Abstract
Italy and Belgium have been among the first western countries to face the Coronavirus disease 2019 (COVID-19) emergency, imposing a total lockdown over the entire national territories. These limitations have proven effective in slowing down the spread of the infection. However, the benefits obtained in public health have come with huge costs in terms of social, economic, and psychological well-being. In the current study, we aimed to investigate how the period of home confinement affected self-reported sleep characteristics in Italians and Belgians, with special regard to sleep timing and subjective quality. Using an online survey we collected data from 2272 participants, 1622 Italians (Mage = 34.1 ± 13.6 years, 1171 F), and 650 Belgian (Mage = 43.0 ± 16.8 years, 509 F). Participants reported their sleep pattern (eg, bedtime, risetime) and perceived sleep quality during and, retrospectively, before the lockdown. During the lockdown, sleep timing was significantly delayed, time spent in bed increased, and sleep quality was markedly impaired in both Italians and Belgians. The most vulnerable individuals appeared to be women, subjects experiencing a more negative mood, and those perceiving the pandemic situation as highly stressful. However, the two samples differed in the subgroups most affected by the changes, possibly because of the different welfare systems of the two countries. In fact, in the Italian sample sleep quality and timing underwent significant modifications especially in unemployed participants, whereas in the Belgian sample this category was the one who suffered less from the restrictions. Considering that the novel coronavirus has spread across the whole globe, involving countries with different types of health and welfare systems, understanding which policy measures have the most effective protective role on physical and mental health is of primary importance.
Keywords: Circadian rhythms, COVID-19, Home confinement, Sleep, Working status
1. Introduction
Italy has been the first western country to face the Coronavirus disease 2019 (COVID-19) emergency and, starting from February 2020, the epidemic spread quickly through Europe. In Italy, more than 8000 people had officially contracted the disease by March 9th 2020 [1], so that on this date the Italian Government imposed a total lockdown over the entire national territory (effective from March 10th until May 3rd). A similar scenario occurred in Belgium, with a total lockdown imposed by the Government on March 18th 2020, and effective until May 4th.
During the lockdown, most activities were provisionally closed, including schools, universities, the majority of firms and industries, and non-essential stores. People could leave their homes only when strictly necessary (eg, to buy food and medicines or to seek medical help). Education (both for school and university grades) was carried out through the Internet, as well as most working activities (ie, through home working). Indeed, only a limited number of workers were allowed to reach their usual workplace, while many had to interrupt or even lost their jobs. Families had to look after their children at home round the clock and dear ones living in different houses were separated for weeks.
These limitations have proven effective in slowing down the spread of the infection (its curve started sloping down by the end of March 2020 in Italy and a few weeks later in Belgium) and reducing the number of casualties due to the COVID-19, so that a shift to less restrictive measures was eventually made possible in May 2020. However, the benefits obtained in public health have come with huge costs in terms of social, economic, and psychological well-being.
It has already been reported that prolonged home confinement affected people's physical and mental health [[2], [3], [4]]. Besides the fear of contagion, the uncertainty of the situation, and the lack of face-to-face social interactions, home confinement is associated with reduced exposure to daylight, limited physical activity, and disruption of daily routines [[5], [6], [7]]. These changes had a dramatic impact on psychological well-being and sleep/wake patterns [3]. Early studies on the effect of COVID-19 restrictions on sleep have shown the presence of relevant sleep problems across the world [[7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18]]. However, only a few studies, with rather small-sized samples, reported comparisons of sleep quality and habits during the lockdown with those before the lockdown. A US-based study on 145 students during the quarantine showed a delay in sleep timing (ie, midsleep) of about 50 min during weekdays and about 25 min on weekends [19]. Another study on 435 participants from Switzerland, Germany, and Austria showed that during the lockdown perceived sleep quality (assessed through a single question) was significantly reduced [20]. An Italian study showed a sleep quality worsening, increased insomnia symptoms, a delayed bed- and risetime on 400 participants, in particular in students and females [15]. Finally, two previous studies from our group (conducted on younger samples than that of the present study), showed delayed sleep timing and lower sleep quality compared to the period preceding the lockdown [9,21]. In sum, the available studies indicate that during the lockdown, 1) sleep quality was markedly compromised, and 2) sleep timing was delayed.
Here, we aimed to more deeply investigate how the COVID-19-related restrictions affected people's self-reported sleep timing and sleep characteristics by addressing these variables in a larger and more heterogeneous population. We investigated the possible changes of these variables during the lockdown not only in a larger Italian sample, with a wider age range and different geographical distribution, but also in the Belgian population, experiencing the same dramatic kind of social confinement but in a country with a different culture, latitude, and baseline sleep-wake habits. In doing so, we also intend to better characterize these changes by taking into account several demographic variables, including age, gender, and working condition during the lockdown.
2. Methods
2.1. Study design and procedure
In both countries, participants completed an anonymous, online survey, from April 1st to May 19th, 2020. The survey was advertised across the whole nation via social media and University websites. To take part in the survey, participants were asked to read the aims of the study and to explicitly agree to participate in the survey by filling the written consent form. After a few sociodemographic questions (eg, age, gender, employment status), and some ad-hoc questions related to the COVID-19, a set of standardized questionnaires were presented to the participants, including the Pittsburgh Sleep Quality Index [22]. Participants had to respond referring to their current situation (ie, after March 11th for Italy and March 20th for Belgium) and, retrospectively, to their situation before the lockdown (ie, until March 10th for Italy and March 19th for Belgium). The survey took approximately 25 min to be completed. There was no money or credit compensation for participating in the study. The study protocol was approved by the local ethical committees and was conducted in accordance with the Declaration of Helsinki.
A total of 2272 participants completed the survey (1622 from the Italian and 650 from the Belgian territory). Data reported here were part of a wider research project designed to assess several aspects of sleep characteristics during the quarantine, and other data with different research purposes will be presented elsewhere.
2.2. COVID-19 questions
Several ad-hoc questions related to the COVID-19 emergency were presented. These included, for instance, whether the participants had individuals infected by the COVID-19 among their acquaintances, whether they were worried about their job or education, about the health of their dear ones or about being infected, etc. (0–1 response). We also asked participants whether their working condition had changed during the lockdown (ie, working from home/remote working, stopped working), how stressed and afraid they felt (on a 3-point scale, ie not at all, moderately, extremely), and how their mood was (on a 5-point scale from extremely positive to extremely negative).
2.3. Sleep timing and quality
Sleep timing and quality were assessed using the PSQI [22]. The scoring ranges from 0 to 21, with higher scores indicating worse sleep quality and 5 as a cut-off score to differentiate good from poor sleep [22]. From the PSQI questions, we also derived information about bedtime (hh:mm) and risetime (hh:mm), hours spent in bed (hrs), sleep duration (hrs), sleep onset latency (min), sleep midpoint (hh:mm), and use of medication for sleeping (either prescribed or over the counter). Each of the questions required two answers: one referring to the current situation and one to the participant's situation before the lockdown.
2.4. Statistical analysis
To assess the changes of sleep parameters across different periods (before and during the lockdown), we employed linear mixed models (LMM), which take into account factors whose levels are randomly extracted from a population (ie, participants), allowing for more generalizable results [23]. We built separate models for sleep quality, sleep timing (bedtime and risetime), time in bed, sleep duration, and sleep onset latency, using Participant as crossed random effects and Lockdown (Before/During Lockdown), Gender (Female/Male), and Work condition (Student, Unemployed/Retired, Stopped working, Remote working, Regular working) as fixed effects, and Age as a covariate. For the Belgian sample, only one participant stopped working during the lockdown and was included in the “Unemployed/Retired” category. Therefore, for the Belgian analysis Work condition was composed of 4 categories (Students, Unemployed/Retired, Remote working, Regular working).
The Holm test was used for post-hoc comparisons. Logistic regressions were conducted to assess the effect of demographic variables (age, gender), presence of sleep issues before the lockdown, use of sleeping pills before the lockdown, and mood, stress, fear of the situation, and fear of being infected (or a relative being infected) in predicting the risk of poor sleep. For each significant predictor, we reported the Odds ratio (OR) and its 95% confidence interval. A p < 0.05 was considered statistically significant. All analyses were run in JASP 0.12.2 (JASP Team, 2020) and JAMOVI 1.2 (The Jamovi Project, 2020).
3. Results
3.1. Descriptive statistics
3.1.1. Italian sample
Out of the 1622 participants (Mage = 34.1 ± 13.6 years, 1171 F), 909 were workers (Mage = 41.4 ± 12.3 years, 608 F), 591 were university students (Mage = 22.5 ± 3.30 years, 473 F), and 122 were unemployed or retired (Mage = 35.7 ± 14.09 years, 90 F). Among the workers, during the lockdown, 22.3% (203, 130 F) continued working at their regular workplace, 49.2% (447, 296 F) started to work in smart modality, and 28.5% (259, 182 F) had to stop working. The majority of the sample (60.2%, n = 974) was from Southern Italy, 28.6% (n = 463) from Central Italy, 11.1% (n = 180) from Northern Italy.
As for psychological factors, 37.5% of the sample reported negative mood, 29.8% reported a neutral mood, whereas the remaining 35.6% reported a positive mood during the quarantine. Most participants (68.2%) reported to be moderately afraid of the COVID-19 emergency, 11.1% to be extremely afraid, and 20.7% to be not at all afraid. Regarding the risk of infection (for oneself or dear ones), 56.3% of the sample reported to be moderately afraid, 36.1% to be extremely afraid, and only 7.6% to be not at all afraid. Similarly, 67.3% of participants reported to be moderately stressed by the COVID-19 situation, 14.2% to be extremely stressed, and 18.5% not to be stressed at all.
Most participants were worried about dear ones (95.6%), economic issues (89%), risk of infection (81.5%), and about working (68.2% of the workers) and academic conditions (92.5% of the students). Also, 37.5% (n = 608) of the sample was acquainted with someone who had been infected by the coronavirus.
3.1.2. Belgian sample
Of the 650 participants (Mage = 43.0 ± 16.8 years, 509 F), 417 were workers (Mage = 40.7 ± 12.2 years, 344 F), 89 were university students (Mage = 23.7 ± 6.4 years, 79 F), and 144 were unemployed or retired (Mage = 61.8 ± 14.8 years, 86 F). Among the workers, during the lockdown, 54.7% (228, 190 F) continued working as usual whereas 45.3% (189, 154 F) started to work in smart modality.
During the quarantine, negative mood was reported by 22.3% of the sample, neutral mood by 27.2%, whereas the remaining 50.5% reported a positive mood. As for general fear about the health emergency, 37% of participants were moderately afraid, 15.7% were extremely afraid, whereas 47.3% reported being not at all afraid. Moreover, 35.2% of the sample reported to be moderately afraid of being infected or that dear ones could be infected, 41.2% to be extremely afraid, and 23.6% to be not at all afraid. Moderate stress related to the COVID-19 situation was reported by 32.3% of the sample, extreme stress by 33.7%, whereas 34.0% did not feel stressed at all.
Two-thirds of the sample were worried about dear ones (67.7%), less than half about economic issues (44.4%), and about being infected (37.2%). Only 24.5% of the workers were worried about their work situation (68.2% of the workers) whereas 86.5% of the students were worried about their academic situation. Finally, 14.5% (n = 94) of the sample knew someone who had been infected by the COVID-19.
3.2. Effects of the lockdown on sleep
3.2.1. Italian sample
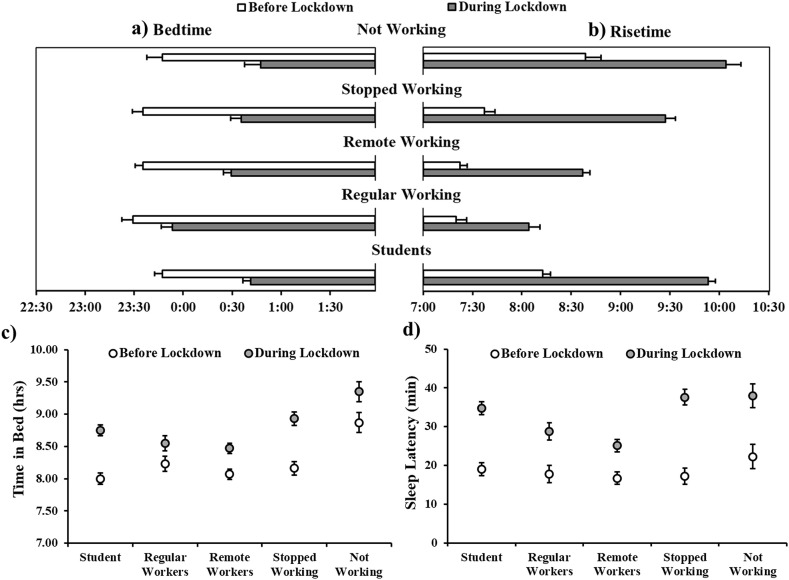
Sleep timing markedly shifted during the lockdown. Subjects tended to go to bed later (F1,1612 = 286.91, p < 0.001), and this effect was mediated by the working status (F4,1611 = 5.40, p < 0.001, Fig. 1 a). Specifically, students and smart workers tended to go to bed 54 min later (p's < 0.001), and participants who were unemployed/retired and those who had to stop working tended to go to bed 1 h later (p's < 0.001). Interestingly, even individuals who continued working regularly tended to delay their bedtime by 24 min (p = 0.004). We also observed a significant effect of Gender (F1,1612 = 12.54, p < 0.001), with males tending, in general, to go to bed later than females, although the Lockdown × Gender interaction was not significant (F1,1612 = 0.20, p = 0.665). Age was not a significant covariate (p = 0.587). The shift in bedtime was mirrored by a delayed risetime during the quarantine (F1,1612 = 783.77, p < 0.001), and, again, this effect was mediated by the working status (F4,1611 = 21.25, p < 0.001, Fig. 1b). In particular, students got up 1 h and 40 min later and individuals who had to stop working tended to get up 1 h and 50 min later than before the lockdown. Unemployed/retired and smart workers got up 1 h and 25 min and 1 h and 14 min later, respectively, whereas individuals who continued working regularly got up 44 min later (all p's < 0.001). Again, we observed a significant effect of Gender (F1,1611 = 5.39, p = 0.020), with females getting up 10 min earlier than males, although the Lockdown × Gender interaction was not significant (F1,1612 = 2.35, p = 0.125). Age turned out to be a significant covariate (coeff. = −0.04, t = −12.33, p < 0.001), with younger subjects getting up later.
Fig. 1.
a) Bedtime b) Risetime, c) Time in Bed, and d) Sleep Latency as a function of the presence of the lockdown and the working condition of the participants in the Italian sample. Error bars represent standard errors of the means.
These changes in bed- and risetimes are reflected in the observed shift in sleep midpoint during the quarantine (F1,1612 = 788.18, p < 0.001), which was found to be affected, again, by working status (F4,1611 = 14.48, p < 0.001). Specifically, sleep midpoint was delayed of 1 h and 18 min in students and in unemployed/retired participants, 1 h and 24 min in subjects who stopped working, and 1 h in smart workers (all p's < 0.001). Though less pronounced, a delay was also observed in regular workers (∼36 min, p < 0.001). We observed a significant effect of Gender (F1,1611 = 10.24, p = 0.001), with males' sleep midpoint occurring 18 min later than that of females, although the Lockdown × Gender interaction was not significant (F1,1612 = 0.05, p = 0.819). Age was again a significant covariate (coeff. = −0.02, t = −6.36, p < 0.001), with younger participants showing later sleep midpoints during the quarantine.
The shift in sleep timing (delayed bedtimes and risetimes) observed during the lockdown was accompanied by an increased duration of time spent in bed (33 min; F1,1612 = 119.85, p < 0.001), with differences depending on working condition (Lockdown × Work: F4,1612 = 4.54, p = 0.001, Fig. 1c) and gender (Lockdown × Gender: F1,1612 = 4.91, p = 0.027). Compared to the period before the restrictions, regular workers spent in bed only 19 min more (p = 0.095), unemployed/retired subjects ∼24 min more (p = 0.056), whereas students, smart workers, and participants who had stopped working significantly increased the time spent in bed up to 46 min (all p's < 0.001). Before the lockdown males tended to spend less time in bed than females (p = 0.037), whereas during the lockdown this difference disappeared (p = 0.934). Age was a significant covariate (coeff. = −0.04, t = −12.09, p < 0.001): the younger the age, the longer the time spent in bed.
Sleep duration showed a trend to increase of 5 min during the lockdown (F1,1612 = 3.03, p = 0.082). There was a significant main effect of Gender (F1,1611 = 8.03, p = 0.005), with females sleeping overall 11 min more than males, and a significant Lockdown × Gender interaction (F1,1612 = 14.76, p < 0.001), with females sleeping 6 min more during the lockdown whereas males slept 16 min more. Age was again a significant covariate (coeff. = −0.03, t = −9.94, p < 0.001): the younger the age, the longest the time spent asleep during the quarantine.
Sleep latency also showed a significant increase during the period of home confinement (∼14.5 min; F1,1612 = 189.04, p < 0.001), again with differences linked to gender (Lockdown × Gender: F1,1612 = 4.07, p = 0.002) and working condition (Lockdown × Work: F4,1612 = 4.13, p < 0.001, Fig. 1d). Before the lockdown, sleep latency did not differ between genders (p = 0.998). During the lockdown, instead, while females took on average 17.5 min more than before to fall asleep, for males the difference was 11 min (all p's ≤ 0.001). The increase in sleep latency in the various working status subgroups ranged from 8.4 min in the regular workers to 20.4 min in those who had to stop working (all p's < 0.001). Age was a significant covariate (coeff. = −0.24, t = −3.83, p < 0.001), with younger subjects taking longer to fall asleep.
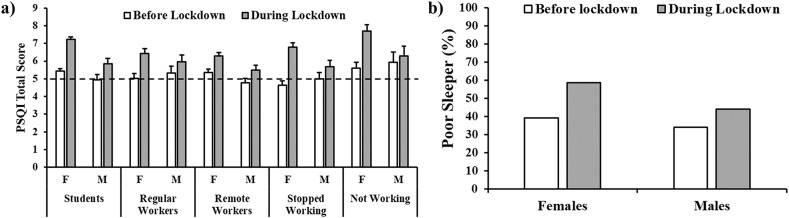
Sleep quality (indexed by the PSQI total score) significantly decreased during lockdown (F1,1612 = 101.51, p < 0.001), especially in female participants (Lockdown × Gender: F1,1612 = 19.31, p < 0.001; see Fig. 2 a). We also observed a significant effect of the working condition (F1,1612 = 2.96, p = 0.019), with unemployed/retired subjects reporting the worst sleep quality, although the interaction Lockdown × Work interaction was not significant (F4,1612 = 1.40, p = 0.232). Age was not a significant covariate (p = 0.232). The proportion of poor sleepers (ie, PSQI>5) increased with the lockdown from 37.7% to 54.2% (χ2 1 = 113, p < 0.001), with a greater increase in females (from 39.11% to 58.07%) than males (from 34.15% to 44.12%, Fig. 2b).
Fig. 2.
a) Pittsburgh Sleep Quality Index (PSQI) total score before and during lockdown as a function of gender and working condition in the Italian sample. Error bars represent standard error of the means. The dashed line represents the cut-off for the good and poor sleepers. b) Frequency of females and males poor sleepers (PSQI >5) before and during the lockdown in the Italian sample.
Lastly, the proportion of responders who used sleeping aids, as assessed by the PSQI, decreased from 12.3% to 10.3%.
Logistic regressions (χ2(15) = 378, p < 0.001. McFadden's R2 = 0.169) confirmed that the risk of poor sleep during the quarantine was higher for subjects already displaying poor sleep before the lockdown (OR = 2.72; 95% CI = 2.13–3.47, p < 0.001), in those who were taking sleeping pills before the lockdown (OR = 1.86; 95% CI = 1.26–2.73, p = 0.002), for women (OR = 1.39; 95% CI = 1.08–1.79, p = 0.011), individuals aged 18–29 yrs (OR = 1.839; 95% CI = 1.41–2.25, p < 0.001, reference: subjects aged 30–49 yrs), subjects who were extremely scared about the COVID-19 emergency (OR = 2.07; 95% CI = 1.23–3.49, p = 0.006, reference: no fear), and those who felt moderately (OR = 2.08; 95% CI = 1.52–2.83, p < 0.001) and extremely stressed (OR = 4.85; 95% CI = 2.95–7.97, p < 0.001, reference: no stress). Mood was also a significant predictor, with positive mood (reference: neutral mood) showing a protective effect against the risk of experiencing poor sleep quality during the lockdown (OR = 0.62; 95% CI = 0.47–0.82, p < 0.001, and OR = 0.6; 95% CI = 0.25–0.84, p = 0.012, for moderate and extreme positive mood, respectively) and negative mood increasing it (OR = 1.61; 95% CI = 1.20–2.16, p = 0.001, and OR = 1.90; 95% CI = 0.90–3.95, p = 0.091, for moderate and extreme negative mood, respectively).
3.2.2. Belgian sample
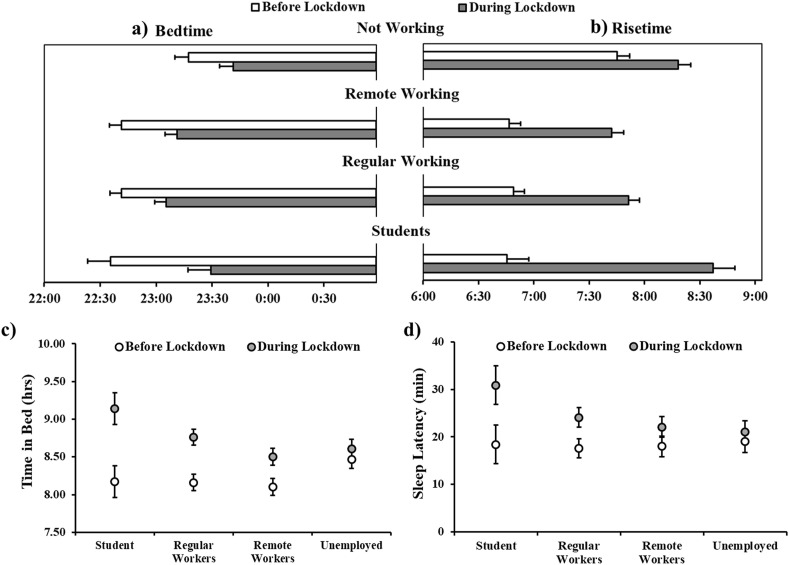
The substantial changes in sleep timing brought about by the lockdown were also observed in the Belgian sample. Participants delayed their bedtimes (F1,642 = 98.03, p < 0.001), an effect which was partially mediated by working status (F3,642 = 2.37, p = 0.070, Fig. 3 a), with students going to bed 54 min later, smart workers ∼30 min later, unemployed/retired subjects and regular workers 24 min later (all p's < 0.001). A significant effect of Gender was observed (F1,641 = 5.01, p = 0.026), with males reporting, in general, later bedtimes than females, although no Lockdown × Gender interaction emerged (F1,642 = 0.26, p = 0.609). Age was a significant covariate (coeff. = −0.01, t = −3.62, p < 0.001), with younger subjects going to bed later. As in the Italian sample, during the lockdown risetime was also delayed (F1,642 = 268.62, p < 0.001), and again this effect was mediated by the working condition (F3,642 = 12.69, p < 0.001, Fig. 3b). Specifically, students got up 1 h and 53 min later, regular workers 1 h and 2 min later, smart workers 56 min later, and unemployed/retired subjects ∼34 min later (all p's < 0.001). We did not observe a significant effect of Gender (F1,642 = 2.00, p = 0.157) but Age was again a significant covariate (coeff. = −0.02, t = −6.75, p < 0.001) with younger participants getting up later.
Fig. 3.
a) Bedtime b) Waketime, c) Time in Bed, and d) Sleep Latency as a function of the presence of the lockdown and the working condition of the participants in the Belgian sample. Error bars represent standard errors of the means.
As expected, a significant delay of sleep midpoint during the quarantine was also found (F1,642 = 242.92, p < 0.001), with differences linked to the working status (Lockdown × Work: F3,641 = 8.88, p < 0.001): the delay was of 1 h and 24 min in students, 48 min in regular and smart workers, 30 min in the unemployed/retired (all p's < 0.001). Age was again a significant covariate (coeff. = −0.02, t = −6.03, p < 0.001): the younger the age, the later the sleep midpoint during the quarantine.
Time spent in bed during the quarantine increased in the Belgian sample by 32 min (F1,642 = 67.23, p < 0.001), with differences depending on the working condition (Lockdown × Work: F3,642 = 6.72, p < 0.001, Fig. 3c) and gender (Lockdown × Gender: F1,642 = 3.85, p = 0.050). Compared to before the lockdown, unemployed/retired participants spent in bed only 9 min more (p > 0.99), smart workers ∼24 min more (p = 0.004), regular workers 36 min more (p < 0.001), whereas students increased their time in bed up to 59 min (p < 0.001). Before the lockdown males tended to spend less time in bed than females (p = 0.064) and this difference increased during the confinement (p < 0.001). Age was a significant covariate (coeff. = −0.01, t = −2.54, p = 0.011), with younger subjects spending more time in bed.
Sleep duration increased by 19 min during the lockdown (F1,642 = 20.87, p < 0.001). While there was a significant main effect of Gender (F1,641 = 5.27, p = 0.022), with females sleeping 17 min more than males, the Lockdown × Gender interaction was not significant (F1,641 = 1.37, p = 0.242). Although the Lockdown × Work interaction was not significant (F3,642 = 2.30, p = 0.076), we observed an increased sleep duration in regular workers (23 min; p = 0.011). Age was again a significant covariate (coeff. = −0.01, t = −3.08, p = 0.002) with younger participants spending more time asleep during the quarantine.
Sleep latency also increased by 6.5 min (F1,642 = 23.24, p < 0.001) during the lockdown, an effect which was partially mediated by the working condition (Lockdown × Work: F3,642 = 2.25, p = 0.081, Fig. 3d). It appeared significantly increased in regular workers (6.3 min, p = 0.044) and students (12.6 min, p = 0.032), but not in the other working status categories (all p's > 0.99). Age was again a significant covariate (coeff. = −0.17, t = −2.66, p = 0.008), with longer sleep latencies in younger individuals.
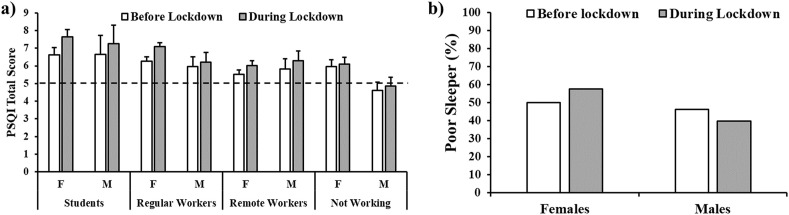
Similarly to Italians, Belgians also displayed decreased sleep quality (indexed by the PSQI total score) during lockdown (F1,642=7.10, p = 0.008). The main effect of working status was observed (F3,641=3.00, p = 0.024), with nominally lower sleep quality in students and regular workers compared to unemployed/retired subjects (both p's = 0.063), though the interaction Lockdown × Work was not significant (F3,642 = 0.40, p = 0.752). Gender was not a significant main effect (F1,641 = 1.82, p = 0.178) and Age was not a significant covariate (F1,641 = 1.92, p = 0.166). The proportion of poor sleepers (ie, PSQI>5) increased from 49.08% to 53.7% during the quarantine (χ2 1 = 103.7, p < 0.001) but this change appeared mainly driven by the female participants. In fact, while male poor sleepers decreased from 46.10% to 39.72%, female poor sleepers increased from 49.90% to 57.56% (Fig. 4 b).
Fig. 4.
a) Pittsburgh Sleep Quality Index (PSQI) total score before and during lockdown as a function of gender and working conditions in the Belgian sample. Error bars represent standard error of the means. The dashed line represents the cut-off for good and poor sleepers. b) Frequency of females and males poor sleepers (PSQI >5) before and during the lockdown in the Belgian sample.
Lastly, the proportion of responders who used sleeping pills, as assessed by the PSQI, decreased from 25.4% to 24.2%.
Logistic regressions (χ2(15) = 214, p < 0.001. McFadden's R2 = 0.250) confirmed that the risk of poor sleep during the quarantine was higher for subjects already reporting poor sleep before the lockdown (OR = 4.11; 95% CI = 2.74–6.16, p < 0.001), in those who were taking sleeping pills before the lockdown (OR = 3.01; 95% CI = 1.81–4.99, p < 0.001), for women (OR = 1.99; 95% CI = 1.21–3.28, p = 0.007), and for participants who felt extremely stressed (OR = 2.34; 95% CI = 1.26–4.35, p = 0.007, reference: no stress). Mood was again a significant predictor, with extremely positive mood (reference: neutral mood) bearing a protective effect against the risk of poor sleep quality during the lockdown (OR = 0.47; 95% CI = 0.26–0.86, p = 0.015), and extremely negative mood increasing its risk (OR = 7.79; 95% CI = 2.14–28.30, p = 0.002).
4. Discussion
In the current study, we aimed to investigate how the period of home confinement imposed by governments to contain the spread of the COVID-19 epidemic in two European countries, Italy and Belgium, affected people's self-reported sleep characteristics, with special regard to sleep timing and subjective quality. Of note, to the best of our knowledge, this is the first report of sleep changes during the lockdown in a Belgian sample. As hypothesized, the two countries showed a similar pattern of changes in the main variables of interest after the introduction of COVID-19-related restrictions: sleep timing was significantly delayed during the lockdown, time spent in bed increased, and sleep quality was markedly impaired in both Italy and Belgium. At the same time, these changes differently affected specific subgroups of participants in the two countries.
First of all, in both Italy and Belgium, participants tended to go to bed later than usual during the lockdown. This delay was more pronounced in students, whose bedtime was delayed of about 54 min in both countries, and in males compared to females. Similarly, people tended to wake up later in the morning, and again in both countries students were the ones showing the most pronounced delay (1 h and 40 min and 1 h and 52 min in the Italian and Belgian sample, respectively). Overall, the shift in sleep midpoint was similar in the two countries, ie, ∼1 h and 1 min and ∼54 min in the Italian and Belgian samples, respectively. Italy and Belgium also showed a similar increase of time spent in bed with the lockdown, ie ∼33 min in the Italian sample and ∼32 min in the Belgian sample.
However, the longer time spent in bed was not accompanied by a corresponding increase in sleep duration in either sample, indicating a decrease in sleep efficiency. In line with this, in both countries subjective sleep quality was significantly impaired, with an increased proportion of poor sleepers (especially females) compared to before the quarantine. This worsening of sleep quality was also reflected in an increased perception of difficulties falling asleep, suggested by the significant increase in self-reported sleep latency. Possibly sleep continuity and stability were also impaired, ie, through increased awakening and arousal frequency [24], although we cannot draw firm conclusions from our data.
Several factors may have played a role in determining the worsening of subjective sleep quality during the period of home confinement. First of all, as suggested by the results of our regressions, showing, in both countries, an increased risk of poor sleep in subjects with higher negative mood and stress, psychological factors related to the COVID-19 crisis have likely had a significant impact on sleep quality and timing [5,25,26]. Second, the changes in daily routines, including working from home and the lack of social activities, have probably contributed to the sleep quality impairments [27,28], either directly or indirectly by affecting mood and stress. Also, the changes in daily habits could have included an increase of daytime naps, which might have resulted, for homeostatic reasons, in decreased sleep pressure at bedtime, on its turn responsible for longer sleep latency and greater sleep fragmentation.
Unsurprisingly, our data show that, both in Italy and Belgium, subjects already experiencing poor sleep quality before the lockdown were at higher risk of being classified as poor sleepers during the lockdown as well. Furthermore, consistent with what predicted by the task force of the European CBT-I Academy [5], women appeared more vulnerable to remaining or becoming poor sleepers during home confinement in both countries. This is likely due to the higher prevalence of insomnia in this population [5], to the “gender gap” in childcare [29] and eldercare [30], and to wages gap, although the latter is quite limited in Belgium [31].
Overall, our data are in line with previous studies on the impact of the pandemic-related restrictive measures on sleep quality in Italy [[8], [9], [10],15,16] and other European countries [7,13,17], as well as in Chinese [11,18], Australian [17], and US samples [19], suggesting that the negative effect of confinement on perceived sleep quality was not specific of a single region, but can be generalized to most of the industrialized countries. Moreover, our data confirm, and extend to Belgium, the marked shift in sleep timing observed during the lockdown in countries with a very different culture, latitude, and longitude such as Italy [9], Austria, Germany and Switzerland [20], and the US [19].
Despite the striking similarities in the lockdown-related sleep changes affecting the two samples as a whole, the two countries differed in the most affected subgroups. In fact, in the Italian sample sleep quality and timing underwent significant modifications especially in unemployed participants, whereas in the Belgian sample this category was the one who suffered less from the restrictions. This difference may be due to the different welfare of the two countries, and to the general income of the population. In the last decades, Belgium has placed a robust and redistributive welfare system (despite its complexity), centered on minimum income protection as well as on social risk such as long term unemployment financial aids [32]. Belgian unemployed individuals have a relatively good protection level, characterized by long-lasting income benefits and unemployment insurance with an initial replacement rate of 60% with no time limit [33]. In Italy, instead, although the welfare system is also quite complex and specific economic measures have been implemented during the lockdown [34], it has been estimated that losses for the lower socioeconomic classes and wage inequality increased during this period more than in Belgium. Although it is unlikely that the general population was aware of these estimations, people in both countries likely had a different perception of health- and economic-related risks. Indeed, Italian participants, compared to the Belgian, reported more frequently a negative mood, more fear about the COVID-19 situation, and a higher proportion of the sample reported to be worried about dear ones and economic issues.
Our results should be considered in light of methodological constraints linked to the nature of survey studies: for instance, we cannot exclude that responses were biased by recall accuracy of respondents or that the questionnaire might have preferentially attracted responders with pre-existing sleep complaints [35]. Nevertheless, it has been recently shown that data elicited by retrospective questions are quite consistent [36]. Moreover, this methodology allowed for the major asset of this study, which is the collection of the same data from quite large samples in two different countries. Our findings clearly showed that the changes in sleep timing and quality described during the lockdown in several countries are related to the restrictions imposed by governments to face the COVID-19 crisis. Indeed, in both Italy and Belgium, we observed longer time spent in bed, delay in sleep timing, and worsening of sleep quality.
Furthermore, in our investigation we have adopted a special focus on factors affecting the risk of developing or worsening sleep complaints as adverse consequences of pandemic-related restrictions, highlighting a particular vulnerability for women, subjects experiencing a more negative mood, and those perceiving the situation as highly stressful. This kind of analysis, which sheds only a partial light on a complex scenario, opens the way to further studies addressing other possible modulating variables (both risk and protective factors, eg, the use of pharmacological and/or behavioral treatments for sleep quality, the presence of different pre-existing psychopathologies or personality traits, the influence of chronotype or of different social roles such as being a health care professional, etc.), to build an increasingly clearer picture of the complex effects of global health emergencies on sleep health.
In particular, in the current study, we were not able to investigate the sleep-wake pattern in specific workers, such as healthcare professionals. This working category is at high risk for poor sleep and insomnia [37,38]. As shown by Ferini-Strambi and colleagues (2020), about 35% of Italian healthcare staff (eg, physicians, nurses) reported sleep disturbances at the subjective (ie, PSQI) and objective (ie, actigraphy) level. The reduced sleep quality in this population is alarming since it can increase the susceptibility of medical staff to COVID-19 infection, therefore increase the probability of infection outbreak, and can negatively affect mental health in a population already under high stress [39].
Another point, not addressed in the current study, is the characterization of sleep during quarantine in individuals suffering from psychiatric disorders (eg, anxiety, depression, psychosis). Indeed, considering that there is a tight relationship between sleep and psychiatric disorders [40], investigating the change in sleep pattern during a quarantine may be of primary importance to improve mental healthcare.
Another important point, not addressed in the current study, is how sleep quality changed across the confinement period. Indeed, as shown by Salfi and colleagues [16], sleep quality seems to remain low across the lockdown, although males tend to show a reduction of sleep quality over time. In the current study we could not replicate the same analysis since 88.1% of the Italian sample (N = 1429) completed the survey in the first week of data collection (31st of March - sixth of April), while only 11.9% of the data (N = 193) have been collected in the period between the seventh to the 21st of April. Similarly, in the Belgian sample, we collected 74.6% of the data (N = 485) in the first week of data collection (8th – 14th of April), while only 25.4% of the data (N = 165) have been collected in the period between the 15th of April to the 19th of May. Therefore, a direct comparison of our data between these two periods could not be done due to the large differences in sample size. Nevertheless, our sleep quality and timing data are consistent with the findings of our previous study in young adults [9], where data were collected during the third week of the Italian lockdown (24th to 28th of March).
Overall, the differences we observed in the current study between countries in the subgroups most vulnerable to sleep quality impairments point to the importance of welfare systems in impacting risk perception, possibly through the development of different narratives of the COVID-19 emergency in the two countries [41]. Specifically, the protective role of a well-functioning welfare system requires further attention. Considering that the novel coronavirus has spread across the whole globe, involving countries with different types of health and welfare systems, understanding which policy measures have the most effective protective role on physical and mental health is of primary importance. Moreover, in light of the new increases in the spread of contagion, politicians, clinicians, and researchers should be ready to propose adequate interventions to reduce the physical and psychological burden of this unprecedented situation, especially for the most vulnerable individuals.
CRediT authorship contribution statement
Nicola Cellini: Conceptualization, Methodology, Formal analysis, Writing - original draft, Visualization, Data curation. Francesca Conte: Conceptualization, Investigation, Methodology, Writing - original draft. Oreste De Rosa: Investigation, Methodology, Writing - review & editing. Fiorenza Giganti: Conceptualization, Methodology, Writing - review & editing, Supervision. Serena Malloggi: Investigation, Writing - review & editing. Mathilde Reyt: Investigation, Writing - review & editing. Camille Guillemin: Investigation, Writing - review & editing. Christina Schmidt: Conceptualization, Methodology, Writing - review & editing. Vincenzo Muto: Conceptualization, Methodology, Writing - original draft, Data curation, Supervision. Gianluca Ficca: Conceptualization, Methodology, Writing - original draft, Data curation, Supervision.
Acknowledgment
MR and VM are supported by a European Research Council starting grant (CS; ERC-StG 757763). CS is a research associate at the Belgian National Funds for Scientific Research. The present work was carried out in the scope of the research program “Dipartimenti di Eccellenza” from MIUR to the Department of General Psychology of the University of Padova.
Footnotes
The Authors declare that there is no conflict of interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2020.11.027.
Conflict of interest
The following are the supplementary data related to this article:
The Authors declare that there is no conflict of interest.
References
- 1.Istituto Superiore di Sanità . 2020. Comunicato stampa N°19/2020. Studio ISS. Un paziente su cinque positivo al coronavirus ha tra 19 e 50 anni.https://www.iss.it/comunicati-stampa1 March 9, 2020) Retrieved March 30, 2020 from. [Google Scholar]
- 2.Mazza C., Ricci E., Biondi S., et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Publ Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2020. Mental health and psychosocial considerations during the COVID-19 outbreak. (No. WHO/2019-nCoV/MentalHealth/2020.1)https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf?sequence=1&isAllowed=y Retrieved 27 March 2020 from. [Google Scholar]
- 5.Altena E., Baglioni C., Espie C.A., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29(4) doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 6.Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Voitsidis P., Gliatas I., Bairachtari V., et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatr Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casagrande M., Favieri F., Tambelli R., et al. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cellini N., Canale N., Mioni G., et al. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franceschini C., Musetti A., Zenesini C., et al. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Front Psychol. 2020;11:574475. doi: 10.3389/fpsyg.2020.574475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Innocenti P., Puzella A., Mogavero M.P., et al. Letter to editor: CoVID-19 pandemic and sleep disorders—a web survey in Italy. Neurol Sci. 2020;41(8):2021–2022. doi: 10.1007/s10072-020-04523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kokou-Kpolou C.K., Megalakaki O., Laimou D., et al. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in France population. Psychiatr Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandelkorn U., Genzer S., Choshen-Hillel S., et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med JCSM. 2020 doi: 10.5664/jcsm.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marelli S., Castelnuovo A., Somma A., et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2020 doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salfi F., Lauriola M., Amicucci G., et al. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol Stress. 2020;13:100259. doi: 10.1016/j.ynstr.2020.100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stanton R., To Q., Khalesi S., et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Publ Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao H., Zhang Y., Kong D., et al. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Mon Int Med J Exp Clin Res Int Med J Exp Clin Res. 2020;26:e923921. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wright K.P., Linton S.K., Withrow D., et al. Sleep in university students prior to and during COVID-19 stay-at-home orders. Curr Biol. 2020;30(14):R797–R798. doi: 10.1016/j.cub.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blume C., Schmidt M.H., Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr Biol. 2020;30(14):795–R797. doi: 10.1016/j.cub.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Giorgio E., Di Riso D., Mioni G., et al. European Child and Adolescent Psychiatry; 2020. The interplay between mothers' and children behavioral and psychological factors during COVID-19: an Italian study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buysse D.J., Reynolds C.F., III, Monk T.H., et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 23.Baayen R.H., Davidson D.J., Bates D.M. Mixed-effects modeling with crossed random effects for subjects and items. J Mem Lang. 2008;59(4):390–412. [Google Scholar]
- 24.Conte F., Cerasuolo M., Fusco G., et al. Sleep continuity, stability and organization in good and bad sleepers. J Health Psychol. 2020 doi: 10.1177/1359105320903098. [DOI] [PubMed] [Google Scholar]
- 25.Alvaro P.K., Roberts R.M., Harris J.K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coles M.E., Schubert J.R., Nota J.A. Sleep, circadian rhythms, and anxious traits. Curr Psychiatr Rep. 2015;17(9):73. doi: 10.1007/s11920-015-0613-x. [DOI] [PubMed] [Google Scholar]
- 27.Carney C.E., Edinger J.D., Meyer B., et al. Daily activities and sleep quality in college students. Chronobiol Int. 2006;23(3):623–637. doi: 10.1080/07420520600650695. [DOI] [PubMed] [Google Scholar]
- 28.Monk T.H., Petrie S.R., Hayes A.J., et al. Regularity of daily life in relation to personality, age, gender, sleep quality and circadian rhythms. J Sleep Res. 1994;3(4):196–205. doi: 10.1111/j.1365-2869.1994.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 29.Craig L., Mullan K. How mothers and fathers share childcare: a cross-national time-use comparison. Am Socio Rev. 2011;76(6):834–861. [Google Scholar]
- 30.Brenna E., Di Novi C. Is caring for older parents detrimental to women's mental health? The role of the European North–South gradient. Rev Econ Househ. 2016;14(4):745–778. [Google Scholar]
- 31.Boll C., Lagemann A. vol. 10. Publication Office of the European Union; Luxembourg: 2018. Gender pay gap in EU countries based on SES (2014) p. 978935. [Google Scholar]
- 32.Marx I., Schuerman N. Challenges to European welfare systems. Springer; 2016. Belgium, or how inertia can have unexpected benefits in times of crisis; pp. 37–57. [Google Scholar]
- 33.Mariña F.S., Figari F., Sutherland H., et al. 2012. Welfare compensation for unemployment in the great recession. [Google Scholar]
- 34.Figari F., Fiorio C.V. Welfare resilience in the immediate aftermath of the covid-19 outbreak in Italy. EUROMOD at the Institute for Social and Economic Research. Tech Rep. 2020 [Google Scholar]
- 35.Jones T., Baxter M., Khanduja V. A quick guide to survey research. Ann R Coll Surg Engl. 2013;95(1):5–7. doi: 10.1308/003588413X13511609956372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hipp L., Bünning M., Munnes S., et al. Problems and pitfalls of retrospective survey questions in COVID-19 studies. Survey Res Methods. 2020;14:109–114. [Google Scholar]
- 37.Chokroverty S. The many faces and fangs of COVID-19: an editorial. Sleep Med. 2020;72:164–166. doi: 10.1016/j.sleep.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferini-Strambi L., Zucconi M., Casoni F., et al. COVID-19 and sleep in medical staff: reflections, clinical evidences, and perspectives. Curr Treat Options Neurol. 2020;22(10):1–6. doi: 10.1007/s11940-020-00642-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maunder R.G., Lancee W.J., Balderson K.E., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Freeman D., Sheaves B., Waite F., et al. Sleep disturbance and psychiatric disorders. Lancet Psychiatr. 2020;7(7):628–637. doi: 10.1016/S2215-0366(20)30136-X. [DOI] [PubMed] [Google Scholar]
- 41.Olagoke A.A., Olagoke O.O., Hughes A.M. Exposure to coronavirus news on mainstream media: the role of risk perceptions and depression. Br J Health Psychol. 2020;25(4):865–874. doi: 10.1111/bjhp.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.