Abstract
Introduction
Trauma exposure is a highly prevalent experience for patients and clinicians in emergency medicine (EM). Trauma-informed care (TIC) is an effective framework to mitigate the negative health impacts of trauma. This systematic review synthesizes the range of TIC interventions in EM, with a focus on patient and clinician outcomes, and identifies gaps in the current research on implementing TIC.
Methods
The study was registered with PROSPERO (CRD42020205182). We systematically searched peer-reviewed journals and abstracts in the PubMed, EMBASE (Elsevier), PsycINFO (EBSCO), Social Services Abstract (ProQuest), and CINAHL (EBSCO) databases from 1990 onward on August 12, 2020. We analyzed studies describing explicit TIC interventions in the ED setting using inductive qualitative content analysis to identify recurrent themes and identify unique trauma-informed interventions in each study. Studies not explicitly citing TIC were excluded. Studies were assessed for bias using the Newcastle-Ottawa criteria and Critical Appraisal Skills Programme (CASP) Checklist.
Results
We identified a total of 1,372 studies and abstracts, with 10 meeting inclusion criteria for final analysis. Themes within TIC interventions that emerged included educational interventions, collaborations with allied health professionals and community organizations, and patient and clinician safety interventions. Educational interventions included lectures, online modules, and standardized patient exercises. Collaborations with community organizations focused on addressing social determinants of health. All interventions suggested a positive impact from TIC on either clinicians or patients, but outcomes data remain limited.
Conclusion
Trauma-informed care is a nascent field in EM with limited operationalization of TIC approaches. Future studies with patient and clinician outcomes analyzing universal TIC precautions and systems-level interventions are needed.
INTRODUCTION
Background
Trauma exposure is a highly prevalent experience in the emergency department (ED) for both patients and clinicians.1–6 The Substance Abuse and Mental Health Services Administration (SAMHSA) defines trauma as “an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life-threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.”7 This definition of trauma encompasses experiences that range from individual (eg, car accident, death of a loved one), to interpersonal (eg, interpersonal violence [IPV], discrimination, abuse), to societal (eg, natural disasters, pandemics, terrorist attacks). Newer publications have expanded this definition to explicitly address structural trauma (eg, racism, sexism).8
Patients frequently present to the ED with the types of trauma defined above: individual (medical traumas/injuries); IPV; and societal traumas (gun violence and community violence). In the United States, the yearly incidence of these events range from 1.7 million ED visits for assault-related injury1 to 88,000 due to firearm-related injuries,2 and over 28,000 ED visits attributed to IPV.3 Patients presenting with acute trauma often are survivors of previous traumatic experiences; a survey of survivors of community violence participating in a hospital-based violence intervention program found that 100% of participants reported at least one adverse childhood experience.9 These previous traumatic experiences are not equally distributed, with those self-identified as female, American Indian/Alaskan Native, and Black being more likely to experience several types of adverse childhood experience than those self-identified as male or White.10
For some survivors of trauma, the experience of the ED may be re-traumatizing or trigger past experiences.11 Survivors of trauma may experience emotional dysregulation (ie, trouble controlling strong emotions) or hypervigilance (ie, increased threat perception and reactivity).12 The close interplay between executive functioning and emotional regulation may impact both the patient and the care team’s navigation of the encounter.12 Similarly, hypervigilance could make the often-hectic environment of the ED, as well as interventional procedures, harder to tolerate.12
The ED setting, by virtue of its emergency-level care, presents multiple potential sources for both direct and secondary trauma (ie, indirect exposure to traumatic events) to clinicians and non-clinical staff. The COVID-19 pandemic demonstrated the toll secondary trauma exposure can have on frontline healthcare workers and staff.4 Staff practicing in the ED also experience high rates of workplace violence (ie, direct trauma). 5,6 The combination of direct trauma and secondary trauma likely contributes to the high rates of post-traumatic stress disorder (PTSD) and secondary traumatic stress (STS) experienced by emergency clinicians. About 11.9–16.8% of emergency physicians screen positive for PTSD and STS symptoms at any one time,13–18 and these rates may be even higher in emergency nurses with 33–64% of nursing staff screening positive for at least one symptom of STS.19–21 There is evidence to suggest that non-clinical staff also experience STS from witnessing acute care.22
Importance
Trauma-informed care (TIC) is a framework that aims to prevent re-traumatization in the healthcare setting and promote resilience for both patient and clinicians.23 It is based on six principles: 1) safety; 2) trustworthiness and transparency; 3) peer support; 4) collaboration and mutuality; 5) empowerment, voice, and choice; and 6) cultural, historical, and gender issues.7 Trauma-informed care is increasingly being adopted as an approach to clinical care in both primary and specialty care, including emergency medicine (EM).23–28 In 2012, the US Attorney General National Task Force on Children Exposed to Violence called for all EDs to provide TIC, and for all clinicians interacting with patients experiencing trauma to be trained in TIC.29 Trauma-informed care has been shown to be a cost-effective intervention with clinical benefits to patients and job satisfaction benefits to staff.30–33 However, despite the immense burden of trauma seen in the ED and the benefits of TIC for patients and clinicians, TIC remains a nascent field within EM.
Goals of This Investigation
This review will synthesize evidence on TIC interventions in EM to describe the following research aims: the breadth of TIC interventions being pursued in the physical ED setting; the potential benefits to patients of TIC interventions in the ED; the potential benefits to clinicians and non-clinical staff of TIC interventions in the ED; and to identify gaps in the current research on implementing TIC interventions in the ED.
METHODS
Search Strategy
We searched peer-reviewed journals and abstracts by searching the databases PubMed, EMBASE (Elsevier), PsycINFO (EBSCO), Social Services Abstract (ProQuest), and CINAHL (EBSCO). The searches included keywords and controlled vocabulary terms for the following concepts: the physical space of the ED; clinicians and staff in the ED; and TIC. A full description of search terms can be found in Appendix 1. The final protocol was registered with PROSPERO (CRD42020205182).
Study Selection
Since TIC as a framework was developed in the 1990s, we included studies from 1990 onward to August 12, 2020, when databases were queried. We included any study that involved emergency clinicians (eg, physicians, nurses, nurse practitioners, and physician assistants) and non-clinical staff (eg, administrative staff, security staff, and environmental services staff). We included studies that examined the physical setting of the ED. The review included studies that reported on TIC interventions. Our study focused on TIC as a framework; therefore, studies had to mention TIC explicitly to be included. Studies that mentioned one element of TIC without referencing the framework were not included. A more detailed explanation of the TIC framework is included in Appendix 2. We defined the criteria for intervention broadly to include any explicit application of TIC. This included TIC related to the physical environment of the ED, TIC clinical care in the ED, TIC guiding policies of the ED, and any educational intervention that explicitly instructs on TIC.
Since TIC is a relatively new conceptual framework, we anticipated there would be few if any randomized controlled trials. We anticipated a breadth of outcomes with a broad definition of “intervention.” For this reason, we did not limit the study design. We excluded the following: non-peer reviewed literature; studies not published in English; studies that did not explicitly name TIC as a framework; studies that did not comment on the operationalization of specific interventions; and studies describing trauma-focused treatment for psychiatric symptoms of stress disorders. Studies not meeting our criteria were excluded in the title and abstract screening phase (Figure 1).
Figure 1.
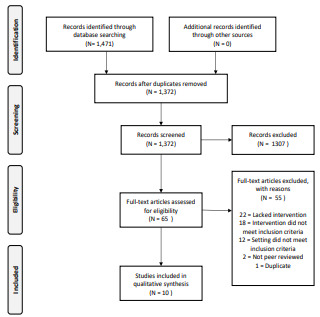
PRISMA flow diagram.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; TIC, trauma-informed care.
The medical librarian (MB) downloaded resulting citations to Covidence Systematic Review Software (Veritas Health Innovation, Melbourne, Australia) and removed duplicate citations. Next, two independent reviews (TB and HA) screened the titles and abstracts of the selected citations for inclusion or exclusion based on our pre-established criteria. When there was disagreement during this phase of screening, the result was included in the full-text review. Reviewers (TB and HA) then assessed full-text articles for inclusion. Conflicts were resolved by a third, more senior reviewer (HS). Risk-of-bias assessment was conducted (HA) using the Newcastle-Ottawa criteria for randomized control trials, cohort studies, and case studies. The Critical Appraisal Skills Programme (CASP) Checklist was used to assess qualitative research studies.
Data Extraction & Analysis
We extracted data manually into Microsoft Excel (Microsoft Corporation, Redmond, WA). For each study we recorded 1) author and date, 2) country, 3) specific intervention, 4) study design, 5) study participants, 6) number of participants, 7) form of trauma, 8) facility type, 9) primary conclusion, and 10) secondary conclusion. Due to the anticipated heterogeneity of results and the early stage of implementation, we did not plan for meta-analysis. We instead chose qualitative thematic analysis across the studies with a focus on unique interventions such as described by Bendall and colleagues.34 Two independent reviewers (TB and HA) used NVivo12 software (QSR International, Melbourne, Australia) to code included studies. We used an inductive content analysis to identify recurrent themes and identify unique trauma-informed interventions in each study.
RESULTS
A total of 1372 studies and abstracts were identified from our search. We excluded 1307 during the title and abstract screen. The majority of the excluded studies in this phase were not relevant as defined by the inclusion and exclusion criteria defined above (ie, trauma studies isolated to physical injury or trauma-focused psychiatric treatment). We assessed 65 articles during the full-text phase and excluded 55 studies, leaving 10 studies for inclusion. Reasons for exclusion during the full-text analysis are included in Figure 1.
Of the 10 studies included, five represent primarily educational interventions and five describe protocols or programs that operationalized a TIC framework. Full details of each article can be found in Table 1. Major quantitative and qualitative results are summarized in Table 2.
Table 1.
Data extraction.
| Author and date | Country | Specific intervention | Design | Study participants | Number of participants | Focus | Facility type |
|---|---|---|---|---|---|---|---|
| Educational interventions | |||||||
|
| |||||||
| Carter-Snell 2020 | Canada | Needs assessment and educational intervention (EESAS) | Participatory action approach | Communities (leaders and stake holders), police, EMS, and ED clinicians | 5 Communities, and 290 Clinicians | Sexual assault | Emergency departments, prehospital |
| Chandramani 2020 | United States | Needs assessment and educational intervention (SANE) | Needs assessment, education intervention | EM nurses, residents and attendings | 95 (41 Nurses, 34 Residents 20 Attendings) | Sexual assault | An urban academic emergency department |
| Cole 2014 | United States | Educational intervention to decrease use of restraints in ED | Case study | EM nurses and emergency physicians | 6 nurses in pilot phase, then “all staff” | Psychologic, mental health | Urban tertiary emergency department |
| Hoysted 2018 | Australia and New Zealand | Web-based training on general TIC principles for pediatric patients | Pilot parallel superiority randomized controlled trial | EM nurses and emergency physicians | 71 (65 Nurses, 6 | Universal precaution | Emergency departments |
| Hall 2016 | Australia | Modular didactic education on TIC and mental health in ED | Exploratory research with a mixed methods design | EM nurses | 34 Nurses | Psychologic, mental health | Emergency department (urban & rural) |
|
| |||||||
| TIC-based programs and protocols | |||||||
|
| |||||||
| Corbin 2010 | United States | Assessment, case management, mentoring, psychoeducational groups, case review | Commentary | Youth (ages 8–30) | NA | Violence | Level 1 trauma center, urban children’s hospital |
| Giles 2019 | United States | TIC assessment and intervention for suicide prevention | Randomized Control trial | Youth | 181 | Suicide and self harm | Tertiary children’s hospital |
| Lakatos 2014 | United States | TIC response to the Boston Marathon bombings | Commentary | Victims of trauma; clinicians | NA | Violence | Level 1 trauma center |
| Stolbach 2017 | United States | TIC screening, support, education, and intervention | Commentary | Youth | NA | Violence | Pediatric emergency department |
| Tiller 2020 | United States | TIC-based protocol for victims of human trafficking (HEAL Toolkit) | Commentary | High-risk patients for trafficking | NA | Human trafficking | Tertiary emergency department |
EMS, emergency medical services; ED, emergency department; EM, emergency medicine; TIC, trauma-informed care.
Table 2.
Major quantitative and qualitative findings for included studies.
| Author and date | Specific intervention | Quantitative findings | Qualitative findings |
|---|---|---|---|
| Education | |||
|
| |||
| Carter-Snell 2020 | Needs assessment and educational intervention (EESAS) | - Comfort providing sexual assault services significantly improved even at 6-month surveys (P <0.01) in emergency clinicians - Knowledge of consequences of sexual assault, mental health considerations, healthcare interventions, and legal considerations improved post training (P < 0.01) |
- Enhanced collaboration across services and issues with ongoing turnover of personnel - Subjective quality of service ratings improved |
| Chandramani 2020 | Needs assessment and educational intervention (SANE) | - Significant improvement in knowledge of elements of assault history 67% to 93% (P < 0.05) and comfort in ability to take history 41% to 86% (P <0.01) in ED residents. -Significant improvement in comfort performing a forensic examination 44% to 87% (P < 0.01) in ED residents. |
- In pre-intervention free response, nine participants mentioned a lack of training and education as a barrier to providing better care - Post survey participants expressed that the educational intervention was very helpful to their ability to care for survivors. |
| Cole 2014 | Educational Intervention to decrease use of restraints in ED | - Initially, 15 to 20 episodes of restraints being used per month, which decreased to no episodes by the end of the intervention. - Overall, ED behavioral health seclusion and restraint hours were reduced from 38.5 h/mo to 0 h/mo after 2 years of the program. |
-Changing the culture through staff understanding of trauma-informed care was key in improving the patient outcomes. -Success of the program depended upon relationship between ED and behavior health department working together. |
| Hoysted 2018 | Web-based training on general TIC principles for pediatric patients | - Training group had significantly greater knowledge following training and at follow-up than the control (P <.001) - Most participants (74.2%) indicated that the training would be useful in their role in the ED |
- Participants liked the online format, found the training to be interesting and informative, and felt the training increased their insight and awareness - Participants stated that there should be more interactive program with the opportunity to practice learned skills |
| Hall 2016 | Modular didactic education on TIC and mental health in ED | - ED nurses reported more confidence in their ability to talk to patients about traumatic experiences (P = 0.001, r = 0.41), respond to disclosures of family violence (P = 0.001, r = 0.41), and understand how their current nursing practice is trauma informed (P = 0.001, r = 0.53) | - Participants had an increased openness to ask questions about trauma and listen to patients’ responses - Participants found the neurobiology component of the education assisted their understanding of trauma |
| TIC-based programs and protocols | |||
| Corbin 2010 | Assessment, case management, mentoring, psychoeducational groups, case review | N/A | Authors concluded a combination of In-hospital peer counseling starting in the ED, outpatient follow-up with home visits to address educational, employment, and behavioral health needs, leads to better all- around care and preventing of future incidents of community violence |
| Giles 2019 | TIC assessment and intervention for suicide prevention | - Patients who received the intervention were significantly more likely to attend outpatient treatment compared with usual care; 79 families (88.8%) received at least one care linkage contact compared to zero in the non-intervention group | - Authors concluded that adding the trauma screening helped to provide trauma-informed care and to link youth directly to trauma- specific, evidenced-based treatments from the ED. |
| Lakatos 2014 | TIC response to the Boston Marathon bombings | N/A | - A team of psychiatric advanced practice nurse using a TIC framework were able to provide comprehensive care to patients, their families, and staff after the Boston Marathon bombings starting in the ED. - Staff reported returning to baseline 3 weeks after the event |
| Stolbach 2017 | TIC screening, support, education, and intervention | N/A | - A TIC-based clinic that first reached out in the ED helped patients recover from the mental harm caused by community violence. |
| Tiller 2020 | TIC-based Protocol for Victims of Human Trafficking (HEAL Toolkit) | N/A | - The development of a TIC standardized protocol ensured that survivors of human trafficking and at-risk patients were treated appropriately and in a standardized manner regardless of the experience of the clinician. |
TIC, trauma-informed care; EMS, emergency medical services; ED, emergency department; EESAS, Enhanced Emergency Sexual Assault Services; SANE, Sexual Assault Nurse Examiners.
No studies were excluded during the risk-of bias assessment. Full results from the risk-of-bias assessment are included in Appendix 3. Themes emerging from the qualitative analysis of unique interventions included the following: education, collaboration, and safety. Our inter-rater reliability score was 0.89. A complete summary of interventions, including those not described fully in the analysis, appears in Table 3.
Table 3.
Unique trauma-informed care interventions by theme.
| Interventions | Publications including intervention |
|---|---|
| Education | |
| Educational needs assessment | 35–37, 39 |
| Education through didactic lecture | 35–38, 40, 41 |
| Education through online modules | 39 |
| Education through standardized patient exercises | 36 |
| Tracking clinician outcomes (knowledge, confidence) | 35, 36, 37, 39, 41 |
| Tracking patient outcomes | 35,37 |
| Education on trauma impacts | 35–39, 42 |
| Education on TIC provision for survivors of sexual assault | 35, 36 |
| Education on mental health and TIC | 37, 41 |
| Education on pediatric traumatic stress | 39 |
| Collaboration | |
| Participatory action model | 35 |
| Educational content production collaboration | 36, 38 |
| Interprofessional collaboration | 35–38, 40, 42 |
| Collaboration between physician specialties | 36, 40, 44 |
| Collaboration with community organizations | 35, 36,38, 40, 44 |
| Collecting patient perspectives | 38 |
| Coordinating outpatient care and follow-up | 38, 40, 43, 44 |
| Safety | |
| Immediate safety assessment | 38, 40, 43, 44 |
| Safety planning prior to discharge | 38, 40, 43, 44 |
| Trauma screening | 38, 40, 43, 44 |
| Psychological first aid for patients and staff | 42 |
| Direction to additional resources and appropriate escalation of care | 38, 41–43 |
| Enhanced patient privacy | 40 |
| ED lockdown with security threat | 40 |
| Leadership | |
| Engage community leaders | 35, 38 |
| Engage hospital leadership | 37, 42 |
| TIC Protocols | |
| Violence intervention and prevention programs | 38, 44 |
| Human trafficking | 40 |
| Environmental Analysis | |
| Analysis of department layout | 35, 37 |
| Analysis of patient care areas | 35, 37 |
| Peer support | |
| Patient peer support groups | 38, 42 |
| Staff peer support groups | 42 |
TIC, trauma-informed care.
Education
Seven papers included an educational component.35–41 Of the interventions collecting data, all reported effectiveness in increasing clinicians’ comfort and knowledge of TIC.35–37,39,41 Educational interventions ranged in length from 15 minutes39 to around eight hours41 and used a variety of mediums including in-person didactics,35–38,40,41 online modules,39 and standardized patient encounters.36 Prior to conducting an educational intervention, many sites conducted needs assessments.35–37,39 Chandramani et al found that clinicians lacked training and confidence in providing TIC to survivors of sexual assault and that they did not understand hospital policy or state laws relating to sexual assault.36 The authors incorporated these findings into subsequent educational interventions.
Educational content across the studies included trauma epidemiology and health impacts,35–39,42 trauma responses,38,42 and TIC clinical skills.35–37,41 All educational interventions focused on specific patient populations including survivors of sexual assault,35,36 community violence,38 human trafficking,40 pediatrics,39 and patients experiencing mental health crises.37,41 Two educational interventions collected patient outcomes data.35,37 One study showed a reduction in the number of patients subjected to restraint and reduced overall patient time in restraints among mental health patients following TIC education of clinicians in the ED.37 Another study showed an improvement in quality of service ratings and consistency of referrals among survivors of sexual assault.35
Collaboration
Eight of the studies included in this review contained a collaboration as an intervention.35–38,40,42–44 Almost all reported how collaboration was important for the success of each intervention. Themes emerging within collaboration included collaboration across physician specialties,36,40,44 collaboration across allied health professions,35–38,40,42 collaboration with community organizations,35,36,38,40,44 and collaboration in arranging post-ED follow-up.38,43,44 Each of the collaborations identified a specific patient population including survivors of community violence,38,44 human trafficking,40 terrorist attacks,42 and pediatric mental health.43
The Healing Hurt People program described by Corbin et al connects survivors of community violence with a host of resources including “obtaining identification and health insurance, substance abuse treatment, post-traumatic stress treatment, healthcare, education, housing, job training and placement, legal assistance, transportation, counseling, and physical rehabilitation” through collaboration with social workers and community organizations.38 Collaborations with community organizations were vital to addressing social determinants of health including housing instability, food insecurity, and economic insecurity.35,36,38,40,44 In developing a protocol for survivors of human trafficking in the ED, Tiller et al collaborated with community organizations to provide survivors with a “list of resources for the patient beyond medical care such as emergency housing, legal assistance, and food pantries.”40 Collaborations with allied health professions were most often with social work38,40 and nursing.36,37,42 Several interventions collaborated with local law enforcement for bi-directional education.35,40
Safety
Six papers detailed interventions operationalizing patient or staff safety using TIC.37,38,40–43 Themes emerging within safety included the following: safety precautions for patient’s emotional and physical wellbeing; interventions to ensure staff’s safety; and safety assessments and planning for patients identified to be victims of violence. Collectively these themes highlighted TIC as an essential component of ensuring a safe environment for both patients and staff.
Trauma-informed care was shown to be critical in fostering patients’ physical and emotional safety. Tiller et al detailed safety precautions as a part of a TIC intervention when caring for victims of suspected human trafficking.40 These interventions included listing the patient under an alias and discussing with the patient how to prevent the discovery of their location through their mobile device.40 However, the most important TIC element of this intervention was empowering the patient to discuss what they thought was best for their safety. This intervention encouraged clinicians to “collaborate with the patient to ensure that we are not jeopardizing safety with our efforts to intervene.”40
Staff safety was discussed in three papers,37,40,42 with the most robust intervention being in response to the Boston Marathon bombings in 2014. Lakatos et al was unique in describing TIC and physiological first aid (PFA) interventions for both patients and staff following the Boston Marathon bombings.42 Using a TIC and complementary PFA framework they constructed nurse-specific groups and interprofessional groups (including members of chaplaincy, occupational health, nursing leadership, psychiatry, psychology, and social services). These groups were designed to provide support for the variety of ways staff might have been affected by the trauma of the bombings.42 The paper emphasizes voluntary supportive services for staff.
Four papers included patient safety assessments,38,40,43,44 and two papers specifically focused on incorporation of TIC principles into these assessments.38,43 Giles et al described how using a TIC framework was foundational in effectively assessing youths at risk for suicide by engaging with them to discuss their hopes, strengths, family support, and ability to practice a safety plan.43 As previously discussed, Corbin et al’s work on the Safety, Emotions, Loss, Future model for youths who have experienced violence includes safety as one of the four foundational concepts.38
Additional Themes
Additional interventions emerging from our analysis included the following: conducting trauma screening and assessment38,40,43,44; securing leadership buy-in from both hospital and community leaders35,37,38,4; developing standardized TIC protocols and programs for vulnerable patient populations36,38,40,44; and environmental analysis of the ED.35,37
DISCUSSION
Trauma-informed care remains an emerging field in EM with limited operationalization despite positive emergency clinician perceptions of TIC.45–48 The concepts formally studied that are related to TIC have shown benefit based on initial, but limited, data.30–32 Our review found 10 studies demonstrating ED interventions explicitly operationalizing a TIC framework. The majority of interventions focused on clinician education and care protocols for historically vulnerable populations (eg, persons impacted by structural racism and oppression). While the data is still preliminary, all included studies showed a positive impact of TIC on either patients or clinicians. Patients reported increased quality of care and increased outpatient referral follow-up rates,35 and when experiencing mental health crises spent less time in restraints.37 Clinicians reported greater clinical knowledge and comfort when providing care for historically vulnerable patient populations.35–37,41,47
Numerous guidelines and best practices for TIC in the ED setting have been published, as we describe in our “Limitations” section. However, operationalization of these best practices and outcomes data remains limited. It may be that the studies are ongoing. For example, the educational interventions included in this review were published between 2014–2020. Most papers included only level 1 and level 2 Kirkpatrick assessments (ie, attitude changes and knowledges gains), and only two included level 3 and level 4 outcomes (ie, clinical practice change and patient outcomes).49 The timing of our review may have been insufficient for most groups to collect patient-centered outcomes. Future studies are needed to establish clinician and patient outcomes related to educational TIC interventions in EM.
Our review identified several gaps in the current interventions: lack of universal precautions education; lack of outcomes data; lack of staff-focused interventions; and lack of cost-effectiveness analysis. Across all interventions, both education- and protocol-driven, there was little to no adoption of TIC as a universal precaution for all patients. All interventions captured in our review rely on a population-specific approach (ie, human trafficking, sexual assault, community violence survivors). While this approach may increase clinicians’ awareness of trauma in specific populations, it does not address needs of patients who do not present with “red flags” or who do not present with trauma-related complaints.
Clinicians cannot always predict which patients have experienced adversity; therefore, future educational and programmatic interventions should emphasize TIC as a universal precaution for all-comers.23 Education should emphasize that TIC offers the opportunity to avoid trauma related to medical care and interventions itself.23 Additionally, only one intervention focused on specifically applying TIC principles to ED staff.42 As detailed in the introduction, both clinical and non-clinical ED staff are at high risk for traumatization and re-traumatization based on their work environment.4,5,22 This remains a key area for application of the TIC framework within EM. An increasingly urgent research need is developing in the wake of the COVID-19 pandemic. Future studies with TIC staff-focused interventions would benefit from outcomes data such as validated measures of burnout, PTSD, and STS screening tools.
This review also uncovered a lack of process analysis and environmental analysis of the ED itself. Only two interventions evaluated how the physical space of the ED could be evaluated and improved using a TIC framework.35,37 None of the interventions examined cost effectiveness or return on investment when TIC models are used, representing another gap in the research. The original studies developing TIC showed no additional cost when the model was employed.32 To fully advocate for TIC interventions, especially operational interventions, future studies must include a cost-effectiveness analysis.
The SAMHSA guidelines on TIC include steps for creating trauma-informed institutions and organziations.12 Many sectors have adopted these guidelines including social work,50 elementary education,51 and juvenile justice.52 Future studies are needed that analyze the ED from an operational level using a TIC framework. These studies should also include non-clinical ED staff.
LIMITATIONS
Our paper has several limitations that warrant discussion. Most importantly, by requiring the explicit reference to TIC, we excluded interventions that used principles of TIC without explicitly naming the theory. For example, Cheng et al describe a peer support-based ED violence intervention program in their 2008 paper, and although peer support is one of the six principles of TIC, we did not include the paper in our review as it did not explicitly mention TIC as a guiding framework.53 Other violence intervention programs similarly were not included, even though referred to in the literature as “trauma-informed,” because their original publications do not mention TIC.54,55 Additionally, many papers were excluded due to lack of operationalization of TIC. Many publications described best practices without describing interventions. Guidelines and best practices for TIC care of ED patients experiencing mental health crises,56,57 sexual assault survivors,58–60 survivors of community violence,28 victims of human trafficking,61–64 and pediatric patients experiencing trauma65 were all excluded due to lack of operationalization. Finally, our search excluded non-English language studies. and we did not conduct a hand search; therefore, we may not have captured all available interventions.
CONCLUSION
This paper represents the first systematic review of trauma-informed care interventions in the ED setting. The results of the review show that TIC is a small but growing field in the clinical practice of EM. However, an urgent need remains for additional studies to evaluate potential benefits for patients and clinician in the field of EM. With wider adoption of TIC interventions, the ED can be a place of healing for patients and clinicians.
Supplementary Information
Footnotes
Section Editor: Leslie Zun, MD, MBA
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. This work was funded by the Robert Wood Johnson Foundation Clinical Scholars Program. There are no conflicts of interest to declare.
REFERENCES
- 1.Centers for Disease Control and Prevention. Violence Prevention at CDC. 2020. [Accessed July 15, 2020]. Available at: https://www.cdc.gov/violenceprevention/publichealthissue/index.html.
- 2.Gani F, Sakran JV, Canner JK. Emergency department visits for firearm-related injuries in the United States, 2006–14. Health Affairs. 2017;36(10):1729–38. doi: 10.1377/hlthaff.2017.0625. [DOI] [PubMed] [Google Scholar]
- 3.Davidov DM, Larrabee H, Davis SM. United States emergency department visits coded for intimate partner violence. J Emerg Med. 2015;48(1):94–100. doi: 10.1016/j.jemermed.2014.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marketing General Incorporated. ACEP Emergency Department Violence Poll Research Results. 2018. [Accessed July 15, 2020]. Available at: https://www.emergencyphysicians.org/globalassets/files/pdfs/2018acep-emergency-department-violence-pollresults-2.pdf.
- 6.Emergency Nurses Association. Emergency Department Violence Surveillance Study. 2011. [Accessed July 15, 2020]. Available at: http://www.ncdsv.org/images/ENA_EmergencyDeptViolenceSurveillanceStudy_November2011.pdf.
- 7.SAMHSA’s Trauma and Justice Strategic Initiative. SAMHSA’s Concept of Trauma and Guidance for a Trauma-informed Approach. 2014. [Accessed June 1, 2020]. Available at: https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf.
- 8.Lewis-O’Connor A, Warren A, Lee JV, et al. The state of the science on trauma inquiry. Womens Health (Lond Engl) 2019;15:174550651986123. doi: 10.1177/1745506519861234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corbin TJ, Purtle J, Rich LJ, et al. The prevalence of trauma and childhood adversity in an urban, hospital-based violence intervention program. J Health Care Poor Underserved. 2013;24(3):1021–30. doi: 10.1353/hpu.2013.0120. [DOI] [PubMed] [Google Scholar]
- 10.Merrick MT, Ford DC, Ports KA, et al. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep. 2019;68(44):999–1005. doi: 10.15585/mmwr.mm6844e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Purkey E, Davison C, MacKenzie M, et al. Experience of emergency department use among persons with a history of adverse childhood experiences. BMC Health Serv Res. 2020;20(1):455. doi: 10.1186/s12913-020-05291-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration. Trauma-informed care in behavioral health services. 2014. [Accessed July 15, 2020]. Available at: https://store.samhsa.gov/product/TIP-57-Trauma-Informed-Care-in-Behavioral-Health-Services/SMA14-4816. [PubMed]
- 13.DeLucia JA, Bitter C, Fitzgerald J, et al. Prevalence of post-traumatic stress disorder in emergency physicians in the United States. West J Emerg Med. 2019;20(5):740–6. doi: 10.5811/westjem.2019.7.42671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roden-Foreman JW, Bennett MM, Rainey EE, et al. Secondary traumatic stress in emergency medicine clinicians. Cognitive Behaviour Therapy. 2017;46(6):522–32. doi: 10.1080/16506073.2017.1315612. [DOI] [PubMed] [Google Scholar]
- 15.Mills LD, Mills TJ. Symptoms of post-traumatic stress disorder among emergency medicine residents. J Emerg Med. 2005;28(1):1–4. doi: 10.1016/j.jemermed.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Pajonk F-GB, Cransac P, Müller V, et al. Trauma and stress-related disorders in German emergency physicians: the predictive role of personality factors. Int J Emerg Ment Health. 2012;14(4):257–68. [PubMed] [Google Scholar]
- 17.Zafar W, Khan UR, Siddiqui SA, et al. Workplace violence and self-reported psychological health: coping with post-traumatic stress, mental distress, and burnout among physicians working in the emergency departments compared to other specialties in Pakistan. J Emerg Med. 2016;50(1):167–77e1. doi: 10.1016/j.jemermed.2015.02.049. [DOI] [PubMed] [Google Scholar]
- 18.Somville FJ, De Gucht V, Maes S. The impact of occupational hazards and traumatic events among Belgian emergency physicians. Scand J Trauma Resusc Emerg Med. 2016;24:59. doi: 10.1186/s13049-016-0249-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duffy E, Avalos G, Dowling M. Secondary traumatic stress among emergency nurses: a cross-sectional study. Int Emerg Nurs. 2015;23(2):53–8. doi: 10.1016/j.ienj.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Morrison LE, Joy JP. Secondary traumatic stress in the emergency department. J Adv Nurs. 2016;72(11):2894–906. doi: 10.1111/jan.13030. [DOI] [PubMed] [Google Scholar]
- 21.Dominguez-Gomez E, Rutledge DN. Prevalence of secondary traumatic stress among emergency nurses. J Emerg Nurs. 2009;35(3):199–204. doi: 10.1016/j.jen.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Chesham B, Dawber C. The “All of Us” study – Non-clinical staff members’ experience of performing cardiopulmonary resuscitation in acute care settings. Australasian Emergency Care. 2019;22(4):243–8. doi: 10.1016/j.auec.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Raja S, Hasnain M, Hoersch M, et al. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health. 2015;38(3):216–26. doi: 10.1097/FCH.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 24.Machtinger EL, Cuca YP, Khanna N, et al. From treatment to healing: the promise of trauma-informed primary care. Women’s Health Issues. 2015;25(3):193–7. doi: 10.1016/j.whi.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Marsac ML, Kassam-Adams N, Hildenbrand AK, et al. Implementing a trauma-informed approach in pediatric health care networks. JAMA Pediatr. 2016;170(1):70. doi: 10.1001/jamapediatrics.2015.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimberg L, Wheeler M. Trauma and trauma-informed care. In: Gerber MR, editor. Trauma-Informed Healthcare Approaches. Springer International Publishing; 2019. 2019. pp. 25–56. [Google Scholar]
- 27.Raja S, Hoersch M, Rajagopalan CF, et al. Treating patients with traumatic life experiences. J Am Dent Assoc. 2014;145(3):238–45. doi: 10.14219/jada.2013.30. [DOI] [PubMed] [Google Scholar]
- 28.Fischer KR, Bakes KM, Corbin TJ, et al. Trauma-informed care for violently injured patients in the emergency department. Ann Emerg Med. 2019;73(2):193–202. doi: 10.1016/j.annemergmed.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 29.Listenbee R, Torre J, Boyle G, et al. Report of the Attorney General’s National Task Force on Children Exposed to Violence. 2012. [Accessed January 29, 2021]. Available at: https://www.justice.gov/defendingchildhood/cev-rpt-full.pdf.
- 30.Shibru D, Zahnd E, Becker M, et al. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–9. doi: 10.1016/j.jamcollsurg.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 31.Purtle J, Dicker R, Cooper C, et al. Hospital-based violence intervention programs save lives and money. J Trauma Acute Surg. 2013;75(2):331–333. doi: 10.1097/TA.0b013e318294f518. [DOI] [PubMed] [Google Scholar]
- 32.Cocozza JJ, Jackson EW, Hennigan K, et al. Outcomes for women with co-occurring disorders and trauma: program-level effects. J Subst Abuse Treat. 2005;28(2):109–19. doi: 10.1016/j.jsat.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 33.Hales TW, Nochajski TH, Green SA, et al. An association between implementing trauma-informed care and staff satisfaction. ASW. 2017;18(1):300–12. [Google Scholar]
- 34.Bendall S, Eastwood O, Cox G, et al. A systematic review and synthesis of trauma-informed care within outpatient and counseling health settings for young people. Child Maltreat. 2021;26(3):313–24. doi: 10.1177/1077559520927468. [DOI] [PubMed] [Google Scholar]
- 35.Carter-Snell C, Jakubec S, Hagen B. Collaboration with rural and remote communities to improve sexual assault services. J Community Health. 2020;45(2):377–87. doi: 10.1007/s10900-019-00744-4. [DOI] [PubMed] [Google Scholar]
- 36.Chandramani A, Dussault N, Parameswaran R, et al. A needs assessment and educational intervention addressing the care of sexual assault patients in the emergency department. J Forens Nurs. 2020;16(2):73–82. doi: 10.1097/JFN.0000000000000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cole R. Reducing restraint use in a trauma center emergency room. Nurs Clin North Am. 2014;49(3):371–81. doi: 10.1016/j.cnur.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 38.Corbin TJ, Rich JA, Bloom SL, et al. Developing a trauma-informed, emergency department–based intervention for victims of urban violence. J Trauma Dissociation. 2011;12(5):510–25. doi: 10.1080/15299732.2011.593260. [DOI] [PubMed] [Google Scholar]
- 39.Hoysted C, Jobson L, Alisic E. A pilot randomized controlled trial evaluating a web-based training program on pediatric medical traumatic stress and trauma-informed care for emergency department staff. Psychol Serv. 2019;16(1):38–47. doi: 10.1037/ser0000247. [DOI] [PubMed] [Google Scholar]
- 40.Tiller J, Reynolds S. Human trafficking in the emergency department: improving our response to a vulnerable population. West J Emerg Med. 2020;21(3):549–54. doi: 10.5811/westjem.2020.1.41690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall A, McKenna B, Dearie V, et al. Educating emergency department nurses about trauma informed care for people presenting with mental health crisis: a pilot study. BMC Nurs. 2016;15(1):21. doi: 10.1186/s12912-016-0141-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lakatos BE, Delisle L, Mitchell M, et al. Psychiatric advanced practice nurses’ contributions to supporting survivors and caregivers affected by the Boston Marathon bombings. Clin Nurse Spec. 2014;28(2):92–6. doi: 10.1097/NUR.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 43.Giles L. Utilizing a trauma-informed therapeutic intervention in the emergency department for risk assessment. J Am Acad Child Adolesc Psychiatry. 2019;58(10):S305–S306. [Google Scholar]
- 44.Stolbach B. The University of Chicago Medicine React Program: recovery and empowerment after community trauma. J Am Acad Child Adolesc Psychiatry. 2017;56(10):S29. [Google Scholar]
- 45.Gerace A, Muir-Cochrane E. Perceptions of nurses working with psychiatric consumers regarding the elimination of seclusion and restraint in psychiatric inpatient settings and emergency departments: An Australian survey. Int J Ment Health Nurs. 2019;28(1):209–25. doi: 10.1111/inm.12522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kassam-Adams N, Rzucidlo S, Campbell M, et al. Nurses’ views and current practice of trauma-informed pediatric nursing care. J Pediatr Nurs. 2015;30(3):478–84. doi: 10.1016/j.pedn.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 47.Hoysted C, Babl FE, Kassam-Adams N, et al. Perspectives of hospital emergency department staff on trauma-informed care for injured children: An Australian and New Zealand analysis: perspectives on trauma-informed care. J Paediatr Child Health. 2017;53(9):862–9. doi: 10.1111/jpc.13644. [DOI] [PubMed] [Google Scholar]
- 48.Bruce MM, Kassam-Adams N, Rogers M, et al. Trauma providers’ knowledge, views, and practice of trauma-informed care. J Trauma Nurs. 2018;25(2):131–8. doi: 10.1097/JTN.0000000000000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kirkpatrick DL, Kirkpatrick JD. Evaluating Training Programs: The Four Levels. Syndey, AUS: ReadHowYouWant; 2010. [Google Scholar]
- 50.Levenson J. Trauma-Informed Social Work Practice. Soc Work. 2017;62(2):105–13. doi: 10.1093/sw/swx001. [DOI] [PubMed] [Google Scholar]
- 51.Walkley M, Cox TL. Building trauma-informed schools and communities. Children & Schools. 2013;35(2):123–6. [Google Scholar]
- 52.Griffin G, Germain EJ, Wilkerson RG. Using a trauma-informed approach in juvenile justice institutions. Journ Child Adol Trauma. 2012;5(3):271–83. [Google Scholar]
- 53.Cheng TL, Haynie D, Brenner R, et al. Effectiveness of a mentor-implemented, violence prevention intervention for assault-injured youths presenting to the emergency department: results of a randomized trial. Pediatrics. 2008;122(5):938–46. doi: 10.1542/peds.2007-2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Becker MG, Hall JS, Ursic CM, et al. Caught in the crossfire: the effects of a peer-based intervention program for violently injured youth. J Adolesc Health. 2004;34(3):177–83. doi: 10.1016/j.jadohealth.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 55.James TL, Bibi S, Langlois BK, et al. Boston Violence Intervention Advocacy Program: a qualitative study of client experiences and perceived effect. Acad Emerg Med. 2014;21(7):742–51. doi: 10.1111/acem.12409. [DOI] [PubMed] [Google Scholar]
- 56.Molloy L, Fields L, Trostian B, et al. Trauma-informed care for people presenting to the emergency department with mental health issues. Emerg Nurse. 2020;28(2):30–5. doi: 10.7748/en.2020.e1990. [DOI] [PubMed] [Google Scholar]
- 57.Heppell PJ, Rao S. Social services and behavioral emergencies. Child Adolesc Psychiatr Clin N Am. 2018;27(3):455–65. doi: 10.1016/j.chc.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 58.Banvard-Fox C, Linger M, Paulson DJ, et al. Sexual assault in adolescents. Prim Care. 2020;47(2):331–49. doi: 10.1016/j.pop.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alpert EJ. A just outcome, or ‘just’ an outcome? Towards trauma-informed and survivor-focused emergency responses to sexual assault. Emerg Med J. 2018;35(12):753–4. doi: 10.1136/emermed-2018-208099. [DOI] [PubMed] [Google Scholar]
- 60.Smith T, Chauvin-Kimoff L, Baird B, et al. The medical evaluation of prepubertal children with suspected sexual abuse. Paediatr Child Health. 2020;25(3):180–6. doi: 10.1093/pch/pxaa019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Macias-Konstantopoulos W. Human trafficking: the role of medicine in interrupting the cycle of abuse and violence. Ann Intern Med. 2016;165(8):582–8. doi: 10.7326/M16-0094. [DOI] [PubMed] [Google Scholar]
- 62.Hachey LM, Phillippi JC. Identification and management of human trafficking victims in the emergency department. Adv Emerg Nurs J. 2017;39(1):31–51. doi: 10.1097/TME.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 63.Greenbaum J. Identifying victims of human trafficking in the emergency department. Clin Pediatr Emerg Med. 2016;17(4):241–8. [Google Scholar]
- 64.Nichols A, Edmond T, Heil E, editors. Social Work Practice with Survivors of Sex Trafficking and Commercial Sexual Exploitation. New York NY: Columbia University Press; 2018. Identification, assessment, and outreach; pp. 18–32. [Google Scholar]
- 65.Jordan KS. Minimizing pediatric traumatic stress through a trauma-informed approach in the emergency department. J Emerg Nurs. 2019;45(3):319–22. doi: 10.1016/j.jen.2018.12.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


