 |
| Multivariable Model | Ref | 1.04 (0.97–1.11) |
1.02 (0.94–1.11) |
1.07 (0.97–1.18) |
0.244 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.84 (0.72–0.97) |
0.66 (0.56–0.79) |
0.55 (0.45–0.68) |
<0.001 |
| Multivariable Model | Ref | 1.11 (0.95–1.29) |
0.98 (0.81–1.19) |
1.05 (0.83–1.34) |
0.848 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.93 (0.80–1.08) |
0.91 (0.77–1.07) |
0.84 (0.69–1.01) |
0.062 |
| Multivariable Model | Ref | 1.03 (0.88–1.20) |
1.05 (0.88–1.26) |
1.05 (0.84–1.31) |
0.598 |
Crude HR did not adjust for anything. Multivariable HR adjusted for age, race/ethnicity, BMI, family income–poverty ratio, smoking status, drinking status, leisure-time physical activity, total energy intake, diabetes, hypertension, and cardiovascular disease.
3.5. Subgroup and Sensitivity Analysis
The results of the subgroup analyses are presented in Tables S1–S6. The relationships of dietary folate, vitamin B6, and vitamin B12 with all-cause and cause-specific mortality appeared to be similar to the main results, although several subgroup findings did not reach statistical significance. Statistically significant interactions were observed for some factors. For male participants, we observed stronger negative associations of folate and vitamin B6 intake with cardiovascular mortality in older adults than in younger adults. For female participants, a statistically significant interaction was observed for the relationship between dietary vitamin B12 and cardiovascular mortality in the analyses stratified according to BMI at baseline (P for interaction = 0.008), even though the difference did not reach statistical significance in both groups.
Sensitivity analyses suggested that the significant associations of dietary folate and vitamin B6 with all-cause and cause-specific mortality remained similar after excluding the participants who died within the first 2 years of follow-up (Table S7) and the participants with cardiovascular disease at baseline (Table S8).
4. Discussion
To the best of our knowledge, this is the largest study so far to comprehensively investigate the relationships of the dietary intakes of folate, vitamin B6, and vitamin B12 with all-cause and cause-specific mortality in a large, nationally representative U.S. adults cohort. We found that dietary folate and vitamin B6 intakes were inversely associated with mortality from all-cause, cardiovascular disease, and cancer for men and with mortality from all-cause and cardiovascular disease for women. No significant associations were seen between the intake of vitamin B12 and all-cause and cause-specific mortality in either men or women.
Our findings of the inverse association between dietary folate intake and all-cause and cause-specific mortality are in line with several previous studies. The Swedish Mammography Cohort suggested that the dietary intake of folate was associated with a reduced risk of all-cause mortality in women diagnosed with breast cancer [19]. The Japan Collaborative Cohort Study found that the dietary intake of folate was associated with a reduced risk of mortality from heart failure for men and of mortality from stroke, CHD, and total cardiovascular disease for women [9]. One study from the same cohort suggested that folate intake was associated with lower all-cause and CVD mortality among participants at a high risk of CVD [20]. One ecological study in Spain found that folate intake was associated with a reduced risk of death from ischemic heart disease and cerebrovascular disease in men and of death from cerebrovascular disease in women [8]. However, some other studies have inconsistent results. The American Association of Retired Persons Diet and Health Study did not find a significant association between folate intake and liver disease mortality [6]. Another study in the U.S. reported that dietary folate was neither associated with all-cause nor breast-cancer-specific mortality [10]. This inconsistency can be ascribed to a series of factors, including the variations in the health outcomes, research methods, study populations, and study regions.
Previous data on the associations between dietary vitamin B6 intake and mortality risk have been limited. Our findings of inverse relationships of dietary vitamin B6 intake with all-cause, cardiovascular, and cancer mortality for men and with all-cause and cardiovascular mortality for women are in line with some previous studies. Three prospective cohort studies found that a higher intake of dietary vitamin B6 was associated with a lower risk of all-cause mortality [21], cardiovascular mortality [9], and prostate cancer mortality [22]. Contrary to our findings, an ecological analysis in Spain did not observe a significant association between dietary vitamin B6 intake and cardiovascular mortality [8]. Among 1508 women with breast cancer, Xu et al. [10] reported non-significant associations between dietary vitamin B6 intake and all-cause or breast-cancer-specific mortality. In a Chinese study, dietary vitamin B6 intake was inversely associated with all-cause and cardiovascular mortality, but it was not associated with cancer mortality [23]. A recent study in U.K. reported that dietary vitamin B6 intake was not statistically associated with colorectal-cancer-specific mortality [24]. Of these previous studies, one was an ecological analysis, three were among participants with cancer, and the other three were among middle-aged or older adults. Thus, it may be difficult to compare them directly with our study.
To date, only seven studies have investigated the relationships between dietary vitamin B12 intake and the risk of death. Four studies reported that a higher intake of dietary vitamin B12 was associated with a lower risk of death from cerebrovascular disease in the general population [8], as well as from all-cause [25] and cancer [25,26] among participants with cancer, which is similar to our findings. However, the three other studies found no significant associations for all-cause [10], breast-cancer-specific [10], prostate-cancer-specific [22], or colorectal-cancer-specific mortality [24]. More interestingly, the Japan Collaborative Cohort Study observed a positive association between dietary vitamin B12 intake and stroke mortality in older men [9]. Again, a direct comparison of these studies is difficult considering the heterogeneity of the study populations and study methods.
Our study has a series of strengths. Firstly, this study was based on a reliable and robust design with a complex, stratified, multistage probability sampling method, which made it possible to select a representative sample of the general U.S. population. Secondly, the relatively large sample size enabled us to provide more stable and precise estimates and made it possible for us to conduct a series of subgroup and sensitivity analyses. Thirdly, given the comprehensive data collection in the NHANES, we could adjust for a variety of potential confounders, including race/ethnicity, socioeconomic status, lifestyle factors, and comorbidities.
It should also be acknowledged that out study has several limitations. Firstly, the dietary nutrients intake was collected via one or two 24 h diet recalls for each person, which may not reflect the long-term intake since food intake varies from day to day. However, the National Cancer Institute method was used to reduce the measurement bias due to dietary intake estimation using 24 h diet recalls [27,28]. In addition, this measurement bias seems to be random, and there is no evidence suggesting that the potential measurement bias is different between the participants who survived and those who died. We thus speculate that this limitation should not affect the study’s conclusion. Secondly, the mortality outcomes were determined by linkage to the National Death Index through a probabilistic match, which might result in misclassification. However, a prior validation study showed that 99.4% of the living participants and 96.1% of the decedents were classified correctly [29]. Thirdly, we could not investigate the effect for cancer-cause-specific mortality due to the limited information. Fourthly, we used the pre-existing data analyses of the relationships of diet folate, vitamin B6, and vitamin B12 intake with all-cause and cause-specific mortality, which may not be considered initially in the NHANES survey. In addition, the biomarkers of vitamins were not considered. However, previous studies suggested that diet intake was highly correlated with B vitamin status [30,31,32].
5. Conclusions
In summary, using data from a nationally representative survey of U.S. adults, we found that dietary folate and vitamin B6 intakes were inversely associated with mortality from all-cause, cardiovascular disease, and cancer for men and with mortality from all-cause and cardiovascular disease for women. Our findings suggest that increasing the intake of folate and vitamin B6 may lower the mortality risk among U.S. adults.
Acknowledgments
The authors sincerely thank the NHANES of the CDC for providing the publicly available data.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14112253/s1, Table S1. Stratified analyses of the associations between dietary folate intake and all-cause and cause-specific mortality in men; Table S2. Stratified analyses of the associations between dietary vitamin B6 intake and all-cause and cause-specific mortality in men; Table S3. Stratified analyses of the associations between dietary vitamin B12 intake and all-cause and cause-specific mortality in men; Table S4. Stratified analyses of the associations between dietary folate intake and all-cause and cause-specific mortality in women; Table S5. Stratified analyses of the associations between dietary vitamin B6 intake and all-cause and cause-specific mortality in women; Table S6. Stratified analyses of the associations between dietary vitamin B12 intake and all-cause and cause-specific mortality in women; Table S7 Hazard Ratios (HRs) and 95% CIs for all-cause and cause-specific mortality according to the quartiles of dietary folate, vitamin B6, and B12 intake after excluding the participants with cardiovascular disease at baseline; Table S8 Hazard Ratios (HRs) and 95% CIs for all-cause and cause-specific mortality according to the quartiles of dietary folate, vitamin B6, and B12 intake after excluding the participants who died within two years of follow-up.
Author Contributions
Conceptualization, Y.B. and Z.Y.; methodology, Y.B.; data curation, Y.B.; writing—original draft preparation, Y.B.; writing—review and editing, H.X., J.Z., Z.W. and Z.Y.; visualization, H.Z.; supervision, X.Z. and Z.Y.; project administration, Z.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study used de-identified, nationally representative survey data that are publicly available upon request to the NHANES. This work was deemed to be of minimal risk. We did not seek the approval of an ethics committee.
Informed Consent Statement
No specific informed consent was required on account of using de-identified data.
Data Availability Statement
The data are publicly available online (https://wwwn.cdc.gov/nchs/nhanes/Default.aspx; accessed on 22 March 2022). The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Open Research Fund of the National Health Commission Key Laboratory of Birth Defects Prevention and the Henan Key Laboratory of Population Defects Prevention, No. ZD202203.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tsai M.Y., Loria C.M., Cao J., Kim Y., Siscovick D.S., Schreiner P.J., Hanson N.Q. Polygenic association with total homocysteine in the post-folic acid fortification era: The CARDIA study. Mol. Genet. Metab. 2009;98:181–186. doi: 10.1016/j.ymgme.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Looker H.C., Fagot-Campagna A., Gunter E.W., Pfeiffer C.M., Sievers M.L., Bennett P.H., Nelson R.G., Hanson R.L., Knowler W.C. Homocysteine and vitamin B(12) concentrations and mortality rates in type 2 diabetes. Diabetes Metab. Res. Rev. 2007;23:193–201. doi: 10.1002/dmrr.660. [DOI] [PubMed] [Google Scholar]
- 3.Ntaios G., Savopoulos C., Grekas D., Hatzitolios A. The controversial role of B-vitamins in cardiovascular risk: An update. Arch. Cardiovasc. Dis. 2009;102:847–854. doi: 10.1016/j.acvd.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Blount B.C., Mack M.M., Wehr C.M., MacGregor J.T., Hiatt R.A., Wang G., Wickramasinghe S.N., Everson R.B., Ames B.N. Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: Implications for cancer and neuronal damage. Proc. Natl. Acad. Sci. USA. 1997;94:3290–3295. doi: 10.1073/pnas.94.7.3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Um H.J., Ko J.W., Won S.B., Kwon Y.H. Effects of Dietary Vitamin B6 Restriction on Hepatic Gene Expression Profile of Non-Obese and Obese Mice. Nutrients. 2020;12:3821. doi: 10.3390/nu12123821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Persson E.C., Schwartz L.M., Park Y., Trabert B., Hollenbeck A.R., Graubard B.I., Freedman N.D., McGlynn K.A. Alcohol consumption, folate intake, hepatocellular carcinoma, and liver disease mortality. Cancer Epidemiol. Biomark. Prev. 2013;22:415–421. doi: 10.1158/1055-9965.EPI-12-1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li B., Lu Y., Wang L., Zhang C.X. Folate intake and breast cancer prognosis: A meta-analysis of prospective observational studies. Eur. J. Cancer Prev. 2015;24:113–121. doi: 10.1097/CEJ.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 8.Medrano M.J., Sierra M.J., Almazán J., Olalla M.T., López-Abente G. The association of dietary folate, B6, and B12 with cardiovascular mortality in Spain: An ecological analysis. Am. J. Public Health. 2000;90:1636–1638. doi: 10.2105/ajph.90.10.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cui R., Iso H., Date C., Kikuchi S., Tamakoshi A. Dietary folate and vitamin b6 and B12 intake in relation to mortality from cardiovascular diseases: Japan collaborative cohort study. Stroke. 2010;41:1285–1289. doi: 10.1161/STROKEAHA.110.578906. [DOI] [PubMed] [Google Scholar]
- 10.Xu X., Gammon M.D., Wetmur J.G., Bradshaw P.T., Teitelbaum S.L., Neugut A.I., Santella R.M., Chen J. B-vitamin intake, one-carbon metabolism, and survival in a population-based study of women with breast cancer. Cancer Epidemiol. Biomark. Prev. 2008;17:2109–2116. doi: 10.1158/1055-9965.EPI-07-2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jenkins D.J.A., Spence J.D., Giovannucci E.L., Kim Y.I., Josse R., Vieth R., Blanco Mejia S., Viguiliouk E., Nishi S., Sahye-Pudaruth S., et al. Supplemental Vitamins and Minerals for CVD Prevention and Treatment. J. Am. Coll. Cardiol. 2018;71:2570–2584. doi: 10.1016/j.jacc.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Ebbing M., Bønaa K.H., Nygård O., Arnesen E., Ueland P.M., Nordrehaug J.E., Rasmussen K., Njølstad I., Refsum H., Nilsen D.W., et al. Cancer incidence and mortality after treatment with folic acid and vitamin B12. JAMA. 2009;302:2119–2126. doi: 10.1001/jama.2009.1622. [DOI] [PubMed] [Google Scholar]
- 13.Roswall N., Olsen A., Christensen J., Hansen L., Dragsted L.O., Overvad K., Tjønneland A. Micronutrient intake in relation to all-cause mortality in a prospective Danish cohort. Food Nutr. Res. 2012;56:5466–5474. doi: 10.3402/fnr.v56i0.5466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mursu J., Robien K., Harnack L.J., Park K., Jacobs D.R., Jr. Dietary supplements and mortality rate in older women: The Iowa Women’s Health Study. Arch. Intern. Med. 2011;171:1625–1633. doi: 10.1001/archinternmed.2011.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey Data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD, USA: 2022. [(accessed on 9 May 2022)]. Available online: https://www.cdc.gov/nchs/nhanes/index.htm. [Google Scholar]
- 16.National Center for Health Statistics (NCHS) About the National Health and Nutrition Examination Survey. NCHS; Hyattsville, MD, USA: 2017. [(accessed on 9 May 2022)]. Available online: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. [Google Scholar]
- 17.U.S. Department of Agriculture Food Surveys Research Group . Food and Nutrient Database for Dietary Studies. U.S. Department of Agriculture Food Surveys Research Group; Beltsville, MD, USA: 2021. [(accessed on 2 December 2021)]. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds/ [Google Scholar]
- 18.Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann. Transl. Med. 2016;4:30. doi: 10.3978/j.issn.2305-5839.2015.12.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris H.R., Bergkvist L., Wolk A. Folate intake and breast cancer mortality in a cohort of Swedish women. Breast Cancer Res. Treat. 2012;132:243–250. doi: 10.1007/s10549-011-1838-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu X., Wei W., Jiang W., Song Q., Chen Y., Li Y., Zhao Y., Sun H., Yang X. Association of folate intake with cardiovascular-disease mortality and all-cause mortality among people at high risk of cardiovascular-disease. Clin. Nutr. 2022;41:246–254. doi: 10.1016/j.clnu.2021.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Huang Y.C., Lee M.S., Wahlqvist M.L. Prediction of all-cause mortality by B group vitamin status in the elderly. Clin. Nutr. 2012;31:191–198. doi: 10.1016/j.clnu.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 22.Kasperzyk J.L., Fall K., Mucci L.A., Håkansson N., Wolk A., Johansson J.E., Andersson S.O., Andrén O. One-carbon metabolism-related nutrients and prostate cancer survival. Am. J. Clin. Nutr. 2009;90:561–569. doi: 10.3945/ajcn.2009.27645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao L.G., Shu X.O., Li H.L., Gao J., Han L.H., Wang J., Fang J., Gao Y.T., Zheng W., Xiang Y.B. Prospective cohort studies of dietary vitamin B6 intake and risk of cause-specific mortality. Clin. Nutr. 2019;38:1180–1187. doi: 10.1016/j.clnu.2018.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lochhead P., Nishihara R., Qian Z.R., Mima K., Cao Y., Sukawa Y., Kim S.A., Inamura K., Zhang X., Wu K., et al. Postdiagnostic intake of one-carbon nutrients and alcohol in relation to colorectal cancer survival. Am. J. Clin. Nutr. 2015;102:1134–1141. doi: 10.3945/ajcn.115.115162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ricci C., Freisling H., Leitzmann M.F., Taljaard-Krugell C., Jacobs I., Kruger H.S., Smuts C.M., Pieters M. Diet and sedentary behaviour in relation to cancer survival. A report from the national health and nutrition examination survey linked to the U.S. mortality registry. Clin. Nutr. 2020;39:3489–3496. doi: 10.1016/j.clnu.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Galván-Portillo M.V., Oñate-Ocaña L.F., Pérez-Pérez G.I., Chen J., Herrera-Goepfert R., Chihu-Amparan L., Flores-Luna L., Mohar-Betancourt A., López-Carrillo L. Dietary folate and vitamin B12 intake before diagnosis decreases gastric cancer mortality risk among susceptible MTHFR 677TT carriers. Nutrition. 2010;26:201–208. doi: 10.1016/j.nut.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Willett W.C. Nutritional Epidemiology. 3rd ed. Oxford University Press; New York, NY, USA: 2013. [Google Scholar]
- 28.Danaei G., Ding E.L., Mozaffarian D., Taylor B., Rehm J., Murray C.J., Ezzati M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menke A., Muntner P., Batuman V., Silbergeld E.K., Guallar E. Blood lead below 0.48 micromol/L (10 microg/dL) and mortality among US adults. Circulation. 2006;114:1388–1394. doi: 10.1161/CIRCULATIONAHA.106.628321. [DOI] [PubMed] [Google Scholar]
- 30.Lavriša Ž., Hristov H., Hribar M., Žmitek K., Kušar A., Koroušić Seljak B., Gregorič M., Blaznik U., Gregorič N., Zaletel K., et al. Dietary Intake and Status of Vitamin B12 in Slovenian Population. Nutrients. 2022;14:334. doi: 10.3390/nu14020334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hustad K.S., Ottestad I., Olsen T., Sæther T., Ulven S.M., Holven K.B. Salmon fish protein supplement increases serum vitamin B12 and selenium concentrations: Secondary analysis of a randomised controlled trial. Eur. J. Nutr. 2022:1–9. doi: 10.1007/s00394-022-02857-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pravst I., Lavriša Ž., Hribar M., Hristov H., Kvarantan N., Seljak B.K., Gregorič M., Blaznik U., Gregorič N., Zaletel K., et al. Dietary Intake of Folate and Assessment of the Folate Deficiency Prevalence in Slovenia Using Serum Biomarkers. Nutrients. 2021;13:3860. doi: 10.3390/nu13113860. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are publicly available online (https://wwwn.cdc.gov/nchs/nhanes/Default.aspx; accessed on 22 March 2022). The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.