Abstract
The global prevalence of eye diseases continues to grow, bringing with it a reduction in the activity levels and quality of life of patients, and partial or complete blindness if left untreated. As such, there is considerable interest in identifying more effective therapeutic options and preventive agents. One such agent is vitamin D, known to have a range of anti-cancer, anti-angiogenic, anti-inflammatory and anti-oxidative properties, and whose deficiency is linked to the pathogenesis of a range of cardiovascular, cancer, and inflammatory diseases. This review presents the current stage of knowledge concerning the link between vitamin D and its receptor and the occurrence of eye disease, as well as the influence of analogues of calcitriol, an active metabolite of vitamin D. Generally, patients affected by various ocular disorders have vitamin D deficiency. In addition, previous findings suggest that vitamin D modulates the course of eye diseases and may serve as a marker, and that its supplementation could mitigate some disorders. However, as these studies have some limitations, we recommend further randomized trials to clarify the link between vitamin D and its activity with eye disease.
Keywords: 25-hydroxyvitamin D, calcitriol, eye diseases, vitamin D
1. Introduction
The human eye is a delicate structure that receives optical information from the environment, allowing light perception and vision. However, its operation is inhibited by a range of factors, such as aging, genetic predisposition, excessive light exposure, chronic hyperglycemia, autoimmune diseases, angiogenesis, inflammation and oxidative stress; these may lead to the development of a range of eye diseases such as age-related macular degeneration, diabetic retinopathy or dry eye syndrome. In addition, most ocular disorders result in visual impairment or blindness. Approximately 405 million individual cases of visual impairment were reported in 2015, with 36 million people living with vision loss that year. Moreover, the number of patients with blindness is expected to increase about threefold by the year 2050 [1]. Visual impairment is also related to considerable economic burden for patients, their caregivers and medical care in developed countries [2]. In addition, blindness and visual impairment are two of the strongest risk factors for social isolation, reduced quality of life and decline of functional status. Furthermore, the majority of ocular diseases are diagnosed in advanced stages, which excludes effective therapy [3,4]. As such, prevention is a priority and a significant element of therapeutic approaches.
Numerous studies have demonstrated that a healthy diet limits the development or progression of eye disorders. Indeed, vitamin D deficiency, i.e., a 25-hydroxyvitamin D level lower than 20 ng/mL, is a global health problem [5]. The consumption of fruits and vegetables, which are source of polyphenols and carotenoids, as well as vitamins A, C and E, play a significant role in the prevention and treatment of ocular diseases. These compounds have multiple pro-health properties, mainly comprising anti-inflammatory, anti-oxidant and anti-angiogenic activities [6,7,8]. Nevertheless, other agents believed to more effectively inhibit the development of eye diseases have been the focus of many studies. One such agent is vitamin D, commonly defined as the “sunshine vitamin”. Although it is a multifunctional hormone, its primary purposes are arguably to maintain calcium homeostasis, mineral metabolism and skeletal health. Vitamin D binds calcitriol, an activated metabolite of vitamin D, to the vitamin D receptor (VDR). Interestingly, recent studies indicate that vitamin D and calcitriol derivatives may mitigate the course of many diseases inter alia cancers, psoriasis, multiple sclerosis, diabetes and autoimmune diseases [9,10,11]. In addition, increasing numbers of studies show that vitamin D, VDR and calcitriol analogues can play an important role in the maintenance of ocular health [12]. This aim of this paper is to review existing literature regarding the role of vitamin D, VDR and calcitriol analogues in eye diseases.
2. Vitamin D—Sources, Metabolism and VDR
In humans, vitamin D can be obtained from three potential sources: food, local synthesis in the skin and supplementation. It is available in two major forms: cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2). The main dietary sources are fatty fishes and fish oils, primarily mackerel, sardines, salmon and cod liver oil in the case of vitamin D3, and sundried mushrooms for vitamin D2 [13].
Endogenous production in the skin is stimulated by exposure to ultraviolet B radiation, resulting in the synthesis of biologically-inactive vitamin D3 from 7-dehydrocholesterol. This vitamin D then binds with the vitamin D binding protein and albumin and is transported in the blood. In the liver, vitamin D is hydroxylated to 25-hydroxyvitamin D by cytochrome P450 enzymes (CYP2R1 and CYP27A1). Further modifications occur in kidneys, where 25-hydroxyvitamin D is converted to the biologically-active form, 1,25-dihydroxyvitamin D (calcitriol), by 1-α-hydroxylase (CYP27B1). Calcitriol level is regulated by a renal negative feedback loop and the CYP24A1 enzyme (24-hydroxylase), which inactivates calcitriol [13].
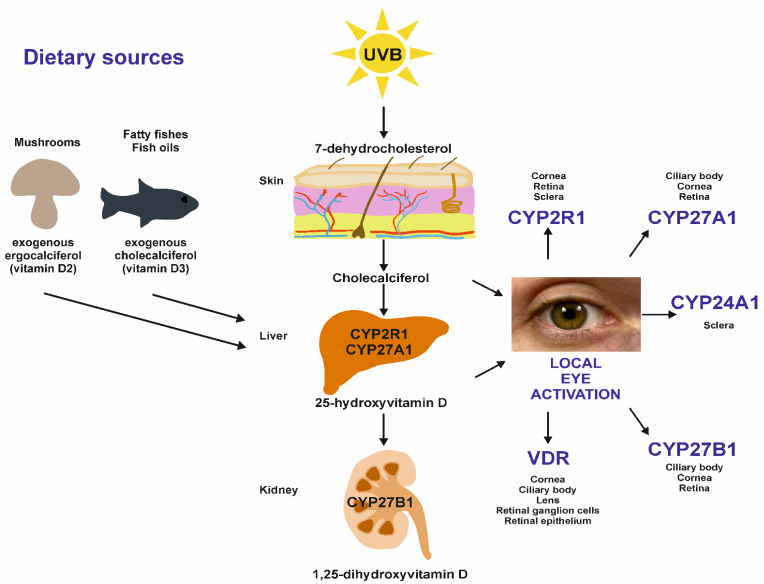
Vitamin D can also be metabolized locally, including in the eyes (Figure 1). Recent studies indicate that vitamin D hydroxylases are present in ocular structures such as the cornea, ciliary body, sclera and retina, suggesting that vitamin D may be an important intraocular mediator in eye diseases [14,15]. Finally, vitamin D supplementation can be used to maintain adequate concentrations.
Figure 1.
A schematic view of vitamin D metabolism, including local eye activation of vitamin D. Eye cells possess the enzymes to activate and regulate vitamin D metabolism. The figure specifies eye structures having the vitamin D receptor (VDR) and enzymes taking part in the metabolism of vitamin D. In addition, the schematic shows the dietary sources of vitamin D. Sundried mushrooms and fatty fishes, including fish oils, are the sources of ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3), respectively. Both are metabolized to 25-hydroxyvitamin D2/D3 in the liver and, subsequently, to other metabolites. Nevertheless, vitamin D3 is almost twice as potent as ergocalciferol in increasing serum 25-hydroxyvitamin D, and the supplementation of vitamin D2 does not result in as high a blood level of 25-hydroxyvitamin D [16,17].
The biological action of calcitriol, the active form of vitamin D, is mediated by VDR, a member of the nuclear hormone receptor superfamily. VDR functions as a heterodimer with the retinoid X receptor. This complex interacts with specific DNA sequences belonging to the vitamin D response element (VDRE), resulting in the activation or repression of transcription of genes influencing the function of vitamin D [18,19]. It must be emphasized that VDR is expressed in the structural elements of eye [14,20], and that certain polymorphisms of the VDR gene may be related to the occurrence of eye disease [21,22].
3. Calcitriol Analogues
As mentioned above, calcitriol takes part in the homeostasis of calcium and phosphate, and seems to be a potent agent in the treatment of many diseases. However, the therapeutic effect of exogenous calcitriol often require it to be present in supraphysiological concentrations resulting in toxic and undesirable effects, primarily hypercalcemia, hypercalciuria, excessive bone resorption and vascular calcification [23,24]. To avoid these side effects, structural analogues of calcitriol have been created, e.g., 22-oxacalcitriol and 2-methylene-19-nor-(20S)-1α,25-dihydroxyvitamin D3, and these have been found to have potential efficacy in ocular disorders [25,26]. These compounds deserve attention, and their detailed role in some eye diseases are described in the next section.
4. Vitamin D, VDR and Calcitriol Analogues in Ocular Diseases
4.1. Age-Related Macular Degeneration (AMD)
AMD is an acquired eye disease that affects the macula, resulting in visual impairment, and even blindness. Various risk factors have associations with development and progression of AMD, including angiogenesis, the inflammatory response, lipofuscin accumulation in retinal pigment epithelial cells, aging, smoking and sunlight exposure [27,28]. In addition, an important component of the neovascular form of AMD is the formation of new retinal blood vessels, as is apoptosis, pyroptosis and necroptosis of retinal cells, and impaired autophagy. It has been reported that vitamin D modulates programmed death pathways, and that it may influence autophagy and possess anti-angiogenic properties [29]. In addition, vitamin D deficiency is associated with a thinning of the ganglion cell complex and retinal nerve fiber layer [30]. Thus, vitamin D could modulate the course of AMD. Some studies indicate a potential association between 25-hydroxyvitamin D deficiency in serum, possibly associated with low vitamin D intake, and the risk of AMD, including the neovascular form [31,32,33,34]. In addition, some studies suggest that high levels of 25-hydroxyvitamin D can decrease the risk of AMD [35,36]. Nevertheless, most available studies, including meta-analyses, do not indicate that high serum vitamin D levels have a significant protective influence against the occurrence of any stages or subtypes of AMD [37,38,39,40,41,42,43]. In addition, in one study, vitamin D was not found to have any significant overall effect on the incidence and progression of AMD [44]. While it is reasonable to expect discrepancies between studies as a result of heterogeneity in study procedures and lack of longitudinal designs, the literature does not provide any clear evidence of a definitive association between serum 25-hydroxyvitamin D level and AMD
4.2. Diabetic Retinopathy (DR)
One common microvascular ocular complication of diabetes mellitus that remains the leading cause of preventable blindness is diabetic retinopathy (DR). As of 2010, this eye disorder affected over 100 million patients worldwide, and this number is expected to almost double by the year 2030 [45,46]. Studies indicate that that patients with DR had lower serum levels of vitamin D compared with those without [47] and that vitamin D (25-hydroxyvitamin D) deficiency is significantly associated with an almost twofold greater risk of DR [48,49,50,51,52,53], especially the proliferative form [54,55]. This dependence has been observed for patients with type 1 and type 2 diabetes mellitus [56,57,58]. Furthermore, it has been proposed that a serum concentration of 25-hydroxyvitamin D ≤ 18.6 ng/mL may serve as a sensitive and specific indicator for the proliferative type among subjects with DR [59]. Interestingly, endogenous vitamin D3 metabolites, such as 1,25-dihydroxyvitamin D, 25-hydroxyvitamin D and 24,25-dihydroxyvitamin D, could be better for predicting DR than total vitamin D level [60].
These findings regarding vitamin D deficiency in patients with DR suggest that vitamin supplementation may offer a protective effect. Indeed, vitamin D has been found to have neuroprotective properties, and its deficiency led to thinning and reduction of mean retinal nerve fiber layer thickness in early-stage DR subjects [61]. In addition, the protective effect of vitamin D in DR may also result from its ability to reduce cholesterol level, improve HDL cholesterol concentration, inhibit the activity of pro-inflammatory cytokines or pro-angiogenic and fibrotic factors, and downregulate ROS production, which play an important role in the pathogenesis of DR [62,63,64,65].
On the other hand, meta-analyses suggest that some polymorphisms of the VDR gene may also act as susceptibility markers for predicting the risk of DR and for earlier diagnosis of eye disease. Polymorphisms BsmI, ApaI, and FokI of the VDR gene are all significantly associated with DR susceptibility [66,67].
4.3. Optic Neuritis (ON)
ON is an inflammatory condition of the optic nerve and is a frequent cause of acute injury in adults and children. Its most common etiology is multiple sclerosis (MS) [68]. As vitamin D insufficiency appears to be a risk factor for the development of MS [69], it is possible that vitamin D may indirectly have an impact on the occurrence of ON and related changes. ON is typically associated with a thinning of the retinal nerve fiber layer (RNFL) caused by declines in axonal and macular volume [70]. Studies have found that vitamin D supplementation does not protect from the loss of RNFL and macula thickness in patients with unilateral ON (i.e., who do not fulfill the McDonald criteria for MS) concomitant with vitamin D insufficiency [70]. Nevertheless, ON may be the first manifestation of MS and occur before a full diagnosis of MS itself. Subjects with acute monosymptomatic ON are often characterized by low 25-hydroxyvitamin D levels in serum; however, these low levels of vitamin D are not correlated with the severity of ON [71]. Nevertheless, in ON patients with a low serum level of vitamin D but without a diagnosis of MS, vitamin D supplementation may delay the occurrence of secondary ON and the subsequent conversion to MS [72]. However, vitamin D levels lower than 30 ng/mL did not appear to be associated with RNFL and macular volume thickness in subjects with MS who were not affected by ON [73]. Therefore, the protective effect of vitamin D in ON is uncertain and requires further clinical trials.
4.4. Retinal Vein Occlusion (RVO)
One of the most common second causes of retinal vascular abnormality, and a frequent sight-threatening disorder, is retinal vein occlusion (RVO). This disease is classified as central RVO (CRVO), hemi central RVO (HCRVO) and branch RVO (BRVO) depending on the location of occlusion of the vein [74,75]. As vitamin D deficiency is believed to be associated with endothelial dysfunction and vascular diseases [76], RVO patients could have low levels of vitamin D in their serum. Indeed, significantly lower mean 25-hydroxyvitamin D serum levels have been noted in Indian subjects with RVO compared to controls; however, subjects with CRVO and BRVO did not demonstrate significant differences in mean vitamin D level compared to controls [77]. Interestingly, among CRVO patients, the mean concentration of 25-hydroxyvitamin D can be statistically significant in subjects aged under 75 years [78]; therefore, vitamin D level may be a helpful indicator for the prophylaxis, therapy or diagnosis of CRVO in this group.
4.5. Myopia
Myopia is the most frequent eye disorder worldwide and is a refractive anomaly. It is primarily caused by an increase in the axial length of the eyeball and elevates the risk of other ocular diseases. Typically, myopia starts in childhood [79,80]. Data indicate that the prevalence of longer axial length and myopia is significantly higher in children, young adults and adults with vitamin D deficiency compared to those with sufficient levels [81,82,83,84,85,86]. However, the relationship between myopia and vitamin D has been contradicted in some studies [87,88,89,90,91]. This discrepancy may result from other factors affecting vitamin D metabolism, such as the time spent outdoors (ultraviolet radiation exposure). It has been demonstrated that increased time spent outdoors, and ultraviolet B exposure, are effective in preventing the onset of myopia and slowing the myopic shift in refractive error associated with reduced myopia [92,93]. Further longitudinal studies are needed to determine whether higher serum 25-hydroxyvitamin D concentration is protective against myopia.
4.6. Retinoblastoma
Retinoblastoma is the most common intraocular cancer in children, and new options and strategies for disease therapy are being sought [94]. Initial studies indicate that retinoblastoma cells have VDR expression [95,96]. Treatment with calcitriol has been found to inhibit Y79 cell growth, inducing apoptosis by increasing the level of Bax protein and decreasing that of Bcl-2 protein [95,96]. Calcitriol was also able to induce cell cycle arrest in the G0/1 phase [96]. Moreover, 1,25-dihydroxyvitamin D significantly limited retinoblastoma growth in athymic mice with subcutaneously-injected cancer cells, as well as tumor angiogenesis in a transgenic retinoblastoma murine model [97,98]. However, calcitriol treatment was found to be toxic, resulting in elevated mortality, hypercalcemia and kidney damage [95,99]. Thus, there is a need for compounds that can act as VDR agonists but with lower calcemic effects. Such candidates include the calcitriol analogs 1,25-dihydroxy-16-ene-23-yne-vitamin D3, 1α-hydroxyvitamin D2 and 2-methylene-19-nor-(20S)-1α-hydroxybishomopregnacalciferol [95,99,100,101]. It must be emphasized that low doses of calcitriol could consolidate the effect of chemotherapy, one of the therapeutic options of retinoblastoma, and improve treatment effectiveness. In addition, the combination of cisplatin and calcitriol significantly inhibited tumor growth in athymic mice with subcutaneously injected human Y79 retinoblastoma cells without any increase in mortality and with minimal nephrotoxicity [102].
4.7. Uveal Melanoma (UM)
UM is a malignant and common primary intraocular tumor with a significant propensity to metastasize in adults. In almost all cases, patients with liver metastasis die within six months, and the median survival time after diagnosis of metastasis is only 3.6 months [103,104,105]. Currently, effective adjuvant therapy is not available to prevent metastases, and neither is there any successful treatment once metastases have developed [106]. Due to the lack of any efficient therapy, new strategies for UM prevention and control are urgently required. Studies show that low vitamin D status is associated with an increased risk of cancer and poor prognosis [107]. Recent studies indicate that components of the vitamin D metabolism, such as VDR, CYP27B1 and CYP24A1, are present in the UM cells [108]. Moreover, a marked reduction of the VDR expression is inversely correlated with melanin level in UM cells, as well as an aggressive UM profile, which contributes to an increased risk of metastases and poorer prognosis [108]. Interestingly, one of the most common susceptibility factors for UM is the inability to tan [109]; the ultraviolet radiation needed for the synthesis of vitamin D appears to have a protective activity against UM [110]. Furthermore, compounds such as calcitriol and calcidiol, i.e., the biologically-active metabolites of vitamin D and its precursor, have been found to sensitize melanoma cells to radiation used in the therapy of UM [111].
Clearly, there is a possible role for vitamin D and its signaling elements in the treatment of UM. Nevertheless, little is known about the impact of vitamin D on the development and progression of UM, especially considering the detailed mechanisms of its action.
4.8. Non-Infectious Uveitis
Uveitis is an intraocular inflammatory condition of the uvea (i.e., the iris, ciliary body, and choroid) which may lead to blindness. Uveitis can be classified depending on the primary localization of the inflammation in the eye (as anterior, intermediate and posterior uveitis) or etiology (as infectious and non-infectious). Uveitis may also be clinically divided into active and inactive forms. It is important to note that non-infectious uveitis is an immune-mediated eye disorder associated with systemic diseases such as sarcoidosis [112]. Studies have revealed an association between hypovitaminosis D and an elevated risk of non-infectious uveitis. For example, vitamin D deficiency contributes to higher risk of uveitis in juvenile idiopathic arthritis [113]. Subjects with normal levels of vitamin D had 21% lower odds of non-infectious uveitis than those with low levels of vitamin D [114]. In addition, significantly decreased blood serum levels of 25-hydroxyvitamin D were detected in patients with non-infectious anterior and non-infectious acute anterior uveitis compared to healthy controls [115,116], as well as in subjects with active non-infectious uveitis compared to inactive non-infectious uveitis patients. Vitamin D supplementation and exposure to the sun were associated with lowered disease activity in patients with vitamin D deficiency [117]. However, every unit (1 ng/mL) increase in vitamin D level was found to be associated with 4% to 5% lower odds of developing non-infectious uveitis depending on the literature source [115,118]. Interestingly, patients with sarcoidosis-related uveitis demonstrated elevated median serum levels of 1,25-dihydroxyvitamin D, compared to those with uveitis due to other causes (132.4 vs. 108.0 pmol/L). In addition, patients with sarcoidosis-induced uveitis had a higher median ratio of 1,25-dihydroxyvitamin D/25-hydroxyvitamin D (4.17 vs. 2.56): a ratio higher than 3.5 was found to be associated with the diagnosis of ocular sarcoidosis, with 68% sensitivity and 78% specificity [119].
Hence, vitamin D may play a role in the development and course of non-infectious uveitis; however, no detailed causal relationship has been identified. Further studies are necessary to determine the efficacy of vitamin D supplementation to mitigate and reduce risk of non-infectious uveitis.
4.9. Vogt-Koyanagi-Harada Disease (VKHD)
VKHD is a rare granulomatous autoimmune disorder that affects tissues and organs containing melanocytes: primarily the eye, inner ear, skin hair or meninges. It is characterized by panuveitis, which results in severely reduced visual acuity or even blindness if not treated appropriately. It is also accompanied by a varying degree of auditory, neurological and cutaneous manifestations. VKHD most frequently affects people from Asia, Latin America and the Middle East, as well as Native Americans [120]. It is known that vitamin D deficiency may be involved in the development of autoimmune diseases [121]. Patients with active VKHD were found to have lower serum levels of 1,25-dihydroxyvitamin D compared to subjects with inactive VKHD and healthy controls. Moreover, 1,25-dihydroxyvitamin D was found to inhibit the proliferation of peripheral blood mononuclear cells and CD4+ T cells, and to slow the production of interleukin (IL)-17 and interferon gamma (IFN-γ) by these cells [122].
Some polymorphisms in the genes of the vitamin D pathway may increase the occurrence of VKHD. One study did not find any polymorphisms in genes such as VDR, CYP24A1 and CYP27B1 that could contribute to VKHD; however, one polymorphism (c.852G > A; p.284 M > I) detected in CYP2R1 appears to be associated with disease and may be pathogenic [123].
Hence, vitamin D may be involved in the development of VKHD, and one CYP2R1 polymorphism may have a causative role. Nevertheless, studies on a larger cohort of patients are necessary to confirm these observations.
4.10. Glaucoma
Glaucoma is a leading cause of irreversible vision loss worldwide. It is an optic neuropathy characterized by progressive degeneration of retinal ganglion cells. It is also associated with slow or difficult outflow of aqueous humor, elevated intraocular pressure (IOP) and damage of the trabecular meshwork [124,125]. Interestingly, 1α,25-dihydroxyvitamin D3 is able to protect against oxidative stress-induced damage to the trabecular meshwork known to occur in glaucoma, suggesting that vitamin D may have therapeutic properties [124]. In addition, the same compound has been found to reduce IOP in non-human primates [25]. Unfortunately, this result has not been confirmed in humans: no difference in IOP was found between healthy subjects with low and high serum 25-hydroxyvitamin D levels. Furthermore, vitamin D supplementation in the patients with low serum concentration of 25-hydroxyvitamin D did not change IOP [126].
Interestingly, except for a group of postmenopausal women, vitamin D deficiency may be considered an independent risk factor for open-angle glaucoma. A reverse J-shaped association was found between serum 25-hydroxyvitamin D levels and the risk of open-angle glaucoma, and patients with glaucoma, including open-angle glaucoma, were characterized by lowered serum 25-hydroxyvitamin D (by about 15% compared to the controls) [127,128,129]. Open-angle patients were also found to have significantly lower serum levels of calcitriol, another metabolite of vitamin D, compared with the age-matched controls [130]. Moreover, the serum level of vitamin D could serve as a marker of the severity of primary open-angle glaucoma, as patients with advanced glaucoma had decreased concentrations of 25-hydroxyvitamin D in comparison to early glaucoma and healthy subjects [131].
4.11. Cataract
Cataract is a common ophthalmic disorder that is associated with clouding of the lens [132]. Available data show that almost 100 million people worldwide are affected by cataract. The possible risk factors include increasing age, female sex, eyeball trauma, ultraviolet-B-exposure, cigarette smoking, diet with a high glycemic index, malnutrition, and genetic factors [133]. Other diseases such as diabetes mellitus, renal impairment, metabolic syndrome and arterial hypertension increase the risk of cataract [133]. In addition, vitamin D may have an effect on cataract. Patients with age-related cataract dad lower mean serum levels of 25-hydroxyvitamin D compared to controls (7.6 ± 5.5 ng/mL vs. 18.5 ± 9.6 ng/mL), and this change was statistically significant. In addition, among different types of age-related cataract, cases of nuclear cataract were characterized by the lowest level of vitamin D [134]. Moreover, vitamin D deficiency in serum was found to be associated with age-related cataract, including the early form of disease [135,136]. Interestingly, studies indicate that the risk of nuclear cataract is inversely correlated with the serum level of 25-hydroxyvitamin D, with it appearing to have a protective role against nuclear cataract [137,138].
Although posterior subcapsular cataract resembles hypocalcemic cataract, the relationship between low serum vitamin D levels and posterior subcapsular cataract formation remains unclear. Brown et al. (2015) suggest that vitamin D deficiency may contribute to the development of posterior subcapsular cataract, and that some comorbidities and non-ophthalmic interventions are associated with posterior subcapsular cataract in the presence of decreased levels of 25-hydroxyvitamin D. Interestingly, some patients with early-stage posterior subcapsular cataract co-existing with vitamin D deficiency had a resolution of changes in the lens following daily supplementation of 5000 IU of 25-hydroxyvitamin D over a 2-year follow-up period [139]. In contrast, no vitamin D deficiency was later observed in patients with posterior subcapsular cataract [140]. In turn, diabetic cataract was characterized by significantly higher levels of 25-hydroxyvitamin D in aqueous humor compared to senile cataract [141].
Vitamin D may well play a role in lens metabolism. However, further extensive trials are needed to explain the correlation between vitamin D concentration and cataract, and to understand the detailed mechanisms of vitamin D activity in this regard.
4.12. Scleritis
Scleritis is an infrequent inflammatory disorder of the sclera that may be caused by infectious factors, trauma, drugs or irradiation, and one that frequently accompanies immune-mediated diseases. The immune system appears to play an important role in the pathogenesis of non-infectious scleritis [142]. Therefore, there is an association between scleritis and vitamin D, which is able to suppress the immune response mainly by the modulation of T lymphocyte activity. Multivariate analyses revealed a statistically significant link between non-infectious scleritis and decreased 25-hydroxyviatmin D levels at any time point before or after the onset of scleritis (28.1 ng/mL vs. 34.4 ng/mL in controls, p = 0.009) and any time point before (24.1 ng/mL vs. 34.4 ng/mL in controls, p = 0.033). In addition, the same analysis showed that the odds of developing scleritis were 4% lower for every unit (1 ng/mL) increase in the vitamin D level (OR = 0.96, 95% CI = 0.93–0.99, p = 0.009) [118]. Further studies are necessary to establish the potential role of vitamin D supplementation in the development of scleritis.
4.13. Dry Eye Syndrome (DES)
DES is a common ophthalmic disorder affecting the ocular surface, which is marked by persistent symptoms. One of the main mechanisms contributing to the development of disease is the inflammatory reaction [143]. Studies indicate that calcitriol, an active metabolite of vitamin D, is able to inhibit dry eye-related corneal inflammation and apoptosis in in vitro and in vivo experimental models of DES, highlighting the protective role of vitamin D [144,145,146]. DES patients had significantly lower serum levels of 25-hydroxyvitamin D, and this correlated with ocular surface disease index [147,148,149,150]. Furthermore, DES patients also displayed significantly lower concentrations of vitamin D in their tears [151], which may result from the fact that the vitamin D deficiency is associated with tear hyperosmolarity, a dysfunction of tear film and reduction of Schirmer’s test value [152,153]. Serum level of 25-hydroxyvitamin D was also found to correlate positively with tear break-up time and tear secretion [154].
In contrast, some studies did not show any association between DES and lowered vitamin D levels [155,156]. Vitamin D (cholecalciferol) supplementation was found to improve tear break-up time, tear secretion, eyelid margin hyperemia and the severity of symptoms in patients with DES refractory to conventional treatment concomitant with vitamin D deficiency [157]. In addition, cholecalciferol supplementation enhanced the efficacy of artificial tears and hyaluronate, which are used in the therapy of DES, and may be a useful adjuvant treatment for subjects with DES refractory to topical lubricants [158]. Furthermore, two single nucleotide polymorphisms (Foklrs2228570 and Apal-rs7975232) in the VDR gene seem to be associated with DES and may potentially be used in the diagnosis of disease [22].
4.14. Vernal Keratoconjunctivitis (VKC)
VKC is a chronic, allergic, inflammatory disease of the tarsal and/or bulbar conjunctiva, which occurs seasonally and mainly in the pediatric population [159]. Data show that vitamin D may mitigate allergic diseases [160]. It has been demonstrated that children with VKC have lower serum levels of 25-hydroxyvitamin D in comparison to healthy controls. In addition, a significant correlation has been confirmed between vitamin D level and VKC severity, including VKC objective score and basophils in conjunctival scraping [161]. In contrast, a more recent study confirmed an inverse correlation between serum vitamin D levels and VKC severity; however this difference was not statistically significant [162]. Another study found decreased mean serum concentrations of 25-hydroxyvitamin D in children affected by VKC. In addition, the VKC-children tended to spend less time outdoors during daylight compared to controls (160.7 ± 65.9 vs. 229.5 ± 101.2 min), suggesting that a reduced level of vitamin D may play a role. In addition, a statistically significant correlation was observed between serum 25-hydroxyvitamin D levels and time spent outdoors [163].
Severe VKC is often treated using immunomodulatory drugs, such as cyclosporine or tacrolimus [164]. Furthermore, studies indicate that treatment with 1% cyclosporine or 0.1% tacrolimus as eye drops may contribute to the improvement of VKC signs and symptoms, and that these changes are associated with an increase of 25-hydroxyvitamin D level in serum. This rise was higher in the children with limbal VKC than the tarsal form and could result from the fact that limbal VKC is less symptomatic [161,165]. The above data require confirmation and verification through large-scale clinical trials; however, their findings may provide a greater insight into the pathogenesis of VKC and creation of customized therapy.
4.15. Keratoconus
Keratoconus is a common, progressive, ectatic, degenerative disease of the cornea. It manifests as a thin cone resulting in refractive errors, such as irregular astigmatism or myopia, with impairment of visual acuity. Although the detailed pathogenesis of keratoconus formation remains unclear, environmental and genetic factors are believed to have an important role, and proposed mechanisms include inflammatory reaction, oxidative stress and proteolytic degradation in the corneal stroma [166,167].
Recent data suggest that keratoconus may be also associated with disturbances of the immune system, and the systemic inflammatory response related to autoimmune diseases can induce the onset of eye disease [168]. As vitamin D is known to have immunomodulating properties [169], some studies have attempted to identify a relationship between its level and the onset of keratoconus. One study found that patients with keratoconus had significantly decreased serum levels of vitamin D compared to age- and sex-matched controls; however, no statistically significant correlation was found between 25-hydroxyvitamin D concentrations and keratoconus severity, based on Pentacam measurements including anterior curvature [170]. Similarly, Zarei-Ghanavati et al. (2020) reported that although severe keratoconus (Krumeich criteria stage IV) was associated with the lowest level of 25-hydroxyvitamin D, no significant differences were observed among individual groups of patients [171].
Reduced vitamin D levels have been found to significantly increase the probability of non-progressive and progressive keratoconus compared to controls by 1.23 and 1.29 times, respectively. Nevertheless, despite both groups demonstrating significantly lower concentrations of vitamin D in comparison to controls, no significant differences were found between non-progressive and progressive disease [172].
There is clearly a need for further studies investigating the potential relationship between keratoconus and vitamin D and to determine whether vitamin D supplementation may prevent or inhibit the course of disease.
4.16. Pterygium
Pterygium is a chronic disease of the anterior segment of the eye characterized by benign, uncontrolled, fibrovascular growth of the bulbar conjunctiva across the cornea, leading to impairment of visual acuity [173,174]. Its pathophysiology is not fully known. Inflammation and angiogenesis are considered important in the course of disease. However, chronic exposure to ultraviolet light is believed to have a significant causative relationship with pterygium. Moreover, a strong link has been evidenced between disease and geographical latitude: the prevalence of pterygium is inversely associated with latitude, indicating that ultraviolet radiation in the development of this eye disorders. This may also indirectly suggest that vitamin D plays a role in the formation of pterygium [175,176,177,178].
This was confirmed by Jee et al. (2016), who found that patients with pterygium had higher serum levels of 25-hydorxyvitamin D even after controlling for sunlight exposure time, and these changes were statistically significant. This positive association was found for both sexes. Nevertheless, it must be emphasized that despite significant difference between the patients with and without pterygium, those with eye disease had vitamin D insufficiency, with a mean serum 25-hydroxyvitamin D level of 20.4 ng/mL [179].
These results were later confirmed by another group, who showed significantly higher serum levels of 25-hydroxyvitamin D to be present in men with pterygium compared to healthy male controls. Importantly, the men with pterygium with more outdoor activity had more elevated concentrations than those with dominant indoor activity. No such relationship was observed in controls, indicating that vitamin D has a potential role in the development of pterygium. However, no such differences were found between female patients and healthy subjects [180]. Another study examined the relationship between pterygium, sun exposure, and serum 25-hydroxyvitamin D level in South Korean adults. The frequency of pterygium was found to be increased in elderly subjects and those who lived at low geographical latitudes. In addition, these patients had higher serum levels of 25-hydroxyvitamin D, suggesting that this may be positively correlated with the prevalence of pterygium [178]. However, a recent study in 2021 did not identify any changes in vitamin D concentration in both serum and tear fluid between the subjects with pterygium and healthy subjects [181]. None of the trials mentioned above evaluated or described the mechanisms underlying the relationship between vitamin D and pterygium. Although vitamin D has pro-health properties, including anti-inflammatory activities, it appears to have an insufficient impact on pterygium to prevent disease. Furthermore, many studies have not compared vitamin D concentration with characteristics of pterygium, such as length or histopathological evaluation. Therefore, further clinical trials are warranted.
Interestingly, a recent study did not find any difference between patients with pterygium and healthy subjects with regard to serum vitamin D level; however, VDR protein expression was found to be elevated in endothelial cells of micro-vessels, subepithelial stromal and intravascular inflammatory cells associated with pterygium compared to adjacent healthy conjunctival tissue [182]. Immunohistochemical assays found VDR localization to differ significantly in the pterygium cells compared to normal conjunctival cells. In healthy conjunctiva, VDR was localized mainly in the cytoplasm, while in pterygium cells, VDR was co-localized in the nucleus and cytoplasm. Hence, the nuclear signaling pathways related to VDR may be engaged in the pathogenesis of pterygium [183]. Further analyses and clinical trials are needed to standardize the role of VDR in pathogenesis and the development of pterygium.
4.17. Thyroid Eye Disease (TED)
Graves’ disease, the most common cause of thyrotoxicosis, is an autoimmune disease affecting the thyroid gland. It is characterized by the presence of autoantibodies directed against antigens in the thyroid. These may cross-react with orbital antigens leading to TED, known also as Graves orbitopathy or thyroid-related orbitopathy. It is an inflammatory-fibrotic orbitopathy that includes orbital tissues, mainly extraocular muscles and orbital fat, causing diplopia, photophobia, exposure keratopathy and eye pain; if left untreated, the condition can generate compressive optic neuropathy [184,185].
Studies indicate that the vitamin D insufficiency may contribute to disturbances in immune system activity, which is an important factor in the development of autoimmune diseases [121]. Meta-analyses indicates that low vitamin D levels are related to the occurrence of Graves’ disease, a lower likelihood of remission and a higher recurrence rate [186,187]. Decreased serum concentrations of 25-hydroxyvitamin D have also been noticed in patients with TED. A retrospective study by Sadaka et al. (2019) found that 20% of TED-patients had vitamin D deficiency (a level below 20 ng/mL), and 31% had insufficiency (a level between 20 and 29 ng/mL). However, these results were obtained using a relatively small sample size, and no correlation was made with clinical disease activity or with an unaffected cohort [188].
Assessment of vitamin D level and its supplementation may play an important role in the early management of Graves’ disease by preventing the development of TED. Patients with Graves’ disease concomitant with TED have lower serum levels of 25-hydroxyvitamin D compared to those with Graves’ disease but without TED [189]. Research efforts are now directed toward identifying characteristics, including gene polymorphisms, which could modify the risk of TED and be associated with its occurrence; these could be used to facilitate early diagnosis. Maciejewski et al. (2020) found a C gene polymorphism rs2228570 (FokI) in VDR to occur more frequently in patients compared to unaffected subjects; this may be a risk factor contributing to the development of TED in patients of Caucasian origin with Graves’ disease [190].
4.18. Benign Essential Blepharospasm (BEB)
BEB is a cranial dystonia characterized by hyperactivity and sustained, involuntary spasms of muscles around the eyes, such as orbicularis oculi, corrugator and procerus. This ocular disorder affects approximately 1.4–13.3 cases per 100,000 people, mainly women, and the typical onset of the disease occurs between the fifth and seventh decades of life. Although the detailed causes of BEB remain unknown [191,192,193], they may be associated with disturbances in the regulation of intracellular and extracellular ionized calcium (Ca2+), an ion responsible for triggering muscle contraction [194]. Interestingly, patients with BEB demonstrate significantly lower serum calcium levels than healthy subjects [194]. This may indicate decreased vitamin D concentrations, whose deficiency is related to lowered ionized calcium levels and even hypocalcemia [195]. In one study, no significant differences in serum 25-hydroxyvitamin D level were found between BEB-patients and unaffected subjects, and only a moderate negative correlation was found between vitamin D levels and the severity of BEB based on the Jankovic score [194]. However, in another study, BEB patients demonstrated significantly lower 25-hydroxyvitamin D and calcium levels, which may suggest a potential cause of this disorder [196]. Further long-term prospective clinical trials are necessary to determine the role of vitamin D in the involvement of BEB pathophysiology.
5. Potential Mechanisms of the Vitamin D Action against Ocular Diseases
The ocular diseases described above have various risk factors, etiology and ethiopathogenesis. Inflammation, oxidative stress, angiogenesis, and apoptosis play an important role in the development of most of them [94,143,174]. It was shown that vitamin D was able to mitigate the inflammatory response mainly by inhibition of nuclear factor kappa B (NF-κB) signaling pathway, modulation of the immune cells activity and suppression of pro-inflammatory factor expression, such as cyclooxygenase-2 among others, resulting in a reduction of the prostaglandins level. In addition, vitamin D has been found to modulate apoptosis and downregulate the expression of vascular endothelial growth factor (VEGF) inhibiting angiogenesis [197]. Pro-health effects have also been confirmed for eye disorders. Vitamin D counteracted oxidative stress induced by hydrogen peroxide (H2O2) in human retinal pigment cells, and mitigated the inflammation induced by H2O2 through a decrease of the protein expression of interleukin (IL) 1β (IL-1β), IL-8, tumor necrosis factor alpha (TNF-α). Furthermore, the anti-inflammatory effect of vitamin D was confirmed in another in vitro model using lipopolysaccharide (LPS)-stimulated human retinal pigment epithelial cells. These data show that vitamin D may inhibit retinal diseases, such as AMD and DR, limiting inflammation [198,199]. The intraperitoneal administration of calcitriol and 22-oxacalcitriol significantly attenuated lesion volume in laser-induced choroidal neovascularization using a mouse model. Therefore, vitamin D and calcitriol analogues may have potential as an interventional treatment for ophthalmic neovascular indications [26]. In hyperosmotic stress-induced human corneal epithelial cells, calcitriol inhibited the reactive oxygen species (ROS)-NLR family pyrin domain containing 3 (NLRP3)-IL-1β signaling axis via activation of the Nrf2-antioxidant pathway, indicating that it may prevent and mitigate DES-related corneal inflammation and oxidative stress at an early stage [144]. Calcitriol is also able to prevent human corneal epithelial cells from apoptosis via activation of autophagy via the VDR pathway [146]. The potential therapeutic mechanism of calcitriol was also revealed in glaucoma. This compound attenuated oxidative stress-induced damage in human trabecular meshwork cells by inhibiting the transforming growth factor beta (TGF-β)-SMAD family member 3 (SMAD3)-VDR pathway [124]. On the other hand, VDR, including its activation and inhibition, may play an important role in the development and progression of ocular diseases. For example, inhibition of VDR exerted a protective role in high-level glucose-induced damage of retinal ganglion cells by activating the signal transducer and activator of the transcription 3 (STAT3) pathway, indicating the potential role of VDR in DR [200]. Mechanisms of vitamin D action in ocular diseases are complex and not fully known. It seems that cholecalciferol and calcitriol may exert anti-inflammatory, anti-oxidative and anti-angiogenic effects accompanied by a reduction of development and progression of ocular diseases. Nevertheless, further studies are necessary to explain the detailed mechanisms of vitamin D action in eye disorders and their association with the VDR activity.
6. Summary and Conclusions
Based on the papers included in this review, it appears that vitamin D level may be associated with a range of eye diseases, including DR, ON, RVO, myopia, UM, non-infectious uveitis, VKHD, glaucoma, cataract, scleritis, DES, VKC, keratoconus, pterygium, TED and BEB. Measurement of vitamin D level, primarily 25-hydroxyvitamin D, could be a practical marker of the clinical course and severity of some ocular disorders, or could even be used to predict their risk. The data described in this review indicate that vitamin D has some pro-health properties which can be used against the ocular diseases. Therefore, vitamin D may be an agent supporting the available treatment of eye disorders. For example, it has been suggested that deficiency of the vitamin D occurs in patients with Sjögren’s Syndrome-related dry eye, and this may result in a modulation of the clinical course [201]. That is why vitamin D may be considered as a modulator of the clinical course of ocular diseases. In addition, vitamin D may serve as marker of the advancement of the disease, since its level is correlated with severity of the symptoms [148]. Thus, vitamin D may be a tool in the diagnostic and therapeutic process, although further studies are required to confirm this. In addition, some VDR gene polymorphisms may serve as prognostic markers. Interestingly, calcitriol analogues appear to limit the development and progression of retinoblastoma.
The studies a described above have some limitations. First, vitamin D deficiency is becoming an increasing problem worldwide, and was observed in most study participants, even those without apparent disease. It is also not always clear whether vitamin D deficiency is the cause or consequence of a disorder, and the molecular mechanisms of vitamin D action remain poorly understood. Other significant limitations of the studies include the small number of patients, high heterogeneity of selected groups and variation in previous vitamin D supplementation. In addition, considerable variation has occurred in the methods used to measure vitamin D serum concentration, environmental conditions and individual factors (including sunlight exposure, physical activity). Most importantly, vitamin D levels vary seasonally, and this would affect the results depending on when the study was performed. Therefore, further randomized controlled trials are needed to clarify conflicting results.
Selected clinical studies and trials investigating the link between vitamin D, VDR and ocular diseases are summarized in Table 1.
Table 1.
Summary of clinical studies and trials investigating the relation between vitamin D and eye diseases.
| Type of Study/ClinicalTrials.gov Identifier/Phase (If Specified) | Participants/Enrollment/DeMographics of Population | Method | Findings | Ref |
|---|---|---|---|---|
| Age-related macular degeneration | ||||
| Case-control study | 161 neovascular AMD cases from two university hospitals and 369 population-based control subjects from a cohort study | Brief-type self-administered questionnaire on diet history, which required respondent recall of the usual intake of 58 foods during the preceding month | Logistic regression analysis showed that low intake of vitamin D was associated with neovascular AMD (Trend p < 0.002) | [32] |
| Clinical case–control pilot study | 96 Korean patients: 30 with late AMD, 32 with early AMD, and 34 normal controls | Measurement and comparison serum 25(OH)D levels | Serum vitamin D deficiency may elevate the risk of early (OR = 3.59; 95%CI 0.95–13.58; p = 0.06) and late AMD (OR = 3.61; 95%CI 1.04–12.51; p = 0.043) and may also be associated with subretinal fibrosis | [33] |
| Cross-sectional study | 95 patients with exudative AMD and 95 healthy age- and sex-matched controls | Measurement and comparison serum 25(OH)D levels | Significant lower 25(OH)D levels in patients with AMD compared to the control subjects (p = 0.042) | [34] |
| Population-based, cross-sectional study | 17,045 Korean subjects older than 40 years | Standardized interviews, evaluation of blood 25-(OH)D levels and comprehensive ophthalmic examinations | Inverse association between high level of blood 25(OH)D with late AMD in men but not women | [35] |
| Population-based, prospective analysis | 1225 (196 African American; 1029 Caucasian) | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Logistic regression showed that high 25(OH)D concentrations (>70 nM) may be associated with reduced odds of incident early AMD | [36] |
| Cross-sectional study | 1045 members with AMD and 8124 without AMD | Comparison of serum 25(OH)D levels between the two groups | No association was detected between 25(OH)D levels and the presence of AMD | [37] |
| Population-based study | 697 (264 men, 433 women) | Assessment of associations between AMD and plasma 25(OH)D status using generalized estimating equation logistic regressions | Lack of specific role of vitamin D in AMD | [38] |
| Meta-analysis | Literature database | Identification of the association between serum vitamin D levels and AMD risk | Lack of evidences to inverse association between serum vitamin D levels and any stages and subtypes of AMD risk | [39] |
| Population-based, cross-sectional study | 2137 without AMD, 2209 with early AMD, 150 with late AMD, of whom 104 with neovascular AMD | Comparison of serum 25(OH)D levels | No linear association between 25(OH)D and early or late AMD or neovascular AMD | [40] |
| Cross-sectional study | 9734 (7779 Caucasians, 1955 African American | Secondary data analysis of already existing data from the AtherosclerosisRisk in Communities Study | Lack of association between vitamin D status and early AMD | [41] |
| Pilot study | Treatment group with 15 subjects and control, group with 15 subjects | Measurement and comparison serum 25(OH)D levels | Lack of association between vitamin D status and AMD | [42] |
| Systematic review and meta-analysis | Literature database | Identification of the association between serum vitamin D levels and AMD risk | Lack of a definitive association between serum 25(OH)D and AMD risk | [43] |
| Nationwide, double-blind, placebo controlled randomized clinical trial | 25,871 | Supplementation of 2000 IU/day for a median 5.3 years | Lack of vitamin D supplementation on AMD incidence and progression | [45] |
| Diabetic retinopathy | ||||
| Cross-sectional study | 30 subjects with DR and 30 subjects without DR | Measurement and comparison serum 25(OH)D levels | Lower levels of serum 25(OH)D in DR | [47] |
| Cross-sectional study | 1790 | Measurement and comparison serum 25(OH)D levels | Association between DR and prevalence of vitamin D deficiency | [48] |
| Population-based cross-sectional study | 2113 participants aged ≤ 40 years | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Inverse association of blood 25(OH)D levels with any DR and proliferative DR only in men | [49] |
| Meta-analysis | Literature database | Identification of the association between serum vitamin D levels and DR | Statistically significant association between vitamin D deficiency and DR | [50] |
| Retrospective study | 3054 Asian Indians with type 2 diabetes mellitus | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Association between lower serum 25(OH)D and increased severity of DR. Association between vitamin D deficiency and two-fold increased risk for proliferative DR | [51] |
| Cross-sectional study | 638 patients with type 2 diabetes mellitus | Evaluation of blood 25-(OH)D levels and clinical examinations | Vitamin D deficiency is considered as a risk factor for DR | [52] |
| Cross-sectional study | 4767 diabetic patients | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Association between lower serum 25(OH)D and higher prevalence of DR in middle-aged and elderly diabetic adults | [53] |
| Clinic-based, cross-sectional study | 221subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Diabetic subjects, especially those with PDR, have lower 25(OH)D levels than those without diabetes | [54] |
| Hospital-based cross-sectional study | 889 type 2 diabetic patients with or without DR | Evaluation of blood 25-(OH)D levels and clinical examinations | Vitamin D deficiency is significantly associated with risk of proliferative DR | [55] |
| Cross-sectional study | 517 subjects aged 8–20 years with type 1 diabetes mellitus | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Association between the vitamin D deficiency and increased prevalence of DR in young people with type 1 diabetes mellitus | [56] |
| Meta-analysis | Literature database | Identification of the association between serum vitamin D levels and DR | Association between the vitamin D deficiency and increased risk of DR patients with type 2 diabetes mellitus | [57] |
| Retrospective study | 182 with type 1 diabetes mellitus | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Association between the vitamin D deficiency and increased prevalence of DR in patients with type 1 diabetes mellitus | [58] |
| Cross-sectional study | 460 patients with type 2 diabetes mellitus (median age 55.2 years; age range, 30–90 years; 227 male and 233 female) and 290 non-diabetic control subjects (median age 46.1 years; age range, 30–85 years; 151 male and 139 female) | Evaluation of blood 25-(OH)D, 1,25(OH)2D, 24,25(OH)2D levels and ophthalmic examinations | Association between vitamin D3 metabolites and DR, whereas lack of these dependence for total vitamin D levels | [60] |
| Tertiary care center based cross-sectional study | Diabetes mellitus without DR (24), non-proliferative DR (24), proliferative DR (24) and controls (24) | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Serum vitamin D levels of ≤ 18.6 ng/mL is marker for proliferative DR | [59] |
| Systematic review and meta-analysis | Literature database | Identification of the association between VDR gene polymorphisms and DR susceptibility | The VDR FokI gene variant is associated with DR | [66] |
| Meta-analysis | Literature database | Identification of the association between VDR gene polymorphisms and DR susceptibility | The VDR BsmI, ApaI and FokI gene variants are associated with DR susceptibility | [4] |
| Optic neuritis | ||||
| Placebo-controlled randomized clinical trial | 52 patients with confirmed unilateral ON aged 15–38 years and low serum 25(OH)D levels | Supplementation of 50,000 IU/week vitamin D3 or placebo for 6 months | Adding vitamin D to routine disease therapy had no significant effect on the thickness of RNFL or macula in patients with ON | [70] |
| Cross-sectional study | 164 patients with monosymptomatic ON and 948 patients with MS | Evaluation of blood 25-(OH)D levels and clinical examinations | Lack of correlation between levels of vitamin D and ON severity | [71] |
| Doubleblind, randomized, placebo-controlled pilot clinical trial | 30 patients with ON | Supplementation of 50,000 IU/week vitamin D3 or placebo for 12 months | Administration of vitamin D3 by patients with ON and low serum 25-(OH)D levels may delay the onset of a second clinical attack and the subsequent conversion to MS | [72] |
| Cross-sectional study | 74 patients with MS | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Lack of association between vitamin D deficiency and thinning of RNFL or macular volume in MS eyes unaffected by ON | [73] |
| Retinal vein occlusion | ||||
| Pilot study | 40 patients with RVO and 40 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Significant lower levels of serum 25(OH)D in RVO as compared to age matched controls | [77] |
| Case control study (NCT01793181) | 79 patents with CRVO and 144 control subjects | Evaluation of blood 25-(OH)D levels and clinical examinations | Patients under 75 years with CRVO had significantly lower 25(OH)D levels compared to the control | [78] |
| Myopia | ||||
| Study based on Korea National Health and Nutrition Examination Survey | 2038 Korean adolescent aged 13 to 18 years | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Decreased serum 25(OH)D level was associated with myopia prevalence in Korean adolescents | [81] |
| Study based on the Western Australian Pregnancy Cohort (Raine) Study | 221 patients with myopia, 725 nonmyopic subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Decreased serum 25(OH)D level was associated with myopia | [82] |
| Study based on Korea National Health and Nutrition Examination Survey | 15,126 Korean aged 20 years or older | Evaluation of blood 25-(OH)D levels, daily sun exposure time and ophthalmic examinations | Low serum 25(OH)D levels and shorter daily sun exposure time is independently associated with a high prevalence of myopia | [83] |
| Population-based prospective cohort study | 2666 children aged 6 years | Evaluation of blood 25-(OH)D levels, daily sun exposure time and ophthalmic examinations | Low serum 25(OH)D is associated with axial length and risk of myopia in young children | [84] |
| Systematic review and meta-analysis | Literature database | Identification of the association between serum vitamin D levels and myopia | Lower 25(OH)D is associated withincreased risk of myopia | [85] |
| Study based on Korea National Health and Nutrition Examination Survey | 25,199 subjects aged ≥ 20 years | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Serum 25(OH)D level was inversely associated with myopia in adults | [86] |
| Study based on the Avon Longitudinal Study of Parents and Children (ALSPAC) population-based birth cohort | Children participating in ALSPAC | Evaluation of total vitamin D, vitamin D3, vitamin D2 levels, time outdoors and ophthalmic examinations | Vitamin D may serve as biomarker for time spent outdoors without association with myopia | [87] |
| Mendelian randomization study based on meta-analysis of refractive error genome-wide association study | 37,382 and 8376 adult participants of European and Asian ancestry, respectively | Identification of the association between serum vitamin D levels and myopia | Contribution of vitamin D levels to degree of myopia is very small and indistinguishable from zero | [88] |
| Study based on the Busselton Healthy Ageing Study | Community-based cohort of adults aged 46 to 69 years | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | There was no substantial association between 25(OH)D levels and spherical equivalent or odds of myopia | [89] |
| Prospective, cross-sectional study | Children born prematurely between January 2010 and December 2011 when they reached school age between April 2017 and June 2018 | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | More time spent outdoors is associated with lower odds of myopia. The serum 25(OH)D concentration is not associated with myopia | [90] |
| Case-control study | 457 myopic male cases and 1280 emmetropic male controls | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | The myopia is not related to neonatal vitamin D status | [91] |
| Cross-sectional, population-based random study | 4166 participants 65 years and older | Evaluation of vitamin D3 levels, time outdoors and ophthalmic examinations | Increased UVB exposure is associated with reduced myopia | [92] |
| Systematic review and meta-analysis | Literature database | Identification of the association between time spent outdoor and myopia | Increased time outdoors is effective in preventing the onset of myopia as well as in slowing the myopic shift in refractive error. Outdoor time is not effective in slowing progression in eyes that were already myopic. | [93] |
| Non-infectious uveitis | ||||
| Prospective, multicenter, observational cohort study | 360 Patients ≤ 16 years of age with recently diagnosed JIA (< 12 months) | Evaluation of blood 25-(OH)D levels and clinical examinations | Vitamin D deficiency is associated with the risk for uveitis in juvenile idiopathic arthritis | [113] |
| Case-control study | 558 patients with non-infectious uveitis and 2790 control subjects | Evaluation of blood vitamin D levels and clinical examinations | Association between hypovitaminosis D and non-infectious uveitis | [114] |
| Case-control study | 100 patients with non-infectious anterior uveitis and 100 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Lower vitamin D levels are associated with an increased risk of non-infectious anterior uveitis | [115] |
| Observational case–control study | 20 patients with acute anterior uveitis and 100 consecutive, age and sex matched healthy subjects without any ocular or systemic diseases | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | The patients with acute anterior uveitis have decreased 25(OH)D level | [116] |
| Prospective case-control study | 74 patients with active uveitis and 77 patients with inactive uveitis | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Active uveitis is associated with significantly lower serum 25(OH)D levels than inactive uveitis | [117] |
| Retrospective case-control study | 333 patients with uveitis and 329 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Hypovitaminosis D is associated with increased risk of non-infectious uveitis | [118] |
| Monocentric retrospective cohort study | 59 patients with uveitis | Evaluation of blood 25-(OH)D, 1,25,(OH)D levels and ophthalmic examinations | High 1,25(OH)2D/25(OH)D ratio is useful for the diagnosis of sarcoidosis-related uveitis | [119] |
| Vogt-Koyanagi-Harada disease | ||||
| Case-control study | 25 patients with VKHD and 16 health subjects | Evaluation of blood 1,25(OH)2D levels and clinical examinations | Reduced expression of 1,25(OH)2D may be involved in the development of VKHD | [122] |
| Case-control study | 39 patients with VKHD and 50 control subjects | Sequencing analysis of the VDR, CYP24A1, CYP27B1 and CYP2R1 genes (involved in the metabolism of vitamin D) | Detection of potentially pathogenic sequence variant in CYP2R1 may cause VKH in a subset of patients | [123] |
| Glaucoma | ||||
| Case-control and an intervention study | 39 received vitamin D supplements, 39 received placebo and 42 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations; Supplementation of 40000 IU/week vitamin D3 or placebo for 6 months for participants with low vitamin D level | No difference between IOP and low/high serum 25(OH)D levels. No significant difference between experimental and control groups | [126] |
| Cross-sectional study | 6094 | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Vitamin D deficiency Seems to be independent risk factor for open-angle glaucoma | [127] |
| Case-control study | 150 patients with glaucoma and 164 health subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Serum vitamin D status is associated with the presence but not the severity of primary open angle glaucoma | [128] |
| Cross-sectional and observational study | 20 patients with glaucoma and 20 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Serum Vitamin D level is statistically significantly lower in glaucoma | [129] |
| Case-control study | 73 with glaucoma and 71 age-matched control subjects | Evaluation of blood calcitriol levels and ophthalmic examinations | Decreased calcitriol levels in glaucoma | [130] |
| Case-control study | 357 patients with glaucoma and 178 control subjects of African descent | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Association between the level of 25-(OH)D and glaucoma severity | [131] |
| Cataract | ||||
| Case-control study | 325 patients with cataract and 385 control subjects | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Association of Serum 25(OH)D deficiency and age-related cataract | [134] |
| Observational cross-sectional study based on Korea National Health and Nutrition Examination Survey | 18804 | Evaluation of blood 25(OH)D levels and ophthalmic examinations | The age-related cataract risk is decreased in men with higher serum 25(OH)D levels | [135] |
| Case control study | 37 patients with cataract and 53 health subjects under the age of 60 years | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Vitamin D deficiency is associated with early age-related cataract | [136] |
| Study based on the Carotenoid Age-Related Eye Study | 1278 | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Inverse association between serum 25(OH)D and nuclear cataract in women younger than 70 years | [137] |
| Study based on Korea National Health and Nutrition Examination Survey | 16,086 (7093 males and 8993 females) adults aged 40 years or older | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Serum 25(OH)D levels are inversely associated with the risk of nuclear cataract | [138] |
| Retrospective chart review study | 195 | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Vitamin D deficiency is associated with posterior subcapsular cataract | [139] |
| Prospective hospital-based cross-sectional study | 79 patients with posterior subcapsular cataract or age-related cataract without posterior subcapsular cataract component | Evaluation of blood vitamin D levels and ophthalmic examinations | Posterior subcapsular cataract is not associated with vitamin D insufficiency | [140] |
| Prospective study | 87 patients with senile cataract and 49 patients with diabetic cataract | Evaluation of blood and aqueous humor 25(OH)D levels and ophthalmic examinations | Higher 25(OH)D level in aqueous humor is associated with diabetic cataract | [141] |
| Scleritis | ||||
| Retrospective case-control study | 103 patients with scleritis and 329 control subjects | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Hypovitaminosis D is associated with increased risk of scleritis | [118] |
| Dry eye syndrome | ||||
| Systematic review and meta-analysis | Literature database | Identification of the association between vitamin D level and DES | Significantly lowered serum level of 25(OH)D in DES | [147] |
| Systematic review and meta-analysis | Literature database | Identification of the association between vitamin D level and DES | Vitamin D deficiency is associated with severity of DES | [148] |
| Systematic review and meta-analysis | Literature database | Identification of the association between vitamin D level and DES | Vitamin D deficiency may be a risk factor for DES | [149] |
| Study based on Korea National Health and Nutrition Examination Survey | 17,542 adults (7434 men and 10,108 women) aged 19 years | Evaluation of blood 25(OH) levels and clinical examinations | Decreased serum 25(OH)D levels and inadequate sunlight exposure are associated with DES. The vitamin D supplementation may be useful in DES treatment | [150] |
| Cross-sectional study | 47 patients with evaporative DES and 33 control subjects | Evaluation of blood/tear 25(OH) levels and clinical examinations | Significantly lowered tear level of 25(OH)D in DES | [151] |
| Observational study | 34 patients with vitamin D deficiency and 21 control subjects with normal level of vitamin D | Evaluation of blood/tear 25(OH) levels and ophthalmic examinations | Vitamin D deficiency results in the TBUT and Schirmer’s test values | [152] |
| Single-center, cross-sectional observational study | 30 patients with vitamin D deficiency and 30 control subjects with normal level of vitamin D | Evaluation of blood/tear 25(OH) levels and ophthalmic examinations | Vitamin D deficiency is associated with tear hyperosmolarity and tear film dysfunction | [153] |
| Retrospective observational study | 79 patients (22 male and 57 female) | Evaluation of blood 25(OH)D levels and ophthalmic examinations | Tear break-up time and tear secretion were correlated with serum vitamin D levels | [154] |
| Study based on Korea National Health and Nutrition Examination Survey | 16,396 participants aged >19 years | Evaluation of blood 25(OH)D levels and ophthalmic examinations | There is no association between 25(OH)D levels and DES | [155] |
| Study based on Study Group for Environmental Eye Disease | 740 subjects (253 men and 487 women) | Evaluation of blood 25(OH)D levels and ophthalmic examinations | There is no association between 25(OH)D levels and DES | [156] |
| Observational study | 105 (21 men and 84 women) with mean serum 25(OH)D level of 10.52 ± 4.61 ng/mL | Evaluation of blood 25-(OH)D levels and ophthalmic examinations; Intramuscular injection of 200,000 IU cholecalciferol for participants with deficient or insufficient vitamin D level | The supplementation of vitamin D is effective and useful in the treatment of patients with DES | [157] |
| Retrospective, observational study | 116 patients with DES | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | The effect of topical artificial tears and hyaluronate in the therapy of DES is dependent on serum 25(OH)D levels. The cholecalciferol supplementation enhanced the efficacy of topical DES treatment | [158] |
| Case-control study | 64 patients with DES and 51 control subjects | Identification of the association between VDR gene polymorphisms and DES susceptibility | Two polymorphisms (Foklrs2228570 and Apal-rs7975232) in the VDR gene are 1.72 and 1.66 times more likely in DES-patients than in control, respectively | [22] |
| Vernal keratoconjunctivitis | ||||
| Case-control study | 47 patients with VKC, aged between 5 and 12 years, and 63 healthy children | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Children affected by VKC have lower vitamin D levels. Significant correlation between the disease severity and the level of vitamin D | [161] |
| Prospective, observational, caseـcontrol study | 39 patients with VKC (21 men and 18 women) and 32 health subjects (19 men and 13 women) with the mean age of 18.38 ± 8.83 and 21.6 ± 9.43, respectively | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Patients with VKC have lower vitamin D levels; No significant reverse correlation between the disease severity and the level of vitamin D | [162] |
| Prospective, single-centered, observational, case–control study | 29 children with VKC and 62 health children | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Children with VKC should be evaluated for vitamin D deficiency, which might occur secondary to sun avoidance | [163] |
| Observational study | 242 children with VKC | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Ocular treatment using immunomodulatory eye drops results in an improvement in 25OHD serum levels | [165] |
| Keratoconus | ||||
| Prospective, single-centered, observational case-control study | 100 patients with keratoconus and 100 health control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Patients with KC had reduced serum vitamin D levels compared to age- and sex-matched healthy controls | [170] |
| Cross-sectional study | 100 patients with keratoconus and 100 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Lower serum 25(OH)D was found in patients with keratoconus compared to the control group | [171] |
| 55 patients with keratoconus (28 progressive and 27 non-progressive) and 30 age- and sex-matched control subjects | Evaluation of blood vitamin D levels and ophthalmic examinations | Serum vitamin D evaluation in patients with keratocnous at onset and follow-up examinations may help to predict the course of the disease | [172] | |
| Pterygium | ||||
| Study based on Korea National Health and Nutrition Examination Survey | 19,178 participants aged 30 years | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Positive association between blood 25(OH)D levels and pterygium | [179] |
| Prospective study | 63 patients with pterygium and 58 control subjects | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Increased level of blood 25(OH)D in only male subjects with pterygium and in those with more outdoor activity | [180] |
| Population-based, cross-sectional study based on Korea National Health and Nutrition Examination Survey | 12,258 adults (aged ≥ 19 years) | Evaluation of blood 25-(OH)D levels and ophthalmic examinations | Association of daily sun exposure and serum 25(OH)D levels in pterygium | [178] |
| Case-control study | 35 (21 male, 14 female) patients with unilateral pterygium and 25 (18 male, 7 female) healthy controls | Evaluation of blood/tear vitamin D levels and ophthalmic examinations | Tear fluid and serum vitamin D concentrations do not have a role in pterygium pathogenesis | [181] |
| Cross-sectional study | 50 patients with pterygium and 50 control subjects | Identification of the VDR gene expression in pterygium; Identification of the VDR gene polymorphisms and DES susceptibility | VDR expression is increased in thepterygium tissue compared to the adjacent healthy tissue. No significant difference in BsmI, FokI and TaqI polymorphisms in comparison to the control | [182] |
| Thyroid eye disease | ||||
| Retrospective chart review | 35 patients with TED | Evaluation of blood 25-(OH)D levels and clinical examinations | 20% prevalence of vitamin D deficiency in TED | [188] |
| Retrospective case-control study | 89 TED patients and 89 Graves disease patients without TED, and 2 healthy control groups matched 4:1 to the cases; 356 health control patients matched to the TED group and 356 health control patients matched to the Graves disease | Evaluation of blood 25-(OH)D levels and clinical examinations | Low serum vitamin D is associated with TED diagnosis | [189] |
| Case-control study | 108 patients with thyroid-associated orbitopathy and 130 health control subjects (Caucasian Polish origin) | Identification of the VDR gene polymorphisms and thyroid-associated orbitopathy susceptibility | C allele of rs2228570 VDR gene polymorphism may contribute to the development of thyroid-associated orbitopathy | [190] |
| Benign essential blepharospasm | ||||
| Prospective study | 50 patients with BEB and 22 health subjects | Evaluation of blood 25-(OH)D levels and clinical examinations | Serum vitamin D levels showed a moderate negative correlation with disease severity | [194] |
| Retrospective case-control study | 20 patients with BEB and 20 age- and gender-matched health subjects | Evaluation of blood 25-(OH)D levels and clinical examinations | Strong negative correlation between disease severity and reduced 25(OH) vitamin D in patients with BEB | [196] |
Acknowledgments
The study was supported by grant No. 503/1-156-04/503-11-001-19-00 from the Medical University of Lodz, Poland.
Abbreviations
AMD, age-related macular degeneration; DES, dry eye syndrome; DR, diabetic retinopathy; IOP, intraocular pressure; ON, optic neuritis; RVO, retinal vein occlusion; UM, uveal melanoma; VDR, vitamin D receptor; VKC, vernal keratoconjunctivitis; VKHD, Vogt-Koyanagi-Harada disease.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bourne R.R.A., Flaxman S.R., Braithwaite T., Cicinelli M.V., Das A., Jonas J.B., Keeffe J., Kempen J., Leasher J., Limburg H., et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob. Health. 2017;5:e888–e897. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 2.Köberlein J., Beifus K., Schaffert C., Finger R.P. The economic burden of visual impairment and blindness: A systematic review. BMJ Open. 2013;3:e003471. doi: 10.1136/bmjopen-2013-003471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bahrami B., Hong T., Gilles M.C., Chang A. Anti-VEGF therapy for diabetic eye diseases. Asia-Pacific J. Ophthalmol. 2017;6:535–545. doi: 10.22608/APO.2017350. [DOI] [PubMed] [Google Scholar]
- 4.Moore N.A., Bracha P., Hussain R.M., Morral N., Ciulla T.A. Gene therapy for age-related macular degeneration. Expert Opin. Biol. Ther. 2017;17:1235–1244. doi: 10.1080/14712598.2017.1356817. [DOI] [PubMed] [Google Scholar]
- 5.Holick M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. 2017;18:153–165. doi: 10.1007/s11154-017-9424-1. [DOI] [PubMed] [Google Scholar]
- 6.Xu Z., Sun T., Li W., Sun X. Inhibiting effects of dietary polyphenols on chronic eye diseases. J. Funct. Foods. 2017;39:186–197. doi: 10.1016/j.jff.2017.10.031. [DOI] [Google Scholar]
- 7.Bungau S., Abdel-Daim M.M., Tit D.M., Ghanem E., Sato S., Maruyama-Inoue M., Yamane S., Kadonosono K. Health Benefits of Polyphenols and Carotenoids in Age-Related Eye Diseases. Oxid. Med. Cell. Longev. 2019;2019:9783429. doi: 10.1155/2019/9783429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ikonne E.U., Ikpeazu V.O., Ugbogu E.A. The potential health benefits of dietary natural plant products in age related eye diseases. Heliyon. 2020;6:e04408. doi: 10.1016/j.heliyon.2020.e04408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plum L.A., Deluca H.F. Vitamin D, disease and therapeutic opportunities. Nat. Rev. Drug Discov. 2010;9:941–955. doi: 10.1038/nrd3318. [DOI] [PubMed] [Google Scholar]
- 10.Prietl B., Treiber G., Pieber T.R., Amrein K. Vitamin D and immune function. Nutrients. 2013;5:2502–2521. doi: 10.3390/nu5072502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bizzaro G., Antico A., Fortunato A., Bizzaro N. Vitamin D and autoimmune diseases: Is vitamin D receptor (VDR) polymorphism the culprit? Isr. Med. Assoc. J. 2017;19:438–443. [PubMed] [Google Scholar]
- 12.Reins R.Y., McDermott A.M. Vitamin D: Implications for ocular disease and therapeutic potential. Exp. Eye Res. 2015;134:101–110. doi: 10.1016/j.exer.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bikle D.D. Vitamin D metabolism, mechanism of action, and clinical applications. Chem. Biol. 2014;21:319–329. doi: 10.1016/j.chembiol.2013.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alsalem J.A., Patel D., Susarla R., Coca-Prados M., Bland R., Walker E.A., Rauz S., Wallace G.R. Characterization of vitamin D production by human ocular barrier cells. Investig. Ophthalmol. Vis. Sci. 2014;55:2140–2147. doi: 10.1167/iovs.13-13019. [DOI] [PubMed] [Google Scholar]
- 15.Rullo J., Pennimpede T., Mehraban Far P., Strube Y.N., Irrcher I., Urton T., Bona M., Gonder T., Campbell R.J., ten Hove M., et al. Intraocular calcidiol: Uncovering a role for vitamin D in the eye. J. Steroid Biochem. Mol. Biol. 2020;197:105536. doi: 10.1016/j.jsbmb.2019.105536. [DOI] [PubMed] [Google Scholar]
- 16.Romagnoli E., Mascia M.L., Cipriani C., Fassino V., Mazzei F., D’Erasmo E., Carnevale V., Scillitani A., Minisola S. Short and long-term variations in serum calciotropic hormones after a single very large dose of ergocalciferol (vitamin D2) or cholecalciferol (vitamin D3) in the elderly. J. Clin. Endocrinol. Metab. 2008;93:3015–3020. doi: 10.1210/jc.2008-0350. [DOI] [PubMed] [Google Scholar]
- 17.Tripkovic L., Lambert H., Hart K., Smith C.P., Bucca G., Penson S., Chope G., Hyppönen E., Berry J., Vieth R., et al. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2012;95:1357–1364. doi: 10.3945/ajcn.111.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bikle D. Nonclassic actions of vitamin D. J. Clin. Endocrinol. Metab. 2009;94:26–34. doi: 10.1210/jc.2008-1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haussler M.R., Whitfield G.K., Kaneko I., Haussler C.A., Hsieh D., Hsieh J.C., Jurutka P.W. Molecular mechanisms of vitamin D action. Calcif. Tissue Int. 2013;92:77–98. doi: 10.1007/s00223-012-9619-0. [DOI] [PubMed] [Google Scholar]
- 20.Yin Z., Pintea V., Lin Y., Hammock B.D., Watsky M.A. Vitamin D enhances corneal epithelial barrier function. Investig. Ophthalmol. Vis. Sci. 2011;52:7359–7364. doi: 10.1167/iovs.11-7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong Y.J., Kang E.S., Ji M.J., Choi H.J., Oh T., Koong S.S., Jeon H.J. Association between Bsm1 polymorphism in vitamin D receptor gene and diabetic retinopathy of type 2 diabetes in Korean population. Endocrinol. Metab. 2015;30:469–474. doi: 10.3803/EnM.2015.30.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hallak J.A., Tibrewal S., Mohindra N., Gao X., Jain S. Single nucleotide polymorphisms in the BDNF, VDR, and DNASE 1 genes in dry eye disease patients: A case-control study. Investig. Ophthalmol. Vis. Sci. 2015;56:5990–5996. doi: 10.1167/iovs.15-17036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Obiol D.J., Martínez A., Ferronato M.J., Quevedo M.A., Grioli S.M., Alonso E.N., Gómez G., Fall Y., Facchinetti M.M., Curino A.C. Novel calcitriol analogue with an oxolane group: In vitro, in vivo, and in silico studies. Arch. Pharm. 2019;352:e1800315. doi: 10.1002/ardp.201800315. [DOI] [PubMed] [Google Scholar]
- 24.Cardús A., Panizo S., Parisi E., Fernandez E., Valdivielso J.M. Differential effects of vitamin D analogs on vascular calcification. J. Bone Miner. Res. 2007;22:860–866. doi: 10.1359/jbmr.070305. [DOI] [PubMed] [Google Scholar]
- 25.Kutuzova G.D., Gabelt B.T., Kiland J.A., Hennes-Beann E.A., Kaufman P.L., Deluca H.F. 1α,25-Dihydroxyvitamin D 3 and its analog, 2-methylene-19-nor-(20S)-1α,25-dihydroxyvitamin D 3 (2MD), suppress intraocular pressure in non-human primates. Arch. Biochem. Biophys. 2012;518:53–60. doi: 10.1016/j.abb.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merrigan S.L., Park B., Ali Z., Jensen L.D., Corson T.W., Kennedy B.N. Calcitriol and non-calcemic Vitamin D analogue, 22-oxacalcitriol, attenuate developmental and pathological choroidal vasculature angiogenesis ex vivo and in vivo. Oncotarget. 2020;11:493–509. doi: 10.18632/oncotarget.27380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Zamil W.M., Yassin S.A. Recent developments in age-related macular degeneration: A review. Clin. Interv. Aging. 2017;12:1313–1330. doi: 10.2147/CIA.S143508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell P., Liew G., Gopinath B., Wong T.Y. Age-related macular degeneration. Lancet. 2018;392:1147–1159. doi: 10.1016/S0140-6736(18)31550-2. [DOI] [PubMed] [Google Scholar]
- 29.Kaarniranta K., Pawlowska E., Szczepanska J., Jablkowska A., Blasiak J. Can vitamin D protect against age-related macular degeneration or slow its progression? Acta Biochim. Pol. 2019;66:147–158. doi: 10.18388/abp.2018_2810. [DOI] [PubMed] [Google Scholar]
- 30.Uro M., Beauchet O., Cherif M., Graffe A., Milea D., Annweiler C. Age-related Vitamin D deficiency is associated with reduced macular ganglion cell complex: A cross-sectional high-definition optical coherence tomography study. PLoS ONE. 2015;10:e0130879. doi: 10.1371/journal.pone.0130879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Millen A.E., Meyers K.J., Liu Z., Engelman C.D., Wallace R.B., LeBlanc E.S., Tinker L.F., Iyengar S.K., Robinson J.G., Sarto G.E., et al. Association between vitamin D status and age-related macular degeneration by genetic risk. JAMA Ophthalmol. 2015;133:1171–1179. doi: 10.1001/jamaophthalmol.2015.2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aoki A., Inoue M., Nguyen E., Obata R., Kadonosono K., Shinkai S., Hashimoto H., Sasaki S., Yanagi Y. Dietary n-3 Fatty Acid, α-Tocopherol, Zinc, Vitamin D, Vitamin C, and β-carotene are Associated with Age-Related Macular Degeneration in Japan. Sci. Rep. 2016;6:20723. doi: 10.1038/srep20723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim K.L., Park S.P. Association between serum vitamin D deficiency and age-related macular degeneration in Koreans: Clinical case-control pilot study. Medicine. 2018;97:e11908. doi: 10.1097/MD.0000000000011908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kan E., Kan E.K., Yücel Ö.E. The possible link between vitamin D levels and exudative age-related macular degeneration. Oman Med. J. 2020;35:e83. doi: 10.5001/omj.2020.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim E.C., Han K., Jee D. Inverse relationship between high blood 25-hydroxyvitamin D and late stage of age-related macular degeneration in a representative Korean population. Investig. Ophthalmol. Vis. Sci. 2014;55:4823–4831. doi: 10.1167/iovs.14-14763. [DOI] [PubMed] [Google Scholar]
- 36.Millen A.E., Nie J., Mares J.A., Lutsey P.L., Lamonte M.J., Meuer S.M., Sahli M.W., Andrews C.A., Klein B.E.K., Klein R. Serum 25-hydroxyvitamin D concentrations and incidence of age-related macular degeneration: The atherosclerosis risk in communities study. Investig. Ophthalmol. Vis. Sci. 2019;60:1362–1371. doi: 10.1167/iovs.18-25945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Golan S., Shalev V., Treister G., Chodick G., Loewenstein A. Reconsidering the connection between vitamin D levels and age-related macular degeneration. Eye. 2011;25:1122–1129. doi: 10.1038/eye.2011.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cougnard-Grégoire A., Merle B.M.J., Korobelnik J.F., Rougier M.B., Delyfer M.N., Féart C., Le Goff M., Dartigues J.F., Barberger-Gateau P., Delcourt C. Vitamin D deficiency in community-dwelling elderly is not associated with age-related macular degeneration. J. Nutr. 2015;145:1865–1872. doi: 10.3945/jn.115.214387. [DOI] [PubMed] [Google Scholar]
- 39.Wu W., Weng Y., Guo X., Feng L., Xia H., Jiang Z., Lou J. The association between serum vitamin D levels and agerelated macular degeneration: A systematic meta-analytic review. Investig. Ophthalmol. Vis. Sci. 2016;57:2168–2177. doi: 10.1167/iovs.15-18218. [DOI] [PubMed] [Google Scholar]
- 40.McKay G.J., Young I.S., McGinty A., Bentham G.C.G., Chakravarthy U., Rahu M., Seland J., Soubrane G., Tomazzoli L., Topouzis F., et al. Associations between Serum Vitamin D and Genetic Variants in Vitamin D Pathways and Age-Related Macular Degeneration in the European Eye Study. Ophthalmology. 2017;124:90–96. doi: 10.1016/j.ophtha.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 41.Millen A.E., Nie J., Sahli M.W., Mares J.A., Meyers K.J., Klein B.E.K., Lamonte M.J., Lutsey P.L., Andrews C.A., Klein R. Vitamin D status and prevalent early age-related macular degeneration in African Americans and Caucasians: The Atherosclerosis Risk in Communities (ARIC) Study. J. Nutr. Health Aging. 2017;21:772–780. doi: 10.1007/s12603-016-0827-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hashemi R., Bandarian M., Abedi-Taleb E., Khojasteh H., Khedmat L., Asadollahi E., Beytollahi M., Jelodar A.M. The association between blood vitamins D and e with age-related macular degeneration: A pilot study. Interv. Med. Appl. Sci. 2018;10:127–132. doi: 10.1556/1646.10.2018.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ferreira A., Silva N., Furtado M.J., Carneiro Â., Lume M., Andrade J.P. Serum vitamin D and age-related macular degeneration: Systematic review and meta-analysis. Surv. Ophthalmol. 2021;66:183–197. doi: 10.1016/j.survophthal.2020.07.003. [DOI] [PubMed] [Google Scholar]
- 44.Christen W.G., Cook N.R., Manson J.E., Buring J.E., Chasman D.I., Lee I.M., Bubes V., Li C., Haubourg M., Schaumberg D.A. Effect of Vitamin D and ω-3 Fatty Acid Supplementation on Risk of Age-Related Macular Degeneration: An Ancillary Study of the VITAL Randomized Clinical Trial. JAMA Ophthalmol. 2020;138:1280–1289. doi: 10.1001/jamaophthalmol.2020.4409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheung N., Mitchell P., Wong T.Y. Diabetic retinopathy. Lancet. 2010;376:124–136. doi: 10.1016/S0140-6736(09)62124-3. [DOI] [PubMed] [Google Scholar]
- 46.Lechner J., O’Leary O.E., Stitt A.W. The pathology associated with diabetic retinopathy. Vision Res. 2017;139:7–14. doi: 10.1016/j.visres.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 47.Afarid M., Ghattavi N., Johari M. Serum Levels of Vitamin D in Diabetic Patients with and without Retinopathy. J. Ophthalmic Vis. Res. 2020;15:172–177. doi: 10.18502/jovr.v15i2.6734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Patrick P.A., Visintainer P.F., Shi Q., Weiss I.A., Brand D.A. Vitamin D and retinopathy in adults with diabetes mellitus. Arch. Ophthalmol. 2012;130:756–760. doi: 10.1001/archophthalmol.2011.2749. [DOI] [PubMed] [Google Scholar]
- 49.Jee D., Do Han K., Kim E.C. Inverse association between high blood 25-hydroxyvitamin D levels and diabetic retinopathy in a representative Korean population. PLoS ONE. 2014;9:e115199. doi: 10.1371/journal.pone.0115199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang J., Upala S., Sanguankeo A. Relationship between vitamin D deficiency and diabetic retinopathy: A meta-analysis. Can. J. Ophthalmol. 2017;52:S39–S44. doi: 10.1016/j.jcjo.2017.09.026. [DOI] [PubMed] [Google Scholar]
- 51.Ashinne B., Rajalakshmi R., Anjana R.M., Venkat Narayan K.M., Jayashri R., Mohan V., Hendrick A.M. Association of serum vitamin D levels and diabetic retinopathy in Asian Indians with type 2 diabetes. Diabetes Res. Clin. Pract. 2018;139:308–313. doi: 10.1016/j.diabres.2018.02.040. [DOI] [PubMed] [Google Scholar]
- 52.Bener A., Eliaçik M., Cincik H., Öztürk M., Defronzo R.A., Abdul-Ghani M. The Impact of Vitamin D Deficiency on Retinopathy and Hearing Loss among Type 2 Diabetic Patients. Biomed Res. Int. 2018;2018:2714590. doi: 10.1155/2018/2714590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wan H., Wang Y., Zhang K., Chen Y., Fang S., Zhang W., Wang C., Li Q., Xia F., Wang N., et al. Associations between Vitamin D and microvascular complications in middle-aged and elderly diabetic patients. Endocr. Pract. 2019;25:809–816. doi: 10.4158/EP-2019-0015. [DOI] [PubMed] [Google Scholar]
- 54.Payne J.F., Ray R., Watson D.G., Delille C., Rimler E., Cleveland J., Lynn M.J., Tangpricha V., Srivastava S.K. Vitamin D insufficiency in diabetic retinopathy. Endocr. Pract. 2012;18:185–193. doi: 10.4158/EP11147.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yuan J., Zhou J.B., Zhao W., Zhang R.H., Cai Y.H., Shu L.P., Qi L., Yang J.K. Could Vitamin D be Associated with Proliferative Diabetic Retinopathy? Evidence from Pooling Studies. Horm. Metab. Res. 2019;51:729–734. doi: 10.1055/a-1010-6449. [DOI] [PubMed] [Google Scholar]
- 56.Kaur H., Donaghue K.C., Chan A.K., Benitez-Aguirre P., Hing S., Lloyd M., Cusumano J., Pryke A., Craig M.E. Vitamin D deficiency is associated with retinopathy in children and adolescents with type 1 diabetes. Diabetes Care. 2011;34:1400–1402. doi: 10.2337/dc11-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Luo B.A., Gao F., Qin L.L. The association between vitamin D deficiency and diabetic retinopathy in type 2 diabetes: A meta-analysis of observational studies. Nutrients. 2017;9:307. doi: 10.3390/nu9030307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lopes M., Laiginhas R., Madeira C., Neves J.S., Barbosa M., Rosas V., Carvalho D., Falcão-Reis F., Falcão M. Association between serum Vitamin D and diabetic retinopathy in Portuguese patients with type 1 diabetes. Acta Med. Port. 2020;33:459–465. doi: 10.20344/amp.12890. [DOI] [PubMed] [Google Scholar]
- 59.Nadri G., Saxena S., Mahdi A.A., Kaur A., Ahmad M.K., Garg P., Meyer C.H. Serum vitamin D is a biomolecular biomarker for proliferative diabetic retinopathy. Int. J. Retin. Vitr. 2019;5:31. doi: 10.1186/s40942-019-0181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ahmed L.H.M., Butler A.E., Dargham S.R., Latif A., Ahmed E.A., Hassan A., Atkin S.L. Relationship between total vitamin d metabolites and complications in patients with type 2 diabetes. Biomed. Rep. 2020;14:18. doi: 10.3892/br.2020.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gungor A., Ates O., Bilen H., Kocer I. Retinal nerve fiber layer thickness in early-stage diabetic retinopathy with vitamin D deficiency. Investig. Ophthalmol. Vis. Sci. 2015;56:6433–6437. doi: 10.1167/iovs.15-16872. [DOI] [PubMed] [Google Scholar]
- 62.Ren Z., Li W., Zhao Q., Ma L., Zhu J. The impact of 1,25-dihydroxy vitamin D3 on the expressions of vascular endothelial growth factor and transforming growth factor-β1 in the retinas of rats with diabetes. Diabetes Res. Clin. Pract. 2012;98:474–480. doi: 10.1016/j.diabres.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 63.Yi X., Sun J., Li L., Wei Q., Qian Y., Chen X., Ma L. 1,25-dihydroxyvitamin D3 deficiency is involved in the pathogenesis of diabetic retinopathy in the uygur population of China. IUBMB Life. 2016;68:445–451. doi: 10.1002/iub.1501. [DOI] [PubMed] [Google Scholar]
- 64.Závorková M., Vetvicka V., Richter J., Kral V., Liehnova I., Rajnohova D.L. Effects of Glucan and Vitamin D Supplementation on Obesity and Lipid Metabolism in Diabetic Retinopathy. Open Biochem. J. 2018;12:36–45. doi: 10.2174/1874091X01812010036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lu L., Lu Q., Chen W., Li J., Li C., Zheng Z. Vitamin D3 protects against diabetic retinopathy by inhibiting high-glucose-induced activation of the ROS/TXNIP/NLRP3 inflammasome pathway. J. Diabetes Res. 2018;2018:8193523. doi: 10.1155/2018/8193523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang Y., Xia W., Lu P., Yuan H. The Association between VDR Gene Polymorphisms and Diabetic Retinopathy Susceptibility: A Systematic Review and Meta-Analysis. Biomed Res. Int. 2016;2016:5305282. doi: 10.1155/2016/5305282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Song N., Yang S., Wang Y.Y., Tang S.Q., Zhu Y.Q., Dai Q., Zhang H. The Impact of Vitamin D Receptor Gene Polymorphisms on the Susceptibility of Diabetic Vascular Complications: A Meta-Analysis. Genet. Test. Mol. Biomarkers. 2019;23:533–556. doi: 10.1089/gtmb.2019.0037. [DOI] [PubMed] [Google Scholar]
- 68.Bennett B.J.L. Optic Neuritis. Continuum. 2019;25:1236–1264. doi: 10.1212/CON.0000000000000768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burton J.M., Eliasziw M., Trufyn J., Tung C., Carter G., Costello F. A prospective cohort study of vitamin D in optic neuritis recovery. Mult. Scler. 2017;23:82–93. doi: 10.1177/1352458516642315. [DOI] [PubMed] [Google Scholar]
- 70.Salari M., Janghorbani M., Etemadifar M., Dehghani A., Razmjoo H., Naderian G. Effects of vitamin D on retinal nerve fiber layer in vitamin D deficient patients with optic neuritis: Preliminary findings of a randomized, placebo-controlled trial. J. Res. Med. Sci. 2015;20:372–378. [PMC free article] [PubMed] [Google Scholar]
- 71.Pihl-Jensen G., Frederiksen J.L. 25-Hydroxyvitamin D levels in acute monosymptomatic optic neuritis: Relation to clinical severity, paraclinical findings and risk of multiple sclerosis. J. Neurol. 2015;262:1646–1654. doi: 10.1007/s00415-015-7740-5. [DOI] [PubMed] [Google Scholar]
- 72.Derakhshandi H., Etemadifar M., Feizi A., Abtahi S.H., Minagar A., Abtahi M.A., Abtahi Z.A., Dehghani A., Sajjadi S., Tabrizi N. Preventive effect of vitamin D3 supplementation on conversion of optic neuritis to clinically definite multiple sclerosis: A double blind, randomized, placebo-controlled pilot clinical trial. Acta Neurol. Belg. 2013;113:257–263. doi: 10.1007/s13760-012-0166-2. [DOI] [PubMed] [Google Scholar]
- 73.Fjeldstad C., Fjeldstad A.S., Weir J.P., Pardo G. Association of vitamin D deficiency with RNFL thickness in MS individuals without history of optic neuritis. Mult. Scler. Relat. Disord. 2014;3:489–493. doi: 10.1016/j.msard.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 74.Rehak J., Rehak M. Branch retinal vein occlusion: Pathogenesis, visual prognosis, and treatment modalities. Curr. Eye Res. 2008;33:111–131. doi: 10.1080/02713680701851902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yin X., Li J., Zhang B., Lu P. Association of glaucoma with risk of retinal vein occlusion: A meta-analysis. Acta Ophthalmol. 2019;97:652–659. doi: 10.1111/aos.14141. [DOI] [PubMed] [Google Scholar]
- 76.Latic N., Erben R.G. Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Int. J. Mol. Sci. 2020;21:6483. doi: 10.3390/ijms21186483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Oli A., Joshi D. Serum vitamin D levels in Indian patients with retinal venous occlusions. Saudi J. Ophthalmol. 2017;31:76–79. doi: 10.1016/j.sjopt.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Epstein D., Kvanta A., Lindqvist P.G. Vitamin D Deficiency in Patients with Central Retinal Vein Occlusion: A Case Control Study. Curr. Eye Res. 2017;42:448–451. doi: 10.1080/02713683.2016.1188117. [DOI] [PubMed] [Google Scholar]
- 79.Cooper J., Tkatchenko A.V. A Review of Current Concepts of the Etiology and Treatment of Myopia. Eye Contact Lens. 2018;44:231–247. doi: 10.1097/ICL.0000000000000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Baird P.N., Saw S.M., Lanca C., Guggenheim J.A., Smith E.L., Zhou X., Matsui K.O., Wu P.C., Sankaridurg P., Chia A., et al. Myopia. Nat. Rev. Dis. Prim. 2020;6:99. doi: 10.1038/s41572-020-00231-4. [DOI] [PubMed] [Google Scholar]
- 81.Choi J.A., Han K., Park Y.M., La T.Y. Low serum 25-hydroxyvitamin D is associated with myopia in Korean adolescents. Investig. Ophthalmol. Vis. Sci. 2014;55:2041–2047. doi: 10.1167/iovs.13-12853. [DOI] [PubMed] [Google Scholar]
- 82.Yazar S., Hewitt A.W., Black L.J., McKnight C.M., Mountain J.A., Sherwin J.C., Oddy W.H., Coroneo M.T., Lucas R.M., Mackey D.A. Myopia is associated with lower vitamin D status in young adults. Investig. Ophthalmol. Vis. Sci. 2014;55:4552–4559. doi: 10.1167/iovs.14-14589. [DOI] [PubMed] [Google Scholar]
- 83.Kwon J.W., Choi J.A., La T.Y. Serum 25-hydroxyvitamin D level is associated with myopia in the Korea national health and nutrition examination survey. Medicine. 2016;95:e5012. doi: 10.1097/MD.0000000000005012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tideman J.W.L., Polling J.R., Voortman T., Jaddoe V.W.V., Uitterlinden A.G., Hofman A., Vingerling J.R., Franco O.H., Klaver C.C.W. Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur. J. Epidemiol. 2016;31:491–499. doi: 10.1007/s10654-016-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tang S.M., Lau T., Rong S.S., Yazar S., Chen L.J., Mackey D.A., Lucas R.M., Pang C.P., Yam J.C. Vitamin D and its pathway genes in myopia: Systematic review and meta-analysis. Br. J. Ophthalmol. 2019;103:8–17. doi: 10.1136/bjophthalmol-2018-312159. [DOI] [PubMed] [Google Scholar]
- 86.Jung B.J., Jee D. Association between serum 25-hydroxyvitamin D levels and myopia in general Korean adults. Indian J. Ophthalmol. 2020;68:15–22. doi: 10.4103/ijo.IJO_760_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Guggenheim J.A., Williams C., Northstone K., Howe L.D., Tilling K., Pourcain B.S., McMahon G., Lawlor D.A. Does vitamin D mediate the protective effects of time outdoors on myopia? Findings from a prospective birth cohort. Investig. Ophthalmol. Vis. Sci. 2014;55:8550–8558. doi: 10.1167/iovs.14-15839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cuellar-Partida G., Williams K.M., Yazar S., Guggenheim J.A., Hewitt A.W., Williams C., JinWang J., Kho P.F., Saw S.M., Cheng C.Y., et al. Genetically low vitamin D concentrations and myopic refractive error: A Mendelian randomization study. Int. J. Epidemiol. 2017;46:1882–1890. doi: 10.1093/ije/dyx068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lingham G., Yazar S., Lucas R.M., Walsh J.P., Zhu K., Hunter M., Lim E.M., Cooke B.R., Mackey D.A. Low 25-hydroxyvitamin D concentration is not associated with refractive error in middle-aged and older Western Australian adults. Transl. Vis. Sci. Technol. 2019;8:13. doi: 10.1167/tvst.8.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Da Chou H., Yao T.C., Huang Y.S., Huang C.Y., Yang M.L., Sun M.H., Chen H.C., Liu C.H., Chu S.M., Hsu J.F., et al. Myopia in school-Aged children with preterm birth: The roles of time spent outdoors and serum vitamin D. Br. J. Ophthalmol. 2021;105:468–472. doi: 10.1136/bjophthalmol-2019-315663. [DOI] [PubMed] [Google Scholar]
- 91.Specht I.O., Jacobsen N., Frederiksen P., Heitmann B.L. Neonatal vitamin D status and myopia in young adult men. Acta Ophthalmol. 2020;98:500–505. doi: 10.1111/aos.14349. [DOI] [PubMed] [Google Scholar]
- 92.Williams K.M., Bentham G.C.G., Young I.S., McGinty A., McKay G.J., Hogg R., Hammond C.J., Chakravarthy U., Rahu M., Seland J., et al. Association between myopia, ultraviolet b radiation exposure, serum Vitamin D concentrations, and genetic polymorphisms in Vitamin Dmetabolic pathways in a multicountry european study. JAMA Ophthalmol. 2017;135:47–53. doi: 10.1001/jamaophthalmol.2016.4752. [DOI] [PubMed] [Google Scholar]
- 93.Xiong S., Sankaridurg P., Naduvilath T., Zang J., Zou H., Zhu J., Lv M., He X., Xu X. Time spent in outdoor activities in relation to myopia prevention and control: A meta-analysis and systematic review. Acta Ophthalmol. 2017;95:551–566. doi: 10.1111/aos.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Caban M., Lewandowska U. Polyphenols and Posterior Segment Eye Diseases: Effects on Angiogenesis, Invasion, Migration and Epithelial-Mesenchymal Transition. Food Rev. Int. 2021;00:1–29. doi: 10.1080/87559129.2021.2012792. [DOI] [Google Scholar]
- 95.Albert D.M., Nickells R.W., Gamm D.M., Zimbric M.L., Schlamp C.L., Lindstrom M.J., Audo I. Vitamin D analogs, a new treatment for retinoblastoma: The first Ellsworth Lecture. Ophthalmic Genet. 2002;23:137–156. doi: 10.1076/opge.23.3.137.7883. [DOI] [PubMed] [Google Scholar]
- 96.Wagner N., Wagner K.D., Schley G., Badiali L., Theres H., Scholz H. 1,25-Dihydroxyvitamin D3-induced apoptosis of retinoblastoma cells is associated with reciprocal changes of Bcl-2 and bax. Exp. Eye Res. 2003;77:1–9. doi: 10.1016/S0014-4835(03)00108-8. [DOI] [PubMed] [Google Scholar]
- 97.Shokravi M.T., Marcus D.M., Alroy J., Egan K., Saornil M.A., Albert D.M. Vitamin D inhibits angiogenesis in transgenic murine retinoblastoma. Investig. Ophthalmol. Vis. Sci. 1995;36:83–87. [PubMed] [Google Scholar]
- 98.Audo I., Darjatmoko S.R., Schlamp C.L., Lokken J.M., Lindstrom M.J., Albert D.M., Nickells R.W. Vitamin D analogues increase p53, p21, and apoptosis in a xenograft model of human retinoblastoma. Investig. Ophthalmol. Vis. Sci. 2003;44:4192–4199. doi: 10.1167/iovs.02-1198. [DOI] [PubMed] [Google Scholar]
- 99.Sabet S.J., Darjatmoko S.R., Lindstrom M.J., Albert D.M. Antineoplastic effect and toxicity of 1,25-dihydroxy-16-ene-23-yne-vitamin D3 in athymic mice with Y-79 human retinoblastoma tumors. Arch. Ophthalmol. 1999;117:365–370. doi: 10.1001/archopht.117.3.365. [DOI] [PubMed] [Google Scholar]
- 100.Albert D.M., Kumar A., Strugnell S.A., Darjatmoko S.R., Lokken J.M., Lindstrom M.J., Patel S. Effectiveness of vitamin D analogues in treating large tumors and during prolonged use in murine retinoblastoma models. Arch. Ophthalmol. 2004;122:1357–1362. doi: 10.1001/archopht.122.9.1357. [DOI] [PubMed] [Google Scholar]
- 101.Albert D.M., Plum L.A., Yang W., Marcet M., Lindstrom M.J., Clagett-Dame M., DeLuca H.F. Responsiveness of human retinoblastoma and neuroblastoma models to a non-calcemic 19-nor Vitamin D analog. J. Steroid Biochem. Mol. Biol. 2005;97:165–172. doi: 10.1016/j.jsbmb.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 102.Kulkarni A.D., Van Ginkel P.R., Darjatmoko S.R., Lindstrom M.J., Albert D.M. Use of combination therapy with cisplatin and calcitriol in the treatment of Y-79 human retinoblastoma xenograft model. Br. J. Ophthalmol. 2009;93:1105–1108. doi: 10.1136/bjo.2008.152843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Augsburger J.J., Corrêa Z.M., Shaikh A.H. Effectiveness of Treatments for Metastatic Uveal Melanoma. Am. J. Ophthalmol. 2009;148:119–127. doi: 10.1016/j.ajo.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 104.Amirouchene-Angelozzi N., Nemati F., Gentien D., Nicolas A., Dumont A., Carita G., Camonis J., Desjardins L., Cassoux N., Piperno-Neumann S., et al. Establishment of novel cell lines recapitulating the genetic landscape of uveal melanoma and preclinical validation of mTOR as a therapeutic target. Mol. Oncol. 2014;8:1508–1520. doi: 10.1016/j.molonc.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chang C.W., Hsieh Y.H., Yang W.E., Yang S.F., Chen Y., Hu D.N. Epigallocatechingallate inhibits migration of human uveal melanoma cells via downregulation of matrix metalloproteinase-2 activity and ERK1/2 pathway. Biomed Res. Int. 2014;2014:141582. doi: 10.1155/2014/141582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yang J., Manson D.K., Marr B.P., Carvajal R.D. Treatment of uveal melanoma: Where are we now? Ther. Adv. Med. Oncol. 2018;10:1–17. doi: 10.1177/1758834018757175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Xu S., Zhang Z.H., Fu L., Song J., Xie D.D., Yu D.X., Xu D.X., Sun G.P. Calcitriol inhibits migration and invasion of renal cell carcinoma cells by suppressing Smad2/3-, STAT3- and β-catenin-mediated epithelial-mesenchymal transition. Cancer Sci. 2020;111:59–71. doi: 10.1111/cas.14237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Markiewicz A., Brożyna A.A., Podgórska E., Elas M., Urbańska K., Jetten A.M., Slominski A.T., Jóźwicki W., Orłowska-Heitzman J., Dyduch G., et al. Vitamin D receptors (VDR), hydroxylases CYP27B1 and CYP24A1 and retinoid-related orphan receptors (ROR) level in human uveal tract and ocular melanoma with different melanization levels. Sci. Rep. 2019;9:9142. doi: 10.1038/s41598-019-45161-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kaliki S., Shields C.L. Uveal melanoma: Relatively rare but deadly cancer. Eye. 2017;31:241–257. doi: 10.1038/eye.2016.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Moan J., Cicarma E., Setlow R., Porojnicu A.C., Grant W.B., Juzeniene A. Time trends and latitude dependence of uveal and cutaneous malignant melanoma induced by solar radiation. Dermatoendocrinology. 2010;2:3–8. doi: 10.4161/derm.2.1.11745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Podgorska E., Drzal A., Matuszak Z., Swakon J., Slominski A., Elas M., Urbanska K. Calcitriol and calcidiol can sensitize melanoma cells to low–LET proton beam irradiation. Int. J. Mol. Sci. 2018;19:2236. doi: 10.3390/ijms19082236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rosenbaum J.T., Bodaghi B., Couto C., Zierhut M., Acharya N., Pavesio C., Tay-Kearney M.L., Neri P., Douglas K., Pathai S., et al. New observations and emerging ideas in diagnosis and management of non-infectious uveitis: A review. Semin. Arthritis Rheum. 2019;49:438–445. doi: 10.1016/j.semarthrit.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 113.Sengler C., Zink J., Klotsche J., Niewerth M., Liedmann I., Horneff G., Kessel C., Ganser G., Thon A., Haas J.P., et al. Vitamin D deficiency is associated with higher disease activity and the risk for uveitis in juvenile idiopathic arthritis—Data from a German inception cohort. Arthritis Res. Ther. 2018;20:276. doi: 10.1186/s13075-018-1765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sobrin L., Stanwyck L.K., Pan W., Hubbard R.A., Kempen J.H., VanderBeek B.L. Association of hypovitaminosis d with increased risk of uveitis in a large health care claims database. JAMA Ophthalmol. 2018;136:548–552. doi: 10.1001/jamaophthalmol.2018.0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Grotting L.A., Davoudi S., Palenzuela D., Papaliodis G.N., Sobrin L. Association of lowvitamin d levels with noninfectious anterior uveitis. JAMA Ophthalmol. 2017;135:150–153. doi: 10.1001/jamaophthalmol.2016.4888. [DOI] [PubMed] [Google Scholar]
- 116.Dadaci Z., Cetinkaya S., Oncel Acir N., Oncel M., Borazan M. Serum Vitamin D Levels in Patients with Acute Anterior Uveitis. Ocul. Immunol. Inflamm. 2017;25:492–496. doi: 10.3109/09273948.2016.1139735. [DOI] [PubMed] [Google Scholar]
- 117.Chiu Z.K., Lim L.L., Rogers S.L., Hall A.J. Patterns of Vitamin D Levels and Exposures in Active and Inactive Noninfectious Uveitis Patients. Ophthalmology. 2020;127:230–237. doi: 10.1016/j.ophtha.2019.06.030. [DOI] [PubMed] [Google Scholar]
- 118.Llop S.M., Davoudi S., Stanwyck L.K., Sathe S., Tom L., Ahmadi T., Grotting L., Papaliodis G.N., Sobrin L. Association of Low Vitamin D Levels with Noninfectious Uveitis and Scleritis. Ocul. Immunol. Inflamm. 2019;27:602–609. doi: 10.1080/09273948.2018.1434208. [DOI] [PubMed] [Google Scholar]
- 119.Rohmer J., Hadjadj J., Bouzerara A., Salah S., Paule R., Groh M., Blanche P., Mouthon L., Monnet D., Le Jeunne C., et al. Serum 1,25(OH)2 Vitamin D and 25(OH) Vitamin D Ratio for the Diagnosis of Sarcoidosis-Related Uveitis. Ocul. Immunol. Inflamm. 2020;28:341–347. doi: 10.1080/09273948.2018.1537399. [DOI] [PubMed] [Google Scholar]
- 120.Lavezzo M.M., Sakata V.M., Morita C., Rodriguez E.E.C., Abdallah S.F., Da Silva F.T.G., Hirata C.E., Yamamoto J.H. Vogt-Koyanagi-Harada disease: Review of a rare autoimmune disease targeting antigens of melanocytes. Orphanet J. Rare Dis. 2016;11:29. doi: 10.1186/s13023-016-0412-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Illescas-Montes R., Melguizo-Rodríguez L., Ruiz C., Costela-Ruiz V.J. Vitamin D and autoimmune diseases. Life Sci. 2019;233:116744. doi: 10.1016/j.lfs.2019.116744. [DOI] [PubMed] [Google Scholar]
- 122.Yi X., Yang P., Sun M., Yang Y., Li F. Decreased 1,25-dihydroxyvitamin D3 level is involved in the pathogenesis of Vogt-Koyanagi-Harada (VKH) disease. Mol. Vis. 2011;17:673–679. [PMC free article] [PubMed] [Google Scholar]
- 123.Al-Barry M.A., Albalawi A.M., Sayf M.A., Badawi A., Afzal S., Latif M., Samman M.I., Basit S. Sequence analysis of four Vitamin D family genes (VDR, CYP24A1, CYP27B1 and CYP2R1) in Vogt-Koyanagi-Harada (VKH) patients: Identification of a potentially pathogenic variant in CYP2R. BMC Ophthalmol. 2016;16:172. doi: 10.1186/s12886-016-0354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lv Y., Han X., Yao Q., Zhang K., Zheng L., Hong W., Xing X. 1α,25-dihydroxyvitamin D3 attenuates oxidative stress-induced damage in human trabecular meshwork cells by inhibiting TGFβ-SMAD3-VDR pathway. Biochem. Biophys. Res. Commun. 2019;516:75–81. doi: 10.1016/j.bbrc.2019.06.027. [DOI] [PubMed] [Google Scholar]
- 125.Huynh B., Shah P., Sii F., Hunter D., Carnt N., White A. Low systemic vitamin D as a potential risk factor in primary open-angle glaucoma: A review of current evidence. Br. J. Ophthalmol. 2021;105:595–601. doi: 10.1136/bjophthalmol-2020-316331. [DOI] [PubMed] [Google Scholar]
- 126.Krefting E.A., Jorde R., Christoffersen T., Grimnes G. Vitamin D and intraocular pressure—Results from a case -control and an intervention study. Acta Ophthalmol. 2014;92:345–349. doi: 10.1111/aos.12125. [DOI] [PubMed] [Google Scholar]
- 127.Yoo T.K., Oh E., Hong S. Is vitamin D status associated with open-angle glaucoma? A cross-sectional study from South Korea. Public Health Nutr. 2014;17:833–843. doi: 10.1017/S1368980013003492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Goncalves A., Milea D., Gohier P., Jallet G., Leruez S., Baskaran M., Aung T., Annweiler C. Serum Vitamin D status is associated with the presence but not the severity of primary open angle glaucoma. Maturitas. 2015;81:470–474. doi: 10.1016/j.maturitas.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 129.Arar Ž.V., Praveček M.K., Miškić B., Vatavuk Z., Rodriguez J.V., Sekelj S. Association between serum vitamin D level and glaucoma in women. Acta Clin. Croat. 2016;55:203–208. doi: 10.20471/acc.2016.55.02.04. [DOI] [PubMed] [Google Scholar]
- 130.Lv Y., Yao Q., Ma W., Liu H., Ji J., Li X. Associations of Vitamin D deficiency and Vitamin D receptor (Cdx-2, Fok I, Bsm i and Taq I) polymorphisms with the risk of primary open-angle glaucoma. BMC Ophthalmol. 2016;16:116. doi: 10.1186/s12886-016-0289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ayyagari R., der I Chen Y., Zangwill L.M., Holman M., Dirkes K., Hai Y., Arzumanyan Z., Slight R., Hammel N., Girkin C.A., et al. Association of severity of primary open-angle glaucoma with serum vitamin D levels in patients of African descent. Mol. Vis. 2019;25:438–445. [PMC free article] [PubMed] [Google Scholar]
- 132.Thompson J., Lakhani N. Cataracts. Prim. Care Clin. Off. Pract. 2015;42:409–423. doi: 10.1016/j.pop.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 133.Liu Y.-C., Wilkins M., Kim T., Malyugin B., Mehta J.S. Seminar Cataracts. Lancet. 2017;390:600–612. doi: 10.1016/S0140-6736(17)30544-5. [DOI] [PubMed] [Google Scholar]
- 134.Abdellah M.M., Mohamed Mostafa E., Salama E.H., Roshdy Mohamed E. Association of Serum 25-Hydroxyl Vitamin D Deficiency and Age-Related Cataract: A Case-Control Study. J. Ophthalmol. 2019;2019:9312929. doi: 10.1155/2019/9312929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jee D., Kim E.C. Association between serum 25-hydroxyvitamin D levels and age-related cataracts. J. Cataract Refract. Surg. 2015;41:1705–1715. doi: 10.1016/j.jcrs.2014.12.052. [DOI] [PubMed] [Google Scholar]
- 136.Öktem C., Aslan F. Vitamin D Levels in Young Adult Cataract Patients: A Case-Control Study. Ophthalmic Res. 2021;64:116–120. doi: 10.1159/000509602. [DOI] [PubMed] [Google Scholar]
- 137.Rao P., Millen A.E., Meyers K.J., Liu Z., Voland R., Sondel S., Tinker L., Wallace R.B., Blodi B.A., Binkley N., et al. The relationship between serum 25-hydroxyvitamin D levels and nuclear cataract in the carotenoid age-related eye study (CAREDS), an ancillary study of the women’s health initiative. Investig. Ophthalmol. Vis. Sci. 2015;56:4221–4230. doi: 10.1167/iovs.15-16835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Park S., Choi N.K. Serum 25-hydroxyvitamin D and Age-Related Cataract. Ophthalmic Epidemiol. 2017;24:281–286. doi: 10.1080/09286586.2017.1281427. [DOI] [PubMed] [Google Scholar]
- 139.Brown C.J., Akaichi F. Vitamin D deficiency and posterior subcapsular cataract. Clin. Ophthalmol. 2015;9:1093–1098. doi: 10.2147/OPTH.S84790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Atalay K., Savur F.G., Kirgiz A., Kaldirim H.E., Zengi O. Serum vitamin d levels in different morphologic forms of age related cataract. Acta Endocrinol. 2020;16:178–182. doi: 10.4183/aeb.2020.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Cho M.C., Kim R.B., Ahn J.Y., Yoo W.S., Kim S.J. Aqueous humor and serum 25-Hydroxyvitamin D levels in patients with cataracts. BMC Ophthalmol. 2020;20:6. doi: 10.1186/s12886-019-1293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Vergouwen D.P.C., Rothova A., Berge J.C.T., Verdijk R.M., van Laar J.A.M., Vingerling J.R., Schreurs M.W.J. Current insights in the pathogenesis of scleritis. Exp. Eye Res. 2020;197:108078. doi: 10.1016/j.exer.2020.108078. [DOI] [PubMed] [Google Scholar]
- 143.Caban M., Owczarek K., Chojnacka K., Lewandowska U. Overview of Polyphenols and Polyphenol-rich Extracts as Modulators of Inflammatory Response in Dry Eye Syndrome. Food Rev. Int. 2021:1–28. doi: 10.1080/87559129.2021.1874412. [DOI] [Google Scholar]
- 144.Dai Y., Zhang J., Xiang J., Li Y., Wu D., Xu J. Calcitriol inhibits ROS-NLRP3-IL-1β signaling axis via activation of Nrf2-antioxidant signaling in hyperosmotic stress stimulated human corneal epithelial cells. Redox Biol. 2019;21:101093. doi: 10.1016/j.redox.2018.101093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang J., Dai Y., Wu D., Xu J. Calcitriol, the Active Metabolite of Vitamin D3, Inhibits Dry Eye Related Corneal Inflammation In Vivo and In Vitro. Ocul. Immunol. Inflamm. 2019;27:257–265. doi: 10.1080/09273948.2017.1372486. [DOI] [PubMed] [Google Scholar]
- 146.Lyu N., Zhang J., Dai Y., Xiang J., Li Y., Xu J. Calcitriol inhibits apoptosis via activation of autophagy in hyperosmotic stress stimulated corneal epithelial cells in vivo and in vitro. Exp. Eye Res. 2020;200:108210. doi: 10.1016/j.exer.2020.108210. [DOI] [PubMed] [Google Scholar]
- 147.Askari G., Rafie N., Miraghajani M., Heidari Z., Arab A. Association between vitamin D and dry eye disease: A systematic review and meta-analysis of observational studies. Contact Lens Anterior Eye. 2020;43:418–425. doi: 10.1016/j.clae.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 148.Kuo C.Y., Huang Y.C., Lin K.J., Tsai T.Y. Vitamin d deficiency is associated with severity of dry eye symptoms and primary sjögren’s syndrome: A systematic review and meta-analysis. J. Nutr. Sci. Vitaminol. 2020;66:386–388. doi: 10.3177/jnsv.66.386. [DOI] [PubMed] [Google Scholar]
- 149.Liu J., Dong Y., Wang Y. Vitamin D deficiency is associated with dry eye syndrome: A systematic review and meta-analysis. Acta Ophthalmol. 2020;98:749–754. doi: 10.1111/aos.14470. [DOI] [PubMed] [Google Scholar]
- 150.Yoon S.Y., Bae S.H., Shin Y.J., Park S.G., Hwang S.H., Hyon J.Y., Wee W.R. Low serum 25-hydroxyvitamin D levels are associated with dry eye syndrome. PLoS ONE. 2016;11:e0147847. doi: 10.1371/journal.pone.0147847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Khamar P., Nair A.P., Shetty R., Vaidya T., Subramani M., Ponnalagu M., Dhamodaran K., D’Souza S., Ghosh A., Pahuja N., et al. Dysregulated tear fluid nociception-associated factors, corneal dendritic cell density, and vitamin D levels in evaporative dry eye. Investig. Ophthalmol. Vis. Sci. 2019;60:2532–2542. doi: 10.1167/iovs.19-26914. [DOI] [PubMed] [Google Scholar]
- 152.Kurtul B.E., Özer P.A., Aydinli M.S. The association of Vitamin D deficiency with tear break-up time and Schirmer testing in non-Sjögren dry eye. Eye. 2015;29:1081–1084. doi: 10.1038/eye.2015.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Demirci G., Erdur S.K., Ozsutcu M., Eliacik M., Olmuscelik O., Aydin R., Kocabora M.S. Dry eye assessment in patients with Vitamin D deficiency. Eye Contact Lens. 2016;44:S62–S65. doi: 10.1097/ICL.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 154.Jin K.W., Ro J.W., Shin Y.J., Hyon J.Y., Wee W.R., Park S.G. Correlation of vitamin D levels with tear film stability and secretion in patients with dry eye syndrome. Acta Ophthalmol. 2017;95:e230–e235. doi: 10.1111/aos.13241. [DOI] [PubMed] [Google Scholar]
- 155.Jee D., Kang S., Yuan C., Cho E., Arroyo J.G., Kang S.W., Baek S.H., Kim C.Y., Kim S.D., Kim S.H., et al. Serum 25-hydroxyVitamin D levels and dry eye syndrome: Differential effects of Vitamin D on ocular diseases. PLoS ONE. 2016;11:e0149294. doi: 10.1371/journal.pone.0149294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Jeon D.H., Yeom H., Yang J., Song J.S., Lee H.K., Kim H.C. Are serum vitamin D levels associated with dry eye disease? Results from the study group for environmental eye disease. J. Prev. Med. Public Health. 2017;50:369–376. doi: 10.3961/jpmph.17.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bae S.H., Shin Y.J., Kim H.K., Hyon J.Y., Wee W.R., Park S.G. Vitamin D Supplementation for Patients with Dry Eye Syndrome Refractory to Conventional Treatment. Sci. Rep. 2016;6:33083. doi: 10.1038/srep33083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hwang J.S., Lee Y.P., Shin Y.J. Vitamin D enhances the efficacy of topical artificial tears in patients with dry eye disease. Cornea. 2019;38:304–310. doi: 10.1097/ICO.0000000000001822. [DOI] [PubMed] [Google Scholar]
- 159.Di Zazzo A., Bonini S., Fernandes M. Adult vernal keratoconjunctivitis. Curr. Opin. Allergy Clin. Immunol. 2020;20:501–506. doi: 10.1097/ACI.0000000000000672. [DOI] [PubMed] [Google Scholar]
- 160.Kim Y.H., Kim K.W., Kim M.J., Sol I.S., Yoon S.H., Ahn H.S., Kim H.J., Sohn M.H., Kim K.E. Vitamin D levels in allergic rhinitis: A systematic review and meta-analysis. Pediatr. Allergy Immunol. 2016;27:580–590. doi: 10.1111/pai.12599. [DOI] [PubMed] [Google Scholar]
- 161.Zicari A.M., Cafarotti A., Occasi F., Lollobrigida V., Nebbioso M., Pecorella I., De Castro G., Spalice A., Loffredo L., Villa M.P., et al. Vitamin D levels in children affected by vernal keratoconjunctivitis. Curr. Med. Res. Opin. 2017;33:269–274. doi: 10.1080/03007995.2016.1254602. [DOI] [PubMed] [Google Scholar]
- 162.Sorkhabi R., Ahoor M.H., Ghorbanihaghjo A., Jafari S. Serum vitamin D levels in patients with vernal keratoconjunctivitis and its relationship with disease severity. Eur. J. Ophthalmol. 2021;31:3259–3264. doi: 10.1177/1120672120978886. [DOI] [PubMed] [Google Scholar]
- 163.Bozkurt B., Artac H., Ozdemir H., Ünlü A., Bozkurt M.K., Irkec M. Serum Vitamin D Levels in Children with Vernal Keratoconjunctivitis. Ocul. Immunol. Inflamm. 2018;26:435–439. doi: 10.1080/09273948.2016.1235714. [DOI] [PubMed] [Google Scholar]
- 164.Pucci N., Caputo R., di Grande L., de Libero C., Mori F., Barni S., di Simone L., Calvani A., Rusconi F., Novembre E. Tacrolimus vs. cyclosporine eyedrops in severe cyclosporine-resistant vernal keratoconjunctivitis: A randomized, comparative, double-blind, crossover study. Pediatr. Allergy Immunol. 2015;26:256–261. doi: 10.1111/pai.12360. [DOI] [PubMed] [Google Scholar]
- 165.Ghiglioni D.G., Bruschi G., Gandini S., Osnaghi S., Peroni D., Marchisio P. Vitamin d serum levels in children with vernal keratoconjunctivitis and disease control. Int. J. Immunopathol. Pharmacol. 2019;33:2058738419833468. doi: 10.1177/2058738419833468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Davidson A.E., Hayes S., Hardcastle A.J., Tuft S.J. The pathogenesis of keratoconus. Eye. 2014;28:189–195. doi: 10.1038/eye.2013.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gordon-Shaag A., Millodot M., Shneor E., Liu Y. The genetic and environmental factors for keratoconus. Biomed Res. Int. 2015;2015:24–32. doi: 10.1155/2015/795738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Claessens J.L.J., Godefrooij D.A., Vink G., Frank L.E., Wisse R.P.L. Nationwide epidemiological approach to identify associations between keratoconus and immune-mediated diseases. Br. J. Ophthalmol. 2021:1–5. doi: 10.1136/bjophthalmol-2021-318804. online ahead of print . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sassi F., Tamone C., D’amelio P. Vitamin D: Nutrient, hormone, and immunomodulator. Nutrients. 2018;10:1656. doi: 10.3390/nu10111656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Akkaya S., Ulusoy D.M. Serum Vitamin D Levels in Patients with Keratoconus. Ocul. Immunol. Inflamm. 2020;28:348–353. doi: 10.1080/09273948.2019.1604002. [DOI] [PubMed] [Google Scholar]
- 171.Zarei-Ghanavati S., Yahaghi B., Hassanzadeh S., Mobarhan M.G., Hakimi H.R., Eghbali P. Serum 25-hydroxyvitamin D, selenium, zinc and copper in patients with keratoconus. J. Curr. Ophthalmol. 2020;32:26–31. doi: 10.1016/j.joco.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Aslan M.G., Fındık H., Okutucu M., Aydın E., Oruҫ Y., Arpa M., Uzun F. Serum 25-Hydroxy Vitamin D, Vitamin B12, and Folic Acid Levels in Progressive and Nonprogressive Keratoconus. Cornea. 2021;40:334–341. doi: 10.1097/ICO.0000000000002475. [DOI] [PubMed] [Google Scholar]
- 173.Koç M., Yavrum F., Uzel M.M., Aydemir E., Özülken K., Yılmazbaş P. The Effect of Pterygium and Pterygium Surgery on Corneal Biomechanics. Semin. Ophthalmol. 2018;33:449–453. doi: 10.1080/08820538.2017.1297839. [DOI] [PubMed] [Google Scholar]
- 174.Caban M., Lewandowska U. Inhibiting effects of polyphenols on angiogenesis and epithelial-mesenchymal transition in anterior segment eye diseases. J. Funct. Foods. 2021;87:104761. doi: 10.1016/j.jff.2021.104761. [DOI] [Google Scholar]
- 175.Shiroma H., Higa A., Sawaguchi S., Iwase A., Tomidokoro A., Amano S., Araie M. Prevalence and Risk Factors of Pterygium in a Southwestern Island of Japan: The Kumejima Study. Am. J. Ophthalmol. 2009;148:766–771.e1. doi: 10.1016/j.ajo.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 176.Liu L., Wu J., Geng J., Yuan Z., Huang D. Geographical prevalence and risk factors for pterygium: A systematic review and meta-analysis. BMJ Open. 2013;3:e003787. doi: 10.1136/bmjopen-2013-003787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Song P., Chang X., Wang M., An L. Variations of pterygium prevalence by age, gender and geographic characteristics in China: A systematic review and meta-analysis. PLoS ONE. 2017;12:e0174587. doi: 10.1371/journal.pone.0174587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chun Y.H., Paik J.S., Oh J.H., Kim H.S., Na K.S. Association between pterygium, sun exposure, and serum 25-hydroxyvitamin in a nationally representative sample of Korean adults 11 Medical and Health Sciences 1117 Public Health and Health Services. Lipids Health Dis. 2018;17:260. doi: 10.1186/s12944-018-0902-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Jee D., Kim E.C., Cho E., Arroyo J.G. Positive association between blood 25-hydroxyvitamin D levels and pterygium after control for sunlight exposure. PLoS ONE. 2016;11:e0157501. doi: 10.1371/journal.pone.0157501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Kara N., Ceri S. Vitamin D level in patients with pterygium. Arq. Bras. Oftalmol. 2017;80:229–233. doi: 10.5935/0004-2749.20170056. [DOI] [PubMed] [Google Scholar]
- 181.Örnek N., Oğurel T., Kısa Ü. Tear Fluid and Serum Vitamin D Concentrations in Unilateral Pterygium. Optom. Vis. Sci. 2021;98:170–174. doi: 10.1097/OPX.0000000000001640. [DOI] [PubMed] [Google Scholar]
- 182.Bilak Ş., Çevik M.Ö., Erdoğdu G.İ.H., Bağış H. Expression of Vitamin D Receptor and Vitamin D Receptor Gene Polymorphisms (BsmI, FokI, and TaqI) in Patients with Pterygium. Arq. Bras. Oftalmol. 2021;84:241–248. doi: 10.5935/0004-2749.20210032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Maxia C., Murtas D., Corrias M., Zucca I., Minerba L., Piras F., Marinelli C., Perra M.T. Vitamin D and vitamin D receptor in patients with ophthalmic pterygium. Eur. J. Histochem. 2017;61:257–263. doi: 10.4081/ejh.2017.2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Means J.H., Littlefield J. Graves’ disease. Am. Pract. Dig. Treat. 1948;2:488–493. doi: 10.1056/nejmra1510030. [DOI] [PubMed] [Google Scholar]
- 185.Xia N., Ye X., Hu X., Song S., Xu H., Niu M., Wang H., Wang J. Simultaneous induction of Graves’ hyperthyroidism and Graves’ ophthalmopathy by TSHR genetic immunization in BALB/c mice. PLoS ONE. 2017;12:e0174260. doi: 10.1371/journal.pone.0174260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Vieira I.H., Rodrigues D., Paiva I. Vitamin d and autoimmune thyroid disease—Cause, consequence, or a vicious cycle? Nutrients. 2020;12:2791. doi: 10.3390/nu12092791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wang J., Lv S., Chen G., Gao C., He J., Zhong H., Xu Y. Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients. 2015;7:2485–2498. doi: 10.3390/nu7042485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Sadaka A., Nguyen K., Malik A., Brito R., Berry S., Lee A.G. Vitamin D and Selenium in a Thyroid Eye Disease Population in Texas. Neuro-Ophthalmology. 2019;43:291–294. doi: 10.1080/01658107.2019.1566382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Heisel C.J., Riddering A.L., Andrews C.A., Kahana A. Serum Vitamin D Deficiency Is an Independent Risk Factor for Thyroid Eye Disease. Ophthal. Plast. Reconstr. Surg. 2020;36:17–20. doi: 10.1097/IOP.0000000000001437. [DOI] [PubMed] [Google Scholar]
- 190.Maciejewski A., Kowalczyk M.J., Gasińska T., Szeliga A., Prendecki M., Dorszewska J., Żaba R., Łącka K. The Role of Vitamin D Receptor Gene Polymorphisms in Thyroid-Associated Orbitopathy. Ocul. Immunol. Inflamm. 2020;28:354–361. doi: 10.1080/09273948.2019.1629605. [DOI] [PubMed] [Google Scholar]
- 191.Defazio G., Hallett M., Jinnah H.A., Conte A., Berardelli A. Blepharospasm 40 years later. Mov. Disord. 2017;32:498–509. doi: 10.1002/mds.26934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Hwang C.J., Eftekhari K. Benign Essential Blepharospasm: What We Know and What We Don’t. Int. Ophthalmol. Clin. 2018;58:11–24. doi: 10.1097/IIO.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 193.Yen M.T. Developments in the treatment of benign essential blepharospasm. Curr. Opin. Ophthalmol. 2018;29:440–444. doi: 10.1097/ICU.0000000000000500. [DOI] [PubMed] [Google Scholar]
- 194.Serefoglu Cabuk K., Tunc U., Ozturk Karabulut G., Fazil K., Karaagac Gunaydin Z., Asik Nacaroglu S., Taskapili M. Serum calcium, magnesium, phosphorus, and vitamin D in benign essential blepharospasm. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020;258:1293–1297. doi: 10.1007/s00417-020-04650-7. [DOI] [PubMed] [Google Scholar]
- 195.Bouillon R., Suda T. Vitamin D: Calcium and bone homeostasis during evolution. Bonekey Rep. 2014;3:480. doi: 10.1038/bonekey.2013.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Eroğul Ö., Beysel S., Doğan M., Gobeka H.H., Kaşikci M., Eryiği Eroğul L. Biochemical analysis of serum mineral and vitamin levels in benign essential blepharospasm. J. Surg. Med. 2021;5:495–499. doi: 10.28982/josam.924395. [DOI] [Google Scholar]
- 197.El-Sharkawy A., Malki A. Vitamin D Signaling in Inflammation and Cancer: Molecular Mechanisms and Therapeutic Implications. Molecules. 2020;25:3219. doi: 10.3390/molecules25143219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Fernandez-Robredo P., González-Zamora J., Recalde S., Bilbao-Malavé V., Bezunartea J., Hernandez M., Garcia-Layana A. Vitamin D Protects against Oxidative Stress and Inflammation in Human Retinal Cells. Antioxidants. 2020;9:838. doi: 10.3390/antiox9090838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Tohari A.M., Alhasani R.H., Biswas L., Patnaik S.R., Reilly J., Zeng Z., Shu X. Vitamin D Attenuates Oxidative Damage and Inflammation in Retinal Pigment Epithelial Cells. Antioxidants. 2019;8:341. doi: 10.3390/antiox8090341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lei X.-J., Xu L.-Y., Yang Y.-Q., Bing Y.-W., Zhao Y.-X. Vitamin D receptor regulates high-level glucose induced retinal ganglion cell damage through STAT3 pathway. Eur. Rev. Med. Pharmacol. Sci. 2018;22:7509–7516. doi: 10.26355/eurrev_201811_16292. [DOI] [PubMed] [Google Scholar]
- 201.Caban M., Omulecki W., Latecka-Krajewska B. Dry eye in Sjögren’s syndrome—Characteristics and therapy. Eur. J. Ophthalmol. 2022:11206721221091375. doi: 10.1177/11206721221091375. online ahead of print . [DOI] [PubMed] [Google Scholar]